Professional Documents
Culture Documents
4 2 PDF
Uploaded by
Glad EscasuraOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
4 2 PDF
Uploaded by
Glad EscasuraCopyright:
Available Formats
Cancer-associated thrombosis (CAT) - New challenges for the hematologist - Section 2
Clinical prediction scores for venous thromboembolism in patients
with a hematological malignancy
Frits I. Mulder,1,2 Nick van Es1
1
Department of Vascular Medicine, Academic Medical Center, Amsterdam; 2Department of Internal Medicine,
Tergooi hospital, Hilversum, The Netherlands
Take Home Messages
- The performance of the Khorana score in predicting venous thromboembolism in patients with a hematological malig-
nancy is uncertain.
- ThroLy is a promising score for prediction of arterial or venous thromboembolism in lymphoma patients, but needs fur-
ther external validation.
- The clinical benefit of all risk scores remains uncertain, since they have not been thoroughly evaluated in randomized
controlled trials of risk-adapted thromboprophylaxis.
Introduction was derived in a prospective cohort of 2,701 cancer patients, of
whom 12% patients had lymphoma. In the internal validation
Venous thromboembolism (VTE) is a common complication in cohort of 1,365 patients, the observed 3-month VTE risk was
patients with hematological malignancy with an overall inci- 6.7% in patients with a high-risk score (≥3 points) compared to
dence of approximately 3.5% per 100 person years1. The risk of 1.5% in patients with a low or intermediate risk score (0-1
VTE varies substantially across different types of hematological points), corresponding to a relative risk (RR) of 4.5 (95% con-
malignancy, and also depends on cancer treatment, presence of fidence interval [CI], 2.1-9.6; Table 1). Results were not report-
a central venous catheter, and cancer stage.2 International guide- ed separately for lymphoma patients, which limits the generaliz-
lines recommend routine thromboprophylaxis in patients with ability of the findings for this particular group. In addition, the
multiple myeloma treated with immunomodulatory chemother- score was not intended to be used in patients with other types of
apy,3,4 but not in those with other hematological malignancies. hematological malignancies. In the past 3 years, several studies
Several risk scores have been developed to identify cancer addressed these issues by evaluating the performance of the
patients at high risk of VTE in whom thromboprophylaxis may Khorana score in patients with various hematological malignan-
be justified, but only a few were specifically evaluated in patients cies, as summarized in Table 1. Taken together, these external
with a hematological malignancy. This review aims to provide validation studies show that the relative risk of VTE in patients
an overview of the performance and potential clinical utility of with a hematological malignancy and a high-risk Khorana score
the currently available risk scores for cancer-associated VTE in is lower (RR 1.2 to 2.4) than reported in the original derivation
patients with a hematological malignancy. study. Whether this is due to differences in case-mix, study
design, or follow-up duration, or reflects a lower performance in
Khorana score patients with a hematological malignancy in general remains
unknown. Another concern is the low proportion of patients
The most widely used risk assessment tool for cancer-associated classified as high risk, ranging between 5 and 15%, which, in
VTE is the Khorana score, which is now endorsed by several combination with the modest relative risks, limits the clinical
guidelines.5,6 This risk score aims to identify ambulatory patients utility of the score in selecting patients for thromboprophylaxis.
with solid cancer or lymphoma at high risk of VTE prior to can- The reported positive predictive values (7 to 19%) may be high
cer therapy based on five clinical and laboratory parameters: enough to justify thromboprophylaxis, but differences in follow-
primary tumor site (e.g. +1 point for lymphoma), platelet count up duration and types of included cancers make it difficult to
of 350×109/L or more (+1 point), hemoglobin concentration of translate these findings to clinical practice (Table 1). The score
less than 10 g/dL and/or use of erythropoiesis-stimulating agents has not been validated in patients with acute leukemia, because
(+1 point), leukocyte count of more than 11×109/L (+1 point), these patients often have abnormal blood counts. Whether
and body mass index of 35 kg/m2 or more (+1 point).7 The score extending the Khorana score with D-dimer and soluble
Educational Updates in Hematology Book | 2018; 2(S2) | 37 |
F.I. Mulder, N. van Es Clinical prediction scores for venous thromboembolism in patients with a hematological malignancy
P-selectin levels, as proposed by Ay and colleagues, improves in the high-risk group (≥3 points) ranged between 13 and 23%
risk stratification in lymphoma patients is unknown.8 in the original derivation, internal validation, and external vali-
dation cohorts. Several external validation studies confirmed the
ThroLy score discriminatory performance of the IPSET score with reported
relative risks of thrombosis between 3.0 and 15 in high risk
The ThroLy score was developed by Antic and colleagues for patients (Table 1). The group that introduced the IPSET-score
predicting venous and arterial thrombotic events in ambulatory subsequently proposed a ‘practice-relevant revision’ by stratify-
lymphoma patients.9 The score is composed of seven clinical and ing patients into four groups based on age, previous thrombosis,
laboratory variables and was derived in 1,236 patients with lym- and JAK2V617F mutation.11 Although the score appeared to
phoma or chronic lymphocytic leukemia receiving chemothera- perform well in an external validation study,12 its ability to
py. In the internal validation cohort of 584 patients, the risk of improve risk-adapted prophylaxis needs to be confirmed in
arterial or venous thromboembolism was 29% in patients with prospective studies.
an intermediate or high-risk score (≥2 points) compared to 2.4%
in those with a low risk score (0-1 points). The c-statistic of the
Thromboprohylaxis risk assessment tool for multiple
score was 0.86. However, important information needed to fully
myeloma
appreciate the score’s performance, such as follow up-duration
and proportion of patients classified as being at risk, were unfor- A VTE risk assessment tool was developed by the International
tunately not reported. Both venous and arterial thromboembolic Multiple myeloma Working Group (IMWG) for patients with
events, including superficial thrombophlebitis, were part of the multiple myeloma receiving immunomodulatory drugs.4 The tool
outcome, which limits the use of the score when deciding about consists of a list of 17 patient-, myeloma-, and treatment-specific
primary VTE prevention. Although the ThroLy score appears risk factors. If no or any one of the risk factors are present in a
promising, it needs to be validated in external patient cohorts patient receiving thalidomide or lenalidomide, aspirin once daily
before it can be implemented in clinical practice. is recommended. If two or more risk factors are present, a pro-
phylactic dose of low-molecular-weight heparin or warfarin tar-
IPSET-thrombosis score geted at an INR of 2 to 3 is recommended. The IMWG risk score
is based on expert opinion without any validation studies, and
The International Prognostic Score for Essential should therefore not be regarded a firm guideline.
Thrombocythemia (IPSET) score was developed to predict arte-
rial or venous thrombotic events in patients with essential
Future perspectives
thrombocythemia (ET).10 The score is based on four variables:
age 60 years or older (+1 point), cardiovascular risk factors (+1 The Khorana score has now been evaluated in several studies of
point), previous thrombosis (+2 points), and JAK2V617F muta- patients with hematological malignancies, but results are not
tion (+2 points). The risk of arterial or venous thrombotic event unambiguous. Given the uncertainty, clinicians should be cau-
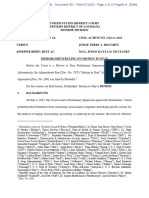
Table 1. Studies evaluating risk scores for thrombosis in patients with a hematological malignancy.
First author Number of Type Follow-up Outcome Overall Patients in high Positive RR for high vs
patients duration incidence risk group predictive value lower risk patients
n (%) n (%) (%) (95% CI)
Khorana score
Khorana 2008 (derivation cohort)7 2701* Lymphoma Median 73 days VTE 60 (2.2)* 340 (12.6)* 7.1* 4.6 (2.8-7.7)*
Khorana 2008 (validation cohort) 1365† Lymphoma Median 73 days VTE 28 (2.1)† 149 (10.9)† 6.7† 4.5 (2.1-9.6)†
Lim 201514 322 DLBCL Median 42 months VTE 34 (10.6) 16 (4.9) 18.8 1.9 (0.6-5.4)
Antic 2016 (cohort 1)15 1236 NHL, HL, CLL, SLL NR ATE, VTE 65 (5.3) NR 14.8 NR
Antic 2016 (cohort 2)15 584 NHL, HL, CLL, SLL NR ATE, VTE 34 (5.8) NR 14.8 NR
Rupa-Matysek 201716 428 DLBCL, HL Median 37 months VTE 64 (15) 64 (15) 17 1.2 (0.7-2.1)
Santi 201717 1189 DLBCL, FL, INFL, MCL 6 months VTE 41 (3.4) 141 (11.9) 7.1 2.4 (1.2-4.8)
ThroLy score
Antic 20169 (derivation cohort) 1236 NHL, HL, CLL, SLL NR ATE, VTE 65 (5.3) NR 25.1 NR
Antic 2016 (validation cohort) 584 NHL, HL, CLL, SLL NR ATE, VTE 34 (5.8) NR 28.9 NR
IPSET thrombosis score
Barbui 2012 (derivation cohort)18 535 ET Median 6.5 years ATE, VTE 59 (11) 63 (12) 17.5 1.7 (0.9-3.1)
Barbui 2012 (internal validation cohort)18 356 ET Median 6.1 years ATE, VTE 44 (12.4) 48 (14) 22.9 2.1 (1.2-3.9)
Barbui 2012 (external validation cohort)18 329 ET Median 5.0 years ATE, VTE 31 (9.4) 164 (50) 12.8 2.1 (1.0-4.4)
Fu 201419 746 ET Median 49 months ATE, VTE 77 (10.3) 221 (29.6) 19.5 3.0 (2.0-4.6)
Sevindik 201520 112 ET Median 4.1 years ATE, VTE 38 (33.9) 45 (40.2) 62.2 4.2 (2.3-7.7)
Navarro 201621 44 ET NR ATE, VTE 19 (43.2) 24 (54.6) 25.0 15.0 (2.2-102.8)
*Of the total study group, 12% had lymphoma and 88% a solid cancer. † Of the total study group, 14% had lymphoma and 86% a solid cancer. Abbreviations: ATE, arterial thromboembolism; CLL, chronic lym-
phocytic lymphoma; DLBCL, diffuse large B-cell lymphoma; ET, essential thrombocythemia; FL, follicular lymphoma; HL, Hodgkin’s lymphoma; INFL, indolent non-follicular lymphoma; NHL, non-Hodgkin lymphoma;
MCL, mantle cell lymphoma; MM, multiple myeloma; NR; not reported; RR; relative risk; SLL, small lymphocytic lymphoma; VTE, venous thromboembolism.
| 38 | Educational Updates in Hematology Book | 2018; 2(S2)
F.I. Mulder, N. van Es Clinical prediction scores for venous thromboembolism in patients with a hematological malignancy
tious to use the score to select patients for thromboprophylaxis. of an International Prognostic Score of thrombosis in World Health
The lymphoma-specific ThroLy score and ET-specific (revised) Organization-essential thrombocythemia (IPSET-thrombosis).
IPSET-scores are promising, but need additional external valida- Blood 2012;120:5128-33.
Derivation, internal validation, and external validation of a clinical
tion before they can be used in clinical practice. Future studies
risk score (IPSET-thrombosis) for arterial and venous thromboem-
need to focus either on validating existing scores in different set- bolism that can be used to guide decisions about providing aspirin
tings or on developing new models that more accurately select in patients with essential thrombocythemia.
patients with a high short-term risk of VTE. Ideally, scores *11. Barbui T, Vannucchi AM, Buxhofer-Ausch V, et al. Practice-relevant
should then be used to guide risk-adapted thromboprophylaxis revision of IPSET-thrombosis based on 1019 patients with WHO-
in randomized trials to confirm their performance and clinical defined essential thrombocythemia. Blood Cancer J 2015;5:2-4.
benefit. A revision of the IPSET-score that aims to further improve risk
stratification and simplify clinical decision making about aspirin in
patients with essential thrombocytemia.
References 12. Haider M, Gangat N, Lasho T, et al. Validation of the revised inter-
1. Horsted F, West J, Grainge MJ. Risk of venous thromboembolism national prognostic score of thrombosis for essential thrombo-
in patients with cancer: a systematic review and meta-analysis. cythemia (IPSET-thrombosis) in 585 Mayo clinic patients. Am J
PLoS Med 2012;9:e1001275. Hematol 2016;91:390-4.
2. Caruso V, Di Castelnuovo A, Meschengieser S, et al. Thrombotic *13. Khorana AA, Kuderer NM, Culakova E, et al. Development and
complications in adult patients with lymphoma: A meta-analysis of validation of a predictive model for chemotherapy-associated
29 independent cohorts including 18 018 patients and 1149 events. thrombosis. Blood 2008;111:4902-7.
Blood 2010;115:5322-8. Derivation and internal validation of a well-known clinical risk
3. Terpos E, Kleber M, Engelhardt M, et al. European myeloma net- score (Khorana score) for venous thromboembolism in ambulatory
work guidelines for the management of multiple myeloma-related patients with solid cancer or lymphoma that may guide decisions
complications. Haematologica 2015;100:1254-66. about thromboprophylaxis.
*4. International Myeloma Working Group (IMWG). IMWG 14. Lim SH, Woo SY, Kim S, et al. Cross-sectional Study of patients
Guidelines for the Prevention of Thalidomide- and Lenalidomide- with diffuse large B-cell lymphoma: Assessing the effect of host sta-
Associated Thrombosis in Myeloma 2010. tus, tumor burden and inflammatory activity on venous throm-
Expert-opinion based list of risk factors for venous thromboem- boembolism. Cancer Res Treat 2015:1-10.
bolism in patients with multiple myeloma receiving immunomodu- 15. Antic D, Milic N, Nikolovski S, et al. Comparative analysis of pre-
latory drugs that is used to guide decisions about primary preven- dictive models for thromboembolic events in lymphoma patients.
tion with aspirin, low-molecular-weight heparin, or vitamin K Hematol Oncol 2017;35:416.
antagonists. 16. Rupa-Matysek J, Gil L, Ka mierczak M, et al. Prediction of venous
5. Lyman GH, Bohlke K, Khorana AA, et al. Venous thromboem- thromboembolism in newly diagnosed patients treated for lym-
bolism prophylaxis and treatment in patients with cancer: phoid malignancies: validation of the Khorana Risk Score. Med
American society of clinical oncology clinical practice guideline Oncol 2018;35:1-8.
update 2014. J Clin Oncol 2015;33:654-56. 17. Santi RM, Ceccarelli M, Bernoccol E, et al. Khorana score and his-
6. Streiff MB, Holmstrom B, Ashrani A, et al. Cancer-associated totype predicts incidence of early venous thromboembolism in non-
venous thromboembolic disease, version 1.2015: Featured updates Hodgkin lymphomas. Thromb Haemost 2017;117:1615-21.
to the NCCN Guidelines. JNCCN J Natl Compr Cancer Netw 18. Barbui T, Finazzi G, Carobbio A, et al. Development and validation
2015;13:1079-95. of an International Prognostic Score of thrombosis in World Health
7. Khorana AA, Kuderer NM, Culakova E, , et al Development and Organization – essential thrombocythemia (IPSET-thrombosis).
validation of a predictive model for chemotherapy-associated Blood 2015;120:5128-34.
thrombosis. Clin Trials Obs 2008;111:4902-8. 19. Fu R, Xuan M, Lv C, et al. External validation and clinical evalua-
8. Ay C, Dunkler D, Marosi C, et al. Prediction of venous thromboem- tion of the International Prognostic Score of Thrombosis for
bolism in cancer patients. Blood 2010;116:5377-82. Essential Thrombocythemia (IPSET-thrombosis) in a large cohort of
*9. Antic D, Milic N, Nikolovski S, et al. Development and validation Chinese patients. Eur J Haematol 2014;92:502-9.
of multivariable predictive model for thromboembolic events in 20. Sevindik OG, Mersin S, Katgi A, et al. IPSET-thrombosis better
lymphoma patients. Am J Hematol 2016;91:1014-1019. identifies thrombosis-free survival: A Turkish cohort. Clin
Derivation and internal validation of a novel risk score (ThroLy) Lymphoma, Myeloma Leuk 2015;15:e101-4.
for arterial and venous thromboembolism in patients with lym- 21. Navarro LM, Trufelli DC, Bonito DR, et al. Application of prog-
phoma, which requires external validation before it should be used nostic score IPSET-thrombosis in patients with essential thrombo-
in clinical practice. cythemia of a Brazilian public service. Rev Assoc Med Bras
*10. Barbui T, Finazzi G, Carobbio A, et al. Development and validation 2016;62:647-51.
Educational Updates in Hematology Book | 2018; 2(S2) | 39 |
You might also like
- Acute LeukemiasFrom EverandAcute LeukemiasStefan H. FaderlNo ratings yet
- Towards Developing A Scoring System For Febrile ThrombocytopeniaDocument5 pagesTowards Developing A Scoring System For Febrile ThrombocytopeniaVimal NishadNo ratings yet
- Imaging in Peripheral Arterial Disease: Clinical and Research ApplicationsFrom EverandImaging in Peripheral Arterial Disease: Clinical and Research ApplicationsNo ratings yet
- Jurnal Padua2Document12 pagesJurnal Padua2inayatul munawarohNo ratings yet
- Saliba 2014Document4 pagesSaliba 2014Damian CojocaruNo ratings yet
- Tse 2014Document5 pagesTse 2014Ke XuNo ratings yet
- Ajbr0012 0097Document8 pagesAjbr0012 0097ResidenPatKlin Juli2022No ratings yet
- Int J of Urology - 2017 - Saluja - Venous Thromboembolism Prophylaxis in Urology A ReviewDocument5 pagesInt J of Urology - 2017 - Saluja - Venous Thromboembolism Prophylaxis in Urology A ReviewsofiaNo ratings yet
- Procal Vs MasccDocument7 pagesProcal Vs MasccRoshan MathewNo ratings yet
- TEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For ManagementDocument10 pagesTEP Systemic Thrombolysis For Pulmonary Embolism Evidence, Patient Selection, and Protocols For Managementbenitez1228No ratings yet
- JApplHematol5258-4238371 114623Document7 pagesJApplHematol5258-4238371 114623Agus SaputraNo ratings yet
- Deep Vein Thrombosis (DVT) Is A Precursor of Potentially Fatal PulmonaryDocument4 pagesDeep Vein Thrombosis (DVT) Is A Precursor of Potentially Fatal PulmonaryHatem ShafelNo ratings yet
- Diagnostic and Prognostic Value of Plasma Volume Status at Emergency Department Admission in Dyspneic Patients Results From The PARADISE CohortDocument11 pagesDiagnostic and Prognostic Value of Plasma Volume Status at Emergency Department Admission in Dyspneic Patients Results From The PARADISE CohortsunhaolanNo ratings yet
- Treating Vte Today: Practice Your Skills: Literature ReviewDocument14 pagesTreating Vte Today: Practice Your Skills: Literature ReviewOanaNo ratings yet
- Platelet To Lymphocyte Ratio and Neutrophil To Lymphocyte Ratio As Risk Factors For Venous ThrombosisDocument7 pagesPlatelet To Lymphocyte Ratio and Neutrophil To Lymphocyte Ratio As Risk Factors For Venous ThrombosisEvan Nanda AdilistyaNo ratings yet
- Prognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergDocument11 pagesPrognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergStephania SandovalNo ratings yet
- Leunase and TrombolismDocument12 pagesLeunase and TrombolismSanta UlinaNo ratings yet
- Thromboprohylaxis and DVT in Surgical PRDocument7 pagesThromboprohylaxis and DVT in Surgical PRAhmed MohammedNo ratings yet
- Ksienski 2021Document15 pagesKsienski 2021tim yuNo ratings yet
- Shungo Imai Bs Takehiro Yamada PHD Kumiko Kasashi PHD Masaki Kobayashi PHD Ken Iseki PHDDocument7 pagesShungo Imai Bs Takehiro Yamada PHD Kumiko Kasashi PHD Masaki Kobayashi PHD Ken Iseki PHDMutiara SeptianiNo ratings yet
- Blom JW - Malignancies, Prothrombotic Mutations, and The Risk of Venous ThrombosisDocument8 pagesBlom JW - Malignancies, Prothrombotic Mutations, and The Risk of Venous ThrombosisFarid RakhmanNo ratings yet
- Baudin 2015Document24 pagesBaudin 2015barbara liuva chia policarpoNo ratings yet
- How I Treat Pediatri CacutemyeloidleukemiaDocument10 pagesHow I Treat Pediatri CacutemyeloidleukemiaValeria FuentesNo ratings yet
- Manejo de Trombosis PulmonarDocument8 pagesManejo de Trombosis PulmonarMartínz A. DiegoNo ratings yet
- Biology of Blood and Marrow Transplantation: Journal HomepageDocument7 pagesBiology of Blood and Marrow Transplantation: Journal HomepageYakobus Antonius SobuberNo ratings yet
- Prognostic Significance of Neutrophil-to-Lymphocyte Ratio and PLRDocument9 pagesPrognostic Significance of Neutrophil-to-Lymphocyte Ratio and PLRdominguezmariela465No ratings yet
- Jurnal Divisi OnkologiDocument19 pagesJurnal Divisi OnkologiAtika PusparaniNo ratings yet
- Tep 2023Document9 pagesTep 2023Sche Fra MediSiNo ratings yet
- LeukemiaDocument10 pagesLeukemiaShapira alNo ratings yet
- Prognostic Markers in Young Patients With Premature Coronary Heart DiseaseDocument5 pagesPrognostic Markers in Young Patients With Premature Coronary Heart DiseaseMano cempakaNo ratings yet
- Machine Learning Prediction of Mortality and Hospitalization in Heart Failure With Preserved Ejection FractionDocument10 pagesMachine Learning Prediction of Mortality and Hospitalization in Heart Failure With Preserved Ejection FractionS. M MEHEDI ZAMAN, 180021128No ratings yet
- Machine Learning Prediction of Mortality and Hospitalization in Heart FailureDocument10 pagesMachine Learning Prediction of Mortality and Hospitalization in Heart Failureabinaya venkateshNo ratings yet
- 0504 NewsPath Breast Carcinoma MarkersDocument2 pages0504 NewsPath Breast Carcinoma MarkersJosé Mauricio PeñalozaNo ratings yet
- Clinical and Etiological Profile of Unprovoked Thrombosis in Young Patients Admitted at A Tertiary Care HospitalDocument5 pagesClinical and Etiological Profile of Unprovoked Thrombosis in Young Patients Admitted at A Tertiary Care HospitalfarhanomeNo ratings yet
- Crit Care Nurse 2011 Raingruber E17 22Document7 pagesCrit Care Nurse 2011 Raingruber E17 22Cathlab RsiaNo ratings yet
- Pi Is 0741521412019982Document8 pagesPi Is 0741521412019982Noor Hafizah HassanNo ratings yet
- C-Reactive Protein and Cardiovascular Diseases-Is It Ready For Primetime?Document7 pagesC-Reactive Protein and Cardiovascular Diseases-Is It Ready For Primetime?dastgirrajaNo ratings yet
- Cerebral Venous Thrombosis: Clinical Predictors and Emerging TreatmentsDocument3 pagesCerebral Venous Thrombosis: Clinical Predictors and Emerging Treatmentschartreuse avonleaNo ratings yet
- Biology of Blood and Marrow TransplantationDocument6 pagesBiology of Blood and Marrow TransplantationFrankenstein MelancholyNo ratings yet
- Misra 2012Document7 pagesMisra 2012Carlos RiquelmeNo ratings yet
- Thrombosis and Acute LeukemiaDocument6 pagesThrombosis and Acute Leukemiaannisa edwarNo ratings yet
- Regular ArticleDocument11 pagesRegular ArticleOmar FernándezNo ratings yet
- Biology of Blood and Marrow TransplantationDocument7 pagesBiology of Blood and Marrow TransplantationAndrés JimenezNo ratings yet
- Plasma Concentration of C-Reactive Protein and Risk of Developing Peripheral Vascular DiseaseDocument8 pagesPlasma Concentration of C-Reactive Protein and Risk of Developing Peripheral Vascular Diseaseashphoenix32No ratings yet
- jhm2616 AmDocument15 pagesjhm2616 Amkishore kumar meelNo ratings yet
- Assessment of Tumor Infiltrating Lymphocytes Using.12Document9 pagesAssessment of Tumor Infiltrating Lymphocytes Using.12Muhammad Rifki100% (1)
- Reference - 04Document9 pagesReference - 04Omar García HernándezNo ratings yet
- Eria 2Document3 pagesEria 2Johan Wijaya KesitNo ratings yet
- Napolitano 2006Document14 pagesNapolitano 2006Olivia Alexandra DavidNo ratings yet
- Journal Pmed 0050097Document9 pagesJournal Pmed 0050097astriaciwidyaNo ratings yet
- Int J Lab Hematology - 2017 - Galtseva - Minimal Residual Disease in Multiple Myeloma Benefits of Flow CytometryDocument9 pagesInt J Lab Hematology - 2017 - Galtseva - Minimal Residual Disease in Multiple Myeloma Benefits of Flow CytometrymatanhibNo ratings yet
- Prediction of Pulmonary Embolism in The Emergency DepartmentDocument10 pagesPrediction of Pulmonary Embolism in The Emergency DepartmenttechiemedicNo ratings yet
- Dose-Adjusted Enoxaparin Thromboprophylaxis in Hospitalized CancerDocument7 pagesDose-Adjusted Enoxaparin Thromboprophylaxis in Hospitalized CancerAnonymous 9dVZCnTXSNo ratings yet
- Raymakers Et Al (2013) - Diagnostic Strategies Incorporating Computed Tomography Angiography For Pulmonary EmbolismDocument8 pagesRaymakers Et Al (2013) - Diagnostic Strategies Incorporating Computed Tomography Angiography For Pulmonary EmbolismNicolaNo ratings yet
- BR J Haematol - 2023 - MahdiDocument13 pagesBR J Haematol - 2023 - MahdiPriyadharshini MuruganNo ratings yet
- XimlagaltranDocument9 pagesXimlagaltranDQ DQNo ratings yet
- Joc 00458Document8 pagesJoc 00458wiyangga92No ratings yet
- Article Ang3Document9 pagesArticle Ang3Ayoub HajjarNo ratings yet
- Risk Factors and Complications of Subconjunctival Hemorrhages in Patients Taking WarfarinDocument5 pagesRisk Factors and Complications of Subconjunctival Hemorrhages in Patients Taking WarfarinSyafar Agus Al-Fath MukminNo ratings yet
- Cardiovascular Therapeutics - 2018 - Yuan - The Incidence of Atrial Fibrillation With Trastuzumab Treatment A SystematicDocument7 pagesCardiovascular Therapeutics - 2018 - Yuan - The Incidence of Atrial Fibrillation With Trastuzumab Treatment A SystematicOttofianus Hewick KalangiNo ratings yet
- Analytical ExpositionDocument5 pagesAnalytical ExpositionMuhammad Rafi AldianzaNo ratings yet
- FINAL-EXAM-level-Vi DESARROLLADODocument5 pagesFINAL-EXAM-level-Vi DESARROLLADOEmerzon GuevaraNo ratings yet
- Lifetech CorpDocument6 pagesLifetech Corpapi-534468863No ratings yet
- ENT DiseasesDocument75 pagesENT DiseasesGudeta shegerNo ratings yet
- Uworld Notes CK PDFDocument123 pagesUworld Notes CK PDFNik KalairNo ratings yet
- Module 4 HandoutsDocument20 pagesModule 4 HandoutsAlazar DejeneNo ratings yet
- PMMAEE Application FormDocument2 pagesPMMAEE Application Formshiero501100% (15)
- Atow 459 00Document9 pagesAtow 459 00Javier Fernando Cabezas MeloNo ratings yet
- Running Head: Contagion Movie Assessment 1Document5 pagesRunning Head: Contagion Movie Assessment 1swathim123No ratings yet
- Principles of Antiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyDocument36 pagesPrinciples of Antiplatelet Therapy: DR Htet Htet Htethtet@Imu - Edu.MyAbby Liew100% (1)
- Umar Muhammad Basalamah 22010112110188 Lap - KTI BAB 7Document25 pagesUmar Muhammad Basalamah 22010112110188 Lap - KTI BAB 7Sofila FilaNo ratings yet
- Gram PosetiveDocument82 pagesGram Posetiveabrham sharewNo ratings yet
- MDH and MDE K-12 Planning GuideDocument116 pagesMDH and MDE K-12 Planning GuideDuluth News Tribune100% (1)
- The History of Hiatal Hernia SurgeryDocument9 pagesThe History of Hiatal Hernia SurgeryDaniel PredaNo ratings yet
- AB-M02-CH2.3-LIVER PATH-Focal Abnormalities PDFDocument40 pagesAB-M02-CH2.3-LIVER PATH-Focal Abnormalities PDFThomas AndersonNo ratings yet
- Smoking Behaviour and Mental Health Disorders-Mutual Influences and Implications For TherapyDocument22 pagesSmoking Behaviour and Mental Health Disorders-Mutual Influences and Implications For TherapyRizza Faye BalayangNo ratings yet
- Genetic Counselling AssignmentDocument3 pagesGenetic Counselling Assignmentjyoti singhNo ratings yet
- Names: MANIRAHO Cyprien Reg. Numbers: 020/04/GN/933 Individual AssignimentDocument70 pagesNames: MANIRAHO Cyprien Reg. Numbers: 020/04/GN/933 Individual AssignimentCyprien Silencer ManirahoNo ratings yet
- +2 Bio Zoo em 7 12 LessonsDocument30 pages+2 Bio Zoo em 7 12 LessonsInnovative IndustryNo ratings yet
- Shoulder InjuriesDocument18 pagesShoulder InjuriesJGP90No ratings yet
- Maxwell Today MattersDocument39 pagesMaxwell Today MattersAnna Castillo100% (5)
- Module 4 RLE Activity NeriDocument9 pagesModule 4 RLE Activity NeriAngela Neri75% (4)
- Sural Nerve BiopsyDocument2 pagesSural Nerve BiopsyArindam MukherjeeNo ratings yet
- Effectiveness of A Network ofDocument6 pagesEffectiveness of A Network ofrichardong lauNo ratings yet
- Gov - Uscourts.lawd.189520.301.0 1Document13 pagesGov - Uscourts.lawd.189520.301.0 1Susie MooreNo ratings yet
- Bronchial AsthmaDocument7 pagesBronchial AsthmaKarolien Faye DongaNo ratings yet
- Review Article: Relevant Biliary Anatomy During CholecystectomyDocument11 pagesReview Article: Relevant Biliary Anatomy During CholecystectomyAbrar SabawiNo ratings yet
- Chapter 4: Flexibility Training ExerciseDocument5 pagesChapter 4: Flexibility Training ExerciseApolonia DayagNo ratings yet
- Research Final Paper111Document21 pagesResearch Final Paper111Carlos DelacruzNo ratings yet
- An Introduction To Vibroacoustic Therapy (Jeff Hooper)Document9 pagesAn Introduction To Vibroacoustic Therapy (Jeff Hooper)Andrea BarresiNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4.5 out of 5 stars4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (60)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)