Professional Documents
Culture Documents
Characteristics and Uses of Biologic Dressings
Uploaded by
Esq. Nelson OduorCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Characteristics and Uses of Biologic Dressings
Uploaded by
Esq. Nelson OduorCopyright:
Available Formats
Characteristics and Uses of Biologic Dressings
and Skin Substitutes
Basil A. Pruitt, Jr, MD, Norman S. Levine, MD
\s=b\ Biologic dressings used for temporary coverage of open skin. Cutaneous allograft is the most frequently used and
wounds exert both mechanical and physiologic effects by most effective biologic dressing. All other such dressings
protecting the wound, maintaining microbial control, and must be compared with allograft to determine their relative
hastening wound maturation. Synthetic wound dressings effectiveness and rank in the hierarchy of biologic dress¬
modeled after the biologic dressings have been evaluated by
several investigators. Those studies have shown unilaminate
ings. In addition to what might be termed natural biologic
synthetic membranes to be ineffective when applied to full\x=req-\ dressings, a variety of synthetic skin substitutes have been
thickness wounds and have identified a bilaminate construc- fabricated since Ivalon sponge (a polyvinyl alcohol polymer
tion as being necessary for membranes to serve as effective with a thin outer layer of silicon rubber; Unipoint Indus¬
skin substitutes. The desirable properties of skin substitutes tries, High Point, NC) was first introduced in 1961, and
have been identified and incorporated in the design of recently recently developed materials have shown promise in early
developed membranes. Recent studies in this and other labo- clinical trials.
ratories have resulted in the development of collagen-syn-
thetic bilaminates, a totally synthetic biologically inert bilami- PROPERTIES AND USES OF BIOLOGIC DRESSINGS
nate, and tissue culture\p=n-\derivedmembranes. The characteris- A variety of beneficial effects have been attributed to
tics and limitations of each skin substitute determine the biologic dressings and, to a greater or lesser (usually lesser)
optimum usage of these composite membranes and define the extent, to synthetic skin substitutes. In areas where a
modifications needed to improve the effectiveness of such
dressings. biologic dressing adheres to the underlying wound bed, the
(Arch Surg 1984;119:312-322) population density of bacteria on the wound surface de¬
creases; the dressing also aids in microbial control when
closure of a wound by the use of material
topical therapy has been discontinued following debride-
Temporary
other than the patient's own skin has become com¬
ment of the bulk of the nonviable burned tissue.1 In
where there is no adherence of a biologic dressing to the
areas
monplace during the past two decades. Biologic dressings wound bed, submembrane suppuration commonly occurs,
play a key role in the treatment of those patients whose and it appears to hasten debridement of residual nonviable
extensive burns leave so little available donor site that their
wounds cannot be covered by a single harvest of autografi
tissue, presumably by the combined action of both bacterial
and WBC enzymes. By physically covering the burn wound,
biologic dressings prevent desiccation of an open wound and
Accepted for publication Nov 7, 1983. decrease evaporative water loss and heat loss. Physical
From the US Army Institute of Surgical Research, Fort Sam Houston,
Tex (Dr Pruitt); and the Division of Plastic Surgery, Oklahoma University
protection of the wound by a biologic dressing also prevents
Health Science Center, Oklahoma City (Dr Levine).
further contamination and injury of the newly developing
The opinions or assertions contained herein are the private views of the granulation tissue. Application of allograft skin also de¬
authors and are not to be construed as official or as reflecting the views of creases wound pain, which, in the case of burns overlying
the Department of the Army or the Department of Defense.
Reprint requests to Librarian, US Army Institute of Surgical Research, joints, facilitates motion of the burned part and the execu¬
Fort Sam Houston, TX 78234. tion of the daily physical therapy program. Finally, the
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
biologie dressings appear to hasten and make more orderly desiccation and a resulting rapid sloughing of the graft.
the healing of second-degree burns; when applied to full- Amnion adherence to the wound bed is also less secure than
thickness burns, they increase granulation tissue capillary is that of cutaneous allograft, and true biologic union with
density.2 host-to-graft vascular connection is uncertain.8 Faulk et al
The beneficial effects of allograft skin are realized when it have reported that application of amnion to wounds exerts
is used for coverage of full-thickness burn wounds after an angiogenic effect and increases the capillary density of
eschar separation and prior to autograft application, and for the underlying wound bed.9
immediate coverage of superficial second-degree burns to Cutaneous xenografts from a variety of species have been
hasten healing. Coverage with allograft skin of excised burn used clinically with porcine material (fresh, fresh-frozen,
wounds and other wounds such as those resulting from and lyophilized) commercially available from several
mechanical trauma or operative procedures that cannot be sources. The sterility and viability of some commercially
closed primarily is also beneficial. Also, allograft skin can available fresh and fresh-frozen porcine xenograft skin has
be used as a test material to determine the likelihood of been uncertain, and contamination of such material, even by
autograft take. When allograft skin shows general ad¬ organisms that are ordinarily considered saprophytic, rep¬
herence to a burn wound and evidence of graft vasculariza- resents a potential risk for the severely burned patient
tion within 48 to 72 hours of application, one can anticipate whose immunologie capacity has been markedly compro¬
an excellent take of autograft skin applied to that wound mised. Porcine cutaneous xenografts are not as effective as
following removal of the allograft skin. Such preparation of cutaneous allografts in reducing the bacterial population
a "receptive" wound bed is particularly important in the density of the underlying wound.10 Moreover, cutaneous
care of those patients with extensive burns and a paucity of xenografts adhere to wound beds less well than do cutane¬
donor sites, to avoid unnecessary loss of autograft skin. ous allografts. The graft-to-host union appears to be ef¬
Allograft skin can be obtained from a family member or fected by fibrovascular ingrowth of granulation tissue into
other living volunteer, but is most commonly harvested the dermis of the graft, and vessel-to-vessel connection
from the bodies of patients who have died in the hospital. between host and graft does not occur as it does with
Consequently, the supply of allograft does not always match cutaneous allografts." The nourishment of the outer layers
the demand for such tissue. Other limitations of fresh of xenograft skin appears to be dependent on a limited
allograft skin include the need for refrigerated storage plasmatic circulation, and the material undergoes progres¬
conditions and a limited "effective" shelf life of approx¬ sive degenerative necrosis rather than classic rejection.
imately seven to ten days when the tissue is stored at 4 °C.3 Moreover, secure union of the graft to the wound bed
The viability and take of allograft skin decrease with time develops over a period of days, during which time the grafts
after harvest and are greatest when allograft skin is used and the involved body part must be immobilized.
immediately after harvest. The possibility of disease trans¬ One additional concern limits the use of all wound dress¬
mission requires careful donor selection. The elimination of ings. If dressings are applied to a heavily contaminated
potential donors with cutaneous malignant neoplasms and wound, marked subgraft microbial proliferation and suppu¬
infections, systemic viral disease such as hepatitis, and ration may occur and rapidly progress to frank infection. In
hématologie malignant disease reduces the size of the donor the case of partial-thickness burns, such infection may
pool available for the harvest of allograft skin. convert the injury to full-thickness necrosis. In the case of
Fresh-frozen allograft skin and lyophilized allograft skin full-thickness burns, the infection may become invasive,
each overcome some of the limitations encountered with the with involvement of local unburned tissue and even, by
fresh material, but have limitations of their own.4·5 The systemic dissemination, remote tissues and organs. To
demanding processing procedures and requirements con¬ avoid that complication, biologic dressings should not be
fine the preparation of either material to special centers applied to deep, partial-thickness burns prior to removal of
having proper facilities. The lyophilized material has an the superficial debris, to full-thickness burns prior to
essentially unlimited nonrefrigerated shelf life, while the eschar separation or removal, or to any wound with a
frozen material has a similarly prolonged shelf life provided bacterial population density of over 105 organisms per gram
proper refrigeration is maintained. Either material can be of tissue, as determined by biopsy monitoring of the burn
easily and rapidly prepared for use by rehydration or wound.
thawing. When harvested at a thickness of greater than Although cutaneous graft viability appears, on the basis
0.381 mm, the lyophilized material is subject to epidermal- of clinical experience, to be important in the control of the
dermal separation that permits desiccation of the subse¬ subgraft microbial population, wound dressing viability
quently exposed dermis and rapid sloughing of the material does not appear to be essential in terms of physical coverage
from the wound. Lyophilized allograft skin generally ad¬ of excised wounds or systemic resistance to infectious
heres less well to the wound and is less able to reduce the challenge following excision of extensive burn wounds. In a
bacterial count on the wound surface than fresh allograft murine model, excision of 60% of the skin results in essen¬
skin.6 tially uniform mortality if the excised area remains uncov¬
Amnion, which has also been used as a biologic wound ered, is covered with fine-mesh gauze, or is covered with an
dressing, is readily available from the delivery room and is impermeable membrane such as Vi-drape surgical drape
inexpensive to prepare.7 When applied to a wound, amnion material (Parke-Davis & Co, Detroit). Coverage of such
must be covered with an occlusive dressing to prevent excised wounds with either viable allograft or a synthetic
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
skin substitute results in survival of over 75% of the
animals. Other animal studies have shown protection from
the lethal effects of an intraperitoneal Pseudomonas chal¬
lenge following burning by immediate wound excision and
coverage of the excised wound with either viable allograft
skin or nonviable formaldehyde-treated allograft skin.12
These and other studies, as well as the increased use of
early burn wound excision procedures that produce wounds
requiring immediate coverage, have reawakened interest in
the development of effective wound dressings—skin substi¬
tutes.
SYNTHETIC WOUND DRESSINGS
Early Wound Dressings
A variety of synthetic wound dressings and skin substi¬
tutes have been evaluated over the past three decades, with
the earliest materials being a spray-on plastic (a copolymer
of hydroxyvinylchloride-acetate and sebacic acid),13 polyox
Fig 1.—Tissue obtained from wound bed following removal of (a polymer of ethylene oxide),1 and Ivalon sponge.14 These
polyvinyl alcohol sponge (Ivalon) dressing. Note irregular retained
fragment of polyurethane foam with intense foreign body inflam¬ materials permitted submembrane suppuration and attend¬
matory reaction in surrounding tissue. ant sepsis, especially when applied to full-thickness inju-
Fig 2.—Left, Full-thickness burn wounds on posterior aspect of leg were covered with viable
cutaneous allograft and gauze-backed, poly-amino acid film. Right, Five days after application,
allograft skin is well vascularized and adherent throughout. Film was adherent only at periphery of
wound through serous crust formation (note remnant of crust at lower margin of wound above
lateral malleolus). Elevation of film reveals that it was semiattached to the wound surface, floating
on layer of serosanguineous fluid visible on undersurface of membrane.
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
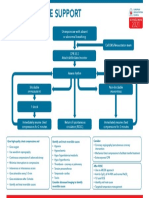
Table 1.—Parametric Analysis of the Change in Mean Log Bacterial Counts for All Wounds
Human Cadaver Porcine Cutaneous
Cutaneous Allograft Xenograft Synthetic Dressing Coarse-Mesh Gauze
Wounds on which allograft took (N = 23)
Bacterial count before treatment 4.72 4.57 4.81 4.61
Change treatment*_-1.20_+0.13_+0.02_-0.25_
in count after
SE for change_038_039_035_O40_
95% confidence limits for change_-0.44 to -1.96_-0.65 to +0.91_-0.68 to +0.72_-0.65 to +1.05
Significance of change, f test_P<.01_NS_NS_NS_
Wounds on which allograft did not take (N 18)t
=
treatment_4^23_4.77_4_24_4J2_
Bacterial count before
treatment*_+1.00_+0.57_+0.95_+0.47_
Change in count after
SE for change_0^54_+0.40_0.47_043_
+1.37_0.00
95% confidence limits for change_-0.09 to +2.09_-0.23 to to +1.90_-0.39 to +1.29
Significance change,
of f test P<.1 P<.2 P<.1 P<.3
*Minus indicates decrease in bacterial count after treatment. Plus sign indicates increase.
fFor the combined results of all four treatments for wounds on which allograft did not take, there was a change of +0.70 (P<.01, =
72).
ries with residual nonviable tissue. Ivalon fragmented on
removal, with the retained particles of sponge eliciting a
foreign-body inflammatory reaction that complicated
wound closure (Fig 1). The spray-on plastic film, when
applied to full-thickness injuries in the immediate postburn
period, was associated with the development of wound
infection, and the polyox gel, if not covered by an impermea¬
ble membrane or a dressing, rapidly desiccated and disap¬
peared.
Subsequent experience has been reported with the use of
laminated nylon velour,15 polyurethane foam laminated to
polypropylene film,16 poly-amino acid films," films of Gore-
tex (polytetrafluoroethylene; W. L. Gore & Associates,
Elkton, Md) and ultrathin (0.8 mil) silicone polymer mem¬
branes laminated to a meshed inner layer.18 The previously
noted problems of submembrane suppuration and highly
variable biologic union with irregular membrane adherence
to the wound were encountered with these materials.
Fig 3.—Unilaminate, small-pore-size polytetrafluoroethylene
Unilaminate impervious, or nearly impervious, films com¬ membrane at top was applied to underlying excised rat wound
monly adhere to the margin of a wound and a highly variable seven days prior to biopsy. Note that membrane is attached to
fraction of the wound surface by formation of a serous crust, granulation tissue that has formed on wound by dark band of
neutrophil-laden, serofibrinous exúdate.
yet are elevated from other portions of the wound surface by
a serous or seropurulent film (Fig 2). Foams and other
laminates permit suppuration within the lacunae or pores of with an average burn extent of 12% of the total body
the inner membrane above the level of the ingrowing wound surface.19 The Hydron dressing was applied to burn wounds
granulation tissue and show variable degrees of fragmenta¬ with an average extent of 5% of the body surface. The
tion on removal, with the residual fragments of the syn¬ investigators found that Hydron applied to a moist ex¬
thetic material enmeshed in the wound-bed granulation udative wound would not cure properly and easily "lifted
tissue serving as foci of inflammatory reaction. off" the wound. In more than half of the patients, the
Recently Developed Wound Dressings dressing lost its integrity, requiring either local repair or
complete reapplication. Eighty percent of the patients
Recently developed unilaminate membranes are best showed significant peeling of the dressing, especially in
considered wound dressings rather than skin substitutes. those areas where it came in contact with the bedclothes.
The Hydron (polyhydroxyethylmethacrylate; Hydron Lab¬ Submembrane serum collections often occurred, and in
oratories, Ine, New Brunswick, NJ) burn dressing is a thin eight patients these showed bacterial growth. Frank infec¬
transparent unilaminate membrane that is formed in situ on tion may occur beneath this material, and instances of septic
the burn wound. Polyhydroxyethylmethacrylate powder conversion of partial-thickness injury to full-thickness loss
and liquid polyethylene glycol are alternately sprayed on have been reported by others, sometimes in association
the burn wound to form the membrane. Warren and Snell- with systemic sepsis. Thirteen of the 15 patients studied
ing have reported on the use of this membrane in 15 patients credited the Hydron with reducing wound pain. The in-
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
vestigators concluded that the optimum use of Hydron was tion, except with those collagen membranes applied to
in the treatment of small, noncircumferential, superficial, granulation tissue, in which case only approximately one
partial-thickness burns with intact blister epithelium that third of the membrane surface was adherent to the wounds
did not cross a joint surface. by that time. Water vapor transmission through collagen
Studies by Dressier et al of the effect of Hydron on the membranes is related to membrane thickness and, in modi¬
healing of full-thickness scald burns in a murine model and fied collagen sheets 6 mils thick, approached that of burn
full-thickness excisional wounds in rabbit ears have shown wound eschar. Burn wounds fully excised seven days after
that the Hydron burn dressing exerted no deleterious burn and covered with collagen membranes showed slightly
effects on wound healing.20 The material has also been higher bacterial counts than did autografted wounds, but
reported to be useful as a donor-site dressing, but the cost of showed lower bacterial densities than did wounds to which
such a material compared with fine-mesh gauze militates for allograft or xenograft skin had been applied. Autograft
use of the latter. skin subsequently applied to wounds initially dressed with
Another unilaminate membrane in the form of a transpar¬ collagen membranes following excision showed only a 42%
ent liquid gel has been developed by Wokalek et al for use as take.
a dressing for fresh operative wounds.21 The gel is composed A collagen sponge membrane, when applied to an excised
of agar copolymerized with acrylamide. The gel is consid¬ animal wound, showed good initial adherence, but gradu¬
ered chemically inert and nonallergenic. The developers ally dried and developed a hardened outer surface as
have reported that the gel reduces wound discomfort and adherence decreased across time.26 The unilaminate col¬
that changes of the dressing are painless. The gel's trans¬ lagen membranes appear to function like a serous crust.
parency allows early identification of submembrane suppu¬ The decrease in adherence with time indicates little, if any,
ration and its porosity allows drainage of wound secretions. fibrovascular ingrowth to form an effective biologic union
The low tensile strength of the gel makes it susceptible to between wound and graft, and reflects the action of both
disruption, and the lack of firm adherence makes this microbial and host-tissue collagenase.
material a poor candidate for use as a skin substitute and
NECESSARY PROPERTIES OF SKIN SUBSTITUTES
speaks for its use solely as a temporary wound dressing.
Fibrin film has also been used as a unilaminate wound Many studies have permitted the identification of those
dressing. Nishi has reported on the use of chrome-hardened properties needed for a clinically effective skin substitute,
fibrin films in 333 burned patients.22 The films are credited which are as follows.
with having an oligodynamic effect and with reducing the Absence of antigenicity
healing time of partial-thickness burns. The material has Tissue compatibility
hemostatic properties and is considered nonantigenic and of Absence of local and systemic toxicity
low tissue reactivity. Application of the fibrin film reduced Water vapor transmission similar to normal skin
wound pain and maintained wound bacterial counts at low Impermeability to exogenous microorganisms
levels in the study patients. The investigator recommended Rapid and sustained adherence to wound surface
that the fibrin film be covered with gauze dressings to Inner surface structure that permits ingrowth of fibro¬
maintain close adherence to the wound bed. The absence of vascular tissue
a control group and of specific bactériologie data in the Flexibility and pliability to permit conformation to irreg¬
study make evaluation difficult, but the fibrin film appears ular wound surface
to function like a serous crust. Elasticity to permit motion of underlying body tissue
Collagen in various forms has been evaluated as a biologic Resistance to linear and shear stresses
dressing by several investigators. Collagen is an attractive Prevention of proliferation of wound surface flora and
skin substitute since it can be isolated from tissues of other reduction of bacterial density of wound
species and purified in large amounts, is of low antigenicity, Tensile strength to resist fragmentation and retention of
exerts a hemostatic effect, can be produced in a variety of membrane fragments when removed
physical forms, ie, gels, films, fibrils, extruded strips, Biodegradability (important for "permanently" im¬
porous mats, sponges, and powder, and can be bonded to planted membranes)
other materials for use as a composite. Generally, the Low cost
tensile strength of collagen is enhanced by chemical or Indefinite shelf life
physical means to prevent fragmentation, but such treat¬ Minimal storage requirements
ment decreases elasticity and drapability when the collagen Studies of an ultrathin silicone polymer membrane identi¬
is used as a film, sponge, or strip. The initial adherence of fied the importance of water vapor permeability of the outer
membranes to granulation tissue appears to be a fibrin- layer of bilaminate membranes in the prevention of subgraft
dependent phenomenon.23 Although fibrin binds preferen¬ fluid collections.18 The early studies of skin substitutes also
tially to native collagen, it is uncertain whether bonding indicated that the pore size of the membrane must be such
occurs between fibrin and the exogenous collagen of mem¬ that it will act as a barrier to microorganisms. Such a small
branes.24 Nevertheless, Tavis et al, using a "modified" pore size will not permit biologic union by ingrowth of
collagen membrane, found good initial adherence to wounds fibrovascular tissues from the wound bed, a process requir¬
on which bacterial population density was low.25 Increased ing a pore diameter of at least 80 µ (Fig 3).26 It appears
adherence to such wounds was noted 72 hours after applica- that optimum function of a skin substitute requires that it
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
be bilaminate, with the pore sizes of the inner and outer membrane has remained soft and pliable during the healing
layers as described. Theoretically, a unilaminate membrane period and lifts off the wound as reepithelialization occurs.
having different pore sizes in the inner and outer portions Laboratory studies in a murine model, using the membrane
should function satisfactorily, but such has not been devel¬ as a dressing for full-thickness wounds, have shown that
oped. connective tissue ingrowth occurs by 72 hours after applica¬
Other properties necessary for a membrane to function as tion with adherence said to be equal to or better than that of
an effective skin substitute include the following: freedom allograft skin.27 Such dressings remained intact for up to
from local or systemic toxicity, absence of antigenicity, and one month after application and apparently inhibited wound
resistance to linear and shear stress. It is also important contraction. In all study animals, "normalize! adherence
'
that the membrane not promote bacterial growth and, of this composite was not as good as that of allograft skin,
ideally, it should reduce the microbial density at the wound- but was better than that of xenograft skin. In a recent
membrane interface by providing an environment in which clinical study, Biobrane was applied over mesh grafts that
host defenses can function. The membrane should also be were expanded to a 6:1 or greater ratio to prevent graft
sufficiently thin, pliable, and elastic to tolerate the stresses slippage, the development of infection in the graft in¬
and motion associated with limb and underlying muscle terstices, and mechanical disruption of the thin mesh of the
activity, and permit the membrane to conform and inti¬ graft. The membrane could be easily removed on the fifth
mately adhere to the many irregularities of a wound bed. postgraft day, by which time the mesh autografts were
Desirable properties from a logistical standpoint include revascularized; maintenance of the prosthetic covering be¬
low cost, an indefinite shelf life, and minimal storage yond that time completely blocked epithelialization of the
requirements. interstices by the autograft.28
Burke et al have developed a bilaminate membrane
RECENTLY DEVELOPED SKIN SUBSTITUTES
consisting of a bovine collagen-based dermal analogue and a
Recent work by several investigative groups has led to Silastic epidermis.29 The biocompatible dermis, which is
the development of three types of membranes for use as skin slowly biodegraded, serves as a template for growth of host
substitutes, ie, bilaminate membranes that are a composite connective tissue to form what has been termed a neo-
of heterologous biodegradable tissue and synthetic mate¬ dermis. The dermal layer of the composite is a porous,
rial, bilaminate membranes that are totally synthetic and collagen-chondroitin 6-sulfate fibrillar matrix that is read¬
biologically inert, and membranes composed of autologous ily populated by fibroblasts and capillaries from the wound
tissue that either persists or is gradually replaced by host bed. The physical and biochemical properties (such as pore
tissue. size, cross-link density, helical structure of collagen, and
Collagen-Synthetic Composite Membranes collagenase resistance) of the dermis are controlled by the
glycosaminoglycan content of the material as well as the
Biobrane (Woodroof Laboratories Ine, Santa Ana, Calif) sterilization procedures (heat and exposure to glutaralde-
is a bilaminate membrane that has been evaluated for use as hyde) used in preparation. The epidermis of the composite
both a wound and skin graft donor-site dressing. The outer is a 0.1-mm-thick layer of Silastic applied in liquid form to
layer of the membrane is composed of an ultrathin layer of the dermal component, to which it firmly binds as it cures.
silicone rubber that is mechanically bonded to a fine-knit, This epidermal analogue permits water flux at levels similar
flexible nylon fabric. The silicone membrane is semiper¬ to normal skin and protects the wound from mechanical
meable and allows passage of water vapor from the wound trauma and microbial invasion. The composite can be stored
surface to the environment while preventing passage of in 70% isopropyl alcohol or in freeze-dried form.
bacteria from the environment to the wound surface. Type I The developers have reported on the use of this material
porcine collagen is covalently bonded to the fabric to for immediate closure of excised burn wounds in ten pa¬
provide an inert hydrophilic mesh inner layer into which tients with extensive burns. The composite was applied to
granulation tissue can grow. The water vapor transport the wounds, which ranged in extent from 15% to 60% of the
characteristics of this composite are directly related to the total body surface (average, 27%). Despite careful place¬
thickness of the membrane, which can be controlled so the ment and suturing of the membranes, some wrinkling
water vapor transmission approximates that of skin. The occurred, necessitating debridement of the wrinkles to
elasticity of the composite (100% elongation in any direc¬ drain underlying serous collections. Although collagen
tion) provides drapability and permits full range of motion sponge laminated to a polyurethane film showed, in studies
of a grafted body part. Bactériologie studies have shown an by Oluwasanmi and Chvapil, less adherence to tangentially
inverse relationship between adhesion and bacterial col¬ excised rabbit wounds than collagen sponge per se,26 this
onization,27 indicating that this material is best suited for composite was firmly adherent to the wound bed within
application to "clean wounds" such as donor sites, or per¬ minutes of application, and early vascularization of the
haps burn wounds excised before heavy microbial coloniza¬ dermal component was evident within three to five days.
tion has occurred. When donor sites were subsequently available, the Silastic
Clinical studies of this material used for immediate cover¬ epidermis was removed and the neodermis was covered
age of split-thickness skin graft donor sites have shown the with thin autograft skin 0.1 mm thick. Adherence of this
membrane to reduce evaporative water loss from the wound membrane to the excised wounds ranged from 95% to 100%,
and to decrease wound pain markedly. In such cases, the and the membranes were left intact for 14 to 64 days, with
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
Fig 4.—Lack of available donor sites required repeated application Totally Synthetic Bilaminate Membrane
of totally synthetic composite membrane to burn wounds on legs of
this patient prior to autografting. Top left, Sheets of totally synthetic Another direction has been taken by Levine et al, who
composite membrane have just been applied over granulation have developed a totally synthetic, biologically inert bilami¬
tissue on burns of legs. Membrane is held in place by elastic net nate membrane. A number of materials were evaluated for
gauze to prevent dislodgment by contact with bedclothes. Note that
membrane elasticity permits flexion of knees. Top right, "Strike- potential use as the inner layer of a composite skin substi¬
through" staining of composite membrane due to exúdate and tute in terms of initial membrane adherence to the wound
debris within membrane interstices indicates that it should be surface, conformation to the wound surface, adherence of
changed. Center left, Removal of third set of composite membranes the membrane to the wound surface five days after applica¬
reveals clean granulation tissue. Note clean appearance of under¬
side of membrane, integrity of membrane, intimate attachment to tion, occurrence of submembrane suppuration, and growth
wound bed, and lack of fragmentation of inner layer at point of of fibroblastic tissue into the membrane. Loose-knit nylon
separation from wound surface, indicated by the reflected edge of stocking fabric, coarse-mesh surgical gauze, and fine-mesh
membrane. Center right, Appearance of full-thickness burn wounds surgical gauze appeared similar, and those materials were
ready for autografting following three applications of totally syn¬ superior in terms of initial adherence, adherence at five
thetic composite membrane. Note uniformity of granulation tissue
and absence of inflammatory changes In wound. Bottom left, Take days, absence of subgraft suppuration, and extent of fibro¬
of subsequently applied mesh autografts expanded in 3:1 ratio was blastic ingrowth to Silastic-coated gauze, collagen mem¬
excellent. Bottom right, Appearance of burns after healing of mesh branes, and three polytetrafluoroethylene membranes.31
grafts. Note paucity of hypertrophie scarring. Lack of wound granu¬ Subsequent testing of the three best materials showed the
loma formation confirms absence of retained membrane fragments.
nylon stocking fabric to be superior in terms of tissue
compatibility, lack of fragmentation and retention of foreign
bodies at the time of membrane removal, flexibility and
take of the subsequently applied autografts ranging from elasticity, and conformity to irregular wound surfaces.
85% to 95%. Submembrane hematoma formation caused Studies of the extent of fibroblastic ingrowth into the
loss of a portion of the skin substitute in one patient and nylon stocking fabric were used to determine the optimal
seroma formation occurred beneath areas of membrane thickness of the dermal analogue. Clot formation occurred
wrinkling in several patients. In areas of wear or motion, beneath the serous crust, which rapidly formed on the outer
epidermal-dermal separation of the composite occurred and surface of wounds covered with single and double layers of
desiccation of the dermal analogue in those areas reduced the fabric. Fibroblastic ingrowth always occurred when
the take of subsequently applied autograft skin. four and eight layers of the mesh fabric were used, with only
Histologie studies showed progressive host tissue inva¬ rare elevation of the dressing from the wound surface
sion and replacement of the dermal analogue with no bovine occurring beneath four layers of fabric. These studies also
collagen evident seven weeks after application. Moderate showed that a minimal thickness of 0.635 mm of the dermal
fibrosis of the neodermis was noted and some scarring was analogue was needed to ensure consistent fibroblastic in¬
also identified below the neodermis, which was considered growth. It was found that a 1-mil-thick poly¬
to represent fibrotic change of unexcised heat-injured tis¬ tetrafluoroethylene membrane with O.l-µ pores permit¬
sue. Pore size appears to be critical to the successful ted passage of water vapor, was impermeable to liquid
function of the dermal analogue, since a pore size signifi¬ water, and impermeable to bacteria inoculated on the
cantly smaller than that of normal dermis retarded cellular membrane with a wetting agent. On the basis of these
invasion and led to development of thick, fibrous tissue. No studies, a composite wound dressing (skin substitute) has
inflammation or immunologie reactions were noted. been developed, consisting of a dermal analogue of six
Long-term follow-up is lacking, but there is said to be no layers of 14 denier nylon stocking fabric and the 1-mil-thick,
evidence to date of hypertrophie scar formation or clinical O.l-µ pore size polytetrafluoroethylene membrane as the
contracture following use of this composite. Areas treated epidermal analogue. This dressing can be sterilized prior to
with the skin substitute were found to be softer and more use in an autoclave or with ethylene oxide.
elastic and pliable than areas in which the excised wounds Animal studies have shown this membrane to be closely
were closed by immediate application of meshed autograft attached to the bed of the excised wound five days after
skin. Although no graft or subgraft infections were noted in application. Fibrovascular tissue of the host extended into
the study patients, the grafts were applied only to excised the lower two thirds of the thickness of the dermal analogue;
wounds, and the material has not been applied to wounds by ten days, organized collagen was identified in the nylon
covered with granulation tissue and contaminated with matrix. When applied to animals with experimentally con¬
microbial organisms. taminated wounds, the membrane limited microbial pro¬
Yannas et al have reported further studies of the skin liferation and prevented the development of fatal invasive
substitute composite using a guinea pig model of a full- infection. The wound protective effect of the bilaminate was
thickness wound. In vitro seeding of the dermal analogue evidenced by its ability to promote survival in rats in which
with dissociated autologous basal cells was followed by excisional wounds of 60% of the body surface area were
rapid basal cell proliferation and formation of sheets of dressed with the membrane—a result not achieved by
keratinized epidermis at the laminar interface of the com¬ covering such wounds with coarse-mesh gauze.32
posite within 14 days of application to a wound.30 In that The membrane has also been evaluated clinically and
model, what was considered to be new, functional skin had compared with cutaneous allograft, porcine xenograft, and
been generated in less than four weeks. coarse-mesh gauze when applied to wounds covered with
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
granulation tissue on 21 patients with burns of from 30% to and were heavily contaminated, the dressing was usually
66% of the total body surface. Each wound was divided into changed daily to effect wound debridement. Since the
four areas and the four dressings were applied to randomly previously noted bactériologie studies showed no reduction
assigned areas. Wound appearance was assessed qualita¬ in microbial density in wounds covered with this dressing,
tively by an experienced burn surgeon when the dressings the laminate was soaked in an antimicrobial solution (5%
were removed 48 hours after application. Quantitative mafenide acetate) immediately prior to application to pre¬
aerobic wound bactériologie studies were performed by the vent bacterial proliferation and reduce subgraft suppura¬
standard surface-swab technique, both before dressing tion. The laminate was held in place with elastic mesh
application and at the time of removal, 48 hours after dressings to ensure apposition to the wound bed and
application. prevent shearing of the graft from the wound surface by
Of those wounds in which allograft skin adhered to the contact with the bedclothes (Figure 4, top left). The dress¬
granulation tissue, no significant difference in wound ap¬ ing conformed well to irregular wound surfaces and its
pearance existed between those covered with autograft flexibility and modest elasticity in two directions were
skin, coarse-mesh gauze, and the bilaminate. Those areas sufficient to permit active motion of extremities to which it
covered with porcine xenograft were judged to be signifi¬ was applied. There was no fragmentation or retention of the
cantly worse in appearance. In wounds on which allograft fabric forming the dermal analogue at the time of removal,
skin did not take, xenograft-treated wounds had the worst even when the dressing had been in place for three or more
clinical appearance, while autograft-treated wounds were days.
significantly worse than those treated with coarse-mesh Although the semitransparency of the composite pre¬
gauze or the synthetic dressing. Wounds treated with vents direct visualmonitoring of the wound surface, wound
coarse-mesh gauze and synthetic dressing were indistin¬ exúdate was readily evident by staining of the outer surface
guishable from each other. of the dressing. Such "strike through" staining was usually
These findings confirm clinical observations indicating apparent in wounds considered unready for grafting within
that if a wound accepts allograft skin, the take of autograft 24 hours of application of the dressing, and reflected the
skin is assured, and that the wound should be closed with presence of debris and exúdate within the dressing (Fig 4,
autografts, if available. If autografting cannot be per¬ top right). Debridement of such material was achieved by
formed for some reason, eg, limited donor sites or intercur¬ daily dressing changes of the bilaminate membrane. In
rent illness, the application of allograft skin is the treat¬ wounds considered ready for grafting, staining was not
ment of choice until autografting can be accomplished. For evident for up to three or four days. The staining did not
wounds on which allograft skin will not adhere, the superior appear to be associated with significant wound infections,
performance of the bilaminate skin substitute and the since take of autografts immediately applied to wounds
coarse-mesh gauze is a reflection of the greater debriding from which stained dressings were removed was usually
action of those materials compared with the allograft and excellent (Fig 4, center left to bottom right).
xenograft tissue. The greater inflammatory response, fiber Tissue Culture-Derived Skin Substitutes
fragmentation, and retention of cotton fibers at the time of
removal of cotton gauze make the synthetic bilaminate the The most recent line of development has been the tissue
preferred dressing for such wounds. culture growth of epidermal cells obtained from the pro¬
The wounds of the study patients were colonized by a spective recipient who will require grafting. Studies by
variety of organisms, most commonly Pseudomonas aeru- Eisinger et al have shown that single-cell suspensions of
ginosa and Staphylococcus aureus. The organism popula¬ human epidermal cells can be grown on collagen film into
tion density significantly decreased in those areas of the confluent multilayered sheets, with the lower layer of cells
wounds on which allograft skin took, but showed no change morphologically similar to the basal cells of normal epider¬
in areas treated with the other materials (Table 1). In mis.33 When these sheets were implanted into nude mice,
wounds on which allografts did not take, there was no either under the kidney capsule or into subcutaneous
significant change in the bacterial population density be¬ tissue, the cells grew into a multilayer structure with
neath any of the materials. However, in over half of the keratohyaline granules in the upper layers. The tumori-
treatment areas of the wounds, the bacterial counts in¬ genie potential of the cells appears to be low, since no
creased after 48 hours of dressing application, indicating abnormal growth was observed in these studies. Canine
that for wounds to which biologic dressings or skin substi¬ epidermal cell sheets, prepared in the same fashion, were
tutes do not adhere, those membranes should be changed applied to either fresh or granulating wounds and held in
more frequently than every two days. place by an occlusive dressing. When the occlusive dressing
The bilaminate dressing has also been applied to areas of remained intact, the sheet of cells expanded to cover the
burn wound granulation tissue representing from 1% to 30% wound in four of six animals by the fifth day. In two of the
of the total body surface in 15 additional patients with burns animals, the grafts became infected thereafter and the cells
of from 30% to 77% of the body surface. In those patients did not survive. In the other two animals, the wounds
whose wounds appeared to be ready for closure, the bilami¬ appeared, by clinical criteria, to be healed after one week,
nate dressing was generally left in place for 48 to 72 hours, but it was uncertain whether the tissue-cultured cells
following which autografting was carried out. In other persisted or were replaced by cells from the recipient.
cases, where the wounds had foci of residual necrotic tissue Wound contraction seemed to occur in the test animals and
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
Table 2.—Uses and Limitations of Wound Dressing Membranes and Skin Substitutes*
Submembrane
Susceptibility Fluid Loss of
Dressing Optimum Use to Infection Collection Integrity Adherence
Hydron Early coverage of small, Low on
noncircumferential, superficial, exudative wounds
partial-thickness burns not involving
joint
Polymerized agar Temporary dressing of clean wounds + + + + Low
Fibrin film Temporary dressing of partial- + + + Requires dressing
thickness burns
Collagen membranes Temporary dressing of excised wounds + Decreases with time
Biobrane Dressing for donor site or excised Less than
wound allograft skin
Silastic-collagen Excised burn wounds + Excellent
composite29
Nylon-microporous Wounds with granulation tissue Excellent on
membrane composite32 (when
treated with clean wound
5% mafenide acetate)
Culture-grown Freshly excised wounds or those with Good under
epithelial sheets granulation tissue occlusive dressing
Culture-grown Excised wounds Good with sutures and
composite an occlusive dressing
*0 indicates none; +, minimal; , moderate; + + +, marked; + + + +, severe.
the cultured cells may have simply been sloughed as the had grown out from fragments of a full-thickness skin
wound narrowed. biopsy, to a solution of Type I collagen caused the collagen to
O'Connor et al cultured recipient epidermal cells until form a fibrillar lattice that subsequently decreased in
confluent sheets filled a 50-mm tissue culture disk (14 to 21 volume and increased in consistency. This lattice prevented
days), and applied the sheets to full-thickness burn wounds shrinkage when implanted and provided tensile strength to
of two patients.34 The epithelial sheets did not have a the composite. When grafted to full-thickness animal
stratum corneum, but developed one "about" eight days wounds, rapid vascularization of the dermal component of
after application to either granulation tissue or freshly the composite was found to prevent graft necrosis. The
excised wounds. Histologie examination performed approx¬ graft is said to inhibit wound contraction, with contraction
imately six months after application showed that all epider¬ being "blocked by at least 75% or more in 80% of the grafts"
mal layers were present, with no adenexal structures. The in a series of 52 grafts.
epidermis was mildly hyperkeratotic, lacked rete pegs, was These composite grafts are said to persist for as long as
thinner than normal, and had flattened basal cells. Mild ten months, but it is uncertain whether the implanted
chronic inflammatory changes were evident in the connec¬ tissue survived or served as a scaffold for replacement by
tive tissue underlying the culture-grown epidermal grafts. host tissue. Considerable remodeling of the dermal compo¬
Similar changes were seen beneath scar epidermis formed nent occurs, as indexed by a progressive increase in bire¬
by migration of epithelium from the wound margins. The fringence and a decrease in the ratio of labeled to unlabeled
absence of a stratum corneum made these epidermal sheets fibroblasts across time, although radioactively labeled fi-
susceptible to desiccation and required that petroleum broblasts do persist for up to five weeks. Ten weeks after
jelly-gauze dressings be applied over the grafts for three to implantation, the graft dermis had thinned to approx¬
four weeks. The main cause of failure of the culture-grown imately half the thickness of adjacent host dermis, and
material was infection, and the authors considered that it birefringence was greatest at the area of transition between
was most successful when applied to freshly excised burn graft and host tissue.36 Additionally, epidermal hypertro¬
wounds. Takes were noted not only with primary cultures phy has been observed and the epidermal scaling described
but also with second and tertiary subcultures, but the take by the investigators may represent sloughing of the graft
of the subcultured tissue was less certain. Noninfected epidermis. Histologie sections showed tongues of host
epidermis taken from patients critically ill with sepsis had a epidermis invading the periphery of such composite grafts
low colony-forming capacity, and the authors recommended along the epidermal-dermal interface of the grafts, sug¬
that epidermis for such culture growth be harvested as soon gesting replacement of the graft epidermis by scar epi¬
after admission as possible. thelium of the host. The time required to form a
Recently, Bell et al have developed what they term "a 100-sq-cm composite graft from a 1-sq-cm biopsy specimen
living skin equivalent," a composite consisting of a fibro- is 20 to 26 days, and represents a major limitation to the
blast-seeded collagen fibrillar lattice upon which dissoci¬ clinical use of this material, since grafting of burn wounds
ated epidermal cells are cultured and proliferate.35 Those must often be performed earlier in the postburn course,
investigators found that the addition of fibroblasts, which particularly if excision is employed.
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
USES AND LIMITATIONS OF are either replaced (to a variable extent) by scar tissue
MEMBRANE DRESSINGS produced by the recipient, or, if persistent, resemble trans¬
During the past decade, the desirable properties of an planted scars. The totally synthetic, biologically inert
effective burn-wound membrane dressing (skin substitute) composite membrane appears to have no intrinsic antibac¬
have been defined and a variety of candidate membranes terial activity and functions best when pretreated with an
have been developed and evaluated. Certain membranes, antimicrobial solution and applied to clean granulation
especially the bilaminate composites, appear, on the basis of tissue. Allograft skin remains the optimum biologic dress¬
early studies, to be promising, but all have functioned ing for temporary wound coverage. Generally, all the com¬
imperfectly and have specific limitations even when used posite skin substitutes appear to function best when applied
optimally (Table 2). The unilaminate membranes and some to excised wounds or wounds with clean granulation tissue.
bilaminates composed of either degradable or nondegrad- Further modifications of such membranes are necessary to
able synthetic materials function like a serous crust, de¬ increase their range of application by enhancing their
creasing wound pain but remaining susceptible to subgraft resistance to infection and accelerating submembrane heal¬
suppuration and infection. The biodegradable and culture- ing to reduce scar formation and subsequent contracture
grown membranes appear to be susceptible to infection and formation.
References
1. Pruitt BA Jr, Silverstein P: Methods of resurfacing denuded skin wound dressing on burned rat and rabbit ear wound healing. J Trauma
areas. Transplant Proc 1971;3:1537-1545. 1980;20:1024-1028.
2. Miller TA, Switzer WE, Foley FD, et al: Early homografting of second 21. Wokalek H, Sch\l=o"\pfE, Vaubel E, et al: Erste erfahrungen mit einem
degree burns. Plast Reconstr Surg 1967;40:117-125. Transparent Flussigkeits-Gel bei der Behandlung frischer operations\x=req-\
3. Donaldson RC, Payne J, Hershey FB: Effects of storage on enzyme wunden und chronischer Epitheldefekte der Haut. Aktuel Dermatol 1979;
activity and viability of skin. Surg Gynecol Obstet 1960;110:1-4. 5:255-265.
4. Graham WB III, Hamilton RW, Lehr HB: Versatility of skin allografts: 22. Nishi S: Clinical application of fibrin film for burns. Med Postgradu-
Desirability of a viable frozen tissue bank. J Trauma 1971;11:494-501. ates 1974;12:419-442.
5. Young JM, Hyatt GW: Stored skin homografts in extensively burned 23. Burleson RL, Ennulat N: Fibrin adherence to biologic tissues. J Surg
patients. Arch Surg 1960;80:208-213. Res 1978;25:523-529.
6. Pruitt BA Jr, Sell K, O'Neill JA Jr, et al: Clinical Evaluation of Freeze\x=req-\ 24. Norton L, Chvapil M: Comparison of newer synthetic and biological
Dried and Fresh Frozen Homograft on Burned Patients, Annual Research wound dressings. J Trauma 1981;21:463-468.
Progress Report. Fort Sam Houston, Tex, US Army Surgical Research 25. Tavis MJ, Harney JH, Thornton JW, et al: Modified collagen mem-
Unit, Brooke Army Medical Center, section 10, June 30, 1967. brane as a skin substitute. J Biomed Mater Res 1975;9:285-301.
7. Robson MC, Krizek TJ, Koss N, et al: Amniotic membranes as a 26. Oluwasanmi J, Chvapil M: A comparative study of four materials in
temporary wound dressing. Surg Gynecol Obstet 1973;136:904-906. local burn care in rabbit model. J Trauma 1976;16:348-353.
8. Colocho G, Graham WB III, Greene AE, et al: Human amniotic 27. Tavis MJ, Woodroof EA, Roth J, et al: New types of skin prostheses:
membrane as a physiologic wound dressing. Arch Surg 1974;109:370-373. Preliminary studies. Read before the 11th Annual Meeting of the American
9. Faulk WP, Matthews R, Stevens PJ, et al: Human amnion as an adjunct Burn Association, New Orleans, March 15, 1979.
in wound healing. Lancet 1980;1:1156-1158. 28. Lin SD, Robb EC, Nathan P: A comparison of IP-758 and Biobrane in
10. Levine NS, Lindberg RA, Salsbury RE, et al: Comparison of coarse rats as temporary protective dressings on widely expanded meshed auto-
mesh gauze with biologic dressings on granulating wounds. Am J Surg grafts. J Biomed Mater Res 1982;3:220-222.
1976;131:727-729. 29. Burke JF, Yannas IV, Quinby WC Jr, et al: Successful use of a
11. Silverstein P, Curreri PW, Munster AM: Evaluation of Fresh Viable physiologically acceptable artificial skin in the treatment of extensive burn
Porcine Cutaneous Xenografts as a Temporary Burn Wound Cover, Annual injury. Ann Surg 1981;194:413-428.
Research Progress Report. Fort Sam Houston, Tex, US Army Surgical 30. Yannas IV, Burke JF, Orgill DP, et al: Wound tissue can utilize a
Research Unit, Brooke Army Medical Center, section 51, June 30, 1971. polymeric template to synthesize a functional extension of skin. Science
12. Levine NS, Salisbury RE, Mason AD Jr: The effect of early surgical 1982;215:174-176.
excision and homografting on survival of burned rats and of interperi- 31. Levine NS, Salisbury RE, Peterson HD: Continued Evaluation of
toneally-infected burned rats. Plast Reconstr Surg 1975;56:423-429. Split-Thickness Cutaneous Xenograft and Synthetic Materials as Tempo-
13. Choy DSJ: Clinical trials of a new plastic dressing for burns and rary Biologic Wound Covers for Burned Soldiers, Annual Research Prog-
surgical wounds. Arch Surg 1954;68:33-43. ress Report. Fort Sam Houston, Tex, US Army Institute of Surgical
14. Chardack WM, Brueske DA, Santomauro AP, et al: Experimental Research, Brooke Army Medical Center, section 40, June 1974.
studies on synthetic substitutes for skin and their use in the treatment of 32. Levine NS, Peterson HD, Mason AD Jr: Use of a Synthetic Dressing
burns. Ann Surg 1962;155:127. on Denuded Wounds in Burned Patients, Annual Research Progress
15. Hall CW, Liotta D, DeBakey ME: Artificial skin. Trans Am Soc Artif Report. Fort Sam Houston, Tex, US Army Institute of Surgical Research,
Intern Organs 1966;12:340-343. Brooke Army Medical Center, June 1975, pp 343-363.
16. Alexander JW, Wheeler LM, Rooney RC, et al: Clinical evaluation of 33. Eisinger M, Morden M, Raaf JH, et al: Wound coverage by a sheet of
Epigard, a new synthetic substitute for homograft and heterograft skin. epidermal cells grown in vitro from dispersed single cell preparations.
J Trauma 1973;13:374-383. Surgery 1980;88:287-293.
17. Walder AI, May PD, Bingham CP, et al: Evaluation of synthetic films 34. O'Connor NE, Mulliken JB, Banks-Schlegel S, et al: Grafting of
as wound covers. Trans Am Soc Artif Intern Organs 1969;15:29-32. burns with cultured epithelium prepared from autologous epidermal cells.
18. Kornberg J, Burns NE, Kafesjian R, et al: Ultra thin silicon polymer Lancet 1981;1:75-78.
membrane: A new synthetic substitute: A preliminary study. Trans Am Soc 35. Bell E, Ehrlich HP, Sher S, et al: Development and use of a living skin
Artif Intern Organs 1972;18:39-43. equivalent. Plast Reconstr Surg 1981;67:386-392.
19. Warren RJ, Snelling CFT: Clinical evaluation of the Hydron burn 36. Bell E, Ehrlich HP, Buttle DJ, et al: Living tissue formed in vitro and
dressing. Plast Reconstr Surg 1980;66:361-368. accepted as skin-equivalent tissue of full thickness. Science 1981;211:1052\x=req-\
20. Dressler DP, Barbee WK, Sprenger R: The effect of Hydron burn 1054.
Downloaded From: http://archsurg.jamanetwork.com/ by a Georgetown University Medical Center User on 05/21/2015
You might also like
- Encouraging TeenagersDocument17 pagesEncouraging TeenagersTahNo ratings yet
- I Notes RETINA PDFDocument251 pagesI Notes RETINA PDFFelipe renquenNo ratings yet
- Black SeedDocument26 pagesBlack SeedAslam Aly Saib100% (1)
- Diagnostic Ultrasound Report TemplatesDocument8 pagesDiagnostic Ultrasound Report TemplatesJay Patel100% (10)
- Dressing PDFDocument4 pagesDressing PDFIndika KarunamuniNo ratings yet
- Dressing PDFDocument4 pagesDressing PDFIndika KarunamuniNo ratings yet
- Principles of Wound ClosureDocument6 pagesPrinciples of Wound ClosureMarnia SulfianaNo ratings yet
- A Review of Wound Dressing PracticesDocument13 pagesA Review of Wound Dressing PracticesAnonymous 1nMTZWmzNo ratings yet
- Pediatric Nursing: Narayan Swami College of NursingDocument10 pagesPediatric Nursing: Narayan Swami College of NursingAnkit KotnalaNo ratings yet
- Tissue Engineering and Wound Healing: A Short Case StudyFrom EverandTissue Engineering and Wound Healing: A Short Case StudyRating: 5 out of 5 stars5/5 (2)
- Pediatrics - Hesi Practice ExamDocument10 pagesPediatrics - Hesi Practice ExamWizzardNo ratings yet
- Assisting IV BTDocument89 pagesAssisting IV BTmhelshy villanuevaNo ratings yet
- Constipation 508Document12 pagesConstipation 508Shishir Kumar SinghNo ratings yet
- Skin Substitutes and Bioscaffolds Temporary and Permanent CoverageDocument8 pagesSkin Substitutes and Bioscaffolds Temporary and Permanent CoverageacanahuateNo ratings yet
- Pspa Yogjakarta Resume Tryout Ukai Nasional April 2018Document16 pagesPspa Yogjakarta Resume Tryout Ukai Nasional April 2018melindaNo ratings yet
- JSRB 19 Ra 2594Document9 pagesJSRB 19 Ra 2594sasibhushanarao poolaNo ratings yet
- Wound: CtosureDocument8 pagesWound: CtosureAnonymous kdBDppigENo ratings yet
- Wound Dressings - An Overview ScienceDirect TopicsDocument1 pageWound Dressings - An Overview ScienceDirect TopicsPavi gunaNo ratings yet
- Applications of Biomaterials in Plastic SurgeryDocument18 pagesApplications of Biomaterials in Plastic SurgeryacanahuateNo ratings yet
- Clinical Dermatology Open Access Journal: A Review of Wound Dressing PracticesDocument12 pagesClinical Dermatology Open Access Journal: A Review of Wound Dressing PracticesnurhariNo ratings yet
- Advanced Wound DressingDocument14 pagesAdvanced Wound DressingGanga DharanNo ratings yet
- Burns Journal of MedicineDocument8 pagesBurns Journal of MedicineInggrid Ayusari AsaliNo ratings yet
- Wound Closure TechniqueDocument5 pagesWound Closure TechniqueToni Mas IrwandaNo ratings yet
- Tissue Engineering of SkinDocument14 pagesTissue Engineering of SkinRaniNo ratings yet
- 1.J of Cosmetic Dermatology - 2023 - Corduff - Introducing Aesthetic Regenerative Scaffolds An Immunological PerspectiveDocument7 pages1.J of Cosmetic Dermatology - 2023 - Corduff - Introducing Aesthetic Regenerative Scaffolds An Immunological PerspectiveRobertoNo ratings yet
- Wound Care The Role of Advanced Wound-Healing TechnologiesDocument9 pagesWound Care The Role of Advanced Wound-Healing TechnologiesJose Antonio Chavez MNo ratings yet
- Bacterial Adherence To Suture Materials: Original ReportsDocument4 pagesBacterial Adherence To Suture Materials: Original ReportsAdityaNo ratings yet
- Biologic Dressings: Jjunkin1@jhmi - EduDocument3 pagesBiologic Dressings: Jjunkin1@jhmi - EduEsq. Nelson OduorNo ratings yet
- Chitosan and Alginate Wound DressingsDocument7 pagesChitosan and Alginate Wound DressingsEliezer BecziNo ratings yet
- Improved Healing of Split Thickness Skin Graft Donor Sites: KEY WORDS: Skin Grafts, Wound Healing, Epidermal DressingDocument9 pagesImproved Healing of Split Thickness Skin Graft Donor Sites: KEY WORDS: Skin Grafts, Wound Healing, Epidermal DressingandiNo ratings yet
- Fascial Closure-Dumanian2020Document15 pagesFascial Closure-Dumanian2020Kevin QuinterosNo ratings yet
- Bishara Soft Tissue Grafting PDFDocument7 pagesBishara Soft Tissue Grafting PDFMark BisharaNo ratings yet
- Smart Bandage TechnologyDocument8 pagesSmart Bandage TechnologyiJordanScribdNo ratings yet
- 22 Abdelrahman T and Newton H 2011Document5 pages22 Abdelrahman T and Newton H 2011ulises arredondo chavezNo ratings yet
- Smart Bandage Technology: Jordan DavidsonDocument8 pagesSmart Bandage Technology: Jordan DavidsoniJordanScribdNo ratings yet
- Ni Hms 490729Document13 pagesNi Hms 490729novelraaaNo ratings yet
- Branski (2011)Document7 pagesBranski (2011)TommysNo ratings yet
- Research Essay - Materials in Wound HealingDocument4 pagesResearch Essay - Materials in Wound HealingJosh ChiuNo ratings yet
- Utilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDocument11 pagesUtilizing Free Skin Grafts in The Repair of Surgical Wounds: Madalene C. Y. HengDefri ChanNo ratings yet
- Observation of Viable Alloskin Vs Xenoskin Grafted Onto Subcutaneous Tissue Wounds After Tangential Excision in Massive BurnsDocument10 pagesObservation of Viable Alloskin Vs Xenoskin Grafted Onto Subcutaneous Tissue Wounds After Tangential Excision in Massive BurnsAngelica SerbulNo ratings yet
- Clinical Experience With Surgical Debridement and Simultaneous Meshed Skin Grafts in Treating Biofilm-Associated Infection: An Exploratory Retrospective Pilot StudyDocument9 pagesClinical Experience With Surgical Debridement and Simultaneous Meshed Skin Grafts in Treating Biofilm-Associated Infection: An Exploratory Retrospective Pilot StudyAsmat BurhanNo ratings yet
- DressingsDocument16 pagesDressingsJose VergaraNo ratings yet
- 2018 KLWC Hansen's RevisedDocument1 page2018 KLWC Hansen's RevisedLinda Luckstead BenskinNo ratings yet
- Mother Touch in Periodontal Therapy: Chorion MembraneDocument7 pagesMother Touch in Periodontal Therapy: Chorion MembraneInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Randomized Clinical Trial Comparing A Collagen-Based Composite Dressing Versus Topical Antibiotic Ointment On Healing Full-Thickness Skin Wounds To Promote EpithelializationDocument5 pagesA Randomized Clinical Trial Comparing A Collagen-Based Composite Dressing Versus Topical Antibiotic Ointment On Healing Full-Thickness Skin Wounds To Promote EpithelializationGevania ArantzaNo ratings yet
- Modern DressingDocument6 pagesModern DressingSri wahyunitaNo ratings yet
- International Wound Journal - 2019 - Chen - in Vitro Cellular Viability Studies On A Concentrated Surfactant Based WoundDocument10 pagesInternational Wound Journal - 2019 - Chen - in Vitro Cellular Viability Studies On A Concentrated Surfactant Based WoundsivaNo ratings yet
- Amnion in The Treatment of Pediatric Partial Thickness Facial BurnsDocument7 pagesAmnion in The Treatment of Pediatric Partial Thickness Facial BurnsInggrid Ayusari AsaliNo ratings yet
- Assessment of Outcome of Using Amniotic Membrane Enriched With Stem Cells in Scar Formation and Wound Healing in Patients With Burn WoundsDocument6 pagesAssessment of Outcome of Using Amniotic Membrane Enriched With Stem Cells in Scar Formation and Wound Healing in Patients With Burn WoundsInggrid Ayusari AsaliNo ratings yet
- 17 4Document5 pages17 4Gunawan SadewoNo ratings yet
- Unusual Encroachers in OKCDocument3 pagesUnusual Encroachers in OKCDIVYABOSENo ratings yet
- View Doc 635470672036959908Document6 pagesView Doc 635470672036959908abhishekbmcNo ratings yet
- Bovine Surger y of The Skin: Matt D. MiesnerDocument10 pagesBovine Surger y of The Skin: Matt D. MiesnerGuadalupe Cristina Chuchón CáceresNo ratings yet
- Tissue Injury and Healing: Brent Kincaid, DDS, John P. Schmitz, DDS, PHDDocument10 pagesTissue Injury and Healing: Brent Kincaid, DDS, John P. Schmitz, DDS, PHDAmith HadhimaneNo ratings yet
- Dressing Selection in Chronic Wound ManagementDocument10 pagesDressing Selection in Chronic Wound ManagementFenni OktoberryNo ratings yet
- An Evidence Based Approach To Soft Tissue APPROXIMATION: A Review of Suture Selection For Optimal Skin ClosureDocument4 pagesAn Evidence Based Approach To Soft Tissue APPROXIMATION: A Review of Suture Selection For Optimal Skin ClosureAnonymous kdBDppigENo ratings yet
- TMP 8020Document2 pagesTMP 8020FrontiersNo ratings yet
- Negative Pressure Wound TherapyDocument9 pagesNegative Pressure Wound TherapySuharyonoNo ratings yet
- Aesthetic Comparison of Wound Closure TechniquesDocument3 pagesAesthetic Comparison of Wound Closure Techniquesluisrmg91No ratings yet
- Benefit and Risk in Tissue Engineering 2004 Materials TodayDocument6 pagesBenefit and Risk in Tissue Engineering 2004 Materials TodayBianca Ionela DraganNo ratings yet
- Clinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesDocument9 pagesClinical Study: Vacuum Assisted Closure Therapy Versus Standard Wound Therapy For Open Musculoskeletal InjuriesAndika FahruroziNo ratings yet
- Biological Prosthetics For Hernia Repair: EditorialDocument2 pagesBiological Prosthetics For Hernia Repair: EditorialtexveerNo ratings yet
- 16 - Trauma MedicineDocument17 pages16 - Trauma MedicinePeterNo ratings yet
- Polymers 03 00509 v2Document18 pagesPolymers 03 00509 v2Branko BabicNo ratings yet
- Open Fractures With Soft-Tissue Loss: Coverage Options and Timing of SurgeryDocument3 pagesOpen Fractures With Soft-Tissue Loss: Coverage Options and Timing of SurgerySaffa AzharaaniNo ratings yet
- Debridamiento QuirurgicoDocument4 pagesDebridamiento QuirurgicoLeandroPeraltaNo ratings yet
- Liu 2018Document15 pagesLiu 2018raden chandrajaya listiandokoNo ratings yet
- Celulas MesenquimalesDocument6 pagesCelulas MesenquimalesDIOGENESNo ratings yet
- Galiano Et Al-2004-Wound Repair and RegenerationDocument8 pagesGaliano Et Al-2004-Wound Repair and RegenerationEric DyneNo ratings yet
- The SurgicalDocument13 pagesThe Surgicalhuyenthanh1807No ratings yet
- Slow Mohs Micrographic Surgery and The Role of The PathologistDocument4 pagesSlow Mohs Micrographic Surgery and The Role of The PathologistEsq. Nelson OduorNo ratings yet
- Early Burn Wound Excision in Children PDFDocument6 pagesEarly Burn Wound Excision in Children PDFEsq. Nelson OduorNo ratings yet
- Metastatic Breast Disease: Presenter: DR Abdi Osman M. Supervisor: DR D. KiptoonDocument32 pagesMetastatic Breast Disease: Presenter: DR Abdi Osman M. Supervisor: DR D. KiptoonEsq. Nelson OduorNo ratings yet
- Regenicin IncDocument2 pagesRegenicin IncEsq. Nelson OduorNo ratings yet
- Comparative Effectiveness of Biobrane®Document12 pagesComparative Effectiveness of Biobrane®Esq. Nelson OduorNo ratings yet
- Dermal SubstitutesDocument9 pagesDermal SubstitutesEsq. Nelson OduorNo ratings yet
- Collagen Dressing Versus Conventional DressingsDocument6 pagesCollagen Dressing Versus Conventional DressingsEsq. Nelson OduorNo ratings yet
- Epicel Autografts PDFDocument1 pageEpicel Autografts PDFEsq. Nelson OduorNo ratings yet
- Dermal Skin SubstitutesDocument25 pagesDermal Skin SubstitutesEsq. Nelson OduorNo ratings yet
- Collagen Dressings in The ManagementDocument5 pagesCollagen Dressings in The ManagementEsq. Nelson OduorNo ratings yet
- Early Burn Wound Excision in Children PDFDocument6 pagesEarly Burn Wound Excision in Children PDFEsq. Nelson OduorNo ratings yet
- Burns Management PDFDocument7 pagesBurns Management PDFRoh Bungaria N Garingging100% (1)
- Biologic Dressings: Jjunkin1@jhmi - EduDocument3 pagesBiologic Dressings: Jjunkin1@jhmi - EduEsq. Nelson OduorNo ratings yet
- Indian Journal of Plastic Surgery Volume 43 Issue 3 2010 [Doi 10.4103_0970-0358.70712] Halim_ AhmadSukari_ Khoo_ TengLye_ Shah_ JumaatMohd. Yussof -- Biologic and Synthetic Skin Substitutes- An OverDocument7 pagesIndian Journal of Plastic Surgery Volume 43 Issue 3 2010 [Doi 10.4103_0970-0358.70712] Halim_ AhmadSukari_ Khoo_ TengLye_ Shah_ JumaatMohd. Yussof -- Biologic and Synthetic Skin Substitutes- An OverMannuela Anugrahing MarwindiNo ratings yet
- Epicel ICD10 Guide PP - US.EPI.0065 PDFDocument14 pagesEpicel ICD10 Guide PP - US.EPI.0065 PDFEsq. Nelson OduorNo ratings yet
- Guide To Burn DressingsDocument4 pagesGuide To Burn DressingsjustanothergunnutNo ratings yet
- Epicel BiopsyOverview FCfinal DIGITAL PDFDocument4 pagesEpicel BiopsyOverview FCfinal DIGITAL PDFEsq. Nelson OduorNo ratings yet
- The Use of Frogskin As A Biological DressingDocument9 pagesThe Use of Frogskin As A Biological DressingEsq. Nelson OduorNo ratings yet
- Epicel Coding Guide PP - US.EPI.0024 PDFDocument28 pagesEpicel Coding Guide PP - US.EPI.0024 PDFEsq. Nelson OduorNo ratings yet
- Epicel Autografts PDFDocument1 pageEpicel Autografts PDFEsq. Nelson OduorNo ratings yet
- Early Burn Wound Excision in Children PDFDocument6 pagesEarly Burn Wound Excision in Children PDFEsq. Nelson OduorNo ratings yet
- Bioelectric DressingDocument27 pagesBioelectric DressingEsq. Nelson OduorNo ratings yet
- Important Classifications PDFDocument42 pagesImportant Classifications PDF330 Himank MehtaNo ratings yet
- Factory Farming in The Developing WorldDocument10 pagesFactory Farming in The Developing WorldDaisyNo ratings yet
- English: Quarter 4 - Module 7 Making GeneralizationsDocument16 pagesEnglish: Quarter 4 - Module 7 Making Generalizationslenra esoj lasorNo ratings yet
- Low Platelet CountDocument9 pagesLow Platelet Countfatimah_zkhanNo ratings yet
- Areport 08Document247 pagesAreport 08Mithilesh JhaNo ratings yet
- Curs de Limba PortughezaDocument16 pagesCurs de Limba PortughezaMădălina TodincaNo ratings yet
- Source and Transmission of InfectionDocument10 pagesSource and Transmission of InfectionInam AliNo ratings yet
- Msds Quik Gel Gold PDFDocument10 pagesMsds Quik Gel Gold PDFBangun KartaNo ratings yet
- Bile Esculine TestDocument2 pagesBile Esculine TestVincent OngNo ratings yet
- Renal Pharmacology 2023Document116 pagesRenal Pharmacology 2023sami MesfinNo ratings yet
- Perioperative Fasting and Feeding in Adults, Obstetric, Paediatric and Bariatric Population-Practice Guidelines From The Indian Society of AnaesthesiologistsDocument29 pagesPerioperative Fasting and Feeding in Adults, Obstetric, Paediatric and Bariatric Population-Practice Guidelines From The Indian Society of Anaesthesiologistsambitiousamit1No ratings yet
- 2017 - Pardede - Penerapan Terapi Suportif Dengan Teknik Bimbingan Untuk Mengurangi Dorongan Bunuh Diri Pada Pasien Skizofrenia PDFDocument8 pages2017 - Pardede - Penerapan Terapi Suportif Dengan Teknik Bimbingan Untuk Mengurangi Dorongan Bunuh Diri Pada Pasien Skizofrenia PDFIra Mayang SNo ratings yet
- Chapter - 2 Microorganisms (Continuation)Document2 pagesChapter - 2 Microorganisms (Continuation)ARSHAD JAMILNo ratings yet
- Presentation List Language Disorders in ChildrenDocument3 pagesPresentation List Language Disorders in Childrenramandeep kaurNo ratings yet
- Alva by VibraSense, Instructions For UseDocument21 pagesAlva by VibraSense, Instructions For Usetov4008No ratings yet
- Book 28Document56 pagesBook 28Er Sana WarsiNo ratings yet
- 3.ALS Algorithms Advanced Life SupportDocument1 page3.ALS Algorithms Advanced Life SupportLucian Alin DinuNo ratings yet
- Seminar On: Organisation and Management of Neonatal Services and NicuDocument27 pagesSeminar On: Organisation and Management of Neonatal Services and NicuDimple SweetbabyNo ratings yet
- De So 3Document6 pagesDe So 3To Minh PhuongNo ratings yet
- Glucagon and Its Metabolic EffectsDocument31 pagesGlucagon and Its Metabolic EffectsnikenNo ratings yet
- Bioaktivni Ugljenihidrati PDFDocument4 pagesBioaktivni Ugljenihidrati PDFmajabulatNo ratings yet
- Knowledge Regarding Immunization Among Mothers of Under Five ChildrenDocument3 pagesKnowledge Regarding Immunization Among Mothers of Under Five ChildrenEditor IJTSRDNo ratings yet

















































































![Indian Journal of Plastic Surgery Volume 43 Issue 3 2010 [Doi 10.4103_0970-0358.70712] Halim_ AhmadSukari_ Khoo_ TengLye_ Shah_ JumaatMohd. Yussof -- Biologic and Synthetic Skin Substitutes- An Over](https://imgv2-1-f.scribdassets.com/img/document/353666090/149x198/d2c76d3c34/1499944652?v=1)