Professional Documents
Culture Documents
Quality Asurance Lec 10&11 PDF
Uploaded by
raju niraulaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Quality Asurance Lec 10&11 PDF
Uploaded by
raju niraulaCopyright:
Available Formats
Quality Assurance in
Hematology Laboratory
Suhair.A.A./ Quality Assurance / 3rd
year 1
Quality Assurance includes
• Pre Analytical Control
• Post Analytical Control
• Analytical Control
➢Internal Quality Control
➢External Quality Assessment
Suhair.A.A./ Quality Assurance / 3rd
2 year
◼ Quality assurance is essential in
hematology to ensure that laboratory tests
are carried out reliably.
◼ Quality assurance is concerned with all
steps of laboratory practice.
◼ The process from specimen collection
included in the pre-analytical portion to
transmission of the report to the clinician
which include the post analytical control.
And the analytical process in-between.
Suhair.A.A./ Quality Assurance / 3rd
year 3
PRE-ANALYTICAL CONTROL
Suhair.A.A./ Quality Assurance / 3rd
4 year
Understanding functionality of
the instrument:
• principles of operation
• startup or daily checks
• shutdown procedure
• normal sights and sounds of the instrument
• familiarize staff to troubleshooting manual
Suhair.A.A./ Quality Assurance / 3rd
5 year
◼ Non-technical people will say that the
instruments can run themselves now you don’t
need to know anything just put the blood on
the instrument and push a button and then you
get the results.
◼ This is so untrue. It is very important for all
staff to understand what happens to that blood
is sampled by the instruments.
◼ When they get the results which is involved in
the Post analytical they need to decide if the
results are correct.
Suhair.A.A./ Quality Assurance / 3rd
year 6
◼ If there are problems then we need to be able to
troubleshoot where the inaccurate result came
from. Is it from the sampling valve? Are the
pressures and vacuums correct to move the
sample about the tubing. Is there a problem with
the reagents? All of these questions can be
answered if the staff to have a good
understanding of the working of the instrument.
◼ Performing startup and daily checks is another
important area. The results can also tell you if
your instrument is functioning correctly.
Suhair.A.A./ Quality Assurance / 3rd
year 7
◼ Then at the end of work day the shutdown. As we all
know blood is very sticky mainly caused by the protein.
This protein will coat all the tubing and parts of the
instrument so that shutdown is important because the
reagent will clean those surfaces.
◼ Next knowing what are the normal sounds and sights of
the instrument. When we walk up to it we should be
looking to make sure we don’t see any leakage. Same
with any unusual sounds.
◼ Part of staff training with a new instrument is familiarizing
them to the troubleshooting manual.
Suhair.A.A./ Quality Assurance / 3rd
year 8
Hematology Subsystems
◼ On most hematology instruments they are
broken into three subsystems
➢ Electronic
➢ Fluidic
▪ Pneumatics (pressure and vacuums)
▪ Hydraulics (liquids)
➢ Reagent
Suhair.A.A./ Quality Assurance / 3rd
9 year
Proper Specimen Collection
◼ Analyze only specimens that were
properly collected and stored.
➢ Correct Tube
➢ Correct amount of specimen in tube
➢ Proper mixing
➢ Cleanliness of puncture area
➢ Storage
Suhair.A.A./ Quality Assurance / 3rd
10 year
Exercise 1
Suhair.A.A./ Quality Assurance / 3rd
year 11
Pre-Analytical Example 1
21-May-2015
13:45
WBC 0.05 x 10^3/L PASS
RBC 0.00 x 10^6/L PASS
Hgb 0.00 x g/dl PASS
Plt 10.0 x 10^3/U FAILED
Suhair.A.A./ Quality Assurance / 3rd
12 year
Example 1 - Here we have a
background printout after start-up. As
you can see the Platelet background
failed. First would look at your
troubleshooting guide.
What would you think most likely first
step would be?
* Perform another background count.
Suhair.A.A./ Quality Assurance / 3rd
year 13
Repeat Background
Here is our rerun and still platelets are out even more. Once
again would check your troubleshooting SOP.
21-May-2015
14:00
WBC 0.05 x 10^3/L PASS
RBC 0.00 x 10^6/L PASS
Hgb 0.00 x g/dl PASS
Plt 15.0 x 10^3/U FAILED
Suhair.A.A./ Quality Assurance / 3rd
14 year
Corrective Action:
◼ some possible corrective actions tobe
perform :
◼ Check when reagent(s) last changed.
◼ Change the most recently added reagent.
◼ If none recently added change the diluent.
◼ Rerun start-up
Suhair.A.A./ Quality Assurance / 3rd
15 year
Repeat Background
21-May-2015
14:30
WBC 0.05 x 10^3/L PASS
RBC 0.00 x 10^6/L PASS
Hgb 0.00 x g/dl PASS
Plt 2.0 x 10^3/U PASS
Suhair.A.A./ Quality Assurance / 3rd
16 year
So for the example background is in and we
can continue with our daily maintenance.
But just like any problem we need to
document the corrective action and try to
figure out possible causes of it.
Suhair.A.A./ Quality Assurance / 3rd
year 17
Causes for high background
◼ The uptake tubing got contaminated.
◼ Reagent agitated before connecting
to instrument.
◼ Dried reagent spills or leaks.
Suhair.A.A./ Quality Assurance / 3rd
18 year
◼ Here we have a typical counting chamber. The
diluted sample enters the chamber and is draw
through the aperture to the other side. If everyone
remembers the coulter principle there is an
external and internal electrode. When sample is
pulled through the aperture there is a change in
electrical current. This change in electrical current
is sized and counted either as a RBC, Platelet or
WBC depending on the aperture. So if there is
salt deposits near the aperture this can create
extra electrical impulses. Always clean all spills
and leaks immediately.
Suhair.A.A./ Quality Assurance / 3rd
year 19
Suhair.A.A./ Quality Assurance / 3rd
20 year
Pre-Analytical Example 2
All parameters have a “P” code
Partial Aspiration
Suhair.A.A./ Quality Assurance / 3rd
year 21
What can give this code?
◼ Sample could be clotted.
◼ Hemoglobin is less than 4 g/dl
◼ Sample volume too low.
◼ The blood detector was turned off.
◼ Check your instrument manual.
Suhair.A.A./ Quality Assurance / 3rd
22 year
• As for any problem the first step is to consult the
troubleshooting guide. Here are some reasons may have
gotten this code/error message.
• Check the sample for clots.
• Even though this seems impossible we have seen patients with
low hemoglobin but usually not the norm. To confirm if it is due
to a low hemoglobin can run through open/manual mode. This
bypasses the blood detector. If there were no clots and the
result repeats manually then we technically can take the result.
One last thing should do is make sure that the blood was not
drawn through or above an IV line and was diluted out by
saline. Check the volume in the tube. If less than 1 ml can’t be
aspirated in auto/closed mode. Could be run in manual mode
but should not. This sample would be diluted out and cause
false low results.
Suhair.A.A./ Quality Assurance / 3rd
year 23
Other Corrective Steps
Here are some other possible steps you
may find in your troubleshooting section:
◼ Troubleshoot for leaks, kinks or plugs
along the sample flow path.
◼ Ensure the aspiration lines are clean.
◼ Check for needle plugs.
◼ Call Service Hot Line
Suhair.A.A./ Quality Assurance / 3rd
24 year
Post-Analytical Control
Understanding your
instrument results:
Suhair.A.A./ Quality Assurance / 3rd
year 25
◼ Next we will look at post-analytical control.
Post analytical looks at the results and
determining if they are correct. Usually
instruments have different flags, codes
and messages. We will look at some of
these.
Suhair.A.A./ Quality Assurance / 3rd
year 26
Flags
• Can be a letter or symbol that appears to
right of the result.
➢ Manufacturer controlled
➢ Aspiration, Linearity, interference
➢ Laboratory controlled
➢ Critical range
➢ Decision rules
Suhair.A.A./ Quality Assurance / 3rd
27 year
◼ Here we have examples. The one on the
left shows the instrument flag. These are
from Coulter instrument. The other
instruments have similar flags. Please
check you manual for them.
◼ The middle one set by the lab showing the
monocytes are above our upper normal
range.
◼ The far right shows a combination of
instrument and laboratory flags.
Suhair.A.A./ Quality Assurance / 3rd
year 28
Suhair.A.A./ Quality Assurance / 3rd
29 year
Codes
◼ Symbols that appear in place of results
➢ Indicatebeyond reportable range +++++
➢ Vote-out of aperture
➢ Unable to calculate result
➢ Clogged flow cell
Suhair.A.A./ Quality Assurance / 3rd
30 year
Messages
◼ Usually manufacturer messages
◼ Indicate possible abnormal cells,
clumping, agglutination
◼ Used to decide on reporting of instrument
vs manual differential or verification of
measured results.
◼ Here are some Messages that you can
see:
Suhair.A.A./ Quality Assurance / 3rd
31 year
I
W
Suhair.A.A./ Quality Assurance / 3rd
32 year
Patient Results
• Are the results consistent with the patient’s
condition?
• Delta checks
➢ Can be set on instrument or LIS.
➢ Checks against previous result.
➢ Value set by laboratory.
Suhair.A.A./ Quality Assurance / 3rd
33 year
H & H Check/Difference
◼ Hgb x 3 = HCT +/- 3%
◼ If > +/-3 can indicate a problem.
➢Instrument
➢Sample
Suhair.A.A./ Quality Assurance / 3rd
34 year
Exercise 2
Suhair.A.A./ Quality Assurance / 3rd
year 35
◼ A 45 year old women had her blood drawn for
routine testing. A CBC was run on a Coulter
GENS instrument?
◼ What stands out on these results?
◼ Low platelets, all the flags
◼ What should be done? Make a slide and
confirm results.
Suhair.A.A./ Quality Assurance / 3rd
year 36
Post Analytical Example 1
Laboratory Results Instrument Differential
WBC - 8,900/uL Neutrophil % - 52.5%
RBC - 4,460,000/uL Lymphocyte % - 35.2%
Hgb -13.4 g/dl Monocyte % - 10.4%
HCT- 40.7% Eosinophil % - 1.4%
Platelets - 56,000/ul Basophil % - 0.5%
MCV - 91.1.1fl Flags
MCH - 29.9pg WBC interference (*)
MCHC - 32.8g/dl Micro/Fragmented RBC
Giant Platelets
RDW - 23.1%
R (Review)-code on
Platelets
Platelet Clumps
Suhair.A.A./ Quality Assurance / 3rd
37 year
◼ So here is what the tech sees • Second possibility is drawing a
when they look at the smear. blue top. Sometimes the EDTA
◼ What is it? in the lavender can cause the
◼ Answer: Platelet clumping. You run it on your
Satalitosis/Platelet clumps instrument and make a slide. If
you see no clumping then the
◼ Couple reporting choices. WBC and platelet count from the
◼ First could try vortexing the blue top can be used. But what
purple top for about 1-2 has to happen to the results
minutes, make a slide then run before reporting them? They
manually on the instrument. need to be multiplied by 1.1 due
This sometimes gets rid of the to the dilution of the
clumps. anticoagulant in the blue top.
• If none of these get rid of the
clumping then should report out
an estimate only no numerical
result.
Suhair.A.A./ Quality Assurance / 3rd
year 38
Suhair.A.A./ Quality Assurance / 3rd
39 year
Here is what it looked like after vortexing. If you choose to use this
procedure you will have to validate it. This can be done by running at
least 20 samples that do not have any platelet clumping seen on the
smears. After the initial run then you would vortex each sample for
specific amount of time. We did 2 minutes. You would make a slide
immediately and run it manually not closed mode through the
instrument. You do it for all 20 samples than calculated the %
difference before and after vortexing. You would want to see less than
10% difference in the results for the platelets.
On patients with clumping what you will see on the post vortex is a
decrease in the WBC and an increase in platelets. Once again you
need to confirm with a smear. Why would you see a decrease in
WBC? The clumps were counted as WBC. For reporting all results
from the pre-vortex sample are reported except the WBC and Platelet
and instrument differential. The vortex WBC and platelet replace the
original if all clumping is gone. Of course if you need a differential on
this sample it should be performed manually.
Suhair.A.A./ Quality Assurance / 3rd
year 40
Suhair.A.A./ Quality Assurance / 3rd
41 year
Post Analytical Example 2
Laboratory Results
WBC - 8,500/uL Instrument Differential
RBC - 4,870,000/uL
Neutrophil% - 60.9%
Lymphocyte % - 28.7%
Hgb - 16.4 g/dl
Monocyte % - 8.2%
HCT - 43.5%
Eosinophil% - 2.0%
Platelets - 356,000/ul
Basophil% - 0.2%
MCV - 89.5 fl
Flags
MCH - 23.6 pg
H-H difference check
MCHC - 37.7 g/dl
Alert (aH) on the MCHC
RDW -12.5%
Spun HCT – 44%
Suhair.A.A./ Quality Assurance / 3rd
year 42
The patient is a 54 year old man. A routine CBC was
drawn in the out-patient department and it was run on a
Coulter LH750.
The technologist reviewed the instrument CBC,
automated Diff and flags
These are the problems that were noted –
MCHC > 36.0
H&H Check Flag - H & H does not pass rule of three
(three times the HGB should equal the HCT +/- 3)
The laboratory policy is to spin a Hematocrit on any
MCHC >36.0
The Spun hematocrit matches the hematocrit from the
instrument.
Therefore, the HGB is the incorrect parameter –
Suhair.A.A./ Quality Assurance / 3rd
year 43
What is the Explanation ?
Spun Plasma
◼ The MCHC is > 36
◼ The spun hematocrit matches the
instrument
◼ It would appear that the Hgb is
incorrect
◼ Lipemia will falsely increase the
hemoglobin result
◼ Follow laboratory policy for lipemic
samples
Suhair.A.A./ Quality Assurance / 3rd
year 44
Post Analytical Example 3
Laboratory Result 1 Laboratory Result 2
WBC - 8,500/uL WBC – 8,300/uL
RBC - 4,870,000/uL RBC – 4,000,000/uL
Hgb - 16.4 g/dl Hgb – 16.2 g/dl
HCT – 48.2% HCT – 36.0%
Platelets - 356,000/ul Platelets – 340,000/uL
MCV - 89.5 fl MCV – 90.0 fl
MCH - 33.7 pg MCH – 40.5 pg
MCHC – 34.0 g/dl MCHC – 45.0 g/dl
No flags H-H difference check
Delta Check on HCT
and MCHC
Suhair.A.A./ Quality Assurance / 3rd
year 45
When we look at the spun hematocrit this is what it
looks like. It shows that the sample is hemolyzed.
A Hemolyzed sample would causes a decrease in
the RBC count which in turn would affect the HCT
result. Hemolysis would not affect the Hgb or MCV
so it will cause an increase in the MCHC. It also
affects the MCH result.
Suhair.A.A./ Quality Assurance / 3rd
year 46
Suhair.A.A./ Quality Assurance / 3rd
47 year
Post Analytical Example 4
Laboratory Result 1 Laboratory Result 2
WBC – 6,300/uL WBC – 6,800/uL
RBC – 2,321,000/uL RBC –3,475,000 /uL
Hgb – 6.5 g/dl Hgb – 9.5 g/dl
HCT – 19.5% HCT – 28.5%
Platelets - 250,000/ul Platelets – 240,000/uL
MCV - 75 fl MCV – 82 fl
MCH – 28.0 pg MCH – 29.0pg
MCHC – 33.3.0 g/dl MCHC – 34.3.0 g/dl
RDW – 9.8 RDW – 13.4
Delta Check on Hgb,
HCT, and MCV
Suhair.A.A./ Quality Assurance / 3rd
year 48
◼ The patient is a 32 year old female. Two routine
CBC was drawn a week apart in the out-patient
department and it was run on a Coulter LH750.
◼ The technologist reviewed the instrument CBC,
automated Diff and flags
◼ We have some differences
◼ We have Delta Checks on the Hgb, Hct, MCV,
and MCHC. Any possible explanations?
Suhair.A.A./ Quality Assurance / 3rd
year 49
Suhair.A.A./ Quality Assurance / 3rd
50 year
Analytical Control
• Internal Quality Control
• External Quality
Assessment
Suhair.A.A./ Quality Assurance / 3rd
year 51
INTERNAL QUALITY CONTROL
Suhair.A.A./ Quality Assurance / 3rd
52 year
Internal Quality Control includes
• Daily control specimen
➢ Commercial Control
➢ Patient Control
• Correlation/Comparison System
• Policy- QC and Troubleshooting
Suhair.A.A./ Quality Assurance / 3rd
53 year
Internal Quality
Control
Commercial Controls
Suhair.A.A./ Quality Assurance / 3rd
year 54
Commercial Controls
◼ Assayed vs Non-assayed
◼ Introducing New QC Lot
◼ Establishing QC Ranges
Suhair.A.A./ Quality Assurance / 3rd
55 year
Establishing Means and Standard
Deviations
1. Analyze the control(s) a minimum of 20 times across several
days.
2. Take the average of these runs.
3. The average should be within the range state on the assay
sheet.
4. Calculate a two Standard Deviation range from your results.
5. Incorporate this SD range around your new mean and
monitor.
6. The mean and SD values should be periodically recalculated
during the life of the new lot.
Suhair.A.A./ Quality Assurance / 3rd
56 year
Factors to Consider for Means
◼ Some hematology parameters, such as MCV,
Platelets and RBC will start to change over
time.
◼ MCV will increase.
◼ RBC values can decrease.
◼ Platelets values will increase.
◼ Mean, SD, and CV should be evaluated
monthly.
Suhair.A.A./ Quality Assurance / 3rd
57 year
8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 8 9 8 8
1 0 2 4 5 6 3 2 1 3 4 5 3 5 4 3 1 3 5 4 3 5 6 5 4 5 6 3 5 5 4 5 6 6 5 6 5 6 7 6 7 6 7 8 8 9 5 6 7 8 9 6 7 8 9 0 8 9 85.20
Suhair.A.A./ Quality Assurance / 3rd
58 year
QC Example 2
◼ Manufacturer RBC mean – 2.29 x 106
◼ Manufacturer RBC Range – 2.18-2.40 x 106
◼ Calculated RBC mean – 2.35 x 106
◼ Is this mean valid?
◼ Our 2SD = 0.15 x 106
◼ Calculated RBC range – 2.20-2.50 x 106
◼ Yes mean within the expected range.
Suhair.A.A./ Quality Assurance / 3rd
59 year
QC Example 3
◼ Manufacturer Platelet mean – 528 x 103
◼ Manufacturer Platelet Range – 407- 649x 103
◼ Calculated Platelet mean – 402x 103
◼ Is this mean valid?
◼ No below the expected range.
Suhair.A.A./ Quality Assurance / 3rd
60 year
Commercial Control
Monitoring
Levey-Jennings Charts
Suhair.A.A./ Quality Assurance / 3rd
year 61
Levey-Jennings QC Charts
Suhair.A.A./ Quality Assurance / 3rd
year 62
Trend
Suhair.A.A./ Quality Assurance / 3rd
year 63
First we will look at a Trend. A trend occurs when
five or more values show a gradual increase or
decrease. The values do not have to be out of your
acceptable range but this pattern can indicate that
a problem exists. Because hematology controls are
cell-based, some trending in sizing parameters can
be expected.
Suhair.A.A./ Quality Assurance / 3rd
year 64
Shift
Suhair.A.A./ Quality Assurance / 3rd
year 65
Next we have a Shift. This is when there is a
sudden change in control results from one run or
day to the next. A shift does not always mean
that a problem exists. What are some reason
you might get a shift? Instrument calibrated.
Service performed.
Suhair.A.A./ Quality Assurance / 3rd
year 66
Bias
Suhair.A.A./ Quality Assurance / 3rd
year 67
Finally we have a bias. A bias is when the control
starts running on one side of the mean. It can occur
with just one or all of your controls. If it is only one of
your control can indicate a problem with just that
level. If it is across all the controls than can indicate
an instrument problem or the need to calibrate.
Suhair.A.A./ Quality Assurance / 3rd
year 68
QC Policy
◼ Each laboratory should adopt QC rules.
◼ Establish policy/corrective action for
controls that are “Out”.
➢ Documentation is important.
◼ Establish policy for Trends, bias and shifts.
◼ Establish when calibration are required.
Suhair.A.A./ Quality Assurance / 3rd
69 year
Thanks
Suhair.A.A./ Quality Assurance / 3rd
year 70
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Autism Symptoms ChecklistDocument1 pageAutism Symptoms ChecklistkarunaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Vocab PDFDocument64 pagesVocab PDFEasy OkNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Lang 10 EditionDocument235 pagesLang 10 Editionraju niraulaNo ratings yet
- Lang 10 EditionDocument235 pagesLang 10 Editionraju niraulaNo ratings yet
- RHEOLOGYDocument39 pagesRHEOLOGYraju niraulaNo ratings yet
- Medicinal Chemistry Exam 1Document16 pagesMedicinal Chemistry Exam 1merbeb89% (18)
- KAPS APRIL, 3rd 2017Document12 pagesKAPS APRIL, 3rd 2017raju niraulaNo ratings yet
- GTE Letter - Sangeeta WaibaDocument7 pagesGTE Letter - Sangeeta Waibaraju niraulaNo ratings yet
- Nurseslabs Lab Values PDFDocument2 pagesNurseslabs Lab Values PDFJan BularioNo ratings yet
- Puberty Self-CareDocument13 pagesPuberty Self-CareAira MendozaNo ratings yet
- KENT Application Form (V18)Document6 pagesKENT Application Form (V18)raju niraulaNo ratings yet
- Quality Asurance Lec 7Document26 pagesQuality Asurance Lec 7raju niraula100% (1)
- Quality Assurance Lec 10Document42 pagesQuality Assurance Lec 10raju niraulaNo ratings yet
- Person DistributionDocument11 pagesPerson Distributionraju niraulaNo ratings yet
- Quality Asurance Lec 5&6Document42 pagesQuality Asurance Lec 5&6raju niraula100% (1)
- LABORATORY ERRORS CAUSES AND PREVENTIONDocument24 pagesLABORATORY ERRORS CAUSES AND PREVENTIONraju niraulaNo ratings yet
- Pharmaceutical Validation: Why Is Validation Required?Document26 pagesPharmaceutical Validation: Why Is Validation Required?raju niraulaNo ratings yet
- Quality Assurance - Lec2Document18 pagesQuality Assurance - Lec2raju niraulaNo ratings yet
- Quality Assurance - Lec 3Document34 pagesQuality Assurance - Lec 3raju niraula100% (1)
- Quality Assurance Lec 8Document35 pagesQuality Assurance Lec 8raju niraulaNo ratings yet
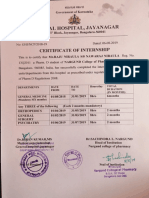
- Internship CertificateDocument1 pageInternship Certificateraju niraulaNo ratings yet
- Quality AssuranceDocument27 pagesQuality Assuranceraju niraulaNo ratings yet
- PharmacyCareerGuide PDFDocument52 pagesPharmacyCareerGuide PDFraju niraulaNo ratings yet
- Recalls KAPS 2009 Paper-1 March PDFDocument4 pagesRecalls KAPS 2009 Paper-1 March PDFraju niraulaNo ratings yet
- Dina-Farouk Q - A NotesDocument120 pagesDina-Farouk Q - A Notesraju niraulaNo ratings yet
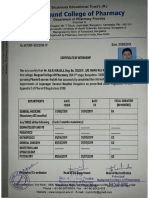
- Training CertificateDocument15 pagesTraining Certificateraju niraulaNo ratings yet
- Adverse Drug Reaction Reporting Form: - Sr. NoDocument2 pagesAdverse Drug Reaction Reporting Form: - Sr. Nosaadtanvir1256No ratings yet
- 2 April 2019Document9 pages2 April 2019raju niraulaNo ratings yet
- Important Drug Doses PDFDocument15 pagesImportant Drug Doses PDFraju niraulaNo ratings yet
- Recalls KAPS 2008 With AnswersDocument4 pagesRecalls KAPS 2008 With Answersraju niraulaNo ratings yet
- SfdfbsDocument18 pagesSfdfbsraju niraulaNo ratings yet
- LojiDocument6 pagesLojiraju niraulaNo ratings yet
- Daepoch Protocolo BccancerDocument9 pagesDaepoch Protocolo BccancerLuiz MeloNo ratings yet
- (Grade 9) MAPEH (Health) - Drugs (2nd)Document3 pages(Grade 9) MAPEH (Health) - Drugs (2nd)KenNo ratings yet
- Congestive Heart Failure 2022Document79 pagesCongestive Heart Failure 2022sara rababah100% (1)
- About DapagliflozinDocument6 pagesAbout DapagliflozinUjjval GandhiNo ratings yet
- Pathology of Female Reproductive SystemDocument33 pagesPathology of Female Reproductive SystemDio Reynaldi SusantoNo ratings yet
- Others Districts Others Districts Others Districts Others DistrictsDocument6 pagesOthers Districts Others Districts Others Districts Others DistrictsThulasiraman AshokkumarNo ratings yet
- Biology 12 Unit 9 Assignment 2 Blood Type and Immune Response Virtual LabDocument2 pagesBiology 12 Unit 9 Assignment 2 Blood Type and Immune Response Virtual Labapi-3385788740% (1)
- Phlebotomy Procedure 3rd PDFDocument4 pagesPhlebotomy Procedure 3rd PDFFranciska Gledy AmbaritaNo ratings yet
- NHM Letter World Diabetes DayDocument9 pagesNHM Letter World Diabetes DayAnonymous RCDcVGlFpzNo ratings yet
- Andrew Solomon Case Study - EditedDocument5 pagesAndrew Solomon Case Study - EditedJefferson KagiriNo ratings yet
- Invasive Cervical Traction Gardner Wells TongsDocument3 pagesInvasive Cervical Traction Gardner Wells TongsErvan Hartanto ErvanNo ratings yet
- Subject: - Topics: Cholecystitis: Adult Health NursingDocument17 pagesSubject: - Topics: Cholecystitis: Adult Health NursingUzma KhanNo ratings yet
- Sindh Rescue 1122 Test Sample PapersDocument12 pagesSindh Rescue 1122 Test Sample PapersMAANJONY100% (1)
- Choledochal CystDocument68 pagesCholedochal CystSyed Waqas HasanNo ratings yet
- Community Outreach ProgramsDocument5 pagesCommunity Outreach ProgramskaranreguNo ratings yet
- Implementation of The Filmarray Me Panel in Laboratory Routine Using A Simple Sample Selection Strategy For Diagnosis of Meningitis and EncephalitisDocument9 pagesImplementation of The Filmarray Me Panel in Laboratory Routine Using A Simple Sample Selection Strategy For Diagnosis of Meningitis and EncephalitisMohinish SNo ratings yet
- Early clinical exposure in the Neonatology unitDocument17 pagesEarly clinical exposure in the Neonatology unitPentolNo ratings yet
- Rehabilitation Medicine Standards to Protect PatientsDocument13 pagesRehabilitation Medicine Standards to Protect PatientsCobi EstacioNo ratings yet
- DM CasesDocument8 pagesDM CasesMelekNo ratings yet
- Lecture-31 Instrumental DeliveryDocument33 pagesLecture-31 Instrumental DeliveryMadhu Sudhan PandeyaNo ratings yet
- Ischialgia Case Report by GaluhDocument22 pagesIschialgia Case Report by GaluhDwi Ulfa AnnisaNo ratings yet
- Acetaminophen Suppository Mechanism of Action Side Effects Nursing ResponsibilitiesDocument2 pagesAcetaminophen Suppository Mechanism of Action Side Effects Nursing ResponsibilitiesNiziu BearsNo ratings yet
- The Benefits of ChocolateDocument2 pagesThe Benefits of ChocolateHanna FairussaniaNo ratings yet
- Revisiting Diuretic Choice in Chronic Kidney.4Document8 pagesRevisiting Diuretic Choice in Chronic Kidney.4FABIO JAVIER BRAVO SALDARRIAGANo ratings yet
- HA Integument ChecklistDocument10 pagesHA Integument ChecklistMa Joanna Elizabeth S. PizarroNo ratings yet
- Cannabinoids and Cancer - Abrams and GuzmanDocument8 pagesCannabinoids and Cancer - Abrams and GuzmanprojectcbdNo ratings yet
- Nicotine Withdrawal SymptomsDocument6 pagesNicotine Withdrawal SymptomsNo OneNo ratings yet