Professional Documents
Culture Documents
Fpsyg 09 02712
Uploaded by
Diego CabralOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fpsyg 09 02712
Uploaded by
Diego CabralCopyright:
Available Formats
ORIGINAL RESEARCH
published: 10 January 2019
doi: 10.3389/fpsyg.2018.02712
The Relationship Between PSG and
Morning/Evening Emotional
Parameters in Patients With Insomnia
Disorder and Good Sleepers
Bernd Feige*, Blanda Baumgartner, Dora Meyer and Dieter Riemann
Department of Clinical Psychology and Psychophysiology, Medical Center–University of Freiburg, Faculty of Medicine,
University of Freiburg, Freiburg, Germany
Objectives and Introduction: It is as yet unclear how polysomnographically determined
sleep parameters determine emotional well-being both generally and particularly in
patients with Insomnia Disorder (ID). ID is a frequent and disabling health condition
associated with both day- and nighttime hyperarousal, linked to negative sleep-related
ruminations as a cognitive component. Information on the immediate influence of
objective sleep quality on emotional parameters is important for therapeutic approaches.
Methods: The relationship between objective sleep parameters and two emotional
questionnaire items obtained both for evening and morning, relaxation and emotional
Edited by:
Nicola Cellini, balance, was determined for both sleep lab nights in 161 ID patients and 161 age and
Universit degli Studi di Padova, Italy gender matched good sleepers (retrospective sample from the Freiburg data base, 98
Reviewed by: female, 63 male in each group, age ID: 42.16 ± 11.55, GSC: 41.91 ± 11.30 years).
Louise Beattie,
University of Glasgow,
Multivariate mixed effects analysis, corrected for global influences of group, age and
United Kingdom first/second night, was employed to determine between- and within-subject influences
Melinda Jackson,
of sleep and emotional parameters.
RMIT University, Australia
*Correspondence: Results: Main effects: Within-subject, relaxation in the evening was strongly associated
Bernd Feige with sleep efficiency, REM latency and low arousal index in NREM sleep. No such
bernd.feige@uniklinik-freiburg.de
influence was significant for emotional balance. Also between subjects, evening
Specialty section: relaxation was related to increased sleep efficiency. Group interactions: Patients with
This article was submitted to larger relaxation values in the evening showed a larger reduction of the number of wake
Emotion Science,
periods and the awakening index in NREM sleep than GSC subjects.
a section of the journal
Frontiers in Psychology Discussion: Unexpectedly, no general influence of emotional balance on sleep was
Received: 07 September 2018 found. The subjective feeling of relaxation, however, was associated with sleep efficiency,
Accepted: 17 December 2018
Published: 10 January 2019
REM latency and low NREM sleep arousal index. While the first association may be
Citation:
obvious, a direct link to REM latency and NREM arousal index has not previously been
Feige B, Baumgartner B, Meyer D and shown. We could also directly observe that the number of wake periods in the PSG
Riemann D (2019) The Relationship
is more strongly influenced by evening relaxation in ID patients than in good sleepers,
Between PSG and Morning/Evening
Emotional Parameters in Patients With asserting the importance of sleep perception and attitude toward sleep in the therapeutic
Insomnia Disorder and Good process.
Sleepers. Front. Psychol. 9:2712.
doi: 10.3389/fpsyg.2018.02712 Keywords: PSG (Polysomnography), insomnia, emotion, questionnaire, good sleepers
Frontiers in Psychology | www.frontiersin.org 1 January 2019 | Volume 9 | Article 2712
Feige et al. PSG and Emotional Parameters in Insomnia
INTRODUCTION correlation between insomnia severity, restless REM sleep and
duration of emotional distress (specifically shame) overnight.
Theories of chronic insomnia emphasize the role of In the current study we aimed at the relationship between
cognitive, emotional, and physiological hyperarousal for its objective sleep parameters and more general emotional states as
development and maintenance (Harvey, 2002; Espie et al., rated using the SF-A sleep questionnaire (Schlaffragebogen-A,
2006). Own work (Riemann et al., 2010, 2011, 2012, 2015) Görtelmeyer, 1981).
summarized that hyperarousal processes seem to play a key This questionnaire is similar to a sleep diary in that it contains
role in its pathophysiology. Autonomous, neuroendocrine, evening and morning items filled for each night. It measures
neuroimmunological, electrophysiological, neuroimaging, and subjective quality of sleep, feeling recuperated after sleep,
psychological studies deliver converging evidence for increased psychological balance before going to sleep and psychosomatic
levels of arousal in ID without comorbidity compared to good symptoms during sleep. In addition, identical evening and
sleepers. Corresponding to the subjective experience of patients morning items are available for relaxation and emotional balance.
with insomnia having difficulties to “shut down” or to disengage Combined with sleep laboratory examinations, it therefore allows
from wakefulness (especially when trying to sleep), physiological to directly assess the relationship between the latter items—
data reflect increased levels of arousal both during day- and both state in the evening and change across the night with PSG
nighttime compared to good sleepers. It is assumed that the (polysomnographic) parameters. Relaxation can be viewed as
permanent hyperarousal in chronic insomnia—linked to habit inverse arousal, thereby providing a link to the hyperarousal
formation or alternatively to an (epi-) genetic lack in the ability to theories of insomnia. Emotional balance may provide an
down-regulate arousal (e.g., Palagini et al., 2014)—is triggered by assessment of the importance of emotional processes.
stressful life events and maintained by sleep-preventing learned Assessing two nights of every subject in addition allows
associations and maladaptive coping strategies (neurocognitive us to discriminate between- and within-subject, i.e., trait- and
model of insomnia as formulated by Perlis et al., 1997). state- like influences: Subjects generally reporting low emotional
Little is known on the concrete relationship between cognitive balance may, for example, show certain sleep characteristics by
and emotional state in the evening and in the morning and trait; this does not necessarily mean that targeting emotional
objective measures of sleep. It is well-known that in Insomnia balance therapeutically will change sleep as well. A within-subject
Disorder (ID) subjective sleep perception is often worse than relationship (between the nights) however, provides a better hint
objective sleep measures suggest, while healthy subjects tend to at a possible therapeutic pathway. At the same time we can
overestimate their sleep time (Carskadon et al., 1976; Frankel control for a first night effect, which itself is thought to result
et al., 1976; Edinger and Fins, 1995; Means et al., 2003). This bad from elevated arousal during the first night in a sleep laboratory
perception of sleep has been linked to qualitatively different REM (Agnew et al., 1966; Wauquier et al., 1991).
sleep (Feige et al., 2008, 2018; Riemann et al., 2012). The studies As most studies on sleep and emotion refer to subjective sleep
on sleep perception are based upon subjective assessments in the data, the aim of this study was to explore potential relationships
morning after a sleep night. When assessing state variables such between subjective emotional states (relaxation and emotional
as cognitive and emotional state, however, two different aspects balance) and objective sleep patterns in ID ad GSC using data
are equally important: The state at bedtime (evening) and the from first and second night’s sleep assessed at the sleep laboratory.
state change from evening to morning. The state at bedtime may
influence sleep in the successive night, while the state change MATERIALS AND METHODS
across the night may be influenced by the objective characteristics
of sleep. Participants and Procedure
Sleep and affective phenomena have been linked before. Patients With Insomnia Disorder (ID)
People suffering from ID often do not feel refreshed and This comparative observational study was based on a chart
feel impaired in relevant areas of life as stated in DSM-IV and data review of clinical patients with insomnia complaints
(American Psychiatric Association, 2000) and DSM-5 (American evaluated between 1995 and 2012 at the sleep center of
Psychiatric Association, 2013). They also report worse mood than the Department of Psychiatry and Psychotherapy, Freiburg
healthy controls and negative mood in ID correlates positively University Medical Center. During this period, 304 patients had
with subjective sleep latency (Buysse et al., 2007). Additionally, been examined for two nights and diagnosed with Insomnia
epidemiological studies show that insomnia increases the risk Disorder (ID; to ensure continuity, the diagnosis was primary
of developing depression (Baglioni et al., 2011) and anxiety insomnia after DSM-IV before DSM-5 and ID after DSM-5
disorders (Morphy et al., 2007; Neckelmann et al., 2007). A model thereafter, with exclusion criteria ensuring that this corresponded
by Walker (2009) allows to explain this relationship between to primary insomnia after DSM-IV).
sleep and affective disorders. He suggests that sleep plays a crucial All patients had been referred from their primary care
role in emotion regulation and that memories and emotion physician or medical specialist for evaluation of their sleep
are disentangled during sleep. If this disentanglement does complaint. Two weeks before consultation in our outpatient
not work properly, the risk of developing chronic anxiety and sleep disorders clinic, patients received a questionnaire screening
depression increases. Wassing et al. (2016) examined correlations package by mail which included, among others, the Beck
between REM sleep disruption, hyperarousal, insomnia, and Depression Inventory (BDI, Beck and Steer, 1987; German
the resolution of emotional distress. They found a positive version by Hautzinger et al., 1994) and the Pittsburgh Sleep
Frontiers in Psychology | www.frontiersin.org 2 January 2019 | Volume 9 | Article 2712
Feige et al. PSG and Emotional Parameters in Insomnia
Quality Index (PSQI, Buysse et al., 1989; German version by The final matched sample consisted of 63 men and 98 women
Riemann and Backhaus, 1996, see below). During the 1-h intake of each group aged 42.16 ± 11.55 years (ID, 19–67 years) and
interview in the outpatient facility, patients were interviewed 41.91 ± 11.30 years (GSC, 20–69 years). The age distribution did
about: onset and duration of insomnia, sleep habits as well not differ (Wilcoxon W = 13122, p = 0.847).
as history of medical illnesses, psychiatric disorders, use of
medication, drugs, tobacco and alcohol, sleep disorders in first Polysomnography
degree relatives (parents, siblings, and children) as well as All polysomnographic investigations were carried out using a
education and social background. standardized procedure. All subjects underwent two consecutive
A preliminary diagnosis was given on the basis of this nights of PSG sleep monitoring. Sleep was recorded on 14-
interview and a decision was made about the necessity of a sleep channel Nihon-Kohden EEG-polysomnographs for 8 h from
laboratory examination (e.g., in case of: chronicity, persistence “lights out” (23:00 h) until “lights on” (7:00 h) and digitized at a
of insomnia despite adequate therapy, suspicion of possible rate of 200 Hz. All recordings included EEG (C3A2; C4A1), EOG
underlying organic causes). Patients were then scheduled for (horizontal and vertical) and EMG (submental) and were scored
a PSG evaluation approximately 4 to 8 weeks after the first visually by experienced raters according to Rechtschaffen and
outpatient contact. Kales (1968) criteria. Inter-rater reliability is regularly evaluated
During their 2-day stay in the sleep center, all patients and ensured to be above 0.9 as part of laboratory routine. During
underwent a thorough physical, psychiatric (repeating the first night, all subjects were screened for apneas and periodic
the interview taken 4–8 weeks earlier) and neurological leg movements by monitoring abdominal and thoracic effort,
examination, routine blood tests (blood cell count, liver, renal, nasal airflow, oxymetry, and bilateral tibialis anterior EMG.
and thyroid function), ECG, EEG, and urine drug screen Sleep recordings were evaluated for the following parameters
(opiates, barbiturates, benzodiazepines, amphetamines and of sleep continuity and architecture: total sleep time (TST), sleep
cannabis, and viral/bacterial infection). efficiency (SEI): ratio of TST to time in bed (TIB) x 100%;
Exclusion criteria for the present data analysis were: Presence sleep onset latency (SOL): time from lights out until sleep onset
of any other sleep disorder (e.g., sleep apnea syndrome, (defined as first epoch of stage N2). Arousals were analyzed
restless-legs syndrome, narcolepsy, circadian rhythm disorders, according to the criteria of the American Sleep Disorders
organic or psychiatric insomnia as defined by DSM-IV); A Association (Sleep Disorders Atlas Task Force of the American
sleep apnea-/PLMS (period leg movements in sleep)-index with Sleep Disorders Association, 1992). The arousal index is the
arousal ≥ 5.0/TST (total sleep time); Clinically relevant medical number of arousals per hour. We evaluated both the arousal
or neurological disorders or a positive urine drug screen; index within TST and sleep stage specific indices (stage N2,
Consumption of hypnotic medication or medication known to REM). In addition, short awakenings within N2 and REM sleep
affect sleep in the 2 weeks before or during sleep laboratory were captured accordingly as awakening index. Sleep architecture
examination; Pregnancy; Any history of psychiatric disorder, of variables included: amounts of stages wake (W), N1, N2, slow
serious medical illness (e.g., hepatitis), substance abuse or shift wave sleep (SWS), and REM expressed as percentage of sleep
work in the past. period time (SPT: time from sleep onset until final awakening).
During the two nights of sleep laboratory examinations REM sleep variables were REM latency (time from sleep onset
patients had to refrain from alcohol. Decaffeinated coffee was until the first epoch of REM sleep, possible wake time not
only allowed in the morning for breakfast (maximum: two cups). counted) and REM density, calculated as the ratio of 3 s REM
179 patients with confirmed insomnia disorder (ID) fulfilling mini-epochs including rapid eye movements (REMs) to the total
the in- and exclusion criteria were finally eligible for statistical amount of REM mini-epochs x 100%. REMs were defined using
analysis. separate vertical and horizontal EOG traces, requiring a steepness
of excursions of at least 70 µV/s.
Good Sleeper Controls (GSC)
One hundred and ninety-eight good sleeper controls (GSC) were Subjective Sleep Scales
available for the current study. They were selected retrospectively The PSQI (Buysse et al., 1989; Riemann et al., 1996) assesses sleep
from our database of healthy subjects who participated in healthy habits and quality in the preceding 2 weeks. Variables reported
volunteer studies of our sleep center. Control subjects underwent for group descriptives are the subjectively reported sleep onset
the same routine procedure of examinations as ID patients latency, total sleep time, and (derived) sleep efficiency as well
to ensure physical and psychiatric health. In addition to the as the PSQI sum score (ranging from 0 to 21, highest values
exclusion criteria applying to the patients, good subjective sleep denoting severely impaired sleep).
quality was required to be reflected in a PSQI sum score below 6. The SF-A (Schlaffragebogen-A, Görtelmeyer, 1981, in its
Medical problems including sleep apnea or restless legs syndrome revised form Görtelmeyer, 2011) captures subjective aspects of
were excluded. Written informed consent was obtained from all sleep in the preceding night. It was administered in the morning
healthy subjects prior to the investigation in the sleep center. after each sleep recording, after subjects were awake for some
minutes. The questionnaire contains subjective estimates of wake
Matched Groups for Final Analysis times (SOL and wake after sleep onset, WASO) as well as the
From the ID and GSC groups described above, 161 ID patients frequency of awakenings. Of the additional 5-level items (values
and 161 GSC subjects could be matched using automated pair 1-5) asked regarding to experiences in the evening prior to sleep
matching for gender and mean age within each gender group. and in the morning after sleep, “relaxation” and “emotional
Frontiers in Psychology | www.frontiersin.org 3 January 2019 | Volume 9 | Article 2712
Feige et al. PSG and Emotional Parameters in Insomnia
balance” are formulated identically for evening and morning balance. Only the terms involving the target variables alone and
and therefore can be directly compared. Both items are part their GROUP interactions are reported. The remaining terms are
of the SF-A factor scales “psychological balancedness in the regarded as nuisance effects in this analysis. This pertains to the
evening” and “feeling of recuperation in the morning. ”The terms identical to the previous, more descriptive model (Table 2)
German term “Ausgeglichenheit” translated here as “balance” and the NIGHT interactions.
or “balancedness” means absence of disturbing thoughts or The rationale for using evening scores and differences across
emotions and could also be translated as “calmness of the mind. the night instead of evening and morning scores was that evening
”The questions are “how relaxed/how emotionally balanced did and morning scores can be expected to be related to some
you/do you feel”. The relationship of these two variables with degree; also, the difference across the night can be hypothesized
PSG sleep is the major topic of this study. Descriptive subjective to be determined by some property of the intervening sleep. If
sleep quality data for both groups is given in Table 1. evening and morning scores were entered independently into an
analysis, this important change aspect would be reflected only in
Statistical Analysis an interaction term of these covariates, rendering analysis and
Two-tailed non-parametric Wilcoxon tests were employed to conclusions more complex.
ensure that the groups did not systematically differ in age. All statistical analyses were performed using the statistical
χ 2 tests were used to compare dichotomous variables between software suite “R” version 3.5.1 (R Core Team, 2018).
groups. For descriptive purposes, means and standard deviations
were calculated for PSG and subjective sleep parameters. Group
differences (ID vs. GSC), night (first, second) and age effects were RESULTS
assessed using mixed-effects MANOVAs with between-subject
factor GROUP and covariate AGE as well as within-subject factor Main Effects for Group, Night, and Age
NIGHT. Multivariate statistics were based on Wilk’s Lambda. P < Table 2 shows the more descriptive MANOVAs separately for the
0.05 was considered to be significant, proceeding from significant PSG variables and the target variables relaxation and emotional
multivariate effects to univariate effects of the same independent balance. For PSG, multivariate effects are seen for GROUP,
variable. For univariate effects, we report F and p values as well as NIGHT, and AGE but not NIGHT x GROUP. The GROUP
B values (betas) of the linear model, i.e., coefficients or differences effect shows the typical reductions in total sleep time (TST)
between factor levels. For the NIGHT effect this is Night2-Night1 and sleep efficiency index (SEI) in the ID group as well as an
and for the GROUP effect ID-GSC. increased awakening index in NREM sleep. The NIGHT effect
For the main analysis of the influence of relaxation and shows reduced sleep onset latency (SOL), increased TST and SEI,
emotional balance which were assessed before and after each reduced number of wake periods (NWP) as well as arousal and
night, mixed-effects MANOVAS were used with between-subject awakening indices in NREM sleep (AI/N and AWI/N) in the
factor GROUP and covariate AGE as well as within-subject second relative to the first night. Increased AGE is associated
factor NIGHT and covariates morning values as well as changes with reduced TST and SEI, increased NWP as well as increases
across the night (morning-evening) of relaxation and emotional in arousal and awakening indices in both NREM and REM sleep.
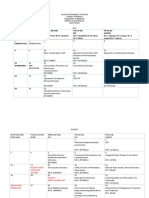
TABLE 1 | Descriptives of subjective sleep quality for both groups.
GSC ID Group Age
Mean ± SD Mean ± SD B F p B F p
Multivariate statistics 0.36 0.000 0.85 0.000
(Wilk’s Lambda)
PSQI SOL 14.25 ± 10.93 41.89 ± 47.50 27.39 42.11 0.000 0.16 0.71 0.401
TST 431.69 ± 56.28 302.17 ± 88.38 −126.30 216.97 0.000 −1.45 13.99 0.000
SEI 87.79 ± 25.03 60.31 ± 26.19 −27.86 242.58 0.000 −0.16 4.20 0.041
PSQI sum score 3.68 ± 2.12 10.96 ± 3.37 7.23 461.27 0.000 0.02 2.70 0.101
SF-A SOL 11.35 ± 11.32 22.20 ± 17.90 10.86 36.50 0.000 0.08 1.00 0.317
TST 452.92 ± 29.85 408.01 ± 61.61 −44.95 58.30 0.000 −0.29 1.20 0.274
SEI 94.25 ± 6.13 84.90 ± 12.80 −9.35 58.43 0.000 −0.05 1.01 0.315
SQ 3.58 ± 0.67 2.90 ± 0.74 −0.69 67.28 0.000 −0.01 3.03 0.083
R_MOR 3.60 ± 0.72 2.80 ± 0.82 −0.84 82.36 0.000 0.01 5.35 0.021
WB_EVE 3.92 ± 0.64 3.53 ± 0.66 −0.41 27.67 0.000 0.00 0.00 0.964
EX_EVE 2.60 ± 0.67 2.92 ± 0.70 0.29 11.88 0.001 −0.01 2.99 0.085
PS 1.49 ± 0.48 1.87 ± 0.47 0.38 52.92 0.000 0.01 13.50 0.000
The SF-A of the second night is used. For the Group effect, B=ID-GSC. GSC, Good Sleeper Controls; ID Patients with Insomnia Disorder; PSQI, Pittsburgh Sleep Quality Index; min,
Minutes; SOL, Sleep Onset Latency; TST, Total Sleep Time; SEI, Sleep Efficiency Index %; SF-A, Schlaffragebogen-A; SQ, Sleep Quality; R_MOR, Recovery in the morning; WB_EVE,
Wellbeing in the evening; EX_EVE, Exhaustion in the evening; PS, Psychosomatic Symptoms. p values below p = 0.05 are set in bold font.
Frontiers in Psychology | www.frontiersin.org 4 January 2019 | Volume 9 | Article 2712
TABLE 2 | Characteristics of PSG data and the variables on relaxation and emotional balance.
Adaptation night Baseline night Effects
Feige et al.
GSC ID GSC ID Group Night Night x Group Age
Mean ± SD Mean ± SD Mean ± SD Mean ± SD B F p B F p B F p B F p
Multivariate statistics 0.84 0.000 0.55 0.000 0.96 0.714 0.66 0.000
(Wilk’s Lambda)
SOL (min) 22.87 ± 19.86 25.39 ± 22.10 17.44 ± 15.38 15.85 ± 11.97 0.45 0.08 0.778 −5.43 45.49 0.000 −4.11 3.42 0.065 0.05 0.55 0.461
TST (min) 391.71 ± 51.29 361.24 ± 64.06 419.22 ± 33.04 396.90 ± 47.24 −26.08 33.75 0.000 27.51 125.10 0.000 8.15 2.08 0.150 −1.29 41.57 0.000
SEI (%) 81.61 ± 10.58 75.35 ± 13.27 87.33 ± 6.85 82.67 ± 9.81 −5.40 33.71 0.000 5.72 125.86 0.000 1.61 1.92 0.167 −0.27 42.61 0.000
NWP 29.27 ± 13.80 31.68 ± 14.95 27.50 ± 14.34 29.56 ± 14.57 2.14 2.65 0.105 −1.77 8.41 0.004 −0.35 0.07 0.795 0.39 42.72 0.000
Frontiers in Psychology | www.frontiersin.org
W (%SPT) 12.95 ± 9.08 17.92 ± 11.92 8.49 ± 5.61 12.68 ± 9.39 4.52 30.85 0.000 −4.46 83.18 0.000 −0.78 0.54 0.461 0.26 50.73 0.000
N1 (%SPT) 9.30 ± 4.92 9.98 ± 4.92 8.02 ± 4.65 8.64 ± 4.22 0.62 2.05 0.153 −1.28 44.32 0.000 −0.06 0.02 0.877 0.14 47.00 0.000
N2 (%SPT) 51.96 ± 8.43 50.39 ± 9.51 54.93 ± 7.24 53.04 ± 9.12 −1.71 4.04 0.045 2.98 44.52 0.000 −0.32 0.14 0.706 −0.07 3.38 0.067
N3 (%SPT) 7.02 ± 6.55 5.05 ± 5.81 7.97 ± 6.78 6.24 ± 7.06 −1.80 8.01 0.005 0.94 26.04 0.000 0.24 0.33 0.566 −0.20 50.39 0.000
REM (%SPT) 18.44 ± 5.44 16.55 ± 5.44 20.39 ± 4.91 19.25 ± 4.57 −1.49 10.10 0.002 1.94 71.57 0.000 0.76 1.90 0.169 −0.12 31.20 0.000
REML (min) 101.51 ± 48.39 107.84 ± 60.51 76.50 ± 33.55 72.94 ± 30.44 1.34 0.13 0.719 −25.01 86.81 0.000 −9.89 2.37 0.125 0.16 0.88 0.348
REMD (%) 24.96 ± 7.51 25.97 ± 8.77 25.36 ± 7.83 26.94 ± 7.41 1.30 2.61 0.107 0.40 3.54 0.061 0.58 0.63 0.429 −0.04 1.32 0.252
AI/REM 18.19 ± 9.32 18.50 ± 9.38 17.59 ± 9.10 17.76 ± 9.03 0.22 0.07 0.795 −0.60 2.41 0.121 −0.14 0.03 0.872 0.09 4.47 0.035
AI/N 12.30 ± 6.23 13.72 ± 7.95 10.33 ± 5.52 10.91 ± 6.07 0.98 2.28 0.132 −1.97 74.12 0.000 −0.85 2.34 0.127 0.09 9.83 0.002
AWI/REM 3.49 ± 3.78 3.66 ± 3.33 3.58 ± 3.69 3.75 ± 3.46 0.16 0.25 0.620 0.09 0.24 0.624 −0.01 0.00 0.985 0.06 13.94 0.000
5
AWI/N 3.90 ± 1.78 4.37 ± 2.20 3.38 ± 1.76 3.68 ± 1.89 0.38 4.67 0.031 −0.52 39.24 0.000 −0.16 0.73 0.393 0.05 39.06 0.000
Multivariate statistics 0.76 0.000 0.91 0.000 0.96 0.019 0.96 0.006
(Wilk’s Lambda)
Relaxation Evening 3.80 ± 0.77 3.22 ± 0.90 3.84 ± 0.81 3.48 ± 0.80 −0.47 36.28 0.000 0.04 9.19 0.003 0.21 4.61 0.033 0.00 0.34 0.560
Em.Balance Evening 3.87 ± 0.78 3.47 ± 0.87 3.93 ± 0.83 3.45 ± 0.91 −0.44 29.63 0.000 0.06 0.19 0.662 −0.07 0.47 0.492 0.01 3.54 0.061
Relaxation M-E −0.09 ± 0.91 −0.49 ± 1.12 −0.01 ± 0.90 −0.39 ± 0.90 −0.39 22.23 0.000 0.08 1.71 0.192 0.02 0.02 0.892 0.00 1.65 0.200
Em.Balance M-E −0.10 ± 0.85 −0.47 ± 1.04 0.01 ± 0.81 −0.16 ± 0.95 −0.27 11.06 0.001 0.11 10.53 0.001 0.20 2.55 0.111 0.01 3.16 0.077
For the Group effect, B=ID-GSC. For the Night effect, B=Night 2 - Night 1. p values below p = 0.05 are set in bold font.
January 2019 | Volume 9 | Article 2712
PSG and Emotional Parameters in Insomnia
Feige et al. PSG and Emotional Parameters in Insomnia
Target Variables (Relaxation and Emotional DISCUSSION
Balance)
For the target variables (lower part of Table 2), all multivariate In the current study, we reported an extensive multivariate
effects are significant. Patients with ID show reductions in analysis of the relationship between relaxation and emotional
all four variables (relaxation and emotional balance, both balance in a large population of patients with insomnia and
evening values and differences morning-evening). In the matched healthy controls.
second night, relaxation in the evening and the emotional The level of relaxation, particularly in the evening, was found
balance difference morning-evening are increased. As evidenced to enhance sleep both between subjects and within subjects. This
by the NIGHT x GROUP effect, the increase in evening suggests that relaxation can be an important therapeutic target
relaxation across nights was significantly higher in ID patients. for treating sleep problems.
Finally, age tended to increase both emotional balance in A single significant group interaction was identified: Evening
the evening and its morning-evening difference, not reaching relaxation reduced the number of wake periods and, specifically,
significance. the awakening index in NREM sleep more strongly in
patients with insomnia disorder. In fact, relaxation techniques
are important components in current cognitive-behavioral
Between-Subject Effects treatments for insomnia (CBT-I, Trauer et al., 2015; Riemann
Table 3 shows the between-subject relationships between the et al., 2017a,b; Friedrich and Schlarb, 2018), although clearly
target variables and PSG, i.e., whether subjects with different only responsible for part of its therapeutic efficacy (Norell-Clarke
sleep characteristics tend to also show different values on et al., 2015). Bertisch et al. (2012) have found that relaxation
relaxation and emotional balance. Multivariate significance is techniques are generally under-used for sleep problems in the
seen for evening relaxation and the evening relaxation x GROUP general population. However, the therapeutic effect of relaxation
interaction. Subjects with larger evening relaxation show reduced alone may not be sustainable, requiring other components of
SOL and increased TST, SEI, and stage N3 % SPT. Patients with CBT-I for a lasting effect.
larger evening relaxation show reduced NWP and awakening The level of emotional balance as assessed by the SF-
index in NREM sleep (AW/N) relative to the control group. A could not be linked to objective sleep parameters in this
Figures 1, 2 show the relationship between evening relaxation multivariate analysis. This is interesting by and of itself, as ID
and SEI as well as NWP, respectively. patients showed clearly reduced levels of emotional balance as a
group, an effect which has been partialled out of the emotional
Within-Subject Effects balance—PSG relationships in our analysis. Therefore, the
Table 4 shows the within-subject relationships between the finding means that, within each group, differences in emotional
target variables and PSG, i.e., whether nights with different balance were related to PSG parameters neither between- nor
sleep characteristics within the same subject tend to show within subjects. It is well-known that emotional reactivity is
different values on relaxation and emotional balance. This impaired in insomnia, as well as some aspects of emotional
is generally more valuable than between-subject effects, since valence (sleep in good sleepers being distinguished by increased
possible different response tendencies across subjects are factored positive but not necessarily reduced negative emotions; Baglioni
out and within-subject effects are more suitable to predict et al., 2010). Since these were group studies comparing insomnia
treatment effects. patients to good sleepers and the current study found clear
Across groups, relaxation in the evening was strongly related group differences in SF-A emotional balance as well, it may
to within-subject PSG sleep quality: Reduced SOL, increased still be that the latter construct captures the deficiencies in
TST and SEI as well as REM % SPT and REM latency (REML) emotional processing characteristic to insomnia to some degree.
and a reduced arousal index in NREM sleep were related to In this case the current finding could be extended to emotional
increased evening relaxation. The awakening index in REM reactivity and valence as well. This in turn would indicate that
sleep was, surprisingly, slightly positively related to evening targeting emotional reactivity, valence or balance itself would
relaxation. rather not present a viable therapeutic approach. Further studies
Unexpectedly, the influence of the Morning-Evening making this link explicit are, however, needed to support this
relaxation difference is for the most part of opposite direction conclusion.
to the evening value, albeit with lower amplitude. This indicates Generally, mutual relationships between sleep and emotions
that evening relaxation is more important than morning have to be considered (Kahn et al., 2013). Complicating the
relaxation; with the scores limited between 1 and 5, a positive matter further, reappraisal processes may be involved (cf. Palmer
Morning-Evening difference can only be attained if the evening and Alfano, 2017), for example general dissatisfaction with sleep
relaxation value is less than 5, associated with a negative impact leading to more negative responses to any sleep-related question.
on sleep quality. Figure 3 shows these relationships graphically This could be a potential mechanism for the more negative
for the example of SEI. judgments on both the relaxation and emotional balance scale in
No other main effects or interactions reached significance, ID patients (Table 3).
particularly no relationship could be found between Wassing et al. (2016) reported that the overnight resolution of
the scales of emotional balance and any PSG sleep emotional distress contributes to hyperarousal. They specifically
parameter. targeted shame. Overnight resolution of emotional distress
Frontiers in Psychology | www.frontiersin.org 6 January 2019 | Volume 9 | Article 2712
TABLE 3 | Between-subject effects of relaxation and emotional balance variables.
Between
Feige et al.
Evening Morning–Evening Evening x Group Morning–Evening x Group
Relaxation Emotional balance Relaxation Emotional balance Relaxation Emotional balance Relaxation Emotional balance
B F p B F p B F p B F p B F p B F p B F p B F p
Multivariate statistics 0.92 0.049 0.92 0.064 0.98 0.963 0.95 0.405 0.90 0.014 0.95 0.407 0.95 0.389 0.94 0.211
(Wilk’s Lambda)
SOL (min) −20.44 10.66 0.001 13.99 0.05 0.829 −11.51 0.14 0.708 −2.10 1.46 0.227 −13.53 1.72 0.191 12.73 0.19 0.665 −4.89 1.44 0.231 22.86 0.30 0.584
TST (min) 32.15 8.28 0.004 −20.01 1.68 0.195 −4.63 1.14 0.287 34.51 0.59 0.443 62.94 0.97 0.325 −57.56 3.63 0.058 67.81 0.28 0.597 −58.81 0.22 0.639
Frontiers in Psychology | www.frontiersin.org
SEI (%) 6.13 7.87 0.005 −4.58 1.53 0.218 −1.05 1.17 0.281 6.91 0.48 0.490 13.94 0.76 0.383 −11.13 3.82 0.052 13.96 0.33 0.568 −11.54 0.28 0.597
NWP −0.82 0.08 0.779 13.46 0.00 0.945 3.04 0.10 0.747 3.35 0.03 0.854 −11.95 5.59 0.019 −12.59 5.17 0.024 −12.42 1.93 0.165 −2.95 0.02 0.896
W (%SPT) −0.64 2.90 0.089 −0.08 1.47 0.226 3.61 1.50 0.222 −8.71 0.20 0.653 −11.74 0.16 0.691 9.21 4.45 0.036 −12.63 0.07 0.793 9.63 1.95 0.164
N1 (%SPT) −2.07 2.52 0.113 0.66 0.34 0.558 2.08 0.01 0.926 −2.05 0.02 0.879 1.17 1.96 0.162 −1.38 0.86 0.356 −2.99 1.57 0.212 0.55 1.84 0.176
N2 (%SPT) −3.82 0.01 0.909 −2.56 0.26 0.613 −5.35 0.65 0.422 0.11 6.14 0.014 11.26 0.03 0.860 −5.49 6.95 0.009 14.06 0.03 0.868 −4.23 0.12 0.728
N3 (%SPT) 3.47 5.85 0.016 1.01 0.91 0.340 1.02 0.10 0.747 5.53 6.70 0.010 −2.04 1.58 0.210 3.15 0.23 0.633 −2.11 1.45 0.230 −2.98 0.01 0.921
REM (%SPT) 2.66 1.61 0.205 0.81 0.04 0.843 −1.30 0.84 0.360 4.26 0.02 0.892 1.42 0.61 0.434 −4.96 0.37 0.545 3.43 0.06 0.806 −1.94 0.28 0.597
REML (min) 8.77 0.71 0.401 −29.24 1.88 0.171 −9.95 0.53 0.468 −15.46 0.09 0.763 −40.13 2.23 0.137 39.68 0.16 0.687 −23.79 0.98 0.324 −6.26 1.23 0.268
REMD (%) −10.69 0.51 0.475 3.31 2.89 0.090 −9.03 0.75 0.386 3.30 0.14 0.712 4.59 2.76 0.098 −9.80 0.40 0.530 2.11 1.31 0.252 −2.11 0.16 0.691
AI/REM −3.80 1.19 0.276 5.89 0.33 0.566 −5.26 0.00 0.954 8.23 0.23 0.630 11.28 0.83 0.364 −3.03 0.49 0.483 8.18 1.58 0.210 −10.00 0.03 0.873
AI/N −2.90 0.18 0.673 5.04 9.32 0.002 0.22 0.57 0.452 −0.39 0.07 0.797 −7.50 1.35 0.246 3.15 3.09 0.080 −4.57 2.53 0.113 −3.14 0.02 0.888
7
AWI/REM 0.83 0.45 0.504 2.87 2.40 0.122 0.40 0.04 0.845 0.97 0.02 0.887 −1.70 0.64 0.423 −2.86 2.35 0.126 −0.66 0.16 0.689 0.34 0.01 0.908
AWI/N −0.86 0.12 0.730 1.87 0.87 0.353 0.25 0.50 0.481 −0.02 0.45 0.502 −1.72 4.31 0.039 −1.07 4.03 0.046 −2.11 1.26 0.262 0.26 0.00 0.988
p values below p = 0.05 are set in bold font.
January 2019 | Volume 9 | Article 2712
PSG and Emotional Parameters in Insomnia
Feige et al. PSG and Emotional Parameters in Insomnia
Night A Night B
100
90
90
80
80
70
SEI
SEI
70
60
60
50
40
50
GSC GSC
ID ID
30
1 2 3 4 5 1 2 3 4 5
Evening relaxation Evening relaxation
FIGURE 1 | Relationship between evening relaxation and SEI (%) for the two groups in first (Left) and second (Right) nights.
Night A Night B
GSC GSC
ID ID
80
80
60
60
NW P
NW P
40
40
20
20
0
0
1 2 3 4 5 1 2 3 4 5
Evening relaxation Evening relaxation
FIGURE 2 | Relationship between evening relaxation and NWP for the two groups in first (Left) and second (Right) nights.
means an amelioration of values during sleep (positive Morning- samples of patients with ID and good sleeper controls.
Evening difference in our study). We did not see an influence While both parameters were lower in ID patients (“trait”),
of emotional balance (or its difference across the night) on particularly increased evening relaxation had a strong within-
sleep parameters, but a measure of (inverse) hyperarousal (i.e., subject influence on PSG sleep quality as a main effect across
relaxation) was included in the same model and apparently both groups and was additionally linked to a reduced number
correlated better with objective sleep parameters than emotional of wake periods in the ID patients, suggesting relaxation as
balance itself. Thus, for the SF-A emotional balance construct it a useful therapeutic target in conjunction with other CBT-I
appears that its change across the night is rather not related to elements.
hyperarousal or objective sleep parameters. Since there is a clear
group difference in emotional balance, it is possible that impaired
emotional balance over longer periods of time (e.g., weeks) leads LIMITATIONS
to increased hyperarousal. This notion cannot be tested using
the data of the current study but should be addressed by future While interpreting the results of this study some limitations
studies. should be taken into account. First of all we used pre-existing
In summary, in the current study we could separately assess data which on the one hand lead to a large sample size but
state- and trait- like influences of two emotional parameters, on the other hand restricted the measurement of the emotional
relaxation and emotional balance, on PSG in large matched state to two subjective items without defined valence. To assess
Frontiers in Psychology | www.frontiersin.org 8 January 2019 | Volume 9 | Article 2712
TABLE 4 | Within-subject effects of relaxation and emotional balance variables.
Feige et al.
Within
Evening Morning–Evening Evening x Group Morning–Evening x Group
Relaxation Emotional balance Relaxation Emotional balance Relaxation Emotional balance Relaxation Emotional balance
B F p B F p B F p B F p B F p B F p B F p B F p
Multivariate 0.84 0.000 0.96 0.608 0.78 0.000 0.94 0.216 0.94 0.209 0.95 0.476 0.95 0.369 0.95 0.541
statistics (Wilk’s
Lambda)
Frontiers in Psychology | www.frontiersin.org
SOL (min) −7.48 15.25 0.000 1.69 2.38 0.124 1.53 6.91 0.009 −2.92 0.58 0.445 2.78 1.39 0.240 0.93 1.42 0.234 1.60 0.70 0.404 7.48 0.89 0.345
TST (min) 17.49 12.08 0.001 −1.14 2.56 0.111 −2.66 29.05 0.000 8.90 4.55 0.034 6.47 3.90 0.049 −28.64 1.21 0.272 7.87 2.90 0.090 −12.99 0.15 0.699
SEI (%) 3.24 12.06 0.001 0.05 2.50 0.115 −0.93 31.70 0.000 2.11 4.47 0.035 2.22 3.51 0.062 −6.45 1.76 0.186 2.00 3.35 0.068 −3.02 0.13 0.718
NWP 0.08 0.09 0.771 −0.86 0.02 0.895 3.96 8.72 0.003 −5.38 1.70 0.194 −4.80 0.76 0.384 5.77 0.44 0.509 −9.67 1.50 0.222 6.99 1.89 0.170
W (%SPT) −0.68 3.04 0.082 −1.12 0.79 0.375 1.24 33.53 0.000 −2.48 0.96 0.329 −5.90 3.35 0.068 9.40 0.07 0.785 −4.16 4.42 0.036 3.78 0.85 0.358
N1 (%SPT) −1.00 10.62 0.001 2.03 0.15 0.699 0.05 4.30 0.039 0.46 2.74 0.099 −0.29 1.39 0.240 −1.21 0.73 0.392 −1.03 1.72 0.190 0.62 3.31 0.070
N2 (%SPT) 2.56 3.07 0.081 −0.78 1.57 0.212 −0.32 26.12 0.000 0.28 0.04 0.844 2.89 2.75 0.098 −4.40 0.38 0.541 4.11 1.07 0.302 −2.25 0.10 0.751
N3 (%SPT) −1.70 0.00 0.999 0.46 0.60 0.438 −0.37 5.72 0.017 1.84 0.94 0.334 2.64 1.07 0.302 −1.64 0.01 0.910 0.35 0.32 0.573 −1.58 0.07 0.798
REM (%SPT) 0.37 8.54 0.004 −0.15 0.60 0.439 −0.82 7.85 0.005 0.07 2.50 0.115 1.00 6.35 0.012 −2.58 1.37 0.244 0.90 8.55 0.004 −0.73 0.46 0.499
REML (min) 7.36 10.28 0.001 −5.38 0.03 0.869 18.87 16.62 0.000 −16.70 2.11 0.147 −49.62 2.69 0.102 30.47 0.82 0.365 −12.41 4.59 0.033 8.09 0.02 0.885
REMD (%) −2.33 3.86 0.050 −0.19 1.34 0.248 −0.55 0.15 0.696 2.65 0.43 0.510 2.43 0.71 0.400 2.74 1.04 0.309 1.39 4.16 0.042 −3.00 0.73 0.394
9
AI/REM 4.25 1.23 0.268 −1.85 0.00 0.975 −0.06 0.03 0.858 −0.30 0.36 0.551 −7.13 0.11 0.738 4.27 0.00 0.979 −2.65 0.37 0.541 3.48 0.54 0.465
AI/N −1.10 20.80 0.000 0.46 2.37 0.125 0.19 14.21 0.000 −1.41 1.46 0.228 −3.28 1.21 0.272 3.04 0.11 0.737 −0.74 5.22 0.023 0.84 0.00 0.997
AWI/REM 2.20 3.94 0.048 −1.65 0.71 0.400 1.53 2.82 0.094 −0.80 0.21 0.648 −1.89 0.20 0.657 2.05 0.00 0.994 −1.55 1.34 0.248 1.15 0.17 0.682
AWI/N −0.36 3.69 0.056 0.07 0.21 0.651 0.43 17.06 0.000 −0.58 1.50 0.221 −0.53 4.06 0.045 0.86 0.07 0.790 −1.30 0.76 0.385 1.01 3.03 0.083
p values below p = 0.05 are set in bold font.
January 2019 | Volume 9 | Article 2712
PSG and Emotional Parameters in Insomnia
Feige et al. PSG and Emotional Parameters in Insomnia
60
60
60
GSC GSC GS C
ID ID ID
40
40
40
SEI night diff erence
SEI night diff erence
SEI night diff erence
20
20
20
0
0
−20
−20
−20
−3 −2 −1 0 1 2 3 −3 −2 −1 0 1 2 3 −6 −4 −2 0 2 4
Ev ening relaxation night diff erence Morning relaxation night diff erence Morning−Ev ening relaxation night diff erence
FIGURE 3 | Within-subject relationships to the SEI captured as differences between nights: Evening (Left), Morning (Middle), and Morning-Evening (Right) relaxation.
the emotional state more broadly, another procedure should chronotype have not been assessed systematically for all subjects
be chosen in future studies. Buysse et al. (2007) presented although these characteristics could be related to potential
a possible procedure that additionally avoids ground effects. subgroup-differences and should therefore be assessed in future
Furthermore the evening data as used here was assessed in studies.
the following morning and could therefore be influenced by
the morning emotional state. To avoid such bias future studies ETHICS STATEMENT
should assess the emotional state in the actual evening. Possibly,
more questionnaires for sample description would have been The current study is a retrospective analysis of studies
useful. carried out in accordance with the recommendations of
Just like in every other sleep laboratory study the ecological the ethics committee of the University of Freiburg Medical
validity of the results can be questioned. The time needed for Center with written informed consent from all subjects. All
adjustment to the changed sleep environment is not known subjects gave written informed consent in accordance with
exactly, although an adaption phase of one night is usually the Declaration of Helsinki. The protocol was approved by
assumed (Le Bon et al., 2001). Since good signal quality and the ethics committee of the University of Freiburg Medical
monitoring options are still lacking for the home environment, Center.
sleep laboratory data in general may lack ecological validity.
This is, however, partially true also for sleep studies conducted AUTHOR CONTRIBUTIONS
at home, because the presence of the recording equipment is a
factor in the “First Night Effect” as well (Blackwell et al., 2017). BF and DR devised the study. BF devised the data analysis,
In the current study we analyzed both between- and within- interpreted the data and wrote the manuscript. BB and DM
subject influences between PSG and emotional parameters. analyzed and interpreted the data. All authors contributed to the
The “First Night Effect” generates welcome within-subject manuscript.
variability in this respect (it can be interpreted as a “stress
probe” for sleep). Part of our within-subject results could be FUNDING
due to this special situation with an unusually disturbed first
night. The article processing charge was funded by the German
Finally, most of our data has been collected during clinical Research Foundation (DFG) and the University of Freiburg in
routine. Therefore characteristics like personality traits or the funding programme Open Access Publishing.
REFERENCES Baglioni, C., Spiegelhalder, K., Lombardo, C., and Riemann, D. (2010).
Sleep and emotions: a focus on insomnia. Sleep Med. Rev. 14, 227–238.
Agnew, H. W. Jr., Webb, W. B., and Williams, R. L. (1966). The first doi: 10.1016/j.smrv.2009.10.007
night effect: an EEG study of sleep. Psychophysiology 2, 263–266. Beck, A. T., and Steer, R. A. (1987). Beck Depression Inventory. San Antonio, TX:
doi: 10.1111/j.1469-8986.1966.tb02650.x The Psychological Corporation.
American Psychiatric Association (2000). Diagnostic and Statistical Manual of Bertisch, S. M., Wells, R. E., Smith, M. T., and McCarthy, E. P. (2012). Use
Mental Disorders, 4th Edn. Text revision. APA, Washington, DC. of relaxation techniques and complementary and alternative medicine by
American Psychiatric Association (2013). Diagnostic and Statistical Manual of american adults with insomnia symptoms: results from a national survey. J.
Mental Disorders, 5th Edn: DSM-5. APA Publishing, Washington, DC. Clin. Sleep Med. 8, 681–691. doi: 10.5664/jcsm.2264
Baglioni, C., Battagliese, G., Feige, B., Spiegelhalder, K., Nissen, C., Voderholzer, Blackwell, T., Paudel, M., Redline, S., Ancoli-Israel, S., and Stone, K. L. (2017).
U., et al. (2011). Insomnia as a predictor of depression: a meta-analytic A novel approach using actigraphy to quantify the level of disruption of sleep
evaluation of longitudinal epidemiological studies. J. Affect. Disord. 135, 10–19. by in-home polysomnography: the MrOS sleep study: sleep disruption by
doi: 10.1016/j.jad.2011.01.011 polysomnography. Sleep Med. 32, 97–104. doi: 10.1016/j.sleep.2016.11.019
Frontiers in Psychology | www.frontiersin.org 10 January 2019 | Volume 9 | Article 2712
Feige et al. PSG and Emotional Parameters in Insomnia
Buysse, D. J., Reynolds, C. F. III., Monk, T. H., Berman, S. R., and Kupfer, Palmer, C. A., and Alfano, C. A. (2017). Sleep and emotion regulation:
D. J. (1989). The Pittsburgh Sleep Quality Index: a new instrument an organizing, integrative review. Sleep Med. Rev. 31, 6–16.
for psychiatric practice and research. Psychiatry Res. 28, 193–213. doi: 10.1016/j.smrv.2015.12.006
doi: 10.1016/0165-1781(89)90047-4 Perlis, M. L., Giles, D. E., Mendelson, W. B., Bootzin, R. R., and Wyatt, J. K. (1997).
Buysse, D. J., Thompson, W., Scott, J., Franzen, P. L., Germain, A., Hall, Psychophysiological insomnia: the behavioural model and a neurocognitive
M., et al. (2007). Daytime symptoms in primary insomnia: a prospective perspective. J. Sleep Res. 6, 179–188. doi: 10.1046/j.1365-2869.1997.00045.x
analysis using ecological momentary assessment. Sleep Med. 8, 198–208. R Core Team (2018). R: A Language and Environment for Statistical Computing.
doi: 10.1016/j.sleep.2006.10.006 Vienna: R Foundation for Statistical Computing.
Carskadon, M. A., Dement, W. C., Mitler, M. M., Guilleminault, C., Zarcone, Rechtschaffen, A., and Kales, A. (1968). A Manual of Standardized Terminology,
V. P., and Spiegel, R. (1976). Self-reports versus sleep laboratory findings in Techniques, and Scoring System for Sleep Stages of Human Subjects. Publication
122 drug-free subjects with complaints of chronic insomnia. Am. J. Psychiatry 204, National Institutes of Health, Washington DC.
133, 1382–1388. doi: 10.1176/ajp.133.12.1382 Riemann, D., and Backhaus, J. (1996). Behandlung von Schlafstörungen - ein
Edinger, J. D., and Fins, A. I. (1995). The distribution and clinical significance psychologisches Gruppenprogramm. Weinheim: Beltz.
of sleep time misperceptions among insomniacs. Sleep 18, 232–239. Riemann, D., Baglioni, C., Bassetti, C., Bjorvatn, B., Dolenc Groselj, L., Ellis, J. G.,
doi: 10.1093/sleep/18.4.232 et al. (2017a). European guideline for the diagnosis and treatment of insomnia.
Espie, C. A., Broomfield, N. M., Macmahon, K. M., Macphee, L. M., and Taylor, J. Sleep Res. 26, 675–700. doi: 10.1111/jsr.12594
L. M. (2006). The attention-intention-effort pathway in the development of Riemann, D., Baum, E., Cohrs, S., Crönlein, T., Hajak, G., Hertenstein, E.,
psychophysiologic insomnia: a theoretical review. Sleep Med. Rev. 10, 215–245. et al. (2017b). S3-Leitlinie Nicht erholsamer Schlaf/Schlafstörungen – Kapitel
doi: 10.1016/j.smrv.2006.03.002 "Insomnie bei Erwachsenen" (AWMF- Registernummer 063-003), Update
Feige, B., Al-Shajlawi, A., Nissen, C., Voderholzer, U., Hornyak, M., Spiegelhalder, 2016. Somnologie 21, 2–44. doi: 10.1007/s11818-016-0097-x
K., et al. (2008). Does REM sleep contribute to subjective wake time in primary Riemann, D., Hohagen, F., König, A., and Schwartz, B. (1996). Advanced vs normal
insomnia? A comparison of polysomnographic and subjective sleep in 100 sleep timing: effects on depressed mood after response to sleep deprivation
patients. J. Sleep Res. 17, 180–190. doi: 10.1111/j.1365-2869.2008.00651.x in patients with a major depressive disorder. J. Affect. Disord. 37, 121–128.
Feige, B., Nanovska, S., Baglioni, C., Bier, B., Cabrera, L., Diemers, S., et al. doi: 10.1016/0165-0327(95)00082-8
(2018). Insomnia - perchance a dream? Results from a NREM/REM sleep Riemann, D., Nissen, C., Palagini, L., Otte, A., Perlis, M. L., and Spiegelhalder,
awakening study in good sleepers and patients with insomnia. Sleep 41:zsy032. K. (2015). The neurobiology, investigation, and treatment of chronic
doi: 10.1093/sleep/zsy032 insomnia. Lancet Neurol. 14, 547–558. doi: 10.1016/S1474-4422(15)00
Frankel, B. L., Coursey, R. D., Buchbinder, R., and Snyder, F. (1976). Recorded and 021-6
reported sleep in chronic primary insomnia. Arch. Gen. Psychiatry 33, 615–623. Riemann, D., Spiegelhalder, K., Espie, C., Pollmächer, T., Léger, D., Bassetti, C.,
doi: 10.1001/archpsyc.1976.01770050067011 et al. (2011). Chronic insomnia: clinical and research challenges–an agenda.
Friedrich, A., and Schlarb, A. A. (2018). Let’s talk about sleep: a systematic review Pharmacopsychiatry 44, 1–14. doi: 10.1055/s-0030-1267978
of psychological interventions to improve sleep in college students. J. Sleep Res. Riemann, D., Spiegelhalder, K., Feige, B., Voderholzer, U., Berger, M., Perlis,
27, 4–22. doi: 10.1111/jsr.12568 M., et al. (2010). The hyperarousal model of insomnia: A review of the
Görtelmeyer, R. (1981). “Schlaffragebogen SF-A und SF-B,” in Internationale concept and its evidence. Sleep Med. Rev. 14, 19–31. doi: 10.1016/j.smrv.2009.
Skalen für Psychiatrie (Weinheim: Collegium Internationale Psychiatriae 04.002
Scolarum (CIPS);Beltz). Riemann, D., Spiegelhalder, K., Nissen, C., Hirscher, V., Baglioni, C., and
Görtelmeyer, R. (2011). “Schlaffragebogen a und b. revidierte fassung,” in Feige, B. (2012). REM sleep instability - A new pathway for insomnia?
Internationale Skalen für Psychiatrie, 6th Edn (Weinheim: Collegium Pharmacopsychiatry 45, 167–176. doi: 10.1055/s-0031-1299721
Internationale Psychiatriae Scolarum (CIPS);Beltz). Sleep Disorders Atlas Task Force of the American Sleep Disorders Association
Harvey, A. G. (2002). A cognitive model of insomnia. Behav. Res. Ther. 40, (1992). EEG arousals: scoring rules and examples. Sleep 15, 173–184.
869–893. doi: 10.1016/S0005-7967(01)00061-4 doi: 10.1093/sleep/15.2.173
Hautzinger, M., Bailer, M., Worall, H., and Keller, F. (1994). Beck-Depressions- Trauer, J. M., Qian, M. Y., Doyle, J. S., Rajaratnam, S. M., and Cunnington,
Inventar (BDI) Handbuch. Bern:Huber. D. (2015). Cognitive behavioral therapy for chronic insomnia – a
Kahn, M., Sheppes, G., and Sadeh, A. (2013). Sleep and emotions: bidirectional systematic review and meta-analysis. Ann. Intern. Med. 163, 191–204.
links and underlying mechanisms. Int. J. Psychophysiol. 89, 218–228. doi: 10.7326/M14-2841
doi: 10.1016/j.ijpsycho.2013.05.010 Walker, M. P. (2009). The role of sleep in cognition and emotion. Ann. N. Y. Acad.
Le Bon, O., Staner, L., Hoffmann, G., Dramaix, M., San Sebastian, I., Murphy, J. R., Sci. 1156, 168–197. doi: 10.1111/j.1749-6632.2009.04416.x
et al. (2001). The first-night effect may last more than one night. J. Psychiatr. Wassing, R., Benjamins, J. S., Dekker, K., Moens, S., Spiegelhalder, K., Feige, B.,
Res. 35, 165–172. doi: 10.1016/S0022-3956(01)00019-X et al. (2016). Slow dissolving of emotional distress contributes to hyperarousal.
Means, M. K., Edinger, J. D., Glenn, D. M., and Fins, A. I. (2003). Accuracy of Proc. Natl. Acad. Sci. U.S.A. 113, 2538–2543. doi: 10.1073/pnas.1522520113
sleep perceptions among insomnia sufferers and normal sleepers. Sleep Med. 4, Wauquier, A., van Sweden, B., Kerkhof, G. A., and Kamphuisen, H. A. (1991).
285–296. doi: 10.1016/S1389-9457(03)00057-1 Ambulatory first night sleep effect recording in the elderly. Behav. Brain Res.
Morphy, H., Dunn, K. M., Lewis, M., Boardman, H. F., and Croft, P. R. (2007). 42, 7–11.
Epidemiology of insomnia: a longitudinal study in a UK population. Sleep 30,
274–280. doi: 10.1093/sleep/30.3.274 Conflict of Interest Statement: The authors declare that the research was
Neckelmann, D., Mykletun, A., and Dahl, A. A. (2007). Chronic insomnia conducted in the absence of any commercial or financial relationships that could
as a risk factor for developing anxiety and depression. Sleep 30, 873–880. be construed as a potential conflict of interest.
doi: 10.1093/sleep/30.7.873
Norell-Clarke, A., Jansson-Fröjmark, M., Tillfors, M., Holländare, F., and Copyright © 2019 Feige, Baumgartner, Meyer and Riemann. This is an open-access
Engström, I. (2015). Group cognitive behavioural therapy for insomnia: Effects article distributed under the terms of the Creative Commons Attribution License (CC
on sleep and depressive symptomatology in a sample with comorbidity. Behav. BY). The use, distribution or reproduction in other forums is permitted, provided
Res. Ther. 74, 80–93. doi: 10.1016/j.brat.2015.09.005 the original author(s) and the copyright owner(s) are credited and that the original
Palagini, L., Biber, K., and Riemann, D. (2014). The genetics of insomnia publication in this journal is cited, in accordance with accepted academic practice.
– Evidence for epigenetic mechanisms? Sleep Med. Rev. 18, 225–235. No use, distribution or reproduction is permitted which does not comply with these
doi: 10.1016/j.smrv.2013.05.002 terms.
Frontiers in Psychology | www.frontiersin.org 11 January 2019 | Volume 9 | Article 2712
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Family Therapy For Autism Spectrum Disorders (Cto)Document21 pagesFamily Therapy For Autism Spectrum Disorders (Cto)Julie Rose AlboresNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Selected Instructional Course LecturesDocument27 pagesSelected Instructional Course LecturesAhmad ShakirNo ratings yet
- Colon, Rectum and Anus-Dr. SigitDocument121 pagesColon, Rectum and Anus-Dr. SigitYuliana Latif100% (1)
- CNA Practice TestDocument12 pagesCNA Practice TestJoe Prempeh50% (4)
- Hazardous Materials Management Plan SMDocument26 pagesHazardous Materials Management Plan SMdarmayunitaNo ratings yet
- Medical Bill 2Document1 pageMedical Bill 2arun_ioclNo ratings yet
- Prepared by Muhammad Salman: This Brand Plan Has Been Designed For The ProductDocument90 pagesPrepared by Muhammad Salman: This Brand Plan Has Been Designed For The ProductMuhammad SalmanNo ratings yet
- Paediatric Clerking SheetDocument5 pagesPaediatric Clerking SheetIamTinesh100% (2)
- + +Sandra+Carter +TMJ+No+More+PDF+ (Ebook) PDFDocument49 pages+ +Sandra+Carter +TMJ+No+More+PDF+ (Ebook) PDFMassimiliano Marchionne0% (1)
- Bacteriological Quality of Street Vended Food PanipuriDocument5 pagesBacteriological Quality of Street Vended Food PanipuriYus EfendiNo ratings yet
- Bio Availability Solved ProblemsDocument2 pagesBio Availability Solved Problemsabdullah2020100% (1)
- Hydralazine Drug StudyDocument1 pageHydralazine Drug Studymilkv71% (7)
- Masterfile Let ReviewerDocument644 pagesMasterfile Let ReviewerApril Claire Pineda Manlangit50% (4)
- How To Measure Dialysis Adequacy - Edit 3Document42 pagesHow To Measure Dialysis Adequacy - Edit 3Dicky SaputraNo ratings yet
- Transtorno de Deficit de AtencioDocument8 pagesTranstorno de Deficit de AtencioCriimiinologiia LoOkkaNo ratings yet
- Autismo CIE11Document2 pagesAutismo CIE11Diego CabralNo ratings yet
- The Infant Preschool Family Mental Health Initiative Compendium of Screening Tools For Early Childhood Social-Emotional Deve PDFDocument70 pagesThe Infant Preschool Family Mental Health Initiative Compendium of Screening Tools For Early Childhood Social-Emotional Deve PDFDiego CabralNo ratings yet
- The Circadian Clock in The Human HealthDocument12 pagesThe Circadian Clock in The Human HealthDiego CabralNo ratings yet
- The Sleeping Infant Brain Anticipates DevelopmentDocument4 pagesThe Sleeping Infant Brain Anticipates DevelopmentDiego CabralNo ratings yet
- Autismo CIE11Document2 pagesAutismo CIE11Diego CabralNo ratings yet
- Section A Schedule - Didactic 2Document5 pagesSection A Schedule - Didactic 2AdityaTiwariNo ratings yet
- Curriculum VitaeDocument7 pagesCurriculum VitaeRossy Del ValleNo ratings yet
- Prenatal RhogamDocument3 pagesPrenatal Rhogamgshastri7No ratings yet
- Oral 5Document236 pagesOral 5Iodeh1985 OdehNo ratings yet
- Components of General Anesthesia: UnconsciousnessDocument17 pagesComponents of General Anesthesia: UnconsciousnessDanieleNo ratings yet
- EMQDocument12 pagesEMQWaleed Mohamed AhmedNo ratings yet
- Training Workshop On Attitudinal ChangeDocument5 pagesTraining Workshop On Attitudinal ChangeSam ONiNo ratings yet
- Arq AmberDocument4 pagesArq AmberMaqsood AnsariNo ratings yet
- Msds Nano PolishDocument5 pagesMsds Nano PolishGan LordNo ratings yet
- Benefits at A Glance: TexasDocument10 pagesBenefits at A Glance: Texasakula_rupeshNo ratings yet
- Observator Ios 2016Document355 pagesObservator Ios 2016ajgamesNo ratings yet
- Corrected Ortho QsDocument48 pagesCorrected Ortho QsMuhamad Danial Kholili Al-JaloriNo ratings yet
- Tracheostomy CareDocument7 pagesTracheostomy CareJoanna MayNo ratings yet
- Carrubba Botanical Guide RDocument247 pagesCarrubba Botanical Guide Rafridikhanjan100% (3)
- Drug To Drug InteractionDocument47 pagesDrug To Drug InteractionMannan SokaNo ratings yet
- Teaching Experience Log All - Sarah WedeDocument2 pagesTeaching Experience Log All - Sarah Wedeapi-647779956No ratings yet