Professional Documents
Culture Documents
10 1001@jama 2019 18254
Uploaded by
Ivan BurgosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1001@jama 2019 18254
Uploaded by
Ivan BurgosCopyright:
Available Formats
Research
JAMA | Original Investigation
Effect of Rocuronium vs Succinylcholine on Endotracheal Intubation
Success Rate Among Patients Undergoing Out-of-Hospital
Rapid Sequence Intubation
A Randomized Clinical Trial
Bertrand Guihard, MD; Charlotte Chollet-Xémard, MD; Philippe Lakhnati, MD; Benoit Vivien, MD, PhD;
Claire Broche, MD; Dominique Savary, MD; Agnes Ricard-Hibon, MD; Pierre-Jean Marianne dit Cassou, MD;
Frédéric Adnet, MD, PhD; Eric Wiel, MD, PhD; Juliette Deutsch, MD; Cindy Tissier, MD; Thomas Loeb, MD;
Vincent Bounes, MD, PhD; Emmanuel Rousseau, MD; Patricia Jabre, MD, PhD; Laetitia Huiart, MD, PhD;
Cyril Ferdynus, PhD; Xavier Combes, MD, PhD
Visual Abstract
IMPORTANCE Rocuronium and succinylcholine are often used for rapid sequence intubation, Supplemental content
although the comparative efficacy of these paralytic agents for achieving successful
intubation in an emergency setting has not been evaluated in clinical trials. Succinylcholine
use has been associated with several adverse events not reported with rocuronium.
OBJECTIVE To assess the noninferiority of rocuronium vs succinylcholine for tracheal
intubation in out-of-hospital emergency situations.
DESIGN, SETTING AND PARTICIPANTS Multicenter, single-blind, noninferiority randomized
clinical trial comparing rocuronium (1.2 mg/kg) with succinylcholine (1 mg/kg) for rapid
sequence intubation in 1248 adult patients needing out-of-hospital tracheal intubation.
Enrollment occurred from January 2014 to August 2016 in 17 French out-of-hospital
emergency medical units. The date of final follow-up was August 31, 2016.
INTERVENTIONS Patients were randomly assigned to undergo tracheal intubation facilitated
by rocuronium (n = 624) or succinylcholine (n = 624).
MAIN OUTCOMES AND MEASURES The primary outcome was the intubation success rate on
first attempt. A noninferiority margin of 7% was chosen. A per-protocol analysis was
prespecified as the primary analysis.
RESULTS Among 1248 patients who were randomized (mean age, 56 years; 501 [40.1%]
women), 1230 (98.6%) completed the trial and 1226 (98.2%) were included in the
per-protocol analysis. The number of patients with successful first-attempt intubation was
455 of 610 (74.6%) in the rocuronium group vs 489 of 616 (79.4%) in the succinylcholine
group, with a between-group difference of −4.8% (1-sided 97.5% CI, −9% to ⬁), which did not
meet criteria for noninferiority. The most common intubation-related adverse events were
hypoxemia (55 of 610 patients [9.0%]) and hypotension (39 of 610 patients [6.4%]) in the
rocuronium group and hypoxemia (61 of 616 [9.9%]) and hypotension (62 of 616 patients
[10.1%]) in the succinylcholine group.
CONCLUSIONS AND RELEVANCE Among patients undergoing endotracheal intubation in an
out-of-hospital emergency setting, rocuronium, compared with succinylcholine, failed to
demonstrate noninferiority with regard to first-attempt intubation success rate.
TRIAL REGISTRATION ClinicalTrials.gov Identifier: NCT02000674
Author Affiliations: Author
affiliations are listed at the end of this
article.
Corresponding Author: Xavier
Combes, MD, PhD, Department of
Emergency, CHU de la Réunion,
Université de la Réunion, Allée des
Topazes, Saint Denis, 97400,
Réunion, France (x.combes.samu974
JAMA. 2019;322(23):2303-2312. doi:10.1001/jama.2019.18254 @chu-reunion.fr).
(Reprinted) 2303
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Research Original Investigation Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation
T
racheal intubation is one of the most critical interven-
tions in emergency settings.1 Several clinical studies Key Points
have reported that sedation greatly improves ease and
Question Is rocuronium noninferior to succinylcholine with
safety of this emergency procedure.2,3 Rapid sequence intu- regard to first-attempt endotracheal intubation success among
bation (RSI) is therefore the most widely recommended seda- patients undergoing rapid sequence intubation in an
tion technique for patients requiring emergency tracheal out-of-hospital emergency setting?
intubation.4 RSI involves administration of rapid-onset drugs,
Findings In this randomized clinical trial that included 1248
including a hypnotic and a paralytic agent. Use of a neuromus- patients, the number of patients with successful first-attempt
cular blocking agent improves the overall intubating condi- intubation was 455 of 610 (74.6%) in the rocuronium group vs
tions and first-attempt intubation success rate, regardless of 489 of 616 (79.4%) in the succinylcholine group, a difference of
the choice of induction agent.5,6 Succinylcholine has tradi- −4.8% (1-sided 97.5% CI, −9% to ⬁), which did not meet criteria
tionally been the preferred neuromuscular blocking agent, ex- for noninferiority.
cept when contraindicated.7 Rocuronium, introduced more re- Meaning The study findings failed to demonstrate noninferiority
cently for use in emergency situations, has been proposed as of rocuronium compared with succinylcholine with regard to
a good alternative to succinylcholine because of its pharma- first-attempt endotracheal intubation success rate.
cokinetic characteristics. When used at a dose of 1.2 mg/kg,
rocuronium has a similar onset time to succinylcholine.8 Be- was required. If no relatives were present at the time of intu-
cause succinylcholine has several clinical contraindications and bation, an information letter offering the opportunity to pro-
rocuronium has no contraindications (except for hypersensi- vide consent or to opt out of inclusion in the study was sys-
tivity to the agent), debate about the paralytic agent of choice tematically sent to the patient if he or she survived and left the
for RSI has persisted for several years. Moreover, succinylcho- hospital or to a relative if the patient died at the hospital. Ad-
line use has been associated with several adverse events not ditional information on the methods for obtaining consent is
reported with rocuronium, including hyperkalemia and in- available in Supplement 2.
crease in oxygen consumption leading to rapid desaturation.9,10 The emergency medical service system in France is a cen-
Numerous reviews have concluded that succinylcholine trally based, 2-tiered system. The first level is composed of ba-
provides better intubating conditions than rocuronium, but sic life support fire department ambulances based at fire sta-
other observational studies have reported that when rocuronium tions. The second level comprises advanced life support
is used at a dose higher than 1 mg/kg, intubation is as success- physician-staffed ambulances. These mobile intensive care units
ful as with succinylcholine.11-13 Consequently, surveys have re- are distributed throughout each region. The physician-staffed
ported a marked increase in rocuronium use in emergency ambulances have a minimum team of a trained ambulance
settings.11,14 To our knowledge, no randomized study has com- driver, a nurse (or a nurse anesthesiologist), a senior physician
pared these paralytic agents in emergency settings.15 specializing in either emergency medicine (in more than 90%
Given these conflicting results and the lack of high- of cases) or anesthesiology, and, sometimes, a medical stu-
quality evidence, a randomized clinical trial was conducted to dent on board. All physicians have at least 2 years of practice
compare rocuronium vs succinylcholine use in emergency out- and are emergency physicians or anesthesiologists. Tracheal in-
of-hospital intubation situations. It was hypothesized that tubation is only performed by advanced life support units.
rocuronium would be noninferior to succinylcholine for fa-
cilitating tracheal intubation. Patient Population
Patients were recruited between January 2014 and August 2016.
The study included all consecutive out-of-hospital adult pa-
tients requiring emergency tracheal intubation as assessed by
Methods
the emergency physician. Patients with all conditions (trauma,
Study Design dyspnea, coma, overdoses, and shock), except cardiac arrest,
The Succinylcholine vs Rocuronium for Out-of-Hospital Emer- were included. Patients who met any of the following criteria
gency Intubation (CURASMUR) trial was a nationwide, single- were excluded from the study: younger than 18 years; preg-
blind, randomized, noninferiority clinical trial conducted from nant women; contraindication to rocuronium (known allergy
January 2014 through August 2016 at 17 out-of-hospital emer- to rocuronium), succinylcholine (personal or family history of
gency medical units in France. The study patients were blinded known malignant hyperthermia, known allergy to succinylcho-
to intervention assignment, but the physicians conducting the line, congenital muscular dystrophy, myasthenia, specific hy-
intubation procedures were not blinded. The Comité de Pro- perkalemia, recent open eye surgery, known congenital deficit
tection des Personnes Sud-Ouest et Outre-Mer ethics commit- in plasma pseudocholinesterases), or sugammadex (the selec-
tee approved the trial protocol (ref 2013-001438-16), which is tive paralytic binding agent for rocuronium reversal); under
available in Supplement 1. Patients undergoing out-of- guardianship; and no health insurance.
hospital emergency intubation are most often not able to pro-
vide informed consent. In accordance with French laws on Randomization
emergency medical research, if a patient's relative was present Patients were randomized in a 1:1 ratio to the rocuronium or
when the medical team had to intubate, written consent from the succinylcholine group (Figure 1). A statistician at the meth-
the relative of the patient to be included in the clinical study odological unit of the La Réunion University Hospital Center,
2304 JAMA December 17, 2019 Volume 322, Number 23 (Reprinted) jama.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation Original Investigation Research
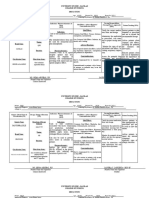
Figure 1. Flow of Participants in CURASMUR, a Study of the Effect of Rocuronium vs Succinylcholine
on Endotracheal Intubation Success Rate Among Patients Undergoing Out-of-Hospital Intubation
1326 Patients assessed for eligibility
78 Excluded
26 Reason not provided
20 Did not meet inclusion criteria
7 No health insurance
6 With cardiac arrest
4 Age <18 years
2 Contraindications to succinylcholine
1 Under guardianship
12 Physician declined to participate
11 Improvement in clinical condition
9 Declined to participate
1248 Patients randomized
624 Randomized to the 624 Randomized to the
rocuronium group succinylcholine group
613 Received intervention 617 Received intervention
as randomized as randomized
11 Did not receive intervention 7 Did not receive intervention
as randomized as randomized
5 Withdrew consent 2 Under guardianship
3 No health insurance 2 Withdrew consent
1 Age <18 years 2 No health insurance
1 Under guardianship 1 Age <18 years
1 Pregnant
613 Included in the randomized 617 Included in the randomized
group analysis group analysis
2 No intubation attempted 1 Received rocuronium
1 Received succinylcholine
610 Included in the per-protocol 616 Included in the per-protocol
analysis analysis
not involved in patient recruitment, generated randomiza- but optional, according to the physician's preference. It was
tion sequences. The sequences were generated using the PROC recommended to perform intubation 60 seconds after
PLAN procedure from SAS, version 9.4 (SAS Institute). Bal- administration of the paralytic agent. Single-use Macintosh
anced and stratified by center, randomization lists were gen- metallic laryngoscope blades (size 3 and 4) were used. The
erated using randomly permuted blocks of 4, 6, and 8 pa- standard intubation procedure did not include use of a stylet;
tients. Numbered and sealed opaque envelopes were then stylet use was considered an alternative airway procedure.
generated from those lists and used by emergency physicians When standard laryngoscopy-assisted intubation was not
in each ambulance to assign patients to the rocuronium or suc- possible, an alternative procedure was recommended in
cinylcholine group. The emergency physicians conducting the accordance with the French Society of Anesthesia and Resus-
intubation procedures were blinded to the contents of the en- citation guidelines on difficult airway management, includ-
velope at the time of assigning an individual patient. ing gum elastic bougie, intubating laryngeal mask airway
(ILMA), or cricothyrotomy.16 If the patient was randomized to
Study Intervention the rocuronium group, the physician could subsequently
In both groups, sedation induction was performed after pre- choose to antagonize the action of the rocuronium with
oxygenation. Emergency physicians were asked to follow the sugammadex, a procedure recommended for patients impos-
French guidelines for sedation and analgesia in emergency sible to intubate under direct laryngoscopy and who could
departments.4 Two hypnotics were recommended. Etomi- neither be intubated nor ventilated by alternative techniques
date (0.3 mg/kg) or ketamine (2 mg/kg), with dosage based for difficult intubation. These airway practices were in accor-
on estimated patient weight, was injected followed immedi- dance with the French Society of Anesthesia and Resuscita-
ately by an intravenous bolus injection of either succinylcho- tion consensus guidelines on difficult airway management.16
line (1 mg/kg) or rocuronium (1.2 mg/kg), with dosage based Aside from the randomization for paralytic agent used
on estimated patient weight. The use of another hypnotic for the induction of sedation, there was no change from usual
(propofol or thiopenthal) was allowed, according to the phy- practices. In particular, hypotension was managed via fluid
sician's preference. The Sellick maneuver was recommended resuscitation with crystalloids and ephedrine and prolonged
jama.com (Reprinted) JAMA December 17, 2019 Volume 322, Number 23 2305
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Research Original Investigation Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation
hypotension was managed with continuous catecholamine Statistical Analysis
administration. Maintenance sedation after intubation was Characteristics at baseline were described by their frequency
performed according to the French Society of Anesthesia and and percentages for categorical variables and by means and SDs
Resuscitation recommendations and included administration or medians and interquartile ranges for quantitative vari-
of benzodiazepine or propofol and opioids. Doses of these ables. To take the randomization stratification factor (ie, the
agents were adapted by the physician to the patient's clinical center) into account, a generalized estimating equations model
status and the objectives of sedation, which vary according to with an identity link function was used to compare the groups
the pathology and the indication for mechanical ventilation. for the percentage of patients with a successful first-attempt
Each physician completed a paper case report form on- orotracheal intubation. Therefore, the center was included as
site. Later, to ensure the quality and completeness of the study the clustering factor and an exchangeable correlation matrix
data, a clinical research associate at each center verified the was specified. Based on this model, noninferiority was as-
case report form data from the source medical file on-site and sessed for the primary outcome by the 1-sided 97.5% CI of the
recorded the data to a centralized database. Patients were fol- absolute difference. As recommended for noninferiority stud-
lowed up until hospital admission. ies, a per-protocol analysis was conducted first.24,25 Patients
who received allocated treatment and for whom intubation was
Outcomes attempted were included in this analysis. An additional analy-
The primary outcome measure was the percentage of pa- sis was conducted that analyzed patients according to their ran-
tients with successful first-attempt orotracheal intubation as- domized group and included all patients who were random-
sessed by the physician and confirmed by a capnography curve ized and completed the trial.
consistent over 3 respiratory cycles. A noninferiority margin In an exploratory post hoc analysis, we performed 2 sub-
of 7% was selected. group analyses to investigate the treatment effect of the pri-
Secondary prespecified outcomes were (1) the Cormack- mary outcome based on patients’ conditions; 1 analysis was
Lehane grade of glottis visibility obtained by direct laryngos- stratified on reason for intubation and the other on patient po-
copy (range, 1-4; 1 indicates full view of glottis; 2, partial view sition at the time of intubation. Analyses included treat-
of glottis; 3, only epiglottis seen; and 4, neither glottis nor ment × subgroup interaction and the subgroup as covariates
epiglottis seen)17; (2) the overall difficulty of the intubation in a generalized estimating equations model defined for analy-
process, measured by the Intubation Difficulty Scale score ses of the primary outcome. The absolute difference between
(range, 0 to infinite; score >5 indicates difficult intubation)18; treatment groups and 1-sided 97.5% CIs were then estimated
(3) intubation conditions, assessed by the Copenhagen score from these models.
(poor, good, or excellent conditions)19; (4) the percentage of We compared secondary outcomes using generalized es-
patients intubated by alternative techniques (stylet, gum timating equations models with an identity link function. To
elastic bougie, ILMA [eg, Fastrach], or cricothyrotomy); and take into account potential nonindependence of patients in the
(5) intubation-related complications in the first 15 minutes same center, the center was included as the clustering factor
after intubation (cardiac arrest, arterial hypotension [systolic and an exchangeable correlation matrix was specified. Abso-
blood pressure <90 mm Hg], hypoxemia [occurrence of new lute differences and their 2-sided 95% CIs were derived from
oxygen desaturation <90%], physician-reported aspiration, these models. All tests for secondary outcomes were per-
severe arrhythmia [ventricular tachycardia, ventricular fibril- formed at a 2-tailed type I error of 5%, with a superiority hy-
lation], or allergic reaction). pothesis. Because of the potential for type I error due to mul-
Post hoc exploratory outcomes were the number of intu- tiple comparisons, findings for analyses of secondary end
bation attempts, the number of intubation failures under di- points should be interpreted as exploratory.
rect laryngoscopy, the time of out-of-hospital care, the num- The amount of missing data in this study was low. Analy-
ber of deaths during out-of-hospital care, the number of ses were performed on complete cases and no assumptions
unintentional extubations, and the amount of sedative drugs were made for the patterns of missing data. All analyses were
and vasopressors used after intubation. performed used SAS version 9.4 (SAS Institute). The statisti-
cal analysis plan is available in Supplement 3.
Sample Size
The sample size was calculated from the previous literature,
with an expected percentage of successful first-attempt oro-
tracheal intubation of 75% for patients in the succinylcho-
Results
line group.3,20,21 After assuming a noninferiority margin of Baseline Characteristics
7% based on out-of-hospital studies that focused on emer- A total of 1248 patients were enrolled in the study. Patients
gency intubation using the same main outcome, with a type were recruited between January 2014 and August 2016, with
I error of 5% and type II error of 20%, it was determined that final follow-up on August 31, 2016. Of the 1326 patients
602 patients were needed in each group (1204 overall).20-23 assessed for eligibility, 1248 were randomized (mean age, 56
We set targeted enrollment at 1300 patients to take into years; 501 [40.1%] women). Of the randomized patients, 1230
account risks of protocol deviations in this emergency ran- (98.6%) completed the trial and 1226 (98.2%) were included
domization context. Thus, we planned to include 650 in the per-protocol analysis (Figure 1). Patient characteristics
patients in each group. and clinical indications for intubation are reported in Table 1
2306 JAMA December 17, 2019 Volume 322, Number 23 (Reprinted) jama.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation Original Investigation Research
Table 1. Baseline Patient Data in a Study of the Effect of Rocuronium Table 1. Baseline Patient Data in a Study of the Effect of Rocuronium
vs Succinylcholine on Out-of-Hospital Endotracheal Intubation Success vs Succinylcholine on Out-of-Hospital Endotracheal Intubation Success
(continued)
No. (%)
Rocuronium Succinylcholine No. (%)
Characteristic (n = 610) (n = 616) Rocuronium Succinylcholine
Age, mean (SD), y 57.2 (18.7) 54.6 (19.1) Characteristic (n = 610) (n = 616)
Sex Patient position during intubation
Men 370 (60.7) 366 (59.3) Lying on a stretcher 324 (53.1) 307 (49.8)
Women 240 (39.3) 250 (40.7) Lying on the ground 161 (26.4) 187 (30.4)
BMI, mean (SD) 25.5 (5.4) 25.8 (5.1) Lying on a bed 112 (18.4) 110 (17.9)
Medical history Other 13 (2.1) 12 (1.9)
Hypertension 208 (35.9) 178 (30.1) Abbreviations: BMI, body mass index (calculated as weight in kilograms divided
(n = 580) (n = 592) by height in meters squared); IQR, interquartile range.
Smoking 151 (26.4) 127 (21.9) a
Coded by the emergency physician.
(n = 572) (n = 580)
b
Range, 3 (deep coma) to 15 (normal consciousness).
Alcoholism 112 (19.4) 107 (18.2)
(n = 576) (n = 589)
Cancer 55 (9.4) 42 (7.1)
(n = 582) (n = 593)
Coronary heart disease 51 (8.8) 42 (7.1)
(n = 580) (n = 592) and eFigure in Supplement 2 (74 patients with missing data).
Chronic obstructive 50 (8.6) 34 (5.7) Coma was the leading reason for intubation.
pulmonary disease (n = 578) (n = 592)
Heart failure 50 (8.6) 29 (4.9)
(n = 579) (n = 591) Primary Outcome
Chronic kidney failure 19 (3.3) 20 (3.4) The number of patients with successful first-attempt intuba-
(n = 580) (n = 591)
tion was 455 of 610 (74.6%) in the rocuronium group vs 489
Reason for intubationa
of 616 (79.4%) in the succinylcholine group, a difference of
Coma due to neurological disease 313 (51.3) 304 (49.4)
−4.8% (1-sided 97.5% CI, −9% to ⬁), which did not meet crite-
Coma due to self-poisoning 107 (17.5) 124 (20.1)
ria for noninferiority (margin of 7%; Figure 2). Additional analy-
Acute respiratory failure 101 (16.6) 71 (11.5) sis of patients according to their randomized group that in-
Trauma 51 (8.4) 52 (8.4) cluded all patients who were randomized and completed the
Shock 8 (1.3) 9 (1.5) trial is presented in the eTable 1 in Supplement 2. Subgroup
Other 30 (4.9) 56 (9.1) analyses for the primary outcome are reported in eTable 2 in
Characteristics at enrollment Supplement 2.
Glasgow Coma Scale score, 6.0 (3.0-8.0) 6.0 (3.0-8.0)
median (IQR)b
Heart rate, mean (SD), beats/min 99.4 (28.4) 95.6 (27.2) Secondary Outcomes
Among the secondary end points assessing tracheal intuba-
Respiratory rate, mean (SD), 21.4 (9.7) 21.1 (9.5)
breaths/min tion difficulty, there was no statistically significant between-
Arterial systolic pressure, mm Hg group difference for the mean (SD) Intubation Difficulty Scale
<90 47 (7.7) 37 (6.0) score (4.2 [2.9] for the rocuronium group vs 4.1 [2.4] for the
>140 258 (42.3) 227 (36.9) succinylcholine group; difference, 0.1 [95% CI, −0.2 to 0.4]).
Arterial diastolic pressure, mm Hg There was also no statistically significant difference in the
<50 43 (7.0) 35 (5.7) Copenhagen score between the groups; 327 of 580 (56.4%)
>90 193 (31.6) 168 (27.3) patients in the rocuronium group vs 313 of 584 (53.6%) in the
Peripheral oxygen saturation, 95.4 (6.8) 95.4 (7.5)
succinylcholine group had excellent intubation conditions
mean (SD), % (difference, 2.8 [95% CI, −0.5 to 6.4]) and 206 of 580 (35.5%)
Sedation given for intubation patients in the rocuronium group vs 222 of 584 (38.0%) in
Etomidate 536 (87.9) 543 (88.1) the succinylcholine group had good intubation conditions
Total dose, median (IQR), mg 30 (20-40) 30 (20-40) (difference, −2.5 [95% CI, −6.1 to 0.5]).
Ketamine 38 (6.2) 34 (5.5) There was no significant difference between the 2 groups
(n = 609) in the use of alternative intubation techniques, such as stylet
Total dose, median (IQR), mg 150 (67-190) 200 (125-250)
or gum elastic bougie, although significantly more patients in
Pentothal 21 (3.4) 19 (3.1) the rocuronium group had use of the ILMA, and 1 patient
(n = 609) (n = 615)
in the succinylcholine group underwent cricothyrotomy.
Total dose, median (IQR), mg 350 (200-400) 325 (250-400)
Intubation-related complications reported within 15 minutes
Propofol 21 (3.4) 21 (3.4)
after intubation were observed more frequently in patients in
Total dose, median (IQR), mg 60 (40-150) 150 (80-160)
the succinylcholine group than the rocuronium group (143 of
Combined administration, No. 6 1
616 [23.2%] vs 111 of 610 [18.2%]; absolute difference, −5%
(continued) [95% CI, −9.8% to −0.03%]; P = .04; Table 2).
jama.com (Reprinted) JAMA December 17, 2019 Volume 322, Number 23 2307
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Research Original Investigation Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation
Figure 2. Difference in Successful First-Attempt Intubation Rate Between Patients Given Rocuronium vs Succinylcholine While Undergoing
Out-of-Hospital Rapid Sequence Intubation
No. of Patients/Total No. (%)
Rocuronium Succinylcholine Absolute Difference Favors Favors
Group Group (1-Sided 97.5% CI), % Rocuronium Succinylcholine
Randomized group analysis 456/613 (74.4) 489/617 (79.2) –4.8 (–9.1 to ∞)
Per-protocol analysis 455/610 (74.6) 489/616 (79.4) –4.8 (–9.0 to ∞)
–15 –10 –5 0 5 10
Between-Group Difference in First-Attempt
Intubation Rate (1-Sided 97.5% CI), %
The dashed line represents the noninferiority margin of 7%. Because the CI lines go above the prespecified noninferiority margin of 7%, the null hypothesis that
succinylcholine is superior cannot be rejected.
Post Hoc Exploratory Outcomes ing room settings.28,29 To our knowledge only 1 randomized trial
Significantly more intubation attempts were required in has examined the intensive care setting, and none have exam-
the rocuronium group than in the succinylcholine group ined emergency departments or out-of-hospital settings.30
(Table 2). Six patients in the rocuronium group and 3 in the Accordingly, the systematic reviews of this comparison essen-
succinylcholine group died during out-of-hospital care. No tially analyze operating room studies only.12,29,31
deaths were attributed to difficult intubation. In the succinyl- For many years, succinylcholine has been the principal
choline group, 100 of 606 (16.5%) patients were treated with paralytic agent recommended for facilitating tracheal intuba-
norepinephrine during the immediate postintubation period, tion in patients needing out-of-hospital tracheal intubation.
compared with 60 of 604 (9.9%) in the rocuronium group One of the main characteristics of succinylcholine is its very
(difference, −6.6% [95% CI, −10.8% to −1.9%]; P < .001; quick onset, which enables optimal intubation conditions to
Table 3). Fifteen patients could not be intubated under direct be obtained in less than a minute after intravenous adminis-
laryngoscopy in the out-of-hospital care period. Among tration. Rocuronium, a nondepolarizing paralytic agent, has
them, 6 were intubated blindly through a laryngeal intuba- pharmacokinetic characteristics that provide optimal intuba-
tion mask. Six more were effectively ventilated by ILMA and tion conditions in almost the same time as succinylcholine, as
were intubated at the hospital. One patient had a cricothy- long as the dose administered is at least 1 mg/kg. For this rea-
rotomy and 2 patients were ventilated with a face mask until son, it has been proposed as an alternative paralytic agent when
arrival at the hospital (Table 2). Eleven of these 15 patients RSI is indicated.32
were assigned to receive rocuronium. Two patients received The primary end point chosen for this trial was the first-
sugammadex to antagonize rocuronium. Airway control was attempt intubation success rate. This criterion is often used in
obtained for 1 of these 2 patients by application of the recom- clinical studies assessing tracheal intubation in the emergency
mended algorithm; an intubating laryngeal mask was put in setting context because several studies of emergency intuba-
place and enabled effective mechanical ventilation until tions report that the complication rate related to airway con-
arrival at the hospital. For the second patient, sugammadex trol increases with the number of intubation attempts.33-36 It ap-
was injected after only 1 intubation attempt failure under pears to be a more relevant and direct criterion than intubation
direct laryngoscopy, without attempting any alternative tech- condition, measured by scores that take into account many ele-
nique. That is, this physician did not follow the recom- ments that may be difficult to accurately assess in the emer-
mended algorithm for difficult intubation for this patient. gency context, which was assessed here only as a secondary out-
The patient awoke 45 minutes later, and the final diagnosis come and did not differ significantly between the groups.
was status epilepticus. Nonetheless, none of the published meta-analyses that com-
pared succinylcholine with rocuronium used this primary end
point. Instead, all used intubation conditions considered to be
good or excellent as their primary outcome.
Discussion Design of a noninferiority study seemed necessary be-
This randomized clinical trial failed to demonstrate noninfe- cause succinylcholine has a tolerance profile that appears to
riority for the success rate of rocuronium compared with suc- be lower than that of rocuronium. The choice of a margin of
cinylcholine for first-attempt intubation in adult patients re- noninferiority is a major element when performing a nonin-
ceiving emergency intubation at a noninferiority margin of 7%. feriority study. For this study, determination of this value was
To our knowledge, this study is the first randomized clini- not straightforward because very little data have been pub-
cal trial comparing rocuronium and succinylcholine in emer- lished on this topic. No randomized trials have been con-
gency settings, even though reports indicate that emergency ducted in an emergency setting to compare succinylcholine and
physicians are adopting rocuronium as a standard practice, with rocuronium. All randomized trials were conducted in a hos-
some departments using this drug more often than pital setting, primarily in the operating room, and the pri-
succinylcholine.26,27 Most of the published trials comparing mary end point of these trials was the intubation conditions
these neuromuscular-blocking agents have examined operat- assessment and not the first-attempt intubation success rate.
2308 JAMA December 17, 2019 Volume 322, Number 23 (Reprinted) jama.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation Original Investigation Research
Table 2. Intubation Characteristics and Outcomes of Patients in a Study of the Effect of Rocuronium
vs Succinylcholine on Out-of-Hospital Endotracheal Intubation Success
No./Total No. (%)
Absolute Difference
Rocuronium Group Succinylcholine Group (95% CI), %a P Valueb
Primary Outcome
(Successful First-Attempt
Intubation)
Per-protocol analysis 455/610 (74.6) 489/616 (79.4) −4.8 (1-sided 97.5% CI,
−9.0 to ⬁)c
Randomized group analysis 456/613 (74.4) 489/617 (79.2) −4.8 (1-sided 97.5% CI,
−9.1 to ⬁)c
Secondary Outcomes
Prespecified analyses
Cormack-Lehane graded
I (best view) 375/609 (61.6) 346/616 (56.2) 5.4 (−0.3 to 10.9) .06
II 125/609 (20.5) 173/616 (28.1) −7.6 (−11.5 to −3.7) <.001 Abbreviation: IQR, interquartile
III 81/609 (13.3) 72/616 (11.7) 1.6 (−2.9 to 6.2) .49 range.
a
The estimated difference between
IV (worst view) 28/609 (4.6) 25/616 (4.0) 0.6 (−1.5 to 2.6) .60
the groups was calculated with a
Intubation Difficulty 4.2 (2.9) 4.1 (2.4) 0.1 (−0.2 to 0.4) .52 2-sided 95% CI using a generalized
Scale score, mean (SD)e
estimated equation model, in which
Intubation Difficulty 138/605 (22.8) 130/614 (21.2) 1.6 (−3.5 to 6.8) .53 center was specified as the
Scale score >5 clustering factor.
Copenhagen score b
(reflecting intubation Not corrected for multiple
conditions)f comparisons.
c
Excellent 327/580 (56.4) 313/584 (53.6) 2.8 (−0.5 to 6.4) .09 The estimated difference between
the groups was calculated with a
Good 206/580 (35.5) 222/584 (38.0) −2.5 (−6.1 to 0.5) .10
1-sided 97.5% CI using a generalized
Poor 47/580 (8.1) 49/584 (8.4) −0.3 (−3.0 to 2.6) .87 estimated equation model, in which
Need for alternative center was specified as the
intubation techniques clustering factor. The margin for
Stylet 55/610 (9.0) 51/616 (8.3) 0.7 (−1.9 to 2.0) .97 noninferiority was set at −7%. A
lower bound of the CI that did not
Gum elastic bougie 114/610 (18.7) 107/616 (17.4) 1.3 (−1.2 to 3.8) .31
exceed this margin indicated
Intubating laryngeal 10/610 (1.6) 2/616 (0.3) 1.3 (0.5 to 2.4) .003 noninferiority.
mask airway d
Reflects glottis visualization. Range,
Cricothyrotomy 0/610 (0.0) 1/616 (0.2) −0.2 (−0.5 to 0.2)
1-4; higher scores indicate less
Early intubation-related .04 glottis visualization.
complications e
Range, 0 (intubation without
Patients with at least 111/610 (18.2) 143/616 (23.2) −5 (−9.8 to −0.03) difficulty) to infinity; a value greater
1 complication
than 5 indicates difficult intubation.
Hypoxemia episodesg 55/610 (9.0) 61/616 (9.9) −0.9 (−4.4 to 2.6) f
The Copenhagen score is composed
Severe arrhythmiah 12/610 (2.0) 26/616 (4.2) −2.2 (−3.8 to −0.7) of 5 items with responses coded as
Cardiac arrest 22/609 (3.6) 13/615 (2.1) 1.5 (−0.1 to 3.3) “excellent,” “good,” or “poor”:
laryngoscopy (easy, fair, difficult),
Pulmonary aspirationi 19/610 (3.1) 21/616 (3.4) −0.3 (−1.7 to 1.1)
vocal cords position (abducted,
Hypotension episodesj 39/610 (6.4) 62/615 (10.1) −3.7 (−6.8 to −0.3) intermediate, closed), vocal cords
Exploratory analysesk movement (none, moving, closing),
movements of the tube during
No. of intubation 1.4 (0.8) 1.3 (0.6) 0.1 (0.05 − 0.2) <.001
attempts, mean (SD) insertion (none, slight, vigorous),
and coughing during tracheal tube
2 110/609 (18.1) 96/615 (15.6) 2.5 (−2.2 to 6.9) .31
insertion (none, diaphragm,
3 34/609 (5.6) 27/615 (4.4) 1.2 (−0.8 to 3.2) .23 sustained); intubation conditions
≥4 10/609 (1.6) 3/615 (0.5) 1.1 (0.2 to 2.0) .01 are defined as excellent if all items
are excellent, good if all items are
Intubation failure 11/610 (1.8) 4/616 (0.7) 1.1 (0.3 − 2.3) .01
under direct excellent or good, and poor if a
laryngoscopy single item is poor.
g
Time of prehospital care, 55 (38 to 78) 55 (39 to 80) −2.2 (−6.9 to 2.5) .35 Defined as any oxygen saturation
median (IQR), min reading of less than 90%.
Death during 6/608 (1.0) 3/615 (0.5) 0.5 (−0.4 to 1.3) .26 h
Ventricular tachycardia and
prehospital care
ventricular fibrillation.
Complications i
Visually detected by the physician
No. of complications 0 0 −0.09 (−0.17 to −0.08) .03 during laryngoscopy.
per patient, j
median (IQR) Defined as a new episode of
arterial systolic pressure of less
≥1 severe complication 115/608 (18.9) 150/615 (24.4) −5.5 (−10.8 to −0.05) .04
than 90 mm Hg.
Unintentional extubation 1/609 (0.2) 4/615 (0.6) 0.4 (−1.0 to 0.03) .06 k
Post hoc outcomes.
jama.com (Reprinted) JAMA December 17, 2019 Volume 322, Number 23 2309
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Research Original Investigation Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation
Table 3. Sedative and Vasopressor Use During the Postintubation Period in a Study of the Effect of Rocuronium
vs Succinylcholine on Out-of-Hospital Endotracheal Intubation Success
No. Who Received Some of the Agent/No. With Available Data (%)
Absolute Difference
Drug Rocuronium (n = 610) Succinylcholine (n = 616) (95% CI), %a,b
Hypnotics
Midazolam 521/610 (85.4) 546/616 (88.6) −3.2 (−5.9 to 0.4)
Total dose, 5.0 (4.0 to 10.0) 8.0 (5.0 to 13.0) −3.0 (−4.3 to −2.3)
median (IQR), mgc
No. of boluses, 1.3 (0.7) 1.5 (0.9) −0.2 (−0.3 to −0.02)
mean (SD)
Propofol 34/608 (5.6) 40/613 (6.5) −0.9 (−2.5 to 0.2)
Total dose, 133.0 (50.0 to 200.0) 200.0 (100.0 to 250.0) −52.3 (−98.9 to −6.0)
median (IQR), mgc
No. of boluses, 1.0 (1.0) 1.5 (1.4) −0.5 (−1.1 to 0.04)
mean (SD)
Analgesics
Fentanyl 50/610 (8.2) 48/614 (7.8) 0.4 (−0.1 to 1.8)
Total dose, 100.0 (50.0 to 200.0) 100.0 (67.5 to 200.0) −13.5 (−59.2 to 32.4)
median (IQR), μgc
No. of boluses, 0.9 (0.8) 1.4 (1.0) −0.3 (−0.4 to −0.2)
mean (SD)
Abbreviation: IQR, interquartile
Sufentanyl 491/610 (80.5) 513/616 (83.3) −2.8 (−6.3 to 0.7)
range.
Total dose, 15.0 (10.0 to 25.0) 20.0 (10.0 to 34.0) −8.0 (−12.0 to −4.0) a
The estimated difference between
median (IQR), μgc
the groups was calculated with a
No. of boluses, 1.2 (0.5) 1.5 (0.8) −0.3 (−0.4 to −0.2) 2-sided 95% CI using a generalized
mean (SD)
estimated equation model, in which
Vasopressors center was specified as the
Epinephrine 26/605 (4.3) 26/605 (4.3) 0.0 (−4.1 to 4.1) clustering factor.
b
Norepinephrine 60/604 (9.9) 100/606 (16.5) − 6.6 (−10.8 to −1.9) Not corrected for multiple
comparisons.
Dopamine 1/604 (0.2) 0/605 (0.0) 0.2 (−0.2 to 0.5)
c
Calculated only from patients who
≥1 vasopressor 77/604 (12.7) 121/608 (19.9) −7.2 (−11.0 to −2.8)
received the agent.
Some observational studies conducted in an emergency situ- cheal intubation was in place. The total dose of hypnotic ad-
ation compared the first-attempt intubation rate between pa- ministered during the out-of-hospital period differed between
tients who did vs patients who did not receive a paralytic agent, the groups because of more frequent bolus administration of
such as succinylcholine. The difference in first-attempt intu- sedative agents in the succinylcholine group. It appears likely
bation rate varies in these observational studies between 20% that in patients with frequent hemodynamic instability, using
and 17%, in favor of succinylcholine use.20,23 Therefore, in the a longer-acting paralytic agent might reduce the likelihood of
present study the standard comparator was succinylcholine the patient fighting the ventilator, which may lead emer-
and the new agent was rocuronium. As suggested for nonin- gency physicians to administer a bolus of midazolam or an opi-
feriority trials, the margin of noninferiority was set to less than oid to avoid adverse respiratory events.37
half of the difference previously reported for the first-
attempt intubation rate, depending on whether succinylcho- Limitations
line was used.25 This study has several limitations. First, this trial was not
While the results of the primary outcome analysis showed double-blinded, and the physician might have been influ-
that rocuronium cannot be considered noninferior to succi- enced by knowledge of which drug was administered. In emer-
nylcholine in terms of ease of intubation, fewer complica- gency situations, it would have been extremely difficult to mask
tions were observed with rocuronium. These results must be the fasciculations observed in more than 90% of individuals
interpreted cautiously. Cardiovascular complications, such as who receive succinylcholine. Moreover, the time between the
hypotension or cardiac arrhythmia, were more frequent after injection of the paralytic agent and the first tracheal intuba-
succinylcholine use. However, it should be noted that more tion attempt was not recorded. It is possible that patients in
deaths were recorded during the prehospital period of care in the rocuronium group might have been intubated before the
the rocuronium group, although this difference was not sta- recommended 60-second delay with incomplete paralysis,
tistically significant. Nearly all patients in both groups re- whereas the fasciculations most often indicated to physi-
ceived postintubation sedation, usually a hypnotic agent (gen- cians the effectiveness of paralysis after succinylcholine ad-
erally midazolam) and an opioid analgesic (most commonly ministration before the intubation attempt.
sufentanil). The total doses of opioids and midazolam admin- Second, these results were obtained in a specific physician-
istered were greater in the succinylcholine group, which might staffed out-of-hospital emergency medical system and may
have contributed to the higher frequency of hemodynamic dis- not be generalizable to a paramedical-based care system.
orders in that group. Continuous sedation began as soon as tra- Third, awareness phenomena was not evaluated. Nevertheless,
2310 JAMA December 17, 2019 Volume 322, Number 23 (Reprinted) jama.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation Original Investigation Research
all patients were sedated according to recommendations, most the sample size calculation was carried out starting from a hy-
often with a combination of an opioid and a benzodiazepine. pothesis of a first-attempt intubation success rate of 75% with
Fourth, only the early intubation-related complications dur- succinylcholine, whereas in the present study, a success rate
ing the out-of-hospital period were collected and later hospi- close to 80% was observed in the succinylcholine group. Ninth,
tal complications were not evaluated. Fifth, although a recom- the noninferiority margin of 7% that was selected was based
mended dose of 1 mg/kg of succinylcholine was used, a higher in part on an expert opinion, which can be considered as a
dose may have been given to patients, as suggested by some methodological limitation.
clinical studies that have reported higher intubation success
rates with administration of 1.5 mg/kg of succinylcholine.38
Sixth, because patients were intubated without use of a sty-
let or video laryngoscope and with only Macintosh metallic
Conclusions
blades, this limits the generalization of the results to other out- Among patients undergoing endotracheal intubation in a
of-hospital systems where these practices are widespread. Sev- medical-based out-of-hospital emergency care system,
enth, the number of intubations performed per year and per rocuronium, compared with succinylcholine, failed to dem-
physician and the number of years of practice for each physi- onstrate noninferiority with regard to first-attempt intuba-
cian who participated in this study were not reported. Eighth, tion success rate.
ARTICLE INFORMATION Hospitalier Universitaire de La Réunion Site Félix Role of the Funder/Sponsor: The funders had no
Accepted for Publication: October 16, 2019. Guyon, Saint-Denis, France (Ferdynus); Department role in the design and conduct of the study;
of Emergency, CHU de la Réunion, Université de la collection, management, analysis, and
Author Affiliations: Department of Emergency, Réunion, Réunion, France (Combes). interpretation of the data; preparation, review, or
CHU de la Réunion, Allée des Topazes, Saint Denis, approval of the manuscript; and decision to submit
Réunion, France (Guihard); Groupe Author Contributions: Dr Ferdynus had full access
to all of the data in the study and takes the manuscript for publication.
Hospitalo-Universitaire Henri Mondor, SAMU 94,
Assistance Publique-Hôpitaux de Paris, Créteil, responsibility for the integrity of the data and the Data Sharing Statement: See Supplement 4.
France (Chollet-Xémard); SMUR 95, Centre accuracy of the data analysis.
Hospitalier de Gonesse, Gonesse, France Concept and design: Guihard, Lakhnati, REFERENCES
(Lakhnati); Department of Anesthesia & Critical Ricard-Hibon, Adnet, Deutsch, Jabre, Huiart, 1. Jabre P, Avenel A, Combes X, et al. Morbidity
Care - SAMU, Assistance Publique - Hôpitaux de Ferdynus, Combes. related to emergency endotracheal intubation—a
Paris, Hôpital Necker-Enfants Malades, Université Acquisition, analysis, or interpretation of data: substudy of the KETAmine SEDation trial.
Paris Descartes, Paris, France (Vivien); Guihard, Chollet-Xémard, Lakhnati, Vivien, Broche, Resuscitation. 2011;82(5):517-522. doi:10.1016/j.
Département d'Anesthésie-Réanimation-SMUR, Savary, Ricard-Hibon, Marianne Dit Cassou, Wiel, resuscitation.2011.01.015
Hôpital Universitaire Lariboisière, AP-HP, Paris, Tissier, Loeb, Bounes, Rousseau, Huiart, Ferdynus,
Combes. 2. Adnet F, Minadeo JP, Finot MA, et al A survey of
France (Broche); Emergency Department, General sedation protocols used for emergency
Hospital of Annecy, Annecy, France (Savary); SMUR Drafting of the manuscript: Ricard-Hibon, Marianne
Dit Cassou, Deutsch, Rousseau, Ferdynus, Combes. endotracheal intubation in poisoned patients in the
de l'hôpital Beaujon, Clichy, France (Ricard-Hibon); French prehospital medical system. Eur J Emerg Med.
Department of Emergency, CHU de la Réunion, Critical revision of the manuscript for important
intellectual content: Guihard, Chollet-Xémard, 1998;5(4):415-419.
Réunion, France (Marianne dit Cassou); AP-HP,
Urgences-SAMU 93, Unité Lakhnati, Vivien, Broche, Savary, Adnet, Wiel, 3. Combes X, Jabre P, Jbeili C, et al. Prehospital
Recherche-Enseignement-Qualité, Hôpital Tissier, Loeb, Bounes, Jabre, Huiart, Ferdynus, standardization of medical airway management:
Avicenne, Bobigny, France (Adnet); Univ Lille, EA Combes. incidence and risk factors of difficult airway. Acad
2694 - Santé Publique: Epidémiologie et Qualité Statistical analysis: Huiart, Ferdynus. Emerg Med. 2006;13(8):828-834. doi:10.1197/j.
des Soins, Lille, France (Wiel); French National Obtained funding: Lakhnati, Savary, Combes. aem.2006.02.016
Out-of-Hospital Cardiac Arrest Registry Research Administrative, technical, or material support: 4. de La Coussaye JE, Adnet F; groupe d’experts
Group - Registre électronique des Arrêts Guihard, Vivien, Savary, Wiel, Bounes. Sfar–SFMU. Sedation and analgesia in emergency
Cardiaques, Lille, France (Wiel); Emergency Supervision: Guihard, Lakhnati, Savary, Adnet, structure: which sedation and/or analgesia for
Medicine Department and SAMU 59, Lille Jabre, Huiart, Ferdynus, Combes. tracheal intubation? [article in French]. Ann Fr
University Hospital, Lille, France (Wiel); Conflict of Interest Disclosures: Dr Huiart Anesth Reanim. 2012;31(4):313-321. doi:10.1016/j.
Department of Emergency Medicine, Groupe reported receiving grants from the French Ministry annfar.2012.01.008
Hospitalier Broca Cochin Hôtel-Dieu, Paris, France of Health during the conduct of the study and a 5. Bozeman WP, Kleiner DM, Huggett V.
(Deutsch); Department of Emergency Medicine, salary from University Hospital of La Réunion from A comparison of rapid-sequence intubation and
University Hospital Dijon, Dijon, France (Tissier); 2011 to 2017, Luxembourg Institute of Health since etomidate-only intubation in the prehospital air
Raymond Poincaré Hospital (APHP), SAMU 92, 2017, and University of La Réunion from 2016 to medical setting. Prehosp Emerg Care. 2006;10(1):8-
Paris, France (Loeb); Pôle Médecine d'Urgence, 2017 outside the submitted work. Dr Ferdynus 13. doi:10.1080/10903120500366854
Hôpital Universitaire de Purpan, Toulouse, France reported receiving grants from the French Ministry
(Bounes); INSERM UMR 1027, Université Paul of Health during the conduct of the study. 6. Okubo M, Gibo K, Hagiwara Y, Nakayama Y,
Sabatier, Toulouse, France (Bounes); Services de Dr Combes reported receiving grants from French Hasegawa K; Japanese Emergency Medicine
Médecine d’Urgence et de Réanimation, Pôle Ministry of Health during the conduct of the study. Network Investigators. The effectiveness of rapid
Urgence Réanimation, SAMU 77, Melun, France No other disclosures were reported. sequence intubation (RSI) versus non-RSI in
(Rousseau); AP-HP, Service d'Aide Médicale emergency department: an analysis of multicenter
Funding/Support: This study was supported by the prospective observational study. Int J Emerg Med.
d'Urgence (SAMU) de Paris and Paris Sudden Death Programme Hospitalier de Recherche Clinique 2012
Expertise Center, Université Paris Descartes, Paris, 2017;10(1):1. doi:10.1186/s12245-017-0129-8
of the French Ministry of Health. The Centre
France (Jabre); INSERM CIC 1410 Clinical and Hospitalier Universitaire de la Réunion is the key 7. Sakles JC, Laurin EG, Rantapaa AA, Panacek EA.
Epidemiology/ CHU Réunion/Université de la sponsor of this study and by delegation the Rocuronium for rapid sequence intubation of
Réunion, Saint-Pierre, Reunion, France (Huiart); Department of Clinical Research and Development emergency department patients. J Emerg Med.
Department of Population Health, Luxembourg supervises all work in accordance with the French 1999;17(4):611-616. doi:10.1016/S0736-4679(99)
Institute of Health, Strassen, Luxembourg (Huiart); public health code. 00046-3
Departement d'Informatique Clinique, Centre
jama.com (Reprinted) JAMA December 17, 2019 Volume 322, Number 23 2311
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
Research Original Investigation Effect of Rocuronium vs Succinylcholine on Successful Out-of-Hospital Rapid Sequence Intubation
8. Magorian T, Flannery KB, Miller RD. Comparison Anesthesiology. 1997;87(6):1290-1297. doi:10.1097/ 29. Tran DT, Newton EK, Mount VA, Lee JS, Wells
of rocuronium, succinylcholine, and vecuronium for 00000542-199712000-00005 GA, Perry JJ. Rocuronium versus succinylcholine for
rapid-sequence induction of anesthesia in adult 19. Viby-Mogensen J, Engbaek J, Eriksson LI, et al. rapid sequence induction intubation. Cochrane
patients. Anesthesiology. 1993;79(5):913-918. doi: Good clinical research practice (GCRP) in Database Syst Rev. 2015;(10):CD002788. doi:10.
10.1097/00000542-199311000-00007 pharmacodynamic studies of neuromuscular 1002/14651858.CD002788.pub3
9. Tang L, Li S, Huang S, Ma H, Wang Z. blocking agents. Acta Anaesthesiol Scand. 1996;40 30. Marsch SC, Steiner L, Bucher E, et al.
Desaturation following rapid sequence induction (1):59-74. doi:10.1111/j.1399-6576.1996.tb04389.x Succinylcholine versus rocuronium for rapid
using succinylcholine vs. rocuronium in overweight 20. Ricard-Hibon A, Chollet C, Leroy C, Marty J. sequence intubation in intensive care:
patients. Acta Anaesthesiol Scand. 2011;55(2):203- Succinylcholine improves the time of performance a prospective, randomized controlled trial. Crit Care.
208. doi:10.1111/j.1399-6576.2010.02365.x of a tracheal intubation in prehospital critical care 2011;15(4):R199. doi:10.1186/cc10367
10. Taha SK, El-Khatib MF, Baraka AS, et al. Effect medicine. Eur J Anaesthesiol. 2002;19(5):361-367. 31. Herbstritt A, Amarakone K. Towards
of suxamethonium vs rocuronium on onset of doi:10.1097/00003643-200205000-00008 evidence-based emergency medicine: best BETs
oxygen desaturation during apnoea following rapid 21. Jabre P, Galinski M, Ricard-Hibon A, et al. from the Manchester Royal Infirmary. BET 3: is
sequence induction. Anaesthesia. 2010;65(4): Out-of-hospital tracheal intubation with single-use rocuronium as effective as succinylcholine at
358-361. doi:10.1111/j.1365-2044.2010.06243.x versus reusable metal laryngoscope blades: facilitating laryngoscopy during rapid sequence
11. Patanwala AE, Stahle SA, Sakles JC, Erstad BL. a multicenter randomized controlled trial. Ann intubation? Emerg Med J. 2012;29(3):256-258. doi:
Comparison of succinylcholine and rocuronium for Emerg Med. 2011;57(3):225-231. doi:10.1016/j. 10.1136/emermed-2012-201100.4
first-attempt intubation success in the emergency annemergmed.2010.10.011 32. Higgs A, McGrath BA, Goddard C, et al; Difficult
department. Acad Emerg Med. 2011;18(1):10-14. doi: 22. Jabre P, Leroux B, Brohon S, et al. A comparison Airway Society; Intensive Care Society; Faculty of
10.1111/j.1553-2712.2010.00954.x of plastic single-use with metallic reusable Intensive Care Medicine; Royal College of
12. Tran DTT, Newton EK, Mount VAH, et al. laryngoscope blades for out-of-hospital tracheal Anaesthetists. Guidelines for the management of
Rocuronium vs. succinylcholine for rapid sequence intubation. Ann Emerg Med. 2007;50(3):258-263. tracheal intubation in critically ill adults. Br J Anaesth.
intubation: a Cochrane systematic review. doi:10.1016/j.annemergmed.2007.04.022 2018;120(2):323-352. doi:10.1016/j.bja.2017.10.021
Anaesthesia. 2017;72(6):765-777. doi:10.1111/anae. 23. Kociszewski C, Thomas SH, Harrison T, 33. Wang HE, Yealy DM. How many attempts are
13903 Wedel SK. Etomidate versus succinylcholine for required to accomplish out-of-hospital
13. Mallon WK, Keim SM, Shoenberger JM, intubation in an air medical setting. Am J Emerg Med. endotracheal intubation? Acad Emerg Med. 2006;
Walls RM. Rocuronium vs. succinylcholine in the 2000;18(7):757-763. doi:10.1053/ajem.2000.18033 13(4):372-377. doi:10.1197/j.aem.2005.11.001
emergency department: a critical appraisal. J Emerg 24. Piaggio G, Elbourne DR, Pocock SJ, Evans SJ, 34. Mort TC. Emergency tracheal intubation:
Med. 2009;37(2):183-188. doi:10.1016/j.jemermed. Altman DG; CONSORT Group. Reporting of complications associated with repeated
2008.07.021 noninferiority and equivalence randomized trials: laryngoscopic attempts. Anesth Analg. 2004;
14. April MD, Arana A, Pallin DJ, et al; NEAR extension of the CONSORT 2010 statement. JAMA. 99(2):607-613. doi:10.1213/01.ANE.0000122825.
Investigators. Emergency department intubation 2012;308(24):2594-2604. doi:10.1001/jama.2012. 04923.15
success with succinylcholine versus rocuronium: 87802 35. Sakles JC, Chiu S, Mosier J, Walker C, Stolz U.
a National Emergency Airway Registry study. Ann 25. Jones B, Jarvis P, Lewis JA, Ebbutt AF. Trials to The importance of first pass success when
Emerg Med. 2018;72(6):645-653. doi:10.1016/j. assess equivalence: the importance of rigorous performing orotracheal intubation in the
annemergmed.2018.03.042 methods. BMJ. 1996;313(7048):36-39. doi:10.1136/ emergency department. Acad Emerg Med. 2013;20
15. Perry JJ, Lee JS, Sillberg VA, Wells GA. bmj.313.7048.36 (1):71-78.
Rocuronium versus succinylcholine for rapid 26. April MD, Schauer SG, Brown Rd CA, et al. A 36. Hasegawa K, Shigemitsu K, Hagiwara Y, et al
sequence induction intubation. Cochrane Database 12-month descriptive analysis of emergency Association between repeated intubation attempts
Syst Rev. 2008;(2):CD002788. doi:10.1002/ intubations at Brooke Army Medical Center: and adverse events in emergency departments: an
14651858.CD002788.pub2 a National Emergency Airway Registry study. US analysis of a multicenter prospective observational
16. Langeron O, Bourgain JL, Laccoureye O, Legras Army Med Dep J. 2017(3-17):98-104. study. Ann Emerg Med. 2012;60(6):749-754.
A, Orliaguet G. [Difficult airway algorithms and 27. Johnson EG, Meier A, Shirakbari A, Weant K, 37. Jaffrelot M, Jendrin J, Floch Y, et al. Prevention
management: question 5. Société Française Baker Justice S. Impact of rocuronium and of awakening signs after rapid-sequence intubation:
d’Anesthésie et de Réanimation]. Ann Fr Anesth succinylcholine on sedation initiation after rapid a randomized study. Am J Emerg Med. 2007;25(5):
Reanim. 2008;27(1):41-45. doi:10.1016/j.annfar.2007. sequence intubation. J Emerg Med. 2015;49(1):43- 529-534. doi:10.1016/j.ajem.2006.09.016
10.025 49. doi:10.1016/j.jemermed.2014.12.028 38. Naguib M, Samarkandi AH, El-Din ME,
17. Cormack RS, Lehane J. Difficult tracheal 28. Sørensen MK, Bretlau C, Gätke MR, Sørensen Abdullah K, Khaled M, Alharby SW. The dose of
intubation in obstetrics. Anaesthesia. 1984;39(11): AM, Rasmussen LS. Rapid sequence induction and succinylcholine required for excellent endotracheal
1105-1111. doi:10.1111/j.1365-2044.1984.tb08932.x intubation with rocuronium-sugammadex intubating conditions. Anesth Analg. 2006;102(1):
18. Adnet F, Borron SW, Racine SX, et al. The compared with succinylcholine: a randomized trial. 151-155. doi:10.1213/01.ANE.0000181320.88283.BE
Intubation Difficulty Scale (IDS): proposal and Br J Anaesth. 2012;108(4):682-689. doi:10.1093/
evaluation of a new score characterizing the bja/aer503
complexity of endotracheal intubation.
2312 JAMA December 17, 2019 Volume 322, Number 23 (Reprinted) jama.com
© 2019 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a University Paris 5 Descartes User on 12/17/2019
You might also like
- 2015 355 Moesm1 EsmDocument3 pages2015 355 Moesm1 EsmIvan BurgosNo ratings yet
- 1 s2.0 S1879522611000054 MainDocument4 pages1 s2.0 S1879522611000054 MainIvan BurgosNo ratings yet
- Pediatria Integral XIX 9 - WEB PDFDocument98 pagesPediatria Integral XIX 9 - WEB PDFIvan BurgosNo ratings yet
- Characteristics of Children 2 To 5 Years of Age With Severe ObesityDocument10 pagesCharacteristics of Children 2 To 5 Years of Age With Severe ObesityIvan BurgosNo ratings yet
- National and State Trends in Sudden Unexpected Infant Death: 1990-2015Document9 pagesNational and State Trends in Sudden Unexpected Infant Death: 1990-2015Ivan BurgosNo ratings yet
- Patent Ductus Arteriosus in Preterm Infants: Clinical ReportDocument8 pagesPatent Ductus Arteriosus in Preterm Infants: Clinical ReportIvan BurgosNo ratings yet
- Congenital Colonic Atresia: Report of One CaseDocument4 pagesCongenital Colonic Atresia: Report of One CaseIvan BurgosNo ratings yet
- Characteristics of Children 2 To 5 Years of Age With Severe ObesityDocument10 pagesCharacteristics of Children 2 To 5 Years of Age With Severe ObesityIvan BurgosNo ratings yet
- BMCPeds - Problemas Relacionados Con Drogas enDocument7 pagesBMCPeds - Problemas Relacionados Con Drogas enIvan BurgosNo ratings yet
- 2017 Update On Pediatric Medical Overuse A ReviewDocument5 pages2017 Update On Pediatric Medical Overuse A ReviewIvan BurgosNo ratings yet
- Referencia Rápida - Control y Seguimiento de LaDocument16 pagesReferencia Rápida - Control y Seguimiento de LaIvan BurgosNo ratings yet
- Commentary: Fever of Unknown Origin: Where Science Meets ArtDocument4 pagesCommentary: Fever of Unknown Origin: Where Science Meets ArtIvan BurgosNo ratings yet
- Jpeds - Investigación Futura en El Sistema InmDocument6 pagesJpeds - Investigación Futura en El Sistema InmIvan BurgosNo ratings yet
- BMCPeds - Neurodesarrollo A Los 2 Años en HipoDocument6 pagesBMCPeds - Neurodesarrollo A Los 2 Años en HipoIvan BurgosNo ratings yet
- Propranolol 0.2% Eye Micro-Drops For RetinopatDocument12 pagesPropranolol 0.2% Eye Micro-Drops For RetinopatIvan BurgosNo ratings yet
- Solamente Amame (You Make Me Fe - Kathalee TruebaDocument18 pagesSolamente Amame (You Make Me Fe - Kathalee TruebaIvan BurgosNo ratings yet
- Fluid and Electrolyte Therapy in Newborns UpToDateDocument19 pagesFluid and Electrolyte Therapy in Newborns UpToDateIvan BurgosNo ratings yet
- Artritis Idiopática Juvenil-Pediatrics - in - Review33 (7) 303Document13 pagesArtritis Idiopática Juvenil-Pediatrics - in - Review33 (7) 303Ivan BurgosNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Applied Therapeutics/Mid Term ExamDocument16 pagesApplied Therapeutics/Mid Term ExamAmina AmiarNo ratings yet
- Sexual and Reproductive Health OverviewDocument7 pagesSexual and Reproductive Health OverviewmmjpgcilNo ratings yet
- Hypersensitivity 2Document3 pagesHypersensitivity 2kuldip.biotechNo ratings yet
- Drug StudyDocument5 pagesDrug StudyTracy Malingin QuimqueNo ratings yet
- Sensory Abnormalities in Children With Autism SpecDocument9 pagesSensory Abnormalities in Children With Autism SpecceavilaNo ratings yet
- Screening Tools For PostpartumDocument9 pagesScreening Tools For PostpartumNeni RochmayatiNo ratings yet
- The Thyroid SolutionDocument21 pagesThe Thyroid SolutionJosh Bill100% (1)
- 3a Competency Assessment - Patient Controlled AnalgesiaDocument2 pages3a Competency Assessment - Patient Controlled AnalgesiaQuijano GpokskieNo ratings yet
- Celebrity Parents Open Up About Raising Children With Special NeedsDocument4 pagesCelebrity Parents Open Up About Raising Children With Special NeedsBarathy ChandrasegranNo ratings yet
- Bijender Sindhu, DR - Manoj Sharma, DR - Raj K Biraynia. Comparison of Clinic and Home Based Exercise Programs After Total Knee Arthroplasty A Pilot StudyDocument12 pagesBijender Sindhu, DR - Manoj Sharma, DR - Raj K Biraynia. Comparison of Clinic and Home Based Exercise Programs After Total Knee Arthroplasty A Pilot StudyDr. Krishna N. SharmaNo ratings yet
- Homeopathic Remedy Pictures Vicki Mathison Frans Kusse.11789 - 1 PDFDocument19 pagesHomeopathic Remedy Pictures Vicki Mathison Frans Kusse.11789 - 1 PDFPrasanta ChatterjeeNo ratings yet
- Pediatric Surgery HandbookDocument75 pagesPediatric Surgery HandbookAlex Vătau100% (2)
- Rai Work Experience SheetDocument2 pagesRai Work Experience Sheetmark langcayNo ratings yet
- ASiT Conference Abstract Book, Belfast 2014Document68 pagesASiT Conference Abstract Book, Belfast 2014Ed FitzgeraldNo ratings yet
- Toxicology and Applied Pharmacology: Marina A. Dobrovolskaia, Michael Shurin, Anna A. ShvedovaDocument12 pagesToxicology and Applied Pharmacology: Marina A. Dobrovolskaia, Michael Shurin, Anna A. ShvedovaKarina EndoNo ratings yet
- PQ 168 MMR MSD Pi July2008Document7 pagesPQ 168 MMR MSD Pi July2008Charles AnthonyNo ratings yet
- Doctor List SL - No. Doctorcode Doctorname Qualification Grade CategoryDocument174 pagesDoctor List SL - No. Doctorcode Doctorname Qualification Grade CategoryumeshNo ratings yet
- 0501 Skin CareDocument9 pages0501 Skin CarekinayungNo ratings yet
- Professional, Ethical and Legal Issues of Nursing MNDocument15 pagesProfessional, Ethical and Legal Issues of Nursing MNJhoana Rose Joaquin SantosNo ratings yet
- Arogya Sanjeevni Policy 1 PDFDocument9 pagesArogya Sanjeevni Policy 1 PDFkrishna-almightyNo ratings yet
- English SbaDocument16 pagesEnglish SbaSatyanand Loutan100% (3)
- Use of Local Anesthesia For Pediatric Dental Patients: Latest RevisionDocument6 pagesUse of Local Anesthesia For Pediatric Dental Patients: Latest RevisionzainaNo ratings yet
- Scholarly PaperDocument6 pagesScholarly Paperapi-607036461No ratings yet
- NCP Cataract SurgeryDocument5 pagesNCP Cataract SurgeryKristaJaneCelmarBagcatNo ratings yet
- Acute Appendicitis PaperDocument6 pagesAcute Appendicitis Paperapi-279084200No ratings yet
- Classification in PsychiatryDocument19 pagesClassification in PsychiatrypaulraviNo ratings yet
- Description: Tags: 0422AppRecvdbySchbySource030404202003Document130 pagesDescription: Tags: 0422AppRecvdbySchbySource030404202003anon-201839No ratings yet
- On LeukemiaDocument28 pagesOn LeukemiaMeena Koushal100% (1)
- Treating Social Anxiety DisorderDocument6 pagesTreating Social Anxiety DisorderIago SalvadorNo ratings yet
- Perio-Prog Class 2012Document80 pagesPerio-Prog Class 2012moorenNo ratings yet