Professional Documents
Culture Documents
BRJ October 2017 - Manash PDF
BRJ October 2017 - Manash PDF
Uploaded by
Manash GogoiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BRJ October 2017 - Manash PDF
BRJ October 2017 - Manash PDF
Uploaded by
Manash GogoiCopyright:
Available Formats
Review
Recent Advances in Nanomedicine for Antimalarial Drug
Delivery
Manashjit Gogoi*
Department of Biomedical Engineering, North-Eastern Hill University, Shillong–793022, India
Malaria is one of the major public health problems caused by parasites belonging to plasmodium genus
in the tropical and subtropical countries. Advancement of nanotechnology is opening up a window of
huge opportunities for better treatment of malaria. Different nano drug delivery systems such as
liposomes, solid lipid nanoparticles, dendrimer, nano-emulsion and polymeric nanoparticles are widely
investigated for treating malaria. In this review, the recent advances in nanomedicine for antimalarial
drug delivery are summarised.
INTRODUCTION
Malaria is one of the major public health Region (2%) (WHO, 2016). One of the
problems in tropical and subtropical reasons behind the large number of
countries. Malaria parasites are malaria associated deaths in WHO Africa
transmitted from infected host to region and WHO South-East Asia
susceptible host by the bite of an infected Region is the emergence of drug
Anopheles mosquito. As per the World resistance parasites especially in East
Health Organization’s (WHO) Malaria Africa (Korenromp et al., 2003) and
Report 2016, nearly 148–304 million Greater Mekong Subregion (Imwong et
people suffered from acute malaria al., 2017). Artemisinin combination
globally and 0.235–0.639 million among therapies (ACTs) are leading options for
the infected died. In 2015, it was treatment of malaria caused by
estimated that globally 429,000 people Plasmodium falciparum in the malaria
died due to malaria, most of them in prevalent regions of the world. But, the
WHO African Region (92%), followed emergence and spread of artemisinin
by the WHO South-East Asia Region resistant P. falciparum across the Greater
(6%) and WHO Eastern Mediterranean Mekong Subregion possess a serious
Key words: Nanomedicine, malaria, nano drug delivery system, nanoparticles.
*Corresponding Author: Manashjit Gogoi, Department of Biomedical Engineering, North-Eastern Hill University,
Shillong–793022, Meghalaya, India.
Email: manash.aec@gmail.com
Biomed Res J 2017;4(2):151-161
Gogoi 152
threat to global malaria control and Malaria and Conventional Therapy
elimination drive. The artemisinin Malaria is an ancient disease and has
resistance evolved in the Thailand- been troubling the mankind since
Myanmar border due to the E252Q thousand years. The Italian word malaria
PfKelch mutation; later it was overtaken means “bad air”. Traits of malaria were
by C580Y as ACTs began to fail reported in ancient history from India,
(Imwong et al., 2017). China, and Egypt. Greek and Roman
Due to lack of funding, limited work medical literature contain accurate
was carried out in the field of malaria descriptions about malaria (Nayak et al.,
research in last few decades; and hence 2013). Malaria is caused by four
limited progress is achieved in Plasmodium species, i.e., P. falciparum,
eradication of malaria. In recent years, P. vivax, P. malariae and P. ovale cause
due to infusion of money from several malaria in humans. P. falciparum and P.
public and private organizations e.g. Bill vivax are the two major species
and Melinda Gates Foundation, responsible for malaria globally (Duong
Medicines for Malaria Venture, Drugs for et al., 2004). Almost all deaths i.e. 99%
Neglected Diseases initiative (DNDi) and resulted from P. falciparum malaria
the Institute for One World Health whereas P. Vivax was estimated to cause
(IOWH), the situation improved to some 3100 deaths in 2015 and most of the
extent. However, as no new drug is deaths (86%) occurred outside Africa
discovered during last several years and (WHO, 2016).
discovery of drug is an expensive and Malaria is a complex disease and the
time consuming affair; nanomedicine has life cycle of protozoan parasite
been explored for eradication of malaria. responsible for malaria is divided
Nanomedicines have the potentials to between a vertebrate host and an insect
increase the therapeutic potency of vector. Plasmodium parasites (except P.
existing drugs by improving their malariae) enter the human blood in the
adsorption, distribution, metabolism and form of sporozoites through mosquito
excretion (ADME) and reducing over bite. These sporozoites infect the liver
drug toxicity (Nayak et al., 2013). cells and proliferate into thousands of
merozoites (Tuteja, 2007). The
Biomed Res J 2017;4(2):151-161
153 Nanomedicine for antimalarial drug delivery
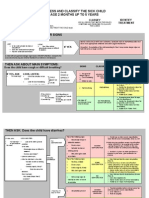
Figure 1: The life cycle of the parasite (adapted from Murambiwa et al., 2011).
merozoites released from the liver enter parasite is shown in Fig. 1.
the red blood cell (RBC) and start an At present, quinine related drugs,
asexual cycle consisting of rings, Artemisinin derivatives, anti-folates
trophozoites, schizonts and merozoites derivatives and new class of combination
for multiplication of parasites. These drugs are extensively used to treat
parasites again become ready to infect malaria. These drugs are used in
fresh RBCs. In this process, a few combination for better malaria treatment.
gametes are also formed which enter the Quinine related drugs are highly potent
mosquito midgut during bite; their sexual in treating malaria. Chloroquine (CQ)
cycles start in the mosquito and it leads has been used for treatment of malaria
to production of sporozoites. Asexual for over eight decades due to its excellent
cycle in human is divided into the exo- pharmacokinetic and pharmacological
erythrocytic cycle in liver and intra- advantages over all other antimalarial
erythrocytic cycle in RBC. The intra- drugs. CQ is known for its fast action in
erythrocytic phase elicits the clinical blood parasite stages, low toxicity, good
manifestations of malaria (Garnham, bioavailability from oral dosage, water
1966; Jarcho, 1968). The life cycle of the solubility, high volume of distribution in
Biomed Res J 2017;4(2):151-161
Gogoi 154
the body and lower cost (Santos- administrations (Murambiwa et al.,
Magalhães and Mosqueira, 2010). 2011).
Primaquine (PQ) is a very toxic drug
used in the prophylaxis against all types Nanomedicine for Drug Delivery
of malaria. Nevertheless, quinine related Nanocarriers with prolong blood
drugs are effective against malaria; P. circulation time i.e. stealth nanocarriers
falciparum is developing resistance have been used for delivering
against these classes of drugs. antimalarial drugs in order to increase the
ACT is the frontline treatment against resident time in the human body and to
malaria. Artemisinin and its derivatives increase the probability of drug
have the ability to kill a broad range of molecules to interact with infected red
asexual parasite stages at safe blood cells and parasites (Mosqueira el
concentrations (Santos-Magalhães and al., 2004). In addition to this, nano-drug
Mosqueira, 2010). In 2005–06, ACTs delivery systems (NDDs) provide
were deployed as first-line treatment in protection to unstable drugs, cell
several endemic countries in Africa, as a adhesion properties, and ability to
result, the malaria cases and deaths were conjugate specific ligands on their
reported to be declining (O'Meara et al., surface (Date et al., 2007; Kayser and
2008). There were reports of high failure Kiderlen, 2003). NDDs such as
rates of ACT along Thai-Cambodian liposomes, polymeric nanoparticles, solid
border (Noedl et al., 2008; Vijaykadga et lipid nanoparticles, dendrimers, nano-
al., 2006). Data showed the development emulsions are extensively studied for
of possible artemisinin resistance. antimalarial drug delivery. These NDDs
Moreover, artemisinin derivatives were are used to deliver encapsulated
reported to show dose, time and route therapeutic agents either by passive or
dependent neurotoxicity in laboratory active targeting strategy. Brief accounts
animals (Petras et al., 2000). of studies done using different NDDs are
Nevertheless, no report is available given below.
regarding the toxicity of artemisinin and
its derivatives in human. The observed Passive targeting
discrepancy between animal and human Malaria infected erythrocytes and
studies may be due to different routes of occasionally hepatocytes are targeted
Biomed Res J 2017;4(2):151-161
155 Nanomedicine for antimalarial drug delivery
using NDDs either by active or passive using passive targeting strategy.
targeting (Santos-Magalhães and Liposomes are spherical vesicles made
Mosqueira, 2010) strategy. In passive up of lipid bilayers. Liposomal drug
targeting, conventional NDDs or surface delivery systems are widely used for
modified long circulating NDDs their biocompatibility, biodegradability
preferentially accumulate at targeted site and their ability to encapsulate both
due to physiochemical and hydrophilic and hydrophobic therapeutic
pharmacological factors (Barratt, 2003; agents. Nayak et al. (2012) investigated
Garnett, 2001). Once these NDDs come the therapeutic efficacy of curcuminoids
into contact with hepatocytes or loaded liposomes alone and in
mononuclear phagocyte system and then combination with α/β arteether following
they internalize these NDDs. It is intravenous administration in P. berghei
difficult to target infected RBCs using infected mice. Animals treated with
conventional NDDs as the RBCs are curcuminoids-loaded liposomes showed
phagocytically and endocytically lower parasitemia and higher survival in
inactive. The main strategy of the passive comparison to control group (no
targeting is to increase the plasma treatment). The combination therapy of
maximum concentration (Cmax) of a drug curcuminoids-loaded liposomes (40
which is proportional to the toxicity of mg/kg b.w.) along with α/β arteether (30
drug and the efficacy is proportional to mg/kg b.w.) was able to cure infected
the area under the curve (AUC) of drug mice as well as prevent recrudescence.
plasma concentration (Wong et al., Artemether loaded solid lipid
2008). Availability of higher nanoparticles were produced using
concentration of drug improves the glyceryl trimyristate and soybean oil for
interaction with infected RBCs and treating malaria. Mean particle size, zeta
parasite membranes (Mosqueira et al., potential and drug encapsulation
2004). Long-circulating NDDs are able efficiency were around 120 nm, −38 mV
to improve the AUC of the drugs, and 97% (w/w) respectively.
enhance selectivity and thereby able to Experimental results showed that these
reduce the doses (Owens and Peppas, nanoparticles were effective than free
2006). A good number of novel NDDs drug and corresponding marketed
were investigated for treating malaria formulation in treating malaria (Nayak et
Biomed Res J 2017;4(2):151-161
Gogoi 156
al., 2010a). Akhtar et al. (2012) curcuminoids loaded lipid nanoparticles
developed curcumin loaded chitosan as compared to free curcuminoids
nanoparticles for treating malaria. The (Nayak et al., 2010b).
mean particle size and zeta potential of In addition to delivery of traditional
the nanoparticles were 178 nm and antimalarial drugs, NDDs are used for
+78±7.6 mV, respectively. Experimental delivering genetic materials which
results showed delay in degradation of interfere with gene expression by
curcumin encapsulated in nanoparticles preventing the translation of proteins
in comparison to free curcumin in mouse from mRNA. In one study, antisense
plasma. In vivo results showed better oligonucleotides (ODNs) against
antimalarial activity of these malarial topoisomerase II gene were
nanoparticles than free curcumin. loaded in chitosan nanoparticles.
Chloroquine loaded chitosan Antisense interferes with the gene
nanoparticles were prepared using expression by preventing translation of
ionotropic gelation between chitosan and proteins from mRNA and thereby
sodium tripolyphosphate. These inhibits the growth of P. falciparum.
nanoparticles were evaluated for Chitosan and oligonucleotides in 1:1 or
attenuation of P. berghei infection in 2:1 proportions were prepared with
Swiss mice. Results showed that these negative and positive surface charge
nanoparticles have the capability of fight respectively. Positively charged antisense
parasite infection, oxidative stress, ODN chitosan nanoparticles showed
inflammation and DNA damage similar P. falciparum growth inhibition
(Tripathy et al., 2013). Curcuminoids- as the free ODN, and the negatively
loaded lipid nanoparticles for parenteral charged nanoparticles showed the highest
administration were successfully growth inhibition (87%). This may due to
prepared using trimyristin, tristerin, the fact that less stable chitosan-ODN
glyceryl monostearate and medium chain complexes, as the anionic ones obtained
triglyceride. Particle size and zeta in presence of excess of nucleic acid,
potential were 120−250 nm and −28 to may have led to an earlier complex
−45 mV, respectively, depending nature dissociation and faster onset of action
of lipid used. In vivo results showed 2- (Foger et al., 2006). Recently, a NDD
fold increase in antimalarial activity of based DNA vaccine formulation has been
Biomed Res J 2017;4(2):151-161
157 Nanomedicine for antimalarial drug delivery
prepared for magnetic transfection. the target site (Torchilin, 2006). In
Plasmid DNA encoding for a fragment of malaria, the disease infected erythrocytes
the merozoite surface protein MP1 was in blood and hepatocytes can be targeted
attached to the surface of polyethylene- by tagging the ligands on the surface of
imine-coated superparamagnetic iron the NDDs specific to them. In another
oxide nanoparticles. Due to magnetic study, immunoliposomes using 1,2-
transfection, the magnetic NDDs have Dioleoyl-sn-glycero-3-phospho -choline
been proven to improve efficiency and (DOPC) and cholesterol were developed
rate of gene delivery to different tissues for delivering chloroquine and
and they elicited IgG2a and IgG1 fosmidomycin. These liposomes were
responsible for the protective immunity tagged with monoclonal antibody
against malaria (Al-Deen et al., 2013). In BM1234 specific to parasite infected
another study dihydroartemisinin loaded RBCs. In vitro experiments showed 10
solid lipid nanoparticles (DHA-SLNs) fold increase in antimalarial activity of
were prepared to overcome the poor drug following encapsulation in
water-solubility, poor pharmacokinetic immunoliposomes as compared to free
profile and inadequate clinical outcome drug (Urban et al., 2011). Dendritic
of monotherapy. In vitro and in vivo derivatives based on 2,2-bis(hydroxy-
results showed the enhancement of methyl) propionic acid and pluronic
therapeutic efficacy of DHA-SLNs in polymers have been studied for
comparison to the free DHA. Results delivering antimalarial drugs CQ and PQ
showed the potential of using this to target Plasmodium-infected red blood
formulation of clinical application cells (pRBCs). Experimental results
(Omwoyo et al., 2016). demonstrated the possibility of using
dendrimers for effective targeted delivery
Active targeting of therapeutic agents to pRBCs
In active targeting, the surface of the (Movellan et al., 2014). Owais et al.
NDDs are conjugated with specific (1995) developed chloroquine loaded
ligands such as carbohydrates, proteins, liposomes tagged with antibody against
peptides or antibodies specific to the infected erythrocytes and tested their
disease infected cells or tissue, which efficacy in chloroquine-resistant P.
guide the NDDs or drug to accumulate in berghei infected mice. Results showed
Biomed Res J 2017;4(2):151-161
Gogoi 158
+
that selected homing of chloroquine to reduce CD8 T cell and supress pRBC
malaria-infected erythrocytes helped in sequestration in the brain. It is an ideal
curing of the chloroquine-resistant adjuvant drug to prevent and treat
malarial infections with reduced dose cerebral malaria. Dende et al. (2015)
(Owais et al., 1995). Quinine dihydro- showed that curcumin alone was
chloride is one of the drugs of effective effective in reducing leukocyte as well as
in treating cerebral malaria, but, pRBC sequestration in the brain,
delivering it to the brain capillaries is maintaining BBB integrity whereas
difficult. Transferrin has high affinity for arteether prevented pRBC sequestration
receptors present in brain capillaries and in the brain, parasitemia builds up in
hence transferrin-targeted SLNs were blood. Combination of Curcumin-
prepared for targeted delivery of quinine artether administered after the onset of
hydrochloride to brain. SLNs prepared neurological symptoms, was very
using hydrogenated soy phosphatidyl- effective in counteracting all the
choline, triolein, cholesterol and distearyl investigated parameters governing
phosphatidylethanolamine, followed by leukocyte as well as pRBC sequestration.
covalent coupling of transferrin were All the animals were protected against
reported to be effective in delivering mortality at least for 90 days.
quinine hydrochloride to brain (Gupta et
al., 2007). Challenges and Future Prospects
Zhao et al. (2014) demonstrated Malaria is affecting large number of
during experimental cerebral malaria people worldwide with huge mortality
(ECM) that brain becomes severely rate. Nanoscale materials are offering
dysfunctional due to multiple unique and novel opportunities to
pathological events such as blood–brain address the issues related to the anti-
barrier (BBB) disruption, vascular malarial therapy. Today advancement of
leakage, and immune cell accumulation nanotechnology is providing powerful
(especially CD8 T cell infiltration). They platforms ranging from diagnostic,
demonstrated using mice model that detection of diseases in the early stage
olfactory bulb region is a vulnerable and delivery of therapeutics for the
location for vascular leakage during neglected diseases like malaria. But,
ECM. Curcumin has the potential to safety is a major concern for production
Biomed Res J 2017;4(2):151-161
159 Nanomedicine for antimalarial drug delivery
of these NDDs/ nanoparticles. Owing to nanomedicine (Sanhai et al., 2008).
smaller size, these nanoparticles are But, seeing the potential of NDDs in
highly reactive due to huge surface area, biomedical engineering and healthcare
which must be addressed before using sector, large amount of works are being
them in clinical setup. Moreover, prior done globally to overcome these
knowledge of biodistribution of NDDs in challenges; more and more NDDs are
the body following systemic reaching the clinical applications. As a
administration; pictorial evidence of result, number of nano-formulation
NDDs distribution in vivo following getting FDA approval is increasing in
administration, understanding the mass recent years.
transport across the body's
compartmental boundaries; developing CONCLUSIONS
new mathematical and computer models Malaria is a complex disease that has
that will contribute to a 'periodic table' of been affecting the people from tropical
nanoparticles for predicting risk and and subtropical countries. But, the recent
benefit parameters as well as development in nanomedicine is opening
establishment of standards or reference up new possibilities and is providing
materials and consensus testing protocols better solution in treating complex
that can provide benchmarks for the diseases like malaria. Effective malaria
development of novel classes of treatment strategies are anticipated in
materials, are few concerns related to the near future.
REFERENCES
Akhtar F, Rizvi MM, Kar SK. Oral delivery of 60(1):21–37.
curcumin bound to chitosan nanoparticles Date AA, Joshi MD, Patravale VB. Parasitic
cured Plasmodium yoelii infected mice. diseases: Liposomes and polymeric
Biotechnol Adv 2012;30(1):310–320. nanoparticles versus lipid nanoparticles. Adv
Al-Deen FN, Ma C, Xiang SD, Selomulya C, Drug Deliv Rev 2007;59(6):505–521.
Plebanski M, Coppel RL. On the efficacy of Dende C, Meena J, Nagarajan P, Panda AK,
malaria DNA vaccination with magnetic Rangarajan PN, Padmanaban G.
gene vectors. J Control Release 2013; Simultaneously targeting inflammatory
168(1):10–17. response and parasite sequestration in brain
Barratt G. Colloidal drug carriers: Achievements to treat experimental cerebral malaria. Sci
and perspectives. Cell Mol Life Sci 2003; Report 2015;5:12671–12685.
Biomed Res J 2017;4(2):151-161
Gogoi 160
Duong S, Lim P, Fandeur T, Tsuyuoka R, Antimicrob Agent Chemother 2004;48(4):
Wongsrichanalai C. Importance of 1222–1228.
protection of anti-malarial combination Movellan J, Urbán P, Moles E, de la Fuente JM,
therapies. Lancet 2004;364(9447):1754– Sierra T, Serrano JL, Fernàndez-Busquets
1755. X. Amphiphilic dendritic derivatives as
Foger F, Noonpakdee W, Loretz B, Joojuntr S, nanocarriers for the targeted delivery of
Salvenmoser W, Thaler M, Bernkop- antimalarial drugs. Biomater 2014;35(27):
Schnürch A. Inhibition of malarial 7940–7950.
topoisomerase II in Plasmodium falciparum Murambiwa P, Masola B, Govender T,
by antisense nanoparticles. Int J Pharm Mukaratirwa S, Musabayane CT. Anti-
2006;319(1–2):139–146. malarial drug formulations and novel
Garnham PC. Comments on biology of human delivery systems: A review. Acta Tropica
malaria. Mil Med 1966;131(9):961–962. 2011;118(2):71–79.
Garnett MC. Targeted drug conjugates: Principles Nayak AP, Patankar S, Madhusudhan B, Murthy
and progress. Adv Drug Deliv Rev 2001; RS, Souto EB. Artemeter-loaded lipid
53(2):171–216. nanoparticles produced by modified thin-
Gupta Y, Jain A, Jain SK. Transferrin-conjugated film hydration: pharmacokinetics,
solid lipid nanoparticles for enhanced toxicological and in vivo anti-malarial
delivery of quinine dihydrochloride to the activity. Eur J Pharm Sci 2010a;40(5):448–
brain. J Pharm Pharmacol 2007;59(7):935– 455.
940. Nayak AP, Tiyaboonchai W, Patankar S,
Jarcho S. Malaria and murder (Joseph Jones, Madhusudhan B, Souto EB. Curcuminoids-
1878). Bull N Y Acad Med 1968;44(6):759– loaded lipid nanoparticles: Novel approach
760. towards malaria treatment. Colloid Surf B:
Kayser O, Kiderlen AF. Delivery strategies for Biointerface 2010b;81(1):263–273.
antiparasitics. Expert Opin Invest Drugs Nayak AP, Chimote G, Gunalan K, Banerjee R,
2003;12(2):197–207. Patankar S, Madhusudhan B.
Korenromp EL, Williams BG, Gouws E, Dye C, Curcuminoids-loaded liposomes in
Snow RW. Measurement of trends in combination with arteether protects against
childhood malaria mortality in Africa: an Plasmodium berghei infection in mice. Exp
assessment of progress toward targets based Parasitol 2012;131(3):292–299.
on verbal autopsy. Lancet Infect Dis Nayak AP, Vathsala PG, Vieira V, Murthy RSR,
2003;3(6):349–358. Souto EB. Advances in nanomedicines for
Mosqueira VCF, Loiseau PM, Bories C, Legrand malaria treatment. Adv Colloid Interface Sci
P, Devissaguet JP, Barratt G. Efficacy and 2013;201–202;1–17.
pharmacokinetics of intravenous Noedl H, Se Y, Schaecher K, Smith BL, Socheat
nanocapsule formulations of halofantrine in D, Fukuda MM. Evidence of artemisinin-
Plasmodium berghei-infected mice. resistant malaria in western Cambodia;
Biomed Res J 2017;4(2):151-161
161 Nanomedicine for antimalarial drug delivery
Artemisinin Resistance in Cambodia 1 560–575.
(ARC1) Study Consortium. N Engl J Med Torchilin VP. Multifunctional nanocarriers. Adv
2008;359(24):2619–2620. Drug Deliv Rev 2006;58(14):1532–1555.
O'Meara WP, Bejon P, Mwangi TW, Okiro EA, Tripathy S, Mahapatra SK, Chattopadhyay S, Das
Peshu N, Snow RW, et al. Effect of a fall in S, Dash SK, Majumder S, Pramanik P, Roy
malaria transmission on morbidity and S. A novel chitosan based antimalarial drug
mortality in Kilifi, Kenya. Lancet 2008; delivery against Plasmodium berghei
372(9649):1555–1562. infection. Acta Tropica 2013;128(3):494–
Omwoyo WN, Melariri P, Gathirwa JW, Oloo F, 503.
Mahanga GM, Kalombo L, Ogutu B, Swai Tuteja R. Malaria – an overview. FEBS J 2007;
H. Development, characterization and 274(18):4670–4679.
antimalarial efficacy of dihydroartemisinin Urban P, Estelrich J, Adeva A, Cortes A,
loaded solid lipid nanoparticles. Fernandez-Busquets X. Study of the
Nanomedicine 2016;12(3):801–809. efficacy of antimalarial drugs delivered
Owais M, Varshney GC, Choudhury A, Chandra inside targeted immunoliposomal
S, Gupta CM. Chloroquine encapsulated in nanovectors. Nanoscale Res Lett 2011a;6:
malaria-infected erythrocyte-specific 620.
antibody-bearing liposomes effectively Vijaykadga S, Rojanawatsirivej C, Cholpol S,
controls chloroquine-resistant Plasmodium Phoungmanee D, Nakavej A,
berghei infections in mice. Antimicrob Wongsrichanalai C. In vivo sensitivity
Agents Chemother 1995;39(1):180–184. monitoring of mefloquine monotherapy and
rd
Owens DE 3 , Peppas NA. Opsonization, artesunate-mefloquine combinations for the
biodistribution and pharmacokinetics of treatment of uncomplicated falciparum
polymeric nanoparticles. Int J Pharm 2006; malaria in Thailand in 2003. Trop Med Int
307(1):93–102. Health 2006;11(2):211–219.
Petras J, Young GD, Bauman RA, Kyle DE, Wong J, Brugger A, Khare A, Chaubal M,
Gettayacamin M, Webster H. Arteether- Papadopoulos P, Rabinow B, Kipp J, Ning
induced brain injury in Macaca mulatta. I. J. Suspensions for intravenous (IV)
The precerebellar nuclei: the lateral reticular injection: a review of development,
nuclei, the paramedian reticula nuclei, and preclinical and clinical aspects. Adv Deliv
perihypoglossal nuclei. Anat Embryol 2000; Rev 2008;60(8):939–954.
20(5):383–397. WHO. World Malaria Report 2016. Geneva:
Sanhai WR, Sakamoto JH, Canady R, Ferrari M. World Health Organization. 2016.
Seven challenges for nanomedicine. Nat Zhao H, Aoshi H, Kawai S, Mori Y, Konishi A,
Nanotechnol 2008;3(5):242–244. Ozkan M, et al. Olfactory plays a key role
Santos-Magalhães NS, Mosqueira VC. in Spatiotemporal pathogenesis of Cerebral
Nanotechnology applied to the treatment of Malaria. Cell Host Microbe 2014;15(5):
malaria. Adv Drug Del Rev 2010;62(4–5): 551–563.
Biomed Res J 2017;4(2):151-161
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5811)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Omni 1983 01 PDFDocument82 pagesOmni 1983 01 PDFMatthew Levi StevensNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- West Africa Ghana Nigeria Specific Pharmaceutical Industry PDFDocument32 pagesWest Africa Ghana Nigeria Specific Pharmaceutical Industry PDFMadisonCloeNo ratings yet
- Assess and Classify The Sick Child Age 2 Months Up To 5 YearsDocument30 pagesAssess and Classify The Sick Child Age 2 Months Up To 5 YearsRommel G. Santiago100% (2)
- Pharmacy MCQSDocument132 pagesPharmacy MCQSomair zafar100% (6)
- What Are AlkaloidsDocument29 pagesWhat Are AlkaloidsmhadhiehNo ratings yet
- Química de Los AntibióticosDocument227 pagesQuímica de Los AntibióticosArturo García FloresNo ratings yet
- Integrated Management of Childhood IllnessesDocument65 pagesIntegrated Management of Childhood IllnessesJocel LañasNo ratings yet
- Magnetic Nanostructures For Cancer Theranostic ApplicationsDocument9 pagesMagnetic Nanostructures For Cancer Theranostic ApplicationsManash GogoiNo ratings yet
- Nano - Biphasic Magnetic Nanoparticles - Nanovesicle Hybrids For Chemotherapy and Self-Controlled HyperthermiaDocument14 pagesNano - Biphasic Magnetic Nanoparticles - Nanovesicle Hybrids For Chemotherapy and Self-Controlled HyperthermiaManash GogoiNo ratings yet
- IB - Biocompatibility and Therapeutic Evaluation of Magnetic Liposomes Designed For Self-Controlled Cancer Hyperthermia and ChemotherapyDocument11 pagesIB - Biocompatibility and Therapeutic Evaluation of Magnetic Liposomes Designed For Self-Controlled Cancer Hyperthermia and ChemotherapyManash GogoiNo ratings yet
- Paper On HyperthermiaDocument7 pagesPaper On HyperthermiaManash GogoiNo ratings yet
- Cancer HyperthermiaDocument14 pagesCancer HyperthermiaManash GogoiNo ratings yet
- Pharmacology of AntimalarialsDocument39 pagesPharmacology of AntimalarialsAntonyNo ratings yet
- Mechanism of Action of Hydroxychloroquine As An Antirheumatic DrugDocument10 pagesMechanism of Action of Hydroxychloroquine As An Antirheumatic DrugJim MorrisonNo ratings yet
- Team Motivation: Test and DiscussionDocument82 pagesTeam Motivation: Test and Discussionfascondahens_5777232No ratings yet
- 1 SM PDFDocument15 pages1 SM PDFJuan LunaNo ratings yet
- B.K. Tyagi - Desert Malaria - An Emerging Malaria Paradigm and Its Global Impact On Disease Elimination-Springer (2023)Document424 pagesB.K. Tyagi - Desert Malaria - An Emerging Malaria Paradigm and Its Global Impact On Disease Elimination-Springer (2023)drcsraoclinicNo ratings yet
- Artemether LumefantrineDocument43 pagesArtemether LumefantrineneisslabsNo ratings yet
- Isoflurane Inhalation: Outer Restrict Use Cost $ADocument8 pagesIsoflurane Inhalation: Outer Restrict Use Cost $AportosinNo ratings yet
- Chloroquine - Drug Information - UpToDateDocument9 pagesChloroquine - Drug Information - UpToDatedfdfffffNo ratings yet
- Antimalarial Drug CologyDocument15 pagesAntimalarial Drug CologyManthan ChauhanNo ratings yet
- MALARIADocument7 pagesMALARIAjeccomNo ratings yet
- Chart Booklet National Mac 2012Document42 pagesChart Booklet National Mac 2012Suhazeli AbdullahNo ratings yet
- Stephen Danso - MensahDocument126 pagesStephen Danso - MensahfikrifazNo ratings yet
- Block G Pre Proff KGMC 2022-PrintDocument23 pagesBlock G Pre Proff KGMC 2022-PrintF ParikhNo ratings yet
- Reading Comprehension Test 8Document4 pagesReading Comprehension Test 8Adán Yanes LopezNo ratings yet
- Pharma - CCRDocument24 pagesPharma - CCRPrathik YanalaNo ratings yet
- Anti Protozoal P1Document5 pagesAnti Protozoal P1N Gv FcNo ratings yet
- Malaria ChemopreventionDocument38 pagesMalaria Chemopreventionmiruna apostolNo ratings yet
- COPAR ReadingDocument2 pagesCOPAR ReadingDizerine Mirafuentes RolidaNo ratings yet
- Part-2-ParasitologyDocument33 pagesPart-2-ParasitologyAli AhmedNo ratings yet
- Malaria: DR MD Mamunul Abedin ShimulDocument41 pagesMalaria: DR MD Mamunul Abedin ShimulDr. Mamunul AbedinNo ratings yet
- Antimalaria Drug PolicyDocument35 pagesAntimalaria Drug PolicyBobskinny100% (1)
- Malaria Rapid Diagnostic Test Performance: Results of Who Product Testing of Malaria RDTS: Round 7 (2015-2016)Document164 pagesMalaria Rapid Diagnostic Test Performance: Results of Who Product Testing of Malaria RDTS: Round 7 (2015-2016)clive.mascarenhas909No ratings yet
- Dr. Naitik D. Trivedi & Dr. Upama N. Trivedi: AntimalariaDocument19 pagesDr. Naitik D. Trivedi & Dr. Upama N. Trivedi: AntimalariaSuraj PatilNo ratings yet