Professional Documents
Culture Documents
Pediatric Cardiology
Pediatric Cardiology
Uploaded by
Jhara0 ratings0% found this document useful (0 votes)
8 views43 pagesCopyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views43 pagesPediatric Cardiology
Pediatric Cardiology
Uploaded by
JharaCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 43
Pediatric
Cardiology 101
Misty Carlson, M.D.
DISCLAIMER:
= This lecture is based on generalizations.
= In reality, a congenital heart defect (CHD)
can act completely different from one
patient to the next (eg- classic ToF vs
“pink” ToF).
= There are many more CHDs than what
I've listed and | hope you can use these
principles to help you out with those.
Fetal Circulation
™ For the fetus the placenta is the oxygenator
so the lungs do little work
= RV &LV contribute equally to the systemic
circulation and pump against similar
resistance
™ Shunts are necessary for survival
ductus venosus (bypasses liver)
foramen ovale (RL atrial level shunt)
ductus arteriosus (RL arterial level shunt)
Transitional Circulation
= With first few breaths lungs expand and
serve as the oxygenator (and the placenta
is removed from the circuit)
= Foramen ovale functionally closes
= Ductus arteriosus usually closes within
first 1-2 days
EE
Neonatal Circulation
= RV pumps to pulmonary circulation and
LV pumps to systemic circulation
= Pulmonary resistance (PVR) is high; so
initially RV pressure ~ LV pressure
= By 6 weeks pulmonary resistance drops
and LV becomes dominant
Normal Pediatric Circulation
= LV pressure is 4-5 x RV pressure (this is
feasible since RV pumps against lower
resistance than LV)
= RV is more compliant chamber than LV
EE
NORMAL HEART
= No shunts
™ No pressure gradients
= Normal AV valves
= Normal semilunar
valves
= If this patient was
desaturated what
would you think?
.
If you have a hole in the heart what
affects shunt flow?
1. Pressure — easy enough to understand
2. Resistance — impedance to blood flow
Remember, the LV has higher pressure and
a higher resistive circuit relative to the RV.
Now onto the nitty-gritty ...
EEL
Congenital Heart Disease (CHD)
™ Occurs in 0.5-1% of all live births
= Simple way to classify is:
LR shunts
Cyanotic CHD (RL shunts)
Obstructive lesions
L—R Shunts (“Acyanotic” CHD)
= Defects
VSD
PDA
ASD
AVSD (or complete atrioventricular canal)
= May not be apparent in neonate due to
high PVR (ie- bidirectional shunt)
L—R Shunts — General Points
PDA&VSD | ASD
™ Presents in infancy w/ Fizssebie ii Grilehised wi
heart failure, murmur, intolerance (AVSD or 1° ASD
z poor g presents earlier)
Feft heartenlargement ig Right heart enlargement
(CHE) (RHE)
= Transmits flow and = ‘Transmits flow.onik
pressure y
[AVSD can present as either depending on size of ASD & VSD component|
entricular Septal Defect (perimembranous) i Defect (secundum)
. oy
fentncular Sept fect (perimembranous) lal Septal Defect (secundum)
Left Heart Right Heart
Overload Overload
Pulm vase
markings
equal in
upper and
lower zones
.
Eisenmenger’s Syndrome
= A long standing L—R shunt will eventually
cause irreversible pulmonary vascular
disease
= This occurs sooner in unrepaired VSDs
and PDAs (vs an ASD) because of the
high pressure
™ Once the PVR gets very high the shunt
reverses (ie- now R->L) and the patient
becomes cyanotic
EE
R—L Shunts (CCHD)
* “Blue blood bypasses the lungs”
* Degree of cyanosis varies
* Classify based on pulmonary blood flow (PBF)
+ PBF PBF
= Truncus arteriosus = Tetralogy of Fallot
= Total anomalous pulm. = Tricuspid atresia
venous return (TAPVR) = Ebstein's anomaly
= Transposition of the great
arteries (TGA)
Please note: This is a generalization. In reality most of these defects can present with
low or high PBF (eg- ToF with little PS acts more like a VSD with high PBF)
Truncus Arteriosus (Type |)
Left Aortic Arch
There is unimpeded
PBF; thus, extreme
pulmonary
overcirculation.
R—L Shunts
+ PBF
= Presents more often
with heart failure
(except TGA)
= Pulmonary congestion
worsens as neonatal
PVR lowers
= Sats can be 93-94% if
there is high PBF
R—L Shunts
Tetralogy of Fallot
Left Aortic Arch
PBF
= Presents more often
with cyanosis
= See oligemic lung
fields
= Closure of PDA may
worsen cyanosis
Dynamic subvalvular
obstruction here
causes “et spells”
ssessWhy are
“© pressures
equal?
[
metelogy of Fait
Left Aortic Arch
eS
—
Different amounts of PBF
(Truncus vs ToF)
Obstructive Lesions
Ductal Dependent
Critical PS/AS
Critical CoA/IAA
HLHS
Presents in CV shock at
2-3 days of age when
PDA closes
+/- cyanosis
= Needs PGE,
Non-Ductal Dependent
1. Mild-moderate AS
2. Mild-moderate CoA
3. Mild-moderate PS
a
Presents in older
child w/ murmur,
exercise intolerance,
or HTN (in CoA)
= Not cyanotic
ao N=
A
manners Ductal-Dependent
Lesion
Without a PDA there is no
blood flow to the abdomen
and lower extremities.
(Blue blood is better than no blood.)
Physical Exam
= Inspection and palpation
Cardiac cyanosis must be central
Differential cyanosis = R-L PDA shunt
Differential edema/congestion implies
obstruction of SVC or IVC
Increased precordial activity
Displaced PMI
RV heave = RV hypertension
Physical exam
= Lungs
Respiratory rate and work of breathing
| Oxygen saturations
= Abdominal exam
~ Liver size
= Extremities
Perfusion
| Edema
— Clubbing
Physical Exam
= Pulses (very important)
Differential pulses (weak LE) = CoA
Bounding pulse = run-off lesions (_+R PDA
shunt, Al, BT shunt)
Weak pulse = cardiogenic shock or CoA
Pulsus paradoxus is an exaggerated SBP
drop with inspiration — tamponade or bad
asthma
Pulsus alternans — altering pulse strength >
LV mechanical dysfunction
Physical Exam
= Heart sounds
Ejection click = AS or PS
Mid-systolic click = MVP
Loud S2 = Pulmonary HTN
Single S2 = one semilunar valve (truncus),
anterior aorta (TGA), pulmonary HTN
Fixed, split S2 = ASD, PS
Gallop (S3) — may be due to cardiac
dysfunction/ volume overload
Muffled heart sounds and/or a rub = pericardial
effusion + tamponade
Physical Exam
= Types of Murmurs
Systolic Ejection Murmur (SEM) =
turbulence across a semilunar valve
Holosystolic murmur = turbulence begins
with systole (VSD, MR)
Continuous murmur = pressure difference
in systole and diastole (PDA, BT shunt)
Innocent murmurs
= Peripheral pulmonic stenosis (PPS)
Heard in newborns — disappears by one year
of age (often earlier)
Soft SEM at ULSB w/ radiation to axilla and
back (often heard best in axilla/back)
Need to differentiate b/w PPS and actual
pulmonic stenosis. PS often associated with
a valvular click and heard best over
precordium
Innocent murmurs
= Still's murmur
Classic innocent murmur
Heard most commonly in young children (3-5 yrs of
age) but can be heard in all ages
“Vibratory” low-frequency murmur often heard along
LSB and apex
Positional — increases in intensity when pt is in supine
position
Also louder in high output states (i.e. dehydration,
fever)
Need to differentate from VSD
Innocent murmurs
= Pulmonary flow murmur
— Often heard in older children and adolscents
Soft SEM at ULSB, little radiation; normal second
heart sound
— Not positional
Need to differentiate b/w mild PS and especially an
ASD
® Hint: ASD would have a fixed split second heart sound
Innocent murmurs
= Venous hum
| Often heard in toddlers, young children
Low pitched continuous murmur often heard best in
infraclavicular area, normal heart sounds
~ Positional — diminishes or goes completely away
when pt in supine position or with compression of
jugular vein
Need to differentiate between a PDA
EE
Syndrome Associations
= Down — AV canal and VSD
= Turner — CoA, AS
= Trisomies 13 and 18 — VSD, PDA
= Fetal alcohol - L—R shunts, ToF
=™ CHARGE - conotruncal (ToF, truncus)
EE
Hereditary Diseases
= Marfan (AD)- aortic root aneurysm + dissection, MVP,
MR, Al
HCM (AD) — outflow tract obstruction, arrhythmias
Noonan (AD) — HCM, PS
DMD/BMD (X-link) —- DCM (>12 y.o.)
Williams (AD) — supravalvar AS
Tuberous sclerosis — rhabdomyoma
Romano-Ward — AD LQTS
Jervell & Lange-Nielsen — AR LQTS & deafness
A
Kawasaki Disease (KD)
= Now the #1 cause of acquired heart
disease
= A systemic vasculitis (etiology-unknown)
= Tests - CBC, CMP, CRP, ESR, EKG,
ECHO
= Rx -—IVIG at 2g/kg and high-dose ASA
= Prognosis — Coronary artery dilatation
in 15-25% wio IVIG and 4% wi IVIG (if
given within 10 days of fever onset). Risk
of coronary thrombosis.
Kawasaki — Clinical criteria
= Fever for at least 5 days AND 4 of the
following 5 criteria:
Eyes - conjunctival injection (ie- no exudate)
Lips & mouth - erythema, cracked lips, strawberry
tongue
Hands & feet - edema and/or erythema
Skin - polymorphous exanthem (ie- any rash)
Unilateral, cervical lymphadenopathy
Rheumatic Fever
A post-infectious connective tissue disease
Follows GAS pharyngitis by 3 weeks (vs. nephritogenic
strains of GAS)
= Injury by GAS antibodies cross-reacting with tissue
= Dx —JONES criteria (major and minor)
= Tests — Throat Cx, ASO titer, CRP, ESR, EKG, +/-
ECHO
™ Rx—PCN x10 days and high-dose ASA or steroids
= 2 Prophylaxis — daily po PCN or monthly IM PCN
.
Rheumatic Fever — organs
affected
1. Heart muscle & valves — myocarditis &
endocarditis (pericarditis rare w/o the others)
2. Joints — polyarthritis
3. Brain — Sydenham’s Chorea (“milkmaid’s grip” or
better yet, “motor impersistance”)
4, Skin — erythema marginatum (serpiginous border)
due to vasculitis
5. Subcutaneous nodules — non-tender, mobile and on
extensor surfaces
:
In case you haven’t had enough....
Hypoplastic Left Heart Syndrome
O A ductal-dependent
lesion
Q One ventricle pumps
both PBF & SBF
Q Difficult to balance
PBF & SBF
Norwood Procedure
™ What is the purpose
of the BT shunt?
= Is there a murmur?
= What is your guess
for the arterial
saturation?
Tricuspid atresia s/p
bidirectional Glenn
Bidirectional Glenn
= What is the purpose
of the Glenn?
= Is there a murmur?
= What is your guess
for the arterial
saturation?
.
| Tricuspid atresia s/p
Fontan
onca0
1
Fontan circuit
= What is the path of
blood?
= Is there a murmur?
= What is your guess
for the arterial
saturation?
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Fiebre ReumáticaDocument19 pagesFiebre ReumáticaZOfii SnhzNo ratings yet
- PreexcitationDocument83 pagesPreexcitationJoanLeeCramerNo ratings yet
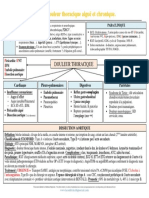
- Ritmos de Soporte Vital Cardiovascular AvanzadoDocument1 pageRitmos de Soporte Vital Cardiovascular AvanzadoPaula Castañeda100% (1)
- Preguntas y dsgvsDGEDSAGGGGGGGGGGGXZVVVVVVde Nefrología............. Jhoam Edwin Mas GuadalupeDocument36 pagesPreguntas y dsgvsDGEDSAGGGGGGGGGGGXZVVVVVVde Nefrología............. Jhoam Edwin Mas GuadalupeJhoam Edwin Mas GuadalupeNo ratings yet
- PERICARDITISDocument39 pagesPERICARDITISEdwin RivasNo ratings yet
- 1700 MCQ Revised VersionDocument485 pages1700 MCQ Revised VersionLu YaNo ratings yet
- Insuficiencia Renal, El Enemigo Silencioso: Renal Insufficiency, The Silent EnemyDocument12 pagesInsuficiencia Renal, El Enemigo Silencioso: Renal Insufficiency, The Silent EnemydanielgvazNo ratings yet
- I-11-197-Douleur Thoracique Aiguë Et Chronique FICHEDocument1 pageI-11-197-Douleur Thoracique Aiguë Et Chronique FICHETaxo HaNo ratings yet
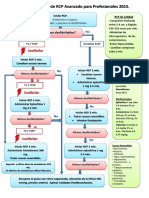
- RCP PediatriaDocument5 pagesRCP Pediatriajainson007649No ratings yet
- Primeros Auxilios Septiembre 2Document3 pagesPrimeros Auxilios Septiembre 2Kevin Jesid Obando TrochezNo ratings yet
- Sva 2015Document1 pageSva 2015Yanely AlmaguerNo ratings yet
- Coartación Aortica: Yisell Mantilla Quitian 15022017 Instrumentacion Quirurgica Universidad de Santander 2020Document20 pagesCoartación Aortica: Yisell Mantilla Quitian 15022017 Instrumentacion Quirurgica Universidad de Santander 2020api-522438695No ratings yet
- Pediatric Advanced Life Support (PALS) - UpToDate (1) .En - EsDocument57 pagesPediatric Advanced Life Support (PALS) - UpToDate (1) .En - EsSofíaNo ratings yet
- Cardiología: EnarmDocument10 pagesCardiología: EnarmCharly FlowNo ratings yet
- Acute Coronary SyndromeDocument19 pagesAcute Coronary SyndromeSherree HayesNo ratings yet
- 8 - Disritmias Peri-ParagemDocument31 pages8 - Disritmias Peri-ParagemirisbrancoNo ratings yet
- Hematuria - SX NefriticoDocument45 pagesHematuria - SX NefriticopaulaNo ratings yet
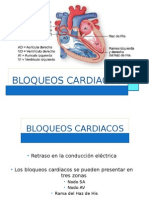
- Bloqueos EkgDocument17 pagesBloqueos EkgMariana ArmentaNo ratings yet
- 236 - Fibrillation AuriculaireDocument7 pages236 - Fibrillation AuriculaireAlpha ZeroNo ratings yet
- ARRITMIASDocument3 pagesARRITMIASLucero DHNo ratings yet
- Hopkins Medicine Review Cardiology SectionDocument54 pagesHopkins Medicine Review Cardiology SectiondrsalilsidhqueNo ratings yet
- Mid-Term PresentationDocument18 pagesMid-Term Presentationapi-480918653No ratings yet
- Daftar BHP e KatalogDocument6 pagesDaftar BHP e KatalogSuastari PutuNo ratings yet
- Cardioversion and DefibrillationDocument15 pagesCardioversion and DefibrillationShalini ChanduNo ratings yet
- Caso Clínico ScacsstDocument31 pagesCaso Clínico ScacsstPaul SalvadorNo ratings yet
- GlomerulopatiasDocument7 pagesGlomerulopatiasElianChicasNo ratings yet
- Clase 5. Indicaciones HemodialisisDocument33 pagesClase 5. Indicaciones HemodialisispaulinaNo ratings yet
- Presion Venosa YugularDocument2 pagesPresion Venosa YugularJuan WoodsNo ratings yet
- RCP - para Reflexionar y Analizar.Document4 pagesRCP - para Reflexionar y Analizar.Paco MoraNo ratings yet
- Risk Stratification of The J Wave SyndromeDocument11 pagesRisk Stratification of The J Wave SyndromepuchioNo ratings yet