Professional Documents
Culture Documents
General Characteristics: Absorption
Uploaded by
Lenny NovitaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
General Characteristics: Absorption
Uploaded by
Lenny NovitaCopyright:
Available Formats
About Sections
Journal of Pharmaceutical Sciences / Volume 94, Issue 8
Commentary Free Access
Biowaiver monographs for immediate
release solid oral dosage forms: Ranitidine
hydrochloride
H. Kortejärvi , M. Yliperttula , J.B. Dressman ,
H.E. Junginger , K.K. Midha , V.P. Shah , D.M. Barends
First published: 15 June 2005
https://doi.org/10.1002/jps.20392
Cited by: 25
This study reflects the scientific opinion of the authors
and not the policies of regulating agencies.
Abstract
Literature and experimental data relevant to the
decision to allow a waiver of in vivo
bioequivalence testing for the approval of
immediate release (IR) solid oral dosage forms
containing ranitidine hydrochloride are
reviewed. According to the current
Biopharmaceutics Classification System (BCS),
ranitidine hydrochloride should be assigned to
Class III. However, based on its therapeutic and
therapeutic index, pharmacokinetic properties
and data related to the possibility of excipient
interactions, a biowaiver can be recommended
for IR solid oral dosage forms that are rapidly
dissolving and contain only those excipients as
reported in this study. © 2005 Wiley Liss, Inc.
and the American Pharmacists Association J
Pharm Sci 94:1617–1625, 2005
INTRODUCTION
A monograph based on literature data is presented
on ranitidine hydrochloride with respect to its
biopharmaceutical properties and the risk of
waiving in vivo bioequivalence testing for the
approval of new and reformulated IR solid oral
dosage forms. The purpose and scope of these
monographs were discussed previously.1 Briefly,
the aims of the present study were to evaluate all
pertinent data available from literature sources to
assess the appropriateness of such a biowaiver
from the biopharmaceutical point of view and also
from the perspective of public health risks.
EXPERIMENTAL
The databases Caplus, Ipa, and Medline were
utilized to search using the keyword permeability
and Caplus and Ipa using the keywords dissolution,
solubility, and degradation. The pharmacokinetic
data search was initiated from the Martindale and
the Drug Information Fulltext, followed by
reviewing the references cited. Information with
regard to the double peak phenomenon, site
dependent absorption, first pass metabolism,
enterohepatic recycling, and bioequivalence
studies were reviewed from the cited literature
obtained from Medline, using the keyword
pharmacokinetics. Only literature written in English
and German was included and the searches were
not limited to a certain time period. As the
solubility data from literature did not cover the
entire physiological pH range, these were obtained
experimentally at Orion Pharma. Triplicate
determinations were carried out in which the
solute was shaken with buffers pH 1, 3, 5, and 7.4
at room temperature for 3 h and the obtained
solutions analyzed by high performance liquid
chromatography.
RESULTS
General Characteristics
The INN and World Health Organization (WHO)
name for ranitidine, is N [2 [[[ 5
[(dimethylamino)methyl] 2
furanyl]methyl]thio]ethyl] N methyl 2 nitro 1,1
ethenediamine.
Structure
See Figure 1.
Figure 1
Open in figure viewer PowerPoint
Structure of ranitidine.
Salt, Esters, Polymorphs
Most preparation contain the hydrochloride 2 and
this monograph covers only that salt of ranitidine.
Ranitidine hydrochloride exhibits polymorphism.2
Immediate release (IR) tablets containing ranitidine
hydrochloride with different polymorphic forms
were reported to be bioequivalent.3
Partition Coefficient
LogP (water/n octanol) was reported to be 0.2.4
This value is likely for the ionized form, i.e., logD.
LogP (for the neutral molecule) was calculated to
be 1.28.5
pKa
The two pKa values reported 8.2 and 2.7 4 are in
agreement with the values of 8.4 and 3.5,
respectively, calculated with a structure fragment
based approach.5
Indication
Ranitidine is a histamine H2 antagonist used in the
treatment of gastric and duodenal ulceration with
or without Helicobacter pylori infection and for
gastro oesophageal reflux disease.2 Ranitidine
inhibits gastric acid secretion, which is stimulated
by pentagastrin, histamine, and normal meals.6
The incidence of adverse drug reactions with H2
receptor antagonists are low (<3%) and are usually
minor in nature.7 For Zollinger–Ellison syndrome
doses up to 900 mg daily have been used without
troublesome side effects.6
The WHO recommended dose for ranitidine tablets
is 150 mg ranitidine base, given as the
hydrochloride salt.8 Strengths currently having a
marketing authorization (MA) in Germany (DE)9,
Finland (FI),10 and The Netherlands (NL)11 are the
equivalents of 75, 150, and 300 mg ranitidine base.
Solubility
The solubility of ranitidine hydrochloride in water is
660 mg/mL and it is reported to be freely soluble in
water.2 The solubility in the pH range 1–7.4 was
experimentally found to be over 550 mg/mL. As the
highest strength is 300 mg, the dose: solubility ratio
is less than 0.55 mL, far below the critical value of
250 mL.12,13 However, these data were obtained
at room temperature and the criteria of “highly
soluble” according to FDA and EMEA Guidelines are
defined at 37°C.12,13 But, supposing that the
solubility will be higher at 37°C than at room
temperature, it is reasonable safe to classify
ranitidine hydrochloride as a “highly soluble” active
pharmaceutical ingredient (API).
Pharmacokinetics
Absorption
The oral bioavailability (BA) of ranitidine is 50%–
60%. The drug is reported to be rapidly absorbed
when administered via the oral route14-18 and
absorption after oral administration is linear.19 A
first peak in plasma concentrations is reached
within 0.5–1.5 h and a second peak is observed
within 3–4 h after single doses.20,21 The reasons
for this double peak phenomenon are unclear. This
is likely not due to biliary excretion, as biliary
excretion is only 0.4% after oral administration.22
Variations in gastric emptying may also not be a
satisfactory explanation, since when ranitidine was
administered as a solution directly to the jejunum,
double peaks were observed even more often than
after administration to the stomach.23 In any case,
this double peak phenomenon is not relevant for
biowaiver decisions, as there is no indication that it
is formulation dependent.
The BA of ranitidine is significantly lower when
administered as a solution directly to the colon
instead of stomach, jejunum, or ileum.23,24 Since
the tight junctions in the colon are considerably
less permeable than those in the small intestine, it
can be hypothesized that ranitidine is absorbed by
a paracellular mechanism, with the main
absorption site in the small intestine. Food in
general has no effect on the rate and extent of
absorption.25
Permeability
Results of permeability measurements are shown
in Table 1.
Table 1. Permeability of Ranitidine
Concentration Method Papp/Peff Reference
Used (mM) (×10−7
cm/s)
0.000142–14.25 Caco 2 1.03 26
0.1–5 Caco 2 18–7.5 27
0.005–5 Caco 2 20–12 28
2.56 Caco 2 3.1 a 29
— Caco 2 12.4 30
0.5 Intestinal 270 31
perfusion
a Furosemide, atenolol, and propranolol were
used as reference compounds.
The results of the Caco 2 studies and the human
intestinal permeability technique show large
differences. These differences have been reported
and discussed earlier as these observations can be
explained on the basis that tight junctions in the
intestinal cell tissues are more permeable than the
tight junctions in the Caco 2 monolayers.1 Despite
these differences, both permeability techniques
demonstrate that the permeability is low. Indeed,
ranitidine is recommended as a low permeability
internal standard in the FDA guideline for Caco 2
permeability studies.12 The Caco 2 permeability
increases when calcium concentration is decreased
in the test medium,26 which can be explained on
the basis that low calcium concentrations cause
opening of the tight junctions of the paracellular
route or change the membrane integrity by
disturbing the phospholipid bilayers. Thus, the
main absorption mechanism of ranitidine is
paracellular passive diffusion. In vitro and
nonclinical studies have suggested that ranitidine is
a substrate for P gp.28,30,32 But it is likely that
high doses of this highly soluble drug, formulated
in rapidly dissolving tablets, will cause saturation of
the P gp efflux protein.
Distribution
The apparent volume of the distribution for
terminal phase is about 1.16–1.87
L/kg.14,15,21,25,33 Ranitidine has a low protein
binding of about 15%.15
Metabolism and Excretion
The urinary excretion of unchanged ranitidine
following intravenous (i.v.) administration is 70%–
80%,4,17,18,21,25 whereas the renal excretion of
unchanged drug after oral dosing is 25%–
30%.4,15,17,21 Less than 10% of the dose is
metabolized and excreted via the urinary route
after either i.v. or oral dosing.15,17 Of orally
administered ranitidine, 26% is excreted with the
feces.10 Half life of elimination phase is 1.7–2.1 h
after i.v. dose.14,15,19,21 There are no reports that
ranitidine follows non linear pharmacokinetics.
Dosage Form Performance
Excipients
The excipients used in the formulations of IR
products having a MA in DE, FI, and NL are shown
in Table 2. In previous monographs, MA's were
taken as indicators that these formulations had
passed in vivo bioequivalence requirements.1
However, for ranitidine formulations with a MA in
DE, this cannot always be assumed, because in
1998 the bioavailability committee of the
regulatory authorities of DE classified ranitidine as
an API for which in vivo bioequivalence testing is
not always necessary, in view of its wide
therapeutic index and non critical therapeutic
use.34 The DE list was recently withdrawn, but not
the MA granted under that provision.35 FI and NL
might also have granted MA's without requiring in
vivo bioequivalence studies.
Table 2. Excipients a Present in Ranitidine
Hydrochloride IR Solid oral Drug Products b with
an Marketing Authorization (MA) in Germany (DE),
Finland (FI), and The Netherlands (NL)
Basic butylated DE (1–3) NL (4) FI (5,6)
methacrylate
copolymer
Calcium hydrogen DE (7–13) NL (14)
phosphate
Carmellose sodium NL (15, 16)
Carnauba wax DE (17–20) NL (21, 22)
Castor oil DE (23–26) NL (27, 28)
Cellulose DE (1–3, 7–13, 17–19, 23–26, 29–52)
NL (4, 14–16, 21, 22, 27, 28, 53–66)
FI (5, 6, 67–74)
Copovidone DE (1–3)
Croscarmellose DE (17–21, 23–26, 29, 30, 32, 36, 38,
sodium 40, 41, 43, 45–47, 49, 52) NL (4, 22,
27, 28, 56, 59, 61, 62, 64) FI (5, 6, 67,
69, 73, 74)
Dextran DE (17, 19)
Ethylcellulose FI (70)
Glucose DE (39, 40, 43)
Hydroxypropylcellulose FI (71)
Hypromellose DE (1–3, 7–13, 17–20, 23–26, 29–52)
NL (4, 14–16, 21, 22, 27, 28, 53–66)
FI (5, 6, 67–74)
Lactose DE (7–13) NL (14)
Macrogol DE (1, 3, 7–13, 17–20, 29, 31–41, 43–
47) NL (4, 14, 16, 21, 22, 56–62, 64,
65) FI (5, 6, 67, 69, 70, 73)
Magnesium stearate DE (1–3, 7–13, 17–20, 23–26, 29–52)
NL (4, 14–16, 21, 22, 27, 28, 53–66)
FI (5, 6, 67–74)
Maize starch DE (7–13) NL (14)
Polydextrose DE (18, 20, 31, 32, 35–38, 41, 44–46)
NL (16,21,22,57 61,65) FI (69,73)
Polymethacrylate DE (29, 47) NL (56, 62, 64) FI (67)
Polymethacrylic acid DE (33)
Polymethacrylic acid DE (34)
Copolymer
Polysorbate FI (70)
Povidone DE (33, 34) FI (70)
Shellac DE (25)
Silica DE (1, 7–13, 18, 19, 23–26, 30, 46)
NL (14, 21, 22, 27, 28) FI (73)
Silica, hydrophobic DE (17, 41)
Simethicone DE (25)
Sodium starch DE (7–13) NL (14) FI (70)
glycolate
Soya bean oil FI (70)
Talc DE (1, 23–26, 29, 33, 34, 47) NL (4,
27, 28, 56, 62, 64) FI (5, 6, 67, 70, 73)
Triacetin DE (30, 41, 48–52) NL (15, 53–55) FI
(68, 72, 74)
Triethyl citrate DE (31, 32, 35–41, 43–46) NL (16,
57–61, 65) FI (69, 73)
Sources of data: DE: www.rote liste.de; FI:
www.nam.fi; NL: www.cbg meb.nl
a Printing inkt, colorants, and flavors are not
included.
b Excluded are dosage forms that are
swallowed by the patient in liquid form, such as
effervescent and dispersible tablets. Chewable
tablets are also excluded.
1. Raniberl® 150 mg/ 300 mg Filmtabletten.
2. Ranitidoc 300 mg Filmtabletten.
3. Rani nerton® 150/ 300 Filmtabletten.
4. Ranitidine Sandoz 150/300, tabletten 150
mg/300 mg.
5. Ranitidin Alpharma 150 mg/300 mg
kalvopäällysteinen tabletti.
6. Ranitidine Biochemie 150 mg/300 mg
kalvopäällysteiset tabletti.
7. Ranibeta® 150/ 300 Filmtabletten.
8. Raniprotect® 150/ 300 Filmtabletten.
9. Ranitic® 75 akut bei Sodbrennen
Filmtabletten.
10. Ranitic® 150/ 300/ 150 akut/ 300 akut
Filmtabletten.
11. Ranitidin 75 1 A Pharma Filmtabletten.
12. Ranitidin 150/ 300 1 A Pharma
Filmtabletten.
13. RANITIDIN BASICS 150 mg/ 300 mg
Filmtabletten.
14. Ranitidine 150 mg/300 mg, tabletten.
15. Zantac 300, tabletten 300 mg.
16. Ranitidine Merck 300 mg, tabletten.
17. Ranitidin PB 150 mg/ 300 mg Filmtabletten.
18. Ranitidin Sandoz® 150 mg/ 300 mg
Filmtabletten.
19. Ranitidin STADA® 150 mg/ 300 mg
Filmtabletten.
20. Ran Lich® 150 mg/ 300 mg Filmtabletten.
21. Ranitidine CF 150 mg/300 mg, omhulde
tabletten.
22. Ranitidine 150/300 PCH, tabletten 150
mg/300 mg.
23. Ranitab® 75 mg Filmtabletten.
24. Ranitidin ratiopharm® 75 mg Filmtabletten
gegen Sodbrennen.
25. Ranitidin STADA® 75 mg Filmtabletten.
26. ranitidin von ct 75 mg Filmtabletten.
27. Ranitidine 150/300 Ranbaxy, omhulde
tabletten 150 mg/300 mg.
28. Ranitidine 75 mg Hexal, tabletten.
29. Junizac® 150 mg/ 300 mg Filmtabletten.
30. Rani 150 mg/ 300 mg AbZ Filmtabletten.
31. Ranibloc® 150 Filmtabletten.
32. Ranibloc® 300 Filmtabletten.
33. Ranicux® 75 mg Filmtabletten.
34. Ranicux® 150 mg/ 300 mg Filmtabletten.
35. Ranidura® T 150 mg Filmtabletten.
36. Ranidura® T 300 mg Filmtabletten.
37. Ranimerck® 150 mg Filmtabletten.
38. Ranimerck® 300 mg Filmtabletten.
39. RANI PUREN® 150 Filmtabletten.
40. RANI PUREN® 300 Filmtabletten.
41. ranitidin 150/ 300 von ct Filmtabletten.
42. Ranitidin acis® 300 mg Filmtabletten.
43. Ranitidin AL 150/ 300 Filmtabletten.
44. Ranitidin ISIS® 150 Filmtabletten.
45. Ranitidin ISIS® 300 Filmtabletten.
46. Ranitidin ratiopharm® 150/ 300/ 150 akut/
300 akut Filmtabletten.
47. Ranitidin saar® 150 mg/ 300 mg
Filmtabletten.
48. Sostril® 150 mg Filmtabletten.
49. Sostril® 300 mg Filmtabletten.
50. Zantic® 75 mg Magentabletten
Filmtabletten.
51. Zantic® 150 mg Filmtabletten.
52. Zantic® 300 mg Filmtabletten.
53. Zantac 150, tabletten 150 mg.
54. Zantac 75, tabletten 75 mg.
55. Zantac 150, tabletten 150 mg.
56. Ranitidine Dumex 150 mg, tabletten.
57. Ranitidine Merck 150 mg, tabletten.
58. Ranitidine 150 mg Katwijk, tabletten.
59. Ranitidine 300 mg Katwijk, tabletten.
60. Ranitidine CF 150 mg, tabletten.
61. Ranitidine CF 300 mg, tabletten.
62. Ranitidine Gf 150 mg/300 mg, tabletten.
63. Ranitidine 75 mg/150 mg/300 mg, omhulde
tabletten (Pharmacin Products).
64. Ranitidine 150 mg/300 mg, omhulde
tabletten (Delphi).
65. Ranitidine FLX 75 mg/150 mg/300 mg,
filmomhulde tabletten.
66. Ranitidine 75 mg/150 mg/300 mg Katwijk,
omhulde tabletten.
67. Ranitidin Pliva 150 mg tabletti,
kalvopäällysteinen.
68. ESOFEX® 150 mg tabletti,
kalvopäällysteinen.
69. Ranicur 150 mg/300 mg tabletti,
kalvopäällysteinen.
70. Ranil® 150 mg/300 mg kalvopäällysteinen
tabletti.
71. Ranimex 150 mg tabletti.
72. Ranimex 75 mg tabletti, kalvopäällysteinen.
73. Ranixal 150 mg/300 mg tabletti,
kalvopäällysteinen.
74. Zantac 150 mg/300 mg tabletti.
Studies with specific excipients on the in vitro
permeability of BCS class III drugs have been
reported, some of which include ranitidine
studies.36,37 Excipients such as lactose,
hydroxypropylmethyl cellulose, docusate sodium,
EDTA, propylene glycol, and PEG 400 did not affect
the Caco 2 permeability. However, other excipients
such as sodium lauryl sulfate, sodium caprate,
deoxycholate, glycocholate, taurodyhydrofusidate,
and palmitoylcarnitine increased the Caco 2
permeability. These latter excipients may open the
tight junctions and thus may affect absorption via
the paracellular route.
Excipients which are osmotically active such as
sodium acid pyrophosphate and polyethylene
glycol 400 have been reported to reduce the BA of
ranitidine when present in high concentrations (1–
10 g), likely because these excipients shorten the
small intestinal transit time.38-40
Dissolution
The USP 27 dissolution specification for ranitidine
hydrochloride tablets is not less than 80% (Q)
dissolved in 45 min in 900 mL water, using the
paddle at 50 rpm.41 Relevant dissolution studies
are presented in Table 3. In the reported study of
Ali et al.,42 about 80% of the studied formulations
had trade names that also appear in Table 2. Most
formulations showed rapid dissolution in the
reported medium, however, in most cases the
dissolution curves of these ranitidine products did
not meet the similarity factor (f2)
requirement.12,13 Other studies, using water
instead of the 0.1N HCl as a medium arrived at
analogous results.43-45
Table 3. Dissolution of Ranitidine Hydrochloride IR
Formulations
Formulations Dissolution Rapidly Similarity Re
Method Dissolving of
(>85% in Dissolution
30 min) Profiles (f2)
yes/no yes/no
Generic IR 0.1N HCl, 47: yes; 2: Most
products in DE paddle 50 no profiles: no
rpm
Zantac® 150 Water, 150 mg: 150 mg: no;
and 300 mg paddle 50 no; 300 300 mg: yes
versus BIPI rpm b mg: yes
(USP) 150 and
300 mg
Generic IR Water, Yes —
tablet paddle 50
rpm b
Ranitidine HCl Water, Yes Fast versus
Zantac®, fast, paddle 50 slow: no
medium and rpm b
slow
dissolving IR
tablets a
a The four ranitidine formulations were
bioequivalent to one another.
b Conform to USP 27.
Polli45 investigated the association between the
dissolution rate of three ranitidine hydrochloride IR
tablets and their bioequivalence relative to
Zantac®. The dissolution profiles were recorded
using the USP27 method. There were difference in
dissolution rate, but all four formulations were
found to be bioequivalent in a four way, single
dose bioequivalence study. The author concluded
that differences in dissolution rates observed
earlier than 30 min had negligible consequences in
vivo.
The effect of dissolution rate and gastro intestinal
(GI) transit time on the bioequivalence of ranitidine
has also been studied by computer simulations.46
These simulations also included atenolol (low
permeability) and metoprolol (high permeability). It
was concluded that peak plasma concentrations
(Cmax) appeared to be more sensitive to changes in
dissolution and GI transit times than area under
the curve (AUC). The higher the permeability of the
drug substance, the more sensitive Cmax was to the
dissolution and gastric emptying rates. IR ranitidine
hydrochloride tablets were predicted to be
bioequivalent with an oral solution when
dissolution was as slow as 85% in 1.5 h. This
observation has also been noted for IR tablets of
metformin, which is also a BCS class III drug with a
paracellular transport mechanism. The IR tablets of
metformin had similar in vivo absorption as
modified release tablets if their dissolution rate
was as slow as 85% dissolved in 2 h.47,48
DISCUSSION
Solubility
Ranitidine hydrochloride can be expected to be
“highly soluble” at 37°C over the entire pH range 1–
7.4.12,13
Permeability
The low BA of ranitidine is in line with its low
permeability.
Risks with Respect to Composition
and/or Manufacturing Variations
You might also like
- Ranitidine Hydrochloride PDFDocument9 pagesRanitidine Hydrochloride PDFDanisha LailaNo ratings yet
- Ranitidine HCLDocument9 pagesRanitidine HCLMochammad FerdiansyahNo ratings yet
- PseudoephedrineDocument9 pagesPseudoephedrineStevens GonzalezNo ratings yet
- Ranitidine Hydrochloride PDFDocument9 pagesRanitidine Hydrochloride PDFfadhlyusralNo ratings yet
- Furosemide PDFDocument13 pagesFurosemide PDFariNo ratings yet
- Alicia Delrivo, Carolina Aloisio, Marcela R. Longhi, and Gladys GraneroDocument11 pagesAlicia Delrivo, Carolina Aloisio, Marcela R. Longhi, and Gladys GraneroAyu KarniasariNo ratings yet
- Formulation, Characterization and Evaluation of Sustain Release Table of Selected Drug CandecartanDocument10 pagesFormulation, Characterization and Evaluation of Sustain Release Table of Selected Drug Candecartansimmi kaushikNo ratings yet
- Biowaiver ApproachDocument11 pagesBiowaiver Approachmarco hernandezNo ratings yet
- Sahoo S HPMCDocument19 pagesSahoo S HPMCReza Pahlevi RudiantoNo ratings yet
- In Vitro Studies of Amlodipine Besylate Tablet and Comparison WithDocument7 pagesIn Vitro Studies of Amlodipine Besylate Tablet and Comparison WithBetty Wahyuning TiasNo ratings yet
- Journal of Pharmaceutical and Biomedical Analysi2020.Document13 pagesJournal of Pharmaceutical and Biomedical Analysi2020.mas mnNo ratings yet
- 2014 Aapsj 16 258Document11 pages2014 Aapsj 16 258SCYoungNo ratings yet
- 1 s2.0 S2211383517306767 MainDocument12 pages1 s2.0 S2211383517306767 MainAlah Bacot.No ratings yet
- Ciprofloxacina MonografíaDocument12 pagesCiprofloxacina MonografíaNicolas CastilloNo ratings yet
- Application of Free Radical Diphenylpicrylhydrazyl (DPPH) To Estimate The Antioxidant Capacity of Food SamplesDocument8 pagesApplication of Free Radical Diphenylpicrylhydrazyl (DPPH) To Estimate The Antioxidant Capacity of Food SamplesRashid IlmiNo ratings yet
- Monograph of Chloroquine PhosphateDocument7 pagesMonograph of Chloroquine PhosphateRisa DewiNo ratings yet
- Plank 2012Document9 pagesPlank 2012JOHN HAROLD MENDEZ OREJUELANo ratings yet
- IbuprofenDocument11 pagesIbuprofenЖивка АнгеловаNo ratings yet
- Bcs and BddcsDocument44 pagesBcs and BddcsSiri KalyanNo ratings yet
- Pharmacokinetic of LevodopaDocument10 pagesPharmacokinetic of LevodopaMukesh GamiNo ratings yet
- Dietary Sources of Aldose Reductase Inhibitors: Prospects For Alleviating Diabetic ComplicationsDocument8 pagesDietary Sources of Aldose Reductase Inhibitors: Prospects For Alleviating Diabetic Complicationskhamisi.maryamNo ratings yet
- Nanorifampicin 2Document8 pagesNanorifampicin 2atulskoriNo ratings yet
- LC Determination in Sac Intestine Model PDFDocument12 pagesLC Determination in Sac Intestine Model PDFJose PerezNo ratings yet
- Ritalin ADocument8 pagesRitalin ALeonardo David Dearo SimonettiNo ratings yet
- Food Hydrocolloids: Jianzhong Zhu, Bin Zhang, Chin Ping Tan, Li Ding, Miao Shao, Chun Chen, Xiong Fu, Qiang HuangDocument9 pagesFood Hydrocolloids: Jianzhong Zhu, Bin Zhang, Chin Ping Tan, Li Ding, Miao Shao, Chun Chen, Xiong Fu, Qiang HuangHusnain RazaNo ratings yet
- Formulation Development and Evaluation of Pantoprazole Delayed Release TabletsDocument13 pagesFormulation Development and Evaluation of Pantoprazole Delayed Release TabletsAnish Kumar A0% (1)
- Bio Evailabilitas Dan Bioekivalensi Aciclovir BABEDocument13 pagesBio Evailabilitas Dan Bioekivalensi Aciclovir BABERian Nurdiana100% (1)
- Shulman 2011Document8 pagesShulman 2011Alyna AlynaNo ratings yet
- Method Development, Validation and Forced Degradation Studies of Dapagliflozin and Pioglitazone Hydrochlorides in Synthetic Mixtures by RP HPLCDocument12 pagesMethod Development, Validation and Forced Degradation Studies of Dapagliflozin and Pioglitazone Hydrochlorides in Synthetic Mixtures by RP HPLCEditor IJTSRDNo ratings yet
- PFAS CompendiumCompliantDocument16 pagesPFAS CompendiumCompliantriccadea71No ratings yet
- Peterson 1983Document25 pagesPeterson 1983Ryan PratamaNo ratings yet
- Pioglitazone A Review of Analytical Met - 2014 - Journal of Pharmaceutical AnalDocument8 pagesPioglitazone A Review of Analytical Met - 2014 - Journal of Pharmaceutical AnalDarian HerascuNo ratings yet
- Verbeeck 2017Document35 pagesVerbeeck 2017giyan77No ratings yet
- Jurnal FurosemidDocument13 pagesJurnal FurosemidtyasulistNo ratings yet
- Li Et Al, 2018, Gastric Retention Pellets of Edaravone With Enhanced Oral BioavailabilityDocument8 pagesLi Et Al, 2018, Gastric Retention Pellets of Edaravone With Enhanced Oral Bioavailabilityabdulloh suyutiNo ratings yet
- Formulation, Development and Evaluation of Fast Disintegrating Tablet of Piroxicam Using Solid Dispersion TechniqueDocument20 pagesFormulation, Development and Evaluation of Fast Disintegrating Tablet of Piroxicam Using Solid Dispersion TechniqueEditor IJTSRDNo ratings yet
- Convolution Study On Lansoprazole Delayed-Release Capsules - Application of Similarity Factor To in - Vitro DissolutionDocument11 pagesConvolution Study On Lansoprazole Delayed-Release Capsules - Application of Similarity Factor To in - Vitro DissolutionAnand UbheNo ratings yet
- Formulation and Evaluation of Vilazodone Sublingual Tablets by Using Lyophilization TechniqueDocument9 pagesFormulation and Evaluation of Vilazodone Sublingual Tablets by Using Lyophilization Techniquealamia pharmNo ratings yet
- Sharmin 2016Document9 pagesSharmin 2016skkbd415No ratings yet
- Polymer: Xiaoye Gao, Chaoliang He, Chunsheng Xiao, Xiuli Zhuang, Xuesi ChenDocument8 pagesPolymer: Xiaoye Gao, Chaoliang He, Chunsheng Xiao, Xiuli Zhuang, Xuesi ChenAnda_Ilinca_BooksNo ratings yet
- AcetaminophenDocument11 pagesAcetaminophenShalie VhiantyNo ratings yet
- Characterization of Supersaturatable Formulations For Improved Absorption of Poorly Soluble DrugsDocument11 pagesCharacterization of Supersaturatable Formulations For Improved Absorption of Poorly Soluble DrugsTuan KittiNo ratings yet
- Tsume 2014Document46 pagesTsume 2014Juan PerezNo ratings yet
- Penting BcsDocument26 pagesPenting BcsDEVIANo ratings yet
- 463 PDFDocument4 pages463 PDFandypedeNo ratings yet
- Biorelevant Dissolution Media As A Predictive Tool For Glyburide A Class II Drug PDFDocument8 pagesBiorelevant Dissolution Media As A Predictive Tool For Glyburide A Class II Drug PDFFláviaNo ratings yet
- Commentary Biowaiver Monographs For Immediate Release Solid Oral Dosage Forms: CimetidineDocument11 pagesCommentary Biowaiver Monographs For Immediate Release Solid Oral Dosage Forms: CimetidineManMan AR-llNo ratings yet
- Solubility Evaluations of Osimertinib Mesylate in Physiological BuffersDocument6 pagesSolubility Evaluations of Osimertinib Mesylate in Physiological BuffersBaru Chandrasekhar RaoNo ratings yet
- Evaluating The Degradation, Sorption, and Negative Mass Balances of Pharmaceuticals and Personal Care Products During Wastewater TreatmentDocument7 pagesEvaluating The Degradation, Sorption, and Negative Mass Balances of Pharmaceuticals and Personal Care Products During Wastewater TreatmentLeonardo Andres Acevedo AvilaNo ratings yet
- Lim 2014Document6 pagesLim 2014aprilia ning diahNo ratings yet
- 1 FDocument11 pages1 FSherlyy Kristiani.SNo ratings yet
- Drug SolubilityDocument13 pagesDrug SolubilityBeatrizCamposNo ratings yet
- Latanoprostpaper 2014Document13 pagesLatanoprostpaper 2014ahmed.bouchenakNo ratings yet
- Codein PospatDocument9 pagesCodein PospatDieka Andriani IINo ratings yet
- Journal of PharmaceuticalDocument13 pagesJournal of PharmaceuticaldwiNo ratings yet
- Development and in Vitro Evaluation of Biodegradable Chitosan Microspheres Loaded With Ranitidine and Cross Linked With GlutaraldehydeDocument9 pagesDevelopment and in Vitro Evaluation of Biodegradable Chitosan Microspheres Loaded With Ranitidine and Cross Linked With GlutaraldehydeAnonymous UserNo ratings yet
- Biopharmaceutics Classification System An Industrial ExperienceDocument10 pagesBiopharmaceutics Classification System An Industrial ExperienceanjaniNo ratings yet
- Analytical Biochemistry: T.Z. Rzezniczak, L.A. Douglas, J.H. Watterson, T.J.S. MerrittDocument3 pagesAnalytical Biochemistry: T.Z. Rzezniczak, L.A. Douglas, J.H. Watterson, T.J.S. MerrittGustavo FelpeNo ratings yet
- A Comprehensive Book on Experimental PharmaceuticsFrom EverandA Comprehensive Book on Experimental PharmaceuticsRating: 5 out of 5 stars5/5 (1)
- LIS2sl - 0911 - en SIEMENS SLDocument456 pagesLIS2sl - 0911 - en SIEMENS SLAntonio VazquezNo ratings yet
- Smart Pixel ArrayDocument23 pagesSmart Pixel Arraydevauthor123No ratings yet
- List of Mathematical Symbols - Simple English Wikipedia, The Free EncyclopediaDocument6 pagesList of Mathematical Symbols - Simple English Wikipedia, The Free EncyclopediaRohit RajNo ratings yet
- The Mathematical Gazette Volume 86 Issue 507 2002 (Doi 10.2307 - 3621155) Nick Lord - 86.76 Maths Bite - Sides of Regular PolygonsDocument3 pagesThe Mathematical Gazette Volume 86 Issue 507 2002 (Doi 10.2307 - 3621155) Nick Lord - 86.76 Maths Bite - Sides of Regular PolygonsEduardo CostaNo ratings yet
- High Efficacy of The German Multicenter ALL (GMALL) Protocol For Treatment of Adult Acute Lymphoblastic Leukemia (ALL) - A Single-Institution StudyDocument8 pagesHigh Efficacy of The German Multicenter ALL (GMALL) Protocol For Treatment of Adult Acute Lymphoblastic Leukemia (ALL) - A Single-Institution StudyAnonymous 9dVZCnTXSNo ratings yet
- Test Report 2 4G 4207201Document111 pagesTest Report 2 4G 4207201Ammar OdehNo ratings yet
- Ca 3241Document1 pageCa 3241Tien LamNo ratings yet
- Department of Civil Engineering Lakshmi Narain College of Technology BHOPAL-462021 (INDIA)Document48 pagesDepartment of Civil Engineering Lakshmi Narain College of Technology BHOPAL-462021 (INDIA)Vikash SinghNo ratings yet
- INGEPAC LINE PROTECTION RELAY-overviewDocument2 pagesINGEPAC LINE PROTECTION RELAY-overviewmilan9bNo ratings yet
- WL 80250 4 EA 0510 MainCat Equipment and ServicesDocument116 pagesWL 80250 4 EA 0510 MainCat Equipment and ServicesApetrei Ioan CristianNo ratings yet
- World's Leading Supplier of Infrared (IR) Receivers: OptoelectronicsDocument4 pagesWorld's Leading Supplier of Infrared (IR) Receivers: OptoelectronicsHenry ChanNo ratings yet
- RPI Form PDFDocument1 pageRPI Form PDFJoko WiwiNo ratings yet
- Fast Web View PDF TomcatDocument2 pagesFast Web View PDF TomcatEddieNo ratings yet
- Operating System Interview Questions & AnswersDocument17 pagesOperating System Interview Questions & AnswersBharat AttriNo ratings yet
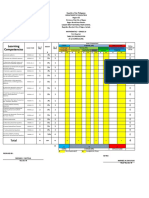
- Learning Competencies: TotalDocument4 pagesLearning Competencies: TotalLaira Joy Salvador - ViernesNo ratings yet
- Science GeographyDocument133 pagesScience Geographysampcant212No ratings yet
- Prmo 2018 QPDocument2 pagesPrmo 2018 QPJatin RatheeNo ratings yet
- Low Shock Stage Separation System For Long Range Missile ApplicationDocument3 pagesLow Shock Stage Separation System For Long Range Missile ApplicationalexNo ratings yet
- ATS (Automatic Trasfer Switch) : 2 Positions (A B)Document4 pagesATS (Automatic Trasfer Switch) : 2 Positions (A B)Berkah Jaya PanelNo ratings yet
- Surpac IntroductionDocument207 pagesSurpac IntroductionKrist Jan Jimenez Separa0% (1)
- Montfort Secondary School Chapter 21: Electromagnetism: Name: Date: ClassDocument12 pagesMontfort Secondary School Chapter 21: Electromagnetism: Name: Date: ClasssonghannNo ratings yet
- Web Technology QuantumDocument335 pagesWeb Technology QuantumabhishekgsNo ratings yet
- BalancesDocument8 pagesBalancescchauling6841No ratings yet
- 24945: FISS 011 - Fisica Experimental II - 005: Coulombs Law SimulationDocument2 pages24945: FISS 011 - Fisica Experimental II - 005: Coulombs Law SimulationAlberto GMNo ratings yet
- FlowLine Level Transmitter Ultrasonic EchoSpan LU80 LU81 LU83 LU84 Data SheetDocument2 pagesFlowLine Level Transmitter Ultrasonic EchoSpan LU80 LU81 LU83 LU84 Data SheetPromagEnviro.comNo ratings yet
- Physical Science Module 3Document22 pagesPhysical Science Module 3Florence-j Pelayo Tupaz100% (1)
- 4 Options To Generate Primary Keys: Generationtype - AutoDocument3 pages4 Options To Generate Primary Keys: Generationtype - AutoAdolfNo ratings yet
- Cambium cmm5 DatasheetDocument2 pagesCambium cmm5 DatasheetSean MarkNo ratings yet
- PP 533-541 HEAT AND MASS TRANSFER IN A SHRINKING CYLINDER DRYINGDocument9 pagesPP 533-541 HEAT AND MASS TRANSFER IN A SHRINKING CYLINDER DRYINGelatani100% (1)