Professional Documents
Culture Documents
Iodo Povidona
Iodo Povidona
Uploaded by
SchuanchOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Iodo Povidona
Iodo Povidona
Uploaded by
SchuanchCopyright:
Available Formats
Pseudobacteremia Attributed to Contamination of Povidone-lodine with
Pseudomonas cepacia
RUTH L BERKELMAN, M.D.; SHARON LEWIN, M.D.; JAMES R. ALLEN, M.D.; ROGER L ANDERSON,
Ph.D.; LAWRENCE D. BUDNICK, M.D.; STANLEY SHAPIRO, M.D.; STEPHEN M. FRIEDMAN, M.D.;
PETER NICHOLAS, M.D.; ROBERT S. HOLZMAN, M.D.; and ROBERT W. HALEY, M.D.; Atlanta,
Georgia; and New York, New York
Pseudomonas cepacia was recovered from the blood Materials and Methods
cultures of 52 patients in four hospitals in New York over EPIDEMIOLOGIC INVESTIGATION
7 months from April through October 1 9 8 0 . At City Hospital Center at Elmhurst we reviewed blood cul-
Epidemiologic investigation in one hospital indicated that ture log books for January through October 1980 to identify all
the positive results of blood culture represented Pseudomonas isolates and all bacteriology reports for June
pseudobacteremias and implicated a 1 0 % povidone- through October to identify isolates of P. cepacia from sites
iodine solution used as an antiseptic and disinfectant other than blood. We further reviewed medical records of all
(Pharmadine; Sherwood Pharmaceutical Company, patients with blood cultures positive for P. cepacia and abstract-
Mahwah, New Jersey) as the source of contamination. ed information on age, sex, underlying illnesses, indications for
Physicians who drew blood cultures positive for P. cepacia blood cultures, and use of intravenous therapy and medications.
were more likely to have left povidone-iodine on the skin We interviewed pharmacy and central supply personnel about
before venipuncture (p=0.026) and were more likely to distribution of supplies to the various areas of the hospital and
have applied povidine-iodine to the blood culture bottle laboratory personnel about methods for processing and han-
tops and to have left it there while inoculating the blood dling blood culture specimens.
culture media ( p = 0 . 0 0 7 ) than those who drew cultures
We conducted a case-control study at City Hospital Center at
negative for P. cepacia. Direct inoculation of Pharmadine
Elmhurst to ascertain whether blood cultures positive for P.
into brain-heart infusion broth yielded P. cepacia;
cepacia were significantly associated with the medical service.
however, 2 weeks after the first cultures, the same
We used a table of random numbers to select 118 control cul-
Pharmadine bottles were culture negative. The iodine
tures from the 2360 blood cultures obtained between 30 June
concentrations of the contaminated Pharmadine solutions
and 4 October 1980. We excluded six cultures from final analy-
were similar to those of 1 0 % povidone-iodine solutions
sis: two that were positive for P. cepacia, one that was actually a
distributed by other manufacturers.
pleural fluid culture, and three for which service was not re-
corded. We compared the bacteriology reports of the remaining
P O V I D O N E - I O D I N E SOLUTION is widely used in hospitals 112 with those of the 17 cultures positive for P. cepacia to
and other health care institutions as a skin and mucous identify differences in services of origin.
A questionnaire was administered to 35 medical and 12 pe-
membrane antiseptic and as a disinfectant. Unlike other diatric house staff working during the investigation. Only the
classes of antiseptics and disinfectants (1), povidone- responses of the 30 medical and 10 pediatric house staff who
iodine solutions have not previously been reported to be indicated that they routinely obtained one or more blood cul-
intrinsically contaminated. tures per week were included in the epidemiologic analysis. We
compared the blood culturing techniques of the medical house
In October 1980, City Hospital Center at Elmhurst
staff with those of the pediatric house staff and the techniques of
reported to the Centers for Disease Control (CDC) that the medical house staff who had drawn the cultures positive for
17 blood cultures obtained over the preceding 3 months P. cepacia with those who had not drawn cultures positive for
were positive for Pseudomonas cepacia. An epidemiolog- the organism.
ic investigation was conducted by hospital personnel, the We telephoned infection control personnel at 27 hospitals in
the New York City area, including all those with more than 500
New York City Department of Health, and C D C at this
beds, and requested them to review their microbiology laborato-
hospital and subsequently at three other New York City ry records for 1980 to identify all isolates of P. cepacia. In the
hospitals identified as having had clusters of blood cul- three hospitals that identified five or more blood cultures posi-
tures positive for P. cepacia over the previous 6 months. tive for P. cepacia, we reviewed the medical records of all pa-
We describe herein the epidemiologic investigation that tients with cultures positive for P. cepacia. Techniques and
products used at each of these hospitals were compared to iden-
implicated contaminated povidone-iodine solution pro- tify those used in common.
duced by one manufacturer (Pharmadine; Sherwood
Pharmaceutical Company, Mahwah, New Jersey) as the LABORATORY STUDIES
source of the problem and that established that the posi- Available blood isolates from three hospitals and isolates re-
covered from povidone-iodine solutions were identified by stan-
tive blood cultures were pseudobacteremias (that is, false-
dard biochemical testing (2) in the Epidemiologic Investigations
positive results of blood culture). We also present find- Laboratory Branch, Bacterial Diseases Division, Center for In-
ings of subsequent laboratory studies that have further fectious Diseases, CDC. Kirby-Bauer antimicrobial susceptibili-
defined the problem. ty testing (3) was done on all isolates identified as P. cepacia.
The following special laboratory studies also were done.
• F r o m the Hospital Infections Branch a n d Epidemiologic Investigations Labora- Isolation of Pseudomonas cepacia from Povidone-lodine So-
tory Branch, Bacterial Diseases Division, Center for Infectious Diseases, Centers lutions: Fifty-four bottles of Pharmadine solution and 11 sets of
for Disease Control, Atlanta, Georgia; a n d M t . Sinai Services at City Hospital Pharmadine swabsticks (Sherwood Pharmaceutical Company)
Center at Elmhurst, M t . Sinai School of Medicine; N e w York City D e p a r t m e n t of
Health; a n d Bellevue Hospital Center, N e w York University School of Medicine, from 19 manufacturing lots were obtained from the stock of
New York, N e w York. three of the hospitals investigated and were examined for the
32 Annals of Internal Medicine. 1981;95:32-36. ©1981 American College of Physicians
Downloaded From: http://annals.org/ by a Michigan State University Libraries User on 08/14/2018
presence of P. cepacia. Three aliquots (0.02, 0.1, and 0.5 mL) of
Pharmadine solution were chosen for direct culture to simulate
quantities of povidone-iodine that might be introduced into
blood culture media if blood were inoculated through a blood
culture bottle top that had povidone-iodine pooled in its depres-
sion. Each aliquot was separately added to 125 mL screw-cap
flasks containing 50 mL of brain-heart infusion broth with
0.5% beef extract. Swabsticks were aseptically bent and placed
directly into wide-mouth jars containing 150 mL of brain-heart
infusion broth. Broth cultures were incubated at 35 °C and ob-
served for turbidity daily for 7 days. Aliquots of broths showing
turbidity were subcultured onto sheep blood agar and MacCon-
key agar. All nonturbid broths were subcultured on day 7.
Two different culture techniques were used for subsequent
attempts to recover P. cepacia from bottles of solution from
which it had been isolated initially: direct inoculation into
brain-heart infusion broth and Millipore filtration (Millipore
Corporation, Bedford, Massachusetts) of 10 mL povidone-
iodine in 50 mL brain-heart infusion broth. The filter was then
washed with 50 mL of brain-heart infusion broth and was incu-
bated on a blood agar plate.
Survival of Pseudomonas cepacia in Povidone-iodine Solu-
tion: Four strains of P. cepacia were tested to establish their
survival in 10% povidone-iodine solutions: an isolate from
Pharmadine, lot X80290, adapted to deionized water; an isolate
from Pharmadine, lot U80250; an isolate from a clinical speci-
men; and a CDC laboratory stock strain. Two povidone-iodine
solutions were used: Pharmadine, lot X80299, from which via-
ble organisms could no longer be recovered; and Betadine, lot
M793136 (Purdue Frederick Company, Norwalk, Connecticut).
For the experiment, 10" to 1010 organisms of each of the four test
strains of P. cepacia were suspended separately in 1 mL deion-
ized water and then were mixed with 10 mL of each of the two
povidone-iodine solutions. For the strain adapted to deionized
water, 2 mL of deionized water containing 1.4 times 106 organ-
isms were mixed with 10 mL of each of the povidone-iodine
solutions. Aliquots of 0.1 mL and 0.5 mL were obtained from
these mixtures at 0, 10, and 60 minutes and at 4 and 24 hours
and were inoculated separately into flasks containing 50 mL
brain-heart infusion broth and either 0.25% or 0.5% or no sodi-
um thiosulfate. Specimens were incubated at 35 °C and were
subcultured as described above.
Measurements of Iodine Concentration in Povidone-iodine
Solutions: Available iodine contents of coded samples of Phar-
madine, Betadine, and Povidine solution (National Pharmaceu-
tical Manufacturing Company, Baltimore, Maryland) were as-
certained by titration with sodium thiosulfate at a commercial
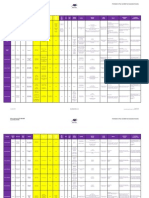
laboratory (MacMillan Research, Marietta, Georgia). The free Figure 1 . Blood cultures positive for Pseudomonas cepacia at four
iodine contents of coded samples of Pharmadine, Betadine, and New York City hospitals, by month of culture, 1 9 8 0 .
Povidine were ascertained by the distribution of iodine between
the aqueous (product) phase and a nonmiscible solvent, hep-
tane, at 25 °C (4) (done by Murray W. Winicov, Kansas City, underlying illnesses and the reasons for obtaining blood
Missouri). All statistical tests used Fisher's exact test; two- cultures varied greatly; the latter included diagnostic
tailed p values are reported unless otherwise indicated. work-up of pyrexia and follow-up of documented infec-
tions at other sites.
Results
Only six of the 14 patients had a maximum tempera-
CLINICAL A N D EPIDEMIOLOGIC F I N D I N G S ture above 38.3 °C the day the blood culture was drawn,
From 30 June to 4 October 1980, P. cepacia was isolat- and no patient had a temperature more than 1 °C higher
ed from 17 blood cultures obtained from 14 patients at than the maximum temperature of the previous day. N o
City Hospital Center at Elmhurst (Figure 1). No isolates patient experienced rigors. Two were hypotensive (systol-
of P. cepacia and only one of a species of Pseudomonas ic blood pressure less than 90 mm Hg) for reasons unre-
other than P. cepacia had been isolated from blood cul- lated to possible septicemia. The median leukocyte count
tures in the preceding 6 months. was 9100/mm 3 (range, 2500 to 30 000/mm 3 ). Although
Fifteen of the blood cultures positive for P. cepacia cultures from other sites were obtained at or near the
were obtained from 12 patients on the medical service; same time as the blood cultures in 12 of the patients,
the other two cultures were taken from two patients on none were positive for P. cepacia. Only four patients were
the hemodialysis unit. The 14 patients were hospitalized treated with antibiotics for possible septicemia as a result
on two of the 10 patient care floors. The median age of of the positive cultures. In summary, the clinical infor-
the 14 patients was 59.5 years (range, 23 to 90 years); mation did not suggest that any of the patients had gram-
eight of the patients were female. Type and severity of negative septicemia.
Berkelman et al. • Pseudomonas Pseudobacteremia 33
Downloaded From: http://annals.org/ by a Michigan State University Libraries User on 08/14/2018
Table 1 . Iodine Concentrations of 1 0 % Povidone-lodine Solutions of the seven physicians who obtained positive cultures
allowed the povidone-iodine to pool in the depression in
10% Povidone- Availat )le Free Iodine
Iodine Solution Iodine *
the stopper of the blood culture bottle and inoculated
directly through the pool of povidone-iodine, whereas
fjig/mL f % jug/mL only three of the 23 who were not known to have drawn a
Pharmadine, lot 10000 1.00 1.2
X80299 contaminated culture used this technique (p = 0.007).
Pharmadine, lot 10 000 1.00 1.5 Thus, epidemiologic evidence implicated povidone-iodine
U80250 as the source of the pseudobacteremias.
Pharmadine, lot 10 200 1.02 1.4 Through our telephone survey we identified three other
V80259
9500 0.95 0.6
hospitals in New York City with apparent clusters of P.
Betadine, lot
M793163 cepacia bacteremias (Figure 1); the positive cultures had
Povidone, lot 01428 11 100 1.11 1.3 occurred from April through October 1980. Review of
the patients' medical records indicated that few of the
* Available iodine equals thiosulfate-titratable iodine.
t One microgram per millilitre equals 1 part per million. patients had clinical features consistent with septicemia
and that pseudobacteremia had been strongly suspected
Because the initial epidemiologic findings suggested by the physicians of most of these patients. Each of the
pseudobacteremia, we studied the circumstances under four hospitals identified as having clusters of pseudobac-
which the positive blood cultures were done and pro- teremias attributed to P. cepacia purchased Pharmadine
cessed. Fifteen of the 17 blood cultures positive for P. for use as an antiseptic or disinfectant; no other brand of
cepacia had been obtained from the medical service, iodophor was available in these hospitals.
whereas only 54 of 112 (48%) randomly selected blood One patient at each of two hospitals was identified as
cultures came from this service (p = 0.003). Because all having cultures positive for P. cepacia from sites other
blood cultures were handled and processed in an identical than blood. One patient had the organism isolated from
manner in the laboratory, the clustering of the positive an abdominal wound that had been treated with Pharma-
cultures on the medical service made it highly improba- dine wet-to-dry dressings. A second patient had a sputum
ble that contamination of the specimens occurred in the culture positive for P. cepacia after use of Pharmadine for
laboratory. Also, because the same brand of blood cul- care of her tracheostomy site.
ture medium was distributed as needed to all areas of the
hospital, intrinsic contamination of the medium was an MICROBIOLOGIC RESULTS
unlikely explanation for the pseudobacteremias. Of the 59 isolates of P. cepacia obtained from blood
Pediatrics was the only service other than medicine cultures by the four New York City hospitals, 17 isolates
that obtained more than 10% of the hospital's blood cul- from three hospitals were sent to C D C ; all were con-
tures; none of the blood cultures positive for P. cepacia firmed as being P. cepacia. Antimicrobial susceptibility
had been obtained on this service. Analysis of the ques- testing showed all isolates to be sensitive to trimetho-
tionnaire surveys indicated that the blood culturing tech- prim-sulfamethoxazole and nalidixic acid and resistant to
niques reported by house staff on the medical service dif- gentamicin, nitrofurantoin, cephalothin, ampicillin, tetra-
fered from those reported by house staff on the pediatric cycline, and colistin. Susceptibility to chloramphenicol,
service in 2 ways: Pediatric house staff often obtained less kanamycin, amikacin, and carbenicillin varied among the
than the 10 m L blood, usually drawn by medical house isolates. Biotypes were identical.
staff; and medical house staff differed in their use of povi- Pseudomonas cepacia in pure culture was isolated
done-iodine. Eleven of 30 medical house staff but none of from three previously unopened 16-ounce bottles of
10 pediatric house staff reported doing venipuncture Pharmadine solution, lot X80299, manufactured 10 days
without removing the povidone-iodine used for skin anti- before culture, and from one previously opened 16-ounce
sepsis (p = 0.038). Also, 13 of 30 medical house staff container of Pharmadine solution, lot U80250, manufac-
versus two of 10 pediatric house staff reported using povi- tured 4 months before culture. Pseudomonas cepacia was
done-iodine to disinfect the tops of the blood culture bot- also recovered from lot U80250 9 days after the first cul-
tles before inoculation of a blood specimen (p = 0.27). tures, but it could not be isolated from lots X80299 and
Seven medical house staff, including medical students, U80250 9 days and 16 days, respectively, after the first
interns, and residents, were documented to have drawn positive cultures. Sixteen other lots of Pharmadine solu-
12 of the 15 blood cultures positive for P. cepacia on the tion were cultured, but no viable organisms were recov-
medical service; the persons who drew the remaining ered. One set of Pharmadine swabsticks, lot X80290,
three contaminated cultures could not be identified. Five manufactured 1 month before culture, yielded P. cepacia.
of the seven house staff who drew the contaminated cul- Attempts to recover P. cepacia from povidone-iodine so-
tures versus five of the 23 medical house staff who did not lutions after laboratory inoculation of organisms from
draw contaminated cultures did venipuncture without re- broth culture have not been successful.
moving the povidone-iodine from the skin (p = 0.026). The available iodine concentration of the povidone-io-
Six of seven house staff who obtained positive cultures dine solutions tested ranged from 9500 to 11 100 jag/mL
and seven or 23 house staff who did not draw contami- (0.95% to 1.11%) (Table 1). The free iodine concentra-
nated cultures used povidone-iodine to disinfect the tops tions of samples of three lots of Pharmadine ranged from
of the blood culture bottles (p = 0.025). Moreover, five 1.2 to 1.5 juLg/mL compared with 0.6 to 1.3 juig/mL for
34 July 1981 • Annals of Internal Medicine • Volume 95 • Number 1
Downloaded From: http://annals.org/ by a Michigan State University Libraries User on 08/14/2018
samples of two povidone-iodine solutions manufactured pyrrolidone-iodine powder with water. The water source
by other companies. was a municipal supply that was then processed through
resin deionizers at the plant. Although significant con-
Discussion tamination of municipal water supplies with Pseudomo-
Pseudomonas cepacia is a motile nonfermentative nas would be unlikely (13), microbial contamination of
gram-negative bacillus able to use a large number of sub- resins is a well-described problem (14). In this outbreak
strates over a wide range of temperatures; it has a diverse P. cepacia probably proliferated on the deionizing resin
geographic distribution and has been isolated from soil, in the water system and contaminated the water supply
rivers, and vegetation (5). More recently, the hospital en- and possibly manufacturing surfaces within the plant. Af-
vironment has become an important source for isolation ter the problem was identified, a Millipore filtration sys-
of P. cepacia; the organism has been recovered from irri- tem with a 0.22-jam filter was installed between the
gating fluids, anesthetics, ultrasonic nebulizers, deter- deionizing resin and the mixing tanks; this system is be-
gents, and disinfectants, including chlorhexidine and ing evaluated to ascertain whether it will prevent bacteri-
quaternary ammonium compounds (6). Pseudomonas ce- al contamination of the water supply used in manufactur-
pacia has only infrequently caused disease in humans; ing povidone-iodine products.
bacteremia associated with contaminated intravenous We considered several hypotheses as possible explana-
fluid (7) and blood pressure transducers (8), and endocar- tions for survival of P. cepacia in the povidone-iodine
ditis in heroin addicts (9), pneumonitis, urinary tract in- solution. First, we hypothesized that the product was de-
fections, and wound infections caused by contaminated fective and contained a low concentration of iodine active
solutions have all been described (6). against microorganisms. We measured the iodine concen-
Among the clusters of pseudobacteremias previously tration of several povidone-iodine solutions. The "avail-
described (10, 11), several have been attributed to con- able" or sodium thiosulfate titratable iodine is the most
taminated benzalkonium chloride or other antiseptics (1). commonly obtained measurement of iodine content of
Contamination of iodophor products, however, has not povidone-iodine solutions (12). Both Pharmadine and po-
been described previously and represents a newly identi- vidone-iodine solutions by other manufacturers had an
fied source of pseudobacteremia. False-positive blood cul- available iodine content of approximately 1% (10 000
tures may have several adverse consequences including jag/mL), conforming with USP standards for a 10% po-
additional laboratory studies, administration of unneces- vidone-iodine solution (Table 1).
sary and potentially dangerous antibiotics, and prolonga- The available iodine is known to be divided between
tion of hospital stay. iodine in complex (iodine bound by the carrier molecule
Contaminated products in hospitals may cause true in- and iodides) and "free" iodine, which may be as little as
fections as well as false-positive laboratory tests. Povi- 1.0 juLg/mL (15, 16). The free iodine in solution has been
done-iodine solutions are used for many purposes, includ- well established to possess microbicidal activity (12, 17);
ing skin antisepsis before surgery, cleansing and packing in contrast, there is little evidence to substantiate micro-
of wounds and ulcers, treatment of vaginitis, and disin- bicidal activity of the complexed iodine. Therefore, the
fection of patient care items. Although only a few pa- free iodine concentration may be a more accurate mea-
tients in this outbreak were identified as being colonized sure of bactericidal activity than available iodine. Mea-
with P. cepacia secondary to use of contaminated Phar- surements of free iodine in the three samples of Pharma-
madine and no patient had a clinically adverse effect dine solution were similar to those of two other
clearly established, the potential exists for patients to de- povidone-iodine solutions analyzed. Thus, we could not
velop serious infection from use of contaminated povi- show by chemical measurements of iodine content that
done-iodine solution. the contaminated Pharmadine solution was less bacteri-
Iodine in solution has a broad spectrum of antimicrobi- cidal than other marketed solutions.
al activity against both gram-negative and gram-positive Our second hypothesis was that organic or inorganic
vegetative bacteria, fungi, viruses, protozoa, and even debris had mechanically protected P. cepacia organisms
bacterial spores (12); however, elemental iodine solutions from Pharmadine. Although a small quantity of debris
have numerous side effects (such as staining, odor, and was present on the filter after Millipore filtration, we
skin or mucous membrane irritation) that have limited were unable to identify constituents of the debris other
their usefulness in patient care practices. Iodophors, than numerous bacteria.
complexes of iodine and a surfactant or nonsurfactant Finally, we considered that the strains of P. cepacia
carrier molecule, were developed to reduce these side ef- isolated from Pharmadine possessed a greater iodine tol-
fects. Povidone-iodine solution, USP, is the common erance than other strains. Few studies of microbial resist-
name for iodine in complex with the nonsurfactant com- ance to povidone-iodine solutions have been published. In
pound polyvinylpyrrolidone in a 10% solution. one study a minimal inhibitory concentration of iodine
We tried to learn how the povidone-iodine solution for a wild strain of P. cepacia was reported to be 16 jag/
had become contaminated and what factors had allowed mL (18); in another study organisms were reported not to
survival of organisms in the solution. Discussions with develop resistance to povidone-iodine after serial passages
the manufacturer of Pharmadine indicated that the povi- through that solution (19). These studies, however, might
done-iodine solution was prepared in a multistage process not be accurate for two reasons. First, these experiments
that included mixing commercially available polyvinyl- were based on measurements of available iodine concen-
Berkelman et al. • Pseudomonas Pseudobacteremia
35
Downloaded From: http://annals.org/ by a Michigan State University Libraries User on 08/14/2018
trations although available iodine has not been shown to Hospital Infections Branch, Center for Infectious Diseases, Centers for Dis-
ease Control; Atlanta, G A 30333.
be responsible for the inhibitory and bactericidal activity
References
of povidone-iodine (15). Second, because the iodine in a
1. K A S L O W RA, M A C K E L DC, M A L L I S O N G F . Nosocomial pseudobac-
10% povidone-iodine solution may be in a tighter com- teremia: positive blood cultures due to a contaminated benzalkonium
plex than that of a more dilute preparaton, dilution of antiseptic. JAMA. 1976;236:2407-9.
2. W E A V E R RE, T A T U M WW, H O L L I S D G . The Identification of Unusual
povidone-iodine may paradoxically increase the concen- Pathogenic Gram-Negative Bacteria (Elizabeth O. King). Atlanta: Cen-
tration of free iodine and possibly increase its bactericidal ter for Disease Control; 1972.
activity ([4], W I N I C O V M W . Personal communication). 3. B A U E R AW, K I R B Y W M M , SHERRIS JC, T U R C K M. Antibiotic suscep-
tibility testing by a standardized single disk method. Am J Clin Pathol.
In this outbreak P. cepacia may have developed toler- 1966;45:493-6.
ance to the levels of free iodine present in povidone-io- 4. WINICOV MW, SCHMIDT W, inventors. West Laboratories, Inc., assign-
dine; tolerance of P. cepacia to levels of free iodine higher ees. Germicidal compositions and methods for preparing the same. U.S.
patent 3,028,299. 1962 April 3. 16 p. Int CI 167-17.
than those found in currently marketed povidone-iodine 5. H U G H R, G I L A R D I GL. Pseudomonas. In: L E N N E T T E EH, B A L O W S A,
solutions has been described ( F A V E R O MS. Personal HAUSLER WJ J R , T R U A N T JP, eds. Manual of Clinical Microbiology.
3rd ed. Washington, D.C.: American Society for Microbiology;
communcation). Although we could not document toler- 1980:288-317.
ance to 10% povidone-iodine solutions in the laboratory, 6. EDERER GM, MATSEN JM. Colonization and infection with Pseudomo-
we used organisms isolated from Pharmadine that had nas cepacia. J Infect Dis. 1972;125:613-8.
7. M E Y E R GW. Pseudomonas cepacia septicemia associated with intrave-
been passed through artificial media; partial or complete nous therapy. Calif Med. 1973;119 (July):15-8.
loss of iodine resistance after subculturing in broth has 8. W E I N S T E I N RA, E M O R I T G , A N D E R S O N RL, S T A M M WE. Pressure
been documented (20). transducers as a source of bacteremia after open heart surgery: report of
an outbreak and guidelines for prevention. Chest. 1976;69:338-44.
Although we favor the hypothesis that the P. cepacia 9. N O R I E G A ER, R U B I N S T E I N E, SIMBERKOFF MS, R A H A L JJ J R . Sub-
was tolerant to levels of free iodine found in povidone- acute and acute endocarditis due to Pseudomonas cepacia in heroin
addicts. Am J Med. 1975;59:29-36.
iodine solution, further work is needed with organisms 10. WEINSTEIN RA, STAMM WE. Pseudoepidemics in hospital. Lancet.
comparable to those free growing in deionized water. 1977;2:862-4.
Further work is also needed to ascertain whether free 11. C E N T E R FOR DISEASE CONTROL. Nosocomial pseudobacteremia. Mor-
bid Mortal Weekly Rep. 1980;29:243-4,249.
iodine alone accounts for the microbicidal activity of the 12. F O O D AND D R U G ADMINISTRATION. O-T-C topical antimicrobial prod-
solution. ucts. Fed Reg. 1978:1218,1231-6.
Iodophors fill a unique and useful role in current medi- 13. H E R M A N LG. Sources of the slow-growing pigmented water bacteria.
Health Lab Sci. 1976;13:5-10.
cal practice. Confirmation of bacterial contamination of 14. S T A M M JM, E N G E L H A R D WE, PARSONS JE. Microbiological study of
povidone-iodine solution, however, has raised serious water-softener resins. Appl Microbiol. 1969;18:376-86.
15. RODEHEAVER G , TURNBULL V, EDGERTON M T , K U R T Z L , EDLICH
questions about the way in which these products should RF. Pharmocokinetics of a new skin wound cleanser. Am J Surg.
be manufactured and used. More complete information is 1976;132:67-74.
needed on the mechanism of the microbicidal activity of 16. HARVEY SC. Antiseptics and disinfectants; fungicides; ectaparasiticides.
In: G I L M A N A G , G O O D M A N LS, G I L M A N A, eds. Goodman and Gil-
iodophors and the efficacy of the iodophor products. man's The Pharmacological Basis of Therapeutics. 6th ed. New York:
A C K N O W L E D G M E N T S : The authors thank Mr. Murray W. Winicov, Macmillan Publishing Co., Inc.; 1980:973.
West Agro-Chemical, Inc., for measuring free iodine concentrations and for 17. A L L A W A L A NA, RIEGELMAN S. The properties of iodine in solutions of
his discussions with the authors on povidone-iodine chemistry; Ms. Betty W. surface-active agents. J Am Pharm Assoc. 1953;42:396-401.
Holland and Ms. Claudine B. Bryant, Hospital Infections Laboratory Sec- 18. P R I N C E H N , N O N E M A K E R WS, N O R G A R D RC, P R I N C E DL. Drug re-
tion, Centers for Disease Control, for their assistance with the laboratory sistance studies with topical antiseptics. J Pharm Sci. 1978;67:1629-31.
investigations; Lilla Lyon, M.D., New York City Department of Health, for 19. H O U A N G ET, G I L M O R E OJA, R E I D C, S H A W EJ. Absence of bacterial
her assistance with the epidemiologic investigation; and Ms. Ruth W. Slade resistance to povidone iodine. J Clin Pathol. 1976;29:752-5.
for her excellent secretarial support. 20. FAVERO MS, D R A K E CH. Factors influencing the occurrence of high
numbers of iodine-resistant bacteria in iodinated swimming pools. Appl
• Requests for reprints should be addressed to Ruth L. Berkelman, M.D.; Microbiol. 1966;14:627-35.
36 July 1981 • Annals of Internal Medicine • Volume 95 • Number 1
Downloaded From: http://annals.org/ by a Michigan State University Libraries User on 08/14/2018
You might also like
- Is The VolumeDocument5 pagesIs The VolumePaola NapoliNo ratings yet
- Usefulness of Blood CultureDocument5 pagesUsefulness of Blood CultureADINo ratings yet
- Case 22-2017: A 21-Year-Old Woman With Fever, Headache, and MyalgiasDocument11 pagesCase 22-2017: A 21-Year-Old Woman With Fever, Headache, and MyalgiasMaria Dolores Herrero MendozaNo ratings yet
- Benezech 1975Document1 pageBenezech 1975amor letrasNo ratings yet
- J. Clin. Microbiol. 2011 Weinstein S26 9Document4 pagesJ. Clin. Microbiol. 2011 Weinstein S26 9Prakarsa Adi Daya NusantaraNo ratings yet
- PPT HiponatremiDocument9 pagesPPT HiponatremiArini NurlelaNo ratings yet
- Immunohematology ASCPi Review Booklet (Part 1)Document22 pagesImmunohematology ASCPi Review Booklet (Part 1)Mark Justin OcampoNo ratings yet
- Diagnostic Utility of Clinical Laboratory Data Determinations For Patients With The Severe COVID-19Document18 pagesDiagnostic Utility of Clinical Laboratory Data Determinations For Patients With The Severe COVID-19Carla CANo ratings yet
- Sphingomonas KoreensisDocument11 pagesSphingomonas KoreensisSMIBA MedicinaNo ratings yet
- NEJM. COVID CHINA. 10.1056@NEJMoa2002032Document13 pagesNEJM. COVID CHINA. 10.1056@NEJMoa2002032Boris CabreraNo ratings yet
- Zimmerman 2019Document5 pagesZimmerman 2019Software InvestigaciónNo ratings yet
- Hemorrhagic Fevert in Hubei Province, The People's Republic of China: ClinicalDocument15 pagesHemorrhagic Fevert in Hubei Province, The People's Republic of China: ClinicalADC, desde 1936.No ratings yet
- Blood Cells and Plasma Proteins: Their State in NatureFrom EverandBlood Cells and Plasma Proteins: Their State in NatureJames L. TullisNo ratings yet
- Identification of Microbial Contaminants in Sinus Rinse Squeeze Bottles Used by Allergic Rhinitis PatientsDocument4 pagesIdentification of Microbial Contaminants in Sinus Rinse Squeeze Bottles Used by Allergic Rhinitis PatientsRiaNo ratings yet
- Shrivastava Bhanu, Shrivastava Vandana, Shrivastava ArchanaDocument3 pagesShrivastava Bhanu, Shrivastava Vandana, Shrivastava Archana420192420192No ratings yet
- Staphylococcinum - A Multicenter Clinical Verification StudyDocument7 pagesStaphylococcinum - A Multicenter Clinical Verification StudyRosi KunevaNo ratings yet
- Diagnostic Value of Bone Marrow Culture in Typhoid FeverDocument4 pagesDiagnostic Value of Bone Marrow Culture in Typhoid FevershafarinamauliaNo ratings yet
- Yield of Blood Cultures in Children Presenting With Febrile Illness in A Tertiary Care HospitalDocument5 pagesYield of Blood Cultures in Children Presenting With Febrile Illness in A Tertiary Care Hospitalfaraz.mirza1No ratings yet
- A Randomized Trial of Convalescent Plasma in Covid-19 Severe PneumoniaDocument11 pagesA Randomized Trial of Convalescent Plasma in Covid-19 Severe PneumoniaChintia GautamaNo ratings yet
- Study On Invasive Fungal Infections in Immunocompr PDFDocument7 pagesStudy On Invasive Fungal Infections in Immunocompr PDFMelody PardilloNo ratings yet
- Study On Invasive Fungal Infections in Immunocompr PDFDocument7 pagesStudy On Invasive Fungal Infections in Immunocompr PDFMelody PardilloNo ratings yet
- Separata InglesDocument6 pagesSeparata InglesaniuskadtNo ratings yet
- Case 18 - 2009Document9 pagesCase 18 - 2009Gustavo AngelesNo ratings yet
- Lectura 3seminario Micosis ProfundaDocument8 pagesLectura 3seminario Micosis ProfundaSebastian CastroNo ratings yet
- Relationship Between The ABO Blood Group and The COVID-19 SusceptibilityDocument18 pagesRelationship Between The ABO Blood Group and The COVID-19 SusceptibilitySaifuddin HaswareNo ratings yet
- Clinical Characteristics of CoronavirusDocument13 pagesClinical Characteristics of Coronavirusleonardo almeidaNo ratings yet
- Nejmoa 2002032Document13 pagesNejmoa 2002032Juan Antonio LópezNo ratings yet
- Correspondence To: Professor Changxin Shen Department of Blood TransfusionDocument13 pagesCorrespondence To: Professor Changxin Shen Department of Blood TransfusionMayur DadhaniyaNo ratings yet
- Antinuclear Antibodies by Indirect Immunofluorescence: Optimum Screening Dilution For Diagnosis of Systemic Lupus ErythematosusDocument5 pagesAntinuclear Antibodies by Indirect Immunofluorescence: Optimum Screening Dilution For Diagnosis of Systemic Lupus ErythematosusMargriet MayasinNo ratings yet
- 1 s2.0 S1684118219301331 MainDocument9 pages1 s2.0 S1684118219301331 Mainyuwengunawan7No ratings yet
- Clinical Characteristics of Coronavirus Disease 2019 in ChinaDocument13 pagesClinical Characteristics of Coronavirus Disease 2019 in ChinaAzuraa DarmawanNo ratings yet
- Clinical Characteristics of Coronavirus Disease 2019 in ChinaDocument13 pagesClinical Characteristics of Coronavirus Disease 2019 in ChinaprimaNo ratings yet
- Veterinary Internal Medicne - November 1996 - Dye - Bronchopulmonary Disease in The Cat Historical Physical RadiographicDocument16 pagesVeterinary Internal Medicne - November 1996 - Dye - Bronchopulmonary Disease in The Cat Historical Physical RadiographicRetno PamungkasNo ratings yet
- Babesia Venatorum Infection in Child, China: To The Editor: BabesiosisDocument2 pagesBabesia Venatorum Infection in Child, China: To The Editor: BabesiosisMark ReinhardtNo ratings yet
- 10) Blood Culture Contaminants - S.dawsonDocument10 pages10) Blood Culture Contaminants - S.dawsonimaguestuserNo ratings yet
- Covid 19Document10 pagesCovid 19MonicaNo ratings yet
- Detection of Babesia RNA and DNA in Whole Blood Samples From US Blood DonationsDocument12 pagesDetection of Babesia RNA and DNA in Whole Blood Samples From US Blood DonationsEnrique Salvador Padial RamosNo ratings yet
- Clinical Research & BioethicsDocument4 pagesClinical Research & BioethicsNallagondla ThulasiramNo ratings yet
- Relationship Between The ABO Blood Group and The COVID-19 SusceptibilityDocument18 pagesRelationship Between The ABO Blood Group and The COVID-19 SusceptibilityVidinikusumaNo ratings yet
- Typhoid Fever: Accuracy in Laboratory Diagnosis by Widal Test and Blood Culture TechniquesDocument3 pagesTyphoid Fever: Accuracy in Laboratory Diagnosis by Widal Test and Blood Culture TechniquesRD ComputersNo ratings yet
- Free Download A Familial Cluster of Pneumonia Associated With The 2019 Novel Coronavirus Indicating Person To Person Transmission A Study of A Family Cluster Jasper Fuk Woo Chan Full Chapter PDFDocument33 pagesFree Download A Familial Cluster of Pneumonia Associated With The 2019 Novel Coronavirus Indicating Person To Person Transmission A Study of A Family Cluster Jasper Fuk Woo Chan Full Chapter PDFdavid.peterson448100% (23)
- Bookmass 2296Document33 pagesBookmass 2296david.brown752No ratings yet
- Safety and Activity of The Immune Modulator HE2000 On The Incidence of Tuberculosis and Other Opportunistic Infections in AIDS PatientsDocument3 pagesSafety and Activity of The Immune Modulator HE2000 On The Incidence of Tuberculosis and Other Opportunistic Infections in AIDS PatientsJosueNo ratings yet
- Author Proof Copy Not F or Publica TionDocument4 pagesAuthor Proof Copy Not F or Publica TionYona MbalibulhaNo ratings yet
- Homewp Contentuploads201708jo50 Ja03 PDFDocument8 pagesHomewp Contentuploads201708jo50 Ja03 PDFRamiel ChristopherNo ratings yet
- Posters: A Sample of 156 of 232 Nurses Answered An Anonymous QuestionDocument7 pagesPosters: A Sample of 156 of 232 Nurses Answered An Anonymous QuestionFiras DrNo ratings yet
- Medmicro 38 6 391Document4 pagesMedmicro 38 6 391Annisa YohanesNo ratings yet
- Predicting Sepsis Severity at First Clinical Presentation: The Role of Endotypes and Mechanistic SignaturesDocument15 pagesPredicting Sepsis Severity at First Clinical Presentation: The Role of Endotypes and Mechanistic Signaturesbrhpcn2rrfNo ratings yet
- A New Coronavirus Associated With Human Respiratory Disease in ChinaDocument20 pagesA New Coronavirus Associated With Human Respiratory Disease in ChinaAbraham Guerra OspinoNo ratings yet
- Two Case Reports of Successful Treatment of Cholestasis With Steroids in Patients With PFIC-2Document9 pagesTwo Case Reports of Successful Treatment of Cholestasis With Steroids in Patients With PFIC-2AstiaNingrumSanjayaNo ratings yet
- 5 Pernpasan Bagian BawahDocument4 pages5 Pernpasan Bagian BawahWita Citra DewiNo ratings yet
- Enzymology in the Practice of Laboratory Medicine: Proceedings of a Continuation Course Held at the University of Minnesota, Minneapolis, Minnesota, 10-12 May 1972From EverandEnzymology in the Practice of Laboratory Medicine: Proceedings of a Continuation Course Held at the University of Minnesota, Minneapolis, Minnesota, 10-12 May 1972Philip BlumeNo ratings yet
- SM, Journal Manager, 1394531387Document4 pagesSM, Journal Manager, 1394531387ali.malik16778No ratings yet
- Isolation and Characterization of Pathogenic Pseudomonas Species From Urinary Tract Infection (Uti) and Wounds in Saudi Arabia at Makkah RegionDocument6 pagesIsolation and Characterization of Pathogenic Pseudomonas Species From Urinary Tract Infection (Uti) and Wounds in Saudi Arabia at Makkah RegionIJAR JOURNALNo ratings yet
- Blood Culture-Negative EndocarditisDocument7 pagesBlood Culture-Negative EndocarditisIkhsan Amadea9969No ratings yet
- Diagnosis and Testing in Bronchiolitis: A Systematic ReviewDocument8 pagesDiagnosis and Testing in Bronchiolitis: A Systematic ReviewKathy JunesNo ratings yet
- Adenosine Deaminase Level in Drug Resistant TuberculosisDocument9 pagesAdenosine Deaminase Level in Drug Resistant TuberculosisIJAR JOURNALNo ratings yet
- IDR 334161 Comparison of Clinical Characteristics and Outcomes BetweenDocument15 pagesIDR 334161 Comparison of Clinical Characteristics and Outcomes BetweenWen GonzalezNo ratings yet
- Cel Tumorales Mostoles 2008-CytopathologyDocument4 pagesCel Tumorales Mostoles 2008-CytopathologygemaNo ratings yet
- Herbal Medicine For Treatment of Children Diagnosed With COVID-19Document5 pagesHerbal Medicine For Treatment of Children Diagnosed With COVID-19wiwiNo ratings yet
- Dwnload Full Microbiology An Introduction 11th Edition Tortora Test Bank PDFDocument36 pagesDwnload Full Microbiology An Introduction 11th Edition Tortora Test Bank PDFgambolrapinous.ggqcdr100% (6)
- VoipDocument4 pagesVoipVinod MalikNo ratings yet
- Grouting in Difficult DamDocument68 pagesGrouting in Difficult DamTam Eng Sun67% (3)
- Software Project Management (Unit 9) PDFDocument56 pagesSoftware Project Management (Unit 9) PDFIshan TimilsinaNo ratings yet
- ZRBF's MEAL FrameworkJuly2016Document31 pagesZRBF's MEAL FrameworkJuly2016Shiela MagnoNo ratings yet
- IIML - IPMX - Ankit - ANKITDocument1 pageIIML - IPMX - Ankit - ANKITGurkirat BediNo ratings yet
- Class 9 Science TamilMediumDocument312 pagesClass 9 Science TamilMediumsimpletontsNo ratings yet
- Scope2 PDFDocument2 pagesScope2 PDFGregorNo ratings yet
- Template - Post Implementation ReviewDocument14 pagesTemplate - Post Implementation ReviewGryswolf100% (4)
- T2 E 1636 Year 4 Reading Assessment Reading BookletDocument10 pagesT2 E 1636 Year 4 Reading Assessment Reading BookletStanley TioNo ratings yet
- VDZ 3 5 En-Bypass SystemsDocument22 pagesVDZ 3 5 En-Bypass SystemsAndreea Ștefura100% (3)
- Fisiologi Sistem Pencernaan: Kristanti, DRDocument64 pagesFisiologi Sistem Pencernaan: Kristanti, DRFeny Maharani100% (1)
- TOG Online SBA Resource, Vol. 20 Issue 2Document6 pagesTOG Online SBA Resource, Vol. 20 Issue 2FA KhanNo ratings yet
- Specification For Carbon Structural Steel: SA-36 /SA-36MDocument7 pagesSpecification For Carbon Structural Steel: SA-36 /SA-36MBowo Edhi Wibowo100% (2)
- Coasts Knowledge OrganiserDocument2 pagesCoasts Knowledge OrganiserAbdellahNo ratings yet
- 1.3 Understanding GriefDocument24 pages1.3 Understanding GriefDavid Danao Franco MendezNo ratings yet
- Prese Pentru DeseuriDocument42 pagesPrese Pentru DeseuriAndreea AlinaNo ratings yet
- DNA Profiling Student HandoutDocument9 pagesDNA Profiling Student HandoutNoah HolznerNo ratings yet
- 1.fundamentals of nutrition-BHMDocument47 pages1.fundamentals of nutrition-BHMBakhtawarNo ratings yet
- NCM 114 Care of Older AdultsDocument47 pagesNCM 114 Care of Older Adultsbrilliant dumayNo ratings yet
- Mattoc 160mm, Main Spring 40 Psi, IRT Pressure ComparisonDocument1 pageMattoc 160mm, Main Spring 40 Psi, IRT Pressure ComparisonFandy SugiartoNo ratings yet
- Dokumen - Tips - JCB 455zx Wheel Loader Service Repair Manual SN 2414602 and Up 1594977672 PDFDocument21 pagesDokumen - Tips - JCB 455zx Wheel Loader Service Repair Manual SN 2414602 and Up 1594977672 PDFهندسه الكنانيNo ratings yet
- Excel FormatDocument38 pagesExcel FormatSaad QureshiNo ratings yet
- Analytical Framework: This Guide Provides You With Explanations To Help You Work With The Analytical Framework TemplateDocument4 pagesAnalytical Framework: This Guide Provides You With Explanations To Help You Work With The Analytical Framework Templatemohammed mahfoudhNo ratings yet
- Irrigation ManagementDocument185 pagesIrrigation Managementaravind ragavanNo ratings yet
- Laboratory Manual For Acid/Base TitrationDocument27 pagesLaboratory Manual For Acid/Base TitrationamitNo ratings yet
- Mountain Dog Shoulder TrainingDocument11 pagesMountain Dog Shoulder TrainingÂdâm Jônês83% (6)
- Guide On PMA Per PED PDFDocument6 pagesGuide On PMA Per PED PDFJean-Noël LerouxNo ratings yet
- BIOL 3150 Lab Manual Labs 5-7Document10 pagesBIOL 3150 Lab Manual Labs 5-7arshiafathiNo ratings yet
- AlgapdfDocument22 pagesAlgapdfDaniel BahamondeNo ratings yet