Professional Documents
Culture Documents
09a - ED Risk Assessment For COVID-19 4 - 6 - 2020 PDF
09a - ED Risk Assessment For COVID-19 4 - 6 - 2020 PDF
Uploaded by
Pepe UM0 ratings0% found this document useful (0 votes)
15 views1 pageOriginal Title
09a - ED Risk Assessment for COVID-19 4_6_2020.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
15 views1 page09a - ED Risk Assessment For COVID-19 4 - 6 - 2020 PDF
09a - ED Risk Assessment For COVID-19 4 - 6 - 2020 PDF
Uploaded by
Pepe UMCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
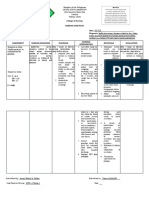
UW Medicine Emergency Department Risk Assessment Algorithm for COVID-19
Symptomatic COVID-19+ or PUI
Stable Vital Signs Abnormal Vital Signs
Without O2 Requirement and/or O2 Requirement
(≥94%) (<94%)
Increased Risk Moderate illness Critical illness
Low Risk
- Risk Factors or abnormal SPO2 ≥94% and SPO2 <94% and/or
-No Risk Factors and unstable vitals on 5L
physical exam stable vitals on ≤ 5L
normal physical by Nasal Cannula
by Nasal Cannula
exam -COVID-19 Test*
-Rapid -Rapid Influenza/RSV
-Rapid Influenza/RSV -Rapid Influenza/RSV, COVID
Influenza/RSV per per clinical judgement
and/or COVID-19 Test Labs, and COVID Imaging per
per clinical judgment*
clinical judgement
clinical judgement -COVID-19 Test
-COVID-19 Test
-COVID Labs
-COVID Labs
Considerable Risk -COVID Imaging
Consider Discharge* NO# Factors and/or YES -COVID Imaging
-10L O2 by face mask
with COVID-19 considerable Risk
Isolation
-Admit COVID-19 or intubation and
Factors for Progression
Instructions Hospitalist# Admit ICU#
to Severe Disease
* See UW med ID testing recommendations. Consider COVID-19 testing and/or special discharge assistance for pregnant women, people living homeless
or in congregant facilities, for those with known positive exposures, and healthcare workers. # for confirmed COVID-19 +, consider ID consult for
hydroxychloroquine for patients with hypoxia or patients with risk factors without hypoxia.
Risk Factors COVID labs COVID Imaging Risk Factors for Progression to
Severe Disease
Age ≥ 60 CBC with diff Consider the following:
D-Dimer > 1.0 ug/ml
Comorbidities: HTN, CVD,
CMP 1.Portable Chest Xray CPK > 2x ULN
cardiomyopathy, pulmonary
disease, Renal disease, DM, CRP 2.POC Lung Ultrasound CRP > 100, LDH >245
transplant.
Immune deficiency: immune
LDH 3. Chest CT only if Hepatic Transaminase elevation
modulators, above imaging is New Creatinine elevation
DIC Panel (PT, aPTT,
immunosuppressive inconclusive or
medications including fibrinogen, D-dimer) Troponin elevation
considering alternative
corticosteroid treatment at the
Cardiac: ECG, CPK, diagnosis (trauma, PE, Abs lymphocyte count <0.8
equivalent of 20 mg of oral
prednisone or more daily, Troponin, and BNP dissection, ACS)
Lactate > 4
detectable HIV VL or CD4
count<200 cells/mm3) Venous lactate Extensive bilateral and/or
worsening pulmonary infiltrates
Altered mental status (GCS < 15) With pneumonia =
blood cultures Exertional SPO2 <90% during one-
Evidence of Lower Respiratory minute walk in place or unable to
Tract Infection complete.
Adapted from: CDC, WHO, UW Medicine guidelines, Cornell ED COVID guide, MGH ICU guide for COVID-19, and available literature.
1. CDC coronavirus clinical guidelines: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html
2. World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. March 2020
3. Zhou F, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China…The Lancet. 2020 Mar 11.
Updated March 31, 2020(Version 2.0)
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Eliminasi Meliputi Informasi / Riwayat Pasien Pemeriksaan - Pola BAB, BAKDocument7 pagesEliminasi Meliputi Informasi / Riwayat Pasien Pemeriksaan - Pola BAB, BAKNareswari KenitenNo ratings yet
- Vital Signs: Nursing Assessment Techniques ModuleDocument24 pagesVital Signs: Nursing Assessment Techniques ModuleSHELLAH MARIE MAMAWAGNo ratings yet
- CoopMED Health Insurance Doctor Examination FormDocument2 pagesCoopMED Health Insurance Doctor Examination FormKammieNo ratings yet
- Alison Martin A PDFDocument4 pagesAlison Martin A PDFtom riddleNo ratings yet
- Tonsil Cancer: Cedars-Sinai ResourceDocument4 pagesTonsil Cancer: Cedars-Sinai ResourceSiRa DiktaraNo ratings yet
- Obstetric EmergenciesDocument96 pagesObstetric Emergenciessembakarani thevagumaranNo ratings yet
- Fever With Rash SeminarDocument98 pagesFever With Rash SeminarSYAZRIANA SUHAIMINo ratings yet
- Aphasia: NIDCD Fact SheetDocument4 pagesAphasia: NIDCD Fact SheetscorpionmaironNo ratings yet
- Special Forms of PeritonitisDocument10 pagesSpecial Forms of PeritonitisGx NavinNo ratings yet
- Pediatric Community Acquired PneumoniaDocument9 pagesPediatric Community Acquired PneumoniaJopaii TanakaNo ratings yet
- Monthly Census of Chemotherapy Administration-Surgery-1Document13 pagesMonthly Census of Chemotherapy Administration-Surgery-1myvi317No ratings yet
- Superior Orbital Fissure Aka Tolosa Hunt SyndromeDocument5 pagesSuperior Orbital Fissure Aka Tolosa Hunt SyndromeKalpana GunasekarNo ratings yet
- Lesson 2 3 Feedback DiaryDocument5 pagesLesson 2 3 Feedback DiaryDon Aldrich SantosNo ratings yet
- Webinar Famiy Doctors 1 - 10 - 2020Document62 pagesWebinar Famiy Doctors 1 - 10 - 2020NoaEfratBen-BaruchNo ratings yet
- Makalah Bahasa Inggris Unit 6Document10 pagesMakalah Bahasa Inggris Unit 6Nadia NadNo ratings yet
- FNCPDocument1 pageFNCPThunderNo ratings yet
- AcneDocument24 pagesAcnefarmasi_hm100% (2)
- Bipolar DisorderDocument9 pagesBipolar DisorderAnqelicus AsacinevaNo ratings yet
- Nursing 202: Module B Cardiovascular System AlterationsDocument121 pagesNursing 202: Module B Cardiovascular System AlterationssenthilmnurseNo ratings yet
- NCPDocument3 pagesNCPJerome Vergel RubianesNo ratings yet
- Quercetin A Promising Treatment For The Common Cold 2329 8731.1000111Document3 pagesQuercetin A Promising Treatment For The Common Cold 2329 8731.1000111Sameer SamouaNo ratings yet
- 2-Constipation and CRCDocument36 pages2-Constipation and CRCAbdulrahman NanakaliNo ratings yet
- ALS Fact SheetDocument4 pagesALS Fact SheetGovar Miqdad GardiNo ratings yet
- Tuckey Et Al 2019 Efficacy of Acupuncture in Treating Scars Following Tissue TraumaDocument12 pagesTuckey Et Al 2019 Efficacy of Acupuncture in Treating Scars Following Tissue TraumaosmarcruzNo ratings yet
- Indication and Contraindication of ExodontiaDocument9 pagesIndication and Contraindication of ExodontiaSagad AlaaNo ratings yet
- Palileo NCPDocument5 pagesPalileo NCPAeron PalileoNo ratings yet
- Sleep Medicine ReviewsDocument16 pagesSleep Medicine ReviewsCami ElenaNo ratings yet
- Schizophrenia - Practice Essentials, Background, PathophysiologyDocument10 pagesSchizophrenia - Practice Essentials, Background, PathophysiologydilaNo ratings yet
- Interpretation: A06 - Raj Hospital - Cash (Cghs - 20) Main Road Ranchi Jharkhand 834001Document4 pagesInterpretation: A06 - Raj Hospital - Cash (Cghs - 20) Main Road Ranchi Jharkhand 834001AlokNo ratings yet
- Disruptive Mood Dysregulation DisorderDocument13 pagesDisruptive Mood Dysregulation DisorderNyoman SuryaNo ratings yet