Professional Documents
Culture Documents
12 PDF
Uploaded by
SvetlanaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
12 PDF
Uploaded by
SvetlanaCopyright:
Available Formats
British Journal of Dermatology 2003; 149: 94–98.
Dermatological Surgery and Lasers
Red ink tattoo reactions: successful treatment
with the Q-switched 532 nm Nd:YAG laser
F.C.ANTONY AND C.C.HARLAND
Department of Dermatology, St Helier Hospital, Carshalton, Surrey, SM5 1AA, U.K.
Accepted for publication 17 November 2002
Summary Background In the South-west Thames region there were an unprecedented number of lichenoid
tattoo reactions to red ink in patients who had visited a local tattoo parlour. The red ink was found
to contain mercuric sulphide, a compound known to cause allergic reactions. Topical DermovateÒ
(clobetasol propionate 0Æ05%, GlaxoWellcome) ointment alone had little impact.
Objectives To investigate whether the Q-switched 532 nm Nd:YAG laser could produce permanent
flattening of the reaction.
Methods This was an open nonrandomized clinical trial. Biopsies were taken from the lichenoid
areas within the tattoos. Subjects were patch tested to 1% ammoniated mercury in petrolatum prior
to treatment with the Q-switched 532 nm Nd:YAG laser. Laser treatments were delivered at
6-weekly intervals by a single operator. Patients also applied topical DermovateÒ between
treatments. Therapy was discontinued when the lesions flattened. Clinical photographs were
assessed at baseline and prior to each laser treatment.
Results Seven patients with Fitzpatrick skin types I–III were enrolled in the study (four females,
three males, mean age 39 years). All patients completed the trial. Patch testing to mercury was
universally negative at 48 and 96 h. Substantial flattening and depigmentation of the red ink
within the tattoos was noted after six laser treatments. No adverse effects were recorded.
Conclusions The Q-switched 532 nm Nd:YAG laser in combination with topical DermovateÒ
ointment is a safe and effective method of treating red ink tattoo reactions.
Key words: 532 nm Nd:YAG laser, red ink tattoo reaction
Tattoos occasionally have unfortunate consequences. The reactions were unresponsive to topical
The introduction of a foreign substance into the skin DermovateÒ ointment (clobetasol propionate 0Æ05%,
can promote a toxic or an immunological response. GlaxoWellcome Stevenage, UK) under occlusion. There
This reaction is more common with red ink, which may have been two previous cases reporting the success of
contain mercury-related compounds. We had an influx the Q-switched 532 nm Nd:YAG laser in a red tattoo
of patients with red ink tattoo reactions to the reaction so we wished to establish the benefit of this
Department of Dermatology, St Helier Hospital over laser in our group of patients.2,3
the course of 6 months. Most of these patients had
visited the same tattoo parlour. The batch of red ink
was later found to contain cinnabar (mercuric sul- Methods
phide). Laser intervention for red tattoo reactions has
Patients
been hitherto considered to be unsafe because of the
theoretical risk of anaphylaxis.1 All patients were referred by their general practitioners
and presented similarly with pruritus, swelling and
discomfort in the red portion of their tattoos. The
Correspondence: Dr F.C.Antony. symptoms had all developed 2 days after having the
E-mail: fiantony@hotmail.com tattoo performed and were unresponsive to topical
94 Ó 2003 British Association of Dermatologists
RED INK TATTOO REACTIONS 95
DermovateÒ ointment under occlusion for 2 months. and of the remote possibility of a type I hypersensitivity
Patients had Fitzpatrick skin types I–III. Examination reaction.
revealed erythema, swelling and induration of the red
areas of the tattoos; other colours were unaffected.
Results
There was no evidence of peripheral lymphadenopathy.
Biopsies were taken for histology from the indurated Seven patients were enrolled in the study (four females,
areas. three males, mean age 39 years). All patients comple-
ted the study.
Table 1 illustrates the demographic details of the
Chest X-ray and patch tests
patients, histology and laser treatments required. The
A chest X-ray was performed to rule out bilateral chest X-ray in all the patients was normal. Patch testing
inguinal lymphadenopathy suggestive of concomitant to mercury was universally negative at 48 and 96 h.
sarcoidosis. Patch testing to 1% ammoniated mercury On average, substantial flattening and depigmenta-
in petrolatum only was performed at 48 and 96 h tion of the red tattoo reactions was noted after six laser
using standardized techniques. A full supply of all the treatments (Fig. 1a,b). However, hypertrophic, licheni-
pigments within the red dye was unavailable. fied reactions on the lower leg were much slower to
respond, requiring eight laser treatments (Fig. 2a,b).
Laser therapy
Safety and tolerability
We employed the Q-switched 532 nm Nd:YAG laser
(Medlite, Continuum Biomedical, Santa Clara, CA, Initial erythema after the laser treatment lasted for 1 day
U.S.A.), 2–3 mm beam diameter, pulse width and was followed by superficial erosion and crust forma-
) 20 ns, at increasing fluences of 1Æ4–6Æ4 J cm)2 tion of the area, which took approximately 1 week to heal
following an initial test area. Laser treatments were with the application of aloe vera gel. No other adverse
carried out at 6-weekly intervals by the same events were recorded. In particular, no lymphadenopathy
operator. Patients were instructed to use topical was noted. Patients reported relief of pruritus on comple-
DermovateÒ ointment in between visits. Treatment tion of the treatment. One patient required topical EmlaÒ
was confined to the affected areas, aiming to produce (AstraZeneca, Luton, UK) cream (lignocaine 25 mg g)1,
a temporary whitening of the epidermis. Laser prilocaine 25 mg g)1) prior to laser treatment.
therapy was discontinued after flattening of the
lesion occurred. Examination for lymphadenopathy
Histology
was done at each visit. Clinical photographs were
assessed at baseline and prior to each laser interven- The most common histological pattern noted was a
tion. lichenoid reaction. Figure 3 illustrates the histological
reaction patterns seen.
Consent
Follow-up
Written, informed consent was obtained from all the
patients warning of depigmentation, scarring, the rare At 6 months all affected areas remained flat. One
development of black pigmentation within the red area patient with a hypertrophic lichenoid reaction on the
Table 1. Demographic details of the patients, histology and laser treatments required
Age Tattoo Mean Mean no. of No. of laser
Sex (years) location Histology fluence (J cm)2) shots per laser treatment treatments to flatten the lesion
M 36 Leg Nodular inflammatory infiltrate 5Æ3 1018 7
M 50 Leg Lichenoid inflammatory infiltrate 5Æ3 1763 8
F 31 Back Lichenoid inflammatory infiltrate 5Æ4 2103 6
M 45 Arm Lichenoid inflammatory infiltrate 4Æ2 1846 7
F 39 Back Granulomatous inflammatory infiltrate 3Æ3 1491 7
M 51 Arm Lichenoid inflammatory infiltrate 4Æ6 1634 6
F 35 Back Nodular inflammatory infiltrate 5Æ2 1966 6
Ó 2003 British Association of Dermatologists, British Journal of Dermatology, 149, 94–98
96 F.C.ANTONY AND C.C.HARLAND
Figure 1. (a) Red tattoo reaction on the back before treatment. (b)
Red tattoo reaction on the back after six laser treatments showing
depigmentation and flattening.
Figure 2. (a) Red tattoo reaction on the lower leg before treatment.
(b) Red tattoo reaction after eight laser treatments.
lower leg had residual erythema in the area treated but
the remaining pigment was insufficient to excite a
recrudescence of the lichenoid reaction. Pruritus was legislation governing the production of tattoo dyes
eliminated in all cases. and thus it is often not known which substances are
used to produce them.6
Of note, all our patients were negative on patch
Discussion
testing to mercury suggesting that other pigments
Allergic reactions can occur to any tattoo pigment within the red dye may evoke the lichenoid reaction.
but lichenoid reactions to red tattoo dye are the most However, negative patch testing does not rule out
common.4 In the 1960s patch testing revealed mercury as a cause because the hypersensitivity
sensitivity to mercury and this compound was initially created by the tattoo was provoked by intra-
replaced by alternative red dyes such as cadmium cutaneous rather than epicutaneous challenge.
red, sienna and organic substances such as sandal- Various histological tattoo reaction patterns are
wood and brazilwood.5 However, despite the availab- recognized. The chronic inflammatory cell infiltrate
ility of these mercury-free alternatives, reactions to may be nodular with a well-defined Grenz zone,7 liche-
red tattoo dye are still occurring as evidenced by our noid with attenuation of the basal layer of the epider-
cluster of cases. The problem lies in the lack of mis8 or granulomatous.9 A pseudolymphomatous
Ó 2003 British Association of Dermatologists, British Journal of Dermatology, 149, 94–98
RED INK TATTOO REACTIONS 97
pattern has also been reported where the infiltrate is so
dense that it may be indistinguishable from lymphoma
and immunohistochemistry may be necessary to con-
firm the diagnosis.10 It is always advisable to request a
chest X-ray and biopsy of a patient with a red tattoo
reaction as sarcoidosis may present as a granuloma-
tous reaction confined to a red tattoo.11
Three types of laser are currently used for tattoo
removal: the Q-switched ruby laser (694 nm), the
Q-switched Nd:YAG laser (532 nm, 1064 nm) and
the Q-switched alexandrite laser (755 nm).12 The
Q-switched ruby and alexandrite lasers are useful for
removing black, blue and green pigments. The
Q-switched 532 nm Nd:YAG laser can be used to
remove red pigments and the 1064 nm Nd:YAG laser is
used for removal of black and blue pigments. The
carbon dioxide laser has also been reported to be
beneficial for red ink tattoo removal. However, this
laser may also be associated with a significant degree of
scarring and local anaesthesia prior to laser therapy is
required.13 Other treatment options include surgical
excision, dermabrasion and intralesional triamcino-
lone. Our patients were keen to preserve the rest of
their tattoo so we used the Nd:YAG laser to produce
depigmentation and flattening of the reaction without
producing scarring.
No adverse type I hypersensitivity events were
recorded at any stage of the treatment period. However,
there has been widespread concern of anaphylactoid
reactions following a report by Ashinoff et al. who
described two cases of a generalized urticarial rash
7 days after using the Q-switched ruby laser for the
treatment of red tattoo reactions.1 They hypothesized
that the laser targeted the intracellular tattoo pigment
causing it to fragment and become extracellular. This
extracellular pigment was recognized by the patient’s
immune system as foreign and then initiated a local
and a generalized allergic reaction. In our experience of
over 500 episodes of treatment with the Nd:YAG laser
for tattoo removal no such reactions have occurred.
One possibility is that the Nd:YAG laser causes
fragmentation of the pigment which is then eliminated
in a transepidermal fashion. In addition there has been
a report of a tattoo producing localized lymphadenop-
athy.14 The lymph node in that case was found to
Figure 3. (a) A nodular inflammatory infiltrate with extracellular
contain pigment material characteristic of a tattoo. All
pigment. (b) A lichenoid inflammatory infiltrate with extracellular our patients were examined for lymphadenopathy prior
pigment. (c) A granulomatous inflammatory infiltrate with extracel- to each laser treatment and no evidence of reactive
lular pigment. lymphadenopathy was found.
In conclusion, we have reported the safe and effective
use of the Q-switched 532 nm Nd:YAG laser in
Ó 2003 British Association of Dermatologists, British Journal of Dermatology, 149, 94–98
98 F.C.ANTONY AND C.C.HARLAND
combination with topical DermovateÒ in treating red 6 Lehmann G, Pierchalla P. Tattooing dyes. Derma Beruf Umwelt
tattoo reactions. However, further legislation is re- 1988; 36: 152–6.
7 Slater DN, Durrant TE. Tattoos: light and transmission electron
quired to govern the use of pigments in dyes to prevent microscopy studies with X-ray microanalysis. Clin Exp Dermatol
a resurgence of these red tattoo reactions and we would 1984; 9: 167–73.
suggest that classic dyes such as cinnabar are com- 8 Clarke J, Black MM. Lichenoid tattoo reactions. Br J Dermatol
pletely replaced by synthetic dyes. 1979; 100: 451–4.
9 Goldstein AP. Histological reactions in tattoos. J Dermatol Surg
Oncol 1979; 5: 896–900.
10 Amann U, Luger TA, Metze D. Lichenoid pseudolymphomatous
References tattooing reaction. Hautarzt 1997; 48: 410–13.
1 Ashinoff R, Levine VJ, Soter NA. Allergic reactions to tattoo 11 Sowden JM, Cartwright PH, Smith AG et al. Sarcoidosis presenting
pigment after laser treatment. Dermatol Surg 1995; 21: 291–4. with a granulomatous reaction confined to red tattoos. Clin Exp
2 Hindson C, Foulds I, Cotterill J. Laser therapy of lichenoid red Dermatol 1992; 17: 446–8.
tattoo reaction. Br J Dermatol 1995; 133: 665–6. 12 Kuperman-Beade M, Levine VJ, Ashinoff R. Laser removal of
3 Dave R, Mahaffey P. Successful treatment of an allergic reaction tattoos. Am J Clin Dermatol 2001; 2: 21–5.
in a red tattoo with the Nd:YAG laser. Br J Plast Surg 2002; 55: 13 Kyanko ME, Pontasch MJ, Brodell RT. Red tattoo reactions:
456. treatment with the carbon dioxide laser. J Dermatol Surg Oncol
4 Taaffe A, Knight A, Marks R. Lichenoid tattoo hypersensitivity. 1989; 15: 652–6.
Br Med J 1978; i: 616–18. 14 Zirkin HJ, Avinoach I, Edelwitz P. A tattoo and localised lymph-
5 Sowden JM, Byrne JPH, Smith AG et al. Red tattoo reactions: adenopathy: a case report. Cutis 2001; 67: 471–2.
X-ray microanalysis and patch-test studies. Br J Dermatol 1991;
124: 576–80.
Ó 2003 British Association of Dermatologists, British Journal of Dermatology, 149, 94–98
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 1 Bible Changes 41 Translations Compared 3 12 2012 8inchDocument16 pages1 Bible Changes 41 Translations Compared 3 12 2012 8inchapi-209701690No ratings yet
- The Outsiders Study GuideDocument24 pagesThe Outsiders Study GuideSal TellezNo ratings yet
- Pte Academic Practice Tests Plus2Document18 pagesPte Academic Practice Tests Plus2Majin BalaNo ratings yet
- A To Z Orthodontics Vol 8 CephalometryDocument17 pagesA To Z Orthodontics Vol 8 CephalometryYury Tenorio Cahuana50% (2)
- FRM-012 A D4 Change NoteDocument4 pagesFRM-012 A D4 Change NoteSvetlanaNo ratings yet
- PALE Casals v. CusiDocument2 pagesPALE Casals v. CusiCharm Pedrozo100% (1)
- Espano v. CA, 288 Scra 588Document9 pagesEspano v. CA, 288 Scra 588Christia Sandee SuanNo ratings yet
- 2017 Novel Method For Facial RejuvenationDocument6 pages2017 Novel Method For Facial RejuvenationSvetlanaNo ratings yet
- 2016 Lasers in Surgery and MedicineDocument6 pages2016 Lasers in Surgery and MedicineSvetlanaNo ratings yet
- 2018 Lasers in Surgery and MedicineDocument9 pages2018 Lasers in Surgery and MedicineSvetlanaNo ratings yet
- Women, Leadership, and Empowerment: UniversityDocument14 pagesWomen, Leadership, and Empowerment: Universityedo Tegar SugiartoNo ratings yet
- ITL Mod 4Document22 pagesITL Mod 4Nicole CruzNo ratings yet
- Agus SubiyantoDocument3 pagesAgus Subiyantogufronf18No ratings yet
- Scene 6Document4 pagesScene 6Yuanlong LiNo ratings yet
- Ihtm Rohtak Syllabus BHMDocument60 pagesIhtm Rohtak Syllabus BHMManish PooniaNo ratings yet
- HSER4380 Final Study GuideDocument13 pagesHSER4380 Final Study GuideBrandie SandersNo ratings yet
- SCCA2103 Leadership CommunicationDocument16 pagesSCCA2103 Leadership CommunicationsarahNo ratings yet
- A Snake and The MirrorDocument65 pagesA Snake and The Mirroralone smoothNo ratings yet
- List Two (2) Areas of Legislative and Regulatory Context of An Organisation and Briefly Describe What They InvolveDocument19 pagesList Two (2) Areas of Legislative and Regulatory Context of An Organisation and Briefly Describe What They InvolveTanveer MasudNo ratings yet
- Conexión HT-PAC Drill PipeDocument3 pagesConexión HT-PAC Drill PipeAnibal Perdomo SaldañaNo ratings yet
- 5 L1 Aspen TutorialDocument28 pages5 L1 Aspen TutorialariefNo ratings yet
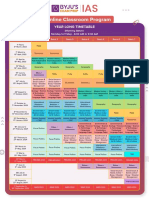
- BHLP Year Long Plan Required English Medium 2023 24 Batch Final 991676721629413Document3 pagesBHLP Year Long Plan Required English Medium 2023 24 Batch Final 991676721629413A V GamingNo ratings yet
- CH4 Recommended Problems PDFDocument3 pagesCH4 Recommended Problems PDFnomio12No ratings yet
- Nanorobotii in Aplicatii MedicaleDocument9 pagesNanorobotii in Aplicatii MedicaleLaura CursaruNo ratings yet
- Evolution of Routing TechniquesDocument69 pagesEvolution of Routing Techniquestusarkar85No ratings yet
- Factors Influencing LearningDocument12 pagesFactors Influencing Learningrosmery15No ratings yet
- AcdDocument482 pagesAcdAnu PreethyNo ratings yet
- Detailed Instructional Plan 2Document99 pagesDetailed Instructional Plan 2Sol JerNo ratings yet
- Pidato Menyantuni Anak YatimDocument2 pagesPidato Menyantuni Anak YatimsagwaNo ratings yet
- Mandatory ROTCDocument7 pagesMandatory ROTCphoebe lagueNo ratings yet
- Fixed Capital Working CapitalDocument26 pagesFixed Capital Working CapitalShweta TrivediNo ratings yet
- Ecosystem Structure and Processes: Environmental ManagementDocument4 pagesEcosystem Structure and Processes: Environmental ManagementAzalia Delgado VeraNo ratings yet
- Mariano vs. CallejasDocument3 pagesMariano vs. CallejasJoy Carmen CastilloNo ratings yet
- Chapter 3Document62 pagesChapter 3Amira FawzyNo ratings yet