Professional Documents
Culture Documents
PIIS2665991320301648
Uploaded by
wedib17801Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PIIS2665991320301648
Uploaded by
wedib17801Copyright:
Available Formats
Articles
Anakinra for severe forms of COVID-19: a cohort study
Thomas Huet, Hélène Beaussier, Olivier Voisin, Stéphane Jouveshomme, Gaëlle Dauriat, Isabelle Lazareth, Emmanuelle Sacco,
Jean-Marc Naccache, Yvonnick Bézie, Sophie Laplanche, Alice Le Berre, Jérôme Le Pavec, Sergio Salmeron, Joseph Emmerich, Jean-Jacques Mourad,
Gilles Chatellier, Gilles Hayem
Summary
Background Coronaviruses can induce the production of interleukin (IL)-1β, IL-6, tumour necrosis factor, and other Lancet Rheumatol 2020
cytokines implicated in autoinflammatory disorders. It has been postulated that anakinra, a recombinant IL-1 receptor Published Online
antagonist, might help to neutralise the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-related May 29, 2020
https://doi.org/10.1016/
hyperinflammatory state, which is considered to be one cause of acute respiratory distress among patients with
S2665-9913(20)30164-8
COVID-19. We aimed to assess the off-label use of anakinra in patients who were admitted to hospital for severe
See Online/Comment
forms of COVID-19 with symptoms indicative of worsening respiratory function. https://doi.org/10.1016/
S2665-9913(20)30165-X
Methods The Ana-COVID study included a prospective cohort from Groupe Hospitalier Paris Saint-Joseph (Paris, For a French translation of the
France) and a historical control cohort retrospectively selected from the Groupe Hospitalier Paris Saint-Joseph abstract see Online for appendix
COVID cohort, which began on March 18, 2020. Patients were included in the prospective cohort if they were aged Rheumatology Department
18 years or older and admitted to Groupe Hospitalier Paris Saint-Joseph with severe COVID-19-related bilateral (T Huet MD, G Hayem MD),
Clinical Research Centre
pneumonia on chest x-ray or lung CT scan. The other inclusion criteria were either laboratory-confirmed SARS-CoV-2 (H Beaussier Pharm D,
or typical lung infiltrates on a lung CT scan, and either an oxygen saturation of 93% or less under oxygen 6 L/min or E Sacco PhD), Internal Medicine
more, or aggravation (saturation ≤93% under oxygen 3 L/min) with a loss of 3% of oxygen saturation in ambient air Department (O Voisin MD,
over the previous 24 h. The historical control group of patients had the same inclusion criteria. Patients in the Prof J-J Mourad MD),
Pulmonology Department
anakinra group were treated with subcutaneous anakinra (100 mg twice a day for 72 h, then 100 mg daily for 7 days) (S Jouveshomme MD,
as well as the standard treatments at the institution at the time. Patients in the historical group received standard J-M Naccache MD,
treatments and supportive care. The main outcome was a composite of either admission to the intensive care unit S Salmeron MD), Vascular
(ICU) for invasive mechanical ventilation or death.The main analysis was done on an intention-to-treat basis Medicine Department
(I Lazareth MD,
(including all patients in the anakinra group who received at least one injection of anakinra). Prof J Emmerich MD), Pharmacy
Department (Y Bézie Pharm D),
Findings From March 24 to April 6, 2020, 52 consecutive patients were included in the anakinra group and 44 historical Biochemistry and Microbiology
patients were identified in the Groupe Hospitalier Paris Saint-Joseph COVID cohort study. Admission to the ICU for Department
(S Laplanche Pharm D),
invasive mechanical ventilation or death occurred in 13 (25%) patients in the anakinra group and 32 (73%) patients in Radiology Department
the historical group (hazard ratio [HR] 0·22 [95% CI 0·11–0·41; p<0·0001). The treatment effect of anakinra remained (A Le Berre MD), Hôpital Paris
significant in the multivariate analysis (HR 0·22 [95% CI 0·10–0·49]; p=0·0002). An increase in liver aminotransferases Saint-Joseph, Paris, France;
occurred in seven (13%) patients in the anakinra group and four (9%) patients in the historical group. Division of Lung
Transplantation and Thoracic
Surgery, Hôpital Marie
Interpretation Anakinra reduced both need for invasive mechanical ventilation in the ICU and mortality among patients Lannelongue, Le Plessis-
with severe forms of COVID-19, without serious side-effects. Confirmation of efficacy will require controlled trials. Robinson, France
(G Dauriat MD, J Le Pavec MD);
Université de Paris, INSERM
Funding Groupe Hospitalier Paris Saint-Joseph. 1153-CRESS, Paris, France
(Prof J Emmerich); and
Copyright © 2020 Elsevier Ltd. All rights reserved. Assistance Publique—Hôpitaux
de Paris, Hôpital Européen
Georges-Pompidou, Université
Introduction of SARS-CoV-2 infection includes hyperinflammation de Paris, CIC 14-18 INSERM,
The outbreak of COVID-19, due to severe acute respiratory that resembles cytokine storm syndromes (eg, secondary Paris, France
syndrome coronavirus 2 (SARS-CoV-2), began in Wuhan, haemophagocytic lymphohistiocytosis or macrophage (Prof G Chatellier MD)
Hubei Province, China, and has subsequently spread all activation syndrome), involving pro-inflammatory inter Correspondence to:
Dr Gilles Hayem, Rheumatology
over the world. Up to 30% of patients admitted to hospital leukins (IL-1β and IL-6) and tumour necrosis factor.3,4
Department, Hôpital Paris Saint-
with COVID-19 need admission to intensive care units SARS-CoV-2 is thought to bind to toll-like receptors, which Joseph, 75014 Paris, France
(ICUs) to receive ventilation assistance because they activate the inflammasome and the cleavage of pro-IL-1β ghayem@hpsj.fr
develop acute respiratory distress syndrome (ARDS).1–3 So by caspase-1, followed by the production of active mature
far, no specific treatment has shown efficacy in preventing IL-1β, a mediator of fever, lung inflamma tion, and
worsening of respiratory symptoms in patients admitted fibrosis.5 Coronaviruses encode viroporins, which facilitate
to hospital for COVID-19-associated pneumonia requir viral dissemination through their interaction with cellular
ing oxygen therapy. Finding such a treatment is a public ion channels. Additionally, the viroporins E and open
health emergency. reading frame 3a can induce transcription of the gene
Similarly to other types or coronaviruses (eg, Middle encoding pro-IL-1β and secretion of IL-1β by activation of
East respiratory syndrome coronavirus), the pathogenesis the NLRP3 inflammasome.6,7
www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8 1
Articles
Research in context
Evidence before this study of 100 mg twice daily for 3 days, then 100 mg daily for 7 days,
With more than 5 103 000 reported cases in the world as of we observed a significant reduction of mortality, along with a
May 23, 2020, the COVID-19 pandemic has become a major significant decrease in the need of mechanical invasive
cause of acute respiratory distress syndrome and mortality. ventilation, with no obvious adverse events, including
Analogy with previous outbreaks of other coronaviruses, bacterial infections.
combined with the accumulating evidence of the pivotal role of
Implications of all the available evidence
the inflammasome pathway in the life-threatening severe acute
Our data suggest that an in-depth evaluation of anakinra in
respiratory distress syndrome coronavirus 2-induced systemic
patients with an exacerbating form of COVID-19, mainly
disease, led us to consider interleukin-1 as a target of choice in
resulting from an otherwise uncontrolled cytokine storm,
this particular condition.
is warranted.
Added value of this study
In a cohort of patients with severe forms of COVID-19 who were
treated with anakinra, administered subcutaneously at a dose
Anakinra is a 17 kD recombinant, non-glycosylated Exclusion criteria were the refusal of the patient to
human IL-1 receptor antagonist with a short half-life of participate, patients who were bedridden and near the
about 3–4 h and good safety profile. After the approval end of life, patients with respiratory failure explained by
of the subcutaneous formulation to treat patients with an alternative aetiology, and patients already admitted to
rheumatoid arthritis, anakinra was found to have some the ICU.
beneficial effects in severe sepsis, but only in the subgroup The historical comparison group was identified retro
of patients with multiple organ dysfunction syndrome, spectively from the Groupe Hospitalier Paris Saint-Joseph
in which the inflammasome pathway is also involved.8 COVID cohort, which began on March 18, 2020, and
Similar positive results were reported in paediatric included all patients with a COVID-19-related disease. All
patients with secondary haemophagocytic lymphohistio historical patients had to fulfil the same inclusion and
cytosis or macrophage activation syndrome, including exclusion criteria as those of the anakinra group.
cases triggered by viral infection.8–10 The COVID cohort protocol has been approved by the
These data led us to hypothesise that anakinra could institutional ethics committee (institutional review board
represent an efficient treatment for severe forms of number IRB00012157, initial agreement 401) and regis
COVID-19, predominantly involving the inflammasome tered on the French National Institute of Health Data
pathway. Therefore, we aimed to assess the off-label use of platform (MR4810020420). All patients were given both
anakinra in patients who were admitted to hospital for oral and written information by their physician about
severe forms of COVID-19 with symptoms indicative of anakinra, and could either accept or refuse this treatment.
worsening respiratory function. Their choice was noted in the medical record. All patients
in both groups agreed to have their data used for research
Methods purposes. This study corresponds to an institutional off-
Study design and patients label drug evaluation. In this context, French research
We did a retrospective cohort study. The Ana-COVID regulation (Journal Officiel de la République Française
study included a prospective cohort of patients who [Official Journal of the French Republic] 0160, July 13, 2018;
received anakinra and a historical com parison group paragraph 110, MR-004) states that the patient’s written
who received standard care. Patients were included in the consent is not mandatory but investigators are required
prospective cohort if they were aged older than 18 years to give the patient an information leaflet explaining the
and admitted to Groupe Hospitalier Paris Saint-Joseph purpose of the research. The patients’ non-opposition to
with severe COVID-19-related bilateral pneumonia; were the use of their data for research was also collected in
diagnosed with SARS-CoV-2 infection confirmed by either accordance with European regulations (General Data
a positive result from an RT-PCR assay or a typical aspect Protection Regulation).
on CT scan of the lungs (multiple ground-glass abnormal
ities with crazy paving, absence of lymphadenopathy, and Procedures
pulmonary nodules); had bilateral lung infiltrates on a Patients in the anakinra group received subcutan
lung CT scan or chest x-ray; and had critical pulmonary eous anakinra (Swedish Orphan Biovitrum, Stockholm,
function defined by oxygen saturation of 93% or less Sweden) at a dose of 100 mg twice daily for 72 h, followed
under 6 L/min of oxygen or more or oxygen saturation of by 100 mg daily for 7 days, in addition to the standard
less than 93% on 3 L/min with a saturation on ambient air treatment administered at Groupe Hospitalier Paris Saint-
decreasing by 3% in the previous 24 h. Joseph at the time and supportive care. The dose of
2 www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8
Articles
anakinra was adapted to renal function and reduced to one was based mainly on age and comorbidities, along with
daily injection of 100 mg for 72 h, followed by an injection the opinion of the physician in charge of the patient,
every other day for the next 7 days, in patients under dialysis with the help of an ad hoc ethics committee.
or with a glomerular filtration rate of less than 30 mL/min. Chest CT was done with a single inspiratory phase
Patients in the historical group received the standard with patients in the supine position. Radiologists
treatments and supportive care. Standard treatments classified the CT as typical, equivocal, or negative for
in Groupe Hospitalier Paris Saint-Joseph at the time COVID-19 and described the main CT features: ground-
included oral hydroxychloroquine 600 mg/day for glass opacity, crazy-paving pattern, and consolidation. A
10 days, oral azithromycin 250 mg/day for 5 days, and semi-quantitative scoring system was used to estimate
parenteral β-lactam antibiotics (intravenous ceftriaxone 1 g the pulmonary involvement of all of these abnor
per day or intravenous amoxicillin 3 g per day) for 7 days, malities on the basis of the area involved: less than
in the absence of their respective contraindica tions. 25% (mild involvement); 25–50% (moderate involve
All patients received thromboembolic prophylaxis. No ment); 51–75% (severe involvement); or more than 75%
oral corticosteroids or vasopressors were used, but (diffuse involvement).11
some patients received an intravenous bolus of methyl
prednisolone (500 mg). Supportive care included low-flow Outcomes
oxygen therapy (≤6 L/min through low-flow nasal cannula) The main outcome was the composite of either need
or high-flow oxygen therapy (>6 L/min with high-flow for admission to the ICU with invasive mechanical ventila
nasal cannula or face mask). None of the patients had tion or death. The other outcomes were death, need for
invasive or non-invasive mechanical ventilation at baseline.
All data were extracted from our computerised medical
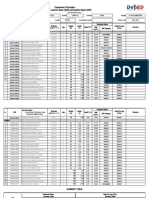
record (DxCare [version 12.2.0.1.0], Medasys, Le Plessis- Anakinra group Historical group p value
(n=52) (n=44)
Robinson, France) by two investigators (TH and GD)
independently. The data were reported into an electronic Age, years 71·0 (13·1) 71·1 (14·9) 0·97
case report form that is accessible via an internet browser, Age category ·· ·· 0·80
using personal accounts. Data were confidentially collec <50 years 2 (4%) 1 (2%) ··
ted and coded according to the local cohort statements 50–69 years 23 (44%) 22 (50%) ··
responding to all regulatory points in accordance with ≥70 years 27 (52%) 21 (48%) ··
French regulations (law 78-17 of Jan 6, 1978, relating Sex ·· ·· 0·21
to data processing, files, and freedoms) and European Male 36 (69%) 25 (57%) ··
General Data Protection Regulation regarding patient Female 16 (31%) 19 (43%) ··
information and confidential treatment of all data. The Body-mass index, kg/m² 25·5 (4·0) 29·0 (5·7) 0·0009
study design and data collection were approved by the Comorbidities ·· ·· ··
institutional review board. All data were monitored by a Hypertension 31 (60%) 29 (66%) 0·53
representative of Groupe Hospitalier Paris Saint-Joseph. Diabetes 14 (27%) 16 (36%) 0·32
The database was frozen for statistical analysis on Cardiopathy 9 (17%) 11 (25%) 0·36
April 11, 2020. The computerised file used for this Stroke 4 (8%) 7 (16%) 0·21
research was implemented in accordance with French Pulmonary disease* 8 (15%) 12 (27%) 0·15
regulations (law 78-17 of Jan 6, 1978, relating to data Number of comorbidities ≥2 vs 0–1 29 (56%) 20 (45%) 0·22
processing, files, and freedoms) and European General Not to be resuscitated 26 (50%) 20 (45%) 0·66
Data Protection Regulation. Positive swab RT-PCR† 36/41 (88%) 33/34 (97%) 0·14
Demographic and medical characteristics, including Chest CT ·· ·· 0·55
age, sex, body-mass index (BMI), hypertension, diabetes, Lung infiltrates <50% 31 (60%) 25/38 (66%)‡ ··
cardiopathy, stroke, asthma, emphysema, sleep apnoea, Lung infiltrates ≥50% 21 (40%) 13/38 (34%)‡ ··
chronic obstructive pulmonary disease, not to be resusci Duration of symptoms before inclusion, days 8·4 (4·3) 6·2 (3·6) 0·0088
tated status, the severity of the CT lung damage, and the Clinical inclusion parameters ·· ·· 0·076
value of the RT-PCR assay at the diagnosis, were rec SpO2 ≤93% under 6 L/min or more oxygen 42 (81%) 41 (93%) ··
orded from the medical charts. Clinical manifestations, therapy
including persistent fever above 38°C, respiratory rate, SpO2 ≤93% under 3 L/min oxygen therapy 10 (19%) 3 (7%) ··
oxygen saturation, and oxygen therapy requirement, with aggravation§
and biological parameters, including neutrophil, lympho Oxygen saturation, % 91·6% (2·4) 92·1% (3·9) 0·53
cyte, and platelet count, C-reactive protein (CRP), alanine Oxygen therapy, L/min 7·9 (3·6) 5·6 (3·7) 0·33
and aspartate aminotransferase, creatinine, lactate dehy Low-flow oxygen therapy 32 (62%) 25 (57%) 0·22
drogenase, IL-6, serum ferritin, and D dimer, were recorded High-flow oxygen therapy 20 (38%) 19 (43%) ··
at baseline and at discharge from hospital or death. Persistent fever >38°C 28 (54%) 28 (64%) 0·33
Not to be resuscitated meant that patient was not (Table 1 continues on next page)
eligible for transfer to the ICU. The limitation of care
www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8 3
Articles
We did the main efficacy analysis on an intention-to-treat
Anakinra group Historical group p value
(n=52) (n=44) basis (including all patients in the anakinra group who
received at least one injection of anakinra). We analysed
(Continued from previous page)
time-dependent events with a two-sided log-rank test, with
Laboratory values ·· ·· ··
the hazard ratio (HR) and two-sided 95% CIs based on a
Neutrophil count, × 10⁹ cells per L (normal 7·48 (5·73) 5·61 (2·89) 0·054
Cox proportional hazards model and the associated Kaplan-
range 1·8–7·5)
Meier survival estimates. We assessed the proportional
Lymphocyte count, × 10⁹ cells per L (normal 0·84 (0·38) 1·14 (1·12) 0·12
range 1–4) hazards assumption by testing the interaction between
Platelet count, × 10⁹ cells per L (normal range 259 (114) 201 (83) 0·0071 covariates and time. Patients alive were censored on the
150–400) date of discharge from hospital. We used a multivariate
C-reactive protein, mg/L (normal <5) 173 (67) 154 (76) 0·20 Cox proportional hazards model to take into account effect
Lactate dehydrogenase, U/L (normal range 514 (216) 428 (190) 0·16 of covariates on the estimate of treatment effect. Variables
125–220) were included in the model when they differed statistically
Interleukin-6, pg/L (normal <7) 92·7 (59·5) ·· ·· between the two groups (p value threshold of <0·05) or
Serum ferritin, µg/L (normal range 30–300) 2025 (2303) ·· ·· when the absolute difference between the two groups
D dimer, ng/mL (normal <500) 5061 (8689) 2511 (3162) 0·32 (qualitative variables) was greater than 10%.
Alanine aminotransferase, IU/L (normal <35) 51 (42) 40 (27) 0·18 We compared characteristics of the two groups by use of
Aspartate aminotransferase, IU/L 68 (39) 70 (50) 0·79 the χ² test or Fisher test when appropriate, for categorical
(normal <45) variables and the Student’s t test for continuous variables.
Creatinine, mg/dL (normal range 0·84–1·21) 1·08 (0·69) 0·99 (0·41) 0·45 We used a repeated-measures mixed-model testing group
Concomitant treatments ·· ·· ·· effect to analyse CRP concentrations changes over time. A
Hydroxychloroquine 47 (90%) 27 (61%) 0·0007 p value of less than 0·05 was deemed to be significant.
Azithromycin 49 (94%) 34 (77%) 0·015 We used the SAS (version 9.4) for analyses.
β-lactams 51 (98%) 43 (98%) 0·90
Corticosteroid pulse 2 (4%) 0 0·11 Role of the funding source
Data are mean (SD) or n (%). *Pulmonary disease included asthma, emphysema, sleep apnoea, and chronic obstructive The funder of the study had no role in study design, data
pulmonary disease. †Swab RT-PCR was not done for 11 patients in the anakinra group and ten patients in the historical collection, data analysis, data interpretation, or writing of
group. ‡In the historical group, six patients had a chest x-ray that demonstrated bilateral pneumonia, and no chest CT
the report. TH, HB, SJ, ES, GC, and GH had access to
was done. §Aggravation was defined by a loss of 3% of the oxygen saturation in ambient air over the last 24 h.
the raw data. The corresponding author had full access
Table 1: Baseline demographic and clinical characteristics to all of the data and the final responsibility to submit
for publication.
invasive mechanical ventilation, difference in the mean Results
oxygen therapy requirements between day 0 and day 7, From March 24 to April 6, 2020, 52 consecutive patients
and changes in CRP con centration from day –4 until were included in the anakinra group and 44 historical
discharge from hospital or death. In the anakinra group, patients were identified in the Groupe Hospitalier Paris
day 0 corresponds to the date of initiation of anakinra. In Saint-Joseph COVID cohort study. Clinical, biological, and
the historical group, day 0 corresponds to the first day CT-scan characteristics of the patients in the two groups
during which each patient fulfilled the inclusion criteria are compared in table 1. Significant differences between
defined for the anakinra group. Safety outcomes were an the two cohorts were a lower BMI (mean difference
increase in liver aminotransferase enzymes (more than –3·5 kg/m² [95% CI –5·5 to –1·5]; p=0·0009), a longer
three times the upper limit of normal), thromboembolic duration of symptoms before inclusion (2·2 days
events (confirmed by a CT pulmonary angiogram for [0·6 to 3·9]; p=0·0088), a higher platelet count (58 × 10⁹ cells
pulmonary embolism and by a venous doppler for deep per L [16 to 99]; p=0·0071), and a higher proportion of
vein thrombosis of the lower limbs), bacteraemia (con patients treated with hydroxychloroquine (29% [12 to 45];
firmed when the patient had a recognised pathogen p=0·0007) and azithromycin (17% [3 to 32]; p=0·015) in the
cultured from one or more blood cultures), and premature anakinra group than in the historical group.
discontinuation of treatment. Need for invasive mechanical ventilation or death
occurred in 13 (25%) of 52 patients in the anakinra group
Statistical analysis compared with 32 (73%) of 44 patients in the historical
The original total sample size of the prospective cohort group (HR 0·22 [95% CI 0·11–0·41; p<0·0001; figure 1A).
study was arbitrarily set at 50 patients in the absence of Similar results were observed for death alone (HR 0·30
information on treatment effect. In a classic two-arm [95% CI 0·12–0·71; p=0·0063; figure 1B) and need for
trial, with 50 patients per group, there would be 86% invasive mechanical ventilation alone (0·22 [0·09–0·56];
power to detect a 50% risk reduction of the primary p=0·0015; figure 1C).
endpoint, at a two-sided significance level of α=0·05 and The treatment effect of anakinra versus historical
assuming a 60% incidence of the primary endpoint. group on the composite of need for invasive mechanical
4 www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8
Articles
A Death or invasive mechanical ventilation in the ICU B Death C Invasive mechanical ventilation in the ICU
1·0 Historical group
Anakinra group
0·9
0·8
Probability of event-free survival
0·7
0·6
0·5
0·4
0·3
0·2
0·1
HR 0·22 (95% CI 0·11–0·41); p<0·0001 HR 0·30 (95% CI 0·12–0·71); p=0·0063 HR 0·22 (95% CI 0·09–0·56); p=0·0015
0·0
0 2 4 6 8 10 12 14 16 18 20 0 2 4 6 8 10 12 14 16 18 20 0 2 4 6 8 10 12 14 16 18 20
Time from inclusion (days) Time from inclusion (days) Time from inclusion (days)
Number at risk
(number censored)
Anakinra group 52 47 42 37 28 20 14 9 1 0 0 52 51 47 43 34 26 19 11 3 0 0 52 47 42 37 28 20 14 9 1 0 0
(0) (0) (1) (7) (15) (22) (27) (34) (38) (39) (39) (0) (0) (1) (7) (15) (22) (31) (38) (43) (45) (45) (0) (3) (6) (12) (22) (29) (34) (41) (45) (46) (46)
Historical group 44 25 16 15 10 7 6 4 1 1 1 44 38 31 30 24 21 19 16 12 7 3 44 25 16 15 10 7 6 5 2 1 1
(0) (2) (4) (4) (6) (8) (9) (11) (11) (11) (11) (0) (2) (4) (4) (7) (9) (10) (13) (17) (19) (22) (2) (8) (13) (17) (20) (22) (23) (25) (26) (26) (26)
Figure 1: Kaplan-Meier cumulative estimates of probability of death or invasive mechanical ventilation in the ICU (A), death (B) and invasive mechanical ventilation in the ICU (C) in the
anakinra group compared with the historical group
HR=hazard ratio. ICU=intensive care unit.
ventilation or death remained significant in the multi
Hazard ratio 95% CI p value
variate analysis taking into account factors differing at
inclusion between the two groups (HR 0·22 [95% CI Anakinra group vs historical group 0·22 0·10–0·49 0·0002
0·10–0·49]; p=0·0002; table 2). Male vs female 1·34 0·69–2·62 0·38
Among the 39 patients in the anakinra group who were Symptom duration >7 days vs ≤7 days 1·12 0·51–2·43 0·78
alive and did not require mechanical ventilation, the mean Body-mass index (per kg/m²) 0·99 0·94–1·05 0·75
need for oxygen decreased from a median of 7 L/min Number of comorbidities ≥2 vs 0–1 0·82 0·41–1·66 0·58
(IQR 6–9) at day 0 to a median of 2 L/min (0–4) at day 7 Hydroxychloroquine: treated vs untreated 1·35 0·57–3·17 0·50
(two missing values). The median difference was –4 L/min Azithromycin: treated vs untreated 0·82 0·34–1·99 0·66
(IQR 0–4; p<0·0001, signed-rank test). ICU=intensive care unit.
From day –4 to day 0, there was a sharp increase in CRP
Table 2: Estimation of anakinra effect on the composite of invasive mechanical ventilation in the ICU or
concentration followed by a decrease as early as day 4 of
death, after adjustment for potential confounding factors, using a multivariable Cox proportional
treatment in the anakinra group (figure 2). This result hazards model
contrasts with the relative stability of CRP concentration
over the same time period in the historical group.
The difference between the two groups was significant Discussion
(p<0·0001; interaction test, mixed model). At day 0, In this cohort study, anakinra significantly reduced both
45 (87%) patients in the anakinra group and 36 (82%) need for invasive mechanical ventilation in the ICU
patients in the historical group had a CRP concentration and mortality among patients with severe COVID-19,
higher than 100 mg/L. No patient had a CRP concentration without serious side-effects. So far, no specific treatment
lower than 50 mg/L in both groups. has been shown to reduce the need for invasive mech
Seven (13%) patients in the anakinra group and anical ventilation and intensive care in patients admitted
four (9%) patients in the historical group had an increase for COVID-19-associated pneumonia requiring oxygen
in liver aminotransferase (more than three times the therapy. A number of ongoing trials are currently testing
upper limit of normal). Ten (19%) patients in the various pharmacological approaches.12
anakinra group and five (11%) in the historical group A randomised, controlled, open-label trial of lopinavir–
developed a thromboembolic event during the hos ritonavir in adults with confirmed COVID-19 did not
pital stay. Among the anakinra group, seven (13%) had show any beneficial effect in terms of either clinical
a pulmonary embolism, three (6%) had deep vein improvement or mortality.13 Remdesivir, a new nucleo
thrombosis of the lower limbs, and one (2%) had arte side analogue prodrug that inhibits RNA polymerase,
rial thrombosis. None of the patients in the anakinra was administered to 61 patients on a compassionate-use
group had a documented bacterial infection during the basis, with a clinical improvement seen in 36 (68%)
hospital stay. of 53 patients with available data, but a randomised,
www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8 5
Articles
280 Historical group
macrophage activation syndrome, haemophagocytic
Anakinra group lympho histiocytosis, or CAR T-cell-mediated cytokine
260
release syndrome varied from 100 mg to 400 mg per
240 day.9,19,22,23 Concerning a new indication, in a condition in
220 which the persistence of SARS-CoV-2 cannot be ruled out,
we decided to select an intermediate dose of anakinra for
200
treating our patients. The dose we chose was irrespective
180 of bodyweight or BMI because the pharmacokinetic
Mean CRP (mg/L)
160 profile investigated in healthy individuals of various body
weights demonstrated modest pharmacokinetic changes.24
140
Additionally, given the large therapeutic index of anakinra,
120 we argued that the benefits of fixed dosing (excepting
100 patients under haemodialysis), which reduced the risk
80
of medication error, outweighed the potential reduction
in pharmacokinetic variance relative to individuals of
60
heavier bodyweight.
40 Considering the reduction in both the need for invasive
20 mechanical ventilation and mortality, our study suggests
that anakinra might represent an effective treatment for
0
the hyperinflammatory phase of COVID-19. The efficacy
–4 –3 –2 –1 0* 1 2 3 4 5 6 7 8 9 of inhibition of IL-1 in patients who received anakinra is
Time before and after inclusion (days)
Number with CRP data reflected by the significant decrease in CRP concentration
Anakinra group 11 9 16 21 45 16 22 30 16 12 16 13 4 12
Historical group
in the anakinra group, as compared with the historical
9 6 9 9 36 16 19 10 8 5 5 7 6 8
group (figure 2). The concomitant clinical and biological
Figure 2: Comparison of the mean CRP concentration over time among all patients of the anakinra and improvements might provide indirect support for a
historical groups, until discharge from hospital or death causal relationship between anakinra treatment and both
Error bars indicate SD. CRP=C-reactive protein. *In the anakinra group, day 0 corresponds to the date of initiation
reduced mortality and admission to ICU for invasive
of anakinra. In the historical group, day 0 corresponds to the first day during which each patient fulfilled the
inclusion criteria defined for the anakinra group. mechanical ventilation.
Notably, a previous Italian study evaluating high-dose
double-blind, placebo-controlled trial, which included intravenous anakinra in patients with severe COVID-19,
237 patients, found no clinical benefit of remdesivir ARDS, and hyperinflammation also reported significant,
versus placebo.14,15 comparable benefits for survival and clinical outcomes.25
The current absence of evidence for antiviral drug Obviously, both treated and historical groups reported
efficacy, along with the high mortality associated with here are not representative of all patients with COVID-19
severe COVID-19, raises the question of the respective but correspond to a subpopulation with altered pulmonary
roles of the virus itself and the subsequent occurrence of function and hyperinflammation, since the majority of our
hyperinflammation, or the so-called cytokine storm. In a patients had a CRP concentration higher than 100 mg/L.
study of 150 confirmed COVID-19 cases, predictors of We believe that anakinra should be tested in patients who
mortality included elevated concentrations of ferritin and are admitted to hospital, when clinical and biological
IL-6, suggesting a virally driven hyper inflammation,16 parameters are becoming suggestive of a hyperinflam
sharing common features with other autoinflammatory matory status. However, some questions remain, par
disorders, either inherited or acquired (such as adult Still’s ticularly about the optimal situation and time to prescribe
disease, macrophage activation syndrome, haemophago this biologic agent, since it is potentially useless in the vast
cytic lymphohistiocytosis, or chimeric antigen recep majority of patients with COVID-19, who will only have a
tor [CAR] T-cell-mediated cytokine release syndrome). benign influenza-like syndrome. A rapid and substantial
Furthermore, pulmonary involvement (including ARDS) increase in CRP concentration could represent the best
has been des cribed in secondary haemophagocytic predictor of an evolution from a common viral disease to a
lymphohistiocytosis and in CAR T-cell-mediated cytokine systemic and life-threatening disorder.
release syndrome.17,18 Despite the absence of data from Assessment of the side-effects of a specific treatment
randomised controlled trials, the use of the IL-1 inhibitor remains difficult in the context of a systemic disease, even
anakinra seems to be promising in both haemophagocytic more so when a great number of other drugs are pre
lymphohistiocytosis and CAR T-cell-mediated cytokine scribed simultaneously to the same patient. In this context,
release syndrome.9,19–21 we only noticed an increase in liver aminotransferase
All these data led us to hypothesise that anakinra levels of more than three times the upper normal limit
could represent an efficient treatment for severe forms of in seven (13%) patients in the anakinra group and in
COVID-19. Depending on the reported series, the dose four (9%) patients in the historical group. The transient
of anakinra that was administered in patients with increase in liver enzymes is mentioned in the summary of
6 www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8
Articles
anakinra characteristics and some cases of reversible drug- Declaration of interests
induced hepatitis have been reported with this biologic.26 TH reports consultancy fees from Bristol-Myers Squibb. J-JM reports
consultancy for Mylan, Pfizer, and Servier. GH reports consultancy fees
However, the frequency of elevated liver enzymes in this from Sobi, AbbVie, Bristol-Myers Squibb, Lilly, Novartis, Pfizer, Roche,
study was similar between patients who received anakinra and Sanofi. All other authors declare no competing interests.
and historical controls. Similar findings in an Italian study Acknowledgments
suggest that it is unlikely that anakinra might be causally We thank Helena Pereira (Hôpital Européen Georges-Pompidou,
linked to such abnormalities in these patients.25 CIC 14-18 INSERM, Paris, France) for her help in statistical analysis.
The implication of a coagulopathy in patients with We thank our first-line colleagues for taking constant care of the patients
and for their appreciable help in data collection. We also thank
COVID-19 strengthens the importance of the detection Jean-Patrick Lajonchère (Hospital General Manager at Groupe
and management of thromboembolic events.27 Although Hospitalier Paris Saint-Joseph, Paris, France). We express our solidarity
such events were not systematically investigated in our with all patients with COVID-19, their families, and the health-care
study, ten (19%) patients in the anakinra group and workers on the front lines of this pandemic.
five (11%) in the historical group developed such a References
1 Huang C, Wang Y, Li X, et al. Clinical features of patients infected
complication during the hospital stay. Our data did not with 2019 novel coronavirus in Wuhan, China. Lancet 2020;
allow us to determine whether the inhibition of IL-1 was 395: 497–506.
beneficial or detrimental respective to COVID-19-related 2 Wang D, Hu B, Hu C, et al. Clinical characteristics of 138
hospitalized patients with 2019 novel coronavirus-infected
coagulopathy. Although it has been established that pneumonia in Wuhan, China. JAMA 2020; 323: 1061–69.
IL-1 increases the level of tissue factor, one of the main 3 Chen N, Zhou M, Dong X, et al. Epidemiological and clinical
activators of coagulation, published data are some characteristics of 99 cases of 2019 novel coronavirus pneumonia in
what contradictory about the effect of blocking IL-1 on Wuhan, China: a descriptive study. Lancet 2020; 395: 507–13.
4 Mehta P, McAuley DF, Brown M, et al. COVID-19: consider
coagulability.28,29 cytokine storm syndromes and immunosuppression. Lancet 2020;
Our study has several limitations. Taking into account 395: 1033–34.
the poor prognosis of COVID-19-related ARDS and the 5 Shrivastava G, León-Juárez M, García-Cordero J, et al.
Inflammasomes and its importance in viral infections. Immunol Res
devastating progression of the pandemic, we decided an 2016; 64: 1101–17.
off-label use of anakinra for all patients with severe forms 6 Castaño-Rodriguez C, Honrubia JM, Gutiérrez-Álvarez J, et al.
of the disease. Therefore, the anakinra cohort was com Role of severe acute respiratory syndrome coronavirus viroporins E,
3a, and 8a in replication and pathogenesis. MBio 2018; 9: e02325-17.
pared with an historical group of patients. Consequently, a
7 Siu KL, Yuen KS, Castaño-Rodriguez C, et al. Severe acute
physician learning curve bias could be hypothesised. respiratory syndrome coronavirus ORF3a protein activates the
However, the recruitment of historical patients in the NLRP3 inflammasome by promoting TRAF3-dependent
ubiquitination of ASC. FASEB J 2019; 33: 8865–77.
same institution, during a very short 2-week period is
8 Shakoory B, Carcillo JA, Chatham WW, et al. Interleukin-1 receptor
likely to limit this bias. Second, the historical group blockade is associated with reduced mortality in sepsis patients with
differed sizeably from the anakinra group for several features of macrophage activation syndrome: reanalysis of a prior
potentially confounding variables. Obesity was more phase III trial. Crit Care Med 2016; 44: 275–81.
9 Eloseily EM, Weiser P, Crayne CB, et al. Benefit of anakinra in
frequent in the historical group and might have worsened treating pediatric secondary hemophagocytic lymphohistiocytosis.
the effects of SARS-CoV-2.30 In the multivariate analysis of Arthritis Rheumatol 2020; 72: 326–34.
our data, this comorbidity, as well as the other between- 10 Mehta P, Cron RC, Hartwell J, Manson JJ, Tattersall RS. Silencing
the cytokine storm: the use of intravenous anakinra in
group differences, did not affect the estimated effect of haemophagocytic lymphohistiocytosis or macrophage activation
anakinra on the outcome. Nevertheless, we cannot rule syndrome. Lancet Rheumatol 2020; published online May 4.
out the possibility that the observed association could be https://doi.org/10.1016/S2665-9913(20)30096-5.
11 Chang YC, Yu CJ, Chang SC, et al. Pulmonary sequelae in
due, at least in part, to confounding. convalescent patients after severe acute respiratory syndrome:
In conclusion, in severe forms of COVID-19-related evaluation with thin-section CT. Radiology 2005; 236: 1067–75.
pneumonia requiring oxygen therapy, a 10-day treatment 12 Thorlund K, Dron L, Park J, Hsu G, Forrest J, Mills E. A real-time
with subcutaneous anakinra was associated with the dashboard of clinical trials for COVID-19. Lancet Digital Health
2020; published online April 24. https://doi.org/10.1016/
reduction of both need of mechanical ventilation and S2589-7500(20)30086-8.
mortality, as compared with a historical group with 13 Cao B, Wang Y, Wen D, et al. A trial of lopinavir–ritonavir in adults
similar characteristics. In the context of this pandemic, hospitalized with severe Covid-19. N Engl J Med 2020; 382: 1787–99.
14 Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe
with exponential curves of admittances in ICUs, the use COVID-19: a randomised, double-blind, placebo-controlled,
of anakinra should be tested more extensively, preferen multicentre trial. Lancet 2020; 395: 1569–78.
tially through randomised trials, among patients with 15 Grein J, Ohmagari N, Shin D, et al. Compassionate use of
remdesivir for patients with severe Covid-19. N Engl J Med 2020;
COVID-19 and symptoms suggesting a virus-induced published online April 10. DOI:10.1056/NEJMoa2007016.
cytokine storm. 16 Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of
Contributors mortality due to COVID-19 based on an analysis of data of 150
patients from Wuhan, China. Intensive Care Med 2020; 46: 846–48.
TH, J-MN, YB, SL, JE, J-JM, GC, and GH contributed to the study
concept and design. TH, OV, SJ, GD, IL, SL, ALB, JLP, SS, JE, and 17 Seguin A, Galicier L, Boutboul D, Lemiale V, Azoulay E. Pulmonary
involvement in patients with hemophagocytic lymphohistiocytosis.
J-JM contributed to patient inclusion. TH, HB, GD, and ES contributed
Chest 2016; 149: 1294–301.
to the acquisition of the datasets. GC did the statistical analysis.
18 Shimabukuro-Vornhagen A, Gödel P, Subklewe M, et al. Cytokine
All authors developed drafts of the manuscript and approved the
release syndrome. J Immunother Cancer 2018; 6: 56.
final draft.
www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8 7
Articles
19 Rajasekaran S, Kruse K, Kovey K, et al. Therapeutic role of anakinra, 25 Cavalli G, De Luca G, Campochiaro C, et al. Interleukin-1 blockade
an interleukin-1 receptor antagonist, in the management of with high-dose anakinra in patients with COVID-19, acute
secondary hemophagocytic lymphohistiocytosis/sepsis/multiple respiratory distress syndrome, and hyperinflammation:
organ dysfunction/macrophage activating syndrome in critically ill a retrospective cohort study. Lancet Rheumatol 2020; published
children. Pediatr Crit Care Med 2014; 15: 401–08. online May 7. https://doi.org/10.1016/S2665-9913(20)30127-2.
20 Norelli M, Camisa B, Barbiera G, et al. Monocyte-derived IL-1 and 26 Canna S, Frankovich J, Higgins G, et al. Acute hepatitis in three
IL-6 are differentially required for cytokine-release syndrome and patients with systemic juvenile idiopathic arthritis taking interleukin-1
neurotoxicity due to CAR T cells. Nat Med 2018; 24: 739–48. receptor antagonist. Pediatr Rheumatol Online J 2009; 7: 21.
21 Giavridis T, van der Stegen SJC, Eyquem J, Hamieh M, Piersigilli A, 27 Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant
Sadelain M. CAR T cell-induced cytokine release syndrome is treatment is associated with decreased mortality in severe
mediated by macrophages and abated by IL-1 blockade. Nat Med coronavirus disease 2019 patients with coagulopathy.
2018; 24: 731–38. J Thromb Haemost 2020; 18: 1094–99.
22 Shah NN, Highfill SL, Shalabi H, et al. CD4/CD8 T-cell selection 28 Osnes LT, Westvik AB, Joø GB, Okkenhaug C, Kierulf P. Inhibition
affects chimeric antigen receptor (CAR) T-cell potency and toxicity: of IL-1 induced tissue factor (TF) synthesis and procoagulant activity
updated results from a phase I anti-CD22 CAR T-cell trial. (PCA) in purified human monocytes by IL-4, IL-10 and IL-13.
J Clin Oncol 2020; published online April 14. DOI:10.1200/ Cytokine 1996; 8: 822–27.
JCO.19.03279. 29 Liberale L, Holy EW, Akhmedov A, et al. Interleukin-1β mediates
23 Divithotawela C, Garrett P, Westall G, Bhaskar B, Tol M, arterial thrombus formation via NET-associated tissue factor.
Chambers DC. Successful treatment of cytomegalovirus associated J Clin Med 2019; 8: E2072.
hemophagocytic lymphohistiocytosis with the interleukin 1 30 Simonnet A, Chetboun M, Poissy J, et al. High prevalence of obesity
inhibitor—anakinra. Respirol Case Rep 2015; 4: 4–6. in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2)
24 Yang BB, Gozzi P, Sullivan JT. Pharmacokinetics of anakinra in requiring invasive mechanical ventilation. Obesity 2020; published
subjects of heavier vs. lighter body weights. Clin Transl Sci 2019; online April 9. DOI:10.1002/oby.22831.
12: 371–78.
8 www.thelancet.com/rheumatology Published online May 29, 2020 https://doi.org/10.1016/S2665-9913(20)30164-8
You might also like
- FdarDocument2 pagesFdarkasandra dawn Beriso67% (3)
- Carol Rivers'board Review FlashcardsDocument440 pagesCarol Rivers'board Review FlashcardsJennelle CadoganNo ratings yet
- 7 F1 EURAMOS1 AA Protocol COSS 31072007 Gesamt PDFDocument457 pages7 F1 EURAMOS1 AA Protocol COSS 31072007 Gesamt PDFJemma ArakelyanNo ratings yet
- VAE Prevalence, Outcome, and Relationship With Ventilator-Associated Pneumonia - Bouadma2015Document9 pagesVAE Prevalence, Outcome, and Relationship With Ventilator-Associated Pneumonia - Bouadma2015Maxi BoniniNo ratings yet
- FichaDocument9 pagesFichamariaNo ratings yet
- Avouac 2021Document8 pagesAvouac 2021Sanghita BiswasNo ratings yet
- Implementation of A Non-Invasive Oxygenation Support Strategy During The COVID-19 Pandemic in An Ephemeral Respiratory Intermediate Care UnitDocument3 pagesImplementation of A Non-Invasive Oxygenation Support Strategy During The COVID-19 Pandemic in An Ephemeral Respiratory Intermediate Care UnitJHNo ratings yet
- Timing of Tracheostomy For Prolonged Respiratory Wean in Critically Ill Coronavirus Disease 2019 Patients A Machine Learning ApproachDocument9 pagesTiming of Tracheostomy For Prolonged Respiratory Wean in Critically Ill Coronavirus Disease 2019 Patients A Machine Learning ApproachDewa OkaNo ratings yet
- Lancet Emed Covid Stemcell ArticleDocument9 pagesLancet Emed Covid Stemcell ArticleShanmuga SundaramNo ratings yet
- 1 s2.0 S0012369221004815 MainDocument10 pages1 s2.0 S0012369221004815 Mainkritis ardiansyahNo ratings yet
- Impact of Medical Care Including Use of Anti Infec - 2020 - International JournDocument9 pagesImpact of Medical Care Including Use of Anti Infec - 2020 - International Journragod2No ratings yet
- SorbonneDocument12 pagesSorbonnenathalia souzaNo ratings yet
- NUTRIREA-3 - Lancet Respiratory MedicineDocument11 pagesNUTRIREA-3 - Lancet Respiratory MedicineROBERTO CARLOS BLANQUICETT CORTINANo ratings yet
- Journal Pre-ProofDocument23 pagesJournal Pre-ProofFadhilNo ratings yet
- Early Treatment of COVID-19 Patients With HydroxycDocument9 pagesEarly Treatment of COVID-19 Patients With HydroxycRocky AditNo ratings yet
- Discontinuing β-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC) : a double-blind, randomised, placebo-controlled, non-inferiority trialDocument9 pagesDiscontinuing β-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC) : a double-blind, randomised, placebo-controlled, non-inferiority trialSil BalarezoNo ratings yet
- Journal of Critical Care: ArticleinfoDocument5 pagesJournal of Critical Care: ArticleinfoIon CorbuNo ratings yet
- Epistaxis in Hospitalized Patients With COVID-19Document4 pagesEpistaxis in Hospitalized Patients With COVID-19Olivia Chandra DeviNo ratings yet
- Use of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaDocument10 pagesUse of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaLingga AniNo ratings yet
- 1 5177078803217777111 PDFDocument9 pages1 5177078803217777111 PDFLais Win AndradeNo ratings yet
- Hydroxychloroquine and Azithromycin As A Treatment of COVID-19Document6 pagesHydroxychloroquine and Azithromycin As A Treatment of COVID-19Larissa ChaveirinhoNo ratings yet
- Betalactamicos NAC RCT ENI Lancet 2021 PDFDocument9 pagesBetalactamicos NAC RCT ENI Lancet 2021 PDFLindsay PinargottyNo ratings yet
- Dexamethasone in Hospitalized Patients With Covid-19 - Preliminary ReportDocument11 pagesDexamethasone in Hospitalized Patients With Covid-19 - Preliminary ReportGino IturriagaNo ratings yet
- Nej Mo A 2310307Document11 pagesNej Mo A 2310307Víctor C. ValverdeNo ratings yet
- Dexamethasone in Hospitalized Patients With Covid-19Document11 pagesDexamethasone in Hospitalized Patients With Covid-19michaelwillsonNo ratings yet
- Hospital-Acquired Infection in Public Hospital Buildings in The Philippines: Is The Type of Ventilation Increasing The Risk?Document7 pagesHospital-Acquired Infection in Public Hospital Buildings in The Philippines: Is The Type of Ventilation Increasing The Risk?Khim Joshua MagtibayNo ratings yet
- Covid 19Document9 pagesCovid 19MonicaNo ratings yet
- Prodige 23Document14 pagesProdige 23josebaNo ratings yet
- Individualised Perioperative Open-Lung Approach Versus Standard Protective Ventilation in Abdominal Surgery (IPROVE) - A Randomised Controlled TrialDocument11 pagesIndividualised Perioperative Open-Lung Approach Versus Standard Protective Ventilation in Abdominal Surgery (IPROVE) - A Randomised Controlled TrialVic HNNo ratings yet
- Strongyloides Stercoralis Hyperinfection Syndrome: A Case SeriesDocument8 pagesStrongyloides Stercoralis Hyperinfection Syndrome: A Case SerieslfjuradozNo ratings yet
- NET Vs NPT en Shock Nov 2017Document11 pagesNET Vs NPT en Shock Nov 2017Annison Hector Ramos BravoNo ratings yet
- Spinal Anaesthesia For Patients With Coronavirus DiseaseDocument6 pagesSpinal Anaesthesia For Patients With Coronavirus DiseaseyafetNo ratings yet
- Emergency Tracheal Intubation in 202 Patients With COVID-19 in Wuhan, China: Lessons Learnt and International Expert RecommendationsDocument10 pagesEmergency Tracheal Intubation in 202 Patients With COVID-19 in Wuhan, China: Lessons Learnt and International Expert RecommendationsKOASS UMY PKU GampingNo ratings yet
- Allou 2018Document7 pagesAllou 2018jq4rhbh2pzNo ratings yet
- Nejmoa 2209502Document11 pagesNejmoa 2209502carb0ne14rNo ratings yet
- Jamainternal Hermine 2020 Oi 200097 1635362112.64537 PDFDocument9 pagesJamainternal Hermine 2020 Oi 200097 1635362112.64537 PDFLita SyabaniyahNo ratings yet
- EJEMFactors Associated With Difficult Intubation In.99735Document6 pagesEJEMFactors Associated With Difficult Intubation In.99735tttttNo ratings yet
- Artemisin PiperaquineDocument8 pagesArtemisin PiperaquineIrma Rahayu LatarissaNo ratings yet
- 1 s2.0 S0300957220301210 MainDocument2 pages1 s2.0 S0300957220301210 MainEswari PerisamyNo ratings yet
- Amikinhal TrialDocument11 pagesAmikinhal TrialBreno Bertozo SilvaNo ratings yet
- Boutolleau 2021Document9 pagesBoutolleau 2021nathalialusman98No ratings yet
- Prediction of Outcome of Nasal High Flow Use During COVID-19-related Acute Hypoxemic Respiratory FailureDocument3 pagesPrediction of Outcome of Nasal High Flow Use During COVID-19-related Acute Hypoxemic Respiratory FailureDiego MerchánNo ratings yet
- 1 s2.0 S0924857920301059 MainDocument13 pages1 s2.0 S0924857920301059 MainNini RinNo ratings yet
- Claire Dahyot Fizelier Ceftriaxone To Prevent EarlyDocument11 pagesClaire Dahyot Fizelier Ceftriaxone To Prevent EarlyFermin LombardiaNo ratings yet
- Sancho2021 Article TracheostomyInPatientsWithCOVIDocument9 pagesSancho2021 Article TracheostomyInPatientsWithCOVIJavier BlancNo ratings yet
- En 13Document8 pagesEn 13Bruna CarvalhoNo ratings yet
- De-Escalation of Antimicrobial Treatment in Neutropenic Patients With Severe Sepsis: Results From An Observational StudyDocument10 pagesDe-Escalation of Antimicrobial Treatment in Neutropenic Patients With Severe Sepsis: Results From An Observational StudyyostiNo ratings yet
- Dolivet 2020Document6 pagesDolivet 2020Jasper RaelisonNo ratings yet
- COVID 19 and ENT SurgeryDocument6 pagesCOVID 19 and ENT SurgeryYukiko CalimutanNo ratings yet
- Covid Ihu 2 1 PDFDocument28 pagesCovid Ihu 2 1 PDFhlim_13No ratings yet
- Covid Ihu 2 1 PDFDocument28 pagesCovid Ihu 2 1 PDFSayed MachfudNo ratings yet
- 1 4927188483425960087 PDFDocument8 pages1 4927188483425960087 PDFDanielSilvadaFonsecaNo ratings yet
- Articles: BackgroundDocument8 pagesArticles: BackgroundsamuelNo ratings yet
- Gouzien 2021Document4 pagesGouzien 2021Andreea CiorneaNo ratings yet
- The Egyptian Journal of Critical Care Medicine: Ahmed Abdelrazik Othman, Mohsen Salah AbdelazimDocument3 pagesThe Egyptian Journal of Critical Care Medicine: Ahmed Abdelrazik Othman, Mohsen Salah AbdelazimAquardoleo ValentinoNo ratings yet
- Aerosol-Generating Procedures inDocument5 pagesAerosol-Generating Procedures inHaris WidodoNo ratings yet
- Bionikk Lancet 2022 VanoDocument13 pagesBionikk Lancet 2022 VanomarieNo ratings yet
- Jama 2020 17022Document13 pagesJama 2020 17022wiwiNo ratings yet
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Download 2024 Full ChapterDocument32 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang Download 2024 Full Chaptervito.lyons426100% (9)
- Clinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Download 2024 Full ChapterDocument32 pagesClinical Features of Patients Infected With 2019 Novel Coronavirus in Wuhan China Chaolin Huang 2 Download 2024 Full Chaptervito.lyons426100% (11)
- Effect of HydroxychloroquineDocument11 pagesEffect of HydroxychloroquineJoseph FurgiaruNo ratings yet
- Cavalli 2020Document7 pagesCavalli 2020Elizabeth Gallegos YanaricoNo ratings yet
- Covid-19 Airway Management and Ventilation Strategy for Critically Ill Older PatientsFrom EverandCovid-19 Airway Management and Ventilation Strategy for Critically Ill Older PatientsNicola VargasNo ratings yet
- PIIS1473309920304370Document1 pagePIIS1473309920304370wedib17801No ratings yet
- Correspondence: Implication of Sars-Cov-2 Evolution in The Sensitivity of RT-QPCR Diagnostic AssaysDocument2 pagesCorrespondence: Implication of Sars-Cov-2 Evolution in The Sensitivity of RT-QPCR Diagnostic Assayswedib17801No ratings yet
- Dinesh C Sharma: Lancet Oncol 2020Document1 pageDinesh C Sharma: Lancet Oncol 2020wedib17801No ratings yet
- Ebiomedicine: Qi Cheng, Yue Yang, Jianqun GaoDocument6 pagesEbiomedicine: Qi Cheng, Yue Yang, Jianqun Gaowedib17801No ratings yet
- Green Endoscopy: A Call For Sustainability in The Midst of COVID-19Document3 pagesGreen Endoscopy: A Call For Sustainability in The Midst of COVID-19wedib17801No ratings yet
- Tropical Veterinary Science: Ready Today For TomorrowDocument8 pagesTropical Veterinary Science: Ready Today For TomorrowEsdinawan Carakantara SatrijaNo ratings yet
- 10 Facts On Mental HealthDocument11 pages10 Facts On Mental HealthDit DotNo ratings yet
- Latihan Abbreviation 2Document2 pagesLatihan Abbreviation 2Sherly AmeliaNo ratings yet
- Visual Diagnosis and Traditional Chinese Medicine: Face Reading - What Your Face SaysDocument8 pagesVisual Diagnosis and Traditional Chinese Medicine: Face Reading - What Your Face SaysTaniaNo ratings yet
- J Clinic Periodontology - 2023 - RattuDocument19 pagesJ Clinic Periodontology - 2023 - RattutzulinNo ratings yet
- 2021 AHA ASA Guideline For The Prevention of Stroke in Patients With Stroke and TIA Clinical UpdateDocument43 pages2021 AHA ASA Guideline For The Prevention of Stroke in Patients With Stroke and TIA Clinical UpdateLê Thị HươngNo ratings yet
- Case Study On GynaeDocument22 pagesCase Study On GynaeJay PaulNo ratings yet
- 8 Laws of Health: Streams of Light MinistryDocument9 pages8 Laws of Health: Streams of Light Ministryanjani kumarNo ratings yet
- Metaanalisis AfricaDocument14 pagesMetaanalisis AfricaRosy AlcayagaNo ratings yet
- Erata Ghid PDFDocument2 pagesErata Ghid PDFAna-Maria MihalceaNo ratings yet
- Annual Report 20-21Document3 pagesAnnual Report 20-21Nagesh SoodNo ratings yet
- CAIE Biology A-Level: Topic 10 - Infectious DiseasesDocument3 pagesCAIE Biology A-Level: Topic 10 - Infectious Diseasesstephen areriNo ratings yet
- Meconium Aspiration Syndrom1Document3 pagesMeconium Aspiration Syndrom1Nikael Patun-ogNo ratings yet
- Micoses Superficiais - GlobalDocument19 pagesMicoses Superficiais - GlobalJosé Paulo Ribeiro JúniorNo ratings yet
- Updated NCCN Guidelines For Cervical Cancer.22Document2 pagesUpdated NCCN Guidelines For Cervical Cancer.22Hari NugrohoNo ratings yet
- 1 s2.0 S0040162520312774 Main PDFDocument7 pages1 s2.0 S0040162520312774 Main PDFCardboard GamingNo ratings yet
- 5. Chronic pancreatitis. СholelithiasisDocument58 pages5. Chronic pancreatitis. Сholelithiasischai rinNo ratings yet
- Case Based Discussion: Sindy Helda PutriDocument30 pagesCase Based Discussion: Sindy Helda PutriSindyputri HeldaNo ratings yet
- Biostat 2020 62 QDocument270 pagesBiostat 2020 62 Q'محمد علي' محمد لافيNo ratings yet
- DuPont-Bi-07 TMDocument19 pagesDuPont-Bi-07 TMAshlee TanNo ratings yet
- Pyrexia of Unknown Origin 3Document27 pagesPyrexia of Unknown Origin 3Ausu OfficialNo ratings yet
- The Side Effects of Platinum-Based ChemotherapyDocument10 pagesThe Side Effects of Platinum-Based Chemotherapyyour happinesNo ratings yet
- 5 - Anemias Associated With Abnormal Heme SynthesisDocument24 pages5 - Anemias Associated With Abnormal Heme SynthesisSara BakerNo ratings yet
- Travel and Return Policy The State of QatarDocument7 pagesTravel and Return Policy The State of Qataralbanlobo100No ratings yet
- Anxiety Disorders AssignmentDocument4 pagesAnxiety Disorders AssignmentMatilda SwintonNo ratings yet
- Parmacist 1Document45 pagesParmacist 1AHAMED SHIFAAN100% (1)
- Sf8 Nutritional-Stat-Baseline 6 Pearl 2022Document8 pagesSf8 Nutritional-Stat-Baseline 6 Pearl 2022Dante Maligsa BautistaNo ratings yet