Professional Documents
Culture Documents
Mandibular Reconstruction With Lateral Tibial Bone Graft: An Excellent Option For Oral and Maxillofacial Surgery
Uploaded by
Dwifitri MaretaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mandibular Reconstruction With Lateral Tibial Bone Graft: An Excellent Option For Oral and Maxillofacial Surgery
Uploaded by
Dwifitri MaretaCopyright:
Available Formats
292 Case Report
Mandibular Reconstruction with Lateral Tibial
Bone Graft: An Excellent Option for Oral and
Maxillofacial Surgery
Ana Lucia Carpi Miceli1 Livia Costa Pereira, DDS1 Thiago da Silva Torres, DDS1
Mônica Diuana Calasans-Maia, DDS, MSc, PhD2 Rafael Seabra Louro, DDS, MSc, PhD1,2
1 Department of Oral and Maxillofacial Surgery, Servidores do Estado Address for correspondence Rafael Seabra Louro, DDS, MSc, PhD,
Federal Hospital, Rio de Janeiro, Rio de Janeiro, Brazil Department of Oral and Maxillofacial Surgery, Servidores do Estado
2 Oral Surgery Department, Dentistry School, Fluminense Federal Federal Hospital, Rua Sacadura Cabral, 178 Rio de Janeiro, Rio de
University, Niterói, Rio de Janeiro Janeiro 20221-903, Brazil (e-mail: rafaelseabra@id.uff.br).
This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited.
Craniomaxillofac Trauma Reconstruction 2017;10:292–298
Abstract Autogenous bone grafts are the gold standard for reconstruction of atrophic jaws, pseu-
doarthroses, alveolar clefts, orthognathic surgery, mandibular discontinuity, and augmenta-
tion of sinus maxillary. Bone graft can be harvested from iliac bone, calvarium, tibial bone, rib,
and intraoral bone. Proximal tibia is a common donor site with few reported problems
compared with other sites. The aim of this study was to evaluate the use of proximal tibia as a
donor area for maxillofacial reconstructions, focusing on quantifying the volume of cancellous
graft harvested by a lateral approach and to assess the complications of this technique. In a
retrospective study, we collected data from 31 patients, 18 women and 13 men (mean age:
36 years, range: 19–64), who were referred to the Department of Oral and Maxillofacial
Surgery at the Servidores do Estado Federal Hospital. Patients were treated for sequelae of
orthognathic surgery, jaw fracture, nonunion, malunion, pathology, and augmentation of
bone volume to oral implant. The technique of choice was lateral access of proximal tibia
metaphysis for graft removal from Gerdy tubercle under general anesthesia. The mean volume
Keywords of bone harvested was 13.0 T 3.7 mL (ranged: 8–23 mL). Only five patients (16%) had minor
► tibia complications, which included superficial infection, pain, suture dehiscence, and unwanted
► cancellous bone graft scar. However, none of these complications decreases the result and resolved completely. We
► complications conclude that proximal tibia metaphysis for harvesting cancellous bone graft provides
► volume bone graft sufficient volume for procedures in oral and maxillofacial surgery with minimal postoperative
► maxillofacial surgery morbidity.
A variety of bone grafting materials, ranging from autologous complications, such as delayed unions, nonunions, mal-
bone to bone graft substitutes, are available in the clinical unions, and traumatic bone defects, as well as other situa-
setting to enhance bone regeneration. Autologous cancellous tions, including joint fusions, avascular necrosis, and diverse
bone grafting is the gold standard in maxillomandibular reconstruction procedures.2
reconstruction because its properties such as osteoconduc- Several techniques and autogenous bone grafting have
tion, osteoinduction, and osteogenesis fulfil the requisites for been described. Donor sites vary depending on the amount
bone repair and regeneration. 1 and types of bone available for harvest, and each site has
Bone grafting is performed to stimulate bone healing in advantages and disadvantages. Regions such as the mandib-
various adverse situations, including posttraumatic skeletal ular symphysis; rib; anterior and posterior iliac crest; and,
received Copyright © 2017 by Thieme Medical DOI https://doi.org/
March 12, 2016 accepted Publishers, Inc., 333 Seventh Avenue, 10.1055/s-0036-1593475.
after revision July 30, New York, NY 10001, USA. ISSN 1943-3875.
2016 Tel: +1(212) 584-4662.
published online
November 1, 2016
Mandibular Reconstruction with Proximal Tibial Graft Miceli et al. 293
more recently, the intercalvarial diploic bone have been used
as important donor sites for bone grafting.1,3–8
Procurement of cancellous bone from any site is not
without relative biological insult to the patient. These include
an additional surgical site, possible increased postoperative
morbidity, weakened donor site, and potential serious com-
plications from these conditions.8 Among alternatives, the
use of the proximal tibia as a donor site shows minimal
complications as well as a satisfactory amount of bone graft.
Use of the proximal tibia as a donor site has been applied in
jawbone reconstruction3 since 1990; thus, the tibia has
subsequently been used for grafting in orthognathic surgery,
clef surgery, and preprosthetic surgery, and for major jaw
reconstruction. 9
This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited.
Several studies of bone harvesting have compared the
complication rate, morbidity, and amount of cancellous bone
harvested from the tibia with other donor sites such as the iliac
crest. These studies have concluded that in comparison with an
iliac crest graft, tibia bone harvesting is easier and quicker,
with less blood loss and fewer donor site complications. 10
This article aimed to evaluate the volume of cancellous
bone harvested by a lateral approach on proximal metaphysis
of tibia in 31 patients at the Department of Oral and Maxillo- Fig. 1 Anterior view of knee showing the anatomic landmarks to
facial Surgery, Servidores do Estado Federal Hospital (Rio de access the Gerdy tubercle in the tibia bone.
Janeiro, Brazil) and the associated complications.
to obtain a sterilized field. Anatomic bony landmarks were
Materials and Methods
palpated and highlighted with a sterile skin marker pen. The
A retrospective study of 31 patients (18 women and 13 men) midpoint of a line from the fibular head to the anterior tibial
with a median age of 35 years (range: 19–64) referred to the tuberosity reveals the location of the Gerdy tubercle, which
Oral and Maxillofacial Surgery Service at Servidores do Estado was palpated and marked (►Figs. 1 and 2). Once the Gerdy
Federal Hospital (Rio de Janeiro, Brazil) was performed. The tubercle was localized, the soft tissue was infiltrated with 2%
study was accepted by the Ethics Committee and Research of xylocaine with 1:100.000 epinephrine to promote proper
the Servidores do Estado Federal Hospital (CEP 731470). vasoconstriction and facilitate the incision.
The inclusion criteria were ASA I, II and III patients, A 3- to 4-cm oblique skin incision was made superolaterally
without presence of infection, metabolic or metastatic bone to inferomedially paralleling the tendinous fibers over the Gerdy
disease, or trauma to the extremity that would further tubercle. Dissection was performed through the subcutaneous
compromise the integrity of the leg. Indications for recon- tissue and iliotibial tract to expose the bony prominence. Then,
struction using tibial graft were sequelae of orthognathic the periosteum was incised and elevated. The correct identifica-
surgery, jaw fracture, nonunion, pathology, and augmenta- tion of bony landmarks is essential to avoid neurovascular
tion of bone volume in oral implantology. structures during dissection, which is relatively safe. Electro-
The surgical technique used to harvest the cancellous graft coagulation was utilized to manage any hemorrhage.
was lateral approach from the Gerdy tubercle on the proximal Osteotomy using a drill bit was performed to create a bony
metaphysis of the tibia. Gerdy tubercle is the insertion site of window of 2.0 × 2.0 cm square over the Gerdy tubercle.
the iliotibialis tract on the proximal and lateral aspects of the Cancellous bone was harvested with curettes medially to
tibia. This bony protuberance is almost subcutaneous and it is laterally until cortical bone was reached and inferiorly.
exposed with minimal dissection. 11 The major anatomic Thus, the maximum possible amount of cancellous marrow
landmarks are the patella, patellar ligament, tibial tuberosity, bone was harvested from the proximal tibial metaphysis
and fibular head, which were palpated. The tibial tuberosity is (►Fig. 3). Caution was taken superiorly to avoid the tibial
localized below the midline of the knee, and the fibular head plateau and joint space. The cancellous bone graft was placed
is found laterally. The Gerdy tubercle is located between these into a 20-mL syringe to measure the bone volume (►Fig. 4).
structures (►Figs. 1 and 2). After bone graft removal, the area was irrigated with sterile
Surgical procedures were performed under general anes- saline. The closure of the iliotibial tract and subcuta- neous
thesia, and Cefazolin 2 g (Kefazol, ABL LTDA., Cosmópolis, SP, tissue was performed with 3.0 polyglactin (Vicryl, Ethicon,
Brazil) was used preoperatively and intraoperatively. Patients LLC, Somerville, NJ). Skin was closed with 3.0 nylon
were positioned supine with the knee flexed to approximately (Mononylon, Ethicon, M & I Medical) and a bulky gauze
45degrees to elevate the anterolateral surface of the tibia. dressing was placed on the wound with a light-pressure
Antisepsis with povidone-iodine solution was then conducted bandage.
Craniomaxillofacial Trauma and Reconstruction Vol. 10 No. 4/2017
294 Mandibular Reconstruction with Proximal Tibial Graft Miceli et al.
This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited.
Fig. 4 Cancellous bone graft into a 20-mL syringe to measure the bone
volume. Note a volume of 15 mL harvested in this case.
Analgesia was achieved with metamizole (Novalgina, Sanofi-
Aventis Farmacêutica Ltda, Suzano, São Paulo, Brazil), and
ibuprofen was used as a nonsteroidal anti-inflammatory drug
(Alivium; Mantecorp LTDA, Rio de Janeiro, Brazil).
Results
A total of 18 women (average age: 37, age range: 21–64 years)
and 13 men (average age: 35, age range: 19–57 years) were
included in the study. We used a lateral approach to remove a
cancellous tibial bone graft from the Gerdy tubercle on the
Fig. 2 Anterolateral view of knee showing the anatomic landmarks in proximal metaphysis of the tibia on the upper extremity.
the bones involved with the access to Gerdy tubercle (a) and in the Indications for reconstruction using a tibial graft were sequelae
patient during transoperatory period (b). P, patella; L, patellar liga- ment;
T, tibial tuberosity; F, fibular head; and GT, Gerdy tubercle. The square in of orthognathic surgery (n ¼ 1), jaw fracture (n ¼ 8), nonunion
(a) marks the location for the osteotomy to create a bony window of 2.0 of the jaw fracture (n ¼ 2), pathology (n ¼ 12), and bone
× 2.0 cm over the Gerdy tubercle with a drill to harvest the cancellous volume augmentation in oral implantology (n ¼ 8) (►Table 1).
bone with curettes. The interrupted line in (b) marks the location of the The mean amount of graft harvested from the tibial site by the
incision (a 3- to 4-cm oblique skin incision was made
superolaterally to inferomedially paralleling the tendinous fibers over the lateral approach was 13.0 T 3.7 mL (range: 8–23 mL)
Gerdy tubercle). No tourniquet was used. (►Table 1). This volume was sufficient in all surgical procedures.
At the donor site, only five patients (16%) exhibited minor
morbidity, and all complications were resolved during outpa-
During postoperative care, the patients were instructed to tient care (►Table 1). In three cases, whose indications for graft
keep the site of incision dry for 48 hours, to avoid weight harvesting were pathology and fracture sequel, local pain and
bearing on the operated leg for 3 weeks, and to always use a suture dehiscence occurred. Pain was managed with oral
stick to walk. Sutures were removed after 10 to 14 days. analgesics for 1 week, and no debridement was necessary
Fig. 3 (a) The window formed over the Gerdy tubercle during osteotomy. (b) Cancellous tibial bone harvested with curettes. (c) The aspect of bone
after the curettage.
Craniomaxillofacial Trauma and Reconstruction Vol. 10 No. 4/2017
Mandibular Reconstruction with Proximal Tibial Graft Miceli et al. 295
Table 1 Distribution of patients, the volume of graft harvested from the proximal tibial site by lateral approach, and complications
Gender Age Indication Volume Complication
F 21 Orthognathic sequel 14 No
F 22 Pathology 15 Local pain
F 22 Pathology 15 Superficial infection
F 24 Implantology 12 No
F 24 Fracture sequel 18 No
F 31 Pathology 14 No
F 33 Pathology 17 No
F 34 Fracture sequel 8 No
F 64 Pathology 11 No
This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited.
F 35 Pathology 9 No
F 38 Implantology 9 No
F 38 Fracture sequel 10 No
F 41 Implantology 20 No
F 43 Fracture sequel 9 No
F 43 Fracture sequel 13 Suture dehiscence
F 48 Pathology 16 No
F 48 Pathology 16 No
F 49 Pathology 12 No
Mean 37 13.5
SD 12 3.4
Min 21 8
Max 64 20
Gender Age Indication Volume Complication
M 19 Fracture sequel 9 No
M 22 Pathology 15 No
M 23 Fracture sequel 8 No
M 23 Fracture sequel 10 No
M 25 Pathology 15 Local pain
M 28 Implantology 13 No
M 33 Nonunion 10 No
M 36 Implantology 9 No
M 40 Implantology 23 No
M 44 Implantology 10 No
M 45 Nonunion 10 Unaesthetic scar
M 56 Pathology 15 No
M 57 Implantology 14 No
Mean 35 12.4
SD 13 4.1
Min 19 8
Max 57 23
Abbreviations: F, female; M, man; m, media; max, maximal; min, minimal; SD, standard deviation.
Craniomaxillofacial Trauma and Reconstruction Vol. 10 No. 4/2017
296 Mandibular Reconstruction with Proximal Tibial Graft Miceli et al.
for dehiscence. In another case whose indication for graft In accordance with many authors,5,8,11,16 we consider that
harvesting was a sequela of jaw fracture, an unaesthetic scar the lateral approach has advantages over the medial approach
could be noted at the donor site. Infiltration with cortico- because the Gerdy tubercle is a prominent anatomic land-
steroids for 2 weeks was performed successfully. Finally, one mark to perform a safe skin incision that avoids the anterior
patient who received a graft for nonunion of a jaw fracture had tibial muscle and local vessels and nerves. The lateral
a superficial infection. Antisepsis with local chlorhexidine 2% approach also features a smaller required angle of hand
for 2 weeks and oral antibiotics for 1 week reversed the case. instrumentation to access nearly all the procurable area of
Follow-up of approximately 6 months was performed, and all the tibial plateau. Thus, less effort and time are expended.17
complications resolved in approximately 3 weeks. Engelstad et al performed a study of 10 fresh frozen
No patients had hard infection, gait disturbance, hemato- cadavers to compare the amount of volume of cancellous
ma formation, fractures, paresthesia, or other donor site bone harvested from donor sites (anterior iliac crest, posterior
complications. In general, all patients were satisfied with iliac crest, and proximal tibia) within the same cadaver. The
the surgical procedure and exhibited excellent recovery of the results showed that the bone volumes from the proximal tibia
donor site. (11.3 mL) and posterior iliac crest (10.1 mL) were significantly
This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited.
greater than those from the anterior iliac crest (7.0 mL). In
uncompressed volume groups, the mean volume of cancellous
Discussion
bone from the proximal tibia (15.2 mL) was higher than that
Autologous bone graft is the gold standard for reconstruc- from the anterior and posterior iliac crests. The mean volume
tions in maxillofacial surgeries because these grafts possess of uncompressed cancellous bone from the posterior iliac crest
properties required for grafting success, such as osteocon- (11.7 mL) was greater than that from the anterior iliac crest
duction, osteoinduction, and osteogenesis. The physiological (10.4 mL), but the difference was not statistically significant. 18
process of bone reconstruction involves the union of these Many studies have reported significant complications
three processes. Cancellous tibial bone possesses all of these when the iliac crest is removed compared with tibia bone
characteristics and is therefore an excellent graft for orofacial grafts. Studies reported that 25% of patients who have been
procedures. Cancellous bone grafts harvested from the prox- treated with autogenous bone harvested from the iliac crest
imal tibia are used in oral and maxillofacial surgery for filling experience postoperative pain at an average of 5 years after
the osteotomy gap in orthognathic surgery, alveolar cleft surgery.19 Furthermore, in addition to pain, 6 to 20% of
bone grafting, alveolar ridge augmentation, maxillary sinus patients experience hypersensitivity or numbness in the
grafting, and other maxillomandibular reconstructions. 3,4,8 buttocks, and 3 to 9% of patients report major complications
Using the lateral approach, Catone and colleagues 8 with hernia or even peritoneal perforation.20 Thus, compared
obtained a noncompressed volume of 25 mL of cancellous with iliac crest harvesting, tibia bone removal is easier and
bone from the proximal tibial metaphysis in 21 cases. Other quicker, is associated with less blood loss and fewer donor site
studies of cadavers yielded similar amounts of bone.12 A complications, and offers a source of low–to-moderate
retrospective study of 78 patients who underwent 80 can- volumes of autologous bone.21
cellous tibial graft procurements as part of their maxillofacial Harvesting bone grafts from the proximal tibia is safe,
procedures revealed a mean graft volume of 17.8T 5.3 mL effective, and with a relatively low amount of adverse out-
(range: 8–32 mL).3 In our study, the amount of proximal tibial comes, but should be careful while using because it is not
bone harvested by the lateral approach from the 31 patients completely without adverse outcomes. Schmidt and Town-
was satisfactory for all procedures, with a mean volume of send described a case of a 47-year-old patient with a medical
13.0 T 3.7 mL (range: 8–23 mL). Correlations with quantity, history of controlled hypertension, asthma, osteoporosis, and
degree of morbidity, operating time, postoperative compli- osteoarthritis of the hands and knees and using alendronate.
cations, surgical complexity, and removal of cancellous bone After the surgery to augmentation maxillary sinus using tibial
graft are more attractive for the proximal tibial bone than for bone graft, the tibial bone progressed with osteomyelitis that
other sites. was treated with appropriate antibiotics and debridement. 22
Equal amounts of bone graft material are procurable from Possible causes of infection in this case might include the fact
the medial and lateral aspects of the proximal tibia. 7 Some that the patient was taking alendronate, an oral bisphosph-
authors prefer the medial approach to the proximal tibia onate that is known to produce localized bone vascular
because medial approach offers an easily palpable bone plane insufficiency and inhibit normal bone turnover remodeling. 23
and avoids potential injury to important structures, such as This fact serves to alert clinicians about these kind of patients.
detachment of the anterior tibial muscle and trauma of the In this article, 5 of 31 patients had minor complications
anterior tibial recurrent artery, which decreases surgical that did not impair the outcome and were resolved in a few
trauma.13,14 A study suggested that the medial proximal weeks. In three cases, local pain and suture dehiscence
tibial bone harvest approach had fewer serious structures were observed. In another case, an unaesthetic scar was
in harm’s way compared with the lateral; however, the lateral noted. Finally, one patient had a superficial infection. All
approach would have the benefit of muscle coverage and complications resolved in approximately 3 weeks with
therefore healing might be expedited in particular patient appropriate management. No patients exhibited hard
sub-groups.15 Thus, each approach can benefit different infection, hematoma formation, fractures, paresthesia, or
patient subgroups (►Fig. 5). other donor site complications.
Craniomaxillofacial Trauma and Reconstruction Vol. 10 No. 4/2017
Mandibular Reconstruction with Proximal Tibial Graft Miceli et al. 297
This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited.
Fig. 5 Anterior view of knee to show anatomic landmarks and incisions to lateral and medial approaches.
O’Keeffe et al reported 230 cases of bone grafts harvested experienced tibial fracture, and all fractures occurred between
from the proximal tibia. One case of fracture occurred in a 2 and 7 weeks after surgery and were caused by external
patient who, despite being non weight bearing for 6 weeks, trauma. Because tibial fractures occurred only during this
experienced an undisplaced fracture on the tibia eminence.24 specific period, the authors concluded that patient education
Hughes and Revington reported 2 proximal tibia fractures is a very important factor to prevent tibial fractures. The
among 75 cases. One case (a displaced fracture) occurred authors assumed that tibial fractures are vulnerable to direct
during a school sport 3 months following the harvest; the or indirect external trauma rather than physical condition,
second (an undisplaced stress fracture) was noted 9 days such as body weight or age.26
postoperatively following a fall.4 Ohya et al reported a case of
a woman who fell while removing her slacks 3 months after
tibia bone harvesting and suffered spontaneous pain in the
Conclusion
left tibia at the site of bone removal.25 We conclude that proximal tibia metaphysis for harvesting
There is no difference in the force required to induce a tibial cancellous bone graft provides sufficient volume for maxillo-
plateau fracture between the intact and decancellated proxi- facial surgery procedures with minimal postoperative
mal tibia. Cases of fracture have occurred when patients morbidity.
performed weight bearing.4,16,24 Our patients were instructed
to avoid weight bearing for 3 weeks and to avoid contact with
sports for 6 months. No cases of fracture occurred. In a study Conflict of Interest
conducted by Kim et al, only 4 of 105 tibial graft patients None.
Craniomaxillofacial Trauma and Reconstruction Vol. 10 No. 4/2017
298 Mandibular Reconstruction with Proximal Tibial Graft Miceli et al.
References 14 Jakse N, Seibert FJ, Lorenzoni M, Eskici A, Pertl C. A modified
1 Vittayakittipong P, Nurit W, Kirirat P. Proximal tibial bone graft: the technique of harvesting tibial cancellous bone and its use for sinus
volume of cancellous bone, and strength of decancellated tibias by the grafting. Clin Oral Implants Res 2001;12(5):488–494
medial approach. Int J Oral Maxillofac Surg 2012;41(4):531–536 15 Benninger B, Ross A, Delamarter T. Approaches to proximal
2 De Long WG Jr, Einhorn TA, Koval K, et al. Bone grafts and bone tibial bone harvest techniques. J Oral Maxillofac Res 2012;3;
graft substitutes in orthopaedic trauma surgery. A critical analysis. (2):e2
J Bone Joint Surg Am 2007;89(3):649–658 16 Thor A, Farzad P, Larsson S. Fracture of the tibia: complication of
3 Ko EC, Chang CM, Chang P, et al. Tibial cancellous bone grafting in bone grafting to the anterior maxilla. Br J Oral Maxillofac Surg
jaw reconstruction: 10 years of experience in Taiwan. Clin Implant 2006;44(1):46–48
Dent Relat Res 2015;17(Suppl 1):e321–e331 17 Kushner GM. Tibia bone graft harvest technique. Atlas Oral
4 Hughes CW, Revington PJ. The proximal tibia donor site in cleft Maxillofac Surg Clin North Am 2005;13(2):119–126
alveolar bone grafting: experience of 75 consecutive cases. 18 Engelstad ME, Morse T. Anterior iliac crest, posterior iliac crest,
J Craniomaxillofac Surg 2002;30(1):12–16, discussion 17 and proximal tibia donor sites: a comparison of cancellous bone
5 Mazock JB, Schow SR, Triplett RG. Proximal tibia bone harvest: volumes in fresh cadavers. J Oral Maxillofac Surg 2010;68(12):
review of technique, complications, and use in maxillofacial 3015–3021
surgery. Int J Oral Maxillofac Implants 2004;19(4):586–593 19 Leonetti JA, Koup R. Localized maxillary ridge augmentation with a
block allograft for dental implant placement: case reports. Implant
This document was downloaded for personal use only. Unauthorized distribution is strictly prohibited.
6 Gerressen M, Riediger D, Marx R, Saxe J, Ghassemi A. Stability
behavior of human tibias after bone removal—comparative examina- Dent 2003;12(3):217–226
tion in 15 cadaver tibia pairs. J Oral Maxillofac Surg 2010;68(1):60–67 20 Zemann W, Feichtinger M, Kowatsch E, Kärcher H. Extensive
7 Herford AS, King BJ, Audia F, Becktor J. Medial approach for tibial ameloblastoma of the jaws: surgical management and immediate
bone graft: anatomic study and clinical technique. J Oral Maxillo- reconstruction using microvascular flaps. Oral Surg Oral Med Oral
fac Surg 2003;61(3):358–363 Pathol Oral Radiol Endod 2007;103(2):190–196
8 Catone GA, Reimer BL, McNeir D, Ray R. Tibial autogenous cancel- 21 Wang K, Almeida LE, Olsson AB. Volume analysis of the proximal
lous bone as an alternative donor site in maxillofacial surgery: a tibial metaphysis. J Oral Maxillofac Surg 2007;65(12): 2425–
preliminary report. J Oral Maxillofac Surg 1992;50(12):1258–1263 2429
9 Besly W, Ward Booth P. Technique for harvesting tibial cancellous 22 Schmidt ER, Townsend J. Unusual complication of subacute oste-
bone modified for use in children. Br J Oral Maxillofac Surg 1999; omyelitis following tibial bone graft: report of a case. J Oral
37(2):129–133 Maxillofac Surg 2008;66(6):1290–1293
10 Ilankovan V, Stronczek M, Telfer M, Peterson LJ, Stassen LF, Ward- 23 Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of
Booth P. A prospective study of trephined bone grafts of the tibial the jaws associated with the use of bisphosphonates: a review of
shaft and iliac crest. Br J Oral Maxillofac Surg 1998;36(6):434–439 63 cases. J Oral Maxillofac Surg 2004;62(5):527–534
11 Brutus JP, Loftus JB. Gerdy’s tubercle as a source of cancellous bone 24 O’Keeffe RM Jr, Riemer BL, Butterfield SL. Harvesting of autogenous
graft for surgery of the upper extremity: description of technique. cancellous bone graft from the proximal tibial metaphysis.
J Hand Surg Am 2006;31(1):147–149 A review of 230 cases. J Orthop Trauma 1991;5(4):469–474
12 Gerressen M, Prescher A, Riediger D, van der Ven D, Ghassemi A. 25 Ohya M, Fujimoto T, Ito Y, Watabe M, Yamamoto N, Ueda M. Tibial
Tibial versus iliac bone grafts: a comparative examination in 15 bone fracture after bone harvesting from the tibia. Asian J Oral
freshly preserved adult cadavers. Clin Oral Implants Res 2008; Maxillofac Surg 2008;20:106–109
19(12):1270–1275 26 Kim IK, Cho HY, Pae SP, Jung BS, Cho HW, Seo JH. Tibial bone
13 Hernández-Alfaro F, Martí C, Biosca MJ, Gimeno J. Minimally fractures occurring after medioproximal tibial bone grafts for oral
invasive tibial bone harvesting under intravenous sedation. and maxillofacial reconstruction. J Korean Assoc Oral Maxillofac
J Oral Maxillofac Surg 2005;63(4):464–470 Surg 2013;39(6):257–262
Craniomaxillofacial Trauma and Reconstruction Vol. 10 No. 4/2017
You might also like
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Algun DiaDocument6 pagesAlgun DiaMarco Antonio García LunaNo ratings yet
- Microsaw and Piezosurgery in Harvesting Mandibular Bone Blocks From The Retromolar Region: A Randomized Split-Mouth Prospective Clinical TrialDocument8 pagesMicrosaw and Piezosurgery in Harvesting Mandibular Bone Blocks From The Retromolar Region: A Randomized Split-Mouth Prospective Clinical TrialdivyaNo ratings yet
- Mandibular Bone Block Harvesting From The Retromolar Region: A 10-Year Prospective Clinical StudyDocument10 pagesMandibular Bone Block Harvesting From The Retromolar Region: A 10-Year Prospective Clinical StudyFerenc NagyNo ratings yet
- Three-Dimensional Vertical Alveolar Ridge Augmentation in The Posterior Maxilla: A 10-Year Clinical StudyDocument10 pagesThree-Dimensional Vertical Alveolar Ridge Augmentation in The Posterior Maxilla: A 10-Year Clinical StudyFabian Sanabria100% (1)
- The Effect of Conventional Surgery and Piezoelectric Surgery Bone Harvesting Techniques On The Donor Site Morbidity of The Mandibular Ramus and SymphysisDocument7 pagesThe Effect of Conventional Surgery and Piezoelectric Surgery Bone Harvesting Techniques On The Donor Site Morbidity of The Mandibular Ramus and SymphysisguhanderNo ratings yet
- 2015 Article 7Document7 pages2015 Article 7TikaZyka16No ratings yet
- Split Technique 2Document8 pagesSplit Technique 2Alejandro RuizNo ratings yet
- Drughelp - Care 6.22Document10 pagesDrughelp - Care 6.22Joko RifaiNo ratings yet
- Corticotomia Tunel AsistidoDocument7 pagesCorticotomia Tunel Asistidokatya Serrano LemusNo ratings yet
- Oh 2010Document5 pagesOh 2010gbaez.88No ratings yet
- Journal ProstoDocument6 pagesJournal ProstoAvila Aita Harun RasyidNo ratings yet
- Recovery of Pulp Sensibility After the Surgical Management of a Large radicular cystDocument5 pagesRecovery of Pulp Sensibility After the Surgical Management of a Large radicular cystmeryemeNo ratings yet
- Ams 5 108Document4 pagesAms 5 108Alice EmailsNo ratings yet
- Floratos Et Al. Bone Window Technique in Endodontic Microsurgery Report of Two Cases. Volume 2 2023Document10 pagesFloratos Et Al. Bone Window Technique in Endodontic Microsurgery Report of Two Cases. Volume 2 2023Edward AbadiaNo ratings yet
- Large Cystic Lesion Treated Surgically and EndodonticallyDocument5 pagesLarge Cystic Lesion Treated Surgically and EndodonticallyanamaghfirohNo ratings yet
- Optimization of Ligature or Bone Defect InducedDocument19 pagesOptimization of Ligature or Bone Defect InducednoorasyillaNo ratings yet
- Schlund 2019Document3 pagesSchlund 2019mesescuNo ratings yet
- Carlino 2019Document9 pagesCarlino 2019Isabella WilkeNo ratings yet
- Intrusion of Incisors in Adult Patients With Marginal Bone LossDocument10 pagesIntrusion of Incisors in Adult Patients With Marginal Bone LossYerly Ramirez MuñozNo ratings yet
- Cirugía OralDocument7 pagesCirugía OralLenny GrauNo ratings yet
- Split Technique 3Document13 pagesSplit Technique 3Alejandro RuizNo ratings yet
- Autogenous Corticocancellous Iliac Bone Graft in Reconstruction of Mandibular Defect: Point of TechniqueDocument4 pagesAutogenous Corticocancellous Iliac Bone Graft in Reconstruction of Mandibular Defect: Point of TechniquekumerrajandrNo ratings yet
- Complications in The Use of The Mandibular Body, Ramus and Symphysis As Donor Sites in Bone Graft Surgery. A Systematic ReviewDocument9 pagesComplications in The Use of The Mandibular Body, Ramus and Symphysis As Donor Sites in Bone Graft Surgery. A Systematic ReviewBrenda Carolina Pattigno ForeroNo ratings yet
- 1 s2.0 S1991790221001732 MainDocument6 pages1 s2.0 S1991790221001732 MainAlejandro MejiaNo ratings yet
- Ma 2021Document6 pagesMa 2021bigben9262No ratings yet
- Fuhrmann 2002Document6 pagesFuhrmann 2002DentalErNo ratings yet
- Articulo en Inglés 2Document8 pagesArticulo en Inglés 2Luis Ramirez BenaventeNo ratings yet
- Calvarial Bone Grafting For Three-Dimensi Reconstruction of Severe Maxillary Defects: A CDocument11 pagesCalvarial Bone Grafting For Three-Dimensi Reconstruction of Severe Maxillary Defects: A Cmatias112No ratings yet
- Exostosis MandibularDocument6 pagesExostosis MandibularCOne Gomez LinarteNo ratings yet
- Physical Properties of Root Cementum: Part 26. Effects of Micro-Osteoperforations On Orthodontic Root Resorption: A Microcomputed Tomography StudyDocument10 pagesPhysical Properties of Root Cementum: Part 26. Effects of Micro-Osteoperforations On Orthodontic Root Resorption: A Microcomputed Tomography StudyMonojit DuttaNo ratings yet
- Extraction Socket Presenvation Using A Collagen Plug Combined With Platelet Rich Plasma (PRP) RADIOGRAPIHICDocument7 pagesExtraction Socket Presenvation Using A Collagen Plug Combined With Platelet Rich Plasma (PRP) RADIOGRAPIHICrachmadyNo ratings yet
- Razavi 1995Document5 pagesRazavi 1995rodrigoNo ratings yet
- 2020 Article 73180Document11 pages2020 Article 73180rachmadyNo ratings yet
- 179-Article Text-302-1-10-20171121 PDFDocument5 pages179-Article Text-302-1-10-20171121 PDFMichael XuNo ratings yet
- 26 3 MovahedDocument4 pages26 3 Movahedbalab2311No ratings yet
- Fotos OclusalesDocument6 pagesFotos OclusalesMarco Antonio García LunaNo ratings yet
- Alveolar Ridge Augmentation by Distraction OsteogenesisDocument8 pagesAlveolar Ridge Augmentation by Distraction OsteogenesisCarlos Santiago VivenzaNo ratings yet
- Bone Graft Literature ReviewDocument4 pagesBone Graft Literature Reviewea7gjrm5100% (1)
- Use of Titanium Mesh For Staged Localized Aeveolar Ridge AugmentationDocument12 pagesUse of Titanium Mesh For Staged Localized Aeveolar Ridge AugmentationAnonymous bOhsjs1Y7mNo ratings yet
- Augmentation of The Sinus Floor With Mandibular Bone Block and Simultaneous Implantation: A 6-Year Clinical InvestigationDocument8 pagesAugmentation of The Sinus Floor With Mandibular Bone Block and Simultaneous Implantation: A 6-Year Clinical InvestigationWesley Silva100% (1)
- Evaluation of Corticotomy - Facilitated Orthodontics and Piezocision in Rapid Canine RetractionDocument8 pagesEvaluation of Corticotomy - Facilitated Orthodontics and Piezocision in Rapid Canine RetractionJose CollazosNo ratings yet
- Retrieve 4Document8 pagesRetrieve 4dreneanastriNo ratings yet
- A Literature Based Comparison of Bone Augmentation.1Document6 pagesA Literature Based Comparison of Bone Augmentation.1drzana78No ratings yet
- Materials: A Modified Ridge Splitting Technique Using Autogenous Bone Blocks-A Case SeriesDocument10 pagesMaterials: A Modified Ridge Splitting Technique Using Autogenous Bone Blocks-A Case SeriesLouis HutahaeanNo ratings yet
- Bone Grafts SatyaDocument153 pagesBone Grafts SatyaArchanaNo ratings yet
- Sequential Piezocision A Novel Approach To Acelerated Orthodontic TreatmentDocument11 pagesSequential Piezocision A Novel Approach To Acelerated Orthodontic TreatmentMargareth BritoNo ratings yet
- Raffaini Bioss CollagenDocument7 pagesRaffaini Bioss CollagenÂngelo Rosso LlantadaNo ratings yet
- 737 Ijar-23255Document7 pages737 Ijar-23255Louis HutahaeanNo ratings yet
- Pi Is 1010518215004084Document8 pagesPi Is 1010518215004084Ceza CezaaNo ratings yet
- The Influence of Cortical Bone Perforation On Guided Bone Regeneration in HumansDocument6 pagesThe Influence of Cortical Bone Perforation On Guided Bone Regeneration in Humanspin.to.teethNo ratings yet
- Clinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesDocument11 pagesClinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesraynaldidjohariofcNo ratings yet
- 2 Art EdhitDocument7 pages2 Art EdhitJarvin Miguel Buitrago GalindezNo ratings yet
- 2019 Hahn LeeDocument4 pages2019 Hahn LeeR KNo ratings yet
- Ort 7Document2 pagesOrt 7Siddharth DhanarajNo ratings yet
- Artículo Khoury2018Document10 pagesArtículo Khoury2018Basma Derdabi100% (1)
- Rde 39 51Document5 pagesRde 39 51Sashwat SathishNo ratings yet
- Surgical Management of Periapical Lesion Inmaxillary Incisorswith Combined Bone Graft and Platelet - Rich Fibrin: A Case ReportDocument5 pagesSurgical Management of Periapical Lesion Inmaxillary Incisorswith Combined Bone Graft and Platelet - Rich Fibrin: A Case ReportTMDCH JournalNo ratings yet
- Witek 2019Document7 pagesWitek 2019Alejandro FereñoNo ratings yet
- Augmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudyDocument7 pagesAugmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudytomimacagnoNo ratings yet
- 10 1111j 1600-9657 2009 00857 XDocument4 pages10 1111j 1600-9657 2009 00857 XDwifitri MaretaNo ratings yet
- Alveoler Process Fracture in Mandibular Immature Permanent Incisors RegionDocument3 pagesAlveoler Process Fracture in Mandibular Immature Permanent Incisors RegionDwifitri MaretaNo ratings yet
- JurnalDocument18 pagesJurnalDwifitri MaretaNo ratings yet
- Fourth Universal Definition of Myocardial Infarction (2018) PDFDocument33 pagesFourth Universal Definition of Myocardial Infarction (2018) PDFPamela LacentvaneseNo ratings yet
- ParkMediclaim Insurance TPA PVT LTD Group Policy Search - KarnatakaDocument21 pagesParkMediclaim Insurance TPA PVT LTD Group Policy Search - KarnatakakumarNo ratings yet
- SJK (C) Chung Hua Lingga Monthly Test (1) Year 4 ScienceDocument21 pagesSJK (C) Chung Hua Lingga Monthly Test (1) Year 4 ScienceChia CassyNo ratings yet
- Blocking Polyspermy and Pregnancy Tests ExplainedDocument13 pagesBlocking Polyspermy and Pregnancy Tests ExplainedHafizah ZakiahNo ratings yet
- 1 - Indications For Removal of TeethDocument7 pages1 - Indications For Removal of TeethLama NahedNo ratings yet
- Oxford Case Histories in General Surgery (gnv64) PDFDocument514 pagesOxford Case Histories in General Surgery (gnv64) PDFTelugukurraaadu100% (3)
- People vs. BanezDocument21 pagesPeople vs. BanezFlo PaynoNo ratings yet
- High Yield Omm For Comlex IIDocument28 pagesHigh Yield Omm For Comlex IIMartinez_DO100% (4)
- Mania: Caring For A Person ExperiencingDocument6 pagesMania: Caring For A Person ExperiencingGutsy JewelNo ratings yet
- Herbal Materia Medica 5th Ed. by Michael MooreDocument57 pagesHerbal Materia Medica 5th Ed. by Michael MooreIreneRains100% (3)
- BDJ Volume 201 Issue 6 2006 (Doi 10.1038/sj - bdj.4814041) Chee, W Jivraj, S - Treatment Planning of The Edentulous MandibleDocument9 pagesBDJ Volume 201 Issue 6 2006 (Doi 10.1038/sj - bdj.4814041) Chee, W Jivraj, S - Treatment Planning of The Edentulous MandibleahmadNo ratings yet
- Coconut Oil Offers Hope For Antibiotic Resistant GermsDocument5 pagesCoconut Oil Offers Hope For Antibiotic Resistant GermsLiza Y. EspinosaNo ratings yet
- Dapus SimonDocument6 pagesDapus SimonMang RamaNo ratings yet
- 123 Anywhere ST., Any City ST 12345 (123) 456-7890Document2 pages123 Anywhere ST., Any City ST 12345 (123) 456-7890Ken SimonNo ratings yet
- How To Have Sex in An EpidemicDocument27 pagesHow To Have Sex in An EpidemicchbartsNo ratings yet
- Deep Brain Stimulation For The Treatment of Chronic, Intractable PainDocument15 pagesDeep Brain Stimulation For The Treatment of Chronic, Intractable PainnaimNo ratings yet
- MAPEH 10 TOS 1st GradingDocument4 pagesMAPEH 10 TOS 1st Gradingelyn75% (4)
- 3 NsaidsDocument23 pages3 NsaidsHagai MagaiNo ratings yet
- (Scott A. Farrell) Pessaries in Clinical Practice (B-Ok - Xyz)Document105 pages(Scott A. Farrell) Pessaries in Clinical Practice (B-Ok - Xyz)AleceandraNo ratings yet
- Sensus Jamal Terbaru (Fix)Document38 pagesSensus Jamal Terbaru (Fix)chrisvivani ruatakureiNo ratings yet
- Lab and Blood Bank Safe DisposalDocument8 pagesLab and Blood Bank Safe DisposalShawqi AlmughniNo ratings yet
- Vince McMahon's Testimony To Waxman CommitteeDocument122 pagesVince McMahon's Testimony To Waxman Committeeestannard100% (2)
- NCTF 135 and NCTF 135 HaDocument3 pagesNCTF 135 and NCTF 135 Hajosli100% (2)
- Electrical Conduction System of the HeartDocument7 pagesElectrical Conduction System of the HeartHUAWEI HUAWEINo ratings yet
- 0610 s17 Ms 41Document12 pages0610 s17 Ms 41pkrajenpillaygmailcomNo ratings yet
- Renal - MedbulletsDocument74 pagesRenal - Medbulletssmian08No ratings yet
- Various Methods of Ligation Ties: Review ArticleDocument6 pagesVarious Methods of Ligation Ties: Review ArticleDivine Macaranas CordovizNo ratings yet
- Ef310 Unit 8 Carls Assessment Part 2Document3 pagesEf310 Unit 8 Carls Assessment Part 2api-473700764No ratings yet
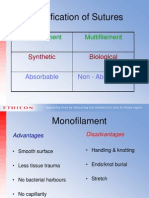
- Classification of Sutures: Monofilament MultifilamentDocument17 pagesClassification of Sutures: Monofilament Multifilamentlina_m354No ratings yet
- Youth Advocacy Letter Commission On Narcotic DrugsDocument2 pagesYouth Advocacy Letter Commission On Narcotic DrugsAB-No ratings yet
- Biology Investigatory Project: Samiksha Subhashish SarkarDocument35 pagesBiology Investigatory Project: Samiksha Subhashish SarkarSamiksha SarkarNo ratings yet