Professional Documents
Culture Documents
Ajcpath117 0259 PDF
Ajcpath117 0259 PDF
Uploaded by
Caecilia CindyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ajcpath117 0259 PDF
Ajcpath117 0259 PDF
Uploaded by
Caecilia CindyCopyright:
Available Formats
Hematopathology / EBER AND LMP1 INTERPRETATION GUIDELINES
Guidelines for Interpreting EBER In Situ Hybridization
and LMP1 Immunohistochemical Tests for Detecting
Epstein-Barr Virus in Hodgkin Lymphoma
Margaret L. Gulley, MD,1 Sally L. Glaser, PhD,2 Fiona E. Craig, MD,3 Michael Borowitz, MD, PhD,4
Risa B. Mann, MD,4 Sarah J. Shema, MS,2 and Richard F. Ambinder, MD, PhD4
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
Key Words: Epstein-Barr virus; Hodgkin lymphoma; EBER; In situ hybridization; LMP1; Immunohistochemistry
Abstract Epidemiologic, molecular, and immunologic evidence
Histochemical stains demonstrate Epstein-Barr links Hodgkin lymphoma to Epstein-Barr virus (EBV) infec-
virus (EBV) in approximately 40% of all Hodgkin tion. A history of infectious mononucleosis is associated with
lymphomas, suggesting a role in tumorigenesis and the an increased risk of Hodgkin disease, and serologic studies
potential for EBV-targeted therapy. As research demonstrate high titers against viral antigens before tumor
progresses, it is important to define criteria for diagnosis.1-3 EBV has been detected in the malignant Reed-
interpreting histochemical stains. Four hemato- Sternberg/Hodgkin (RS/H) cells in approximately 40% of
pathologists independently interpreted EBV-encoded patients with Hodgkin disease, but EBV-relatedness depends
RNA (EBER) and latent membrane protein 1 (LMP1) on age, sex, geographic location, HIV status, and other char-
histochemical stains from 40 cases of Hodgkin acteristics of the study population. 3-5 Of the 4 major
lymphoma and then reviewed the stains as a group to histopathologic subtypes of Hodgkin lymphoma, the mixed
resolve discrepancies and to develop interpretation cellularity subtype is most frequently EBV-associated (70%),
guidelines. To call a Hodgkin case EBV-related, the followed by lymphocyte depletion (50%), nodular sclerosis
EBER and/or LMP1 signal must be unequivocally (20%), and lymphocyte predominant subtypes (<5%).4,6
present in Reed-Sternberg/Hodgkin (RS/H) cells. The Accurate laboratory tests to detect EBV are needed for
cytologic features and distribution of stained cells purposes of basic and epidemiologic research and for clinical
should be matched with those on the corresponding management. From a clinical standpoint, tests for EBV can
H&E-stained slide to help interpret whether the EBER be used to help establish a correct diagnosis in patients whose
or LMP1 signal is in malignant or reactive cells. The histologic lesion has overlapping features of Hodgkin
EBER signal is localized to the nucleus, whereas LMP1 lymphoma, anaplastic large cell lymphoma, or reactive
is in the cytoplasm and surface membrane. In some lymphoid hyperplasia.7 In addition, identification of tumor-
cases, only a fraction of RS/H cells express these factors associated EBV implies that the patient is a candidate for
for technical or biologic reasons. Before calling a case laboratory monitoring of tumor burden based on molecular
EBER-negative, it is essential to show that tumor cell assays for EBV viral load8-10 and for treatment using EBV-
RNA is preserved and available for hybridization. targeted oncologic therapies.11-13 Although somewhat unset-
LMP1 staining, although usually strong among all tled, evidence from several studies suggests that EBV related-
tumor cells in a given case, may alternatively be focal ness is a prognostic factor and influences survival.8,14-19
and weak, contributing to false-negative interpretation. Histochemical assays are widely used for localizing
EBER and LMP1 assays in combination are more Epstein-Barr viral nucleic acid or protein to the malignant
effective than either assay alone for identifying EBV- RS/H cells. These tumor cells express a limited spectrum of
related Hodgkin lymphoma. viral proteins, including EBV nuclear antigen 1 and the latent
membrane proteins (LMP1, LMP2a, and LMP2b). In addition,
© American Society for Clinical Pathology Am J Clin Pathol 2002;117:259-267 259
Gulley et al / EBER AND LMP1 INTERPRETATION GUIDELINES
EBV-encoded RNA (EBER1 and EBER2) is expressed Although histochemical assays for EBER and LMP1 are
abundantly, although EBER transcripts are nonpolyadeny- widely used in research and clinical settings, assay reliability
lated and remain untranslated. EBER in situ hybridization has never been characterized, and literature providing tech-
has been recommended as the best test for detecting and nical and interpretive guidance is sparse. As part of a study
localizing latent EBV in tissue samples.20-25 EBER tran- of interobserver agreement, we used evidence from interob-
scripts are naturally abundant in latently infected cells, with server performance to develop guidelines for interpreting
levels often exceeding 1 million copies per cell.26 Although EBER in situ hybridization and LMP1 immunohistochem-
EBER in situ hybridization is widely used to define cases of ical stains in the setting of Hodgkin lymphoma. To accom-
EBV-related Hodgkin disease, several pitfalls in technique plish this, Hodgkin lymphoma tissues from 40 patients were
and interpretation have been described. For example, false- stained in 2 separate testing laboratories and were indepen-
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
positive EBER interpretations are attributable to confusion dently interpreted by 4 hematopathologists (M.L.G., F.E.C.,
related to latent infection of background lymphocytes, M.B., and R.B.M.), who then met jointly to review the cases,
nonspecific staining, or cross-reactivity with mucin, yeast, or discuss technical and interpretive pitfalls, and recommend
plant materials.20 False-negative results may be a conse- interpretive criteria.
quence of RNA degradation.27 To overcome this problem,
some laboratories use a control stain for a ubiquitous cellular
transcript to ensure that RNA is preserved and available for
Materials and Methods
hybridization in the cells of interest. The U6 cellular tran-
script is a particularly appropriate control because it is We obtained 40 cases of Hodgkin lymphoma from the
similar to EBER in terms of size, abundance, and intranu- archival paraffin-embedded tissue files of 2 of us (R.F.A. and
clear distribution.28 Even when RNA is well preserved, some M.L.G.). These cases previously had been diagnosed as
investigators have described false-negative EBER results in Hodgkin lymphoma, subclassified using standard morpho-
tumors shown to contain EBV by other methods or at logic criteria,7 and assessed for EBV status by EBER in situ
previous time points.29-31 One tantalizing explanation is the hybridization and/or LMP1 immunohistochemical analysis.
hit-and-run hypothesis, which theorizes that EBV might On this basis, the 40 cases were selected to include 20 cases
once have been present in a tumor, but that all or part of the of nodular sclerosis (10 EBV-positive and 10 EBV-negative)
EBV genome subsequently was lost. 31,32 To facilitate and 20 cases of mixed cellularity (10 EBV-positive and 10
research into this hypothesis, it is important to define criteria EBV-negative) Hodgkin lymphoma. A single representative
for interpreting analytic tests for EBV and to describe an block chosen from each case was used for all subsequent
approach for handling focal EBER expression among RS/H histochemical studies. Paraffin sections were cut and distrib-
cells of the same tumor. To date, such guidelines are lacking. uted to 2 testing laboratories (Johns Hopkins University,
An alternative strategy commonly used for identifying Baltimore, MD, and the University of Texas Health Science
EBV-related Hodgkin lymphoma is immunohistochemical Center at San Antonio) for EBER, U6, and LMP1 histo-
detection of viral LMP1. LMP1 is expressed in the cyto- chemical stains using these laboratories’ routine analytic
plasm and surface membrane of RS/H cells but is rarely procedures as described in the following sections. All studies
expressed in latently infected background lymphocytes of were carried out under the supervision of an institutional
Hodgkin lymphoma.33 LMP1 is, however, expressed in the review board.
benign lymphocytes of infectious mononucleosis and in a
minute fraction of lymphocytes in healthy, remotely infected EBER In Situ Hybridization Procedures
viral carriers. 34,35 LMP1 immunostains are appealing EBER in situ hybridization was performed on each case
because they are more economic and rapid than EBER at each of the 2 testing laboratories using digoxigenin-
hybridization and more easily incorporated into routine clin- labeled riboprobes produced from plasmid templates
ical laboratories. LMP1 immunostains usually are performed obtained from one of us (R.F.A.).40 A step-by-step descrip-
using commercial antibodies on fixed, paraffin-embedded tion of one of the testing protocols, which uses EBER1 ribo-
tissues.36 Results should be interpreted with caution since probes, has been published.41 The other laboratory’s proce-
false-positive staining is reported in poorly fixed tissues, in dure differed in that a cocktail of EBER1 and EBER2
cells of the nervous system, and in some uninfected riboprobes was used, and the secondary structures of the
hematopoietic elements, including eosinophils and plasma riboprobes were disrupted immediately before use by boiling
cells.20,36,37 False-negative immunostain results are more in hybridization buffer for 3 minutes followed by plunging in
frequent in decalcified tissues. In addition, failure to identify ice. One laboratory hybridized overnight, whereas the other
EBV could occur if LMP1 is down-regulated, as is seen in hybridized for only 3 hours. To control for RNA preserva-
Burkitt lymphoma.33,38,39 tion, both laboratories used the same type of riboprobe,
260 Am J Clin Pathol 2002;117:259-267 © American Society for Clinical Pathology
Hematopathology / ORIGINAL ARTICLE
namely one targeting cellular U6 RNA. Both laboratories Negative staining was defined as the absence of chromogen
used RNase to facilitate washing away unbound probe and a above background levels in the cells of interest. Each case
detection system based on application of antibody to digoxi- was rated as easy, intermediate, or difficult to interpret. The
genin linked to alkaline phosphatase. One laboratory coun- pathologist also noted any factors that hampered interpreta-
terstained with 0.5% eosin, whereas the other used methyl tions, and these comments were recorded on data sheets
green counterstain. Known cases of EBV-related Hodgkin accompanying each shipment.
lymphoma were used as controls by both laboratories.
Development of Interpretive Guidelines
Immunohistochemical Detection of LMP1 Expression Following all reviews of each of the 40 Hodgkin cases, a
LMP1 immunohistochemical stains were performed at summary sheet was prepared listing the results of the 16
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
each of the 2 testing laboratories using similar methods. interpretations and 16 difficulty ratings for the EBER and
Both laboratories used a commercial cocktail of 4 mono- LMP1 stains performed at each of the 2 testing laboratories.
clonal antibodies against LMP1 (CS1-4, DAKO, Carpinteria These data, together with any pathologist comments, were
CA). Antigen availability was enhanced by pretreatment for reviewed along with the slides at a consensus conference in
5 minutes with Proteinase K (DAKO) at room temperature. which interpretation guidelines were developed and tech-
Endogenous peroxidase was quenched with sodium azide nical and interpretive pitfalls were discussed. For this
and hydrogen peroxide, and slides were incubated with anti- purpose, all investigators assembled around a multiheaded
body diluted at 1:200. Bound antibody was detected with microscope to review the cases. For the first time, the pathol-
biotinylated secondary antibody followed by peroxidase- ogists were able to compare the EBER and LMP1 stains on a
labeled streptavidin and diaminobenzidine color reagent given case, and they assigned a consensus interpretation on
(LSAB2/HRP System, DAKO). Automated instrumentation the EBV relatedness of each case. Discrepancies in their
(DAKO Autostainer, DAKO) was used to facilitate sequen- original interpretations were resolved, and the difficulty
tial application of reagents. One testing laboratory used ratings were discussed in conjunction with notes about
hematoxylin counterstain, whereas the other used methyl factors initially hindering interpretation. Based on these
green counterstain. Known cases of EBV-related Hodgkin discussions, guidelines for evaluating results were devel-
lymphoma were used as positive controls. oped, and specific criteria for interpreting results were estab-
lished by consensus.
Data Collection
After staining, the 40 EBER/U6 slide sets and 40 LMP1 Data Analysis
slide sets from each preparing laboratory (ie, 80 for each Data were tabulated and analyzed by an epidemiologist
assay), together with the corresponding H&E-stained slides, (S.L.G.) and a statistician (S.J.S.). For each of the 320 slides
were combined by the study epidemiologist (S.L.G.) into reviewed, interpretation agreement among the 4 pathologists
assay-specific batches of 40 tumors. These batches were was evaluated using the kappa statistic and associated 95%
distributed to the 4 hematopathologists so that each patholo- confidence interval. A kappa greater than 0 indicates more
gist independently interpreted each EBER stain and, at a agreement than expected by chance; kappa is considered to
separate sitting, each LMP1 stain. Every slide was distrib- indicate fair to good agreement between 0.40 and 0.75, and
uted for a second round of interpretations so that each of the very good agreement above 0.75.42 For each of the 320
4 pathologists saw each of the 160 slides twice for a total of slides reviewed, a consensus difficulty rating among the 4
1,280 interpretations. Each batch of 40 tumors was assem- reviewers was assigned according to the following criteria:
bled randomly to include both histologic subtypes, materials The interpretation was considered easy if 3 or more patholo-
from both laboratories, and both first and second reviews gists rated the interpretation as easy, difficult if 2 or more
(except for the first and last batches). Between reviews, pathologists rated it as difficult, and intermediate for all other
slides were relabeled to blind raters to review sequence and combinations. The kappa statistics stratified by difficulty
preparing laboratory. This design enabled analysis of both level were computed for interpretation agreement among the
interobserver and intraobserver reliability of assay interpreta- 4 pathologists.
tion.
Each pathologist was asked to evaluate the EBER or
LMP1 slide in conjunction with an associated H&E-stained
Results
slide and to interpret each result as positive, negative, or
uncertain with respect to the presence of EBV in RS/H cells. For all 160 EBER in situ hybridization reviews (ie, 40
The pathologist was asked to interpret a slide as positive if from each laboratory, each reviewed twice), consensus inter-
chromogen was localized to any proportion of these cells. pretation was considered easy in 70% of reviews, intermediate
© American Society for Clinical Pathology Am J Clin Pathol 2002;117:259-267 261
Gulley et al / EBER AND LMP1 INTERPRETATION GUIDELINES
1.2 uncertain for both markers. When both markers were evalu-
ated in tandem, all 40 cases could be confidently assigned as
1.0
EBV-positive or EBV-negative. EBER and LMP1 were coex-
0.8 pressed in 17 cases, neither marker was expressed in 17
cases, 2 cases were uncertain for EBER and negative for
0.6
kappa
LMP1, 2 cases were uncertain for EBER and positive for
0.4 LMP1, and the remaining 2 cases were positive for EBER
and uncertain for LMP1. Discussion of the discrepancies led
0.2
to the conclusion that proper interpretation required the
0.0 ability to morphologically identify RS/H cells and to distin-
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
guish them from background lymphocytes and other
– 0.2
nontumor cells. In addition, it was recommended that an
Easy Intermediate Difficult
H&E-stained section always be reviewed in parallel with
Difficulty of Interpretation each EBER or LMP1 stain, so that the prevalence, distribu-
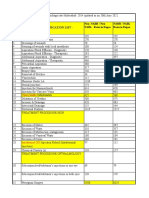
❚Figure 1❚ Agreement among 4 pathologists interpreting 320 tion, and cytologic features of the RS/H cells on the H&E-
Epstein-Barr virus–encoded RNA and latent membrane protein stain section could guide assessment of RS/H cells on the
1 histochemical stains. Difficulty ratings are displayed on the x corresponding EBER- or LMP1-stained slide.
axis, and the corresponding kappa statistic and 95% confidence
interval (denoted by error bars) representing level of agreement EBER In Situ Hybridization
among the 4 pathologists are displayed on the y axis. The pathologists made the following observations about
EBER hybridizations and their interpretation. The EBER
❚Table 1❚ signal was localized to the nucleus ❚Image 1❚. Sometimes the
Agreement Among Four Pathologists Interpreting EBER and chromogen obliterated the entire nucleus, and other times the
LMP1 Histochemical Stains Stratified by Difficulty Ratings
staining was weaker and appeared to segregate with the chro-
Agreement: Multirater kappa matin, sparing the nucleolus. No cytoplasmic signal was seen
Analyte/Consensus Difficulty Rating* Statistic (95% CI) in tumor cells, except during mitosis where the nuclear
Epstein-Barr virus–encoded RNA membrane was dissolved.
Easy (n = 112) 0.982 (0.965 to 1.00) Before concluding that a slide is EBER-negative, it is
Intermediate (n = 39) 0.485 (0.331 to 0.645)
Difficult (n = 9) –0.091 (–0.223 to 0.073) essential to evaluate a control slide, run in parallel, demon-
Latent membrane protein 1 strating that RNA is present and available for hybridization
Easy (n = 117) 0.983 (0.964 to 1.00)
Intermediate (n = 30) 0.696 (0.579 to 0.825)
in the cells of interest. The U6 control RNA targeted in this
Difficult (n = 13) 0.157 (–0.006 to 0.356) study was localized to the nucleus of all types of cells
(Image 1B). In the experimental samples, RNA often was
CI, confidence interval.
* Interpretation was considered easy if 3 or more pathologists rated the interpretation only partially preserved, as evidenced by U6 signal in some
as easy, difficult if 2 or more pathologists rated it as difficult, and intermediate for
all other combinations.
but not all cells of a given field or in some but not all areas
of the section.
The EBER stains evaluated in the present study had a
in 24%, and difficult in 7%. For all 160 LMP1 immunostain purple chromogen and either a methyl green counterstain
reviews, consensus interpretation was considered easy in 73%, producing a green backdrop or an eosin counterstain
intermediate in 19%, and difficult in 8%. These ratings producing a pink backdrop (Images 1C and 1D). The methyl
suggest that difficulty of interpretation did not differ substan- green counterstain was easier to interpret for several reasons.
tially between EBER stains and LMP1 stains. There was First, purple and green contrasted better than did purple and
generally very good interobserver agreement among the 4 pink. Second, eosinophils were distracting on eosin stains
pathologists for EBER (kappa = 0.813; 95% confidence but not on methyl green stains. Third, eosin counterstain
interval, 0.767-0.859) and for LMP1 (kappa = 0.826; 95% sometimes resulted in “slivers” of crystalline stain precipitate
confidence interval, 0.782-0.871). Not surprisingly, the level that were not formed when methyl green was used. Finally,
of agreement tended to vary by consensus difficulty rating, as methyl green staining provided improved discrimination of
shown in ❚Figure 1❚ overall and in ❚Table 1❚ by assay. benign vs malignant cytologic features because methyl green
At the consensus conference, consensus interpretation of highlighted chromatin, whereas eosin primarily highlighted
the cases yielded 19 EBER-positive, 17 EBER-negative, and cytoplasmic proteins.
4 uncertain EBER results, and 19 LMP1-positive, 19-LMP1 The EBER signal varied from weak to strong in intensity.
negative, and 2 uncertain cases for LMP1. No cases were Intensity seemed to relate primarily to the degree of RNA
262 Am J Clin Pathol 2002;117:259-267 © American Society for Clinical Pathology
Hematopathology / ORIGINAL ARTICLE
A B
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
C D
❚Image 1❚ Epstein-Barr virus–encoded RNA (EBER) in situ hybridization of Hodgkin tumors. A, Purple EBER signal is localized to
the nucleus of a Reed-Sternberg/Hodgkin cell. Multiple black pigment deposits represent fixation artifact. B, U6 control
hybridization confirms RNA preservation in the tissue as evidenced by U6 expression in the nuclei of reactive and malignant
cells alike. C, A single small lymphoid cell in the center expresses the purple EBER signal, while the remaining nucleated cells
stain only with methyl green counterstain. D, A single small lymphoid cell in the center expresses the purple EBER signal,
while the remaining cells stain pink owing to the eosin counterstain, including bright pink eosinophils. (×150)
preservation. It was impossible to assess the extent to EBER-negative. To distinguish mononuclear RS/H cells
which natural levels of EBER varied from cell to cell or from latently infected benign lymphocytes, the pathologists
case to case. One of the most difficult aspects of inter- relied on the small size of the nucleolus, scant cytoplasm,
preting EBER stains was distinguishing background and lack of “lacunae” surrounding benign lymphocytes. In
lymphocytes from RS/H cells. Rare (<0.1%), small, EBER- questionable cases, it is important to carefully scan the slide
positive cells with scant cytoplasm and clumped chromatin for EBER positivity in the more obvious RS cells having
were seen in many of the cases, and these were interpreted large, lobated nuclei, prominent nucleoli, and more abun-
as latently infected lymphocytes that might be present in dant cytoplasm. The morphologist should be cautious in
any viral carrier. More difficult to interpret were occasional interpreting a case as EBER-positive unless EBER is
medium-sized lymphocytes with visible nucleoli expressing expressed in at least 1 unequivocal tumor cell. As discussed
EBER in a tumor in which the more obvious RS cells were in the following section, immunohistochemical detection of
© American Society for Clinical Pathology Am J Clin Pathol 2002;117:259-267 263
Gulley et al / EBER AND LMP1 INTERPRETATION GUIDELINES
A B
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
C D
❚Image 2❚ Latent membrane protein 1 (LMP1) immunohistochemical stains of Hodgkin tumors. A, Brown, granular LMP1 signal
is localized to the cytoplasm and surface membrane of a Reed-Sternberg cell. B, A mononuclear Reed-Sternberg/Hodgkin cell
expresses LMP1 in the upper right, several smaller eosinophils exhibit false-positive cytoplasmic staining, and black carbon
pigment deposits are seen in the lower left. C, Occasional plasma cells exhibit false-positive cytoplasmic staining with the CS1-
4 cocktail of antibodies used to identify LMP1. D, Nonspecific cytoplasmic staining in tumor cells and nontumor cells alike along
the edge of the slide is the so-called edge artifact. (Methyl green counterstain, ×150)
LMP1 expression is quite helpful for resolving cases with contrast, a faint homogeneous blush of cytoplasmic color was
poor RNA preservation or equivocal EBER results. nonspecific and could be seen in fibroblasts as well as apop-
totic or “mummified” tumor cells.
LMP1 Immunohistochemical Findings False-positive cytoplasmic signal was seen in
Microscopic visualization of LMP1 immunostains eosinophils, which often are quite numerous in classic
revealed that LMP1 was localized to the cytoplasm and Hodgkin tissues. Eosinophils could be readily distinguished
surface membrane of RS/H cells ❚Image 2❚. In some cells, the from RS/H cells based on cell size and nuclear size and
LMP1 signal was concentrated in one segment of the surface shape and by the different character of cytoplasmic granu-
membrane to form a “cap.” LMP1 was not identified in larity (Image 2B).
benign-appearing lymphocytes. Intensity of LMP1 staining in False-positive cytoplasmic LMP1 signal was evident in
RS/H cells varied from strong to weak. It is important to note some but not all plasma cells, suggesting cross-reactivity of
that the chromogen had a distinctly granular character. In the antibody cocktail with certain plasma cell antigens.
264 Am J Clin Pathol 2002;117:259-267 © American Society for Clinical Pathology
Hematopathology / ORIGINAL ARTICLE
Plasma cells were readily distinguished from RS/H cells based ❚Table 2❚
on cell size, nuclear size and contours, and chromatin pattern Guidelines for Interpreting Epstein-Barr Virus–Encoded RNA
(EBER) In Situ Hybridization and Latent Membrane Protein 1
(Image 2C). In some tissues, particularly spleen, hemosiderin- (LMP1) Immunohistochemical Stains in Hodgkin Lymphoma
laden macrophages contained brown pigment that must not be
confused with LMP1 signal. Presumably carbon, melanin, or • The morphologist must be competent in distinguishing Reed-
Sternberg/Hodgkin (RS/H) cells from nontumor cells. The
other pigments could likewise mimic the chromogen. cytologic features and distribution of RS/H cells should be
Matching the cytomorphologic features and distribution assessed on matched H&E-stained sections before interpreting
EBER or LMP1 results.
of the RS/H cells on the H&E stain to those on the LMP1 • To interpret a case as positive, the EBER or LMP1 signal must
stain should help ensure that the correct cell population is be unequivocally localized to RS/H cells. The fraction of RS/H
cells expressing EBER and LMP1 varies among cases, with
evaluated. A positive control slide is essential for demon- most cases having a high fraction of positive tumor cells. For
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
strating that the system is working and to serve as a gauge of purposes of identifying all Epstein-Barr virus–related Hodgkin
the expected color and granular character of true-positive cases, just 1 unequivocal RS/H cell expressing EBER or LMP1
should be considered sufficient to call a case positive. Equivocal
staining. Likewise, a negative control stain in which the anti- cases frequently are resolved when EBER, LMP1, and H&E
body is omitted should help assess nonspecific staining. stains are evaluated in parallel.
• The EBER signal is localized to the nucleus, sometimes sparing
or rimming the nucleus. A negative EBER result can be
Focal Variation in EBER or LMP1 Expression Within a interpreted as negative only if RNA is shown to be preserved
Given Tissue Sample and available for hybridization in tumor cells. A variable
proportion of background lymphocytes express EBER (usually
When EBER was expressed in any RS/H cells, it usually 0%-1%), and these must be distinguished from RS/H cells.
• The LMP1 signal is localized to the cytoplasm and surface
was expressed in all RS/H cells. However, in some cases, only membrane and has a granular character. False-positive
a proportion of RS/H cells were positive. The most common cytoplasmic staining is seen in eosinophils and a fraction of
reason for focal EBER staining seemed to be focal RNA plasma cells. “Edge artifact” and other “background staining”
may contribute to false-positive signal in benign and malignant
preservation. For this reason, it is important to evaluate the cells alike.
corresponding U6 stain to identify areas where RNA was well • As with any histochemical stain, quality control measures should
be used to ensure adequacy of staining, preservation of
preserved and available for hybridization in the RS/H cells. If cytomorphologic features, and interpretive competency.
EBER analysis is restricted to areas with adequate RNA preser-
vation, then EBER is nearly always expressed in an “all-or-
nothing” manner in the RS/H cell population of a given tumor.
When LMP1 was expressed in any RS/H cells, it usually stains that are most commonly used to identify EBV in
was expressed in all RS/H cells. Focal LMP1 was an alter- Hodgkin lymphoma.
nate outcome, occurring in 6 (15%) of 40 Hodgkin cases, or In the present study of 40 Hodgkin tumors evaluated by
6 (30%) of 20 LMP1-positive cases. In some of these cases, 4 expert hematopathologists, EBER stains were considered
fewer than 5% of tumor cells expressed LMP1. interpretable in 36 cases and LMP1 stains in 38 cases. By
“Edge artifact,” whereby the edges of the tissue had a using the 2 stains in tandem, EBV status was assigned in all
variably wide rim of nonspecific staining, was seen in some 40 cases. Testing and interpretation of these cases provided a
of the LMP1 immunostains but in none of the EBER framework for developing guidelines for interpreting EBER
hybridizations (Image 2D). LMP1 and EBER stains occa- and LMP1 histochemical stains in Hodgkin tissue samples,
sionally had large (30-100 µm) spots of nonspecific staining as summarized in ❚Table 2❚. A critical factor in interpreting
that we speculated were a consequence of either fixation arti- stain results is the ability to morphologically identify RS/H
fact (especially with B-5 fixative) or bubbles in the staining cells and to distinguish them from background lymphocytes,
reagents. Such zones of nonspecific staining were localized histiocytes, and other nontumor cells. We recommend that an
to clusters of cells regardless of their histogenesis. H&E-stained section be reviewed along with the histochem-
ical stain so as to match the prevalence, distribution, and
cytologic features of the RS/H cells on the H&E-stained
section to those on the corresponding EBER- or LMP1-
Discussion
stained slide.
Previous molecular studies revealed monoclonal EBV In our experience, EBER and LMP1 usually were
DNA in Hodgkin tumor tissue, suggesting that the virus was expressed in an all-or-nothing manner among the RS/H cells
present before expansion of the malignant clone.43 The role of a given case. However, in some cases, only a proportion of
of EBV in disease pathogenesis and the prognostic and ther- RS/H cells were positive for these markers. The most
apeutic value of EBV infection remain subjects of ongoing common reason for focal EBER staining seemed to be focal
investigation. To facilitate basic and clinical research, it is RNA preservation. For this reason, it is important to evaluate
important to define criteria for interpreting the histochemical the corresponding control hybridization to identify areas in
© American Society for Clinical Pathology Am J Clin Pathol 2002;117:259-267 265
Gulley et al / EBER AND LMP1 INTERPRETATION GUIDELINES
which RNA was well preserved and available for hybridiza- In the present study, Proteinase K was used to facilitate
tion in the cells of interest. To avoid a technical pitfall that antigen or nucleic acid retrieval before application of anti-
might lead to false-negative EBER results, it is important that body or probe. It is important that Proteinase K digestion be
the EBER signal be at least as strong as the control signal so sufficient to achieve this objective without destroying the
that control gene expression signifies that enough RNA is cytomorphologic features of the tissue. Individual tumors
preserved to allow detection of any EBER-positive cells. may benefit from different digestion conditions, and it may
Cases in which RNA is lacking in the RS/H cells cannot be necessary to adjust the Proteinase K concentration or
be interpreted as negative for EBER, since it is likely that the incubation time to optimize stain quality.
RNA has been destroyed at some point during tissue prepara- A number of technical and interpretive issues influence
tion. To minimize RNA degradation during sectioning, we the outcome of EBER and LMP1 histochemical tests applied
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
recommend the use of a sterile water bath to float sections and to Hodgkin tumors. The guidelines provided herein,
the wearing of gloves so that the slides are never touched with combined with proper attention to the quality control
bare hands. Since treatment with RNase is an integral part of measures that guide all histochemical procedures, should
the posthybridization wash procedures, the RNase solutions facilitate uniform interpretation of these tests. Because
must not be allowed to contaminate any of the reagents or EBER and LMP1 stains are each subject to false-negative
surfaces to which slides are exposed before hybridization. At interpretation, we recommend that future studies of EBV-
the time of tissue procurement, tissues should be sliced and related Hodgkin lymphoma rely on EBER and LMP1 histo-
fixed as soon as possible, but not overfixed before processing. chemical stains in concert when determining the EBV relat-
Formalin and B-5 are both suitable fixatives. Fixation artifact edness of a particular Hodgkin tumor.
often is seen with B-5 fixative and sometimes with formalin
fixation, resulting in black spider-like precipitants that inter- From the 1Department of Pathology, University of Texas Health
fere with visualization of the intended chromogen. Decalcifi- Science Center at San Antonio; 2Northern California Cancer
cation does not necessarily interfere with EBER or LMP1 Center, Union City, CA; 3Department of Pathology, University of
staining, and appropriate control stains can be done to assess Pittsburgh, Pittsburgh, PA; and 4Johns Hopkins University,
Baltimore, MD.
the ability to detect similar targets known to be expressed in
these types of tissues. As always, small biopsy specimens and Funded by a grant R03 CA77125 from the National Cancer
those with few RS/H cells are fraught with concerns about Institute, Bethesda, MD.
sampling error. Address reprint requests to Dr Gulley: Dept of Pathology,
When only a fraction of atypical cells express EBER or University of North Carolina, Chapel Hill, NC 27599-7525.
LMP1, it often is difficult to be certain that these are RS/H Acknowledgments: We thank Phyllis Eagan, Alexandra
Morgan, Patricia Harasty, and Susan Stewart, PhD, for their
cells. For this reason, it is important that the microscopist be
contributions to this study.
well versed in the morphologic diagnosis of Hodgkin
lymphoma and that the tissue sample be of adequate size and
quality to permit accurate interpretation. In the present study,
References
LMP1 expression was focal in about 15% of cases. Because
staining could be focal and weak, we consider it important to 1. Hjalgrim H, Askling J, Sorensen P, et al. Risk of Hodgkin’s
disease and other cancers after infectious mononucleosis.
scan the entire slide using a medium to high-power objective. J Natl Cancer Inst. 2000;92:1522-1528.
Otherwise, weak, focal LMP1 staining could be overlooked. 2. Mueller N, Evans A, Harris NL, et al. Hodgkin’s disease and
The biologic explanation for variation in LMP1 expression Epstein-Barr virus: altered antibody pattern before diagnosis.
levels is not well understood. Down-regulation of LMP1 N Engl J Med. 1989;320:689-695.
could be a function of the degree of tumor cell differentiation 3. Mueller N. Hodgkin’s disease. In: Scottenfeld D, Fraumeni JF
Jr, eds. Cancer Epidemiology and Prevention. New York, NY:
or of the immune system’s ability to recognize and destroy Oxford University Press; 1996:893-919.
cells expressing foreign antigens. Further research is 4. Glaser SL, Lin RJ, Stewart SL, et al. Epstein-Barr
required to define the factors influencing LMP1 expression virus–associated Hodgkin’s disease: epidemiologic
levels. For purposes of identifying all EBV-related Hodgkin characteristics in international data. Int J Cancer.
1997;70:375-382.
cases, we propose that just 1 unequivocal RS/H cell
5. Siebert JD, Ambinder RF, Napoli VM, et al. Human
expressing EBER or LMP1 should be considered sufficient immunodeficiency virus–associated Hodgkin’s disease
to call a tumor positive for EBV. Equivocal cases are contains latent, not replicative, Epstein-Barr virus. Hum
frequently resolved when EBER, LMP1, and H&E stains are Pathol. 1995;26:1191-1195.
evaluated in parallel. When many EBER-positive small 6. von Wasielewski R, Werner M, Fischer R, et al. Lymphocyte-
predominant Hodgkin’s disease: an immunohistochemical
lymphocytes are present, it is wise to consider infectious analysis of 208 reviewed Hodgkin’s disease cases from the
mononucleosis in the differential diagnosis. German Hodgkin Study Group. Am J Pathol. 1997;150:793-803.
266 Am J Clin Pathol 2002;117:259-267 © American Society for Clinical Pathology
Hematopathology / ORIGINAL ARTICLE
7. Harris NL. Hodgkin’s disease: classification and differential 25. Wu TC, Mann RB, Charache P, et al. Detection of EBV gene
diagnosis. Mod Pathol. 1999;12:159-175. expression in Reed-Sternberg cells of Hodgkin’s disease. Int J
8. Gallagher A, Armstrong AA, MacKenzie J, et al. Detection of Cancer. 1990;46:801-804.
Epstein-Barr virus (EBV) genomes in the serum of patients 26. Clemens MJ. The small RNAs of Epstein-Barr virus. Mol Biol
with EBV-associated Hodgkin’s disease. Int J Cancer. Rep. 1993;17:81-92.
1999;84:442-448. 27. Arber JM, Weiss LM, Chang KL, et al. The effect of
9. Lei KI, Chan LY, Chan WY, et al. Quantitative analysis of decalcification on in situ hybridization. Mod Pathol.
circulating cell-free Epstein-Barr virus (EBV) DNA levels in 1997;10:1009-1014.
patients with EBV-associated lymphoid malignancies. Br J 28. Andersen J, Zieve GW. Assembly and intracellular transport
Haematol. 2000;111:239-246. of snRNP particles. Bioessays. 1991;13:57-64.
10. Drouet E, Brousset P, Fares F, et al. High Epstein-Barr virus 29. Srinivas SK, Sample JT, Sixbey JW. Spontaneous loss of viral
serum load and elevated titers of anti-ZEBRA antibodies in episomes accompanying Epstein-Barr virus reactivation in a
patients with EBV-harboring tumor cells of Hodgkin’s disease.
Downloaded from https://academic.oup.com/ajcp/article-abstract/117/2/259/1758556 by guest on 17 December 2019
Burkitt’s lymphoma cell line. J Infect Dis. 1998;177:1705-
J Med Virol. 1999;57:383-389. 1709.
11. Rooney CM, Roskrow MA, Suzuki N, et al. Treatment of 30. Delecluse HJ, Marafioti T, Hummel M, et al. Disappearance of
relapsed Hodgkin’s disease using EBV-specific cytotoxic T the Epstein-Barr virus in a relapse of Hodgkin’s disease.
cells. Ann Oncol. 1998;9(suppl 5):S129-S132. J Pathol. 1997;182:475-479.
12. Su Z, Peluso MV, Raffegerst SH, et al. The generation of 31. Razzouk BI, Srinivas S, Sample CE, et al. Epstein-Barr virus
LMP2a-specific cytotoxic T lymphocytes for the treatment of DNA recombination and loss in sporadic Burkitt’s lymphoma.
patients with Epstein-Barr virus–positive Hodgkin disease. J Infect Dis. 1996;173:529-535.
Eur J Immunol. 2001;31:947-958.
32. Sixbey JW. Epstein-Barr virus DNA loss from tumor cells and
13. Roskrow MA, Suzuki N, Gan Y, et al. Epstein-Barr virus the geography of Burkitt’s lymphoma. EBV Rep. 2000;7:37-40.
(EBV)-specific cytotoxic T lymphocytes for the treatment of
patients with EBV-positive relapsed Hodgkin’s disease. Blood. 33. Hummel M, Anagnostopoulos I, Dallenbach F, et al. EBV
1998;91:2925-2934. infection patterns in Hodgkin’s disease and normal lymphoid
tissue: expression and cellular localization of EBV gene
14. Armstrong AA, Lennard A, Alexander FE, et al. Prognostic products. Br J Haematol. 1992;82:689-694.
significance of Epstein-Barr virus association in Hodgkin’s
disease. Eur J Cancer. 1994;7:1045-1046. 34. Reynolds DJ, Banks PM, Gulley ML. New characterization of
infectious mononucleosis and a phenotypic comparison with
15. Vestlev PM, Pallesen G, Sandvej K, et al. Prognosis of Hodgkin’s disease. Am J Pathol. 1995;146:379-388.
Hodgkin’s disease is not influenced by Epstein-Barr virus
latent membrane protein. Int J Cancer. 1992;50:670-671. 35. Babcock GJ, Thorley-Lawson DA. Tonsillar memory B cells,
latently infected with Epstein-Barr virus, express the restricted
16. Morente MM, Piris MA, Abraira V, et al. Adverse clinical pattern of latent genes previously found only in Epstein-Barr
outcome in Hodgkin’s disease is associated with loss of virus–associated tumors. Proc Natl Acad Sci U S A.
retinoblastoma protein expression, high Ki67 prolifer- 2000;97:12250-12255.
ation index, and absence of Epstein-Barr virus–latent
membrane protein 1 expression. Blood. 1997;90:2429- 36. Jiwa NM, Oudejans JJ, Dukers DF, et al. Immunohisto-
2436. chemical demonstration of different latent membrane
protein-1 epitopes of Epstein-Barr virus in lymphoproliferative
17. Murray PG, Billingham LJ, Hassan HT, et al. Effect of diseases. J Clin Pathol. 1995;48:438-442.
Epstein-Barr virus infection on response to chemotherapy and
37. Hammer RD, Scott M, Shahab I, et al. Latent membrane
survival in Hodgkin’s disease. Blood. 1999;94:442-447.
protein antibody reacts with normal hematopoietic precursor
18. Clarke CA, Glaser SL, Dorfman RF, et al. Epstein-Barr virus cells and leukemic blasts in tissues lacking Epstein-Barr virus
and survival after Hodgkin disease in a population-based series genome by polymerase chain reaction. Am J Clin Pathol.
of women. Cancer. 2001;91:1579-1587. 1996;106:469-474.
19. Glavina-Durdov M, Jakic-Razumovic J, Capkun V, et al. 38. Tao Q, Robertson KD, Manns A, et al. Epstein-Barr virus
Assessment of the prognostic impact of the Epstein-Barr (EBV) in endemic Burkitt’s lymphoma: molecular analysis of
virus–encoded latent membrane protein-1 expression in primary tumor tissue. Blood. 1998;91:1373-1381.
Hodgkin’s disease. Br J Cancer. 2001;84:1227-1234.
39. Niedobitek G, Agathanggelou A, Rowe M, et al. Hetero-
20. Gulley ML. Molecular diagnosis of Epstein-Barr virus–related geneous expression of Epstein-Barr virus latent proteins in
diseases. J Mol Diagn. 2001;3:1-10. endemic Burkitt’s lymphoma. Blood. 1995;86:659-665.
21. Ambinder RF, Mann RB. Detection and characterization of 40. Barletta JM, Kingma DW, Ling Y, et al. Rapid in situ
Epstein-Barr virus in clinical specimens. Am J Pathol. hybridization for the diagnosis of latent Epstein-Barr virus
1994;145:239-252. infection. Mol Cell Probes. 1993;7:105-109.
22. Brousset P, Meggetto F, Chittal S, et al. Assessment of the 41. Fan H, Gulley ML. Molecular methods for detecting Epstein-
methods for the detection of Epstein-Barr virus nucleic acids Barr virus. In: Killeen AA, ed. Molecular Pathology Protocols.
and related gene products in Hodgkin’s disease. Lab Invest. Totowa, NJ: Humana Press; 2001.
1993;69:483-490. 42. Posner KL, Sampson PD, Caplan RA, et al. Measuring
23. Hamilton-Dutoit SJ, Pallesen G. Detection of Epstein-Barr interrater reliability among multiple raters: an example of
virus small RNAs in routine paraffin sections using non- methods for nominal data. Stat Med. 1990;9:1103-1115.
isotopic RNA/RNA in situ hybridization. Histopathology. 43. Gulley ML, Eagan PA, Quintanilla-Martinez L, et al. Epstein-
1994;25:101-111. Barr virus DNA is abundant and monoclonal in the Reed-
24. Armstrong AA, Weiss LM, Gallagher A, et al. Criteria for the Sternberg cells of Hodgkin’s disease: association with mixed
definition of Epstein-Barr virus association in Hodgkin’s cellularity subtype and Hispanic American ethnicity. Blood.
disease. Leukemia. 1992;6:869-874. 1994;83:1595-1602.
© American Society for Clinical Pathology Am J Clin Pathol 2002;117:259-267 267
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Basics in Clinical Nutrition 5Document24 pagesBasics in Clinical Nutrition 5Tanya Dubey18% (17)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 16.1.6 - Sport and Exercise PharmacologyDocument26 pages16.1.6 - Sport and Exercise PharmacologyJuanMa Correa SanabriaNo ratings yet
- Amiodarone: Reevaluation of An Old Drug: Ann Intern Med. 1995 122:689-700Document12 pagesAmiodarone: Reevaluation of An Old Drug: Ann Intern Med. 1995 122:689-700DenisseRangelNo ratings yet
- Case Study About Ischemic StrokeDocument5 pagesCase Study About Ischemic StrokeMoath MahmoudNo ratings yet
- Amr FactsheetDocument6 pagesAmr FactsheetAhmed .YNo ratings yet
- PRDocument6 pagesPRSiti Nur FadillahNo ratings yet
- The Peroral Pneumocolon Examination:, PoorDocument3 pagesThe Peroral Pneumocolon Examination:, PoormanishbabuNo ratings yet
- Pediatric Cutaneus of Larva MigransDocument12 pagesPediatric Cutaneus of Larva MigransSarah M PanjaitanNo ratings yet
- Gendec - 2022-02-04T121135.640Document1 pageGendec - 2022-02-04T121135.640Robinson llanos ceraNo ratings yet
- Result-Based Performance Management System Teachers' ProfileDocument3 pagesResult-Based Performance Management System Teachers' ProfileMARITES TUMOLVANo ratings yet
- 10D Health Problems Should MustDocument1 page10D Health Problems Should MustKin100% (1)
- Lesson 1 Oxygenation Suctioning Bronchial HygieneDocument14 pagesLesson 1 Oxygenation Suctioning Bronchial HygieneRENEROSE TORRESNo ratings yet
- Picornaviridae & Adenoviridae - Raja Pardomuan HarahapDocument63 pagesPicornaviridae & Adenoviridae - Raja Pardomuan HarahapM. RamazaliNo ratings yet
- Occupational Health Surveillance by Fiona DavidsonDocument33 pagesOccupational Health Surveillance by Fiona DavidsonMuhammad Teguh DPNo ratings yet
- Low-Dose Naltrexone (LDN) Fact Sheet 2016: Contact: Linda Elsegood Email: Skype Phone No'sDocument8 pagesLow-Dose Naltrexone (LDN) Fact Sheet 2016: Contact: Linda Elsegood Email: Skype Phone No'scristiNo ratings yet
- D'Dimer, Fibrinogen Dan IL6 PAD CovidDocument8 pagesD'Dimer, Fibrinogen Dan IL6 PAD CovidWartimah imahNo ratings yet
- CGHS Rates 2014 - HyderabadDocument60 pagesCGHS Rates 2014 - HyderabadPradeep PaswanNo ratings yet
- Inhibitors of AngiotensinDocument37 pagesInhibitors of AngiotensinBoyu GrtrNo ratings yet
- Chapter 30Document19 pagesChapter 30utama stNo ratings yet
- Laporan-Laporan ObatDocument83 pagesLaporan-Laporan Obatsofyan hadyNo ratings yet
- Clarastill™ Can-C (CE Approved As Medical Device) .Document1 pageClarastill™ Can-C (CE Approved As Medical Device) .dokter Hewan AdhonaNo ratings yet
- Module 7 - Health-and-Promotion-and-EducationDocument7 pagesModule 7 - Health-and-Promotion-and-EducationPascua, Aliah M.No ratings yet
- DocusateDocument3 pagesDocusateAaliyah OralloNo ratings yet
- NABL Certified MEDICAL Labs-2014Document99 pagesNABL Certified MEDICAL Labs-2014Singh PushpanjaliNo ratings yet
- Hospital List MedicareDocument484 pagesHospital List MedicareVaibhav BahetiNo ratings yet
- Roxithromycin TabletDocument13 pagesRoxithromycin Tabletno debedeNo ratings yet
- Medical-Surgical 1 Nursing Samplex: Exam CompilationDocument75 pagesMedical-Surgical 1 Nursing Samplex: Exam CompilationMarvie TorralbaNo ratings yet
- Ra and Osteoarthritis R IfDocument43 pagesRa and Osteoarthritis R IfsnfhanNo ratings yet
- Deferomidad Angular Articulo 1Document5 pagesDeferomidad Angular Articulo 1yarianna2No ratings yet
- Grade 5 Ut4 Revision UploadDocument10 pagesGrade 5 Ut4 Revision UploadFasi HaiderNo ratings yet