Professional Documents
Culture Documents
Difteri Who PDF
Difteri Who PDF
Uploaded by
mecca fiandraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Difteri Who PDF
Difteri Who PDF
Uploaded by
mecca fiandraCopyright:
Available Formats
Diphtheria
Diphtheria is a bacterial infection caused by toxigenic strains of Corynebacterium diphtheria (C. diphtheria), and most often causes
infection of the upper respiratory tract and leads to the clinical syndromes including pharyngitis, naso-pharyngitis, tonsillitis, laryngitis (or
any combination of these) and a firmly adherent pseudo membrane over the tonsils, pharynx, larynx and/or nares. In severe cases,
infection can spread into trachea causing tracheiitis and/or severe cervical adenopathy leading to life-threatening airway obstruction.
Probable Case
A person with an illness characterized by laryngitis or pharyngitis or tonsillitis, and an
adherent membrane of the tonsils, pharynx and/or nose OR gross lymphadenopathy
Five things to do with a probable case*
1. Isolate patient immediately and apply standard droplet and contact precautions when
caring for the patient.
2. Administer diphtheria antitoxin (DAT) as soon as possible if in field hospital.
3. Administer antibiotics (penicillin or erythromycin) following DAT as soon as possible.
4. Monitor closely and provide supportive therapy for severe complications (i.e. airway
management, cardiac, neurologic and renal failure).
5. Vaccinate
*See flow chart on back of page
Infection Prevention and Control
1. Place patients with suspected or confirmed diphtheria in isolation room (area).
2. Apply standard precautions, including hand hygiene at all times.
3. In addition, also apply droplet and contact precautions.
4. The disease is usually not contagious 48 hours after treatment.
5. After discharge, restrict contact with others until completion of antibiotic therapy.
For all identified close contacts:
1. Identify all close contacts
2. Administer prophylaxis for close contacts
IM benzathine penicillin: a single dose
For children aged ≤ 5 years: administer 600 000 units
For those > 5 years: administer 1 200 000 units
OR
Oral azithromycin
Children: 10-12 mg/kg once daily, to a max of 500mg/day. Treat for total 7 days
Adults: 500mg once daily. Treat for total 7 days.
OR
Oral erythromycin
For children: 40 mg/kg/day, administered in divided dose, 10 mg per dose, every 6 hours
For adults: 1 g/day for adults, administered in divided dose, 250 mg per dose every 6 hours Treat for total 7 days
3. All identified contacts should be closely monitored for seven days and seek treatment if symptomatic
TRIAGE
Some patients may
present weeks after URTI Sore throat
symptoms with new onset URTI symptoms
+/- Fever Refer to Infection
of cardiac renal or
+/- Malaise Prevention and
neurological symptoms
Control measures
Clinician wearing protection
examines throat
Early Pseudo-
membrane URTI
Pseudo-membrane seen
OR gross No Advice to return if no
lymphadenopathy improvement.
Give Paracetamol
Yes
Contact Tracing, Vaccination, and Prophylaxis for Contacts
Are there Clinical Warning Signs?
Pseudo-Membrane
Bull Neck
Stridor
Fast Respiratory Rate
Chest in-drawing
Restlessness or lethargy
Bull neck
Delayed capillary refill
Fast Heart rate and cold extremities
Central Cyanosis
Yes No
DAT (give as soon as possible)
Antibiotics (give as soon as possible)
Antibiotics (give as soon as possible)
Field Hospital Isolation facility for at least 48 hours
DAT dose Oral penicillin V
Contac IU
20,000-100,000 10-15 mg/kg/dose administered every 6 hours.
t Maximum is 500 mg per dose. Treat for 14 days.
Aqueous benzyl penicillin (penicillin G): (IM or IV)
Tracing
25 000 units/kg every 6 hours*. Treat for 14 days.
Oral erythromycin
10 mg/kg administered every 6 hours. Maximum is
When patients are able to swallow, switch to oral 500 mg per dose. Treat for 14 days.
antibiotics to complete course (14 days) Oral azithromycin
10 mg/kg administered once daily.
Laboratory sampling on a case by case basis Maximum is 500 mg per day. Treat for 14 days.
*Maximum dose is 4 MIU
Monitor for deterioration, refer to field hospital if patient worsens
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 2014 Bauman - 4th Chapter 14Document20 pages2014 Bauman - 4th Chapter 14add100% (1)
- MCQS IdDocument24 pagesMCQS IdWaleed SofiNo ratings yet
- The Speckled Monster: National Curriculum Links (England) Key Learning OutcomesDocument14 pagesThe Speckled Monster: National Curriculum Links (England) Key Learning OutcomesweiliNo ratings yet
- Certificate For COVID-19 Vaccination: Beneficiary DetailsDocument1 pageCertificate For COVID-19 Vaccination: Beneficiary Detailskonduru revanthNo ratings yet
- Immunity - B and T CellsDocument12 pagesImmunity - B and T CellsmclNo ratings yet
- COVID 19 Quarantine Vs IsolationDocument1 pageCOVID 19 Quarantine Vs IsolationBláck GhøstNo ratings yet
- The Comparison of Nasaleze and Mometasone Nasal Spray To Control The Symptoms of Allergic RhinitisDocument5 pagesThe Comparison of Nasaleze and Mometasone Nasal Spray To Control The Symptoms of Allergic RhinitisCarlos Alberto Aliaga DulantoNo ratings yet
- Hemolytic Transfusion ReactionDocument3 pagesHemolytic Transfusion ReactionAinin SofiyaNo ratings yet
- DermatitisDocument6 pagesDermatitisNader SmadiNo ratings yet
- Diarrhoea Patient InformationDocument3 pagesDiarrhoea Patient InformationIgor DemićNo ratings yet
- SerologyDocument442 pagesSerologyPura Javier100% (2)
- ANTIBIOTICSDocument14 pagesANTIBIOTICSAll NewtNo ratings yet
- MICROPARADocument61 pagesMICROPARAKyla RamonesNo ratings yet
- Parasitic Zoonoses and Diagnostics For Dogs Dr.Document3 pagesParasitic Zoonoses and Diagnostics For Dogs Dr.pundaipundaiNo ratings yet
- 04 Task Performance Batch 2-Group2 - Pre - FinalDocument5 pages04 Task Performance Batch 2-Group2 - Pre - FinalAirizh GadianNo ratings yet
- Peran Perawat Mencegah Penularan HIV Dan Merawat ODHA XXDocument110 pagesPeran Perawat Mencegah Penularan HIV Dan Merawat ODHA XXApel HijauNo ratings yet
- Penatalaksanaan Petugas Terpapar COVID-19Document30 pagesPenatalaksanaan Petugas Terpapar COVID-19Taupick ArsyNo ratings yet
- Patient Report View in PDFDocument1 pagePatient Report View in PDFSyed Wajahat BokhariNo ratings yet
- Pre-And Postnatal Risk Factors in The Pathogenesis of BPD: The Role of InfectionsDocument35 pagesPre-And Postnatal Risk Factors in The Pathogenesis of BPD: The Role of InfectionslordofthewebNo ratings yet
- Public Health Facilities and Services in Palakkad District, KeralaDocument154 pagesPublic Health Facilities and Services in Palakkad District, Keralajaison100% (1)
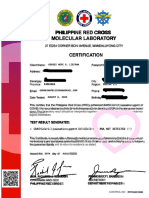
- Molecular Laboratory: Philippine Red CrossDocument4 pagesMolecular Laboratory: Philippine Red CrossVianne MagsinoNo ratings yet
- Hiv/Aids Stadium Iii With Opportunistic Infection: (Laporan Kasus)Document4 pagesHiv/Aids Stadium Iii With Opportunistic Infection: (Laporan Kasus)yantiNo ratings yet
- CLMDocument13 pagesCLMBhica Wrahty AdetaNo ratings yet
- Case 1556 enDocument3 pagesCase 1556 enSergio ZambranoNo ratings yet
- ABO Grouping - Overview, Clinical Indications - Applications, Test PerformanceDocument7 pagesABO Grouping - Overview, Clinical Indications - Applications, Test PerformanceleandroNo ratings yet
- Whooping Cough (Pertussis)Document5 pagesWhooping Cough (Pertussis)coooleNo ratings yet
- Serocheck TP DevicekkkkDocument4 pagesSerocheck TP DevicekkkkMatibar RahmanNo ratings yet
- Soi 2016-17Document280 pagesSoi 2016-17venkat_nsnNo ratings yet
- Food Allergy NestleDocument11 pagesFood Allergy NestleRositaMagda MataNo ratings yet
- Lymphomas With PathophysiologyDocument30 pagesLymphomas With Pathophysiologymabec pagaduan91% (11)