Professional Documents
Culture Documents
Mucin-Containing Rectal Carcinomas: Overview of Unique Clinical and Imaging Features
Uploaded by
Lu ChoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mucin-Containing Rectal Carcinomas: Overview of Unique Clinical and Imaging Features
Uploaded by
Lu ChoCopyright:
Available Formats
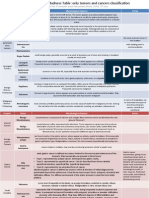
G a s t r o i n t e s t i n a l I m a g i n g • R ev i ew
Wnorowski et al.
Imaging Features of Mucin-Containing Rectal Carcinomas
Gastrointestinal Imaging
Review
Mucin-Containing Rectal
FOCUS ON:
Carcinomas: Overview of Unique
Clinical and Imaging Features
Amelia M. Wnorowski1 OBJECTIVE. The purpose of this study is to review the unique clinical and imaging fea-
Christine O. Menias 2 tures of mucin-containing rectal carcinomas.
Perry J. Pickhardt 3 CONCLUSION. Mucinous rectal carcinoma is an uncommon tumor subtype with a
David H. Kim 3 worse prognosis. At MRI, it is marked by T2-hyperintense extracellular mucin. Difficulty in
Amy K. Hara2 distinguishing cellular from acellular mucin and persistent tumor bulk can cause errors at re-
staging. Signet ring cell carcinoma contains intracellular mucin. The classic imaging appear-
Meghan G. Lubner 3
ance is rectal linitis plastica. Both tumor subtypes have a unique metastatic pattern.
Wnorowski AM, Menias CO, Pickhardt PJ, Kim DH,
ucin-containing rectal tumors was first described in 1923 [6] and is defined
M
Hara AK, Lubner MG
can be classified into three dis- by the World Health Organization as great-
American Journal of Roentgenology
tinct types, two of which are un- er than 50% tumor composition by extra-
common primary subtypes of cellular mucin [1]. At histopathologic anal-
rectal carcinoma and one of which is encoun- ysis, these tumors show extracellular mucin
tered as a response to treatment. We consider pools surrounded by neoplastic epithelial
mucinous carcinoma and signet ring cell car- cells [7]. The mucinous composition results
cinoma, two separate histologic subtypes of in a classic radiologic and histologic appear-
rectal cancer, as the first two types [1]. Muci- ance. Colorectal mucinous carcinoma most
Keywords: MRI, mucinous rectal carcinoma, rectal nous carcinoma contains extracellular mucin commonly affects the right colon [8]. It less
cancer, signet ring cell carcinoma
at the time of diagnosis, before any treatment, commonly occurs in the rectum, with an in-
doi.org/10.2214/AJR.18.20864 whereas signet ring cell carcinoma contains cidence of 0.8 cases per 100,000 population
intracytoplasmic mucin. Mucinous and signet according to the U.S. Surveillance, Epide-
Received November 7, 2018; accepted after revision ring cell carcinomas are considered distinct miology, and End Results database [1], ac-
February 10, 2019. histologic entities by the World Health Orga- counting for 10% of all rectal tumors [9]. It is
P. J. Pickhardt is an adviser to Bracco and a shareholder
nization [1], though signet ring cells can also associated with a worse prognosis than non-
in Elucent, SHINE, and Cellectar. D. Kim is a shareholder occur within mucinous carcinomas (i.e., mu- mucinous rectal adenocarcinoma. Recogni-
in Elucent and Cellectar. A. K. Hara has a licensure cinous carcinoma with signet ring cells) [2]. tion of this tumor subtype has important pa-
agreement with GE Healthcare for CT colonography This is considered separate from true signet tient care implications in a multidisciplinary
software. M. G. Lubner has received prior grant funding
ring cell carcinoma, which does not contain care setting [10].
to her institution from Philips and Ethicon.
extracellular mucin [2]. The third type of mu- Mucinous rectal carcinoma is associat-
Based on a presentation at the Radiological Society of cin-containing rectal tumor encompasses tu- ed with a unique genetic pattern, suggest-
North America 2017 annual meeting, Chicago, IL. mors that are originally nonmucinous but de- ing that this histologic type reflects a distinct
1
velop acellular mucin pools as a response to pathologic entity [11]. It more commonly has
Department of Radiology, University of Maryland School
therapy. The distinctions among these three several genetic aberrations that indicate ag-
of Medicine, 22 S Greene St, Baltimore, MD 21201.
Address correspondence to A. M. Wnorowski types of mucin-containing rectal tumors are gressiveness and therapy resistance, includ-
(AmeliaWnorowski@umm.edu). important because they have varied imaging ing BRAF and KRAS mutations and MUC-2
appearances and carry varied prognoses. Sig- overexpression [10]. These tumors also more
net ring cell carcinoma carries the worst commonly show microsatellite instability
2
Department of Radiology, Mayo Clinic Arizona, Phoenix, AZ.
3
Department of Radiology, University of Wisconsin
prognosis [3], whereas mucin production as a (MSI), which is caused by a defect in DNA
School of Medicine and Public Health, Madison, WI. response to neoadjuvant chemoradiation is mismatch repair. Colonic tumors with MSI
considered a good prognostic sign [4, 5]. are associated with better prognosis, even af-
AJR 2019; 213:1–9 ter adjusting for tumor stage [12]. The prog-
0361–803X/19/2131–1
Mucinous Rectal Carcinoma nostic significance of MSI in rectal cancer is
Mucinous rectal carcinoma is a distinct less well studied, but MSI in rectal cancers
© American Roentgen Ray Society histopathologic subtype of rectal cancer; it has been linked to a poorer prognosis, unlike
AJR:213, July 2019 1
Wnorowski et al.
its colonic counterpart [13]. In one recent The genetic basis of signet ring cell histo- duced mucinous change had significantly
study of over 5000 patients with locally ad- logic subtype has been better studied in gas- greater 2-year recurrence-free survival than
vanced rectal cancer, MSI was independent- tric cancer than in colorectal cancer [22]. did tumors that were mucinous before treat-
ly associated with a reduction in pathologic Gastric signet ring cell carcinoma is associat- ment (91.2% vs 39.3%) [4].
complete response after neoadjuvant therapy ed with a mutation in the CDH-1 gene, which
[14]. Several studies have shown that rectal leads to E-cadherin deficiency, with germline Imaging Features
tumors with MSI are more often hereditary mutations predisposing patients to heredi- MRI
and related to Lynch syndrome, rather than tary gastric cancer [22]. Further research is Diagnosis of mucinous carcinoma at initial
sporadic [13, 15]. Additional tumor screen- required to identify potential genetic associ- biopsy is prone to sampling error, with mis-
ing and genetic counseling are important in ations specific to rectal signet ring cell car- classification in approximately 25% of cases
this patient subgroup. cinoma, especially in light of its increasing [28]. However, this tumor subtype has a clas-
The prognostic significance of mucinous incidence among young patients. Compared sic appearance at MRI, allowing the radiolo-
histologic type in the rectum was previously with colorectal adenocarcinoma, signet ring gist to diagnose it confidently and accurate-
debated. However, older studies often com- cell carcinoma is associated with varied ge- ly in almost all cases. Extracellular mucin
bined tumors that become mucinous after netic alterations, including MSI, oncogene is T2 hyperintense; thus, mucinous carcino-
chemoradiation with true mucinous carci- (KRAS and BRAF) and tumor suppressor mas have significantly higher T2-weighted
nomas, which are now being recognized as gene (p53 and p16) mutations, disruption of signal than do nonmucinous tumors [29]. Us-
separate entities with different prognoses. cell adhesion–related genes (E-cadherin and ing T2-weighted signal, MRI is 96–97% ac-
More recent studies have shown that, com- β-catenin), and higher expression of mucin- curate at predicting the mucinous histologic
pared with nonmucinous adenocarcinoma, related genes [2, 25]. It is hypothesized that type with sensitivities of 94–100% and spec-
mucinous carcinoma of the rectum is asso- decreased expression of the cell-cell adhesion ificities of 95–98% [30]. MRI is more accu-
ciated with a higher T category at diagnosis molecules may contribute to more aggressive rate than biopsy for the diagnosis of muci-
[11], greater risk of metachronous metastases tumor behavior through increased local and nous histologic subtype [19] and can predict
[16], and worse survival [17–19]. However, metastatic spread [2]. Several studies have histologic quantification of mucin [16]. MRI
the difference in survival between patients shown an association of signet ring cells with has excellent interobserver agreement [30–32]
American Journal of Roentgenology
with mucinous and nonmucinous rectal can- poor prognosis, even at minor (< 50%) tumor with rare false-positive cases due to conges-
cers may be decreasing as a result of modern composition of signet ring cells [2, 26]. tion, abscess, necrosis, or mural edema [30].
advances in imaging, surgical technique, and Furthermore, the presence of T2-hyperintense
neoadjuvant therapy [9]. Tumors With Posttreatment Mucin mucin within a tumor at pretherapy MRI has
Mucinous change can be induced as a re- been shown to be an independent biomarker
Signet Ring Cell Carcinoma sult of neoadjuvant therapy. At imaging, this for poor prognosis and poor therapy response
Signet ring cell carcinoma is a rare distinct is reflected by the development of mucin [19]. Thus, when T2-hyperintense signal is
histopathologic subtype of rectal cancer. It pools within a tumor that was not mucinous subjectively assessed as present in greater
can develop in other sites of the gastrointes- before therapy. The mucin pools induced by than 50% of tumor volume, radiologists can
tinal tract, most commonly the stomach, but therapy are usually acellular. This induced accurately diagnose mucinous rectal carcino-
does also account for 0.1–2.4% of all colorec- mucinous change is an indicator of treatment ma with important patient care implications.
tal tumors [20]. Signet ring cell carcinoma is response and is associated with better prog- Because of their overall decreased cellu-
defined by the World Health Organization as nosis [4, 27]. In one study, tumors with in- larity, mucinous tumors show less enhance-
a tumor with more than 50% of cells contain-
ing intracytoplasmic mucin [1]. At histopath-
ologic analysis, the intracellular mucin dis-
places the nuclei, resulting in a characteristic
signet ring appearance. It affects younger pa-
tients, is considered undifferentiated and high
grade, and carries a poor prognosis [20–22].
In fact, despite the overall stable incidence
of rectal cancer since 1980, the incidence of
rectal cancer in patients younger than 40 has
quadrupled in this period with an increased
risk of signet ring cell histologic subtype in
this young subgroup [22]. Rectal signet ring
cell carcinomas tend to be larger, later stage,
and lower in location than mucinous carcino-
mas and nonmucinous adenocarcinomas [23]. A B
They also grow in the submucosa, which can
Fig. 1—47-year-old man with mid rectal mucinous carcinoma.
lead to false-negative biopsy [24]. Deeper bi- A, Sagittal T2-weighted MR image shows T2-hyperintense mucinous tumor (arrows).
opsy or even surgical exploration may be re- B, Sagittal contrast-enhanced T1-weighted MR image shows heterogeneous and overall decreased
quired to make the diagnosis. enhancement of mass (arrow).
(Fig. 1 continues on next page)
2 AJR:213, July 2019
Imaging Features of Mucin-Containing Rectal Carcinomas
Fig. 1 (continued)—47-year-old man with mid rectal
mucinous carcinoma.
C, Axial DW image (left) and corresponding apparent
diffusion coefficient (ADC) map (right) show overall
intermediate-to-high signal throughout mass on DW
image, mostly reflecting T2 signal shine-through on
ADC map (arrow).
ment and diffusion restriction compared
with nonmucinous tumors (Fig. 1). On con-
trast-enhanced images, there is enhancement
of the cellular portions of the tumor with a
predominantly peripheral and heterogeneous
enhancement pattern [32]. At DWI, there
is lower signal on high-b-value images and
higher mean apparent diffusion coefficient
values than for nonmucinous tumors as a re-
sult of the lower cellular density in the mu-
cinous components [16, 33]. If a radiologist
relies heavily on the presence of diffusion re-
striction for tumor identification and assess-
ment of tumor extent in otherwise subtle cas-
es, the lack of diffusion restriction can be a A B
potential pitfall in interpretation.
American Journal of Roentgenology
Fig. 2—34-year-old man with signet ring cell carcinoma of rectum.
The appearance of signet ring cell carcino- A and B, Sagittal (A) and axial (B) T2-weighted MR images show long segment of infiltrative tumor (arrows, A
ma varies, but it is classically a scirrhous tu- and B). Length of involvement and soft-tissue infiltration of submucosa producing malignant target appearance
mor with a submucosal growth pattern and seen on axial image (B) are characteristic of rectal linitis plastica. Note mesorectal and pelvic side wall lymph
node metastases (arrowheads, B). Signet ring cell carcinoma has propensity for lymph node metastases.
is associated with linitis plastica of the rec-
tum. “Linitis plastica” is a term first used to
describe the macroscopic appearance of tu-
mors infiltrating the stomach and resembling
a leather bottle. The term was later applied to
any part of the gastrointestinal tract when in-
filtrative tumor and the associated desmoplas-
tic reaction cause thickening of the wall, rigid-
ity, and lack of distensibility [24, 34, 35]. At
MRI, linitis plastica is characterized by long-
segment thickening and a cross-sectional tar-
get or ring appearance on T2-weighted images
[20, 24, 34] (Fig. 2). The infiltrative and sub-
mucosal growth patterns cause long-segment
strictures without the typical shouldering as-
sociated with most colorectal tumors [24]. The
submucosal growth pattern leads to the imag-
ing appearance of the malignant target sign,
wherein the submucosa is replaced by soft- A B
tissue signal, rather than the signal of edema,
Fig. 3—59-year-old man with obstructing mucinous rectal carcinoma.
and sequentially and progressively enhances A and B, Coronal (A) and axial (B) contrast-enhanced CT images show large high rectal mass (arrows) causing
on the delayed phase contrast-enhanced imag- upstream obstruction. Central mucin is marked by low attenuation at CT.
es, similar to that reported in other scirrhous
tumors of the gastrointestinal tract [36]. have been few reports examining the appear- tion at CT (Fig. 3). Because of this, muci-
ance of mucinous rectal carcinomas at CT. nous colorectal tumors are overall more hy-
CT However, CT remains heavily used in many poattenuating than are nonmucinous tumors
Prior literature has focused primarily on institutions, especially for distant staging. [37, 38]. At CT, mucinous tumors also show
the imaging appearance of mucin at MRI be- Therefore, it is important to recognize fea- more heterogeneous enhancement with less
cause MRI is used more commonly in eval- tures at CT that can indicate the presence of enhancement of the solid tumor components
uation of the primary tumor. Overall, there a mucinous tumor. Mucin has low attenua- overall and more severe and eccentric wall
AJR:213, July 2019 3
Wnorowski et al.
thickening [37, 38]. Mucin acts as an ion-ex- is a recognized rare complication of chronic Metastasis
change resin, often leading to calcium depo- perianal fistula [46, 47]. This can be a diffi- Mucinous tumors from other sites can
sition in the primary tumor, as well as me- cult diagnosis because of its nonspecific pre- occasionally metastasize to the rectum and
tastases [39]. At CT, mucinous colorectal sentation, chronic symptoms, and misleading mimic a primary mucinous carcinoma. The
tumors show intratumoral calcification more physical examination findings. Cross-section- most common primary sites include the co-
frequently [37, 38]. In one series comparing al imaging has a low sensitivity because the lon, stomach, and ovaries. Peritoneal depos-
86 mucinous colorectal tumors to 105 non- appearance of a mucinous tumor overlaps its within the deep pelvis can involve the an-
mucinous tumors, calcifications were present with that of a perianal abscess. Heterogeneous terior rectal wall. In these cases, the mass
in 21% of the mucinous subtype compared internal enhancement of mucinous carcinoma will be primarily eccentrically located with
with only 5% of the nonmucinous subtype is a clue to differentiate the two entities be- possible growth into the rectal wall (Fig. 5).
[38]. The overall specificity of these findings cause an abscess will more commonly show Secondary linitis plastica of the rectum
is 87% if multiple features are present [38]. peripheral enhancement only [46, 48] (Fig. 4). due to metastatic disease is more common
Signet ring cell carcinoma is more likely
to be concentrically thickened, producing the
malignant target sign, and homogeneously en-
hancing on CT [37] and often shows significant
perirectal infiltration [40]. As in MRI, the di-
agnosis should be considered when CT shows
a long length of concentric thickening and a
target sign; the mean length of involvement
was 6 cm and the mean thickness was 2 cm in
one series [40]. The linitis plastica appearance
can mimic an inflammatory or ischemic pro-
cess [34, 40]. A high level of suspicion must
be maintained because neoplasm is often not
American Journal of Roentgenology
the primary consideration in young patients,
who are, unfortunately, more commonly af-
fected by signet ring cell carcinoma.
PET
Mucinous rectal carcinoma may show vari- A B
able FDG uptake at PET/CT or PET/MRI de-
Fig. 4—61-year-old man with Crohn disease and mucinous carcinoma arising in perianal fistula. Patient
pending on the degree of mucin content. There required seton placement for transsphincteric perianal fistula. Surveillance MRI showed increased size of
is a negative correlation between the amount ischiorectal fossa collection, prompting biopsy that confirmed invasive mucinous carcinoma.
of mucin present and FDG avidity [41]. There- A, Coronal T2-weighted MR image shows T2-hyperintense mucinous mass (arrows) arising in perianal fistula.
Asterisk marks skin drainage site.
fore, the utility of PET may be limited in tumors B, Axial contrast-enhanced T1-weighted MR image shows heterogeneous internal enhancement (arrows).
with a large amount of mucin. However, con-
trary to their mucinous counterpart in the colon,
mucinous rectal carcinomas are more likely to
be as FDG-avid as nonmucinous tumors [16,
42]. Several reports have suggested value in
dual-time-point PET to increase sensitivity [43,
44]. This is thought to be due to different enzy-
matic expression in malignant tumors that leads
to continued FDG accumulation and retention
over time compared with normal tissue, which
more readily clears FDG [45]. This results in
higher contrast of FDG uptake between malig-
nant and benign tissue over time, which could
be helpful in detecting mucinous tumors, which
are classically less conspicuous [43].
Rare Presentations of Mucinous A B
Perirectal Tumors Fig. 5—56-year-old man with mucinous metastasis to rectum from cecal primary tumor.
Complication of Perianal Fistula A, Sagittal T2-weighted MR image shows mass in rectovesical pouch (arrows). Mass is T2-hyperintense and
Tumors arising within a perianal fistu- appears eccentric along anterior rectal wall, which suggests its cause as metastatic deposit rather than
primary rectal tumor.
la may be either squamous cell carcinomas B, Coronal contrast-enhanced CT image shows T4a mucinous cecal tumor (arrow) that was resected 2 years
or adenocarcinomas. Mucinous carcinoma earlier. Resection of pelvic mass confirmed metastatic mucinous carcinoma.
4 AJR:213, July 2019
Imaging Features of Mucin-Containing Rectal Carcinomas
than primary rectal signet ring cell carcino- surgery to maintain fecal continence. MRI one to three regional lymph nodes, and N2 as
ma [49]; however, the imaging findings are has been shown to be highly accurate in pre- involvement of four or more regional lymph
similar. Metastatic linitis plastica can oc- dicting the possibility of complete surgical nodes [54]. Nonregional lymph node involve-
cur as a result of direct invasion of the rec- resection [55]. The staging of mucin-contain- ment such as paraaortic adenopathy above
tum by bladder or prostate carcinoma or dis- ing rectal tumors is no different than that of the origin of the inferior mesenteric artery is
tant peritoneal, lymphatic, or hematogenous nonmucinous adenocarcinoma. T category is designated M1a. Mucinous lymph node me-
spread from a gastric signet ring cell carcino- assessed by greatest depth of invasion (Fig. tastases may be T2 hyperintense as well.
ma or breast cancer [34, 50–53]. Distinction 6). T1 tumors are those that grow through the
in these cases may be possible because of the muscularis mucosa and extend into the sub- Assessment of Treatment Response
patient’s history and presence of other meta- mucosa. T2 tumors grow through the sub- One of the most important prognostic fac-
static disease elsewhere, especially peritone- mucosa and extend into the muscularis pro- tors in rectal cancer is complete surgical re-
al carcinomatosis. pria. T3 tumors grow through the muscularis section at total mesorectal excision. Neo-
propria and into the mesorectum. Finally, T4 adjuvant chemoradiation is the standard of
Local Staging tumors extend through the mesorectum to care for locally advanced disease. It results
Local staging is best performed with MRI penetrate the visceral peritoneum (T4a) or in frequent downstaging and lower local re-
via the American Joint Committee on Can- adjacent organs or structures (T4b). currence rates after subsequent surgery. The
cer’s TNM system [54]. MRI staging allows N category is determined by regional nod- degree of tumor regression after neoadjuvant
determination of the depth of invasion and al involvement. N0 is defined as no region- therapy correlates with disease-free surviv-
whether the anal sphincter can be spared at al nodal involvement, N1 as involvement of al [56].
At restaging MRI, mucinous composition
should be noted [27]. This may reflect mu-
cinous change in an originally nonmucinous
tumor, an indicator of treatment response
and better prognosis [4, 27]. Mucin seen af-
ter neoadjuvant therapy is most commonly
American Journal of Roentgenology
acellular. Acellular mucin is not considered
residual tumor in the TNM category [57] and
has no effect on disease-free survival [58].
In tumors that are mucinous before treat-
ment, mucin persists despite neoadjuvant
therapy. Restaging MRI is less accurate for
these tumors because of the difficulty in dis-
tinguishing persistent cellular mucin (lack
of response) from acellular mucin (treatment
effect). These tumors will remain T2 hyper-
A B
intense regardless of treatment effect. In ad-
dition, DWI may not be helpful because muci-
nous carcinomas are commonly bright on the
apparent diffusion coefficient map both be-
fore and after treatment [16, 59]. Tumor het-
erogeneity can help distinguish cellular from
acellular mucin. Acellular mucin generally
has more homogeneous T2-weighted signal,
whereas cellular mucin tends to be more het-
erogeneous with areas of intermediate signal
and enhancement [27]. However, cellular and
acellular mucin can be difficult to differenti-
ate at MRI [5] and both are resected.
Mucinous rectal carcinomas are less like-
C D ly to decrease in tumor bulk as a response to
Fig. 6—Four patients with different mucinous rectal tumors. T2-hyperintense signal of each tumor reflects neoadjuvant therapy [5, 60]. This is due to
extracellular mucin. the persistence of acellular mucin and is true
A, 38-year-old man. Axial T2-weighted MR image shows category T2 mucinous low rectal tumor contained
within muscularis propria (arrow). Surgical resection confirmed T2 tumor.
even in cases of complete response [5]. Per-
B, 60-year-old man. Axial T2-weighted MR image shows T3 mucinous anorectal tumor with areas that extend sistent tumor bulk and difficulty differentiat-
through muscularis propria into mesorectal fat (arrows). ing cellular from acellular mucin can result
C, 57-year-old man. Axial T2-weighted MR image shows T4a mucinous mid rectal tumor that extends through in overstaging [5]. Because of the difficulty
mesorectal fat to involve anterior peritoneal reflection (arrow).
D, 45-year-old man. Axial T2-weighted MR image shows T4b mucinous mid rectal tumor (arrow) invading in distinguishing treatment effect and residu-
seminal vesicles (arrowheads). al disease, restaging MRI is more error prone
AJR:213, July 2019 5
Wnorowski et al.
for mucinous carcinoma than for nonmuci-
nous tumors (Fig. 7). In one study by Allen et
al. [5], accurate prediction of complete resec-
tion was more difficult for mucinous tumors
(82%) than nonmucinous tumors (94%). In
that same study, they found that acellular mu-
cin pools at the resection margin were a fre-
quent confounder and resulted in overstaging.
Similarly, in tumors that develop mucinous
change as a response to neoadjuvant therapy,
the development of acellular mucin pools can
result in erroneous overstaging [61]. Despite A
difficulties with restaging mucinous tumors,
MRI remains useful in this setting to delin-
eate areas of potential residual disease and to
assist in surgical planning.
Mucinous rectal carcinomas are less like-
ly to be downstaged with neoadjuvant ther-
apy, less likely to show pathologic complete
response, and more likely to have positive
resection margins [9, 17–19, 62, 63]. In one
large review of over 85,000 patients with rec-
tal cancer, mucinous and signet ring cell his-
tologic subtype were associated with higher
margin positivity with adjusted odds ratios B C
American Journal of Roentgenology
of 1.51 and 2.49, respectively [64]. In another Fig. 7—55-year-old man with mucinous rectal carcinoma with near-complete treatment response.
study of 88 patients with rectal cancer, mu- A, Axial contrast-enhanced CT image obtained before treatment shows large low rectal mucinous tumor (arrows).
Note low-attenuation mucin at CT.
cinous carcinomas were the only tumors to B, Axial T2-weighted restaging MR image obtained after neoadjuvant chemoradiation shows that mass extends into
show disease progression after neoadjuvant prostate (arrow) and abuts levator musculature (arrowheads).
therapy [60]. This poor response to neoadju- C, Axial DW image (top) and apparent diffusion coefficient map (bottom) show lack of significant diffusion restriction
in bulk of tumor (arrows). Despite persistence of large tumor bulk at imaging, pathologic examination at pelvic
vant therapy is thought to be due to the low- exenteration showed near-complete treatment response with large amount of acellular mucin and rare tumor cells.
er microvascular density within mucinous tu-
mors [65]. Unfortunately, no imaging markers
have yet been shown to predict neoadjuvant
nonresponse in mucinous carcinoma [16].
Patients with rectal signet ring cell carci-
noma generally have a very poor prognosis
despite neoadjuvant therapy. However, sev-
eral studies have noted that some patients
are able to achieve complete response with
chemoradiation [34, 66]. In one series of pa-
tients with rectal signet ring cell carcinoma,
more extensive lymph node involvement (N
category) at pretreatment MRI was associ-
ated with a lack of treatment response [66].
Imaging of Local Recurrence
With optimal oncologic surgical technique A B
(i.e., total mesorectal excision) and neoadju- Fig. 8—64-year-old woman with locally recurrent mucinous rectal carcinoma.
vant chemoradiation, the 10-year cumulative A, Axial T2-weighted MR image at level of bladder and vaginal canal shows infiltrative disease recurrence in
frequency of local relapse is less than 10% pelvis with innumerable small T2-hyperintense tumor deposits (arrows) that replace vaginal and bladder walls.
B, Axial T2-weighted MR image inferior to image shown in panel A at level of urethra shows additional tumor
[67]. Most tumors recur in the first 3 years, deposits encasing urethra (arrow). Patient had history of primary rectal carcinoma with mucinous and signet
and over 50% of patients have additional met- ring cell features treated with abdominoperineal resection and adjuvant chemotherapy.
astatic disease at the time of recurrence [68].
The risk of local recurrence is greater with locally recurrent mucinous carcinoma is also at MRI or low attenuation at CT, similar to
higher original tumor category [68], positive T2 hyperintense (Fig. 8). Its appearance may that of fluid. Recurrence may be differentiated
resection margin [60], and spillage of cellu- mimic that of postoperative fluid collections by central or peripheral enhancement, FDG
lar mucin at the time of surgery [27]. At MRI, [68] because of their T2-hyperintense signal uptake (Fig. 9), or growth on sequential scans.
6 AJR:213, July 2019
Imaging Features of Mucin-Containing Rectal Carcinomas
through tissue planes and direct extension
into the peritoneal cavity [69] (Fig. 10). C to-
reductive surgery with hyperthermic intra-
peritoneal chemotherapy has shown promise
in the treatment of patients with colorectal
cancer metastatic to the peritoneal cavity
[76]. However, unfortunately, the signet ring
cell histologic subtype is associated with a
high rate of recurrence [77].
Conclusion
In conclusion, mucinous rectal carcinoma
and signet ring cell carcinoma are uncommon
histologic subtypes of rectal cancer that por-
A B tend a poor prognosis. Mucinous rectal car-
Fig. 9—56-year-old man with local recurrence of mucinous carcinoma 2 years after initial resection. cinoma is defined as greater than 50% tumor
A and B, Restaging contrast-enhanced CT (A) and PET (B) images obtained 2 years after initial surgery reveal composition by extracellular mucin. MRI has
low-attenuation collection in operative bed (arrows) with peripheral enhancement and FDG uptake. This was
confirmed to be mucinous local recurrence.
a high diagnostic accuracy, superior to that of
biopsy. The hallmark of the mucinous histo-
logic subtype is T2-hyperintense signal at
Metastatic Patterns Mucinous rectal and signet ring cell car- MRI. Mucin has low attenuation at CT and
Radiologists need to be aware of the unique cinomas have a higher frequency of both can be a cause of false-negative PET examina-
pattern and appearance of mucinous rectal lymph node and peritoneal metastases [69, tions. Restaging MRI is error prone because
carcinoma metastases. The mucinous histo- 75]. Additional rare metastatic sites, such as of difficulties in distinguishing residual cellu-
logic subtype is associated with an increased the heart, ovary, pancreas, and skin, are also lar from acellular mucin and persistent tumor
American Journal of Roentgenology
risk of metachronous metastases and in- more common in mucinous and signet ring bulk despite potential treatment response. Tu-
creased number of metastatic sites [16, 69]. cell carcinomas. Signet ring cell carcinoma mors with extracellular mucin before thera-
Mucinous metastases usually have imaging in particular has a very high rate of lym- py—that is, true mucinous carcinomas—must
features similar to those of the primary tu- phatic spread. Metastatic disease to the peri- be distinguished from nonmucinous tumors
mor with T2-hyperintense signal at MRI. Im- toneal cavity portends a very poor progno- that develop acellular mucin only as response
portantly, PET may be limited when there are sis. The frequencies of peritoneal spread for to therapy, which is a good prognostic sign.
large amounts of mucin in metastatic lesions, nonmucinous adenocarcinomas, mucinous Signet ring cell carcinoma is diagnosed patho-
and this can lead to false-negative results [70– carcinomas, and signet ring cell carcinomas logically by the presence of intracellular mu-
72]. A high index of suspicion, careful corre- were 20.1%, 48.2%, and 51.2%, respectively, cin. The classic imaging appearance of this
lation with CT or MR images, and lower stan- in one series [69]. The increased frequency subtype reflects its scirrhous morphologic fea-
dardized uptake value cutoffs may increase of peritoneal dissemination in mucinous tu- tures and submucosal growth pattern, giving
the sensitivity of PET in this setting [73]. mors is thought to be due to mucin dissection rise to rectal linitis plastica. The metastatic
In a study of close to 6000 autopsies of pa-
tients with colorectal tumors, compared with
patients with nonmucinous tumors, patients
with mucinous and signet ring cell carcino-
mas more commonly had metastatic disease
(27.6%, 33.9%, and 61.2%, respectively) and
were more likely to have multiple metastatic
sites (49.9%, 58.6%, and 70.7%, respectively)
[69]. Although mucinous and signet ring cell
carcinomas metastasize to the liver less com-
monly than nonmucinous tumors [20, 69], mu-
cinous liver metastases have been shown to be
an independent marker of poor prognosis [74].
Compared with nonmucinous metastases, mu-
cinous liver metastases are more commonly
single, larger, and unilateral [74]. Because of A B
the T2-hyperintense signal of mucinous liver Fig. 10—38-year-old woman with mucinous and signet-ring cell rectal carcinoma.
metastases, they can be confused with cysts or A, Sagittal T2-weighted MR image shows T2-hyperintense rectal mass (arrows) that involves anterior peritoneal
hemangiomas. However, their enhancement reflection (arrowhead). At time of diagnosis, there was peritoneal carcinomatosis with ascites.
B, Coronal T2-weighted MR image shows bilateral heterogeneous T2-hyperintense ovarian masses (arrows),
pattern allows differentiation with very mild consistent with mucinous metastases to ovaries. Neoadjuvant chemotherapy followed by rectosigmoid resection,
and heterogeneous internal enhancement. hysterectomy, bilateral salpingo-oophorectomy, and omentectomy confirmed metastatic mucinous tumor.
AJR:213, July 2019 7
Wnorowski et al.
pattern of mucinous and signet ring cell car- 14. Hasan S, Renz P, Wegner RE, et al. Microsatellite colorectal carcinoma. Ann Surg Oncol 2015;
cinoma is unique with increased frequency of instability (MSI) as an independent predictor of 22:1226–1235
lymph node and peritoneal metastases. pathologic complete response (PCR) in locally 27. Patel UB, Blomqvist LK, Taylor F, et al. MRI after
advanced rectal cancer: a National Cancer Data- treatment of locally advanced rectal cancer: how
References base (NCDB) analysis. Ann Surg 2018 Sep 13 to report tumor response—the MERCURY expe-
1. [No authors listed.] WHO classification of tu- [Epub ahead of print] rience. AJR 2012; 199:[web]W486–W495
mours, 4th ed., vol. 3. WHO classification of tu- 15. de Rosa N, Rodriguez-Bigas MA, Chang GJ, et al. 28. Younes M, Katikaneni PR, Lechago J. The value
mours of the digestive system. In: Bosman FT, DNA mismatch repair deficiency in rectal cancer: of the preoperative mucosal biopsy in the diagno-
Carneiro F, Huban RH, Theise ND, eds. Paris, benchmarking its impact on prognosis, neoadju- sis of colorectal mucinous adenocarcinoma. Can-
France: World Health Organization, 2010 vant response prediction, and clinical cancer ge- cer 1993; 72:3588–3592
2. Börger ME, Gosens MJ, Jeuken JW, et al. Signet netics. J Clin Oncol 2016; 34:3039–3046 29. Imai Y, Kressel HY, Saul SH, et al. Colorectal tu-
ring cell differentiation in mucinous colorectal 16. Barbaro B, Leccisotti L, Vecchio FM, et al. The mors: an in vitro study of high-resolution MR im-
carcinoma. J Pathol 2007; 212:278–286 potential predictive value of MRI and PET-CT in aging. Radiology 1990; 177:695–701
3. Hyngstrom JR, Hu CY, Xing Y, et al. Clinicopath- mucinous and nonmucinous rectal cancer to iden- 30. Kim MJ, Park JS, Park SI, et al. Accuracy in dif-
ology and outcomes for mucinous and signet ring tify patients at high risk of metastatic disease. Br J ferentiation of mucinous and nonmucinous rectal
colorectal adenocarcinoma: analysis from the Na- Radiol 2017; 90:20150836 carcinoma on MR imaging. J Comput Assist To-
tional Cancer Data Base. Ann Surg Oncol 2012; 17. McCawley N, Clancy C, O’Neill BD, Deasy J, Mc- mogr 2003; 27:48–55
19:2814–2821 Namara DA, Burke JP. Mucinous rectal adenocar- 31. Kim MJ, Huh YM, Park YN, et al. Colorectal mu-
4. Nagtegaal I, Gaspar C, Marijnen C, Van De Velde cinoma is associated with a poor response to neo- cinous carcinoma: findings on MRI. J Comput As-
C, Fodde R, Van Krieken H. Morphological adjuvant chemoradiotherapy: a systematic review sist Tomogr 1999; 23:291–296
changes in tumour type after radiotherapy are ac- and meta-analysis. Dis Colon Rectum 2016; 32. Hussain SM, Outwater EK, Siegelman ES. Muci-
companied by changes in gene expression profile 59:1200–1208 nous versus nonmucinous rectal carcinomas: dif-
but not in clinical behaviour. J Pathol 2004; 18. Shin US, Yu CS, Kim JH, et al. Mucinous rectal ferentiation with MR imaging. Radiology 1999;
204:183–192 cancer: effectiveness of preoperative chemoradio- 213:79–85
5. Allen SD, Padhani AR, Dzik-Jurasz AS, Glynne- therapy and prognosis. Ann Surg Oncol 2011; 33. Nasu K, Kuroki Y, Minami M. Diffusion-
American Journal of Roentgenology
Jones R. Rectal carcinoma: MRI with histologic 18:2232–2239 weighted imaging findings of mucinous carci-
correlation before and after chemoradiation thera- 19. Yu SK, Chand M, Tait DM, Brown G. Magnetic noma arising in the ano-rectal region: compari-
py. AJR 2007; 188:442–451 resonance imaging defined mucinous rectal carci- son of apparent diffusion coefficient with that of
6. Parham D. Colloid carcinoma. Ann Surg 1923; noma is an independent imaging biomarker for tubular adenocarcinoma. Jpn J Radiol 2012;
77:90–105 poor prognosis and poor response to preoperative 30:120–127
7. Symonds DA, Vickery AL. Mucinous carcinoma chemoradiotherapy. Eur J Cancer 2014; 50:920– 34. Boustani J, Kim S, Lescut N, et al. Primary linitis
of the colon and rectum. Cancer 1976; 37:1891– 927 plastica of the rectum: focus on magnetic reso-
1900 20. Lee NK, Kim S, Kim HS, et al. Spectrum of mu- nance imaging patterns and treatment options.
8. Verhulst J, Ferdinande L, Demetter P, Ceelen W. cin-producing neoplastic conditions of the abdo- Am J Case Rep 2015; 16:581–585
Mucinous subtype as prognostic factor in colorec- men and pelvis: cross-sectional imaging evalua- 35. Laufman H, Saphir O. Primary linitis plastica
tal cancer: a systematic review and meta-analysis. tion. World J Gastroenterol 2011; 17:4757–4771 type of carcinoma of the colon. AMA Arch Surg
J Clin Pathol 2012; 65:381–388 21. Nagtegaal ID, Hugen N. The increasing relevance 1951; 62:79–91
9. Hugen N, van de Velde CJ, Bosch SL, et al. Mod- of tumour histology in determining oncological 36. Gollub MJ, Schwartz MB, Shia J. Scirrhous me-
ern treatment of rectal cancer closes the gap be- outcomes in colorectal cancer. Curr Colorectal tastases to the gastrointestinal tract at CT: the ma-
tween common adenocarcinoma and mucinous Cancer Rep 2015; 11:259–266 lignant target sign. AJR 2009; 192:936–940
carcinoma. Ann Surg Oncol 2015; 22:2669–2676 22. Tawadros PS, Paquette IM, Hanly AM, Mellgren 37. Li ZH, You DY, Gao DP, et al. Role of CT scan in
10. Hugen N, Brown G, Glynne-Jones R, de Wilt JH, AF, Rothenberger DA, Madoff RD. Adenocarci- differentiating the type of colorectal cancer.
Nagtegaal ID. Advances in the care of patients noma of the rectum in patients under age 40 is in- OncoTargets Ther 2017; 10:2297–2303
with mucinous colorectal cancer. Nat Rev Clin creasing: impact of signet-ring cell histology. Dis 38. Ko EY, Ha HK, Kim AY, et al. CT differentiation
Oncol 2016; 13:361–369 Colon Rectum 2015; 58:474–478 of mucinous and nonmucinous colorectal carci-
11. Mekenkamp LJ, Heesterbeek KJ, Koopman M, et 23. Chen JS, Hsieh PS, Hung SY, et al. Clinical sig- noma. AJR 2007; 188:785–791
al. Mucinous adenocarcinomas: poor prognosis in nificance of signet ring cell rectal carcinoma. Int J 39. Yu MH, Kim YJ, Park HS, Jung SI, Jeon HJ. Im-
metastatic colorectal cancer. Eur J Cancer 2012; Colorectal Dis 2004; 19:102–107 aging patterns of intratumoral calcification in the
48:501–509 24. Rudralingam V, Dobson MJ, Pitt M, Stewart DJ, abdominopelvic cavity. Korean J Radiol 2017;
12. Samowitz WS, Curtin K, Ma KN, et al. Microsat- Hearn A, Susnerwala S. MR imaging of linitis 18:323–335
ellite instability in sporadic colon cancer is asso- plastica of the rectum. AJR 2003; 181:428–430 40. Kim HJ, Ha HK, Cho KS, et al. CT features of
ciated with an improved prognosis at the popula- 25. Gopalan V, Smith RA, Ho YH, Lam AK. Signet- primary colorectal signet-ring cell carcinoma.
tion level. Cancer Epidemiol Biomarkers Prev ring cell carcinoma of colorectum: current per- J Comput Assist Tomogr 2001; 25:225–230
2001; 10:917–923 spectives and molecular biology. Int J Colorectal 41. Berger KL, Nicholson SA, Dehdashti F, Siegel
13. Samowitz WS, Curtin K, Wolff RK, Tripp SR, Dis 2011; 26:127–133 BA. FDG PET evaluation of mucinous neoplasms:
Caan BJ, Slattery ML. Microsatellite instability 26. Inamura K, Yamauchi M, Nishihara R, et al. Prog- correlation of FDG uptake with histopathologic
and survival in rectal cancer. Cancer Causes Con- nostic significance and molecular features of sig- features. AJR 2000; 174:1005–1008
trol 2009; 20:1763–1768 net-ring cell and mucinous components in 42. Dos Anjos DA, Habr-Gama A, Vailati BB, et al.
8 AJR:213, July 2019
Imaging Features of Mucin-Containing Rectal Carcinomas
18F-FDG uptake by rectal cancer is similar in mu- tumor invasion at thin-section MR in patients with cally advanced rectal cancer: results of the Ger-
cinous and nonmucinous histological subtypes. rectal cancer: results of the MERCURY study. man CAO/ARO/AIO-94 randomized phase III
Ann Nucl Med 2016; 30:513–517 Radiology 2007; 243:132–139 trial after a median follow-up of 11 years. J Clin
43. Basu S, Baghel NS. Value of delayed PET imaging 56. Patel UB, Taylor F, Blomqvist L, et al. Magnetic Oncol 2012; 30:1926–1933
in mucinous adenocarcinoma rectum: should this resonance imaging-detected tumor response for 68. Sinaei M, Swallow C, Milot L, Moghaddam PA,
be employed while evaluating mucinous tumors locally advanced rectal cancer predicts survival Smith A, Atri M. Patterns and signal intensity
with FDG-PET? Indian J Cancer 2011; 48:374– outcomes: MERCURY experience. J Clin Oncol characteristics of pelvic recurrence of rectal can-
375 2011; 29:3753–3760 cer at MR imaging. RadioGraphics 2013;
44. Basu S, Kembhavi S. Unusual isolated perineal 57. Engstrom PF, Arnoletti JP, Benson AB 3rd, et al; 33:E171–E187
recurrence in mucinous adenocarcinoma of the National Comprehensive Cancer Network. NCCN 69. Hugen N, van de Velde CJ, de Wilt JH, Nagtegaal
rectum after abdominoperineal resection: useful- Clinical Practice Guidelines in Oncology: rectal ID. Metastatic pattern in colorectal cancer is
ness of dual-time-point FDG PET in evaluating cancer. J Natl Compr Canc Netw 2009; 7:838–881 strongly influenced by histological subtype. Ann
mucinous tumors. Clin Nucl Med 2012; 37:989– 58. Shia J, McManus M, Guillem JG, et al. Signifi- Oncol 2014; 25:651–657
990 cance of acellular mucin pools in rectal carcinoma 70. Belcher E, Nicholson AG, Hansell DM, Goldstraw
45. Zhuang H, Pourdehnad M, Lambright ES, et al. after neoadjuvant chemoradiotherapy. Am J Surg P. Imaging characteristics of a mucinous colorec-
Dual time point 18F-FDG PET imaging for differ- Pathol 2011; 35:127–134 tal pulmonary metastasis. Ann Thorac Surg 2008;
entiating malignant from inflammatory processes. 59. Enkhbaatar NE, Inoue S, Yamamuro H, et al. MR 86:1698
J Nucl Med 2001; 42:1412–1417 imaging with apparent diffusion coefficient histo- 71. Whiteford MH, Whiteford HM, Yee LF, et al. Use-
46. Hama Y, Makita K, Yamana T, Dodanuki K. Mu- gram analysis: evaluation of locally advanced rec- fulness of FDG-PET scan in the assessment of
cinous adenocarcinoma arising from fistula in tal cancer after chemotherapy and radiation thera- suspected metastatic or recurrent adenocarcino-
ano: MRI findings. AJR 2006; 187:517–521 py. Radiology 2018; 288:129–137 ma of the colon and rectum. Dis Colon Rectum
47. Surabhi VR, Menias CO, Amer AM, et al. Tumors 60. Oberholzer K, Menig M, Kreft A, et al. Rectal 2000; 43:759–767; discussion, 767–770
and tumorlike conditions of the anal canal and peri- cancer: mucinous carcinoma on magnetic reso- 72. Sarikaya I, Bloomston M, Povoski SP, et al.
anal region: MR imaging findings. RadioGraphics nance imaging indicates poor response to neoad- FDG-PET scan in patients with clinically and/or
2016; 36:1339–1353 juvant chemoradiation. Int J Radiat Oncol Biol radiologically suspicious colorectal cancer recur-
American Journal of Roentgenology
48. Fujimoto H, Ikeda M, Shimofusa R, Terauchi M, Phys 2012; 82:842–848 rence but normal CEA. World J Surg Oncol 2007;
Eguchi M. Mucinous adenocarcinoma arising 61. Barbaro B, Fiorucci C, Tebala C, et al. Locally 5:64
from fistula-in-ano: findings on MRI. Eur Radiol advanced rectal cancer: MR imaging in prediction 73. Yang ZY, Hu SL, Shi W, Zhu BL, Xu JY, Zhang
2003; 13:2053–2054 of response after preoperative chemotherapy and YJ. The clinical value of fluorine-18 fluorodeoxy-
49. Barabino G, Miggino M, Cuilleron M, Abboud K, radiation therapy. Radiology 2009; 250:730–739 glucose positron emission tomography/computed
Phelip JM, Porcheron J. Rectal linitis. Surgery 62. Sengul N, Wexner SD, Woodhouse S, et al. Effects tomography in postoperative patients with gastro-
2013; 154:641–642 of radiotherapy on different histopathological intestinal mucinous adenocarcinoma. Nucl Med
50. Ha HK, Jee KR, Yu E, et al. CT features of meta- types of rectal carcinoma. Colorectal Dis 2006; Commun 2011; 32:1018–1025
static linitis plastica to the rectum in patients with 8:283–288 74. Lupinacci RM, Mello ES, Coelho FF, et al. Prog-
peritoneal carcinomatosis. AJR 2000; 174:463–466 63. Miyakita H, Sadahiro S, Ogimi T, et al. Mucinous nostic implication of mucinous histology in re-
51. Venturini F, Gambi V, Di Lernia S, et al. Linitis components assessed by magnetic resonance im- sected colorectal cancer liver metastases. Surgery
plastica of the rectum as a clinical presentation of aging in primary rectal cancer tissue before and 2014; 155:1062–1068
metastatic lobular carcinoma of the breast. J Clin after chemoradiotherapy and tumor response. Int 75. Nozoe T, Anai H, Nasu S, Sugimachi K. Clinico-
Oncol 2016; 34:e54–e56 J Colorectal Dis 2018; 33:1135–1138 pathological characteristics of mucinous carcino-
52. Dresen RC, Beets GH, Vliegen RF, Creytens DH, 64. Russell MC, You YN, Hu CY, et al. A novel risk- ma of the colon and rectum. J Surg Oncol 2000;
Beets-Tan RG. Linitis plastica of the rectum sec- adjusted nomogram for rectal cancer surgery out- 75:103–107
ondary to bladder carcinoma: a report of two cas- comes. JAMA Surg 2013; 148:769–777 76. Verwaal VJ, Bruin S, Boot H, van Slooten G, van
es and its MR features. Br J Radiol 2008; 65. Oberholzer K, Menig M, Pohlmann A, et al. Rec- Tinteren H. 8-year follow-up of randomized trial:
81:e249–e251 tal cancer: assessment of response to neoadjuvant cytoreduction and hyperthermic intraperitoneal
53. Katsinelos P, Papaziogas B, Chatzimavroudis G, chemoradiation by dynamic contrast-enhanced chemotherapy versus systemic chemotherapy in
et al. Secondary rectal linitis plastica as first man- MRI. J Magn Reson Imaging 2013; 38:119–126 patients with peritoneal carcinomatosis of
ifestation of urinary bladder carcinoma. Ann Gas- 66. Bratland A, Vetrhus T, Grøholt KK, Ree AH. Pre- colorectal cancer. Ann Surg Oncol 2008;
troenterol 2012; 25:173–175 operative radiotherapy in rectal signet-ring cell 15:2426–2432
54. Jessup JM, Goldberg RM, Asare EA, et al. Colon carcinoma: magnetic resonance imaging and 77. van Oudheusden TR, Braam HJ, Nienhuijs SW, et
and rectum. In: Amin MB, Edge S, Greene F, et treatment outcome—report of six cases. Acta On- al. Poor outcome after cytoreductive surgery and
al., eds. AJCC Cancer Staging Manual. Basel, col 2010; 49:42–49 HIPEC for colorectal peritoneal carcinomatosis
Switzerland: Springer Nature, 2017:251–274 67. Sauer R, Liersch T, Merkel S, et al. Preoperative with signet ring cell histology. J Surg Oncol 2015;
55. MERCURY Study Group. Extramural depth of versus postoperative chemoradiotherapy for lo- 111:237–242
AJR:213, July 2019 9
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Neoplasia ExamDocument9 pagesNeoplasia ExamYheng Gaosaii100% (1)
- Kanker Payudara: Dr. Suyatno SPB (K) Onk Divisi Bedah Onkologi Bagian Bedah FK Usu/Rs Ham MedanDocument72 pagesKanker Payudara: Dr. Suyatno SPB (K) Onk Divisi Bedah Onkologi Bagian Bedah FK Usu/Rs Ham Medandinda annisaNo ratings yet
- NeoplasiaDocument78 pagesNeoplasiageetikaNo ratings yet
- Monograph On Lung Cancer July14Document48 pagesMonograph On Lung Cancer July14PatNo ratings yet
- Apocrine Carcinoma of The BreastDocument18 pagesApocrine Carcinoma of The BreastOscar HalumNo ratings yet
- Abstract 2015 in Surgery PDFDocument281 pagesAbstract 2015 in Surgery PDFDrAmmar MagdyNo ratings yet
- EAU Guidelines On: Penile CancerDocument38 pagesEAU Guidelines On: Penile Cancerhypebeast dopeNo ratings yet
- ESGO-ESTRO-ESP Guidelines For The Management of Patients With Endometrial Carcinoma 2021Document31 pagesESGO-ESTRO-ESP Guidelines For The Management of Patients With Endometrial Carcinoma 2021HanKethyanethNo ratings yet
- Clasificación de Lesiones Odontogenicas OMS 2017Document18 pagesClasificación de Lesiones Odontogenicas OMS 2017Yarith Pérez TrejoNo ratings yet
- Follicular Proliferative Lesion Arising in Struma Ovarii: Min Jee Park Min A Kim Mi Kyung Shin Hye Sook MinDocument5 pagesFollicular Proliferative Lesion Arising in Struma Ovarii: Min Jee Park Min A Kim Mi Kyung Shin Hye Sook MinRebecca Agustine KristianNo ratings yet
- Uterine Cancer Pa Tho PhysiologyDocument17 pagesUterine Cancer Pa Tho PhysiologyJeneva L. Lauzon100% (2)
- Oncology CasesDocument96 pagesOncology CasesPrutha Vaidya100% (1)
- Tumori Testisa PDFDocument14 pagesTumori Testisa PDFVuk MilutinovićNo ratings yet
- Neoplasm 20&20 Metabolic 20 DiseasesDocument30 pagesNeoplasm 20&20 Metabolic 20 DiseasesSaraNo ratings yet
- Rosen's Breast Pathology IntroductionDocument18 pagesRosen's Breast Pathology IntroductionyoussNo ratings yet
- Online Term Plan: Shriram LifeDocument10 pagesOnline Term Plan: Shriram LifeSivaramakrishna DavuluriNo ratings yet
- TB and Lung CancerDocument26 pagesTB and Lung CanceraprinaaaNo ratings yet
- Skin Cancer TBL 2 2f3Document19 pagesSkin Cancer TBL 2 2f3api-356476029No ratings yet
- Koss y Honda - Citología Del Tracto Urinario (2012)Document142 pagesKoss y Honda - Citología Del Tracto Urinario (2012)Lord Verminaard Luis Carreño DuranNo ratings yet
- Lung CancerDocument5 pagesLung Cancerreshmivunni100% (1)
- Verrucous Carcinoma of The Foot, M 63, Left FootDocument8 pagesVerrucous Carcinoma of The Foot, M 63, Left FootDeba P Sarma100% (1)
- 2009 Rad Onc Inservice Exam Key - TXIT - RationalesDocument106 pages2009 Rad Onc Inservice Exam Key - TXIT - RationalesTed Ling100% (2)
- Who Classification of Head & Neck Tumors - 2017Document343 pagesWho Classification of Head & Neck Tumors - 2017Pablo Enrique Mejia Paz78% (40)
- The Role of Vitamins in CancerDocument17 pagesThe Role of Vitamins in CancerNadir KoçakNo ratings yet
- Pathology - Research and PracticeDocument5 pagesPathology - Research and PracticeGabriela MilitaruNo ratings yet
- Case Presentation CA MammaeDocument17 pagesCase Presentation CA Mammaefrili adriaNo ratings yet
- Review For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 YearDocument9 pagesReview For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 Yeardjxela89No ratings yet
- Sysoeva Chemical Composition Andbiological Activity of Triterpenes and Steroids of Chaga MushroomDocument8 pagesSysoeva Chemical Composition Andbiological Activity of Triterpenes and Steroids of Chaga MushroomMachfud FauziNo ratings yet
- Final ICP AIPNA Int CME PathologyDocument3 pagesFinal ICP AIPNA Int CME PathologyArnab GhoshNo ratings yet
- Skin Cancer Project Report NewDocument13 pagesSkin Cancer Project Report NewAvinash Vad0% (1)