Professional Documents
Culture Documents
Surgery Multiple Endocrine Neoplasia Type1
Uploaded by
Frances Oscar Gaviola0 ratings0% found this document useful (0 votes)
7 views13 pagesCopyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views13 pagesSurgery Multiple Endocrine Neoplasia Type1
Uploaded by
Frances Oscar GaviolaCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 13
SO De ae
Multiple Endocrine
Neoplasia Type 1
Geoffrey B. Thompson, MD « William F. Young, Jr., MD
‘Multiple endocrine neoplasia type 1 (MEN 1) is an autosomal
dominant-inberited disorder affecting tumorigenesis in at
teas eight endocrine and nonendocrine tissues whose com-
3s were first recognized in the early 20th century. In
1943, Erdheim' described a patient with a pituitary adenoma
and parathyroid hyperplasia discovered at autopsy. Gerste!*
reported on a patient with acromegaly and a severe peptic
ulcer diathesis in 1938, Wermer. in 1954, identified the
autosomal dominant nature of the disease that bears his name
(iermer's syndrome, now referred to as MEN 1). Children
of an affected parent have a 50% chance of inberiting the
disease predisposition that is noted to be highly penetrant.
Larsson and associates,* in 1988, mapped the gene associ-
sued with MEN I (MEN) tothe long arm of chromosome 11
(11q13). MEN/ is a tumor suppressor and encodes a widely
expressed protein called menin. Clinical expression of the
tenwsype requires not oniy inheritance of an MEN! germline
mutation but also inactivation of the wild-type MEN/ allele
derived from the unaffected parent.*” Mutations in the gene
kead to widespread endocrine tumorigenesis. Approximately
90% of affected kindred members have mutations detectable
by genetic testing, and the phenotype develops in virtually
all individuals with germline mutations.
Epidemiology and Clinical
Presentation
The twe prevalence of MEN 1 is likely underestimated; data
‘pgeat a prevalence of 0.2 to 2/100,000.* Major clinical
anifestations in MEN 1 include the “3Ps”: primary hyper-
Fuathyroidism (HPT) (95%), pancreatic endocrine tumors
FETs) (50% to 75%), and pituitary tumors (30% to 55%).
ession of the disease rarely occurs before 10 years of
2: and most often presents between 20 and 40 years of
iE!" Two of the three major lesions must be present for
Slinical diagnosis in probands. In family members of
‘hown MEN 1 kindreds, the presence of one major lesion is
Pe able 16-1), Cinieal diagnosis is confirmed by
sting
All thee major clinical manifestations arise in less
than 12% of affected patients." Any of these three clinical
‘manifestations may be the first component precipitating a
diagnosis, but in most patients, primary HPT appears by the
3rd or 4th decades of life. Biochemical abnormalities can be
detected decades before clinically overt symptoms become
‘manifest.’ For example, biochemical aboormalities may be
noted in affected adolescents in their mid to late tecas when
careful, egular screening is performed. Stodies have shown
that delaying screening until clinical symptoms develop can
be associated with locally advanced disease or distant metasta-
tic disease in as many as 50% of patients with PETs."?
Less common, but overrepresented, manifestations in
MEN | include adrenocortical tumors,'*"” foregut carcinoid
tumors,'*23 nonmedullary thyroid neoplasms (mostly
follicular),** and a host of unusual cutaneous/mucosal or
visceral abnormalities, including multiple subcutaneous and
visceral lipomnas, multiple facial angiofibromas, hypomelan-
otic macules, gingival papules, and collagenomas.*7” Rare
associations with MEN 1 also include meningiomas, ependy-
momas, pinealomas, renal cancers, rhabdomyosarcoma,
leiomyosarcoma, and pancreatic ductal adenocarcinoma 574
The Molecular Biology of MEN 1
‘The gene responsible for MEN 1 was identified in 1997"
and is located on chromosome 11q13. MEN! spans 9 kb of
genomic DNA and consists of 10 exons containing an
1830-base pair coding region. MEN/ encodes a 610-amino
acid nuclear protein, referred to as menin. Menin is
localized to tk: nucleus and interacts with the activating
protein 1 transcription factor JunD and other proteins involved
jn wanscription and cell growth regulation?+35 MENJ muta-
tions are spread over the entire coding region (exons 2 to 10);
approximately 50% are frameshift, 24% are missense, 20%
are nonsense, and 7% are deletion or in-frame insertion
mutations. MEN/ acts as a tumor suppressor gene, and
‘tumor development follows Knudson's “two-hit” hypothesis.”
‘Hence, individuals affected with MEN 1 inherit one MEN
673
674 —— Endocrine Pancreas
TA ses Ren eV ntsc
Manifestations Prevalence (1)
Major ("3 Ps")
Primary hyperparathyroidism >95
Pancreatic/duodenal neuroendocrine 80-75
tumors
Pituitary tumors
Less Common
‘Adrenocortical tumors (functioning
|. nd nonfunctioning; benign and
{,imalignant)
» Fotegut carcinoid tumors (bronchial,
‘thymio, gastrointestinal)
‘Nonmedullary thyroid neoplasms
+ Cutaneous/mucosal and visceral
{abnormalities (multiple ipomas,
facil angiofibromas, hypomelanotic
*°fnacales, gingival papules, colagenomas)
Diagnosis (cinical) of MEN 1: (1) two major manifestations present
'iqrproband or (2) one major manifestation in an atzisk member of
‘Yaixnown MEN 1 kindred. Confirmation is by genetic testing.
‘MEN 1 = multiple endocrine neoplasia type 1. 5
ea
30-55
allele with a germline mutation (the “first hit”), and tumori-
genesis in specific tissues ‘then occurs after a second deleterious
mutation (the “second hit”) is acquired in the remaining wild-
type allele in a single cell.3” Such homozygous-inactivating
MEN! mutations result in menin protein absence or trunca-
tion, and neoplastic clonal expansion from that cell is then ini-
tiated. Thus, the mechanism for tumor formation in MEN 1
involves loss of menin function in a tumor precursor cell.
Unlike the RET protooncogene (associated with MEN 2),
mutations in MENI do not clearly demonstrate significant
‘genotype-phenotype correlations." Recent studies have
found preliminary data suggesting that mutation type or
location within MEN] may be associated with clinical
presentation.“ However, the limited data available regarding
genotype-phenotype correlations do not currently warrant
modification of clinical managemer
‘Several analytic approaches to identifying MEN/ mutations
have been used, but most laboratories currently use direct
DNA sequencing. The first step in the analysis of a sporadic
case or & patient in a kindred with suspected or prover. MEN |
is to identify the specific MEN/ mutation in germline DNA.
Germline testing requires peripheral blood ftom an affected
index case. In mest probands, a disease-causing mutation is
identified. Because MEN/ somatic mutations are commonly
found in endocrine tumors, tumor DNA is rarely useful in
distinguishing germline mutations.*'*”
It is estimated that more than 10% of germline MEN/
mutations arise. de novo and can subsequently be passed
to future generations.“ Mutations in MEN/ are highly
pperietrant; approximately 50% of mutation carriers are
‘symptomatic by 20 years of age, und nearly 100% are symp-
tomatic by 60 years of age. Most large series have failed
to find MEN/ germline mutations in 10% to 20% of index
cases," likely reflecting undetected mutations, such
as large deletions that are transparent 19 DNA. sequence
analysis or mutations in another unknown gene. MEN muta-
tional analysis is clinically available in atleast four molecu-
Jar genetics laboratories in North rica,
>.
Who Should Be Considereg
for Genetic Counseling
and Testing?
In general, genetic screening of presymy :
is appropriate when early therapeutic nee indi,
able for the tumors diagnosed, particularly Whe tag,
ata preclinical stage. Although this has not been ©” © 2B,
domized, prospective studies of MEN 1 paten "nm
somewhat controversial, there is an increasing prt
dence to suppor this contention, particularly wig”
MEN I pancreatic neuroendocrine tumors, 34732 apt
early recognition and intervention with reper jg Mh
roid and pituitary neoplasia does not prolong sat
‘can reduce or prevent morbidity associated with tot
overactivity and mass effect. on
Clinical screening of at-risk family mem
known MEN 1 kindreds should begin in meee
when biochemical abnormalities can begin to be ga
long before overt clinical manifestations and nese
coccut Ifa familial mutation has been dented nega
genetic test in an at-risk family member preclude meq
for routine, lifelong biochemical screening and ix
However, if a mutation is not detected in a proband, fury
testing for MEN! mutations in at-risk family membersisnt
indicated, and presymptomatic testing is not posite by
direct DNA testing. In these cases, at-isk family ments
must continue to be clinically monitored throughout tei
lifetimes. Such families in which a mutation cant be ie
tified may consider pursuing linkage analysis, a les dea
method of tracking the disease allele through the family
Because the process of genetic testing can be conpi
cated, genetic counseling is recommended for all fami
considering this option. Presymptomatic testing of ait
family members can be emotional, and families may bent
from a session with a genetic counselor. The genetic om
selor acts as a guide, explaining the pros and cons of esis
as well as aiding with interpretation of the resalts shouldbe
family choose to proceed.
Regarding testing of apparently sporadic MEN |
patients, mutation screening should be considered in yous
patients (<50 years of age) with HPT, particulary in the
‘with multigland disease or recurrent HPT in the absenee ol
renal disease. Consideration should also be given 1016
patients with prolactinomas because up 10 14% of
patients may actually have MEN 1. Testing is also apm0#7
ate for patients multiple pancreatic newroenlorie
tumors (calcium levels should be checked in all ot
with solitary PETs), patients with any MEN I lest
‘an adrenal lesion, and patients with bronchial and thy
carcinoids (Table 75-2).!"
Pituitary Tumors
fs
In MEN | kindreds, pituitary wmors are found i
quently than primary HPT or PETs.* Signs a4 9 hp
related to a pituitary adenoma are the initial cline Fg”
tation of MEN 1 in up to 25% of “first in the 1 ge
cases but in less than 10% of familial cases
a
Y
{
TE Ce eco ok ae ead
‘jussk fly members in known MEN 1 kindreds
Ag patients (<50 years) with multigland or recurrent
"Pt (normal fenal function)
pauents with prolactinomas (14% MEN 1)
Patient with multiple PETS
Pajents with any MEN 1 lesion and an adrenal k
Fajents with bronchial or thymic carcinoids
ion
SS
jaN 1 = multiple endocrine neoplasia type 1; PET = pancreatic
Meferine tumor; HPT = hyperparathyroidismn
osed prospectively.’® The estimated prevalence of pitu-
jiay tumors in MEN | paticnts ranges from 10% to 60%.5°*%
For example, in a series of 324 patients with MEN 1, pitu-
jiary adenomas occurred in 197 (42%); mean age at diagno-
fas Was 38 years (range. 12 to 83 years). In most MEN 1
patents, the pituitary tumors are macroadenomas (>10 mm)
{Fig. 76-1). All subtypes of pituitary adenoma have been
reported in MEN 1, but most frequently they are prolactino-
‘mas (60%). Patients may present with amenorthea/galact-
hea in women, symptoms related to hypogonadism in
men, and/or sellar mass effect symptoms.***** Less common
gittary tumor subtypes in MEN | include somatotroph
adenoma (acromegaly: ~25%), corticotroph adenoma
(Cushing's syndrome; =5%), and clinically nonfunctioning,
piuitary tumors (=10%). Monitoring for pituitary tumor
development in the MEN I patient should include measure-
iment of serum prolactin and insulin-like growth factor | as
well as imaging of the pituitary by magnetic resonance
imaging (MRI) every 2 to 3 years.” In patients with an
abnormal pituitary MRI, hypothalamic-pituitary testing
should te completed to characterize the type of the pituitary
adenoma and its effects on the secretion of other pituitary
bormones. Treatment of pituitary tumors in MEN 1 is guided
ty the adenoma subtype and is identical to that in patients
with sporadic pituitary tumors (Fig. 76-2). In addition, after
‘Muluple Endocrine Neoplasia Type 11 —— 675
successful pharmacologic or surgical treatment of the pi
itary tumor, MEN 1 patients should continue to be evaluated
with periodic pituitary tumor sercening since a second pitu-
itary adenoma may arise from the remaining pituitary tissue.
Primary Hyperparathyroidism
Most MEN | patients develop hypercalcemia and primary
HPT by the 4th decade of life.* Shepherd described cle-
vated ionized serum calcium levels in 66% of patients
younger than 25 years of age, 85% of patients between 25
‘and 55, and 87% of patients older than 55 in a large cohort of
MEN I family members.* Skogscid and colleagues described
a mean age of onset of HPT at less than 19 years.'* TI
in sharp contrast to patients with sporadic primary HPT
who typically present in their 50s and 60s.
Primary HPT is the initial clinical/biochemical manifes-
tation of MEN 1 in 60% to 90% of patients, but the percentage
may be as low as 30% in young at-risk patients who are
screened.
A serum factor mitogenic for parathyroid cells has been
isolated in MEN 1 patients at levels 20 times those of
normal subjects. Parathyroid mitogenic factor has far greater
activity than any other measurable growth facior, and its
activity has been quantified by in-vitro studies.
Diagnosis
‘The diagnosis of primary HPT (Table 76-3) is dependent on
demonstrating an inappropriaté immunometric parathyroid
hormone (PTH) level in the face of an elevated ionized serum
calcium level. Hypocalciuria due to benign familial hypocal
uric hypercalcemia (BFHH) should be ruled out by calculating
the calcium-creatinine clearance ratio:
(24-hour urine calcium x serum creatinine) + (24-hour
urine creatinine x serum calcium)
ORE 76-1. Head MRI showing coronal (A) and sagittal (B) views of a prolactin-scereting pituitary my
Yearold young man with maltiple endocrine neoplasia type | The patient presé
nadenom (arrows) in an
ly headaches, vision
ted w
a S-year history of da
“sd delayed sexual maturation. The serum prolactin level was 6309 ng/ml. (normal, 1 to 1S ng/ml).
676 — Endocrine Pancreas
and by obtaining a detailed family history. Calcium-creatinine
clearance ratios lower than 0.01 are indicative of BFHH.
Localization Studies
‘Imaging clearly has a role inthe evaluation and management
of patients with sporadic HPT, of whom 85% have a solitary
Burka)
Pere Os aR Rea mie
Diagnosis
Elevated ionized serum calcium level
Inappropriate immunometric parathyroid hormone level
Calcium-creatinine clearance ratio > 0.01,
Indications for Surgical Intervention
‘Any symptomatic patient (nephrolithiasis, osteoporotic
fractures, ot hypercalcemic crisis)
‘Total serum calcium level 2 1.0 mg/dL above the assay
‘upper limit of normal
Nephrocalcinosis
Hypercalciuria (>400 mg/24 hr)
Decreased glomerular filtration rate by 230% for age- and.
‘sex-matched controls
Worsening BMD (hip, radius, or spine)
BMD T-score < -2.5 (2 SD from normal controls)
Zollinger Ellison syndrome
‘MEN 1 = multiple endocrine neop
roldism; GFR = glomerular fire
density.
Modified from Blezikian JP, Potts JT Jr, Fuleihan Gel, et al
‘Summary statement ffom a Workshop on Asymptomatic Primary
‘A Perspective for the 2ist Century. J Bone
ia type 1; HPT = hyperparathy-
‘BMD = bone mineral
Hyperparathyroidism:
‘Miner Rs 2001 17:2
FIGURE 76-2. Endonasal_transsphe
pituitary surgery. (©Mayo, 2001.) "ida
adenoma, rendering many of these patients candidates fora
directed surgical approach. ©® The benefits of minimally inv
sive parathyroidectomy in this subgroup of sporadic patens
ents, however, the pathology is that
of asymmetrical hyperplasia involving all parathyroid
glands. Therefore, regardless of imaging, all glands musi be
‘explored and a transcervical thymectomy performed to rule
out a supemumerary or ectopic gland, which is seen in as
many as 20% of MEN 1 patients. Ima
of multigland disease is often misleading and frequenly
demonstrates only the dominant gland or glands.®?
Sestamibi parathyroid scanning (SPS)* and percutaneous
neck ultrasound* typically demonstrate only the dominant
gland or glands in MEN | patients, that if treated as suc,
will lead to persistent HPT for the unknowing and inexpet-
enced surgeon. SPS may, on occasion, demonstrate an
topic or supernumerary gland that may be easier to find wi
preoperative knowledge of its whereabouts. These incvde
hyperplastic glands located in the low anterior, middle, and desp
posterior mediastinum; the undescended and intrathycisl
glands; and the rare intrapharyngeal gland. Imaging doe.
however, become essential in MEN I patients with recurent
disease (discussed later). 7
Management of MEN 1
Hyperparathyroidism
‘The timing of parathyroidectomy is an important iss
MEN | HPT involves all parathyroid tissue: thus, any Us
ment surgeons provide is considered palliative.”*” Aemp's
at eradicating all parathyroid tissue can result in a treatment
is far worse than the disease itself (permanent
parahyoiism). In the past, 40% to 50% of MEN 1
Fis presented with nephrolithiasis; however, more
only, patents are being explored for mild or relatively
tic disease. In patients with mild disease, it is
fiate to delay surgery until the serum calcium level
@51 mg/dL. above the upper limit of normal.” Other
indications include nephrolithiasis/nephrocalcinosis, hypercal-
“ora, glomerular filtration rate decreased by 230% for age-
fod gender-matched controls, worsening bone (hip, radius, or
spine) mineral density, especially when the T-score is less than
555 (2SD from normal controls),”” and pancreatitis,”® Vague
jeuropsychiatric disturbances and muscle weakness are less
sgeifc indicators. MEN 1 patients with hypergastrinemia and
jyperealcemia should undergo early parathyzoidectomy.”™#
Hypercalcemia is a potent stimulus for gastrin secretion.
Control of hypercalcemia can lower or even normalize serum
in levels, often alleviating symptoms in MEN 1 patients
with Zollinger-Ellison syndrome (ZES).°
Operative Approach
‘AKocher collar incision is made. The incision is deepened
down through the platysma, and superior and inferior sub-
platysmal flaps are developed. The median raphe is divided
aad the strap muscles are retracted laterally without divi-
sion. The thyroid lobes are sequentially elevated, and all
four parathyroid glands and any supernumerary glands are
exposed, Most supernumerary glands are located in proxim-
iy to the other glands or less often in ectopic locations.
Transcervical thymectomy should be performed to rule out
‘supernumerary gland and to evaluate the thyinus for a car-
cinoid tumor. Failure to identify a superior gland necessitates
‘mobilization of the superior thyroid pole by individually lig-
‘ting the superior thyroid artery and vein or their branches on
tte thyroid capsule. This helps avoid injury to the external
branch ofthe superior laryngeal nerve. Rotation of the upper
pole upward and outward often brings the superior gland into
view, Larger superior glands can migrate along the tracheoe-
‘sophageal groove, into the retroesophageal space, and down
into the posterior mediastinum. These can usually be elevated
into the wound with adequate exposure and gentle traction.
Missing inferior glands should be sought within the thymus,
tte carotid sheath, in an undescended location in front of the
‘crotid bifurcation, and just beneath the thyroid capsule, typ-
‘ally along its inferior pole. The rare ed superior
Ferathyroid gland ean be located within the pharyngeal mus-
Silaur. Intraoperative ultrasonography (IOUS) may be of
‘id in locating ectopic glands within the neck.*!
‘Once four glands have been identified and the transcervi-
‘al thymectomy has been performed, the Surgeon then pro-
(2 With a subtotal parathyroidectomy-" Itis our preference
agate behind an inferior gland ora ion thereof, de
its size. Leaving an inferior gland or remnant makes
ation safer because of the inferior gland's distance
the recurrent laryngeal nerve. If a superior gland is
‘ch smaller or grossly normal compared to the rest, we
(hilt consider leaving this as the remnant. The vascularized
‘Seman should be 50 10 60 mg in weight
Pen onl be pepe peor to excising the other
: to ensure its viability prior to completing the
‘Multiple Endocrine Neoplasia Type 1 —— 677
subtotal parathyroidectomy. If the remnant becomes devas-
cularized, it should be removed and the other inferior gland
trimmed. The remnant or remaining gland should be tagged
with a nonabsorbable suture or preferably a metal clip.
Additional parathyroid tissue should be cryopreserved or
immediately autotransplanted (multiple small pieces total-
ing 50 to 60 mg) into a small, infraclavicular, subcutaneous
pocket. Despite earlier reports regarding the efficacy of cry-
‘opreservation®* and the viability of cryopreserved tissue
in vitro studies,® we have used few of the hundreds of cryo-
preserved specimens stored at Mayo Clinic. When used,
rarely have these delayed autotransplants resulted in mean-
ingfal restoration of normal parathyroid function. It is now
this surgeon's (GBT) practice, when performing a subtotal
parathyroidectomy, to transplant 50 0 60 mg of nonmalig
nant parathyroid tissue into a chest wall subcutaneous pocket
just below the clavicle. If the immunometric PTH level is
2 pmol/L (normal, | to 5 pmoVL) 24 hours postoperatively,
the transplant is removed at the bedside. If the postoperative
immunomettic PTH is below the evel of detection, the trans-
plant is left in place. Time will ell whether grafi-dependent
recurrences will be easier to detect and manage in this
location, but itis thought to be the case. By placing the graft
close to the deltopectoral groove, below the clavicle, selective
venous sampling (SVS) (subclavian vein) can be used along
with SPS and ultrasound to evaluate for graft-dependent
recurrence.
‘Another option for managing MEN 1 primary HPT is total
parathyroidectomy, transcervical thymectomy, and immediate
forearm autotransplantation.***”% Autotransplantation is
classically carried out by implanting 10 to 15 (1-mm) pieces
of fresh tissue into multiple pockets of the nondominant,
brachioradialis forearm muscle. Each site is marked with a
fine, monofilament nonabsorbable suture for future refer-
ence. The forearm skin incision should be made in a longi-
tudinal fashion so as to avoid confusion with regard to a
self-inflicted wound. Recurrence rates are extremely low fol-
lowing total parathyroidectomy, but permanent hypoparathy-
roidism rates can be unacceptably high" Later explantation
is also more formidable with regard to intramuscular implants.
Persistent/Recurrent Hyperparathyroidism
in MEN 1 Patients
Permanent hypoparathyroidism occurs in less than 10% of,
patients undergoing subtotal parathyroidectomy, and most
series describe rates in the range of 1% to 2%.529 The rates
of permanent hypoparathyroidism range from 10% to 30%
undergoing total parathyroidectomy with imme-
diate autografting 5% Total parathyroidectomy, however,
has been associated with recurrence rates as low as 0 (range,
0 to 60%), whereas recurrence rates for subtotal parathy-
roidectomy have never been reported less than 4% (range,
4% to 20%).#5519" Persistent HPT is generally less than
5% with both procedures.” Malmaeus and coworkers
found that when 1 to 2.5 glands were removed, persistent
HPT occurred in 24% and recurrent disease in 62%. The
recurrence and persistence rate was 0 in 18 patients under-
‘going total parathyroidectomy (Table 76-4). 2
Persistent HPT occurs because of misdiagnosis of hyper-
plasia and incomplete resection. Recurrent HPT is generally
678 —— Endocrine Pancreas
eee hOniet teen aub ee
jecurren Persistent Permanent Permanent
Operative Procedure ice HPT(%) __Hypoparathyroidism (%) Laryngeal ro
J
‘Subtotal parathyroidectom 420 <6 <10 (mmost 1-2) <1
Total parathyrodecromy 0.60 Formal
Techour fasts for insulinoma and provocative testing for
sastrin are applied selectively.
a ANTERIOR
ae 76-8, Somatostatin receptor scintigraphy (left [anterior] and right [pos
‘tum with muliple hepatic metastases.
Muluple Endocrine Neoplasia Type 1 —— 683
5
FIGURE 76-7. Endoscopic ultrasonography of a hypoechoic islet
cell tumor in the pancreatic body (arrow).
Imaging
Conventional imaging (percutaneous ultrasound, CT, MRI)
modalities for the carly detection of pancreatic duodenal
endocrine tumors is fraught with hazard; both low sensitivi-
ties and specificities have rendered the earlier mentioned
biochemical screening protocol even more important. «74+
The sensitivity for endoscopic ultrasonography, however,
may be as high as 90% (Fig. 76-7)."'5! Diagnostic accuracy
increases when somatostatin receptor scintigraphy (Fig. 76-8)
correlates with endoscopic ultrasonographic findings.'*™'5!
Endoscopic ultrasonography also offers the opportunity for
directed fine-needle aspiration cytology. We discourage this
for tumors in the pancreatic head because efforts at enucleation
may be thwarted by even the slightest amount of bleeding and
inflammation. If this does occur, surgery should be delayed
for several weeks to allow resolution to take place. The efficacy
of PET scanning for pancreatic duodenal endocrine tumors
remains to be determined.'*
Who Should Undergo Surgery?
Patients with two rising independent serum markers, regard
less of negative imaging, should be explored (Table 76-8)."?
PosTrRioR
jor)) demonstrating a gastrinoma in the region of the
sli
684 — Endocrine Pancreas
TABLE 76-8. Indications for Pancreatic/
nese noe u
‘Two rising (independent) biochemical markerst
‘An elovated biochemical marker plus an unequivocal
imaging study?
‘Two concordant unequivocal imaging studies in the
absence of elevated biochemical markers!
dey ae ca a exctaly ea Bb SOA OG
=a
TERE prsoaaia ead iinpenmats poppe tarccg
ee en Sv
y ‘maging study: EUS + fine-needle aspiration.
Se shes das in eee nae
Ma ‘multiple endocrine neoplasia type 1: EUS = endoscopio
Moalited' fom
fom Shogeeld 3, Rastad J, Akarstom 0. Pancreatic
tndocrine tumors mn mutipis endosiae mason ores
Donerty Gut Stogoo p(s}, Suga Endootrology Pein,
placa Was Wala Soo
An elevated biochemical marker and an unequivocal
imaging study (endoscopic ultrasonography plus fine-needle
aspiration) or concordant endoscopic ultrasonography and
somatostatin receptor scintigraphy in the absence of
biochemical markers would be the other indications, in
the absence of distant metastatic disease.!? In carriers of
germline mutations who have a single positive biochemical
marker, imaging should be carried out yearly (but every
3. years for those with negative biochemistry)."? Some
centers now rely exclusively on endoscopic ultrasonography
for screening, but further validation is warranted.
Hypoglycemic Syndrome
Insulinoma associated with endogenous _hyperin-
sulinism is the most common functioning PET in MEN 1
ents younger than 25 years of age."? Although these
patients often have multiple pancreatic tumors, typically
only one is the source of insulin excess."? This raises the
question of whether selective arterial calcium stimulation
testing with hepatic vein sampling for insulin should
be considered.'®”4°5 Although insulinomas are most often
benign, there is no effective medieal therapy. Without
surgery, hormonal sequelae remain debilitating and life-
threatening.
Surgery involves an 80% distal pancreatectomy to the right
of the superior mesenteric vein with enucleation (Fig. 76-9)
of any remaining pancreatic head tumors, using IOUS."
‘This removes the insulinoma(s) as well as many of the non-
functioning tumors capable of malignant transformation.
Splenic preservation may be possible in young, thin patients
by carefully separating the splenic vein from the underside
of the gland using fine metal clips and an ultrasonic dis-
sector. Small spleens can be preserved on the short gastric
vessels alone, Recurrence rates in patients with MEN 1
are higher than in sporadic cases but nonetheless are
acceptable. Leaving behind 20% of the pancreas generally
limits recurrences and avoids endocrine insufficiency in
most cases.
FIGURE 76-8. Enuclestion ofan islet cell tumor in the pan
head, Dissection of the pancreas “away from tumor” wages
endarterectomy spatula and minimal bipolar cautery is iar’,
Grom Thompson GB. Islet cell tumors. In: Mayo Cae’
Gastrointestinal Surgery. Philadelphia, WB Saunders, 20035
Other Pancreatic Endocrine Tumors
MEN I patients with malignant islet cell tumors (glucagono.
mas, VIP tumors, PTHrp tuinors, and some insulinoma
deserve an equally, if not more aggressive approach, includ.
ing an 80% distal pancreatectomy, splenectomy, and
lymphadenectomy, along with enucleation of any residual
tumors. Isolated liver metastases or a finite number of mul-
Uiple hepatic metastases can be successfully managed, with
excellent control of hormonal sequelae, using a combination
of hepatic resection and radiofrequency thermal ablation, 518
Zollinger-Ellison Syndrome
Gastrinomas represent the most common functioning
pancreatic/duodenal endocrine tumors in MEN I patients.!""
Nearly one third of ZES patients are MEN I kindred members,
and more than 50% of MEN 1 patients have hypergastrinemia,
Jn the past, surgery for MEN 1 ZES was carried out with
reluctance, if at all.'5*"® Cure rates were low, based on nor-
malization of gastrin levels, and medical therapy in the form
of proton pump inhibitors (PPIs) has been extremely effec-
tive at eliminating peptic acid sequelae. Medical therapy
does not, however, prevent malignant transformation, not
does it prevent the development of metastatic disease.”
Presently, 30% to 50% of patients undergoing surgical
exploration have at least regional nodal metastases, many o!
which are amenable to resection, often providing excellent
Palliation. 5! More than 80% of gastrinomas in MEN |
Patients are duodenal in origin.3°.157 In addition. ZES
Patients appear at greater risk for malignant transformation
of nonfunctioning tumors when compared to other MEN !
Patients.''®® Norton and colleagues have shown that
patients with nodal metastases can achieve similar survival
benefits with operative intervention compared to those with
out lymph node involvement. '®! Gastrin levels often rise ate
in MEN I patients. Once the gastrin level is elevated. 30%
to 50% of patients already harbor nodal metastases even it
the face of negative imaging studies. Resection of large?
(3-cm) PETs does not appear to reduce the risk of develo?
ing liver metastases, once again making a strong argument fo"
screening, early detection, and early surgical intervention:
‘he ‘most often performed has been popularized
yy De Norman Thompson atthe University of Michigan at
Me Atbor (Fig. 76-10).'29718168 The surgery is carried
A er adequate treatment with PPIs to heal active ulcers.
fanibioics and deep venous thrombosis prophylaxis are
prided. The abdomen is thoroughly explored through
miverse epigastric or chevron incision, Careful attention
i paid to the liver, which is explored both by palpation and
{OUS. The gastrocolic omentum is completely mobilized
fffthe transverse colon from left to right, entering the lesser
Sox Both colonic flexures are mobilized and retracted cau-
{ally. The duodenum is widely kocherized out to the liga-
tren of Treitz, The avascular plane along the inferior border
ifthe pancreas is incised and the pancreatic body is freed to
{s superior border. The lienorenal and iienophrenic liga-
iments are divided using electrocautery, and the spleen, body,
ind til of the pancreas are mobilized to the splenic vein-
siperor mesenteric vein junction. The inferior mesenteric
tein may require division to further facilitate exposure. The
Superior mesenteric vein is then isolated from the neck of
the pancreas. Division of the anteroinferior pancreaticoduo-
denal vein, as well as the right gastroepiploic vessels, aug-
renis exposure of the uncinate and pancreatic head and
reduces the risk of avulsing these delicate veins as the oper-
ation proceeds. At this point, careful bidigital palpation of
theentire gland is carried out along with IOUS in anteropos-
teior planes and transverse-longitudinal directions. S|
attention is paid to the location of the pancreatic and
ducts and their relationship to nearby islet cell tumors.
Lymph nodes are removed from along the posterior aspect of
the pancreatic head, the kepatoduodenal ligament, the subpy-
lore region, branches of the celiac artesy, and the proximal
supetior mesenteric artery. In patients with hypergastrinemia,
2 longitudinal duodenctomy is made along the free wall of
the second portion of the duodenum. The duodenal wall is,
POURE 76-10, Eighty percent distal pancreatectomy (splenic
Ring), enuclestions i 4
(pancreatic head), exploratory duodeno:
pe lymphadenectomy for a patient with multiple endocrine
(Coxeny (MEN) type 1 and Zollinger-Ellison syndrome.
‘toy, 4f.of Dr. Norman Thompson, University of Michigan, Ann
Michigan.)
Multiple Endocrine Neoplasia Type 1 —— 685
carefully palpated between thumb and index finger proxi-
mally across the pylorus and distally beyond the ligament of
Treitz. The duodenal mucosa is intussuscepted into the duo-
‘Duodenal carcinoids are the principle cause of ZES in MEN
1 patients" They are often multiple and frequently
metastasize to regional lymph nodes and subsequent to the
liver, Gastric carcinoids can be gastrin producing (highly
malignant) or can evolve secondary tothe hypergastrinemia
from gastrin;producing duodenal carcinoids (enterochro-
‘maffin cell hyperplasia).2!"% Treatment requires excision
and lymphadenectomy and, less often, gastrectomy or
pancreatoduodenectomy, depending on the extent of foregut
involvement.
herited tumo
disorder caused by mutations in the MEN/ t
ae jumor suppressor
e = (craosome 13) Theiagoose is made in peas
by cucu ‘of the three major manifestations
Cetin HPT [>954], pancreatic neuroendocrine
ie ae 75%}, or pituitary tumors (30% to 55%)
a rating one major manifestation in an at-risk
ly member of a known MEN 1 kindred. Genetic testing
ion is clearly indicate
rseion lt agonoas, VIP irs, ad
Prcioning tumors. There is increasine evidence suggesting
fanetrly surgical intervention for MEN W/ZES patients and
patients with subclinical pancreatic neuroendocrine tumors
ate ult in prolonged palliation and a redvctich © the rate
does gant transformatcn. Since biochemical abnormalities
oral ected decades prior othe development of over lin.
carve Tapioms, genetic testing, biochemical sereening, and
Jnaging of appropriately selected patients appear ‘warranted.
Acknowledgments
“The authors thank Abbie L. Young,
critique ofthis chapter
MS, and Dr. Britt Skogseid for their
REFERENCES
1 Erdem J Zar normalen und pthologchenNistlogie der sana
ern you papi Bes Fo! OE
2. 6 utermalgetmoven der dasen it ine skein be
» fermen nk ao 38233
. Wermer® Gena spss of aenonatosiof endocrine
Med 1954;16:363. 7 ren ee
4, son. StoscidB, Oberg Kt Mul endosine 2
type I gene maps to. ‘chromosome I and is “ in ain tre
opel 11 ands ot in instinoma Nate
3 Ther RBs. Wosdg Ct a Awaxsion pai
rms alipe exer neplaca ype | wih tof les
comune HEN ol Met 9991 218
Brame Laon 6 Bm Ctl Latin fe ee
mt ci apn sa gon win ee
teh yon apg tr, Ps Nas as U 8A
1. Pda
ie hens Bs Sekaguchi iN Bale AE, et al, Clonality of parathyroid
Se W Eat Med
teens
Lis IN, Yen HF, Lan CHW, mute ns nt
5 gran i Re cena oP
Send ML Male ic pnp Gn eae
aim nl ea 1
ice Me Nah oc Cb rae A aia ipl
| memset
oles Yr an Lt Ht. Cra ma
ice nob AEN stepected patients: MEN I axe finding, Bur} CH
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Intro Narration: Even The Things That Give You Life Can Severely Hurt You The MostDocument5 pagesIntro Narration: Even The Things That Give You Life Can Severely Hurt You The MostFrances Oscar GaviolaNo ratings yet
- Name of The Drug Date Ordered Classification Dose Frequency Route Mechanism of Action Specific Indication Side Effects Nursing ImplicationDocument9 pagesName of The Drug Date Ordered Classification Dose Frequency Route Mechanism of Action Specific Indication Side Effects Nursing ImplicationFrances Oscar GaviolaNo ratings yet
- NCPDocument2 pagesNCPFrances Oscar Gaviola100% (1)
- PnssDocument2 pagesPnssFrances Oscar GaviolaNo ratings yet
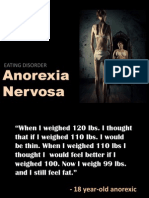
- Anorexia Nervosa: Eating DisorderDocument21 pagesAnorexia Nervosa: Eating DisorderFrances Oscar GaviolaNo ratings yet
- Waist Circumference (Abdominal Girth) and Health: It Is More Than Just Risk of StrokeDocument2 pagesWaist Circumference (Abdominal Girth) and Health: It Is More Than Just Risk of StrokeFrances Oscar GaviolaNo ratings yet
- Red Velvet Cupcakes With Cream Cheese Frosting RecipeDocument2 pagesRed Velvet Cupcakes With Cream Cheese Frosting RecipeFrances Oscar GaviolaNo ratings yet
- Drug StudyDocument4 pagesDrug StudyFrances Oscar GaviolaNo ratings yet