Professional Documents
Culture Documents
Approach To Pediatric Vomiting - 0 PDF
Uploaded by
Mey KhOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Approach To Pediatric Vomiting - 0 PDF
Uploaded by
Mey KhCopyright:
Available Formats
PedsCases Podcast Scripts
This is a text version of a podcast from Pedscases.com on “Approach to Pediatric Vomiting.” These podcasts are
designed to give medical students an overview of key topics in pediatrics. The audio versions are accessible on iTunes
or at www.pedcases.com/podcasts.
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014.
Approach to Pediatric Vomiting (Part 1)
Introduction
Hi, Everyone! My name is Erin Boschee and I’m a medical student at the University of
Alberta. This podcast was reviewed by Dr. Melanie Lewis, a General Pediatrician and
Associate Professor at the University of Alberta and Stollery Children’s Hospital in
Edmonton, Alberta, Canada. This is the first in a series of two podcasts discussing an
approach to pediatric vomiting.
We will focus on the following learning objectives:
1) Create a differential diagnosis for pediatric vomiting.
2) Highlight the key causes of vomiting specific to the newborn and pediatric
population.
3) Develop a clinical approach to pediatric vomiting through history taking, physical
exam and investigations.
Case Example
Let’s start with a case example that we will revisit at the end of the podcasts.
You are called to assess a 3-week old male infant for recurrent vomiting and ‘feeding
difficulties.’ The ER physician tells you that the mother brought the baby in stating that
he started vomiting with every feed since around two weeks of age. In the last three
days he has become progressively more sleepy and lethargic. She brought him in this
afternoon because he vomited so forcefully that it sprayed her in the face. The
physician confirms that the baby is stable, and his vitals are within normal range, except
that he is mildly tachycardic.
What else will you want to ask when you go to see the baby? What will you look for on
physical exam and what tests might you order?
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
Before we think about our clinical approach to this vomiting infant, let’s take a few
minutes to discuss some of the common causes of pediatric vomiting.
Pathophysiology
Vomiting is the forceful expulsion of the stomach contents through the mouth via
contraction of the abdominal and chest wall muscles. An emetic response may be
triggered by irritation of the gastric mucosa by toxins, drugs or overdistension, which
stimulates vagal afferents to the vomiting center in the brain. Afferent impulses from
other areas of the brain, such as the vestibular system, the amygdala (as with emotion
or fear), or from certain organs outside the GI tract can stimulate vomiting in a similar
mechanism. Stimulation of the ‘chemoreceptor trigger zone’ in the area postrema of the
4th ventricle by toxins, electrolyte or metabolic disturbances or increased intracranial
pressure also results in vomiting through activation of the vomiting center.
It can be helpful to think of the pathophysiological mechanisms that cause vomiting
when trying to create a differential diagnosis.
Differential Diagnosis
Vomiting is a very common pediatric presentation, and the differential is extremely
broad. While GI (gastrointestinal) causes tend to come to mind first, there are many
non-GI causes for vomiting that have to be considered. The causes for pediatric
vomiting can be broken into categories including gastrointestinal, infectious,
neurologic, metabolic/endocrine, respiratory, toxin or medication-related and
psychogenic or behavioral.
Now that you know a broad systems approach to the causes of vomiting, let’s focus a
bit more on some of the common specific conditions.
Gastrointestinal Causes
There are several approaches that can be followed when considering the GI causes of
pediatric vomiting. A simple approach is to group the causes by age as different
diagnoses tend explain vomiting in newborns versus vomiting in infants and older
children.
Important causes of vomiting in the newborn period include pyloric stenosis, duodenal
atresia, intestinal malrotation and tracheo-esophageal fistula. We’ll spend a few
minutes now discussing the distinguishing features of these conditions.
Pyloric stenosis is the hypertrophy of the pyloric muscles at the outlet of the stomach.
This results in projectile, non-bilious vomiting immediately following feeds that presents
in the first few weeks of life. Infants are classically firstborn males with a positive family
history of pyloric stenosis, and may have visible abdominal peristalsis or a palpable
olive-shaped mass near the umbilicus. It is considered a medical (not surgical)
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
emergency due to the risk of severe electrolyte disturbances – classically, a
hypochloremic hypokalemic metabolic alkalosis.
Duodenal atresia is the congenital absence of a portion of the first part of the small
bowel. Symptoms typically present shortly after birth. They may present with either
bilious or non-bilious vomiting, depending whether the atresia is distal or proximal to the
ampulla of Vater, the site where bile and pancreatic enzymes are released into the
duodenum from the common bile duct. It typically does not present with abdominal
distension. A classical x-ray finding associated with duodenal atresia is the ‘double
bubble sign.’
In contrast, intestinal malrotation, a congenital anomaly in rotation of the midgut as it
forms, presents as intermittent bilious vomiting, usually with significant abdominal
distension. It may be associated with severe abdominal pain if associated with midgut
volvulus causing bowel ischemia. Since the bowel obstruction is often intermittent, the
timing of presentation can be variable. Bilious or bile-stained vomiting should be treated
as a potential surgical emergency.
Tracheo-esophageal fistula, or TEF, is an abnormal connection between the trachea
and esophagus. TEF usually presents with cough, cyanotic episodes with feeding,
respiratory distress, or recurrent pneumonia. Other defects associated with the
VACTERL association may be present, such as vertebral anomalies, anal atresia,
congenital heart disease, renal or radial anomalies or limb defects. There are five
different forms of TEF, which are distinguished by the location of the esophageal atresia
and connection to the trachea. Types with a complete esophageal atresia typically
present shortly after feeding begins as there is a complete obstruction. However, other
variants such as the H-type of TEF may present later in life with symptoms of recurrent
cough or aspiration pneumonia. This is because the main feature is an abnormal
connection to the trachea, and there is no complete esophageal atresia.
Necrotizing enterocolitis is common in premature infants and may present as
decreased feeding tolerance, vomiting, abdominal distension, diarrhea or
hematochezia. Other neonatal causes of vomiting include meconium ileus,
Hirschsprung disease, and imperforate anus.
After the newborn period, important gastrointestinal causes of vomiting include
gastroesophageal reflux disease (GERD), intussusception and other causes of bowel
obstruction, food allergy, eosinophilic esophagitis and appendicitis.
Gastro-esophageal reflux (GER) is extremely common and typically presents in
infants between 1-3 months of age. It is characterized by frequent small volume
regurgitation of a milky substance, irritability with feeds or when lying supine, or back
arching with feeds. Many infants are asymptomatic. Gastro-esophageal reflux is a
normal physiologic process in infants and must be distinguished from gastro-
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
esophageal reflux disease (GERD), which is associated with esophagitis, failure to
thrive and recurrent aspiration.
Intussusception involves invagination of a portion of the small bowel into another
portion of bowel. It is the most common cause of intestinal obstruction in children six to
36 months of age. In addition to vomiting, the classic triad of features includes
intermittent, progressive abdominal pain, red currant jelly stools and a palpable
sausage-like abdominal mass.
Food allergies such as milk protein allergy in infants or celiac disease in older infants
and children are other fairly common causes of vomiting.
Eosinophilic esophagitis, a disease characterized by eosinophilic infiltrates in the
esophagus is another cause of vomiting often found in older children or adolescents
with a history of asthma, atopy and eczema, who complain of food sticking in the
esophagus.
Lastly, appendicitis is a common GI cause of vomiting in children and adolescents that
should not be missed. Usually, there will also be a history of fever and abdominal pain.
Non-Gastrointestinal Causes
Let’s take a few moments to review the common non-GI causes of vomiting in children.
The classic infectious cause of vomiting is gastroenteritis, and it is likely the most
common cause of vomiting from infancy into adolescence. It is typically associated with
fever, diarrhea and/or abdominal cramping or pain. Often there is a history of sick
contacts. Gastroenteritis can become quite serious, especially in infants and younger
children, who are highly susceptible to dehydration and electrolyte disturbances.
Other common infectious causes in children must also be considered. These can
include urinary tract infections, meningitis and sepsis. Note that meningitis and
pyelonephritis classically present with vomiting and fever.
Neurological causes of vomiting relate to increased intracranial pressure and can
include hydrocephalus, intracranial neoplasms, and pseudotumor cerebri in older
children. The history should be suggestive of other symptoms of increased intracranial
pressure, such as morning headaches, focal neurological deficits or changes in vision.
Migraines can be another common cause for vomiting in older children.
Metabolic and endocrine causes include diabetic ketoacidosis (DKA) associated with
type 1 diabetes mellitus, congenital adrenal hyperplasia (CAH) and inborn errors of
metabolism (IEM). DKA is a cause that should not be overlooked as it can have life-
threatening effects if missed. Typically, a child in DKA may also present with abdominal
pain, changes in respiratory pattern, and confusion or lethargy.
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
Respiratory-related vomiting refers to post-tussive emesis, which is common in
children with asthma, foreign body aspiration or respiratory infections following
prolonged and forceful coughing episodes.
Intoxications such as accidental or intentional ingestions, as well as iron or lead
poisoning can also cause vomiting in children. Certain medications like
anticonvulsants, opiates and aspirin can also produce vomiting.
Less common categories of pediatric vomiting include psychogenic and behavioral
causes, which includes overfeeding in infants and bulimia nervosa in adolescents.
Pregnancy must also be considered in adolescents.
This concludes Part I of this podcast on pediatric vomiting. So far, we have reviewed
the pathophysiology and differential diagnosis, including both GI and non-GI causes.
Check out the supplemental materials to this podcast to view a chart displaying the
common causes of pediatric vomiting, grouped according to age of presentation.
Continue on to Part II to learn about the clinical approach to vomiting - including history
taking, physical exam and investigations, and to hear the conclusion to the case we
presented at the start of the podcast.
Thank you for listening!
Approach to Pediatric Vomiting (Part 2)
Welcome back everyone. This is the part II of the podcast on pediatric vomiting.
My name is Erin Boschee and I’m a medical student at the University of Alberta. This
podcast was reviewed by Dr. Melanie Lewis, a General Pediatrician and Associate
Professor at the University of Alberta and Stollery Children’s Hospital in Edmonton,
Alberta, Canada.
Now that we know about the common causes of vomiting specific to the neonatal and
pediatric population, let’s discuss a clinical approach to the assessment of a child with
vomiting.
History
A complete vomiting history will thoroughly investigate the history of presenting illness.
As with many standard complaints, the onset, frequency, time frame, provoking and
alleviating factors should be explored. The vomit should be characterized in detail
including the amount, color, and consistency.
First, it should be categorized as bilious or non-bilious. Bilious vomit has a greenish
appearance due to the presence of bile and is indicative of obstruction distal to the
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
ampulla of Vater, the opening of the common bile duct into the duodenum. Thus,
determining whether vomit is bilious or non-bilious helps to localize GI problems within
the GI tract.
Second, it should be categorized as bloody or non-bloody. Blood in the vomit
indicates inflammation or damage to the GI mucosa and may indicate need for
endoscopy to rule out acute upper GI bleed.
Third, the vomit should be identified as projectile or non-projectile, as projectile
vomiting may point to a specific diagnosis – namely, pyloric stenosis. True expulsive
vomiting should be distinguished from regurgitation, which is not associated with
retching or prodromal features like nausea, sweating and tachycardia.
Fourth, the age of presentation should be considered. The most common causes of
vomiting in the neonatal period include gastroenteritis, malrotation, pyloric stenosis, TEF
and necrotizing enterocolitis. In infancy, common causes are GERD, gastroenteritis,
bowel obstruction, milk protein allergy and UTI. In children, one must think of
gastroenteritis, UTI, DKA, post-tussive vomiting and increased intracranial pressure. In
adolescents, consider gastroenteritis, appendicitis, DKA and increased intracranial
pressure on the differential.
Fifth, one should determine whether the child is febrile or afebrile. The presence of
fever increases the likelihood of an infectious etiology.
One should also ask about the presence of any associated GI symptoms, including
nausea, abdominal pain, distension, diarrhea, and obstipation. Infectious symptoms
should be elicited, including fever, dysuria, ear pain, cough, coryza, shortness of breath
and meningismus. Other important associated symptoms to ask about are headache,
changes in vision, polyuria, polydipsia and weight loss, to rule out increased intracranial
pressure or DKA.
Red flag symptoms that you do not want to miss include meningismus, costovertebral
tenderness, abdominal pain and any evidence of increased intracranial pressure. Do
not miss a child who is vomiting due to a life-threatening condition such as meningitis,
DKA or pyelonephritis.
Finally, it is very important to elucidate the child’s hydration status, so one should
always ask about oral intake, urine output, tear production and weight changes.
Physical Exam
As with any physical exam, begin with an assessment of the patient’s vital signs and
ask yourself, is this child well or unwell? The initial management and investigations of a
stable versus unstable child can be quite different.
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
The physical exam should then begin with an assessment of hydration status. The
examiner should assess the fontanelles, skin turgor, mucous membranes, and look for
objective measures of stool and urine output.
A thorough abdominal exam should be performed looking for abdominal distension,
masses or visible peristalsis on inspection. Auscultation should be done to look for
hyperactive or absent bowel sounds. Palpation should assess for tenderness, though
this is difficult to assess in infants and younger children, and feel for masses or
organomegaly. In older children, special tests to assess for appendicitis or cholecystitis
can be performed.
A neurological exam should also be done to rule out signs of increased intracranial
pressure. This should include assessment for papilledema, bulging fontanelles and the
presence of focal neurological signs. A full neurological examination should be done
including the cranial nerves, focusing especially on cranial nerve VI, which is typically
the first affected to due its long intracranial course.
Examination for evidence of infection is also important and should include inspection
of the tympanic membranes and pharynx, auscultation of the chest and assessment for
meningismus.
Lastly, particularly in neonates and infants, the presence of dysmorphic features,
ambiguous genitalia or unusual odours should be noted as they may point to an
underlying congenital or metabolic cause.
Investigations
Investigations should be based on the history and age of the patient. For instance, a
three-month old with vomiting, fever and lethargy is at a high risk of sepsis, so this child
should receive a full septic work-up including blood cultures, urine cultures and a
lumbar puncture. An older child with a history clearly suggestive of gastroenteritis who
does not appear unwell will likely not require any investigations.
Standard investigations might begin with a CBC with differential, electrolytes, creatinine,
urea, glucose, liver function tests, and urinalysis with culture and sensitivities to rule out
systemic infectious or common endocrine causes. In the presence of bloody diarrhea or
history of recent travel, stools should be sent for culture and sensitivity.
Abdominal imaging can be very useful to identify the cause of GI-associated vomiting.
An abdominal flat plate can assess for bowel obstruction through the presence of air
fluid levels and bowel distension. A CT scan of the abdomen or upper GI series with
contrast can be used to further identify the location of the obstruction or anatomical
abnormality. Abdominal ultrasound is the modality of choice to assess for suspected
pyloric stenosis.
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
Gastroscopy should be performed in the presence of hematemesis to rule out upper GI
bleeding. A CT head should be ordered if the clinical history and physical exam is
suspicious for increased intracranial pressure.
Further investigations may be required based on the clinical history and presentation.
Treatment
Treatment of pediatric vomiting depends on correction of the underlying cause. The
treatment for specific etiologies of vomiting is beyond the scope of this podcast.
Symptomatic relief for gastroenteritis can be achieved through the use of anti-emetic
agents such as ondansetron (Zofran) in infants and children 6 months of age and older.
All children with vomiting should be assessed and treated for dehydration and
electrolyte disturbances. Mild dehydration can be treated with encouragement of oral
fluids, such as Pedialyte. Moderate to severe dehydration should be treated with IV
fluids.
Case Example – Resolution
Let’s think back to the case example presented at the start of the podcast. The patient
was a 3-week old male infant with a one-week history of recurrent vomiting associated
with feeds.
You ask the mother to describe the vomiting episodes in more detail and clarify that the
vomiting is non-bilious, non-bloody and projectile. He has become more lethargic over
the past three days and, at the same time, the mother noticed that she had only
changed his diaper once or twice per day.
You examine the baby and see that he is pale and severely dehydrated. You check the
CBC, electrolytes, Cr and BUN ordered in the ER, which shows a hypochloremic
hypokalemic metabolic alkalosis. You order the nurses to start an IV and begin infusing
IV fluids to re-hydrate and correct his electrolyte abnormalities.
You present a summary of your history and findings to your staff, stating that this is a 3-
week old infant with new-onset projectile, non-bilious vomiting. Together, you decide to
order an abdominal ultrasound, which confirms a hypertrophied pyloric muscle
consistent with pyloric stenosis. You consult Pediatric General Surgery for surgical
correction.
Summary
Here are a few key points about pediatric vomiting to take away from this podcast:
1) The history can be very helpful to differentiate the cause of vomiting. Use
descriptors such as bilious, projectile, and bloody to help rule out serious or
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
specific causes. Consider the age of the patient to narrow the differential
diagnosis. And always remember to rule out red flag symptoms like
meningismus, CVA tenderness and signs of increased intracranial pressure that
point to a life-threatening cause.
2) The differential diagnosis for vomiting is extremely broad and does not include
only GI causes. Don’t forget to consider non-GI causes like increased
intracranial pressure, pyelonephritis, drugs, and DKA.
3) Dehydration is one of the most common complications of vomiting in children.
Don’t forget to assess hydration status in your history and physical exam, and to
consider this as an important aspect of your treatment plan.
That concludes this series of podcasts. Hopefully now you feel comfortable forming a
broad differential diagnosis and a basic approach to a child who is vomiting.
I want to thank Dr. Melanie Lewis for editing the podcasts and thank you for listening!
References
[1] Di Lorenzo, C. Approach to the infant or child with nausea and vomiting. From
UpToDate 2013. Accessed online 28 Aug 2013.
[2] Walsh, C.A., Simpson, E.A., Zachos, M. Chapter 17. Gastroenterology and
Hepatology. In The Hospital for Sick Children Handbook of Pediatrics, 11th Edition.
2009. Toronto, ON: Elsevier Canada.
[3] Kahan, S., Teitelbaum, J.E., DeAntonis, K.O. In A Page Pediatrics, 2nd Edition.
2008. Baltimore, MD: Lippincott Williams & Wilkins.
[4] Oermann, C.M. Congenital anomalies of intrathoracic airways and
tracheoesophageal fistula. From UpToDate 2013. Accessed online 4 Oct 2013.
[5] Schanler, R.J. Clinical features and diagnosis of necrotizing enterocolitis in
newborns. From UpToDate 2013. Accessed online 4 Oct 2013.
[6] Winter, H.S. Gastroesophageal reflux in infants. From UpToDate 2013. Accessed
online 4 Oct 2013.
[7] Ferry, G.D. Causes of acute abdominal pain in children and adolescents. From
UpToDate 2013. Accessed online 4 Oct 2013.
[8] Kitagawa, S., Miqdady, M. Intussusception in children. From UpToDate 2013.
Accessed online 4 Oct 2013.
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
Supplemental Information
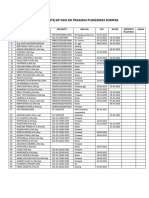
Table 1: Common causes of pediatric vomiting by age of presentation.
Neonatal Newborn Infant Child Adolescent
(0-2 days) (3 days-1 month) (1-36 months) (36 months-12 (12-18 years)
years)
-Duodenal atresia -Gastroenteritis -Gastroenteritis -Gastroenteritis -Gastroenteritis
-TEF (types A/C) -Pyloric stenosis -UTI, -UTI -Appendicitis
-Malrotation +/- pyelonephritis -DKA -DKA
volvulus -GER -Increased -Increased
-TEF (types B/D/H) -GERD intracranial intracranial
-Necrotizing -Ingestion pressure pressure
enterocolitis -Intussusception -Eosinophilic -Eosinophilic
-Milk protein -Milk protein esophagitis esophagitis
intolerance intolerance -Appendicitis -Bulimia nervosa
-CAH -Ingestion -Pregnancy
-IEM -Post-tussive -Post-tussive
vomiting vomiting
Reference: Di Lorenzo, C. Approach to the infant or child with nausea and vomiting.
From UpToDate 2013. Accessed online 28 Aug 2013.
Abbreviations:
TEF = tracheo-esophageal fistula
CAH = congenital adrenal hyperplasia
IEM = inborn errors of metabolism
UTI = urinary tract infection
GER = gastro-esophageal reflux
GERD = gastro-esophageal reflux disease
DKA = diabetic ketoacidosis
Developed by Erin Boschee and Dr. Melanie Lewis for PedsCases.com.
August 25, 2014
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Cerebral Palsy: Classification and Etiology: Beyin Felci: Sını Ama Ve EtyolojiDocument4 pagesCerebral Palsy: Classification and Etiology: Beyin Felci: Sını Ama Ve EtyolojiRe-zha 'Putra'No ratings yet
- Febrile Seizure: DefinitionDocument5 pagesFebrile Seizure: DefinitionRe-zha 'Putra'No ratings yet
- Ramseysedationscale PDFDocument1 pageRamseysedationscale PDFRe-zha 'Putra'No ratings yet
- Salad: Soup: Main Course: Dessert: Drink:: Avocado, Mango, and Shrimp SaladDocument1 pageSalad: Soup: Main Course: Dessert: Drink:: Avocado, Mango, and Shrimp SaladRe-zha 'Putra'No ratings yet
- Form KoassDocument32 pagesForm KoassRe-zha 'Putra'No ratings yet
- CT of Central Nervous System Infections in Immunocompromised PatientsDocument5 pagesCT of Central Nervous System Infections in Immunocompromised PatientsRe-zha 'Putra'No ratings yet
- Diabetic Retinopathy 2013 ArticleDocument3 pagesDiabetic Retinopathy 2013 ArticleRe-zha 'Putra'No ratings yet
- American College of Obstetricians and Gynecologists American Society For Reproductive Medicine Diakses Pada 27-3-2016Document1 pageAmerican College of Obstetricians and Gynecologists American Society For Reproductive Medicine Diakses Pada 27-3-2016Re-zha 'Putra'No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hazard Analysis & Critical Control Point: Prepared By: Eng / Walid I. GahferDocument38 pagesHazard Analysis & Critical Control Point: Prepared By: Eng / Walid I. GahferWalid Gahfer100% (5)
- Coles Medical 2011 - GeorgeDocument272 pagesColes Medical 2011 - GeorgeWong SterlingNo ratings yet
- Chapter IVDocument16 pagesChapter IVRoyceNo ratings yet
- Solicitation Restroom MaintenanceDocument10 pagesSolicitation Restroom MaintenanceDarnel CayogNo ratings yet
- Chemicals of High Concern List (Sorted Alphabetically)Document125 pagesChemicals of High Concern List (Sorted Alphabetically)Marcos ROSSINo ratings yet
- Lab Emergency ProcedureDocument16 pagesLab Emergency ProcedureFre HanyaqNo ratings yet
- Manufacturing Drills 2Document9 pagesManufacturing Drills 2Thirdy AcostaNo ratings yet
- Kings Turon ICT Timbal Edited2Document12 pagesKings Turon ICT Timbal Edited2Precious Abrylle Remperas Timbal100% (1)
- Chemistry & SAR of QuinazolinoneDocument6 pagesChemistry & SAR of Quinazolinonebooksa2zNo ratings yet
- Epidemiological Cutoff Values For Antifungal Susceptibility TestingDocument36 pagesEpidemiological Cutoff Values For Antifungal Susceptibility Testingdadrrui100% (1)
- Case Scenario (Pedia)Document2 pagesCase Scenario (Pedia)Hamima Azis PandapatanNo ratings yet
- Drug AdiictionDocument17 pagesDrug AdiictionRahul PatelNo ratings yet
- Alexander Technique EssayDocument2 pagesAlexander Technique EssayMathematicus MathematicaNo ratings yet
- Physiotherapy For Primary Frozen Shoulder in Secondary Care Hanchard 2019Document11 pagesPhysiotherapy For Primary Frozen Shoulder in Secondary Care Hanchard 2019patinoomar67No ratings yet
- CRC Official TextDocument28 pagesCRC Official TextDavid HundeyinNo ratings yet
- Semi-Solid Applications 101Document1 pageSemi-Solid Applications 101CHARLES RONALD GENATONo ratings yet
- Daftar Ceklis STR, Sip Dan Sik Pegawai Puskesmas SompakDocument1 pageDaftar Ceklis STR, Sip Dan Sik Pegawai Puskesmas SompakAkwila PaudyaNo ratings yet
- Pharmaceutical Biotechnology Question BankDocument3 pagesPharmaceutical Biotechnology Question BankNoorul AlamNo ratings yet
- Siddha InstituteDocument10 pagesSiddha InstituteBala GanapathyNo ratings yet
- Body Fluids BloodDocument31 pagesBody Fluids BloodHardy Allen L. VillarosaNo ratings yet
- Home Care in ElderlyDocument18 pagesHome Care in ElderlyshodhgangaNo ratings yet
- MASTER COPY - Favorito - Magtibay CHAPTER I VDocument95 pagesMASTER COPY - Favorito - Magtibay CHAPTER I VJohn Felix AndalNo ratings yet
- Noorani 2014Document3 pagesNoorani 2014MD Luthfy LubisNo ratings yet
- Gad Plan 2022-2023Document6 pagesGad Plan 2022-2023Melvin AlmeriaNo ratings yet
- (PersonalityCentral) ENFJ CareerReportDocument12 pages(PersonalityCentral) ENFJ CareerReportWidasari WidaNo ratings yet
- Employee Welfare at TcsDocument61 pagesEmployee Welfare at TcsSMILESTONE DIGITALSNo ratings yet
- How Doppelgänger Brand Images Influence The Market Creation Process: Longitudinal Insights From The Rise of Botox CosmeticDocument14 pagesHow Doppelgänger Brand Images Influence The Market Creation Process: Longitudinal Insights From The Rise of Botox Cosmeticmgiesler5229100% (1)
- Week 16Document6 pagesWeek 16Sal MiahNo ratings yet
- SedulousDocument2 pagesSedulousZoe RodriguezNo ratings yet
- Materi Policy Analysis TriangleDocument6 pagesMateri Policy Analysis TriangleRegina Marsha100% (1)