Professional Documents
Culture Documents
Post2020 Sci-533 PDF
Post2020 Sci-533 PDF
Uploaded by
Anonymous kdBDppigE0 ratings0% found this document useful (0 votes)
51 views1 pageOriginal Title
POST2020_SCI-533.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
51 views1 pagePost2020 Sci-533 PDF
Post2020 Sci-533 PDF
Uploaded by
Anonymous kdBDppigECopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
Functional and Radiographic Outcomes Following Minimally Invasive Bunion
Correction
Bradley M. Lamm, DPM, FACFAS, Jordan J. Ernst, DPM, MS, AACFAS, Travis M. Johnson, DPM, AACFAS, Nachika Ibekwe MS4
Foot and Ankle Deformity Correction Fellowship Program
Level of Evidence: Therapeutic, Level IV: Case Series
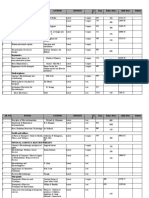
Angle Preoperative Postoperative Change p-value
Statement of Purpose Methodology Continued Mean Mean from Results Conclusions
baseline This is the first study to report
The touted advantages of percutaneous was performed to identify any 31 bunion correction procedures on 25 patients outcomes and radiographic angles
and minimally invasive surgery include complications including revision were reviewed including 22 right and 9 left feet, following MIS bunion correction with
surgery, hardware removal, and First 14.1o 2.7 4.8o 3.1 -9.3o <.05*
quicker operative times, decreased tissue 3 males and 28 females. Mean age 48.8, 12 the exclusive use of internal fixation
post-operative infection. A paired Intermetatarsal
trauma, less scaring, expedited month follow up. Radiographic findings are in and soft tissue balancing. The
rehabilitation, and fewer complications. samples t-test was used to compare Table 1. Average MOFQ score was 94/100. All advantages of MIS bunionectomy are
preoperative and postoperative Hallux Abductus 26.4o 7.8 5.2o 4.9 -21.2o <.05*
The aim of this study was to assess patients were satisfied with their decision to many, including reduced risk of
radiographic and functional outcomes in radiographic measurements with undergo surgery. All but two patients rated their avascular necrosis, reduced post-
p<.05 on two-tailed t-testing Tibial Sesamoid 4.2 1.5 2.1 1.2 -2.1 <.05*
patients after undergoing minimally 1st MTP motion as superior compared to their operative pain and edema,
considered statistically significant. Position
invasive bunion correction with screw pre-operative baseline. There were no reported decreased scar tissue, lack of need
fixation and percutaneous soft tissue Statistical analyses were performed complications of non-union, avascular necrosis, for tourniquet, faster operative times,
rebalancing. using Microsoft Excel. Table 1: Change from baseline in radiographic angle measurements pre- to post-operative minimally deep infection or osteomyelitis. ability to correct frontal plane
invasive HAV correction (n = 31)
Data are reported as mean standard deviation. *denotes statistical significance deformity, and preservation of joint
function. Our modified technique
combines osseous and soft tissue
Methodology & Procedures Surgical Technique Literature Review correction, addressing the complete
deformity as a whole. The findings of
31 Bunions were corrected in 25 patients First, a 10mm medial central first Bosch et al reported on 98 bunions treated with a this study are comparable to the
utilizing a minimally invasive approach metatarsal neck incision is made. The minimally invasive approach citing excellent available literature data.
between 2016 and 2018. The method of osteotomy is performed with 1.8mm wire radiographic outcomes at 8.75 years (2). Magnan
fixation was a single partially-threaded, perforation and osteotome. This and colleagues popularized the Bosch technique,
cannulated 4.0mm screw (Figure 1). minimizes soft tissue trauma and publishing average pre and postoperative IM
Medial capsular reefing was performed via preserves blood supply. Next an elevator angles of 13 and 7, hallux abductus angles 33 and References
a percutaneous approach. Full is inserted to the intramedullary canal to 16 (3). A systematic review of percutaneous 1. Chi TD, Davitt J, Younger A, Holt S, Sangeorzan BJ. Intra-
weightbearing was allowed in a post-op lateralize the capital fragment. A and inter-observer reliability of the distal metatarsal articular
osteotomies for HAV found an average angle in adult hallux valgus. Foot Ankle Int 2002: 23:722–726
shoe on day one. The average follow up percutaneous proximal to distal screw is improvement in the IM angle from 14.6 degrees to 2. Bösch P, Wanke S, Legenstein R. Hallux valgus correction
was12 months. Pre-operative and most then inserted across the osteotomy.0- by the method of Bösch: a new technique with a seven-to-ten-
8.6 degrees, hallux valgus angle from 29.6 to 13.2 year follow-up. Foot Ankle Clin. 2000;5(3):485-98, v-vi
recent post-operative digital weight bearing Vicryl suture is then percutaneously (4). Khosroabadi and Lamm published their 3. Magnan B, Samaila E, Viola G, Bartolozzi P. Minimally
radiographic measurements were made passed from the metatarsal neck incision invasive retrocapital osteotomy of the first metatarsal in hallux
modified percutaneous hallux abductovalgus valgus deformity. Oper Orthop Traumatol. 2008;20(1):89-96
with McKesson Radiology Suite including distally through the MTPJ capsule correction technique which utilized percutaneous 4. Bia A, Guerra-Pinto F, Pereira BS, et al. Percutaneous
the first IM angle, hallux abductus angle, across the joint, then passed back Osteotomies in Hallux Valgus: A Systematic Review. J Foot
screw and Steinman pin fixation that was later Ank Surg 2018: 57: 123-130
and sesamoid position (Table 1). The through the same exit hole proximally removed once the osteotomy healed (5). In this 5. Khosroabadi A, Lamm BM. Modified Percutaneous Hallux
distal metatarsal articular angle was not out the original medial neck incision and Abductovalgus Correction. J Foot Ankle Surg.
study we used internal fixation exclusively. Brogan 2016;55(6):1336-1342.
measured secondary due to its poor inter tied with the hallux rectus to reef the found significant improvement in MOFQ scores in 6. Brogan K, Voller T, Gee C. Third-generation minimally
and intra-observer reliability (1). medial first MTPJ capsule. A invasive correction of hallux valgus: technique and early
45 cases at 6 month follow up from MIS bunion outcomes. International Orthopedics. 2014: 38(10): 2115-212
Functional outcomes were measured with percutaneous release was typically correction (6). The MOxFQ has been validated for .7. Dawson J, Coffey J, Doll H, et al. A patient-based
a Manchester-Oxford Foot Questionnaire. performed of the lateral first MTPJ questionnaire to assess outcomes of foot surgery: validation
HAV and has shown to have better responsiveness
A Retrospective chart review (cont’d) capsule with a #64 Beaver blade.
in the context of surgery for hallux valgus. Qual Life Res.
than AOFAS scores (7). 2006;15(7):1211-22.
Figure 1: Preoperative radiograph, intraoperative surgical technique and post operative radiograph
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- First Aid For The Family Medicine Boards Third Edition 1st TheDocument61 pagesFirst Aid For The Family Medicine Boards Third Edition 1st Thejerry.wolff99198% (40)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Nur - 100 Session 2 - SemillaDocument6 pagesNur - 100 Session 2 - SemillaVon R Semilla100% (1)
- Acute AbdomenDocument58 pagesAcute AbdomenkharisaNo ratings yet
- Locking Plate Techniques For Fracture Stability: Jay D. Ryan, DPMDocument5 pagesLocking Plate Techniques For Fracture Stability: Jay D. Ryan, DPMAnonymous kdBDppigENo ratings yet
- Ptantar Anatomy: Tfie Skin Private SurgicalDocument9 pagesPtantar Anatomy: Tfie Skin Private SurgicalAnonymous kdBDppigENo ratings yet
- An Evidence Based Approach To Soft Tissue APPROXIMATION: A Review of Suture Selection For Optimal Skin ClosureDocument4 pagesAn Evidence Based Approach To Soft Tissue APPROXIMATION: A Review of Suture Selection For Optimal Skin ClosureAnonymous kdBDppigENo ratings yet
- Bouché2012 Chapter ChronicCompartmentSyndromeOfLe PDFDocument6 pagesBouché2012 Chapter ChronicCompartmentSyndromeOfLe PDFAnonymous kdBDppigENo ratings yet
- Evaluation of Outcomes in Patients Following Surgical Treatment of Chronic Exertional Compartment Syndrome in The LegDocument9 pagesEvaluation of Outcomes in Patients Following Surgical Treatment of Chronic Exertional Compartment Syndrome in The LegAnonymous kdBDppigENo ratings yet
- Talar Fractures: The Injury, The Management, and The AftermathDocument17 pagesTalar Fractures: The Injury, The Management, and The AftermathAnonymous kdBDppigENo ratings yet
- Intrinsicmuscleflapsfor Coverageofsmalldefectsin Thefoot: Grace Chuang CraigDocument14 pagesIntrinsicmuscleflapsfor Coverageofsmalldefectsin Thefoot: Grace Chuang CraigAnonymous kdBDppigENo ratings yet
- Open 4-Compartment Fasciotomy For Chronic Exertional Compartment Syndrome of The LegDocument11 pagesOpen 4-Compartment Fasciotomy For Chronic Exertional Compartment Syndrome of The LegAnonymous kdBDppigENo ratings yet
- TOI-) ND: Closi-) ReDocument8 pagesTOI-) ND: Closi-) ReAnonymous kdBDppigENo ratings yet
- Multidirectional Instability of The Ankle: Surgical ReconstructionDocument7 pagesMultidirectional Instability of The Ankle: Surgical ReconstructionAnonymous kdBDppigENo ratings yet
- Minimally Invasive Treatment of Displaced Intra-Articular Calcaneal FracturesDocument14 pagesMinimally Invasive Treatment of Displaced Intra-Articular Calcaneal FracturesAnonymous kdBDppigENo ratings yet
- Internal Fixation Podiatric: SurgeryDocument7 pagesInternal Fixation Podiatric: SurgeryAnonymous kdBDppigENo ratings yet
- Skin: Unique Anatomy: The IowerDocument3 pagesSkin: Unique Anatomy: The IowerAnonymous kdBDppigENo ratings yet
- Percutaneous Osteotomies in Pediatric Deformity Correction: Nickolas Nahm,, Louise Reid Boyce NicholsDocument16 pagesPercutaneous Osteotomies in Pediatric Deformity Correction: Nickolas Nahm,, Louise Reid Boyce NicholsAnonymous kdBDppigENo ratings yet
- ICD-10 PodiatryDocument25 pagesICD-10 PodiatryAnonymous kdBDppigENo ratings yet
- Revision: Scar TechniquesDocument4 pagesRevision: Scar TechniquesAnonymous kdBDppigENo ratings yet
- Bone Marrow Stimulation and Biological Adjuncts For Treatment of Osteochondral Lesions of The TalusDocument12 pagesBone Marrow Stimulation and Biological Adjuncts For Treatment of Osteochondral Lesions of The TalusAnonymous kdBDppigENo ratings yet
- Swanson: Flexible Hinge Toe ImplantDocument14 pagesSwanson: Flexible Hinge Toe ImplantAnonymous kdBDppigENo ratings yet
- Core Decompression in Foot and AnkleDocument9 pagesCore Decompression in Foot and AnkleAnonymous kdBDppigENo ratings yet
- Pathophysiology of Tendinopathy: Michael Girdwood, Sean Docking, Ebonie Rio, and Jill CookDocument22 pagesPathophysiology of Tendinopathy: Michael Girdwood, Sean Docking, Ebonie Rio, and Jill CookAnonymous kdBDppigENo ratings yet
- 1996 19Document5 pages1996 19Anonymous kdBDppigENo ratings yet
- Stress Modulation of Fracture Fixation Implants: Review ArticleDocument9 pagesStress Modulation of Fracture Fixation Implants: Review ArticleAnonymous kdBDppigENo ratings yet
- Piantar AND: 5I AnatomyDocument7 pagesPiantar AND: 5I AnatomyAnonymous kdBDppigENo ratings yet
- Wound: CtosureDocument8 pagesWound: CtosureAnonymous kdBDppigENo ratings yet
- Fijndamental FOR: Principles CT) Rrent TechniqtjesDocument4 pagesFijndamental FOR: Principles CT) Rrent TechniqtjesAnonymous kdBDppigENo ratings yet
- Morton Neuroma: Leslie Grujic and Christina KabbashDocument3 pagesMorton Neuroma: Leslie Grujic and Christina KabbashAnonymous kdBDppigENo ratings yet
- Skin Local: PlastiesDocument14 pagesSkin Local: PlastiesAnonymous kdBDppigENo ratings yet
- English ProjectDocument126 pagesEnglish ProjectShivam GuptaNo ratings yet
- ACS BookletDocument14 pagesACS Bookletmyat25No ratings yet
- Depression and Islam - Iblal Rakha and DR Menaz AkhtarDocument11 pagesDepression and Islam - Iblal Rakha and DR Menaz AkhtarIblal Rakha100% (3)
- Prince Price Alide Price Printer Sr. No Books Author Edition QT Y KinesiologyDocument9 pagesPrince Price Alide Price Printer Sr. No Books Author Edition QT Y KinesiologyNaveed AkhterNo ratings yet
- The Child With CancerDocument6 pagesThe Child With CancerWai SitNo ratings yet
- Obstructive JaundiceDocument29 pagesObstructive JaundiceBaraka SayoreNo ratings yet
- Aspecte Radiologice in SarcoidozaDocument67 pagesAspecte Radiologice in SarcoidozaBianca Balas MafteiNo ratings yet
- Leg and Feet Swelling Natural RemediesDocument4 pagesLeg and Feet Swelling Natural Remediesghica05100% (1)
- Rxprep 2019 Study Chart: ST ND RD TH THDocument5 pagesRxprep 2019 Study Chart: ST ND RD TH THYazan100% (2)
- Meningitis: Laguitao, Ayra B. LLANETA, Marissa Angeline BDocument12 pagesMeningitis: Laguitao, Ayra B. LLANETA, Marissa Angeline BAyra Batore Laguitao100% (1)
- NaraDocument4 pagesNaraLaila RatnalaNo ratings yet
- Homonymous HemianopiaDocument4 pagesHomonymous HemianopiaRA Libert Gatho Reza ValentineNo ratings yet
- Bhagandara NidanaDocument5 pagesBhagandara NidanaSachintha WijesiriwardhanaNo ratings yet
- Opportunistic Infections: Dr. Baldev S. PrajapatiDocument69 pagesOpportunistic Infections: Dr. Baldev S. PrajapatiZazzZaffaNo ratings yet
- Breast AwarenessDocument44 pagesBreast AwarenessLea Tabo MelchorNo ratings yet
- EKG Self Study GuideDocument40 pagesEKG Self Study GuideArgee AlonsabeNo ratings yet
- Efek Radiasi Dan Proteksi RadiasiDocument56 pagesEfek Radiasi Dan Proteksi RadiasiMargana SitumorangNo ratings yet
- Valori Contract An. 2023 - Paraclinic - 20.09.2023Document21 pagesValori Contract An. 2023 - Paraclinic - 20.09.2023Matteo si Sofia vlog'sNo ratings yet
- Consolidation Report Bo Noraina SurayaDocument3 pagesConsolidation Report Bo Noraina SurayaChris Tine ChiaNo ratings yet
- NCP Acute Pain Rhea FinalDocument1 pageNCP Acute Pain Rhea FinalSolsona Natl HS MaanantengNo ratings yet
- Medical AbbreviationsDocument3 pagesMedical AbbreviationsDONA, Randel John T.No ratings yet
- NTCC Srishti K 144Document16 pagesNTCC Srishti K 144srishti kohliNo ratings yet
- Evolution in Techniques For Endsocopic Brow Lift With Deep Temporal Fixation Only and Lower Blepharoplasty-Transconjunctival Fat RepositioningDocument16 pagesEvolution in Techniques For Endsocopic Brow Lift With Deep Temporal Fixation Only and Lower Blepharoplasty-Transconjunctival Fat RepositioningBFF BotoxNo ratings yet
- Prelim Activity 1 - Health TeachingsDocument2 pagesPrelim Activity 1 - Health TeachingsNICOLE MAGLAQUINo ratings yet
- Sars-Cov-2 (Causative Agent of Covid-19) Viral Rna Detected (+)Document1 pageSars-Cov-2 (Causative Agent of Covid-19) Viral Rna Detected (+)Dominica PalacioNo ratings yet
- Cala InjuriesDocument6 pagesCala InjuriesMunashe HogweNo ratings yet
- Av BlockDocument38 pagesAv BlockLanna Harumiya100% (1)