Professional Documents
Culture Documents
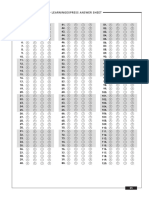
Answers: The Emt-Basic Practice Exam 1
Answers: The Emt-Basic Practice Exam 1
Uploaded by
Jaytee TiryadOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Answers: The Emt-Basic Practice Exam 1
Answers: The Emt-Basic Practice Exam 1
Uploaded by
Jaytee TiryadCopyright:
Available Formats
–the emt-basic Practice exam 1–
Answers 5. c. Fluids containing blood have the highest
potential for disease transmission.
1. b. HEPA respirators are worn when in contact 6. c. An infant who is alert to verbal stimuli will
with patients who have airborne infections still try to locate the parents’ voices; choice a
such as TB. HIV/AIDS and hepatitis B are describes an alert infant; choice d describes
both blood-borne pathogens. Contaminants an infant who is responsive to painful stim-
from open wounds would also be blood uli; choice b is incorrect because infants of
borne. this age are not developed enough to tell you
2. c. Your first action should be to remove your their age regardless of their mental status.
crew and the patient from the possible nox- 7. b. Assess circulation in an infant by palpating
ious gas and to notify the gas company of the the brachial pulse in the upper arm. The
leak. You may also be required to alert the carotid and radial pulses are difficult to locate
hazardous-materials response team. You in infants. Capillary refill time shows that the
should not attempt to locate the gas leak patient has impaired circulation, but it is not
yourself. Treatment for the patient will begin the first tool to use in assessing circulation
with an ABC assessment and management of because it is affected by external f actors (like
any problems you might encounter. the environment) as well as internal factors
3. b. Because ventricular fibrillation is the most like poor perfusion.
common cause of sudden cardiac arrest, it is 8. c. There is no information to indicate that the
critical to apply an AED on an unconscious patient requires ventilatory support. Any
apneic and pulseless patient as quickly as patient experiencing chest discomfort should
possible. The other rhythms can also cause a receive the highest possible concentration of
patient to be in cardiac arrest, but they do oxygen.
not occur as frequently as “V-fib.” 9. a. The rapid trauma survey is used when you
4. a. The patient with chest pain and systolic blood are unsure of the presence of hidden injuries
pressure less than 100 is the highest priority or if the mechanism of injury (MOI) is
patient of the four. A leg injury may be life unclear or severe enough to suggest the need
threatening if the femoral artery is injured, for a rapid assessment. A 2-year-old child
but most often, a single extremity injury is could be severely injured by a medium-speed
not a threat to life. The elderly gentleman may collision, even if he or she appears alert and
be exhibiting his normal mental status, or he was properly restrained. The other choices
may be having problems due to an ongoing do not represent MOIs considered to be high
health problem. You need more information risk for hidden injury.
before you can make that determination, but
he is not in any imminent danger right now.
Labor with contractions six minutes apart is
not considered imminent delivery. If you have
any questions, however, you should continue
assessing this patient as well by asking perti-
nent questions and checking for crowning.
43
03_23-52.indd 43 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
10. c. A supine patient may or may not have jugu- 15. a. You should perform the initial assessment
lar veins that are prominent enough to pal- first, because the unresponsive patient cannot
pate. However, even if the neck veins are direct you to the specific complaint. Vital
normally present when an individual is signs are completed during your second phase
supine, they will not be engorged in blood of patient assessment after you determine
and overly firm to the touch. This is what is treatment priority and have a baseline ABC
meant by the phrase distended neck veins. assessment. You cannot determine the appro-
Distended neck veins (in any position) are a priate course of treatment of any airway
sign of increased circulatory pressure. The problem (including the need for positioning—
carotid pulse should always be palpable. A choice c) until you have first assessed the
decreased radial pulse may indicate hypovo- airway. The SAMPLE history is important
lemic shock or an injured extremity. information to gather, but it should never
11. c. The other rhythms do not benefit from an come before any treatment that may be
electrical shock. The purpose of early defi- needed to correct an ABC abnormality.
brillation is to stop a highly chaotic, disorga- 16. b. Trauma and medical patients who are unre-
nized electrical rhythm such as ventricular sponsive, and all patients who have altered
fibrillation, with the hope that an organized mental status, should receive a detailed phys-
rhythm will begin and generate a pulse. ical assessment. It is easy to overlook some-
12. b. Assess motor function by asking the patient thing when the patient is not conscious
to wiggle his toes; moving the leg or having enough to tell you what hurts or if the MOI
the patient bend the knee can compromise and nature of illness (NOI) are unclear.
spinal stability; option d describes assess- 17. c. The detailed physical assessment is usually
ment of sensation, not motor function. performed in the back of the ambulance
13. b. Patient b is the only one both responsive and during transport; its purpose is to reveal hid-
who has no significant mechanism of injury. den injuries that escaped the initial rapid
14. c. The P component of the OPQRST acronym assessment.
refers to provocation or palliation, or what 18. c. The purpose of ongoing assessment is to
makes the pain feel worse or better. check the adequacy of your initial interven-
tions. The detailed examination is designed
to find missed injuries.
19. d. Do CPR. American Heart Association guide-
lines advise that even if there is an organized
rhythm, a pulse will not be palpable immedi-
ately after a shock. CPR is crucial to main-
tain blood flow and ventilation during this
time.
20. c. Only those patients who are unresponsive,
pulseless, and apneic should have the AED
applied.
44
03_23-52.indd 44 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
21. a. You could make the argument that you need 25. c. During capillary–cellular exchange, oxygen
additional help in the management of each enters the body cells and carbon dioxide
of these situations; however, the one with the enters the capillaries; choices a and b
most critical need is when you must care for describe alveolar-capillary exchange; choice
more than one critical patient. Both patients d describes cellular digestion.
with gunshot wounds need immediate atten- 26. d. Accessory muscles may be seen in use in the
tion, so you should call for backup. In the neck and as retractions above the clavicles
other three situations, you should not and/or between the ribs. These muscles are
require assistance unless some complicating used when greater than normal inspiratory
factor presents itself. Patient b may or may and/or expiratory pressures are needed to
not require ALS assistance, but most (over move air. Normal breathing does not pro-
80%) deliveries are simple and uncompli- duce any audible sounds, but it will produce
cated and can be easily managed by basic life auscultatory sounds (heard with a stetho-
support (BLS) providers. Patient c is having scope). Warm, dry skin and equal chest
a febrile seizure, which is managed by stabi- expansion are both signs of adequate
lizing the ABCs and transporting. In patient breathing.
d, even if your partner is required to stabilize 27. d. Bell’s palsy is the most common form of
the cervical spine, you should be able to facial paralysis. Muscular dystrophy is a
manage the patient for the time being until degenerative disease characterized by the
other assistance arrives to assist with packag- weakening of skeletal muscle fibers. ALS, also
ing and moving the patient. known as Lou Gehrig’s disease, affects the
22. c. The epiglottis is the leaf-shaped structure nerve cells that control voluntary movement.
that closes off the trachea during swallowing. Dystonia describes repetitive motions or
The larynx is the voice box, the structure abnormal posturing.
that produces speech vibrations; the cricoid 28. a. A gurgling sound means that the patient
cartilage forms the lower portion of the lar- needs to be suctioned immediately; ventila-
ynx; the diaphragm is a large muscle that tion cannot be adequate when the airway is
contracts to initiate inhalation. blocked from mucous, blood, or other
23. d. The alveoli are the numerous minute air sacs secretions.
that make up the lungs; bronchioles are 29. b. Correct order of steps would be b, c, a,
small branches of the bronchi, which are the and d.
two main tubes branching from the trachea; 30. b. The seizure event is referred to as ictal, hence
the epiglottis is the structure that closes off postictal refers to the period after the seizure
the trachea during swallowing. wherein a patent is often confused for a
24. a. Other symptoms of pulmonary edema may period of time.
include difficulty breathing, excessive sweat- 31. b. Choice b is the correct procedure. Choice a
ing, anxiety, and pale skin. is correct for a rigid catheter, choice c is the
correct method for inserting an oropharyn-
geal airway, and choice d is applicable only
to endotracheal intubation.
45
03_23-52.indd 45 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
32. c. Choice c is the correct procedure for clearing 40. a. The cricoid cartilage forms a ring of firm car-
the airway when simple suctioning is not tilage and is located inferior to (below) the
working. Choice b is appropriate for a larynx.
patient with copious frothy secretions like 41. a. A means alert. The other letters in the acro-
the kind produced with pulmonary edema. nym stand for verbal, pain, and unrespon-
Choices a and d are inappropriate without sive.
first clearing the airway. 42. b. A bulb syringe is used to suction an infant’s
33. d. The purpose of the head-tilt/chin-lift is to nasal passage or mouth and is generally used
move the tongue and epiglottis out of the with infants up to age 3–4 months. If you are
way of the airway; it is not useful for intuba- using mechanical or hand-powered suction
tion (use the sniffing position), to remove equipment in infants of this age, be very
foreign bodies, or to visualize the larynx. careful to use the lowest possible pressures
34. b. After opening the airway, the EMT should needed to accomplish the job.
assess the rate and depth of ventilations; 43. c. The right ventricle receives oxygen-poor
choices a, c, and/or d would occur only after blood from the right atrium. It then pumps
respiratory adequacy has been assessed and the blood to the lungs via the pulmonary
they are appropriate to use. artery, where it receives oxygen and releases
35. d. Cyanosis, or a bluish coloration of the carbon dioxide.
mucus membranes and skin, is caused by 44. c. The role of the EMT-Basic is not to diagnose
inadequate oxygen supply to the body tis- the exact cause of the patient’s chief com-
sues; the other choices are unrelated to plaint. Maintaining a high suspicion for a
oxygen supply. cardiac emergency will guide your next step
36. a. Masks come in adult and pediatric sizes. In in managing this patient appropriately.
order to deliver the highest possible concen- 45. d. Your first action would be to administer oxy-
tration of oxygen to the patient, you must gen and place the patient in a comfortable
have a properly fitting mask. Steps d, b, and c position; next, if not contraindicated, you
must then be completed (in that order) would request permission to administer
before placing the mask on the patient’s face. nitroglycerin. You should first obtain a set of
37. c. After sealing the mask to the patient’s face, vital signs to ensure he is not in cardiogenic
you should begin mouth-to-mask ventila- shock. Never put defibrillator pads onto a
tion with a long, slow breath; steps a, b, and conscious patient with a pulse; this proce-
d should be done before applying the mask. dure is contraindicated. AED pads are not
38. d. The correct rate is 12 ventilations per minute serving the same function as the electrodes
for an adult (one breath every five seconds), used by ALS providers to monitor the heart
and the correct rate for a child is 20 ventila- rhythm.
tions per minute. 46. a. Prehospital ACLS provides additional medi-
39. d. During a two-person bag-valve-mask proce- cations and other therapies that may help
dure, one EMT ventilates the patient while either terminate the cardiac arrest state or
the other maintains the airway and monitors help prevent the patient who has regained a
the patient’s chest rise. pulse from going back into cardiac arrest.
46
03_23-52.indd 46 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
47. a. Although you note several injuries, you still 54. d. This patient has the classic signs and symp-
need to perform a rapid initial assessment to toms of shock. Do not offer anything to eat
determine if any problems with the ABCs that or drink to a patient you suspect of being in
you have not noted may be more life threat- shock, since surgery may be necessary later.
ening than what you can obviously see. Stop 55. c. Speed is squared in the calculation of kinetic
the bleeding (but do not use a tourniquet) energy. A one-pound object traveling at 30
and treat the patient for shock, but do not ele- mph is nine times more injurious than a
vate the patient’s legs if there is an injury to one-pound object traveling at 10 mph.
the legs, pelvis, head, neck, chest, abdomen, or 56. b. Ventricular tachycardia often converts to
spine. There is no indication that this patient ventricular fibrillation, a life-threatening
needs ventilation at this time. heart rhythm that the AED is designed to
48. d. When the SAED is attempting to analyze the correct.
patient’s electrical rhythm, any movement of 57. c. Stop CPR briefly to verify pulselessness and
the patient or the unit could cause the apnea. Once you have the leads ready for
machine to misinterpret the signal. placement on the chest wall, you should stop
49. c. Safety is critical when performing defibrilla- CPR, clear away from the patient, attach the
tion. Any defibrillation attempt in the rain AED leads, and perform the initial analysis.
may possibly harm anyone near the patient Resume CPR after the first round of shocks
during the discharge of the unit. if they were unsuccessful and the patient
50. c. The pressure point for wounds of the fore- persists in pulselessness. Stop CPR again
arm is the brachial artery. every time you deliver shocks.
51. a. Kinetic energy is the energy an object has 58. d. After three consecutive “no shock indicated”
while in motion. Choice b describes mass, messages, you should make sure to begin
choice c describes energy, and choice d transporting the patient while continuing
describes inertia. CPR. Some jurisdictions may adopt a proto-
52. c. Having the bystander stop CPR will allow col or standing order that requires you to
you to reassess the patient’s ventilatory and consider transporting following the first or
circulatory status. This will tell you whether second set of AED rounds, regardless of
you need to continue CPR or whether the whether you shock. At the minimum, you
patient has regained a pulse or is breathing. should begin your transport by the third time
53. a. Venous bleeding flows in a steady, dark-red you perform an analysis.
stream. Arterial bleeding is bright red and 59. a. If the patient has been resuscitated but is still
spurts from the wound, while capillary unresponsive, check the pulse every 30 sec-
bleeding oozes. Internal bleeding may or onds during transport and keep the AED
may not present externally recognizable leads attached to the patient.
signs or symptoms.
47
03_23-52.indd 47 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
60. c. If it becomes necessary to deliver shocks 67. c. Tertiary blast injury includes those injuries
while en route with the patient, the proper resulting from structural collapse.
procedure is to stop the vehicle before reana- 68. d. Assess pulse, motor function, and sensation
lyzing the rhythm because the AED has a distal to a splint both before and after apply-
motion detector sensor in place that will not ing the splint to ensure that the splint is not
allow the unit to operate in the presence of adversely affecting circulation to the limb.
motion. 69. c. Tilting the head may compromise the stabili-
61. d. The primary action of nitroglycerin is to zation of the cervical spine when using the
dilate the myocardial (coronary) arteries, modified jaw thrust.
therefore easing the heart’s workload by 70. b. The first 60 minutes after the occurrence of
increasing the blood flow. Lowering of blood multisystem trauma is the golden hour.
pressure is a secondary effect seen with vessel 71. a. Blood is too fluid to be cleared adequately by
dilation. Reflex tachycardia, not bradycardia, a finger sweep. The other answers are not
may occur as a result of nitroglycerine appropriate unless the airway was cleared
administration. It does not have any direct first by suction.
effects on the muscles of the heart. 72. d. Before transporting a patient without con-
62. b. Myocardial pain is often difficult to deter- sent, it is best to always seek medical direc-
mine because it can take on many different tion.
characters; however, patients most com- 73. c. While the other answers may be true, they
monly (over 40% of the time) describe the may occur regardless of the time interval.
pain of a myocardial infarction as a crushing, 74. c. The one-way valve minimizes potential
squeezing pressure that radiates outward to cross-exposure of the patient’s secretions
the arms and upper back. and exhaled breath to the rescuer.
63. a. Children often turn toward the impact and 75. a. Administer oral glucose on medical direction
are often thrown down and under the (through protocol or standing order) only to
vehicle. patients with altered mental status and his-
64. a. The combination of direct pressure, eleva- tory of diabetes. Patient b should be first
tion, pressure dressing, and pressure point treated as a trauma patient, and because
pressure is almost always successful in stop- research shows poor outcomes following
ping bleeding in the extremities. Tourniquets brain injuries and glucose administration, it
are seldom needed. PASG use is performed is best to withhold its use until blood sugar
cautiously under direct medical control, and can be checked (which is an ALS-provider
it is never the first line of t reatment. skill in many areas). Patient c is not appro-
65. d. Lifting the jaw is necessary to dislodge the priate because of an inability to swallow
tongue from the back of the throat and pro- properly; ALS should be called to provide IV
vide a patent airway. dextrose to this patient. Glucose should be
66. b. The head-tilt/chin-lift may jeopardize the withheld until you can better determine if
patient’s cervical spine. The other two proce- patient d is actually diabetic or not. (A blood
dures will not adequately open the airway. glucose reading would be helpful with this
patient as well.)
48
03_23-52.indd 48 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
76. c. Common causes of altered mental status 82. c. The goal of care in cases of localized cold
include trauma, diabetes, seizures, and infec- damage is to prevent further damage by
tious disease. Asking about fever helps deter- removing the patient from the cold environ-
mine if there is a history of recent infection. ment and protecting the damaged tissues
77. d. Signs of allergic reactions include increased from further injury. Rewarming is best
heart rate, as the heart attempts to compen- accomplished in the hospital setting, where
sate for hypoperfusion. The two primary pain medication can be administered and
life-threatening events that occur during an the danger of reinjury due to recooling is
allergic reaction are profound vasoconstric- diminished.
tion (resulting in shock) and compromised 83. a. A hyperthermic patient with hot skin must
airway due to swelling, constriction, or be treated aggressively before permanent
mucous production. organ damage sets in. When the skin is hot
78. c. EMTs can administer epinephrine under and dry, the normal sweating mechanisms
medical direction only if the medication was have stopped functioning and the patient is
previously prescribed for this patient. The in danger of brain damage due to excessive
patient will be prescribed the correct dosage high body temperature.
by the physician, and you are only allowed to 84. c. Grabbing a stinger with tweezers or your fin-
administer the patient’s own medication. gers can squeeze more venom into the
79. a. This is the principles of conduct; concerns wound (also, there is personal risk of acci-
for what is right or wrong, good or bad. dental exposure to the venom if you use your
Choice b describes morals, choice c is a bet- hands). Instead, scrape the stinger out of the
ter description of bioethics, and choice d skin with a piece of cardboard or rigid plas-
describes justice for the patient. tic (a credit card is ideal). Cutting around
80. b. Care for a hypothermic patient with a dimin- the stinger causes more tissue damage.
ished level of responsiveness should include 85. a. A tort is a civil wrong committed by one
passive rewarming (blankets and heated individual against another. Improper or neg-
room) only; active rewarming should take ligent patient care would be considered a
place only in the hospital environment, and tort.
hypothermic patients should not be allowed 86. b. Choice b describes early respiratory distress.
to exercise or to take stimulants, such as coffee Choice a describes the signs of impending
or tea. However, your protocols may allow respiratory arrest from insufficiency, choice c
you to give warmed liquids that are not alco- describes respiratory failure, and choice d
holic or caffeinated to slightly hypothermic describes airway obstruction.
patients with a normal mental status. 87. d. For patients who have routine seizures and
81. d. Cool skin on the abdomen is a reliable sign whose condition returns to normal quickly
of hypothermia in a patient because the after a seizure, you should request medical
abdomen is in the central core of the body direction about whether to transport.
and is generally covered under layers of 88. b. Multiple injuries, conflicting stories of the
clothing. cause, and repeated calls to the same address
are characteristic of child abuse.
49
03_23-52.indd 49 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
89. a. Suctioning the baby’s mouth and nose will 97. c. The presence of a bloody show (which is the
help to open the airway while the baby has expulsion of the mucous plug from the
not yet begun breathing. You should not mouth of the cervix) occurs during the first
force any part of the delivery process. stage of labor. It is normal and indicates that
90. b. Care for a responsive child consists of stand- the cervix is beginning to open or dilate and
ing behind the child and attempting to may occur several hours prior to delivery.
relieve the obstruction with a series of sub- The second stage of labor continues until the
diaphragmatic thrusts. baby is born.
91. a. Signs of respiratory failure include altered 98. d. There can be large blood loss suffered by the
mental status and a slow or fast breathing mother during a miscarriage. The EMT-
rate with fatigue. There is not enough infor- Basic should treat the patient for possible
mation to determine if patients b and c are shock as well as provide emotional care.
in respiratory insufficiency, respiratory fail- 99. a. More than 500 mL of blood loss after deliv-
ure, or impending respiratory arrest. Patient ery is excessive; massage the mother’s abdo-
d is in impending respiratory arrest. men by rubbing firmly in one direction from
92. b. Profuse vaginal bleeding may indicate a true the symphasis pubis bone toward the umbi-
obstetrical emergency such as uterine rup- licus. This will help the uterus contract and
ture or torn placenta. stop the bleeding. Oxygen administration,
93. b. Select the correct-size oral airway for an shock treatment, and rapid transport will
infant or child by measuring from the corner follow uterine massage.
of the patient’s mouth to the angle of the 1
00. d. If meconium is present in the amniotic fluid,
jaw. suction the infant before stimulating it to
94. a. Vitreous humor is found behind the lens of cry, then notify the hospital of the presence
the eye. It is the clear gel that fills the space of meconium. An ALS crew may be able to
between the lens and the retina. Aqueous perform tracheal suctioning and intubate the
humor is a thick, watery substance that fills infant. If the lungs are stiff and noncompli-
the space between the lens and the cornea. ant, it may indicate that aspiration of the
95. c. If the cord is wrapped around the infant’s meconium has occurred. Aspiration pneu-
neck and you cannot easily loosen and monia due to meconium is often fatal.
remove it, you should clamp it in two places
and cut the cord.
96. a. This newborn has a high Apgar score; there
is no need for respiratory support unless the
condition changes. You should always follow
the steps in the inverted pyramid for neona-
tal resuscitation by drying and warming,
positioning the head down for drainage, suc-
tioning the airway and nose as needed, and
providing tactile stimulation to stimulate
breathing.
50
03_23-52.indd 50 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
101. d. In addition to providing routine emergency 105. d. Bleeding control with spurting blood carries
care, care for a rape victim should focus on maximum danger of contamination, and
preserving evidence and providing comfort maximum protection is therefore required.
and reassurance. Although you want to pro- Airway suctioning or intubation does not
vide comfort to the patient, you should not generally require the use of a cover gown,
allow him or her to shower or change and cleaning contaminated instruments does
clothes, as this will destroy evidence. Any not generally require eye/facial protection
clothing or personal effects that are removed unless there is danger of splashing.
from the patient should be placed in paper 106. a. Abandonment occurs when you relinquish
bags to prevent the growth of bacteria that care without a patient’s consent or without
might occur if stored in plastic bags. You insuring that care is continued by someone
should not need to examine the genital or of the same or higher level, such as a para-
rectal area unless you note significant medic, ALS unit, or physician.
bleeding. 107. c. EMTs should not enter a crime scene until it
102. a. This condition, called supine hypotension has been secured by police. As you travel to
syndrome, is the result of compression that the scene, you should determine where it is
the enlarged uterus causes on the vena cava most appropriate to park your vehicle. Gen-
of the maternal circulatory system. This cor- erally, you want cover (protection from
rective position, called the left lateral recum- attack) and concealment (out of direct visual
bent position, is accomplished by placing the range) in your staging area.
mother on her left side with her legs bent 108. b. To avoid misunderstanding, always repeat
slightly or kept straight. Maternal positional medical orders exactly as you heard them.
changes have no effect on the speed of labor Once you have done that, you can question
or the position of the infant in the birth any order you do not understand or about
canal. By assisting in venous blood return in which you are unclear. When you complete
the mother, you will get the secondary effect your written patient-care report, you should
of increasing blood flow to the uterus, but include the order in your report.
this is a secondary effect seen in correcting 109. b. The sensation of needing to move one’s bow-
supine hypotension s yndrome. els during labor is the result of the head
103. b. The patient is likely to deliver imminently, so pressing down on the anal sphincter as the
prepare for a normal delivery. baby passes through the birth canal. The
104. c. Never enter a scene where hazardous materi- head is very close to the opening of the birth
als are present until you have verified that canal, and delivery is imminent.
the scene is safe. Use binoculars to survey the 110. b. An adult of sound mind can refuse treat-
scene from a distance in order to identify ment, but the EMT should first make an
hazardous materials placards. Consider vic- effort to clearly explain the consequences;
tims and bystanders contaminated and take refusal of treatment should be documented
appropriate precautions. in writing.
51
03_23-52.indd 51 8/24/11 12:24 PM
–the emt-basic Practice exam 1–
111. a. An emergency move is required in a situation 116. d. Patients with breathing difficulties and seri-
where a patient is in immediate life- ous bleeding receive the highest priority in a
threatening danger. Emergency moves require multiple-casualty situation.
only cervical spine stabilization (if it is a 117. c. Do not assume that an elderly patient is
trauma situation) and should be performed incompetent, deaf, or confused. Address all
quickly. Once the patient is in a safer location, patients respectfully.
you should begin with your initial assessment 118. d. Patient information can be released only if
as you do in all patient situations. the patient has signed a specific consent
12. c. Bacterial meningitis has an incubation
1 form.
period of 2–10 days. Bacterial infections of 119. a. If you are informed of a do not resuscitate
the meninges are extremely serious illnesses, order but do not actually see it, you must
and may result in death or brain damage still provide all necessary care.
even if treated. 120. c. You are responsible for helping make your
113. b. The uterus is most easily felt just above the patient feel at ease, but you are also responsi-
navel. ble for operating your ambulance in the saf-
14. c. An incident management system is a coor
1 est possible way.
dinated system of procedures that allows for
smooth operations at the scene of an
emergency.
15. b. Placing napkins in the birth canal will not
1
stop the source of bleeding. Placing bulky
dressings or sanitary napkins at the vaginal
opening will help prevent the blood from
spreading.
52
03_23-52.indd 52 8/24/11 12:24 PM
You might also like
- Secondary SurveyDocument14 pagesSecondary SurveyNi wayan mirayantiNo ratings yet
- Nursing Iv The Secondary Survey in Basic Cardiac Life Support (BCLS)Document14 pagesNursing Iv The Secondary Survey in Basic Cardiac Life Support (BCLS)Ni wayan mirayantiNo ratings yet
- Chapter 11Document11 pagesChapter 112071317No ratings yet
- Rationale, Pre-Test Post-TestDocument9 pagesRationale, Pre-Test Post-TestNina OaipNo ratings yet
- Exam Questions Samples - NCLEXDocument7 pagesExam Questions Samples - NCLEXJusta Victorin100% (4)
- CardiacDocument10 pagesCardiacMarcus Reynolds100% (1)
- MS Compre 2015A Ans KeyDocument8 pagesMS Compre 2015A Ans KeyPaul Lexus Gomez LorenzoNo ratings yet
- Premature Ventricular Contractions: Reassure or Refer?: ReviewDocument7 pagesPremature Ventricular Contractions: Reassure or Refer?: ReviewFahmi RaziNo ratings yet
- Ngeles Niversity OundationDocument10 pagesNgeles Niversity OundationJhaymee Pineda100% (1)
- FUNDA 2 Ratio 2023Document16 pagesFUNDA 2 Ratio 2023Danielle Ann ChiongNo ratings yet
- Paramedic Exam 4Document27 pagesParamedic Exam 4mohamedarafa01224894064No ratings yet
- Assessment Clients With Life Threatening Conditions / Medical EmergenciesDocument23 pagesAssessment Clients With Life Threatening Conditions / Medical EmergenciesJannen CasasNo ratings yet
- Neuro Nursing With RationaleDocument7 pagesNeuro Nursing With Rationalemaestro1020100% (2)
- IntegumentaryDocument8 pagesIntegumentaryRamon Carlo AlmiranezNo ratings yet
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyFrom EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNo ratings yet
- Vol1 PatientCare.09Document13 pagesVol1 PatientCare.09Ahmad UsmanNo ratings yet
- Nursing Practice 3Document8 pagesNursing Practice 3JhannNo ratings yet
- MS BulongDocument27 pagesMS BulongVia LatrasNo ratings yet
- 100 ThoughtsDocument3 pages100 Thoughtsraju_pnNo ratings yet
- Pre Test Post TestDocument3 pagesPre Test Post TestNina Oaip100% (1)
- Guía para Hacer Examen Físico Por Telemedicina.Document4 pagesGuía para Hacer Examen Físico Por Telemedicina.Juan Carlos CamejoNo ratings yet
- DEMYSTIFIEDDocument22 pagesDEMYSTIFIEDSTUDENTNURSESOONRN2024No ratings yet
- Chapter 38: Cardiovascular Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument7 pagesChapter 38: Cardiovascular Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- FUNDA Part 1 RatioDocument6 pagesFUNDA Part 1 RatioJo Hn VengzNo ratings yet
- Fundamentals in NursingDocument15 pagesFundamentals in NursingAngie Bucio MiraNo ratings yet
- Pre-Operative Assessment Study Guide REVISED: 2018: Created By: Edited By: Dr. Chris Young June 2018Document30 pagesPre-Operative Assessment Study Guide REVISED: 2018: Created By: Edited By: Dr. Chris Young June 2018Navdeep RandhawaNo ratings yet
- Le CompilationDocument5 pagesLe CompilationKhrisha Anne DavilloNo ratings yet
- Evaluation of Neck MassDocument17 pagesEvaluation of Neck MassMuammar Aqib MuftiNo ratings yet
- Reply From The Authors - BjaDocument2 pagesReply From The Authors - BjaRENAULTNo ratings yet
- Approach To A Newborn With Suspected CHD: February 2012Document10 pagesApproach To A Newborn With Suspected CHD: February 2012akshayajainaNo ratings yet
- NLE2Document10 pagesNLE2giansulakisosuNo ratings yet
- Emergency Nursing Ratio Exam No. 1Document8 pagesEmergency Nursing Ratio Exam No. 1Charisse TaylanNo ratings yet
- Free 137 AnswerDocument14 pagesFree 137 Answermerontesfaye51No ratings yet
- All The Questions in The Quiz Along With Their Answers Are Shown BelowDocument26 pagesAll The Questions in The Quiz Along With Their Answers Are Shown BelowRey Pama SaguireNo ratings yet
- New Step 2 CK Free 120 Answer Explanations PDFDocument20 pagesNew Step 2 CK Free 120 Answer Explanations PDFEmad Khan67% (3)
- Practice Test 8 ANSWER KEYDocument17 pagesPractice Test 8 ANSWER KEYRamon Carlo AlmiranezNo ratings yet
- Medical Surgical Nursing Assessment and Management of Clinical Problems Lewis 9th Edition Test BankDocument7 pagesMedical Surgical Nursing Assessment and Management of Clinical Problems Lewis 9th Edition Test BankPeterThomasizbjf100% (86)
- 10 Assessment and Care of Ent Problems: S Carter, C LairdDocument13 pages10 Assessment and Care of Ent Problems: S Carter, C LairdRemaja IslamNo ratings yet
- Trauma in Children PDFDocument11 pagesTrauma in Children PDFLory cNo ratings yet
- Emergency Nursing Exam and RatioDocument5 pagesEmergency Nursing Exam and RatioCharisse TaylanNo ratings yet
- Week 5 NCLEX QuestionsDocument6 pagesWeek 5 NCLEX QuestionsGwenn SalazarNo ratings yet
- NCM NEURO DISORDERS ASSIGN - QDocument14 pagesNCM NEURO DISORDERS ASSIGN - QDanica Joy Vinluan JacobaNo ratings yet
- Screening TestsDocument16 pagesScreening TestsVajirawit PetchsriNo ratings yet
- Nstable Trial Achycardia: A Case For High-Fidelity Simulation in Emergency MedicineDocument37 pagesNstable Trial Achycardia: A Case For High-Fidelity Simulation in Emergency MedicineMaryam Ahmad SharifuddinNo ratings yet
- Acute Ataxia in Children: Practice GapsDocument14 pagesAcute Ataxia in Children: Practice Gapsalain reyes100% (1)
- Neuro ALL DISORDERSDocument17 pagesNeuro ALL DISORDERSizuku midoriyaNo ratings yet
- Cmca Unit2Document25 pagesCmca Unit2Jomil IrisariNo ratings yet
- AoBP Fall 2021Document16 pagesAoBP Fall 2021Juan Carlos LopezNo ratings yet
- Answers and Rationales: P, D, M C Nclex-Rn EDocument20 pagesAnswers and Rationales: P, D, M C Nclex-Rn ENursyNurseNo ratings yet
- CGHMC Laboratory PhlebotomyDocument4 pagesCGHMC Laboratory Phlebotomyjaemin naNo ratings yet
- Forceps Delivery ActivityDocument3 pagesForceps Delivery ActivityReyniel BulaklakNo ratings yet
- MS Ii MT2Document11 pagesMS Ii MT2Rika MaeNo ratings yet
- Examinationofthepatient Withdizzinessorimbalance: Gregory T. WhitmanDocument11 pagesExaminationofthepatient Withdizzinessorimbalance: Gregory T. WhitmanVanetNo ratings yet
- Nursing Care Plan and Drug Study: University of Cebu - Banilad Campus Banilad, Cebu City College of NursingDocument16 pagesNursing Care Plan and Drug Study: University of Cebu - Banilad Campus Banilad, Cebu City College of NursingVinz OñoNo ratings yet
- Section 6: MedicalDocument4 pagesSection 6: MedicalpelukisbintangNo ratings yet
- Basic Life Support: Trinity University of Asia - College of Medical TechnologyDocument8 pagesBasic Life Support: Trinity University of Asia - College of Medical Technologyrgng_18803040No ratings yet
- Cardiac Examination and Evaluation of Murmurs: Education GapsDocument10 pagesCardiac Examination and Evaluation of Murmurs: Education GapsclaudyNo ratings yet
- Anti Bagsak Nira Ante1Document13 pagesAnti Bagsak Nira Ante1Jade CentinoNo ratings yet
- 4TH Year QuizbowlDocument4 pages4TH Year QuizbowlZoe Jeanne GarcianoNo ratings yet
- Step 3 Board-Ready USMLE Junkies: The Must-Have USMLE Step 3 Review CompanionFrom EverandStep 3 Board-Ready USMLE Junkies: The Must-Have USMLE Step 3 Review CompanionNo ratings yet
- E 1 PDFDocument17 pagesE 1 PDFJaytee TiryadNo ratings yet
- Organizational Culture: Jose Tirso B DayritDocument35 pagesOrganizational Culture: Jose Tirso B DayritJaytee TiryadNo ratings yet
- In Partial Fulfillment of The Requirement For The Course of Principles of Nursing Health Care AdministrationDocument6 pagesIn Partial Fulfillment of The Requirement For The Course of Principles of Nursing Health Care AdministrationJaytee TiryadNo ratings yet
- In Partial Fulfillment of The Requirement For The Course of Principles of Nursing Health Care AdministrationDocument6 pagesIn Partial Fulfillment of The Requirement For The Course of Principles of Nursing Health Care AdministrationJaytee TiryadNo ratings yet
- What Color Is Your Parachute A Practical Manual For Job-Hunters and Career-ChangersDocument10 pagesWhat Color Is Your Parachute A Practical Manual For Job-Hunters and Career-Changerskraagesh100% (4)
- DPRC Working Estimate - 2 - Final - 9.3.17 - Part (A+B)Document159 pagesDPRC Working Estimate - 2 - Final - 9.3.17 - Part (A+B)D.V.Srinivasa RaoNo ratings yet
- Case Report: Open Fracture 1/3 Distal Os Tibia and Fibula SinistraDocument34 pagesCase Report: Open Fracture 1/3 Distal Os Tibia and Fibula SinistraFarizka Dwinda HNo ratings yet
- Wärtsilä Dynamic Maintenance Planning (DMP) and Condition Based Maintenance (CBM)Document17 pagesWärtsilä Dynamic Maintenance Planning (DMP) and Condition Based Maintenance (CBM)Heryanto SyamNo ratings yet
- Shilpa B.ed. NotesDocument19 pagesShilpa B.ed. Notesshilpa kumariNo ratings yet
- Fifas Kerala Coconut OilDocument16 pagesFifas Kerala Coconut OilManu MohanNo ratings yet
- ENG 110-Task 4 (Unintended Messages)Document2 pagesENG 110-Task 4 (Unintended Messages)Erika Noreen Dela RosaNo ratings yet
- MoRD Specification For Rural Roads 2014Document626 pagesMoRD Specification For Rural Roads 2014Manoj81% (16)
- MG-880 Specification PDFDocument3 pagesMG-880 Specification PDFMartin HasskelNo ratings yet
- STEM Biology 1 SET 11 Week 7 EnzymesDocument20 pagesSTEM Biology 1 SET 11 Week 7 EnzymesAlea Apruebo67% (3)
- Basics of Energy and Environment - 2024Document14 pagesBasics of Energy and Environment - 2024igiri0% (1)
- Stages of DevelopmentDocument12 pagesStages of DevelopmentGoldenUmbreonNo ratings yet
- Market StudyDocument13 pagesMarket StudyJulie Ann VergadoNo ratings yet
- Apgvb Insurance Consent LetterDocument1 pageApgvb Insurance Consent LetterMahesh PasupuletiNo ratings yet
- Ionic and Covalent Compounds BibleDocument45 pagesIonic and Covalent Compounds Bibleapi-270151265No ratings yet
- Hospital StandardQC FormsDocument22 pagesHospital StandardQC FormstotqmNo ratings yet
- The Olympic Torch IELTS Reading Answers With Explanation: Dol Ielts Đình L CDocument7 pagesThe Olympic Torch IELTS Reading Answers With Explanation: Dol Ielts Đình L CThanh MaiNo ratings yet
- Anaplasma Marginale: Infection in A Buffalo: A Case ReportDocument3 pagesAnaplasma Marginale: Infection in A Buffalo: A Case ReportshivarajuNo ratings yet
- A Walk To Remember, Chapter Quizzes, Part IIIDocument4 pagesA Walk To Remember, Chapter Quizzes, Part IIILisa WardNo ratings yet
- Mining Catalog Combined LRDocument125 pagesMining Catalog Combined LRvitor santosNo ratings yet
- Santiago - Green TechnologiesDocument6 pagesSantiago - Green TechnologiesJoshua SantiagoNo ratings yet
- Colorimetric Determination of PHDocument45 pagesColorimetric Determination of PHJudy Ann CocadizNo ratings yet
- SAB Flexible Cables C1Document20 pagesSAB Flexible Cables C1Carlos OzaetaNo ratings yet
- Postgraduate Diploma in Music Therapy - 輔導、心理學, 音樂及管理, 親子及家庭, 教育, 護理學及健康護理課程Document5 pagesPostgraduate Diploma in Music Therapy - 輔導、心理學, 音樂及管理, 親子及家庭, 教育, 護理學及健康護理課程Maggie WongNo ratings yet
- MankindDocument23 pagesMankindanandkas2005100% (1)
- HW 9 - Incomplete and CodominanceDocument2 pagesHW 9 - Incomplete and CodominanceRanuzejNo ratings yet
- Biology7 Ebooks ListDocument23 pagesBiology7 Ebooks ListHossein HeydariNo ratings yet
- Reverse Vaccinology Basics and Applications 2157 7560.1000194Document5 pagesReverse Vaccinology Basics and Applications 2157 7560.1000194Yooobsan Nii barriitiNo ratings yet
- Contemporary Trends in The Treatment Modalities andDocument4 pagesContemporary Trends in The Treatment Modalities andProsthodontics DeptNo ratings yet
- Poly BraidDocument1 pagePoly BraidMuhammad PandorNo ratings yet