Professional Documents
Culture Documents
Nejmra 043442
Nejmra 043442
Uploaded by
AriefAROriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nejmra 043442
Nejmra 043442
Uploaded by
AriefARCopyright:
Available Formats
The new england journal of medicine
review article
current concepts
Diagnosis from the Blood Smear
Barbara J. Bain, F.R.A.C.P., F.R.C.Path.
a
From the Department of Haematology, St. n examination of the blood smear (or film) may be
Mary’s Hospital, London. Send reprint re- requested by physicians or initiated by laboratory staff. With the
quests to Dr. Bain at St. Mary’s Hospital,
Praed St., London W2 1NY, United development of sophis- ticated automated blood-cell analyzers, the
King- dom, or at b.bain@imperial.ac.uk. proportion of blood-count sam-
ples that require a blood smear has steadily diminished and in many clinical settings
N Engl J Med 2005;353:498-
507. is now 10 to 15 percent or less. Nevertheless, the blood smear remains a crucial
Copyright © 2005 Massachusetts Medical diagnos- tic aid. The proportion of requests for a complete blood count that
Society.
generate a blood smear is determined by local policies and sometimes by financial
A related slide show is available at and regulatory as well as medical considerations. For maximal information to be
www.nejm.org derived from a blood smear, the examination should be performed by an experienced
and skilled person, either a lab- oratory scientist or a medically qualified hematologist
or pathologist. In Europe, only laboratory-trained staff members generally “read” a
blood smear, whereas in the Unit- ed States, physicians have often done this.
Increasingly, regulatory controls limit the role of physicians who are not laboratory-
certified. Nevertheless, it is important for physicians to know what pathologists or
laboratory hematologists are looking for and should be looking for in a smear. In
comparison with the procedure for an automated blood count, the examination of a
blood smear is a labor-intensive and therefore rela- tively expensive investigation and
must be used judiciously.
A physician-initiated request for a blood smear is usually a response to perceived
clinical features or to an abnormality shown in a previous complete blood count. A
lab- oratory-initiated request for a blood smear is usually the result of an abnormality
in the complete blood count or a response to “flags” produced by an automated
instrument. Less often, it is a response to clinical details given with the request for a
complete blood count when the physician has not specifically requested examination
of a smear. For example, a laboratory might have a policy of always examining a
blood smear if the clin- ical details indicate lymphadenopathy or splenomegaly. The
International Society for Laboratory Hematology has published consensus criteria
(available at www.islh.org) for the laboratory-initiated review of blood smears on the
basis of the results of the au- tomated blood count. The indications for smear review
differ according to the age and sex of the patient, whether the request is an initial or
a subsequent one, and whether there has been a clinically significant change from a
previous validated result (referred to as a failed delta check). All laboratories should
have a protocol for the examination of a laboratory-initiated blood smear, which can
reasonably be based on the criteria of the International Society for Laboratory
Hematology. Regulatory groups should permit the examination of a blood smear
when such protocols indicate that it is necessary.
wh e n phys ic ian s sh oul d r eque st a bloo d sm ea r
There are numerous valid reasons for a clinician to request a blood smear (Table 1),
and these differ somewhat from the reasons why laboratory workers initiate a blood-
smear examination. Sometimes it is possible for a definitive diagnosis to be made
from a blood smear. More often, the smear is an important tool in the provision of a
differential di-
498 n engl j med 353;5 www.nejm.org august 4, 2005
The New England Journal of Medicine
Downloaded from nejm.org on September 27, 2014. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
current concepts
agnosis and the indication of further necessary
tests. The blood smear can have an important part Table 1. Clinical Indications for Examination of a Blood Smear.
in the speedy diagnosis of certain specific Features suggestive of anemia, unexplained jaundice, or both
infections. Oth- erwise, its major roles are in the Features suggestive of sickle cell disease — dactylitis or sudden splenic en-
differential diag- nosis of anemia and largement and pallor in a young child or, in an older child or adult, limb,
abdominal, or chest pain
thrombocytopenia and in the identification and
characterization of leukemia and lymphoma. Features suggestive of thrombocytopenia (e.g., petechiae or abnormal bruis-
ing) or neutropenia (e.g., unexpected or severe infection)
Features suggestive of a lymphoma or other lymphoproliferative disorder —
ane mi a lymphadenopathy, splenomegaly, enlargement of the thymus (a mediasti-
nal mass on radiology) or other lymphoid organs, skin lesions suggestive
In patients with anemia, physician-initiated exam- of infiltration, bone pain, and systemic symptoms such as fever, sweating,
itching, and weight loss
inations of blood smears are usually performed in
response to clinical features or to a previously ab- Features suggestive of a myeloproliferative disease — splenomegaly, pletho-
ra, itching, or weight loss
normal complete blood count. The presence of un-
Suspicion of disseminated intravascular coagulation*
explained jaundice, particularly if unconjugated
Acute or recent-onset renal failure or unexplained renal enlargement, particu-
hy- perbilirubinemia is also present, is an larly in a child
additional reason for a blood-smear examination.
On retinal examination, hemorrhages, exudates, signs of hyperviscosity,
Laborato- ry-initiated examinations of blood or optic atrophy
smears for pa- tients with anemia are usually the Suspicion of a bacterial or parasitic disease that can be diagnosed from a
result of a labo- ratory policy according to which blood smear
a blood smear is ordered whenever the Features suggestive of disseminated nonhematopoietic cancer — weight
hemoglobin concentration is unexpectedly low. loss, malaise, bone pain
This policy should be encour- aged, since the General ill health, often with malaise and fever, suggesting infectious mono-
consideration of the blood smear and the red-cell nucleosis or other viral infection or inflammatory or malignant disease
indices is a logical first step in the investigation
* In acute disseminated intravascular coagulation, red-cell fragments may be
of any unexplained anemia.1 Initiat- ing a smear absent.
as a reflex test also means that a further blood
sample does not have to be taken for this
purpose. Despite this wealth of information, there are
Modern automated instruments impart valuable still morphologic abnormalities that are critical in
information about the nature of anemia. They the differential diagnosis of anemia and that can
pro- vide not only a red-cell count, mean cell be determined only from a blood smear. Particu-
volume, mean cell hemoglobin (a measure of the larly important is the detection of variations in
average amount of hemoglobin in an individual cell shape and of red-cell inclusions, such as
red cell), and the mean cell hemoglobin Howell– Jolly bodies (nuclear fragments),
concentration (a measure of the average Pappenheimer bodies (hemosiderin-containing
concentration of hemoglo- bin in a cell) but also granules), and ba- sophilic stippling or punctate
newer variables that give in- formation that basophilia (altered ribosomes).
previously could be derived only from a blood
smear. These variables usually include the red- hemolytic anemia
cell–distribution width, which correlates on a In the hemolytic anemias, red-cell shape is of
blood smear with anisocytosis, and they may also con- siderable diagnostic importance. Some
include the hemoglobin-distribution width and types of hemolytic anemia yield such a
the percentages of hypochromic and distinctive blood smear that the smear is often
hyperchromic cells, which correlate with sufficient for diagno- sis. This is true of
anisochromasia, hypo- chromia, and hereditary elliptocytosis (which is only
hyperchromia. A variety of histograms and infrequently associated with anemia) (Fig.
scatterplots give a visual representation of red- 1A) (a slide show is included in the
cell characteristics. It may be possible to detect Supplementary Appendix, available with the full
in- creased numbers of hyperchromic cells text of this article at www.nejm.org), hereditary
(spherocytes or irregularly contracted cells), small pyropoikilocytosis (Fig. 1B), and Southeast
hyperchromic cells (microspherocytes), Asian ovalocytosis, a dis- tinctive type of inherited
hypochromic microcyt- ic cells, large hemolytic anemia that is common in some parts
normochromic cells (normally hemo- globinized of Southeast Asia and is
macrocytes), and hypochromic macro- cytes
(either reticulocytes or dysplastic red cells).
n engl j med 353;5 www.nejm.org august 4, 2005
499
The new england journa l of medicine
now also seen in Europe and North America as a of considerable clinical significance, since this
result of immigration (Fig. 1C). The presence of type of anemia may indicate pregnancy-
spherocytes is not diagnostically specific, since associated hy- pertension, disseminated cancer,
this may result from hereditary spherocytosis, chronic dissemi- nated intravascular coagulation,
autoim- mune hemolytic anemia, or alloimmune the hemolytic–ure- mic syndrome, or thrombotic
hemolytic anemia (e.g., hemolytic disease of the thrombocytopenic purpura; the latter two
newborn or a delayed transfusion reaction). conditions both require ur- gent diagnosis so that
Nevertheless, con- sideration of the clinical appropriate management can be initiated. In
features, together with the results of a direct microangiopathic hemolytic anemia, examination
antiglobulin test, in patients with spherocytes will of the blood smear is also important to validate
generally indicate the correct diag- nosis. the platelet count, since red-cell frag- ments and
Microspherocytes (i.e., cells that are both hy- platelets may be of similar size. Most au- tomated
perchromic and significantly reduced in size and instruments cannot make this distinction. A
therefore in diameter) may be present in low minority of automated instruments that measure
num- bers in patients with a spherocytic both the size and the refractive index of small
hemolytic ane- mia but are also characteristic of parti- cles in the blood sample can make this
burns and of mi- croangiopathic hemolytic distinction and can be used to exclude red-cell
anemia. The detection of a microangiopathic fragmentation; however, although the fragment
hemolytic anemia (Fig. 1D) is “flag” on such in- struments is sensitive, it is not
specific. Hence, a
A B
C D
Figure 1. Hemolytic Anemias, Characterized by Different Types of Poikilocytes.
In Panel A, the blood smear shows hereditary elliptocytosis, with numerous elliptocytes and smaller numbers of ovalo-
cytes. Panel B shows hereditary pyropoikilocytosis; there is striking poikilocytosis, with elliptocytes, ovalocytes, and frag-
ments. In Panel C, Southeast Asian ovalocytosis shows moderate poikilocytosis, with the poikilocytes including several
macro-ovalocytes (arrows). Panel D shows microangiopathic hemolytic anemia resulting from cyclosporine therapy,
with numerous red-cell fragments. All specimens were stained with May–Grünwald–Giemsa stain.
500 n engl j med 353;5 www.nejm.org august 4, 2005
current concepts
blood smear is still advised for validation.2 hemolysis is most often seen in glucose-6-phos-
Blood- smear features similar to those seen in phate dehydrogenase (G6PD) deficiency but can
microan- giopathic hemolytic anemia are also a also occur with other defects in the pentose shunt
feature of mechanical hemolytic anemia, such as or in glutathione synthesis and when oxidant
that associ- ated with a leaking prosthetic valve, expo- sure overwhelms normal protective
and provide im- portant evidence of this cause of mechanisms. Oxidant damage may be exogenous,
hemolytic anemia. as in exposure to oxidant chemicals or drugs (most
A blood smear is particularly important in the often dapsone), or endogenous, as in Wilson’s
diagnosis of acute hemolysis induced by oxidant disease.3
damage. The characteristic feature is the presence G6PD deficiency affects millions of persons
of keratocytes, or “bite” cells (Fig. 2A and the worldwide. A blood smear is important for the di-
Sup- plementary Appendix), “blister” cells (Fig. agnosis of this condition, for two reasons. First,
2B), and irregularly contracted cells (Fig. 2B); the it is available far more rapidly than are the results
latter must be distinguished from spherocytes of a G6PD assay and, when considered together
(Fig. 2C) be- cause of the quite different with the patient’s ethnic origin and clinical
diagnostic significance. These irregularly history, per- mits a provisional diagnosis. Second,
contracted cells share with sphero- cytes the lack a blood smear can suggest the diagnosis of G6PD
of central pallor but differ in that they have an deficiency even if a G6PD assay is normal.
irregular outline. Oxidant-induced Normal G6PD activity
A B
C D
Figure 2. Red-Cell Changes in Various Types of Hemolytic Anemia.
The blood smear in Panel A depicts acute hemolysis in glucose-6-phosphate dehydrogenase (G6PD) deficiency, with
the presence of a “bite” cell, or keratocyte (arrow). Panel B shows acute hemolysis in G6PD deficiency, with two
“blister cells” (arrows), as well as polychromatic macrocytes and irregularly contracted cells (arrowheads). In Panel C,
hereditary spherocytosis is characterized by numerous spherocytes (hyperchromatic cells with a regular outline). Panel
D shows paroxysmal cold hemoglobinuria, with erythrophagocytosis; the arrow points to a red cell that has been
phagocytosed by a neutrophil. All specimens were stained with May–Grünwald–Giemsa stain.
n engl j med 353;5 www.nejm.org august 4, 2005
501
The new england journa l of medicine
may be found after acute hemolysis in G6PD- ther investigation and a trial of treatment are
defi- cient persons in two situations. First, men of need- ed. Liver disease and excess ethanol
Afri- can or African-American ancestry who are consumption are common causes of macrocytosis,
hemizy- gous for the A¡ alloenzyme (which is with the blood smear usually showing round rather
present at normal levels in reticulocytes) can than oval mac- rocytes and lacking
have normal G6PD levels because the reticulocyte hypersegmented neutrophils; target cells and
count is high after hemolysis. Second, female stomatocytes may also be present.
carriers — for ex- ample, those who are In elderly patients, the myelodysplastic syn-
hemizygous for the common Mediterranean dromes are an important cause of macrocytosis.
variant of G6PD — can have a nor- mal assay Blood-smear features that may point to the
result after an acute hemolytic episode because diagno- sis include hypogranular or
the abnormal cells have lysed preferential- ly, hypolobulated neu- trophils (Fig. 3B), blast cells
leaving mainly the cells expressing the normal (Fig. 3B), giant or hy- pogranular platelets,
allele in the circulation. In both of these circum- Pappenheimer bodies (Fig.
stances, the observation of a typical blood smear 3C), and the presence of a minor population of
in an appropriate clinical setting is an indication hy- pochromic microcytic cells, leading to a
to repeat the assay once the acute hemolytic dimorphic smear (Fig. 3C). Macrocytic anemia
episode is over. resulting from congenital dyserythropoietic
Other features may aid in the differential diag- anemia also yields a characteristic blood smear,
nosis of hemolytic anemia. For example, the with striking poikilocy- tosis (Fig. 3D). When
pres- ence of red-cell agglutinates usually macrocytosis is the result of hemolysis or recent
indicates the presence of a cold agglutinin, and blood loss, the blood smear shows
erythrophagocy- tosis is often a feature of polychromasia, which results from an in- creased
paroxysmal cold hemo- globinuria (Fig. 2D). reticulocyte count.
macrocytic anemia microcytic anemia
The blood smear is of great importance in the dif- The blood smear is generally less important in
ferential diagnosis of macrocytic anemias. For pa- the differential diagnosis of the microcytic than
tients in whom there is a deficiency of vitamin the macrocytic anemias. Red-cell indices and
B12 or folic acid, the blood smear shows not only serum ferritin levels, sometimes supplemented
mac- rocytes but also oval macrocytes and by mark- ers of inflammation, that are interpreted
hypersegment- ed neutrophils (Fig. 3A and the in the con- text of clinical features, permit the
Supplementary Ap- pendix). When the anemia is diagnosis of the majority of cases. However, it is
more severe, there may be marked poikilocytosis, important to note that the presence of
with teardrop poikilo- cytes and red-cell Pappenheimer bodies and red- cell dimorphism in
fragments. Although these defi- ciency states are the sideroblastic anemias and of basophilic
now usually recognized on the ba- sis of assays of stippling in cases of lead poisoning (Fig. 4A and
vitamin B12 and folic acid, the blood smear the Supplementary Appendix) and in some types
remains important for two reasons. First, it of thalassemia is diagnostically sig- nificant.
permits a speedy provisional diagnosis, and initia-
tion of appropriate treatment in severely anemic hemoglobinopathy and thalassemia
patients while assay results are pending. Second, A blood smear is useful in the diagnosis and
occasionally there are patients with a clinically sig- differ- ential diagnosis of sickle cell disease,
nificant vitamin B12 deficiency despite a normal particularly if there is an urgent need for
as- say result. This discrepancy occurs because diagnosis and if the re- sults of hemoglobin
much of the vitamin B12 that is measured in the electrophoresis or high-per- formance liquid
assay is bound to haptocorrin, whereas the chromatography are not instantly available.
functional vita- min B12, which is bound to Patients with sickle cell anemia (in which there is
transcobalamin, con- tributes much less to the homozygosity for hemoglobin S) have ane- mia,
assay of total B12. but those with compound heterozygosity for
Similarly, acute folic acid deficiency sometimes hemoglobin S and hemoglobin C may have a
develops in patients even though the total red-cell nor- mal hemoglobin level, and the condition thus
folate level remains normal. The observation of a may be confused with sickle cell trait if a blood
blood smear that is typical of megaloblastic ane- smear is not examined. Consideration of the
mia despite normal assays is an indication that blood-smear features, of the hemoglobin level,
fur- and of the results of a sickle cell solubility test
usually permits an ac-
502 n engl j med 353;5 www.nejm.org august 4, 2005
current concepts
A B
C D
Figure 3. Red-Cell Changes in Various Types of Macrocytic Anemia.
Pernicious anemia is shown in the blood smear in Panel A, with anisocytosis, macrocytosis, and a hypersegmented neu-
trophil. Panel B shows myelodysplastic syndrome, with a blast cell (arrow) and two neutrophils that have hypolobulated
nuclei, one of which is binucleated and the other hypogranular. Panel C shows myelodysplastic syndrome with anisocy-
tosis, poikilocytosis, macrocytes, stomatocytes, and an erythrocyte with prominent Pappenheimer bodies (arrow); the
smear is also dimorphic, showing both well-hemoglobinized macrocytes and hypochromic microcytes. Panel D depicts
type 1 congenital dyserythropoietic anemia, with anisocytosis, poikilocytosis, and some macrocytes. All specimens were
stained with May–Grünwald–Giemsa stain.
curate diagnosis4,5 (Fig. 4B and 4C). The blood condition (Fig. 4D); sometimes there is coexist-
smear of a compound heterozygote usually shows ing thrombocytopenia.
target cells, irregularly contracted cells, and boat-
shaped cells but few classic sickle cells; typical
he- moglobin SC poikilocytes (formed only when
th rom bo cy to p en i a
an d t hro mb oc yt osi s
he- moglobin S and hemoglobin C are both
present) are often seen. Sometimes the blood A blood smear should always be examined for pa-
smear of a compound heterozygote shows only tients with thrombocytopenia, both to confirm the
target cells and irregularly contracted cells and thrombocytopenia and to look for the underlying
cannot be dis- tinguished from the smear in cause. Falsely low platelet counts may be the
hemoglobin C homo- zygosity; a positive sickle result of small clots, platelet clumping (Fig. 5A
cell solubility test per- mits these conditions to and the Supplementary Appendix), platelet
be distinguished in an emergency situation (e.g., satellitism (Fig.
preoperatively). A blood smear is also important 5B), or abnormally large platelets. Fibrin strands
in the diagnosis of an un- stable hemoglobin, (Fig. 5C) indicate that thrombocytopenia is likely
with irregularly contracted cells and to be factitious. Underlying causes that may be
macrocytosis being characteristic of this re- vealed by the blood smear include the May–
Hegglin
n engl j med 353;5 www.nejm.org august 4, 2005
503
The new england journa l of medicine
anomaly (Fig. 5D), microangiopathic thrombopa-
l e u k e m i a , l y m p h o m a , o r b on e
thies, and leukemias and lymphomas. High plate- m ar ro w f ai lu r e
let counts should be confirmed microscopically
with a blood smear; falsely high counts may be Blood smears must always be examined when
the result of other particles (red-cell fragments, there is unexplained leukocytosis, lymphocytosis,
frag- ments of leukemic cells, or fungi) being or monocytosis or when the flagging system of an
counted as platelets.6-9 Examination of the blood automated instrument suggests the presence of
smear is also important in patients with blast cells. Depending on the instrument and the
thrombocytosis to look for evidence of a practice of the local laboratory, a flag for atypical
myeloproliferative disorder, such as giant or variant lymphocytes may also be an indication
platelets, or an increase in the basophil count; for examination of a blood smear, since this flag
the latter is not reliably detected by auto- mated is sometimes indicative of the presence of blast
counters. A sudden, unexpected improve- ment cells. Low rather than high counts likewise are an
in the platelet count also should be confirmed by indi- cation for a smear, since they may be
blood-smear examination, since such an im- indicative of aplastic anemia, acute leukemia,
provement may be factitious7 (Fig. 5E). hairy-cell leuke-
A B
C D
Figure 4. Red-Cell Changes with Lead Poisoning and in Hemoglobinopathies.
Panel A shows an erythrocyte with prominent basophilic stippling (arrow), a result of lead poisoning. Panel B shows
sickle cell anemia, with a nucleated red cell (black arrow), sickle cells (white arrow), and boat-shaped cells
(arrowhead). Panel C shows sickle cell–hemoglobin C disease, with target cells, irregular contracted cells, and two
hemoglobin SC poikilocytes (arrows). Panel D demonstrates heterozygosity for hemoglobin Hammersmith (an
unstable hemoglobin), with irregularly contracted cells (arrows). All specimens were stained with May–Grünwald–
Giemsa stain.
504 n engl j med 353;5 www.nejm.org august 4, 2005
current concepts
mia, or infiltration of nonhematopoietic malignant produces a highly improbable result. Such results
cells into the bone marrow. The role of the blood may be factitious, resulting from the accidental
smear in the diagnosis of leukemia and freezing or heating of the blood, from
lymphoma is to suggest a likely diagnosis or hyperlipide- mia, or from the presence of cold
range of diag- noses, to indicate which additional agglutinins, a cry- oglobulin (Fig. 6C), bacteria,
tests should be performed, and to provide a or fungi. Factitious results also may stem from
morphologic context without which unusual characteristics of the blood cells or the
immunophenotyping and other so- phisticated plasma, such as a pseudo- neutropenia caused by
investigations cannot be interpreted. For two a myeloperoxidase deficien- cy that occurs when
conditions, Burkitt’s lymphoma (Fig. 6A and the the automated instrument em- ploys a peroxidase
Supplementary Appendix) and acute pro- reaction for the identification of neutrophils,
myelocytic leukemia (Fig. 6B), a blood smear is eosinophils, and monocytes. Falsely low counts
of particular importance because it facilitates also may result from neutrophil or plate- let
rapid diagnosis and specific treatment. clumping or from platelet satellitism.
pr ob ab l e fa ct it io u s re sul t s s er en d ip it y
Members of the laboratory staff should always Occasionally, a blood smear leads to a fortuitous
ini- tiate a blood smear if an automated diagnosis that can be very important to the patient
instrument
A B
C D E
Figure 5. Blood-Smear Features Associated with Thrombocytopenia and Errors in the Platelet Count.
Panel A shows large clumps of platelets that led to a factitiously low platelet count. Panel B demonstrates platelet satel-
litism. Panel C shows fibrin strands (arrow). Panel D shows the May–Hegglin anomaly, with large platelets and a
charac- teristic neutrophil inclusion (arrow). Panel E shows Candida glabrata (arrows) that led to a sudden, unexpected
improvement in the “platelet” count. All specimens were stained with May–Grünwald–Giemsa stain.
n engl j med 353;5 www.nejm.org august 4, 2005
505
The new england journa l of medicine
A B
C D
Figure 6. Miscellaneous Conditions in Which the Blood Smear Can Be Diagnostically Important.
Panel A shows Burkitt’s lymphoma, with three basophilic vacuolated lymphoma cells. Hypogranular promyelocytic
leukemia is shown in Panel B, with two characteristic bilobed leukemic promyelocytes. Panel C depicts cryoglobulin
deposition in a blood sample from a patient with hepatitis C virus infection. Panel D shows target cells (short arrow),
acanthocytes (long arrow), and a Howell–Jolly body (arrowhead) — all features of hyposplenism — in a blood smear
from a patient with iron-deficiency anemia and splenic atrophy as features of celiac disease. All specimens were stained
with May–Grünwald–Giemsa stain.
(Table 2). As an example, the detection of
t h e b l o o d s m e a r as par t
features of unexpected hyposplenism (Fig. 6D) o f th e me d ic a l recor d
may suggest a congenital absence of the spleen,
splenic atrophy, deposition of amyloid in the Sometimes the blood smear provides the primary
spleen, infiltration of neoplastic cells (e.g., in or the only evidence of a specific diagnosis, such
leukemia, lymphoma, or carcinoma) in the as myelodysplastic syndrome, leukemia,
spleen, previous splenic infarc- tion, or even a lymphoma, or hemolytic anemia. It is important
splenectomy of which the patient was unaware that, if possi- ble, such blood smears be stored
— in each case putting the patient at risk for over the long term, just as a tissue that provides a
complications of hyposplenism. Converse- ly, the histologic diagnosis is stored over the long term.
failure to observe expected hyposplenism in a In practice, such stor- age is easily achieved if a
blood smear from a patient who has undergone patient has also had a bone marrow aspirate
splenectomy for the treatment of autoimmune (since a blood smear should al- ways be stored
thrombocytopenic purpura may indicate that there with an aspirate), but it is harder to achieve if the
is functioning residual splenic tissue, either from blood smear alone has provided the diagnosis.
splenosis or from accessory spleens, that may be Individual laboratories should have a
responsible for a relapse of the disease. mechanism to make possible the retention of
such
506 n engl j med 353;5 www.nejm.org august 4, 2005
current concepts
smears or an image derived from them. Some Table 2. Fortuitous Observations That May Be of Diagnostic Importance.
lab- oratories retain all smears that have been
reviewed by a laboratory hematologist or Red-cell fragmentation
Hyposplenism
pathologist; this can create a storage problem,
Cryoglobulinemia (may indicate hepatitis C virus infection or a plasma-cell
and it is likely that, increasingly, digital images of neoplasm)
important abnormal smears will be stored. Red-cell agglutinates (may indicate cold agglutinins, as in mycoplasma infec-
tion, infectious mononucleosis, or lymphoproliferative disorder)
Dysplastic features typical of human immunodeficiency virus infection
th e fu tu r e Presence of leukemic blasts or lymphoma or myeloma cells
The continuing importance of the blood smear is Malaria or other parasitic infections (usually malaria but occasionally babesi-
highlighted by the recent introduction of photo- osis, leishmaniasis, African trypanosomiasis, Chagas’ disease, or filariasis)
graphs of blood smears as a regular feature in Fungal infection (e.g., candidiasis, histoplasmosis)
Bacteria (relapsing fever, ehrlichiosis, meningococcal or pneumococcal
both the journal Blood10 and the British Journal of infection)
Haema-
tology, by ongoing efforts to develop image-recog-
nition technology for the automated examination
of blood smears, and by the development of tele- ry staff should make and examine a blood smear
hematology to permit the remote interpretation or whenever the results of the complete blood count
second opinions of blood smears.11,12 indicate that a blood smear is essential for the
vali- dation or the further elucidation of a
c on c lu sion s detected ab- normality. If error is to be avoided,
sophisticated modern investigations of
Even in the age of molecular analysis, the blood hematologic disorders should be interpreted in
smear remains an important diagnostic tool. Physi- the light of peripheral-blood features as well as the
cians should request a blood smear when there are clinical context.
clinical indications for it. Members of the I am indebted to Dr. Bernadette Garvey of Toronto and Dr.
laborato- LoAnne
Peterson of Chicago for their helpful comments on the manuscript.
re f e re nc e s
1. Case Records of the Massachusetts Gen- cell-haemoglobin C disease. Br J Haematol 9. Kakkar N. Spurious rise in the automat-
eral Hospital (Case 30-2004). N Engl J Med 1993;83:516-8. ed platelet count because of bacteria. J Clin
2004;351:1333-41. 6. Latif S, Veillon DM, Brown D, et al. Pathol 2004;57:1096-7.
2. Lesesve JF, Salignac S, Alla F, et al. Com- Spurious automated platelet count: enu- 10. Shattil SJ. A (blood) smear campaign.
parative evaluation of schistocyte counting meration of yeast forms as platelets by the Blood 2003;101:2453.
by an automated method and by microscop- Cell-DYN 4000. Am J Clin Pathol 2003;120: 11. Abramson N. Inside blood: a picture (in
ic determination. Am J Clin Pathol 2004;121: 882-5. the microscope) is worth a thousand words.
739-45. 7. Arnold JA, Jowri Z, Bain BJ. Candida gla- Blood 2004;103:367-8.
3. Bain BJ. Heinz body haemolytic anaemia brata in a blood smear. Br J Haematol 1999; 12. Luethi U, Risch L, Korte W, Bader M,
in Wilson’s disease. Br J Haematol 1999;104: 104:1. Huber R. Telehematology: critical determi-
647. 8. van der Meer W, MacKenzie MA, Din- nants for successful implementation. Blood
4. Diggs LW, Bell A. Intraerythrocytic he- nissen JW, de Keijzer MH. Pseudoplatelets: 2004;103:486-8.
moglobin crystals in sickle cell-hemoglobin a retrospective study of their incidence and Copyright © 2005 Massachusetts Medical Society.
C disease. Blood 1965;25:218-23. interference with platelet counting. J Clin
5. Bain BJ. Blood smear features of sickle Pathol 2003;56:772-4.
n engl j med 353;5 www.nejm.org august 4, 2005
507
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
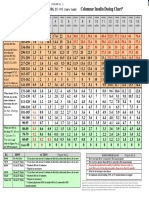
- Columnar Insulin Dosing Chart : (1 ML 1 Unit)Document1 pageColumnar Insulin Dosing Chart : (1 ML 1 Unit)Philippe KinnaerNo ratings yet
- DR Okoruwa-Advancing Sustainable Cold Chain Dev. in NigeriaDocument27 pagesDR Okoruwa-Advancing Sustainable Cold Chain Dev. in NigeriaAugustine Okoruwa50% (2)
- Monte Vista Journal Public Service EntryDocument25 pagesMonte Vista Journal Public Service EntryJennifer AlonzoNo ratings yet
- Introduction To BiostatisticsDocument64 pagesIntroduction To BiostatisticsFadel DeebNo ratings yet
- A Balanced Diet : My Meals (Day 2)Document9 pagesA Balanced Diet : My Meals (Day 2)Rosa Maria Carita VelaNo ratings yet
- B Value DwiDocument5 pagesB Value DwiSergio SanNo ratings yet
- COVID-19 Vaccination Appointment Details: Center Preferred Time SlotDocument1 pageCOVID-19 Vaccination Appointment Details: Center Preferred Time SlotProbhat KumarNo ratings yet
- Japchae (Korean Glass Noodles) With Tofu - Jessica GavinDocument2 pagesJapchae (Korean Glass Noodles) With Tofu - Jessica GavinMichelle BragaNo ratings yet
- Week 3-Fringe Benefit TaxDocument51 pagesWeek 3-Fringe Benefit TaxMARCIAL, Althea Kate A.No ratings yet
- 02 Lecture Kaltenborn Mobilization GradesDocument50 pages02 Lecture Kaltenborn Mobilization GradesSeriopediaNo ratings yet
- Project ReportDocument60 pagesProject ReportPrashant Bankar33% (6)
- Sop Chlorine and Ammonia GasesDocument3 pagesSop Chlorine and Ammonia GasesSE ESTNo ratings yet
- 6Document8 pages6gsk_87No ratings yet
- 1.warm-Up, Work-Out Proper and Cool DownDocument22 pages1.warm-Up, Work-Out Proper and Cool DownMG GadonNo ratings yet
- IRS 3500a Form For California Tax-ExemptionDocument1 pageIRS 3500a Form For California Tax-ExemptionjhbjhbkjhNo ratings yet
- NICE ProceedingsDocument63 pagesNICE Proceedingssn_b5No ratings yet
- RK500-04 Fluorescence Principle DO Sensor Specification v3.0Document2 pagesRK500-04 Fluorescence Principle DO Sensor Specification v3.0Hossein AkbariNo ratings yet
- FINAL - Datwyler Healthcare IM WhitepaperDocument15 pagesFINAL - Datwyler Healthcare IM Whitepaperpascal candillonNo ratings yet
- Intrapartum NCM 101Document92 pagesIntrapartum NCM 101Ellenare RacionNo ratings yet
- 3490 Male Classic Records 15-08-23Document2 pages3490 Male Classic Records 15-08-23TheOne HomosapienNo ratings yet
- SDB - Farbanthren Yellow 3RT - 3579-20 - V1.1 - en - DEDocument8 pagesSDB - Farbanthren Yellow 3RT - 3579-20 - V1.1 - en - DEWaqas AhmedNo ratings yet
- Aetiology and Management 0F Septic ArthritisDocument61 pagesAetiology and Management 0F Septic Arthritissapa hayoNo ratings yet
- Studies On The Effects Cymbopogon Citratus, Ceiba Pentandra and Loranthus Bengwelensis Extracts On Species of Dermatophytes.Document12 pagesStudies On The Effects Cymbopogon Citratus, Ceiba Pentandra and Loranthus Bengwelensis Extracts On Species of Dermatophytes.Freddy Albaro Manayay LLaguentoNo ratings yet
- Bahasa Inggris SPMB 2002 Regional IIIDocument3 pagesBahasa Inggris SPMB 2002 Regional IIIatikah_s0% (1)
- Grade 12 Test Banks 2nd Term Model AnswersDocument101 pagesGrade 12 Test Banks 2nd Term Model AnswersLami DabaNo ratings yet
- Thesis Statement, Topic Sentence, and Supporting Details: Paul Christian Reforsado AbadDocument29 pagesThesis Statement, Topic Sentence, and Supporting Details: Paul Christian Reforsado AbadMicole BrodethNo ratings yet
- Ghee Its Chemistry Processing and Technology PDFDocument7 pagesGhee Its Chemistry Processing and Technology PDFpaulxe100% (2)
- Application of Stem CellsDocument20 pagesApplication of Stem Cellsupkarveerkaur100% (1)
- Radiography For EndodonticsDocument116 pagesRadiography For EndodonticsAndreea Mihaela100% (1)
- Exploring The Impact of The Super Bowl On Sex Trafficking - FULL REPORTDocument16 pagesExploring The Impact of The Super Bowl On Sex Trafficking - FULL REPORTmccaininstituteNo ratings yet