Professional Documents
Culture Documents
2019 Survey 4 - Generic Report PDF
Uploaded by
ridzal RidroidOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2019 Survey 4 - Generic Report PDF
Uploaded by
ridzal RidroidCopyright:
Available Formats
Page 1 of 8
Bacteriology Program
Modules: Throat, Skin, AFB stain, Difficult/Blood culture and
Mycobacteriology culture.
Generic Report
2019, Survey 4
Report prepared by
RCPAQAP Microbiology
Version 1: Initial Publication
Copyright
This material is copyright and may not be used in any form for advertising, sales promotion or publicity. The material may not be reproduced in whole or in part for any
purpose whatsoever (including presentations at meetings and conferences), without the prior written permission of the RCPA Quality Assurance Programs Pty
Limited. Permission must be sought in writing from the Program but will not be unreasonably refused.
Confidentiality
RCPA Quality Assurance Programs Pty Limited keeps all participant details confidential. No information related to any of the participants will be divulged to a third party,
unless required by legislation, without the express written consent of the participant. General information may be discussed at meetings or presented as papers to journals.
RCPA Quality Phone +61 2 9045 6000 © 2019 RCPA Quality Assurance Programs Pty Ltd. All rights reserved
Assurance Programs Fax +61 2 9356 2003 Report Issued Friday, 2 August 2019
ABN 32 003 520 072
Suite 201, 8 Herbert Street Accredited for compliance with ISO/IEC 17043
St Leonards NSW 2065 Accreditation Number: 14863
Report ID: MIBP2019040000000000Gener01
Report issued: 2/08/2019 Page 2 of 8
FINAL RESULTS AND COMMENTS Survey 4, 2019
Item 1 Urine for microscopy, bacterial count, identification and susceptibilities
SPECIAL ATTENTION:
Result entry for the Bacteriology Urine program – Survey 2 (dispatch 4) was captured separately on the
new myQAP platform. As a result, this module will no longer be included in the Bacteriology survey or
generic report.
Participants in the Bacteriology Urine program will now be issued with a separate survey report, which
includes the generic report.
The RCPAQAP is harmonising the approach to the assessment of survey results for all qualitative pro-
grams. The assessment process for survey results for this program will change from the current scoring
system, to one that utilises ‘terms’ such as Concordant or Discordant to assess qualitative responses
against a known target.
It is expected that this report may be delayed by a few weeks for this survey due to extensive testing and
validation required.
ITEM 2019:4:2 THROAT SWAB
ITEM 2019:4:2 Throat swab
Quality Control
This item contained no pathogens. Staphylococcus epidermidis, and an α-haemolytic Streptococcus represented normal flora. This
item passed all homogeneity and stability testing with the normal flora counts remaining above 5.0 x 10 9 CFU/L throughout the
survey period.
Culture and identification results
Two hundred and seventeen participants returned results for this item with 88% correctly reporting “No likely pathogen” or “No
a.
pathogens isolated”. Nine participants reported a pathogen. Four reported Streptococcus group C, two S. pneumoniae, two S.
pyogenes and one S. aureus. Seventeen reported one of the normal flora isolates as the final result while two reported mixed flora.
a.
ITEM 2019:4:2 CLERICAL ERROR
Specimen label: Kate CONNER U/N 622856 Table 1: Clerical errors reported.
Clerical Errors reported in Item 2019:4:2 Number labs (217)
Paperwork: Kate CONNER U/N 568226 No errors reported 12
Error Unit number only 205 (94%)
Prepared by: Bacteriology
RCPAQAP Microbiology Report ID: MIBP2019040000000000Gener01
Report issued: 2/08/2019 Page 3 of 8
ITEM 2019:4:3 SKIN SWAB
Streptococcus pyogenes
Streptococcus pyogene s 163 163 75.8
45 20.9
Streptococcus group A 45
1 0.5
Beta-h aemolytic Stre p. Spe cie s 1
2 0.9
Staphylococcus species 2
2 0.9
Staphylococcus epid ermidis 2
1 0.5
Staphylococcus aure us 1
1 0.5
MRSA isol ate d 1
0 20 40 60 80 100 120 140 160 180
ITEM 2019:4:3
Quality Control
This item contained the pathogen, Streptococcus pyogenes with Staphylococcus epidermidis representing normal skin flora.
Homogeneity and stability testing were satisfactory and viability counts by the end of survey were > 1.0 X 10 10 CFU/L for the
pathogen.
Identification– Streptococcus pyogenes
Two hundred and fifteen participants returned results. All but six participants reported a β-haemolytic Streptococcus species. One
participant reported MRSA. Reporting MRSA could have repercussions for the patient with an incorrect alert to infection control.
Participants used various methods alone or in combination to identify as S. pyogenes/ Streptococcus group A. Results were
submitted for bacitracin susceptibility (n=42), Lancefield grouping (n=124) and commercial kits/systems (n=140). MALDI-ToF-MS
was used by 84 with the next popular kit/system being Vitek2 GP with 40 users.
Susceptibility testing - Streptococcus pyogenes
One hundred and ninety three (90%) participants submitted susceptibility results. Susceptibility testing was performed well.
Susceptibility results reported are tabulated in Table 2.
Prepared by: Bacteriology
RCPAQAP Microbiology Report ID: MIBP2019040000000000Gener01
Report issued: 2/08/2019 Page 4 of 8
Table 2: Streptococcus pyogenes Table 3. Susceptibility methods used. 2019:4:3 Streptococcus pyogenes
Streptococcus Susceptibility method used n
pyogenes
CDS 21
DISK DIFFUSION (CLSI) 83
susceptibilities DISK DIFFUSION (EUCAST) 40
(all methods) Etest 1
Kirby Bauer (CLSI) 11
MicroScan (CLSI) 2
Antibiotic S I/DS R
MicroScan (EUCAST) 1
Amoxycillin-clavulanate 6 - - Not performed 22
Ampicillin/Amoxycillin 35 - - Phoenix (CLSI) 2
Cefazolin 8 - - Vitek 2 (CLSI) 23
Cefotaxime 14 - - Vitek 2 (EUCAST) 9
Ceftriaxone 36 - -
Cefuroxime 5 - -
Cefuroxime (IV) 1 - -
Cephalexin 19 - -
Cephalothin 4 - -
Chloramphenicol 15 1 -
Clindamycin 124 - 1
Doxycycline 10 - -
Erythromycin 153 - 3
Levofloxacin 25 - -
Linezolid 15 - -
Penicillin 180 - -
Tetracycline 73 1 -
Trimethoprim-sulfamethoxazole 33 - 8
Vancomycin 63 - -
Table 4: Streptococcus pyogenes. CDS results
2019:4:3 Streptococcus pyogenes
Skin swab
Antibiotic Disc Content Exception to Interpretation MIC (mg/L)
standard Susceptible
Interpretation strains
Ampicillin/amoxycillin 5 4mm S1,2 ≤2
Benzylpenicillin 0.5 u S1,2 ≤ 0.125
Cefotaxime 0.5 4mm S ≤ 0.5
Clindamycin 2 S3 ≤ 0.5
Erythromycin 5 S3 ≤ 0.5
Tetracycline 10 S ≤4
Vancomycin 5 2mm S ≤4
CDS notes
1. For streptococci groups A, B, C, G and Streptococcus milleri group, the susceptibility to benzylpenicillin, ampicillin, amoxycillin and
cephalosporin antibiotics (except Ceftazidime) is extrapolated from the testing of benzylpenicillin 0.5 u.
2. If the organism is resistant to benzylpenicillin 0.5 u and susceptible to ampicillin 5 µg, report as having a decreased susceptibility.
3. No inducible clindamycin resistance (ICR) detected. Report clindamycin as susceptible.
Prepared by: Bacteriology
RCPAQAP Microbiology Report ID: MIBP2019040000000000Gener01
Report issued: 2/08/2019 Page 5 of 8
ITEM 2019:4:4A,B,C,D CULTURE AND MICROSCOPY FOR AFB
Reference laboratory report Microscopy Results
Slides were prepared in this survey using sputum that was
Table 5: 4A-D expected results examined using a Ziehl-Neelsen stain and tested for M.
tuberculosis and MAC by molecular methods and found to be
Test A B negative. AFB positive smears were seeded with Mycobacterium
AFB Ziehl 10-99/100 HPF (1+) ; 1 None tuberculosis H37Ra.
stain Neelsen -10 /HPF (2+)
Smear
C D Three hundred and nine participants returned results.
Culture Bactec Negative (normal flora M.chelonae Both smears passed homogeneity testing.
MGIT only)
960 Item 4A
(BD)/L-J Smear 4A was positive and contained 10-99/100 HPF (1+).
Some smears contained clumps in some areas which may
account for the higher counts [1-10 /HPF (2+)]. Four reported none
Table 6: Participant smear results (two a possible transposition of results) and two participants
reported “none” for both 4A and 4B. All four used only the Ziehl-
Participant smear results A B Neelsen stain.
>10 /HPF (3+) 7 - Item 4B
1-10 /HPF (2+) 136 - Smear 4B was negative. Five participants reported a false
positive smear. Two of these appear to have transposed results.
10-99/100 HPF (1+) 143 2 The remaining three reported both smears positive.
1-9/100 HPF (Scanty) 19 3
Culture Results
None 4 304 Sixty four laboratories participated and returned a culture result
for at least one of these items.
Item 4C was negative, containing only normal flora. All
Table 7: Participant culture results participants returned a correct “not isolated” result.
Item 4D was positive, containing Mycobacterium chelonae and
normal flora (S.epidermidis and an α-hemolytic streptococcus).
Culture results C D The sample passed all homogeneity and stability testing.
For the positive culture, 38 (60%) used both a manual and
automated method with 95% of these participants reporting at
Mycobacterium species isolated - 60 least one method positive. Over 93% of all participants reported
Mycobacterium species not isolated 64 4 “isolated” by at least one method. Twenty participants use only
an automated method while six use a standalone non-
automated method.
Two participants used two manual methods but no automated
Table 8: Results for media/methods used for specimen 4D method. Their overall result was correct.
Molecular Diagnostics Results
Media^ Total no. Number Thirteen laboratories also performed a molecular method for
Inoculated positive detection of M. tuberculosis. Where tested, all returned a correct,
4D negative result for Item 4C and 4D. Ten used a commercial kit
BD BBL MGIT (manual) 1 1 while the remaining used an Inhouse PCR. Please note that no
Brown and Buckle Slope 3 3 scoring is applied to molecular results from these items. To be
Gerloff with NVAP 2 2
assessed on molecular testing of Mycobacterium tuberculosis/
avium, the Molecular MTB/avium (now includes RIF resistance)
LJ 27 23 module is available for enrolment.
LJ Glycerol 2 1
LJ Pyruvate 8 7
Table 9. Combinations of AFB stains reported.
LJ Pyruvate Glycerol 4 4
Ogawa 4 4 Stain 1 Stain 2 n
B83 agar 1 1
Middlebrook 7H11 Agar 1 1 Ziehl-Neelsen - 162
Kirchner broth 1 1 Auramine O - 95
BacT/ALERT 3D 2 1 Kinyoun - 23
BD BACTEC MGIT 960 System 53 45
Auramine O Ziehl-Neelsen 15
BD BACTEC MGIT 320 System 3 2
AO + Rhodamine B - 6
^more than one medium may have been used by a participant. AO + Rhodamine B Ziehl-Neelsen 5
Auramine O Kinyoun 3
Acridine Orange Ziehl-Neelsen 1
Prepared by: Bacteriology
RCPAQAP Microbiology Report ID: MIBP2019040000000000Gener01
Report issued: 2/08/2019 Page 6 of 8
ITEM 2019:4:5 ISOLATE FOR IDENTIFICATION
%
Abio tro phia defectiva* 123 123 65.4
Abio tro phia sp ecies* 5 5 2.7
11 5.9
Gra nulicatella adiacens* 11
2 1.1
Gra nulicatella sp .* 2
3 1.6
Gemell a morb illorum 3
1 0.5
Gemell a h aemolysa ns 1
2 1.1
Nutritio nally varia nt Streptococcus* 2
2 1.1
Arcano bacter ium ha emolyticum 2
1 0.5
Gra m positive cocco bacilli 1
1 0.5
Gra m positive ba cillu s 1
1 0.5
Gra m neg ative co ccoba cillu s 1
1 0.5
Microbacte rium sp. 1
1 0.5
Leu con ostoc spe cie s 1
1 0.5
Glo bica tel la sang uinis 1
1 0.5
Facklamia lan guida* 1
1 0.5
Erysipelothrix rhusiopathiae * 1
1 0.5
Bacillu s sp eci es (?contaminan t) 1
1 0.5
Ana erococcus sp eci es 1
1 0.5
Aer oco ccus u rinae 1
1 0.5
Acti nobaculum scha alii* 1
1 0.5
Streptococcus vir idans* 1
No growth 1 1 0.5
Unable to Ide ntify - Refe r 25 25 13.3
0 20 40 60 80 100 120 140
* includes presumptive identification(s)
ITEM 2019:4:5
Isolate for Identification– Abiotrophia defectiva
QA Report
This item contained a pure growth of Abiotrophia defectiva and passed homogeneity
testing and counts remained above 4.0 x 10 9 CFU/L throughout the survey period. One
out of three vials failed stability testing so the participant who reported no growth has
not been scored.
Identification
A. defectiva was originally referred to as nutritionally variant streptococci (NVS)
because of its fastidious nutritional requirement for thiol compounds (pyroxidol/ Figure 5.1: Gram stain, Kingella kingae © ICPMR
cysteine).1 Two distinct groups of NVS exist, A. defectiva and A. adiacens. In 1995, 16S rRNA studies in Japan revealed that these
fastidious organisms were not related to the genus Streptococcus at all. They were transferred to the new genus, Abiotrophia. Of the
four species of Abiotrophia, three could be distinguished from A. defectiva and so were placed in another genus called Granulicatella
in 2000, leaving A. defectiva as the sole species in the genus.1,2,3,4
Abiotrophia and Granulicatella are catalase-negative, pleomorphic gram-positive cocci which exhibit satelliting behavior because of
their requirement for pyridoxal (vitamin B6). The presence of α– and β-galactosidase and the absence of β-glucuronidase in A.
defectiva distinguishes it from the closely related Granulicatella species. A. defectiva and Granulicatella are LAP-positive like the
streptococci, but unlike streptococci are PYR-positive.1
Prepared by: Bacteriology
RCPAQAP Microbiology Report ID: MIBP2019040000000000Gener01
Report issued: 2/08/2019 Page 7 of 8
SUMMARY OF PHENOTYPIC AND BIOCHEMICAL RESULTS
Phenotypic characteristics
• Gram stain: gram-positive –mainly cocci but may be pleomorphic with bulbous forms. Maybe Gram variable. Colonial appearance:
viridans-like (α-haemolytic) colonies.
• Catalase: negative
• Oxidase: negative
• Motility: negative
• Vancomycin: susceptible
Growth conditions
growth conditions may vary according to the strain isolated and the degree of B6
requirement.
• Growth on HBA @ 35°C in O2 : +
• Growth on HBA @ 35°C in CO2 : +++
• Growth on HBA @ 35°C in ANO2: +
• Growth on CHOC @ 35°C in CO2 : +++
• Growth on MacConkey agar: no growth
Identification was confirmed by 16S rRNA sequencing.
Supplementary tests Figure 5.2 Abiotrophia defectiva. 48 hours incubation,
CO2. © 2011 RCPA Microbiology QAP
• PYR: positive
• LAP: positive
• Arginine dihydrolase: negative
• α-Galactosidase: positive
• ß-Glucuronidase: negative
• Trehalose: fermented.
• Growth in 6.5% NaCl: negative3
• Satellitism: positive3
Participant results
Excluding the laboratory unable to grow this isolate, 187 participants returned a result with 128/187(68%) reporting Abiotrophia species.
Thirteen percent could not identify in this survey.
As discussed earlier Granulicatella species reported by 13 participants, although pyridoxyl-dependent and closely related to A. defectiva
are distinguished by the α– and β-galactosidase tests and the β-glucuronidase test (A. defectiva is pos/pos/neg and Granulicatella are
neg/neg/pos or neg depending on species). All 13 participants who incorrectly reported Granulicatella species used Vitek2 GP.
Another misidentification reported was Gemella species by four laboratories. Two had used Phoenix, another Vitek2 GP and the
remaining did not report using a kit. Like Abiotrophia, Gemella species (other than G. haemolysans and G. asacchararolyticus) are PYR
and LAP positive, will not grow in 6.5% NaCl and produce slow-growing, α-haemolytic streptococcus-like colonies on blood agar. The test
for satellitism will distinguish Gemella (negative) from the NVS (positive). The isolate is streaked for confluent growth onto a blood agar
plate and a single cross streak of Staphylococcus aureus or S. epidermidis is applied. The plate is incubated at 35°C in CO2 and
examined for enhanced growth of the isolate colonies surrounding the staphylococcal streak. Alternatively, media supplemented with
pyridoxyl HCl (final concentration of 0.001%) or commercial pyridoxyl discs may be used to show vitamin B6 dependency. 3
The pleomorphism of NVS may also have caused confusion. Most laboratories (176/184) reported Gram reactions as gram-positive
cocci/diplococci/coccobacilli. Six reported gram-variable cocci/coccobacilli/rods. Two laboratories reported gram-negative rods/cocci/
coccobacilli with both unable to identify. It is worth noting that pyridoxal HCl added to media may also help convert NVS to a more
Streptococcus-like Gram stain morphology and gram-positivity.4 Aerococcus species reported by one lab have a more staphylococcus-
like Gram reaction. All 93 reporting a catalase result (negative) reported correctly.
Prepared by: Bacteriology
RCPAQAP Microbiology Report ID: MIBP2019040000000000Gener01
Report issued: 2/08/2019 Page 8 of 8
One hundred and forty nine participants used a commercial kit/system to identify this isolate. Below shows the percentage correct for an
identification of A. defectiva/Abiotrophia species for the most commonly used. Sixteen used a second kit or method to confirm
identification.
• API Strep: 7/10 (70%). Aerococcus urinae 1); Facklamia languida (1); NVS (1).
• API Coryne: 0/2. Arcanobacterium haemolyticum (2).
• MALDI-TOF Bruker: 55/55 (100%).
• MALDI-TOF VITEK MS: 32/32 (100%).
• Sequencing 16S rRNA: 3/3 (100%).
• VITEK2 GP (Biomerieux): 21/40 (53%). Gemella morbillorum (1); Granulicatella adiacens (11); Granulicatella species (2);
Globicatella sanguinis (1); NVS (1); Leuconostoc species (1); Unable to Identify - Refer (2).
Abiotrophia are part of the normal flora of the upper respiratory tract and are a known cause of endocarditis and septicaemia. The gram-
positive cocci in the Gram stain of blood cultures may look ‘antibiotic affected’ and laboratories will often fail to isolate any organism. The
frequency of infection and colonisation of cardiac valves by Abiotrophia strongly suggests an affinity for avascular tissue. 5 The clinical
course of endocarditis with NVS is often more severe and difficult to treat than with the viridans streptococci or enterococci and relapse
rates have been documented as being relatively high. 3,4 A high prevalence of β-lactam and macrolide resistance among the NVS has
been reported.6 Predisposing factors for NVS infection among neutropenic patients include chemotherapy-induced neutropenia and oral
mucositis.6
References Item 5
1. The Gram-Positive Cocci: in Koneman's Colour Atlas and Textbook of Diagnostic Microbiology. Winn and Akllen et al. 2016, 7th Ed.
Lippincott Williams and Wilkins, Philadelphia. p774.
2. Collins M.D, Lawson P.A. The genus Abiotrophia (Kawamura et al.) is not monophyletic: proposal of Granulicatella gen. nov., Granulicatella
adiacens comb. nov., Granulicatella elegans comb. nov. and Granulicatella balaenopterae comb. nov. Int J Syst Evol Microbiol 2000;50: 365-
9. http://ijs.microbiologyresearch.org/content/journal/ijsem/10.1099/00207713-50-1-365
3. Christensen, JJ and Ruoff, KL. Aerococcus, Abiotrophia, and other aerobic, catalase-negative, gram-positive cocci: In Manual of Clinical
Microbiology, Editors in chief J.H. Jorgensen and M.A Pfaller. 11th Edition. ASM Press: Chapter 24.
4. Christensen, J. and Facklam R. Granulicatella and Abiotrophia species from human clinical specimens. J Clin Microbiol 2001;39: 3520-3523.
http://www.ncbi.nlm.nih.gov/pubmed/11574566
5. Ince, A et al. Total knee arthroplasty infection due to Abiotrophia defectiva. J Med Microbiol. 2002. 51, 899-902.
6. Senn, L et al. Bloodstream and endovascular infections due to Abiotrophia defectiva and Granulicatella species. BMC Infectious Diseases
2006. 6: 9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1360077/pdf/1471-2334-6-9.pdf
Other references:
7. Rhodes, H.M., Hirigoyen, D., Shabnam, L., Williams, D.N., Hansen, G.T. Infective endocarditis due to Abiotrophia defectiva and
Granulicatella spp. complicated by infectious intracranial cerebral aneurysms: a report of three cases and review of the literature. J Med
Microbiol. 2016;65: 493. https://jmm.microbiologyresearch.org/content/journal/jmm/10.1099/jmm.0.000260#tab1
8. Escarcega, E., Trovato, C., Idahosa, O., Gillard, J., Stankewicz, H. Abiotrophia defectiva endocarditis: an easy miss. Clin Pract Cases Emerg
Med. 2017;1: 229 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5965177/
9. Chowdhury,S., and German, M.L, Rare but not infrequent: infective endocarditis caused by Abiotrophia defectiva, Case Reports in Infectious
Diseases, vol. 2018, Article ID 5186520, 3 pages, 2018. https://www.hindawi.com/journals/criid/2018/5186520/cta/
10. Ratcliffe, P., Fang, H., Thidholm, E., Boräng, S., Westling, K., Özenci, V. Comparison of MALDI-TOF MS and VITEK 2 system for laboratory
diagnosis of Granulicatella and Abiotrophia species causing invasive infections. Diagn Microbiol Infect Dis. 2018;77: 216. https://
www.ncbi.nlm.nih.gov/pubmed/24034902
Prepared by: Bacteriology
RCPAQAP Microbiology Report ID: MIBP2019040000000000Gener01
You might also like
- 5472 - Report Final CommentDocument2 pages5472 - Report Final CommentMarik Gwyneth Diokno SimaraNo ratings yet
- Biolife: Nutrient AgarDocument2 pagesBiolife: Nutrient AgarZoza SalamaNo ratings yet
- Ijms V6i8p103Document6 pagesIjms V6i8p103Azzam SaqrNo ratings yet
- Application of Bacteriophages: April 2017Document5 pagesApplication of Bacteriophages: April 2017Ahmed AlbagerNo ratings yet
- Bacteria and Yeast Work-Up ManualDocument19 pagesBacteria and Yeast Work-Up ManualS ONo ratings yet
- CGH202008000915 - Lab A2 2020 2231 - Laboratory - Covid PCR Test PDFDocument2 pagesCGH202008000915 - Lab A2 2020 2231 - Laboratory - Covid PCR Test PDFMichael JonasanNo ratings yet
- Practices of Usage of Antibiotics in Chicken Farming and Impact of Some of Their Residues in Products Consumed in Yaound Cameroon AnfsDocument8 pagesPractices of Usage of Antibiotics in Chicken Farming and Impact of Some of Their Residues in Products Consumed in Yaound Cameroon AnfsIsabelle sandrine Bouelet NtsamaNo ratings yet
- Antimicrobial Susceptibility Testing: January 2019Document21 pagesAntimicrobial Susceptibility Testing: January 2019Trọng TínNo ratings yet
- Evans Vanodine International PLC: Microbiological ProfileDocument13 pagesEvans Vanodine International PLC: Microbiological Profilet0maxNo ratings yet
- Microbiology 15 Campylobacter, Vibrio Etc 431-449Document18 pagesMicrobiology 15 Campylobacter, Vibrio Etc 431-449JenNo ratings yet
- RTPCRDocument1 pageRTPCRAmit TyagiNo ratings yet
- Lower Nasopharyngeal Viral Load During The Latest Phase of COVIDDocument6 pagesLower Nasopharyngeal Viral Load During The Latest Phase of COVIDFrancy SulcisNo ratings yet
- Certificate of Analysis: Product Name Catalog Number Manufacture Date:2016/09/17 Batch Number Expiration DateDocument2 pagesCertificate of Analysis: Product Name Catalog Number Manufacture Date:2016/09/17 Batch Number Expiration DateLEONARDO ALBERTO GIL LANGNo ratings yet
- Sterility Test ProcedureDocument7 pagesSterility Test ProcedureMusyoka UrbanusNo ratings yet
- A Look at The Principal Bacterial, Fungal and Parasitic Diseases of Farmed ShrimpDocument15 pagesA Look at The Principal Bacterial, Fungal and Parasitic Diseases of Farmed Shrimpthefather_18183925100% (1)
- Molecular Biology: Lab ID Reference No Name MRN ID Sample NoDocument1 pageMolecular Biology: Lab ID Reference No Name MRN ID Sample NoMuhammadnasidiNo ratings yet
- POCKIT Central SARS-CoV-2 Premix Reagent - User Manual (20200601) - US ...Document34 pagesPOCKIT Central SARS-CoV-2 Premix Reagent - User Manual (20200601) - US ...Anisa MaharaniNo ratings yet
- Sample Type: Visit Id: R8539558Document1 pageSample Type: Visit Id: R8539558Ravi KumarNo ratings yet
- Notes Upgraded Validation Protocol For Hold Time Study of Prepared Inoculum SuspensionDocument2 pagesNotes Upgraded Validation Protocol For Hold Time Study of Prepared Inoculum SuspensionsatishbholeNo ratings yet
- Nitika SharmaDocument1 pageNitika Sharmavishal sharmaNo ratings yet
- Paronychia: Incidence During Magh Mela: Original Research ArticleDocument4 pagesParonychia: Incidence During Magh Mela: Original Research ArticleLovely PoppyNo ratings yet
- CGH202008030750 - Lab M 2020 16384 - Laboratory - Covid PCR Test PDFDocument2 pagesCGH202008030750 - Lab M 2020 16384 - Laboratory - Covid PCR Test PDFMichael Vincent Naces AlmueteNo ratings yet
- Comparación de Pruebas Rápidas de Antígenos para COVID-19Document9 pagesComparación de Pruebas Rápidas de Antígenos para COVID-19Cristal Jewels DiamondNo ratings yet
- LPL - Production Test Collection Centre Sector - 18, Block-E Rohini DELHI 110085Document2 pagesLPL - Production Test Collection Centre Sector - 18, Block-E Rohini DELHI 110085Manav ChhabraNo ratings yet
- Dairy Milk 3Document7 pagesDairy Milk 3Fhar AwayNo ratings yet
- Laboratories Performing Microbiological and Chemical Analyses of Food, Dietary Supplements, and Pharmaceuticals")Document6 pagesLaboratories Performing Microbiological and Chemical Analyses of Food, Dietary Supplements, and Pharmaceuticals")SLN TESTING LABORATORYNo ratings yet
- 25.signal HIV Immuno DotDocument5 pages25.signal HIV Immuno DotprastacharNo ratings yet
- Publications ScientifiquesDocument103 pagesPublications ScientifiquesBrowndonNo ratings yet
- Super Sani Cloth Tech Data Bulletin - 0619 UPDATE - 07168610Document4 pagesSuper Sani Cloth Tech Data Bulletin - 0619 UPDATE - 07168610Alexandra' LuqueNo ratings yet
- Lab Policies KOH Prep For Fungal Elements Affiliate Lab 8649 4Document3 pagesLab Policies KOH Prep For Fungal Elements Affiliate Lab 8649 4Geby JeonNo ratings yet
- BTAmediaDocument4 pagesBTAmediaNidia MaradiagaNo ratings yet
- 281659biofire ® CovidDocument3 pages281659biofire ® CoviddrianaudxdNo ratings yet
- BMS Iddt 2020 41Document8 pagesBMS Iddt 2020 41Guneyden GuneydenNo ratings yet
- Abdullahi Ahmad Nasidi - F - 25022022185539Document1 pageAbdullahi Ahmad Nasidi - F - 25022022185539MuhammadnasidiNo ratings yet
- Convid TestDocument3 pagesConvid TestDeepti JajooNo ratings yet
- Test Result Report: Interpretation GuidelinesDocument2 pagesTest Result Report: Interpretation GuidelinessssNo ratings yet
- Partec Microbiology-Industrial 2Document24 pagesPartec Microbiology-Industrial 2Mohd Danial Muhd Ali0% (1)
- Code of Practice TemplatesV3Document9 pagesCode of Practice TemplatesV3Hentai FiendNo ratings yet
- Microbiological Pharmaceutical Quality Control Labs (7 - 93) - FDADocument8 pagesMicrobiological Pharmaceutical Quality Control Labs (7 - 93) - FDAArmando SaldañaNo ratings yet
- Covid Report: Mr. Rakesh SharmaDocument1 pageCovid Report: Mr. Rakesh Sharmavishal sharmaNo ratings yet
- Identification of Bacteria On Cockroach Feet From Hospital Area in Palu City and Test of Sensitivity To AntibioticDocument8 pagesIdentification of Bacteria On Cockroach Feet From Hospital Area in Palu City and Test of Sensitivity To AntibioticWidya AprilianiNo ratings yet
- Ultimos AntimicrobianosDocument3 pagesUltimos Antimicrobianosmargarita rodriguezNo ratings yet
- Pharmaceuticals & Medical Supplies: Amarila Malik Professor, Faculty of Pharmacy - Universitas IndonesiaDocument22 pagesPharmaceuticals & Medical Supplies: Amarila Malik Professor, Faculty of Pharmacy - Universitas IndonesiaAngga AnugrawanNo ratings yet
- Clinical Significance:: Conditions of Laboratory Testing & ReportingDocument2 pagesClinical Significance:: Conditions of Laboratory Testing & ReportingAashwin PoovankunnilNo ratings yet
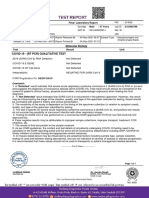
- Covid 19 - (RT PCR) Qualitative Test: Final Laboratory ReportDocument1 pageCovid 19 - (RT PCR) Qualitative Test: Final Laboratory ReportyuvNo ratings yet
- Minutes of The 2021 Qoi WG Meeting and Recommendations For 2021 Last Update On 29th of Nov 2021Document41 pagesMinutes of The 2021 Qoi WG Meeting and Recommendations For 2021 Last Update On 29th of Nov 2021MIGUEL AMAYANo ratings yet
- ICHROMA IgG-IgMDocument5 pagesICHROMA IgG-IgMAlfonso RamosNo ratings yet
- Inserto Control Idg PDFDocument3 pagesInserto Control Idg PDFLoren Orozco0% (1)
- Jemra Campylobacter Summary and ConclusionDocument12 pagesJemra Campylobacter Summary and ConclusionJohnson ojofuNo ratings yet
- Assessment of Inactivation Procedures For Sars-Cov-2: Research ArticleDocument5 pagesAssessment of Inactivation Procedures For Sars-Cov-2: Research ArticleYogiswara KarangNo ratings yet
- BC 7Document8 pagesBC 7Lucky_megaNo ratings yet
- FT Agar Myp - CimpaDocument6 pagesFT Agar Myp - CimpaLuz Katherine MartinezNo ratings yet
- CLIA Microbiology APR 2023Document8 pagesCLIA Microbiology APR 2023Jenn Abad (I am a student)No ratings yet
- Laboratory Report: Name: Patient ID: P577928Document1 pageLaboratory Report: Name: Patient ID: P577928Rustam SiddiquiNo ratings yet
- in Vitro Diagnostic Reagents Clinic Trial Report V2.0Document25 pagesin Vitro Diagnostic Reagents Clinic Trial Report V2.0aditya arsiNo ratings yet
- Detection HA Dan HIDocument21 pagesDetection HA Dan HITim IT Poltekkes BandungNo ratings yet
- Test Result Report: Interpretation GuidelinesDocument2 pagesTest Result Report: Interpretation GuidelinesVivek VinuNo ratings yet
- Editorial and Executive Summary: IFCC Interim Guidelines On Clinical Laboratory Testing During The COVID-19 PandemicDocument6 pagesEditorial and Executive Summary: IFCC Interim Guidelines On Clinical Laboratory Testing During The COVID-19 PandemicHector MarrufoNo ratings yet
- Risk Profile - Group B Streptococcus (GBS) – Streptococcus Agalactiae Sequence Type (ST) 283 in Freshwater FishFrom EverandRisk Profile - Group B Streptococcus (GBS) – Streptococcus Agalactiae Sequence Type (ST) 283 in Freshwater FishNo ratings yet
- Handbook of Microbiological Criteria for FoodsFrom EverandHandbook of Microbiological Criteria for FoodsNo ratings yet
- OMICs - PPT On Personalied Medicines For The Filipino PeopleDocument18 pagesOMICs - PPT On Personalied Medicines For The Filipino PeopleNora O. GamoloNo ratings yet
- Medical Examination FormDocument1 pageMedical Examination FormEric ZarrielloNo ratings yet
- COVID-19 Early Experiences and Challenges of A Resource-Limited CountryDocument4 pagesCOVID-19 Early Experiences and Challenges of A Resource-Limited CountryAlton Nathaniel Nadela DagaleaNo ratings yet
- ASA Physical Status Classification System - American Society of Anesthesiologists (ASA)Document2 pagesASA Physical Status Classification System - American Society of Anesthesiologists (ASA)Anonymous efqPXILEQJNo ratings yet
- Research 10Document4 pagesResearch 10Francis SyNo ratings yet
- Malaria: Signs and SymptomsDocument17 pagesMalaria: Signs and SymptomsJohn PalutlaNo ratings yet
- Denture StomatitisDocument5 pagesDenture Stomatitissarah wilderNo ratings yet
- Leprosy Reaction: Oleh: Aryo Wibowo C11103224 Pembimbing: Dr. Cyntia Yulyana Supervisor: Dr. Muhlis, SP - KK, M.KesDocument14 pagesLeprosy Reaction: Oleh: Aryo Wibowo C11103224 Pembimbing: Dr. Cyntia Yulyana Supervisor: Dr. Muhlis, SP - KK, M.Kesjoe ashikawaNo ratings yet
- NCM 104 10 Herbal MedicinesDocument4 pagesNCM 104 10 Herbal MedicinesElleNo ratings yet
- Churnas DownDocument60 pagesChurnas DownAyyush RajalingaNo ratings yet
- Activity Sheet Oral Com - Q2-W5BDocument2 pagesActivity Sheet Oral Com - Q2-W5BGerrylyn BalanagNo ratings yet
- The Employee Wellbeing Programme (EWP)Document4 pagesThe Employee Wellbeing Programme (EWP)Dieter NeuviansNo ratings yet
- Gastroenterology MnemonicsDocument10 pagesGastroenterology MnemonicsAnnapurna DangetiNo ratings yet
- Health DeclarationDocument5 pagesHealth Declarationust dol100% (1)
- The COVID-19 Outbreak and ImplicationsDocument10 pagesThe COVID-19 Outbreak and ImplicationsxxxdosyaNo ratings yet
- Population and Community HealthDocument10 pagesPopulation and Community HealthMuntasir Alam RahimiNo ratings yet
- Hand - Foot - Mouth Disease: Prepared By: Dr. NGUYEN QUANG DIEN Emergency DepartmentDocument24 pagesHand - Foot - Mouth Disease: Prepared By: Dr. NGUYEN QUANG DIEN Emergency DepartmentRayhan CeinNo ratings yet
- World Health Performance Task Checkpoint 2Document2 pagesWorld Health Performance Task Checkpoint 2Andrew M100% (1)
- Oral Cancer PDFDocument7 pagesOral Cancer PDFDaryAntoNo ratings yet
- Some Common Special StainsDocument4 pagesSome Common Special StainsDrramyRaafatNo ratings yet
- Review On PoisonDocument5 pagesReview On PoisonClarito LopezNo ratings yet
- 500-ALPHA FIT Testers ManualDocument29 pages500-ALPHA FIT Testers ManualDarío Gerpe MeirásNo ratings yet
- Intermediate 3 - Alp Project: Option 3: (For Pair or Group Presentations)Document2 pagesIntermediate 3 - Alp Project: Option 3: (For Pair or Group Presentations)Gary Yauri MayorcaNo ratings yet
- Usmle Medical BiochemistryDocument27 pagesUsmle Medical BiochemistryDr.G.Bhanu Prakash100% (1)
- Explanation Text Raindra (24) XI MIPA 3Document4 pagesExplanation Text Raindra (24) XI MIPA 3Raindra NovemberNo ratings yet
- Criteria For ScreeningDocument13 pagesCriteria For Screeningabisoniya17No ratings yet
- CA EsophagusDocument37 pagesCA EsophagusElandha PutriNo ratings yet
- Anti InfectiveDocument9 pagesAnti InfectiveMae DoctoleroNo ratings yet
- Mudras For LifeDocument4 pagesMudras For LifeKannan Thangavel TNo ratings yet
- Cercospora Leaf Spot and Berry Blotch of CoffeeDocument6 pagesCercospora Leaf Spot and Berry Blotch of CoffeeMoody Infinity100% (1)