Professional Documents
Culture Documents
Emergency Treatment of Dentoalveolar Trauma
Emergency Treatment of Dentoalveolar Trauma
Uploaded by
GeraldineCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emergency Treatment of Dentoalveolar Trauma
Emergency Treatment of Dentoalveolar Trauma
Uploaded by
GeraldineCopyright:
Available Formats
The Physician and Sportsmedicine
ISSN: 0091-3847 (Print) 2326-3660 (Online) Journal homepage: https://www.tandfonline.com/loi/ipsm20
Emergency Treatment of Dentoalveolar Trauma
Essential Tips for Treating Active Patients
Kenneth A. Honsik, Kimberly G. Harmon (Practice Essentials Series Editor) &
Aaron Rubin (Practice Essentials Series Editor)
To cite this article: Kenneth A. Honsik, Kimberly G. Harmon (Practice Essentials Series Editor)
& Aaron Rubin (Practice Essentials Series Editor) (2004) Emergency Treatment of Dentoalveolar
Trauma, The Physician and Sportsmedicine, 32:9, 23-29, DOI: 10.1080/00913847.2004.11440732
To link to this article: https://doi.org/10.1080/00913847.2004.11440732
Published online: 19 Jun 2015.
Submit your article to this journal
Article views: 32
View related articles
Citing articles: 1 View citing articles
Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=ipsm20
PRACTICE
ESSENTIALS
Emergency Treatment of
Dentoalveolar Trauma
Essential Tips for Treating Active Patients
Kenneth A. Honsik, MD
For CME credit,
Practice Essentials Series Editors: see page 47
Kimberly G. Harmon, MD; Aaron Rubin, MD
II: I: liiIJaDentoalveolar tramna b;~ports is common. One third of dental injuries in the United
States occur in sports-related activities, so team physicians should be able to recognize and
properly treat dental injuries on the field. Tooth fracture, luxation, avulsion, and socket injury
are the main types of dentoalveolar tramna. In many cases, other maxillofacial tramna can be
associated with dental injuries, so physicians who examine these patients should be aware of
additional associated injuries. Tooth injury is often preventable with the appropriate use of
properly fitted mouth guards. Physicians should be familiar with different types and be able to
suggest the correct mouth guard for a given activity.
ental injuries on the athletic
D field are common and can have
serious negative consequences
for an athlete. Prevention is the
key, but proper immediate treatment is
essential. Most athletes have some basic
medical insurance; however, not all ath-
letes have dental insurance. Costs for
improperly treated dental injuries can be
sizable and can also have much higher
complication rates and poor cosmetic results. On-field (CDC) in 2001 estimated that approximately one third
sports medicine providers can diminish poor out- of all dental injuries in the United States are sports
comes through appropriate initial treatment and edu- related.' Studies from other countries provide valuable
cate athletes, parents, and coaches about proper statistics on frequency and type of dental injury. For
prevention. example, one large study' examined maxillofacial
The Centers for Disease Control and Prevention trauma in patients registered in the Department of
Maxillofacial Surgery at the University of Innsbruck,
Austria, from 1991 and 2000. Of the 9,543 patients seen
For author disclosure of financial relationships and mention of
unlabeled use of drugs, see the next page. during that time for maxillofacial trauma, 2,991 (31%)
of those injuries were sports related. Dentoalveolar
continued
THE PHYSICIAN AND SPOATSMEDICINE e Vol 32 • No. 9 • September 2004 23
PRACTICE
ESSENTIALS
Dentaoalveolar trauma
continued
trauma occurred in 51% of all maxillofacial trauma, odontalligaments and is covered by cementum. The
and 56% of the dentoalveolar injuries were compli- root houses the vascular pulp, which furnishes the
cated by associated injuries.' Such data are useful in blood and nerve supply for the tooth. The crown is
predicting the prevalence of dental trauma in collision made up of a tough outer shell of enamel that protects
or contact sports, such as skiing, soccer, cycling, an inner layer of dentin and the portion of the pulp
mountain biking, ice hockey, and ball sports, among that extends into crown. The border at which the
many others. crown meets the root is known as the cementoenamel
junction.' The gingival tissue overlies the mandible
Basic Dental Anatomy and maxilla and seals the tooth in the socket.
Teeth are housed within maxillary and mandibular
alveolar bone (figure 1), which contains individual Common Dental Injuries
sockets for each tooth. Each tooth consists of a root Dental injuries include fractures, luxation, avulsion,
and crown. The root attaches to the socket via peri- socket fracture, and associated trauma (eg, lip and
mucosal lacerations, maxillary or mandibular frac-
tures, temporomandibular joint damage, and concus-
Figures 1, 3: Medical Art Services, Inc. sion). Physicians must recognize each injury type to
provide proper initial treatment and refer more seri-
ously injured patients to the emergency department,
team dentist, or other dental professional.
Fractures. Tooth fractures disrupt the enamel or
cementum and may involve dentin or pulp. They are
typically caused by a direct blow to the tooth or by an
indirect blow transmitted through the jaw.' Fractures
can affect the root, crown, or both, producing a wide
range of severity. Fractures can be as simple as a
chipped tooth, which only involves the enamel, as well
as the other extreme, a vertical fracture, which cleaves
the tooth from the crown through the root, involving
enamel, dentin, and pulp along the fissure. When the
pulp is involved, the injury is usually very painful and is
frequently identified as a bleeding site or a pinkish dot
in the center of the dentin (figure 2) ."·'" Treatment and
return to play varies with the severity of the fracture.
Crown fractures are commonly classified into one
of four types (figure 3):
• Type 1 is an enamel only or "chip fracture";
• Type 2 is a fracture through enamel and dentin;
FIGURE 1. Anatomy of a normal tooth shows its position in the • Type 3 involves the enamel, dentin, and pulp; and
jaw. All teeth have an enamel crown that covers the dentin and • Type 4 fractures involve the root.
pulp cavity. The gingival tissue seals the tooth into its socket. The closer a root fracture is to the cementoenamel
Dr Honsik is astaff physician in the department of family practice and on the Fontana, CA 92335; e-mail to kenneth.a.honsik@kp.org.
faculty of the Sports Medicine Fellowship program at Kaiser Permanente in Disclosure information: Dr Honsik discloses no significant relationship
Fontana. California. with any manufacturer of any commercial product mentioned in this article.
Address correspondence to: Kenneth A. Honsik, MD, 9985 Sierra Ave. No drug is mentioned in this article for an unlabeled use.
24 Vol 32 • No. 9 • September 2004 e THE PHYSICIAN AND SPORTSMEDICINE
PRACTICE
ESSENTIALS
Dentaoalveolar trauma
continued
Figures 2,4,5: Courtesy of Marf< Roettger, DDS
FIGURE 2. A fracture can be as simple as a chip in the enamel or FIGURE 3. Type 1, type 2, and type 3 fractures involve the tooth
as serious as involving the pulp chamber (arrow). crown. Type 4 fractures involve the root and require immediate
care by a dentist.
junction, the more unstable it is and the poorer the by bone and the tooth will be lost.
prognosis.' Dental injuries that involve the root and The need for endodontic (root canal) therapy fol-
pulp are considered more severe and require immedi- lowing the proper reirnplantation of an avulsed tooth
ate professional attention. is determined by the maturity of the root at the time of
Luxation. Luxation is the displacement of the tooth injury. A mature root has a closed apex, and this makes
from its normal position (figure 4). Teeth may become revascularization of the dental pulp impossible and
laterally luxated, extruded, or intruded. A laterally lux- always requires endodontic therapy. An immature root
ated tooth will be displaced anterior or posterior to the has an open apex and allows for a chance of revascu-
adjacent teeth. If the tooth is extruded, it will appear larization following reirnplantation, possibly avoiding
longer than the other teeth in the arch (partial avul- endodontic therapy. Only permanent teeth should be
sion). In cases of intrusion, the tooth will be shorter reirnplanted. Primary or "baby teeth" should never be
than its neighboring row and should not be reposi- reirnplanted. n•
tioned on site. Intrusion typically involves disruption Associated injuries. All of the previously described
of the alveolar socket and periodontal ligaments.'·" injuries can be associated with other types of maxillo-
Loose teeth are considered tooth subluxations without facial trauma. In the previously noted study 2 from Aus-
significant displacement or alveolar bone disruption. tria, 56% of dentoalveolar injuries were complicated by
However, in some cases, a "loose tooth" may be the other injuries. Associated maxillofacial injuries can be
result of a transverse root or cementoenamel junction as simple as a gum or lip laceration to as serious as a
fracture. Radiographs are recommended for all concussion, temporomandibular joint damage, or
trauma-induced loose teeth. facial or alveolar bone fracture. The examiner should
Avulsion. Tooth avulsion is a total separation of the always look for these injuries when evaluating an
tooth from the socket (figure 5). This injury involves active patient for dentoalveolar trauma. lip or mouth
complete rupture of the periodontal ligaments. As lacerations should be radiographed before closure to
such, the time from injury to reimplantation of the rule out embedded tooth or bone fragments when
tooth is critical to its survival. Vitality of the periodontal these injuries are associated with a tooth fracture.'
ligament (PDL) cells on the root surface of an avulsed
tooth will determine whether the PDL will regenerate Patient Examination
or if the root will ankylose to the bone. If ankylosis Because of the high velocity forces involved in den-
occurs, the root of the tooth will ultimately be replaced toalveolar trauma, the provider should always begin
continued
THE PHYSICIAN AND SPORTSMEDICINE e Vol 32 • No. 9 • September 2004 25
PRACTICE
ESSENTIALS
Dentaoalveolar trauma
continued
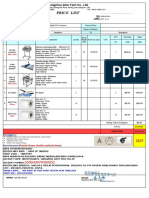
Crown Injury {Type 1-2) Lateral Luxation
Exam Findings Exam Findings
Exposed dentin has yellow hue; presence of pink dot or Tooth may look out of place or feel loose; athlete may complain
bleeding in center of tooth signals pulp involvement; pain of problem with bite; palpation of the alveolar socket may reveal
may occur with or without sensitivity to cold water and air deformity or fracture
Emergency Care Emergency Care
• Recover fragments • Determine the number of teeth affected and the stability of the row
• Handle only by enamel surface • Gently reposition tooth or teeth into original position with a dry,
• Control bleeding gloved handt
• Rinse tooth gently with sterile saline or clean water, if soiled • If repositioning is too painful or not attainable, refer patient
• Transport fragments in saline soaked sterile gauze to a dental professional at once
Treatment • If repositioning is successful, athletes should follow a strict
• Patient may be referred to dentist within 48 hr if only soft food and liquid diet that avoids excessive biting and chewing
enamel or dentin is involved • Consider splinting
• Reconstruction of tooth or fillings Treatment
Return-to-Play Guidelines • If the tooth was significantly displaced, alveolar fracture is
May return immediately if bleeding is controlled and athlete highly probable, and athlete should seek immediate dental care
has a properly fitting mouth guard; patient should have a • If the tooth was minimally displaced or loose, the patient
dental consultation within 48 hr should seek dental consult within 1 day
• Radiographs are usually done
Crown Injury {Type 3) • Endodontic therapy (root canal) possible
Exam Findings Return-to-Play Guidelines
More commonly have severe pain If athlete has a custom mouth guard, immediate return to play
Emergency Care may be considered;* return to play is not recommended for
May place a drop of medical grade cyanoacrylate on exposed athletes without custom mouth guards or if severe alveolar
pulp to decrease risk of infection and reduce pain of exposed nerve injury is suspected. Return to play after dental consult depends
Treatment on recommendations of the team dentist.
• Refer to dentist within 3 hr; pulpitis may arise from bacterial
contamination of sterile pulp space
• Prophylactic antibiotics are recommended; tetanus booster if Extruded Luxation
needed
Exam Findings
• Root canal therapy is done by dental professional Tooth appears longer than adjacent teeth; palpate the entire tooth
Return-to-Play Guidelines row and alveolar sockets; injury may or may not be painful and
Immediate return to play is not recommended;* eventual return to disrupts blood and nerve supply at insertion of root
play determined by dental provider Emergency Care
• Instruct patient to bite down on gauze or mouth guard to
Root Injury {Type 4) assist repositioning the tooth in the sockett
Exam Findings Treatment
Tooth may or may not be loose; can be painless, very painful, • Dental consult within 24 hr of injury if teeth have been
or numb repositioned or immediately if acceptable alignment is not
Emergency Care achieved
• Tooth should be secured to adjacent teeth in row with an • Obtain x-rays to detect possible fracture
improvised splint, such as a mouth guard, dental wire, or • The tooth will require splinting, and endodontic or root
sugar-free gum canal therapy may be needed
Treatment Return-to-Play Guidelines
• All suspected root fractures require x-rays Return to play is not recommended for athletes without
• Patient should seek dental consult immediately after injury custom mouth guards; return to play after dental consult
Return-to-Play Guidelines depends on recommendations of the dental professional.
Immediate return to play is not recommended;* eventual Athletes with custom mouth guards may consider immediate
return to play determined by dental provider return to play if tooth is acceptably repositioned.*
• Adult athletes (> 18 years old) may make an informed decision on return to play, as long as they understand the risks and potential complications.
t Sideline providers with experience in administering dental anesthesia may consider doing so before manipulating teeth.
TMJ =temporomandibular joint
26 Vol 32 • No. 9 • September 2004 e THE PHYSICIAN AND SPORTSMEDICINE
PRACTICE
ESSENTIALS
Dentaoalveolar trauma
continued
Intruded Luxation Alveolar Fracture
Exam Findings Exam Findings
Severe pain likely; tooth appears shorter than adjacent teeth Pain likely present; detected with careful palpation of sockets
in row; typically involves severe injury to alveolar socket, and gum line
periodontal ligaments, and underlying marrow Emergency Care
Emergency Care • If fracture is suspected, do not replace avulsed tooth
• Do not reposition on field • Do not attempt to reduce displaced alveolar fragments
• May be associated with significant alveolar fracture on the field
Treatment Treatment
• Immediate consultation with dental professional •Refer to a dentist immediately
• Tooth may re-erupt or be guided back into place with Return-to-Play Guidelines
orthodontic care Immediate return to play is not recommended;* eventual
Return-to-Play Guidelines return is determined by dental provider
• Immediate return to play is not recommended;* eventual
return to play is determined by dental provider
• Root canal therapy possible
Other Injuries (Lacerations, concussion, facial bone fractures,
and TMJ trauma)
Avulsion Exam Findings
Bleeding, facial asymmetry, abnormal extraocular eye
Exam Findings movement, abnormal bite alignment, altered mental status
Tooth knocked out of socket; associated pain
Emergency Care
Emergency Care • Control bleeding with pressure
• Find the missing tooth • Stabilize suspected fractures and transport patient to
• Control bleeding emergency department
• Rinse tooth with sterile or clean water • Follow standard concussion guidelines
• Do not scrub tooth or handle by the root
• Primary goal is to replace the tooth immediately if alveolar Treatment
socket fracture is not present • Lacerations may be repaired if no obvious displaced tooth
• Do not replace primary ("baby") teeth fragments are present
• Press tooth firmly back into socket, but make certain that • Delay repair if tooth fragments might be embedded in oral
the tooth is correctly positioned mucosa
• Ensure proper positioning; provider should feel palpable • X-ray injury to detect any fragments
click when tooth is properly seated Return-to-Play Guidelines
• If successful on-field implantation occurs, the tooth must Fractures and severe concussions take priority over dental
be temporarily splinted to the adjacent stable teeth trauma and require immediate transport to an emergency
• Splints may be improvised (eg, mouth guards, sugar-free gum) department
Treatment
• Requires immediate dental consultation;
• If on-field rei mplantation is unsuccessful, transport the
athlete and tooth to a qualified provider or dentist for
rei mplantation within 30 min to 2 hr; after 2 hr tooth has
low likelihood of survival or successful rei mplantation
Return-to-Play Guidelines
Immediate return to play not recommended;* eventual
return to be determined by the dental provider
THE PHYSICIAN AND SPORTSMEDICINE e Vol 32 • No. 9 • September 2004 27
PRACTICE
ESSENTIALS
Dentaoalveolar trauma
continued
FIGURE 4. A laterally displaced tooth (luxation). Extruded and FIGURE 5. The site of an avulsed tooth. An avulsed tooth should
laterally displaced teeth should be returned to their proper position be re implanted within 30 minutes to 2 hours. Implantation after
if possible, but intruded teeth should not be repositioned on site. 2 hours greatly decreases the chance for tooth survival.
the exam with the ABCs of trauma (airway, breathing. Currently, three types of mouth guards are available
circulation, and consciousness/alertness). It is ex- to athletes: stock, mouth-formed ("boil-and-bite"},
tremely important to determine alertness because of and custom-fabricated (figure 6; also see the Patient
increased risk of tooth fragment aspiration in con- Adviser, "Steps to Take for Dental Injuries," page 35).
cussed or unconscious athlete. Using a light source, The stock mouth guard comes in set sizes and is the
physicians should visually inspect the entire mouth least protective type. They are commonly trimmed
and maxillofacial region. The athlete's mouth may need down by the athletes for comfort and held in place by
to be rinsed for proper inspection. When doing this, use the bite force of the athlete. Boil-and-bite mouth
clean water for rinsing, and do not discard the rinse guards are the most commonly worn and marketed
immediately to allow inspection for tooth fragments or types but provide only mediocre protection. The boil-
teeth before disposal! If a fracture or avulsion is seen on and-bite mouth guard loses much of its protective
examination and the fragment or missing tooth is not properties during the form-fitting process. An overall
visible within the mouth, the athlete's clothes and site thickness of 3 mm is required for adequate cushion
of injury should be searched immediately. and absorption. Many times the athlete will bite too far
After completing the visual inspection, the provider through the mouth guard during the forming process,
should then palpate all teeth in both arches with a reducing the cushion between the teeth. Also through-
sterile, gloved hand, checking for asymmetry, loose- out the season, athletes will chew through portions of
ness, or mandibular and maxillary deformities. Exami- the mouth guard, further reducing the cushion and
nation procedures, treatment recommendations, and rendering it ineffective.'' Custom mouth guards are
return-to-play guidelines depend on the type of injury recommended by sports physicians and dental profes-
incurred (table 1).'""" sionals. They are significantly more expensive than
over-the-counter types but have been proven to pro-
Preventing Dentoalveolar Injury vide superior protection."·"
The American Dental Association recommends use Custom mouth guards are made by a dentist for an
of mouth guards for participation in football, gymnas- exact fit and are fashioned from a mold or cast of the
tics, basketball, boxing, field hockey, handball, ice patient's mouth. Custom mouth guards may be pro-
hockey, lacrosse, skateboarding, skiing, skydiving, duced by either a vacuum or pressure-lamination pro-
soccer, martial arts, racquetball, squash, roller hockey, cess. The pressure laminate variety is felt to be slightly
rugby, volleyball, water polo, weightlifting, and superior to the vacuum form, because the multiple lay-
wrestling. Mouth guard use has been shown to ers ensure adequate thickness of the device. These
decrease the frequency and severity of dental injuries.' 11 mouth guards may also be further customized by mak-
28 Vol 32 • No. 9 • September 2004 e THE PHYSICIAN AND SPORTSMIDICINE
PRACTICE
ESSENTIALS
Dentaoalveolar trauma
continued
Figures 6 A, B: staff photos; Figures 6 C, 0: Courtesy of Ray Pad ilia, DOS
FIGURE 6. Three basic types of mouth guards are available. Stock (not shown), mouth-formed {"boil-and-bite," A, B), and custom (C,D)
mouth guards provide different levels of protection. Custom mouth guards are expensive, but their form lit provides the greatest protection.
Mouth-formed types are relatively easy to produce, but they may be chewed through and lose their protective qualities.
ing them in the school or team colors (figure 6D}. Much be familiar and comfortable with basic diagnosis and
discussion has centered on the question of whether emergency care for dental injuries. Care for more seri-
mouth guards aid in preventing concussions. To date, ous injuries should be supplied by team dentists or
there is no evidence that mouth guard use decreases other dental providers. If treated correctly on the field,
the incidence of concussion among athletes. 10•13 injured patients can avoid complications such as poor
cosmesis, infection, and extensive dental reconstruc-
Putting the Bite on Dental Injury tion. Use of a properly fitted mouth guard is effective
Dental injuries are very common in most contact in preventing dental injury; with custom types provid-
and collision sports. Sports medicine providers should ing the best protection. '"·' 2 PSM
REFERENCES Am Fam Physician 2003;67(3) :511-516
l. Promoting oral health: interventions for preventing dental 8. International Association of Dental Traumatology: Treat-
caries, oral and pharyngeal cancers, and sports-related ment Guidelines. Available at http://www.iadt-dental-
craniofacial injuries: a report on recommendations of the trauma.org/Trauma/ dental_trauma.htm. Accessed June
Task Force on Community Preventive Services. MMWR. 24,2004
Morb Mortal Wkly Rep 2001;50(RR 21): 1-13 9. Sports Dentistry Online: Sports dentistry facts. Available at
2. Thli T, Hachl 0. Hohlrieder M, et al: Dentofacial trauma in http://www.sportsdentistry.com/facts.htrnl. Accessed June
sports accidents. Gen Dent 2002;50(3):274-279 24,2004
3. Wisniewski JF: Chapter 60: Dental injuries, in: Safran MR, 10. Labella CR, Smith BW, Sigurdsson A: Effect of mouthguards
McKeag DB, Van Camp SP (eds): Manual of Sports Medi- on dental injuries and concussions in college basketball.
cine. Philadelphia, Lippincott-Raven, 1998, pp 500-505 Med Sci Sports Exerc 2002;34(1):41-44
4. Honsik K: Dental injuries, in Rubin A: Sports Injuries and 11. Sports Dentistry Online: Types of athletic mouthguards.
Emergencies: A Quick Response Manual. New York City, Available at www.sportsdentistry.com/mouthguards.htrnl.
McGraw-Hill, 2003, pp 54-59 Accessed June 24, 2004
5. Roberts WO: Field care of the injured tooth. Phys Sports- 12. Newsome PR, Iran DC, Cooke MS: The role of the mouth-
med 2000;28(1):101-102 guard in the prevention of sports-related dental injuries: a
6. Dale RA: Dentoalveolar trauma. Emerg Med Clin North Am review. Int J Paediatr Dent 200 1; 11(6):396-404
2000;18(3):521-538 13. McCrory P: Do mouthguards prevent concussions? Br J
7. Douglass AB, Douglass JM: Common dental emergencies. Sports Med 2000;35(2):81-82
THE PHYSICIAN AND SPORTSMEDICINE e Vol 32 • No. 9 • September 2004 29
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5808)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- History of TandoorDocument3 pagesHistory of Tandoorpiyush100% (2)
- SsangYong Actyon Sports Q149 2011.01 Electrical Wiring DiagramDocument84 pagesSsangYong Actyon Sports Q149 2011.01 Electrical Wiring Diagramcelyoz100% (1)
- Top 25 Food Ideas For Baby Led Weaning: VegetablesDocument1 pageTop 25 Food Ideas For Baby Led Weaning: Vegetablesbecca wiseNo ratings yet
- Reading Questions - Science and BeautyDocument3 pagesReading Questions - Science and BeautyEllen Lam100% (1)
- Price List: With StandDocument1 pagePrice List: With StandAlex TajoNo ratings yet
- The Waves of The Technological InnovationsDocument17 pagesThe Waves of The Technological InnovationsRio AwitinNo ratings yet
- XH260L - XH260V: Dixell Operating InstructionsDocument4 pagesXH260L - XH260V: Dixell Operating InstructionsJennifer Eszter SárközyNo ratings yet
- Download full chapter The First Institutional Spheres In Human Societies Evolutionary Analysis In The Social Sciences 1St Edition Abrutyn pdf docxDocument54 pagesDownload full chapter The First Institutional Spheres In Human Societies Evolutionary Analysis In The Social Sciences 1St Edition Abrutyn pdf docxmarcus.stassinos948No ratings yet
- Use of Stainless Steel CrownsDocument16 pagesUse of Stainless Steel CrownsKaren De la GarzaNo ratings yet
- H BridgeDocument41 pagesH BridgeSheikh IsmailNo ratings yet
- HDES-D0165 General Tolerance in Dimension (Eng)Document1 pageHDES-D0165 General Tolerance in Dimension (Eng)juniorferrari06No ratings yet
- Gear Hobbing Shaping and Shaving A Guide To Cycle Time Estimating and Process Planning PDFDocument183 pagesGear Hobbing Shaping and Shaving A Guide To Cycle Time Estimating and Process Planning PDFvenkat100% (2)
- Vision Document (Template)Document5 pagesVision Document (Template)Andrew MacAulayNo ratings yet
- E SHB 2009 - Vav3Document169 pagesE SHB 2009 - Vav3ictgisNo ratings yet
- Summer Training Finance Project On WORKING CAPITAL MANAGEMENTDocument82 pagesSummer Training Finance Project On WORKING CAPITAL MANAGEMENTPravin chavda100% (2)
- Apxv9r20b C A20 PDFDocument2 pagesApxv9r20b C A20 PDFКонстантин ПетровNo ratings yet
- 8902 LS (Parker)Document20 pages8902 LS (Parker)abdohalim248No ratings yet
- Carbohydrates: MonosaccharidesDocument8 pagesCarbohydrates: MonosaccharidesLily NemphisNo ratings yet
- Non-Mendelian InheritanceDocument12 pagesNon-Mendelian InheritanceBillones Rebalde MarnelleNo ratings yet
- Soal PTS B Inggris 5Document8 pagesSoal PTS B Inggris 5Hasna NurlailiNo ratings yet
- Teens 2 - Resource PackDocument14 pagesTeens 2 - Resource PackGigliane SouzaNo ratings yet
- ArthritisDocument5 pagesArthritismeenuNo ratings yet
- Microprocessor 4th SemDocument316 pagesMicroprocessor 4th SemDaggupatiHarishNo ratings yet
- Critical ResultDocument2 pagesCritical ResultSUSANTONo ratings yet
- Pasler Dufourt PNM2011Document34 pagesPasler Dufourt PNM2011balintkNo ratings yet
- Kode Icd 10Document38 pagesKode Icd 10interna squardNo ratings yet
- Introduction To Biopotential Measurement and Excitation: (Bioelectromagnetism - Jakko Malmivuo, Robert Plonsey)Document23 pagesIntroduction To Biopotential Measurement and Excitation: (Bioelectromagnetism - Jakko Malmivuo, Robert Plonsey)Lynn WankharNo ratings yet
- Redox Reactions: Neet /jee QuestionsDocument27 pagesRedox Reactions: Neet /jee QuestionsAsher LaurierNo ratings yet
- Kothari Sugar Factory Internshipproject SamoleDocument52 pagesKothari Sugar Factory Internshipproject Samolenoobwarrior3No ratings yet
- Identification Tables For Common Minerals in Thin SectionDocument4 pagesIdentification Tables For Common Minerals in Thin SectionTanmay KeluskarNo ratings yet