Professional Documents
Culture Documents
Dental Press Endo Don Tics L
Dental Press Endo Don Tics L
Uploaded by
Doina BarcaruOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dental Press Endo Don Tics L
Dental Press Endo Don Tics L
Uploaded by
Doina BarcaruCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/273765129
Differential diagnosis of non-odontogenic sinusitis
Article · May 2014
DOI: 10.14436/2178-3713.4.2.069-073.oar
CITATIONS READS
0 533
5 authors, including:
Jose Burgos Bruno Martini Guimarães
University of São Paulo INAPÓS - Dental School
25 PUBLICATIONS 17 CITATIONS 46 PUBLICATIONS 300 CITATIONS
SEE PROFILE SEE PROFILE
Lidiane Pinto Ana Lúcia Pompéia Fraga de Almeida
University of São Paulo University of São Paulo
12 PUBLICATIONS 53 CITATIONS 78 PUBLICATIONS 575 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Periodontal Disease in cleft lip and palate individuals View project
Microthomography evaluation of the efficacy of reciprocating and rotary instruments followed by different complementary steps in the retreatment of curved root canals
View project
All content following this page was uploaded by Bruno Martini Guimarães on 19 March 2015.
The user has requested enhancement of the downloaded file.
original article
Differential diagnosis of
non-odontogenic sinusitis
José Burgos PONCE1
Bruno Martini GUIMARÃES2
Lidiane de Castro PINTO3
Celso Kenji NISHIYAMA3
Ana Lucia Pompeia Fraga de ALMEIDA4
doi: http://dx.doi.org/10.1590/2178-3713.4.2.069-073.oar
ABSTRACT achieved by means of cone-beam computed tomogra-
phy. The correct use of radiological evaluation associat-
The close relationship between maxillary posterior teeth ed with clinical findings is crucial for the diagnosis of si-
dental roots and pneumatic cavities poses difficulties in nusitis and can avoid unnecessary treatment procedures.
the clinical diagnosis of pathologies in this area. This ar-
ticle reports a differential diagnosis of non-odontogenic
sinusitis in the region of molars with an intimate rela- Keywords: Cone-beam computed tomography. Diagnosis.
tionship with the maxillary sinus mucosa. Diagnosis was Sinusitis.
How to cite this article: Ponce JB, Guimarães BM, Pinto LC, Nishiyama CK, Almeida » The authors report no commercial, proprietary or financial interest in the prod-
ALPF. Differential diagnosis of non-odontogenic sinusitis. Dental Press Endod. 2014 ucts or companies described in this article.
May-Aug;4(2):69-73. DOI: http://dx.doi.org/10.1590/2178-3713.4.2.069-073.oar
» Patients displayed in this article previously approved the use of their facial and
intraoral photographs.
1
PhD resident in Pathology, School of Dentistry — Bauru/USP.
2
PhD resident in Endodontics, School of Dentistry — Bauru/USP.
Submitted: January 26, 2014. Revised and accepted: March 28, 2014.
3
Professor, Department of Endodontics, Hospital for Rehabilitation of Craniofacial Anomalies/
USP.
Contact address: Bruno Martini Guimarães
4
Professor, Department of Prosthesis, School of Dentistry — Bauru/USP. Departamento de Endodontia - Al. Octávio Pinheiro Brisola, 9-75
Bauru - SP - Brazil - 17012-901 - E-mail: brunomgui@usp.br
© 2014 Dental Press Endodontics 69 Dental Press Endod. 2014 May-Aug;4(2):69-73
[ original article ] Differential diagnosis of non-odontogenic sinusitis
Introduction Case report
In the paranasal sinuses, maxillary teeth are the first A female patient attended the Department of End-
to emerge. Their growth is directly related to the de- odontics at the Hospital for Rehabilitation of Cranio-
velopment and eruption of upper molars which do not facial Anomalies/USP with chief complaint of pain
achieve full size until permanent dentition. A close re- in the region of upper molars. After the first interview
lationship is established between the roots of maxillary and clinical examination, a periapical radiograph was
teeth, from canine to upper molars, and the sinus floor. obtained (Fig 1). The patient had previously sought
These structures are separated by a thin layer of bone an otorhinolaryngologist who assessed her case by
which is often represented by a mucous membrane. means of orthopantomographic and lateral radio-
Knowing the distance between the maxillary si- graphs without finding any alterations.
nus floor and the apices of maxillary posterior teeth Teeth #24 and 25 had undergone satisfactory end-
is of paramount importance for both surgical and odontic treatment without pain at percussion. Teeth
non-surgical endodontic procedures, particularly #26 and 27, however, had no endodontic treatment
due to the risk of penetration into the lower recess and tested positive for sensitivity. The presence of
of the sinus. Measurements demonstrate a longer restorations on teeth #26 and 27, associated with
distance between the sinus and the roots of premo- the intimate relationship between dental roots and
lars in comparison to the roots of molars, with varia- the maxillary sinus cavity was indicative of a change
tions of existing bone thickness in different roots.1 at that level. For this reason, patient’s existing CBCT,
The close relationship established between the which had been taken at the Department of Radiolo-
roots of maxillary posterior teeth and the pneumatic gy of the Hospital for Rehabilitation of Craniofacial
cavities poses difficulties in the clinical diagnosis of Anomalies/USP for previous orthognathic surgery
pathologies in this area.2 A total of 10% to 86% of follow-up, was then analyzed.
pathologies in this area are of odontogenic origin, 3,4 CBCT analysis revealed thickening of the maxil-
and nearly 70% of individuals with odontogenic im- lary sinus mucosa, a condition that might be consid-
pairments in maxillary posterior teeth have altera- ered as sinusitis (Figs 2A, and 2C). CBCT also high-
tions in the maxillary sinus.3 lighted the close relationship established between
The high incidence of maxillary sinusitis result- the apices of upper left premolars and molars and
ing from odontogenic infection should be taken into the maxillary sinus (Fig 3). Following the diagnostic
account during diagnosis5 so as to properly deter- criteria for sinusitis established by Maillet et al,2 we
mine the cause of the disease and to avoid subject- concluded that it was a case of non-odontogenic si-
ing patients with sinusitis to long and unnecessary nusitis. The patient was then referred to the otorhi-
surgical procedures.4,5 nolaryngologist with a copy of the CBCT scan.
Cone-beam computed tomography (CBCT) has Two months later, the patient returned to the De-
been recently introduced into dento-maxillo-facial partment of Endodontics of the Hospital for Reha-
imaging and diagnosis as an alternative to conven- bilitation of Craniofacial Anomalies/USP. She was
tional tomography (CT). It offers advantages such then resubmitted to CBCT which revealed regres-
as lower radiation dose and significant features in sion of inflammation in the sinus mucosa and ab-
comparison to conventional radiography.5,6 sence of painful symptomatology (Fig 2B, 2D).
The objective of this research is to guide dentists
and endodontists with regard to the correct diagno- Discussion
sis of odontogenic sinusitis by means of reporting a The present study reports a case of differential
clinical case conducted at the Hospital for Rehabili- diagnosis of non-odontogenic sinusitis in the region
tation of Craniofacial Anomalies/USP. of upper molars with intimate relationship with the
© 2014 Dental Press Endodontics 70 Dental Press Endod. 2014 May-Aug;4(2):69-73
Ponce JB, Guimarães BM, Pinto LC, Nishiyama CK, Almeida ALPF
Figure 1. Periapical region of right upper teeth.
A B
Figure 2. Axial scans of the relationship be-
tween posterior teeth and maxillary sinus:
A) Initial CBCT; B) Control CBCT after medical
treatment. Coronal scans of the relationship
between posterior teeth and maxillary sinus:
C) Initial CBCT highlighting right maxillary sinus
anterior extension filled with mucosal inflamma-
C D tion; D) Control CBCT after medical treatment.
© 2014 Dental Press Endodontics 71 Dental Press Endod. 2014 May-Aug;4(2):69-73
[ original article ] Differential diagnosis of non-odontogenic sinusitis
Plane
Figure 3. A) Initial CBCT scan (voxel: 0.4 mm)
B) Follow-up CBCT scan two months after
A B medical treatment (voxel: 0.2 mm).
maxillary sinus mucosa. The average distance from CBCT is a useful tool used in the differential di-
molars and premolars to the maxillary sinus floor agnosis of non-endodontic pathologies.2,7 Voxel size
ranges from 0.83 mm in the buccal roots of the sec- plays an important role in tomographic diagnosis.
ond molar to 7.05 mm in the roots of the first pre- Studies demonstrate that the smaller the voxel size,
molar.1 This close relationship requires that we con- the better the results yielded by observation of ana-
duct a detailed survey to assess the communication tomical and endodontic pathologies.8,9 In this study,
between the aforementioned anatomical structures. initial CBCT scan was conducted with a voxel size
Importantly, canines and posterior teeth with odon- of 0.4 mm and a field of view (FOV) of 22 cm as a
togenic infection can cause changes in the maxillary follow-up approach for orthognathic surgery. The sec-
sinus mucosa in approximately 70% of cases.3 ond CBCT scan was requested by the Department of
Pulp sensitivity tests revealed vital molars and as- Endodontics of the Hospital for Rehabilitation of
ymptomatic premolars. Additionally, periapical radio- Craniofacial Anomalies/USP, with a voxel of 0.2 mm
graph revealed satisfactory endodontic treatment in and 6 cm FOV, since the field of observation was only
premolars, and no evident radiographic changes on in the upper jaw, only. The differences between voxel
molars. CBCT proved an essential tool not only in de- size in both CT scans are shown in Figure 3.
termining inflammation of the sinus mucosa, but also Panoramic and bitewing radiographs do not prove
in reaching the diagnosis of sinusitis. These findings to be a reliable alternative for the differential diag-
were associated with the diagnostic criteria advocated nosis of maxillary sinusitis, as they do not estimate
by Maillet et al,2 and disregarded odontogenic sinusitis. the amount of bone loss. Furthermore, periapical
The patient was then referred to an otolaryngologist. radiograph routinely used for endodontic diagnosis
© 2014 Dental Press Endodontics 72 Dental Press Endod. 2014 May-Aug;4(2):69-73
Ponce JB, Guimarães BM, Pinto LC, Nishiyama CK, Almeida ALPF
also have major limitations, since it cannot diagnose Furthermore, it also reaches diagnosis of periapical
oro-antral communication.5 pathologies with greater accuracy in comparison to
Careful analysis of maxillary sinuses by means digital periapical radiographs, as demonstrated by
of CT scans might be a more sensitive tool to de- Lofthag-Hansen et al.10
tect potential causes of sinusitis.4 CBCT was spe-
cifically designed for imaging of the head and neck. Conclusion
Nevertheless, it has proved particularly useful in the The correct use of radiological evaluation asso-
different aspects of endodontic treatment.6,7,10 ciated with clinical findings is crucial for the diagno-
The lower radiation dose emitted by CBCT is anoth- sis of sinusitis and can avoid unnecessary treatment
er interesting advantage over conventional CT scans.7 procedures.
References
1. Eberhardt JA, Torabinejad M, Christiansen EL. A computed 7. Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG.
tomographic study of the distances between the maxillary sinus floor Endodontic applications of cone-beam volumetric tomography.
and the apices of the maxillary posterior teeth. Oral Surg Oral Med J Endod. 2007;33(9):1121-32.
Oral Pathol Oral Radiol Endod. 1992;73(3):345-6. 8. Liedke GS, Silveira HE, Silveira HL, Dutra V, Figueiredo JA.
2. Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M. Influence of voxel size in the diagnostic ability of cone beam
Cone-beam computed tomography evaluation of maxillary sinusitis. tomography to evaluate simulated external root resorption. J Endod.
J Endod. 2011;37(6):753-7. 2009;35(2):233-5.
3. Obayashi N, Ariji Y, Goto M, Izumi M, Naitoh M, Kurita K, et al. 9. Wenzel A, Haiter-Neto F, Frydenberg M, Kirkevang LL. Variable-
Spread of odontogenic infection originating in the maxillary teeth: resolution cone-beam computerized tomography with enhancement
computerized tomographic assessment. Oral Surg Oral Med Oral filtration compared with intraoral photostimulable phosphor
Pathol Oral Radiol Endod. 2004;98(2):223-31. radiography in detection of transverse root fractures in an in
4. Longhini AB, Branstetter BF, Ferguson BJ. Unrecognized vitro model. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
odontogenic maxillary sinusitis: a cause of endoscopic sinus surgery 2009;108(6):939-45.
failure. Am J Rhinol Allergy. 2010;24(4):296-300. 10. Lofthag-Hansen S, Huumonen S, Grondahl K, Grondahl HG.
5. Nair UP, Nair MK. Maxillary sinusitis of odontogenic origin: cone- Limited cone-beam CT and intraoral radiography for the diagnosis
beam volumetric computerized tomography-aided diagnosis. Oral of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol
Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110(6):e53-7. Endod. 2007;103(1):114-9.
6. Patel S. New dimensions in endodontic imaging: Part 2. Cone beam
computed tomography. Int Endod J. 2009;42(6):463-75.
© 2014 Dental Press Endodontics 73 Dental Press Endod. 2014 May-Aug;4(2):69-73
View publication stats
You might also like
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- CBT For DepressionDocument50 pagesCBT For Depressionmeditation timeNo ratings yet
- Hard Gainer - Issue 61 - July 1999Document50 pagesHard Gainer - Issue 61 - July 1999api-3701884100% (7)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Mtu Sales ProgramDocument36 pagesMtu Sales ProgrammajdirossrossNo ratings yet
- Efecto Del Uso de Semilla de Chía (Salvia Hispánica L.) en La Elaboración de Mermelada de Fresa (Fragaria Ananassa Duch.) Como Agente GelificanteDocument7 pagesEfecto Del Uso de Semilla de Chía (Salvia Hispánica L.) en La Elaboración de Mermelada de Fresa (Fragaria Ananassa Duch.) Como Agente GelificanteLuis TasaycoNo ratings yet
- Trimetazidine Drug StudyDocument2 pagesTrimetazidine Drug StudyJULIANNE BAYHON100% (1)
- Tratamentul Chisturilor OdontDocument1 pageTratamentul Chisturilor OdontDoina BarcaruNo ratings yet
- Arhe32 PDFDocument5 pagesArhe32 PDFDoina BarcaruNo ratings yet
- Immunotherapy in Allergic Fungal Sinusitis: The Controversy Continues. A Recent Review of LiteratureDocument5 pagesImmunotherapy in Allergic Fungal Sinusitis: The Controversy Continues. A Recent Review of LiteratureDoina BarcaruNo ratings yet
- Referat:: '' Teoria Probabilitatilor Legea Cifrelor Mari''Document8 pagesReferat:: '' Teoria Probabilitatilor Legea Cifrelor Mari''Doina BarcaruNo ratings yet
- Knauf Insulation GMBH Material Safety Data Sheet: Section I - Chemical Product and Company IdentificationDocument4 pagesKnauf Insulation GMBH Material Safety Data Sheet: Section I - Chemical Product and Company IdentificationUMUTNo ratings yet
- Pengelolaan SampahDocument9 pagesPengelolaan SampaharikaNo ratings yet
- Electricity 1Document9 pagesElectricity 1okguserfucker idontgiveashitNo ratings yet
- Heart Failure Care Plan LippincottDocument62 pagesHeart Failure Care Plan LippincottDyllano100% (1)
- Oil Stability A DSC Alternative For The Active Oxygen MethodDocument2 pagesOil Stability A DSC Alternative For The Active Oxygen MethodTaty mignon princeNo ratings yet
- Eng 11 Unit 8 Become IndependentDocument9 pagesEng 11 Unit 8 Become IndependentLương Quang HiệuNo ratings yet
- IRC Bangladesh Annual Report 2023Document42 pagesIRC Bangladesh Annual Report 2023TasbirNo ratings yet
- OncologyDocument67 pagesOncologyCarlos HernándezNo ratings yet
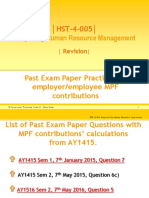
- Answers For MPF QuestionsDocument6 pagesAnswers For MPF QuestionsJack bandannaNo ratings yet
- Activity 1 Rizal Gomburza ExcerptDocument2 pagesActivity 1 Rizal Gomburza ExcerptHyacinth GulbenNo ratings yet
- Analysis of Rate For Providing/Fixing of Single Lights: Amount of 44 Pole 3% ContigencyDocument2 pagesAnalysis of Rate For Providing/Fixing of Single Lights: Amount of 44 Pole 3% Contigencymuhammad iqbalNo ratings yet
- 887 1551 2 PBDocument7 pages887 1551 2 PBAliyah SajaNo ratings yet
- A - Nahm27,+581 1746 4 EDDocument10 pagesA - Nahm27,+581 1746 4 EDistiqamahNo ratings yet
- UZIN Plaster: Safety Data Sheet Wall PlasteringDocument2 pagesUZIN Plaster: Safety Data Sheet Wall PlasteringMon ToonNo ratings yet
- Product CatalogDocument144 pagesProduct CatalogAndre KweeNo ratings yet
- NCM 103 TheoristsDocument9 pagesNCM 103 Theoristskwgchyrn1No ratings yet
- Dewani QuoteDocument2 pagesDewani QuoteAhmed NallaNo ratings yet
- Single Stage Centrifugal Pumps EN 733 (NFE 44111), ISO 5199: Heating - Air Conditioning Industry - AgricultureDocument40 pagesSingle Stage Centrifugal Pumps EN 733 (NFE 44111), ISO 5199: Heating - Air Conditioning Industry - AgriculturePatricia J ÁngelesNo ratings yet
- DaburDocument27 pagesDaburKeshav KalaniNo ratings yet
- Warning: Komatsu PC210-11/PC240-11/PC290-11 and PC360-11/ PC390-11/PC490-11 Excavator Installation InstructionsDocument52 pagesWarning: Komatsu PC210-11/PC240-11/PC290-11 and PC360-11/ PC390-11/PC490-11 Excavator Installation InstructionsTran Trong PhuNo ratings yet
- Nursing Home Private Hospital / ICU Nursing Chart: 6 HR 18 HRDocument2 pagesNursing Home Private Hospital / ICU Nursing Chart: 6 HR 18 HRdavidNo ratings yet
- Soal Gala Putaran 2 Pertemuan 4Document4 pagesSoal Gala Putaran 2 Pertemuan 4Elisya Ayu RiskiNo ratings yet
- Manual For Quality Seed Production in Wheat.: January 2014Document74 pagesManual For Quality Seed Production in Wheat.: January 2014astuteNo ratings yet
- NTEStarterUnit6 Sample StudentbookDocument10 pagesNTEStarterUnit6 Sample StudentbookKeith BrightNo ratings yet
- Ethics Unit 2Document22 pagesEthics Unit 2SaniNo ratings yet