Professional Documents
Culture Documents
Glanzmann Thrombasthenia
Glanzmann Thrombasthenia
Uploaded by
SaumilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Glanzmann Thrombasthenia
Glanzmann Thrombasthenia
Uploaded by
SaumilCopyright:
Available Formats
GLANZMANN THROMBASTHENIA
AR disorder characterized by defective invitro platelet aggregation and life long
bleeding tendency due to qualitative or quantitative abnormality of platelet
glycoprotein GPIIb/IIIa receptor also known as intigrin alpha IIB3.
ETIOLOGY
Biochemical basis is defect in glycoprotein GPIIb/IIIa.Itbis a calcium dependent
heterodimer that preferentially binds to fibrinogen or vWF, but also to fibronectin
or vitronectin.
Incidence is 1 in 1 million .
Genes for both GPIIb/IIIa are located on long arm of chromosome 17.Defect in any of
these genes will cause decreased synthesis of subunit and decrease fibrinogen
receptor and defective binding of fibrinogen after platelet activation.So platelet
aggregation is defective or completely absent.
There are around 100 different mutations that can lead to this disease.
Isoantibodies specific for deleted
GPIIb/IIIa have been demonstrated in blood of multiple transfused patients,which can
produce thrombesthania defect in normal transfused patient.
CLINICAL FEATURES :-
Commonly associated with consanguinous marriages,
Hemorrhagic manifestations are seen in patient homozygous for GT mutation,
heterozygous condition is mostly asymptomatic.
Sites of bleeding:-
Purpura ,epistaxis, gingival bleeding menorrhagia
.
GI bleeding and menorrhagia is less common.
Epistaxis is a common cause of severe bleeding and is typically seen in childhood.
Bleeding tendency decrease with age
.
Post traumatic and postoperative hemorrhage can be serious and pregnancy and delivery
cause serious hemorrhagic risk.
Prognosis usually good with careful supportive care.
Deaths due to bleeding is rare unless associated with trauma, other disease and
chronic isoimmunization.
LAB FINDINGS :-
Prolonged bleeding time.
Deficient clot retraction.
Deficient platelet aggregation with ADP, collagen,epinephrine and thrombin.
Normal Ristocetin induced aggregation and coagulation
Platelet counts are almost normal and they are normal in morphology
TREATMENT:-
Localised bleeding can be treated by Limited measures like fibrin sealants or topical
thrombin and antifibrinolytic Agents.
Epistaxis and gingival bleed:-
nasal packing for application of gel foam soaked in topical thrombin.
Regular proper Dental Care to decrease risk of gingival bleed.
Severe menorrhagia is common and can be treated with high dose of progesterone
followed by maintenance treatment of birth control pills.
Iron deficiency anaemia can develop insidiously with gingival oozing or minor
menorrhagia.
A significant number of transfused patients develop HLA specific alloantibodies or GP
IIb/IIIa specific autoantibodies which complicate transfusion therapy and limit
future treatment.
These isoantibodies can block normal transfused platelet aggregation and lead to
Rapid removal by immune mechanisms.
Pregnancy and delivery pose a serious hemorrhagic risk.
Multiple platelet transfusion are required before and after delivery.
An alternative approach for patients who are refractory to platelet transfusion, is
use of rf VIIa.
It enhances the deposition of AlphaIIb beta 3 deficient platelets on subendothelial
matrix through an interaction with fibrin formed by increased trombin generation
leading to clot stability.
For patient with severe recurrent bleeding episodes,allogenic Bone Marrow
transplantation may be done.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Ats Waveform Slideshow v5MACDocument72 pagesAts Waveform Slideshow v5MACSaumil100% (1)
- Hematology Review NotesDocument28 pagesHematology Review NoteszachNo ratings yet
- bdqfi_folio4986501Document1 pagebdqfi_folio4986501SaumilNo ratings yet
- Ab Pmjay DataDocument19 pagesAb Pmjay DataSaumilNo ratings yet
- 01 Keshvam Skyview 56488Document12 pages01 Keshvam Skyview 56488SaumilNo ratings yet
- 73685500008Document52 pages73685500008SaumilNo ratings yet
- CMTC Guj EngDocument43 pagesCMTC Guj EngSaumilNo ratings yet
- Playstation®5 Safety Guide: Cfi-1008A 7033919Document13 pagesPlaystation®5 Safety Guide: Cfi-1008A 7033919SaumilNo ratings yet
- How To Read Pediatric Ecgs: ReferencesDocument1 pageHow To Read Pediatric Ecgs: ReferencesSaumilNo ratings yet
- Gujarat University Exam: M.S. April - 2020Document6 pagesGujarat University Exam: M.S. April - 2020SaumilNo ratings yet
- Adv Post Special Doctoe New18 PDFDocument10 pagesAdv Post Special Doctoe New18 PDFSaumilNo ratings yet
- Accredited by NAAC With A' GradeDocument9 pagesAccredited by NAAC With A' GradeSaumilNo ratings yet
- 293 PDFDocument1 page293 PDFSaumilNo ratings yet
- 692 693 PDFDocument2 pages692 693 PDFSaumilNo ratings yet
- 36 Sub District Hospitals List 18 PDFDocument1 page36 Sub District Hospitals List 18 PDFSaumilNo ratings yet
- Ijgdbp Vol 3 No 2Document28 pagesIjgdbp Vol 3 No 2SaumilNo ratings yet
- 22 District Hospital List PDFDocument2 pages22 District Hospital List PDFSaumilNo ratings yet
- MD Paediatrics - Plan of Thesis (Year 2016)Document4 pagesMD Paediatrics - Plan of Thesis (Year 2016)SaumilNo ratings yet
- Secondary Hemostasis Lab TestsDocument2 pagesSecondary Hemostasis Lab TestsWho KnowsNo ratings yet
- Libro - Biological Effects of Magnetic and Electromagnetic Fields (The Language of Science)Document243 pagesLibro - Biological Effects of Magnetic and Electromagnetic Fields (The Language of Science)Faiber Soto VargasNo ratings yet
- Effects of Exercise On Laboratory Test ResultsDocument7 pagesEffects of Exercise On Laboratory Test ResultsWade Jackson100% (1)
- UpToDate Massive Blood TransfusionDocument10 pagesUpToDate Massive Blood TransfusionAlice HuiiNo ratings yet
- Thrombin-Activatable Fibrinolysis Inhibitor AKA Procarboxypeptidase UDocument41 pagesThrombin-Activatable Fibrinolysis Inhibitor AKA Procarboxypeptidase UALBERTOLPZNo ratings yet
- Edible By-Products of Meat: VeterinariaDocument4 pagesEdible By-Products of Meat: VeterinariaAristoteles Esteban Cine VelazquezNo ratings yet
- Lab Act Introduction Hemostasis Bleeding Time Tourniquet Test Week 4Document23 pagesLab Act Introduction Hemostasis Bleeding Time Tourniquet Test Week 4Arief AbidinNo ratings yet
- D Dimer Preanalytical Analytical Postanalytical Variables and Clinical ApplicationsDocument31 pagesD Dimer Preanalytical Analytical Postanalytical Variables and Clinical ApplicationsfaizmundzirNo ratings yet
- Nursing Care Plan - Risk For BleedingDocument2 pagesNursing Care Plan - Risk For BleedingDaniel Andre S. SomorayNo ratings yet
- Nursing 2020 1.3 Plasma ProteinsDocument20 pagesNursing 2020 1.3 Plasma ProteinsYogesh NerkarNo ratings yet
- Inflammation in Atrial Fibrillation: Yutao Guo, MDR, Gregory Y. H. Lip, MD, Stavros Apostolakis, MD, P DDocument8 pagesInflammation in Atrial Fibrillation: Yutao Guo, MDR, Gregory Y. H. Lip, MD, Stavros Apostolakis, MD, P DIbrahim HaidarNo ratings yet
- HemostasaDocument4 pagesHemostasaDiynieffNo ratings yet
- 4 EpistaxisDocument51 pages4 EpistaxisNicNo ratings yet
- Mathematical Calculations Involving Blood Components Usage in Transfusion MedicineDocument8 pagesMathematical Calculations Involving Blood Components Usage in Transfusion MedicineNatalie CuNo ratings yet
- 015 Pathology MCQ ACEM Primary General Pathology PDFDocument15 pages015 Pathology MCQ ACEM Primary General Pathology PDFTahseen Jani100% (1)
- Coag Made EasyDocument15 pagesCoag Made Easygus_lionsNo ratings yet
- Evaluation Tests For Secondary Hemostasis (Lab Analysis) HematologyDocument5 pagesEvaluation Tests For Secondary Hemostasis (Lab Analysis) HematologyAudreySlitNo ratings yet
- Edexcel A Level Biology Key TermsDocument2 pagesEdexcel A Level Biology Key TermsShifa RahmanNo ratings yet
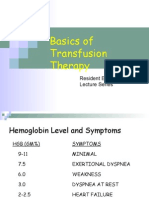
- Basics of Transfusion TherapyDocument43 pagesBasics of Transfusion TherapyMuhammad Afyudin DjumhuriNo ratings yet
- Grand Rounds Fall 2012 Saint Louis University School of MedicineDocument13 pagesGrand Rounds Fall 2012 Saint Louis University School of MedicineSlusom WebNo ratings yet
- Opm M2 V117UV EN Rev11Document58 pagesOpm M2 V117UV EN Rev11Jose Rolando Orellana Rodriguez0% (1)
- Mixing Studies 1pp 08-13-15.pptx 0 PDFDocument49 pagesMixing Studies 1pp 08-13-15.pptx 0 PDFKholifah LintangNo ratings yet
- Hemostatic Disorder in ChildrenDocument4 pagesHemostatic Disorder in ChildrenodiliajessicanpviaNo ratings yet
- Report of Measurement of Plasma Total ProteinDocument11 pagesReport of Measurement of Plasma Total ProteinDoreen AmulenNo ratings yet
- Coagulador Be HNK ElectronikDocument22 pagesCoagulador Be HNK ElectronikHugo GranadosNo ratings yet
- HematologyDocument58 pagesHematologyAchmad DainuriNo ratings yet
- 0610 BIOLOGY: MARK SCHEME For The October/November 2011 Question Paper For The Guidance of TeachersDocument10 pages0610 BIOLOGY: MARK SCHEME For The October/November 2011 Question Paper For The Guidance of TeachershiNo ratings yet
- Fibrinogen 506 EngDocument6 pagesFibrinogen 506 Engالواثقة باللهNo ratings yet