Professional Documents
Culture Documents
Health Financing in Indonesia: A Reform Road Map
Health Financing in Indonesia: A Reform Road Map
Uploaded by
Vita WidyasariCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Health Financing in Indonesia: A Reform Road Map
Health Financing in Indonesia: A Reform Road Map
Uploaded by
Vita WidyasariCopyright:
Available Formats
FACT SHEET
Health Financing in Indonesia: A Reform Road Map
Indonesia has made major improvements in health outcomes
Health outcomes have improved significantly since 1980 when life expectancy was only 52 years compared to almost 70 today,
and some 100 infants out of every 1000 died before their first birthday, compared to less than 30 today. The total fertility rate has
declined from 4.7 children per woman to slightly above 2. Despite these impressive improvements, Indonesia’s achievements
have been less impressive than some of its neighbors, and for certain health outcomes, such as maternal mortality, the country
does not perform as well as other comparable income and health spending level countries.
Indonesia’s health delivery capacity has expanded significantly
Indonesia’s health delivery system expanded significantly over the past 40 years. Virtually all Indonesian’s have access to basic
care through a network of 8000 Puskesmas and 22,200 Puskesmas Pembantu, and some 5,800 mobile health clinics. On the other
hand, while Indonesia has far fewer hospital beds per capita compared to other comparable income countries, these beds are
poorly utilized with occupancy rates on the order of 60 percent. In terms of human resources for health, while nurse mid-wives
are readily available throughout the country, Indonesia’s health workforce overall is small relative to other similar income
countries and concerns over quality and efficiency persist. Its physician workforce is very small relative to comparators, and there
are severe shortages of specialists, which are particularly problematic given the proposed expansions in health insurance
coverage and the oncoming non-communicable disease burden. There are serious equity, quality, and efficiency problems
underlying Indonesia’s current health delivery system which, unless corrected, will result in major access, cost, and sustainability
problems as the country moves to universal health insurance coverage.
Indonesia’s health spending is relatively low and the country gets reasonable ‘value for money’ in terms of some health
outcomes as well as relatively good financial protection
Indonesia spends only slightly more than 2 percent of its GDP on health, about half the level of other comparable income
countries. Half of all health spending is public. About one-third of health spending comes directly from of out of pocket
payments by households. Health is a relatively small share of the government’s budget, some 5 percent, although the share has
been increasing since the implementation of the Askeskin program in 2004. Despite low spending health outcomes and financial
protection are relatively good, although these latter results may be due to Indonesia’s relatively high education levels and
extended family social structure. On the other hand, some health outcomes such as maternal mortality, which is dependent on a
well functioning health system, are worse than other comparators and analyses of technical efficiency suggest that there are some
potentially serious problems.
The reform needs to build on the system’s strength’s and address its weaknesses
The report documents the health system’s strengths and weaknesses based on empirical analyses of health spending, health
outcomes, financial protection, consumer responsiveness, quality, equity, and efficiency.
Strengths Weaknesses
Favorable demographic circumstances Half the population lacks health insurance coverage
High educational and literacy levels Government health subsidies disproportionally benefit
Government commitment for reform the rich
Low levels of health spending Health financing and delivery systems are highly
Reasonable financial protection and consumer fragmented
satisfaction Some health outcomes are poor
Experience with health insurance programs Demographic, epidemiological, and nutrition transitions
An extensive primary care delivery system will place significant pressures on future health care
Generally good availability of pharmaceuticals. costs and delivery system needs
Significant geographic disparities in health outcomes,
availability and use of services persist
Human and physical infrastructures are limited and face
quality and efficiency problems
Significant improvements in the quality and costs of
pharmaceuticals, which account for some one-third of
health spending, are needed
Decentralization has confused the roles and
responsibilities of the different levels of government and
the intergovernmental transfer system does not yet fully
recognize differences in need and fiscal capacity
For more information on the World Bank’s program,
visit: www.worldbank.org/id
Critical data for decision-making are lacking
Design features of the Jamsostek and Askes programs
result in high out of pocket costs for program
beneficiaries and preclude effective operation
No comprehensive studies of the health outcome and
financial impacts, real costs, and future sustainability of
the Askeskin/Jamkesmas programs.
Indonesia’s reform process needs to address both broad policy concerns such as the final system design and transition
options as well as numerous ‘devils in the details’ including the design of the basic benefits package; groups eligible for
public subsidies; identification and collection of premiums from informal sector workers; how medical care providers
will be paid; how the reform will be financed; who will administer the program; and, how will better health outcomes,
financial protection, consumer responsiveness, quality, efficiency, equity, and financial sustainability be assured.
While the Government has made some important progress in developing draft laws to implement the Social Security Reform Law
40/2004, the report notes that much additional work needs to be done. It also highlights the need for the Government to specify
its final vision for universal coverage and develop and cost the various transition options and timing to get there. It highlights
several potential final visions including a single national mandatory health insurance system where the government subsidizes the
poor and other disadvantaged groups as in Turkey, Thailand, Columbia, and Chile as well as a ‘Jamkesmas for all’ approach
which is fully financed by the government and very much approximates the national health service systems in Sri Lanka and
Malaysia. Development of the transition options and final reform impacts will require specification of key program details. The
report develops a policy framework for addressing the key policy issues requiring resolution based on the system’s strengths and
weaknesses, Indonesia-specific and international experience, and underlying public health, health insurance, health economics
and public finance principles.
The report also focuses heavily on the need for solid actuarial analyses of the costs and revenues of the various options and the
challenge to the government to assure sustainability of the reform within its available future fiscal space. If upon achieving
universal coverage Indonesia’s spending jumps to the level in other comparable income countries and Indonesia faces the cost
pressures of the industrialized countries, health spending in 2040 could reach almost 10 percent of GDP compared to just over 2
percent today. If the government can hold future cost pressures to their historic rates of increase, then spending well be on the
order of 6 percent of GDP. The report highlights the importance of getting the key design elements of the reform ‘right’, a rather
complex policy challenge given the interactions among reform components as well as Indonesia’s socioeconomic situation which
includes a large number of poor, much of the population living in rural areas, a high percentage of informal sector workers, and a
large number of very small firms.
For more information on the World Bank’s program,
visit: www.worldbank.org/id
You might also like
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Consulting Casebook MckinseyDocument84 pagesConsulting Casebook MckinseyMaria Pappa100% (2)
- Topic 5 Corporate Social ResponsibilityDocument7 pagesTopic 5 Corporate Social Responsibilitymoza salim100% (1)
- Toward A New World Order by George SorosDocument12 pagesToward A New World Order by George SorosrexxturboNo ratings yet
- INCOTERMS 2010 - Illustrated GuideDocument28 pagesINCOTERMS 2010 - Illustrated Guidevarun_nayak_167% (3)
- ISO 14041: Environmental Management - Life Cycle Assessment - Goal and Scope Definition - Inventory AnalysisDocument1 pageISO 14041: Environmental Management - Life Cycle Assessment - Goal and Scope Definition - Inventory AnalysisSrikanth MeesaNo ratings yet
- Cost Calculation TCG 2020 V16K With CNGDocument2 pagesCost Calculation TCG 2020 V16K With CNGR_afflyNo ratings yet
- Bagasse Based CogenerationDocument13 pagesBagasse Based CogenerationknsaravanaNo ratings yet
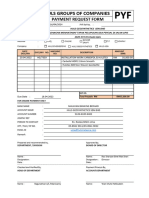
- PRF - SupplierDocument18 pagesPRF - Supplierdeanwolves16No ratings yet
- Iron and Steel Industry Report 2018 enDocument28 pagesIron and Steel Industry Report 2018 enAlexei AlinNo ratings yet
- Chapter 9 QuizDocument9 pagesChapter 9 QuizRaven PicorroNo ratings yet
- Bills of Exchange Bill emDocument5 pagesBills of Exchange Bill emBlue HughesNo ratings yet
- Contabilidad. Plantilla Inventario AnalíticoDocument14 pagesContabilidad. Plantilla Inventario AnalíticoRubenSanchezLopezNo ratings yet
- Multiple Choice QuestionsDocument4 pagesMultiple Choice QuestionsErlina MasoenNo ratings yet
- Coursenotes BFB4133-090212 102219Document101 pagesCoursenotes BFB4133-090212 102219Makisha NishaNo ratings yet
- 2 - P. S. Sikarwar EnterprisesDocument1 page2 - P. S. Sikarwar Enterprisespriyanka singhNo ratings yet
- Domestic Production and Foreign Trade The American Capital Position Re-ExaminedDocument23 pagesDomestic Production and Foreign Trade The American Capital Position Re-ExaminedKevin Mcdonald100% (2)
- Agricultural Economics Exam Bank SummaryDocument66 pagesAgricultural Economics Exam Bank SummaryTsion GetuNo ratings yet
- GSE EnVision UsersListDocument2 pagesGSE EnVision UsersListasamad54No ratings yet
- Introduction On The Study of GlobalizationDocument7 pagesIntroduction On The Study of GlobalizationJezalen GonestoNo ratings yet
- 2014 GIST Tech-I Marrakech BrochureDocument92 pages2014 GIST Tech-I Marrakech BrochureAmandaNo ratings yet
- Migrants' Election ManifestoDocument2 pagesMigrants' Election ManifestoMimi Panes - CorosNo ratings yet
- National Housing Policy (NHP) - 1998Document2 pagesNational Housing Policy (NHP) - 1998Ms. Sangeetha Priya I Assistant Professor I - SPADENo ratings yet
- Environment CASE STUDYDocument2 pagesEnvironment CASE STUDYNosheen JillaniNo ratings yet
- The Legatum Prosperity Index™ 2017Document2 pagesThe Legatum Prosperity Index™ 2017Sputnik MoldovaNo ratings yet
- Sistemas de EcuacionesDocument5 pagesSistemas de EcuacionesRafaNo ratings yet
- Bond YieldsDocument27 pagesBond YieldsSagar TanejaNo ratings yet
- IQSK Issue 31 - April - June 2021 Journal EditionDocument50 pagesIQSK Issue 31 - April - June 2021 Journal Editionbenson njihiaNo ratings yet
- A Brief History of MacroeconomicsDocument13 pagesA Brief History of Macroeconomicsزهير استيتوNo ratings yet
- Banyan HydraulicsDocument1 pageBanyan HydraulicsmshNo ratings yet
- Function of Households Reading, Matching, Multiple ChoiceDocument2 pagesFunction of Households Reading, Matching, Multiple ChoiceMikias TewachewNo ratings yet