Professional Documents
Culture Documents
Dying and Death
Dying and Death
Uploaded by
Vedant Tapadia0 ratings0% found this document useful (0 votes)
21 views16 pagesCopyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views16 pagesDying and Death
Dying and Death
Uploaded by
Vedant TapadiaCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 16
ia preteen,
ace
ommend 2
WOMEN
AGING
WITH
KNOWLEDGE
ws
A TonewstoNe Book
Pususien sy
Stow & Scnuster
NewYork London Toronto
Swiney Tokyo Singepore
THE NEW
OURSELVES,
GROWING
OLDER
a
PAULA B. DORESS-WORTERS
AND DIANA LASKIN SIEGAL
IN COOPERATION WITH THE
BOSTON WOMEN’S HEALTH BOOK COLLECTIVE
ILLUSTRATIONS BY ROSELAINE PERKIS
CONTENTS
+
Foreword to the 1987 Edition xi
Foreword to the 1994 Edition xiii
Project Coordinator's Preface xvi
Preface to the 1994 Edition xix
‘THE POTENTIAL OF THE SECOND HALF OF LIFE xx!
AGING WELL
1. AGING AND WELL-BEING 3.
2. HABITS WORTH CHANGING 22
3, OUR LOOKS AND OUR LLiVes 38
4. WEIGHTY IssUES 47
5. EATING WELL 52
6. MOVING FOR HEALTH 64
LIVING WITH OURSELVES AND OTHERS AS WE AGE,
7. SEXUALITY IN THE SECOND HALF OF LIFE 81
8. BIRTH CONTROL FOR WOMEN IN MIDLIFE 101
9. CHILDBEARING IN MIDLIFE 108
10. EXPERIENCING OUR CHANGE OF LIFE: MENOPAUSE 118.
1, RELATIONSHIPS IN MIDDLE AND LATER LIFE 133
12, HOUSING ALTERNATIVES AND LIVING
ARRANGEMENTS 151
13. WORK AND RETIREMENT 169
14, MONEY MATTERS: THE ECONOMICS OF AGING FOR
WoMEN 187
15, CAREGIVING 204
a ,
UNDERSTANDING, PREVENTING,
AND MANAGING MEDICAL PROBLEMS
16, WOMEN'S HEALTH AND REFORMING THE MEDICAL-CARE
‘SYSTEM 221
17, NURSING Homes 249
18, JOINT AND MUSCLE PAIN, ARTHRITIS, AND RHEUMATIC i
DisorDers 262
19. OSTEOPOROSIS AND FRACTURE PREVENTION 279
20, DENTALHEALTH 293
21, URINARY INCONTINENCE 300
22. HYSTERECTOMY AND OOPHORECTOMY 315
23. HYPERTENSION, HEART DISEASE, AND STROKE 333 ‘
24. CANCER 347
25. DIABETES 374
26. GALLSTONES AND GALLBLADDER DISEASE 382
27. VISION, HEARING, AND OTHER SENSORY LOSS ASSOCIATED
WITH AGING 389
28. MEMORY LAPSE AND MEMORY Loss 403.
29. DYINGAND DEATH 415
30, CHANGING SOCIETY AND OURSELVES 427
RESOURCES
General Resources 441 * Agingand Well-Being 447 © Habits Worth Changing 450
* Our Looks and Our Lives 454% Weighty Issues 454 © EatingWell 456 +
‘Moving for Health 458 + Secualityin the Second Halfof Life 459 © Birth Control
for Women in Midlife 462 + Childbearing in Midlife 463 + Experiencing Our Change
of Life: Menopause 466 + Relationships in Middle and Later Life 468 © Housing
Alternatives and Living Arrangements 472 * Workand Retirement 474 © Money
‘Matters: The Economics of Aging for Women 477 + Caregiving 479 + General
Health 482 + Women's Health and Reforming the Medical-Care System 484
Nursing Homes 487 + Joinrand Muscle Pain, Arthritis, and Rheumatic
Disorders 489 + Osteoporosisand Fracture Prevention 491 « Dental Health 491
‘+ Urinary Incontinence 492+ Hysterectomy and Oophorectomy 493 +
Hypertensiun, Heart Disease, and Sicoke 494 + Carer 494..% Diabetes 497 +
Gallstones and Gallbiadier Disease 493. + "Vision, Hearing, and Uther Sensory Loss
Associated with Aging 498 * Memory Lapseand Memory Loss 501 * Dyingand
Death 502 + Changing Society and Ourselves: 508
Index 507
ne cee ce ee
UPDATE BY PAULA. DORESS WORTERS WITH SPECIAL THANKS TO ANNE ARSENAL
URCES FOR THIS CHAPTER ON PAGES 5024
{ih many cultures, preparing for and making
sense of death is the work of women, especially
of old women, Whether or not it’s fair or best,
women in most societies, including our own, still
act as the nurturers, caregivers, and custodians
fof those near death. Even with the removal of
(death to the institutional sphere, dying remains
he province of women who work in those insti-
rations.
last person most of us see on earth is a woman—the
‘iurse’s aide (significantly one of the east paid aid least
valued workers in our society)... These are, in a sense,
the midwives of death!
Thus, it is most often women who meet the
emotional and pragmatic needs surrounding
death,
By the age. of fifty-seven I had nursed my husband
‘through terminal cancer, lived through widowhood, and
been close to two dear friends who died. 1 assisted one
friend and supported her family through the process of
her committing suicide, 1 feel that my middle years have
been significant in bringing me into close and familiar
contact with dying and death,
BEREAVEMENT AND GRIEF
Grief is a normal reaction to the stress of losing
someone. It is not a pathological reaction that
needs to be “cured.” According to Phyllis R. Sil-
verman, founder of the widow-to-widow move-
ment, we may go through several phases of
grieving the loss of someone we care deep
About. At first, we may fecl numb or dazed,
tunable to believe that such a grievous loss could
have happened. That numbness often carries us
through the first days and weeks, allowing us to
function. Gradually, we begin to come to terms
with the reality of the loss, realizing that we can
no longer live as before. Eventually, when we can
remember our loved one with less pain, most of
us accommodate to our loss. Then we restruc-
ture our lives to make room for new roles and
relationships? - :
The following is excerpted from ‘a woman's
journal recording her feelings about her lover’.
death overa period of years:
Inwhat later seemed to be extraordinary word usage, the
doctor called me to say the operation on Karen was “sue
cessful.” They resectioned her colon and took out the
415
+ THE New OURSELVES, Growine OLDER +
ltonor, she would not need a colostomy. But the tumor
hhas metastasized and she will die: six months to two
years is all they give her. No real hope.
tis 2:30 Aas and T cant sleep because of rage at
God, and then because of guilt. And because of fear jor
nyself, How will live without Karen to tell me Tam brit
liant and beautiful?
Images run through my head. Her hand warming my
asthma-congested chest. Her step—quick, strong, fast up
the stairs. As I remember that sound, I smile; the pain
recedes. But if shut my journal, the pain will return.
Does everyone who is dying look bewildered? Her
head ir my lap: her body spooned in pain, Dying means
deperddency. Pain, Listlessness. Fever. Exhaustion. Dying
is frightening.
Death is frat, but dying can drag on and on and on,
destroying everyone. It saps the strength of the healthy
‘and makes them sick
My first birthday without her. Our anniversary. Her
first birthday dead. My first Christmas and first New Year
without her. One year it was the greatest New Year of my
life, and the nest year the woman who gave it fo me was
dead.
Each marker brings Karen to me and takes her. Soon
any first spring without her. My first summer. Then a year
since I last saw her will pass. A year since her death; a
‘year since her funeral. And I will put «@ headstone in my
heart: Karen, my dearest?
Any one loss can remind us of all the other
losses we have known—especially the earliest
ones, which might not have been fully under-
stood or explo:
When ey lover died I was fifty-six. Over the next two
years Irelived, in away, al ofthe other great saiinesses of
‘ny life—when my father left us when I was little, my
mother’s death, the endings of other love affairs. I don't
think I had realized how much there was for me 10
‘mourn! [a sixty-two-yearold woman]
Acceptance of death can come only after a
full experience of mourning that may last many
months or even years.
My daughter died almost forty years ago, when she was
ten. Um still angry, and [still miss her. But for years after
she died I couldn't quite believe that it had really hap
pened—I kept thinking I heard her in the house, Now 1
ean accept what happened, even if I dont like it. (a sev:
centy-eight-year-old woman}
My husband died eighteen years ago and even though
today 1 have « happy; full if, I still miss him. Lam often
reminded of what he is missing, especially at happy
moments, such as the children’s high school and college
graduations, which are tinged with the wish that he were
alive o share the joy. (afifty-four-year old woman}
Mentalhealth experts have observed that
“troubled mourning’ can be a principal reason
for unhappiness and problems later in life
Mourning can go wrong in a variety of ways. We
may be unable to grieve at the time of loss, feel-
ing too numb to cry or to express our feelings in
any way at all. We may begin to grieve but cut the
process short, because of pressure to appear self-
possessed for a job or family or friends. Or we
may suppress our grief, drive it underground, in
which case it is likely’ to erupt again, perhaps
with surprising intensity, at the time of some
later loss.
In these cases, we may try to protect our-
selves from the pain of grief by adopting a self-
protecting mask of composure that allows us to
carry on with life as usual. Sometimes a physical
illness may appear, or self-destructive behavior
such as drug or alcohol addiction, an eating dis-
order, or repeated involvements in unsatisfac-
tory relationships. One or more aspects of
mourning can become exaggerated. We may
dwell on guilt, self-blame, anger, anxiety, or sad-
ness until we become completely incapacitated
and such feelings take the place of grieving.
In each of the above cases, the underlying
problem is that the person who mourns has i
some way not completed the mourning process.
416
i
i
we
Ste ctegt
© ARIE NAR
+ DeaTH AND Dvinc +
‘Sometimes friends or relatives, in a misguided
desire to be helpful, urge us to “get on with it,”
when in fact what we need is to honor the
urgency and depth of our feelings for as long as
we need to do so. Payiug attention to our feelings
and talking about them with friends or relatives
is extremely important.
When my husband was dying people helped us so much:
They came o visit aed brought food so that I could spend
‘more time with him. They gave flowers and hugs, gave the
children extra attention. Some people were too frightened
to visit and I understood. But the friend who came fifcen
‘hundred miles to see him before he died, the friend who
came five hundred miles to hold my hand during the
funeral, and the fiend who stayed atthe cemetery to cover
bis grave after the service will forever have my gratitude
Twas comforted by the notes and cards people sent
‘me. I read theme over and over again for many months,
nurtured by the care, sympathy, and support they pro-
Vided. Best of all were the handwriten notes that
included something about the writer’ relationship with
‘my husband or memories of times together—sometimes
things rhat were new to me, received notes from people I
had not known and was strengthened by their considera-
tion. Even the printed cards and the simplest notes indi-
cating that someone was thinking of me comforted me.
Nineteen years later, I still have all tke messages in a box
s0 our now grown children can share with their children
how the grandfather they will never know touched the
lives of so many others. (a ffty-four-year-old woman)
When my husband died it was like 1 was paralyzed
socially or months after. My two good friends did me a
(great service just by sitting with me. Sometimes T would
‘ery and sometimes I'd just be angry. Sometimes Iwas so
sad I could hardly talk. They'd come over to visit me at
least ice a week, and they stayed with it for more than a
‘year. When I felt better I could be a good friend to them
‘again. (a sixty-four-year-old woman]
earned a lot about anger after my mother died. Some-
how, when Iwas mouming, lots of anger came out that
didnt know was in me. My daughter suggested beating @
pillow witha stick 0 get the anger out, and finaly 1 g0¢ 0
Teould tall with my husband and also with my daughter
about some of the reasons why felt so much anger at my
oor mother. fa forty-three-year-old wornan}
Observing religious andior cultural tradi-
tions, writing about our feelings in a journal,
talking to family and friends, meditating, read-
ing poetry, watching emotion evoking movies or
plays, and singing or listening to familiar songs
canall help us feel our grief as deeply and fully as
we need. Joining a self-help group of people who
are grieving, such as a widow-to-widow group or
a hospice group, can be a great comfort. Such
groups help us realize that what we are feeling is
“normal” and is shaved by others.
ne same of as i ws get professional
rel rom a clergyman, for example, or per-
haps from a bereavement counselor—to deal
‘with the process of mourning.
1 functioned extremely well most of the time (everyone
always said how well), but I felt like I was just going
through the motions, waiting for my husband to come
home. Three times in the past four years I've arrived at
the point where I felt a need for counseling. Each time
Tve learned more about myself. The counseling has
helped me grow and find new meaning in my life. [a
‘woman in her fifties)
The loss of a child or grandchild can be par-
ticularly painful. If death is caused by a sudden,
unexpected accident that allows little or no time
beforehand for preparation, as is often the case
when someone we love dies young, the loss may
be even more difficult to come to terms with. We
cannot comfort ourselves by saying, “Well, she’s
lived a long and full life and it was her time to
die,” Even if we lose a child in her or his middle
How To HELP A DYING oR
RECENTLY BEREAVED PERSON
‘Give them the time and quiet listening to
express their feelings. Express your own
sadiness and regret, but do not presume to
tell a bereaved or dying person that a
death is “for the best,” even if after a long
illness. We don't really know how some-
‘one feels unless she or he tells us.
* Offer distractions, other topics of mutual
interest, but be comfortable with silence
and resist the need to fill every minute
swith words. Your very presence will help,
Take care of a dying or bereaved person;
do not expect her or him to take care of
you. Bring food if you visit someone's
home.
‘Offer help, and be specific in your sugge:
tions. Say, “I have two hours free on Sat-
urday. Do you want me to shop for you, or
is there something else I can do that
‘would be helpful?”
417
+ THe New Oursetves, Growine OLDER +
or late years, we may feel a sense of unfairness,
as if the natural order of things has been vio-
lated. This was not a loss we expected to sustain.
Losing my only daughter to AIDS was the hardest, most
hheartbreaking thing that has ever happened in my life, 1
kept trying 10 make sense of it. I couldn’ get over my
‘guilt. Why did I have to get sick? Why didi’ I make her
Stay where she was instead of coming here to take care of
‘me? Who would have known that she would fallin love
with « man who would give her AIDS? He shot between
hhis tes and hidden places on his body so she wouldn't
notice the tracks, Only my faith in God and the help of my
therapist carried me through my anger, mty guilt, and
wanting to die myself. Finally, ! was able to accept her
death and to cherish the happy years we had before she
passed on. (asixty-nine-yeat-old woman]
‘When death is expected, not only the
who is dying but also those who expect to be sur-
vvivors have time to make some preparations, get
relationships and business affairs in order, and
reminisce and say good-bye.
My father died of a heart attack and my mother died of
‘cancer My father’ death was a surprise and a shock, and
‘my mother’ death was a long ordeal. ! know that people
sometimes think thar sudden and quick death is east,
drut for me is was importzet to talk with my mother and
‘even jst 10 sit and hold her hand, and though those lat
‘weeks and months were hard Y'm grateful we had them,
With my father there was no time to ay good-bye. I wish
there had been. (a forty-nine-yearold women]
When we are faced with the shock of a sud.
den, unexpected death, we often console our.
selves with the knowiedge that the person we
loved did not suffer. While having time to pre-
pare for a death may be easier on our survivors,
‘many of us would choose an unanticipated and
painless death for ourselves.
When death comes at the end of a prolonged
and chronic illness, our feelings may take longer
to sort out. We may have already grieved, years
ago, for the loss of the whole, well person we
used to know.
My sister developed the first symptoms of Alzheimer’s
when she was sixty-two. [took care of her, moved into
her apartment for five years so she could stay in familiar
surroundings. Then Thad to put her into a nursing home,
‘where [visited her twice a week. I never missed a week
for nine more years until she died. There was very litte
‘that anybody could do for her. It was very hard to see her
‘become just a thin litle curled-up ball in her bed. For the
last seven years she didn’ recognize me or even talk at all.
‘She was my ony siser, and it was torribly sad for me. [a
sixty-two-year-old woman}
We may feel a sense of release for ourselves
and forthe person who died after prolonged su
fering. But later, intense, renewed feelings of loss
may surface.
Even though I thought Ihad prepared myself mentally for
the inevitable, I found I was terribly shocked, even sur
prised, when my mother finally did die. ! understand now
that shock after a death is common among those elose to
‘person, even when the death was expected.*
‘COMING TO TERMS WITH OUR
‘OWN DEATHS:
One of the important developmental tasks of the
second half of life is coming to a personal under-
standing, perhaps even an acceptance, of death.
Some of us continue to feel ambivalent and
scared about acknowledging death.
418
+ DEATH AND DyINo +
of my fiends have died young. We all knew each
for so long. (We had a card-playing group.) Three of
were my age. One of them I met recently and recog.
er name from elementary school, and so we were
same age. Another one was a few. months older sa we
bere all inthe sume age bracket. Now my sister in-law
died and she was only sixty-three. This has been on
ny mind so much lates, you know, reaching this point
t people my age are starting o go. I never used fo think
f these things before, Like if an aunt or an uncle died
f8 one thing, but now its cousins! One cousin my
died this summer, s0 I start to think “Its our turn”
ally, I'm very glib about it, but in my gut J cant
Eaccept that one day I wont be here, [a seventy-fouryear
Mold woman)
Maybe no one can ever be fully “ready” for
death in the sense of knowing about and fully
fPaccepting the experience in advance. But we can
RE prepare ourselves in a variety of ways.*
5. I feel a greater awareness of a mystery and. beauty in life
BP since Ihave accepted death as a personal eventuality for
pe. I dont rememiber exactly when that awareness came,
bi: Before then, Ihad thought of death “out there,” and now I
E friow that one day it wil be a reality for me. Eventually I
jam going (0 die. In a way, that has released me for more
‘vid living, (a seventy-cight-yearold woman]
g: ve dealt with losing loved ones many times in my life
fond after seventy years of repetition ofthat experience of
Ey wrief I find the thing that’s so hard to deal with is that
«Some person who has been a reality in your life no longer
“ists. When you're a kid, you learn how to separate fan.
f#asy front reality. But ther, when you get older, you have
Bo learn how to let goof a reality that person no longer
exists. I've got @ handle on that from years of experience
with it. So I no longer worry about my own personal
death, (a seventy-three-year-old woman}
Some of us are comforted by religious, spiri-
tual, or humanistic beliefs about life and death.
believe that tam not just a body which is perishable but
Lam a spirit which is eternal | believe that death is ony
an exit from this temporary life of unreality into a glori-
ous new life of reality. I hope, therefore, that there will Be
only rejoicing, not grief, at the time of my release. I am
ying to avoid being “earthbound” hy releasing my
attachments to material objects and persons before 1
‘enter this transition. [a ninety-two-year-old woman]
What I've been aware of lately because of a number of
instances of my being thrown up against death is that 1
shave a different perception of relationships. Death is not
@ termination of my life because my influence will con
tinue until the last person who knew me has died. [a
‘woman in her fifties]
Living each moment as fully as possible is
probably the most important way to help our-
selves become less fearful of death.
Ido not look to the future with dread. 11 has to be shorter
than my past but it does not have 10 be less rich. 'm more
relaxed. Idon' try 0 do everything.
That means I can take time for quiet, for meditation,
alternate this with activity, and see how I can keep a
moving, living balance between the two, [a seventy
eight-year-old woman}
Death, I am leamting through my own experience, need
not be frightening. After all, we are all bor terminal
cases, because we will all die, at one time or another,
Deaths is part of life. F have lived life fully and enjoyed it
greatly, which makes it easier to consider bowing out
than ifyou fel that you have missed out on alot.*
Providing support to others can also help us
come to terms with death. We can serve as
resources for one another and create supportive
networks that give us the strength and compan-
ionship we need to get through hard times.
On the day before her jifcy-cighth birthday, my friend
Maggy Krebs died m a Boston hospital. Magay was a femn-
“Tich Sommers, age seventy, ina eter to members of the
Older Women League about her expected death. Teh
founded and led the Sventy-treeshoutand member orga
Nanton after her eancer as dagnosed
419
4+ THE New OURSELVES, GrowiNe OLDER +
inist artist. Her humor, her drawings and paintings, and
her music had filed many lives with joy. Because I
believe that the final months of her life and her death were
‘models forall independent women. 1 want to tell vou part
ofthe story.
For months, Maggy gathered around her a group of
her friends, who tended to her at her home and atthe hos-
ital, In addition to caring for Maggy, we met each other
regularly, often weekly to share our grief and anger atthe
‘anticipated loss of a friend, to find ways to share the
responsibilty of taking care of her and to support one
‘another. We became a family for Maggy and for each
other.
‘One of Magay’s legacies to us isthe pride we fel that
we were able to give her the comfort and love she needed,
But Magey also left a legacy of hope to all women who feel
themselves to be alone by teaching us that we can sup-
port each other through the depths of ines, eshaustion,
fearand oss.*
Sharing the responsibility as this women’s
group did avoids the guilt women sometimes feel
when they cant do everything by themselves, An
illness support group allows each woman to pat
ticipate to the extent she is able to do so.
‘Some Day Tans Fuesit
Some day some atom of tis flesh shall be
commingled with a tree,
Will taste the resinous sap spicing its veins;
Wrestle with tempests; dance with silver rains:
And stand a singing tower against the sky.
My lapping blood existence will partake
with some far; hill-giet lake,
will cherish waterlilies on its flood;
Will shadow winging bird and dreaming cloud;
And hold the evening star within its cup.
Thave so joyed in campfire’s comradeship;
Have felt such grip
of awed delight at dogwood's miracle;
Such rapture in the living slope of hill;
Surely [shall be fire and flower and grass!
Fear? Fear transfiguration glad as this?
Such loveliness?
With these I have so loved, to be enfurled,
inwoven inall the beauty of the world?
ethaps—who knows?—My very heart shall be
for one mad hour of flaming ecstasy
sunset!
Plorence Luscomb
*Sce pages 192 and 206 forcartoons by Maggy Krebs.
In the last four years I have come from the
despair to festing that life is good and that ther stil iat
reason and a need for me to bein this world. Helping
train haspice volunteers continues to Be therapeutic ig
te, With the deat of my shad, things which on
read about in books or heard others talk about becant
very real and personal to me. Much of my own grief work
‘was done with the volunteer training classes, where the
volunteers gave me the opportunity 10 talk about my
experiences and my life, and the aloneness I felt atthe
fos of ny et frend end companion [a woman a
her fifties
Most of my friends are gone. You just have to say toyour-
self that it's something that’ going to happen. But is not
easy. It helps to do all you ean for your friends while
they reliving. {do alot of ealling onthe telephone. Ihave
4a friend [call every day. He's been in the hospital along
time. Thave another friend who lives down in another
town who's quite sick that I call at least once a week.
Death used to be scary (0 me. Four or five years ago, if
thought of dying, 1d push it out of my mind. But now,
think, after al, ve lived out my days and I keow I've got
togo. {a woman in her eighties]
Florence Luscomb, sufjragist labor organizer,
‘ivilrights and peace activist, Died in 1985 at age
nninety-eight Elen Stab
420
+ DEATH AND DytNo +
‘Another way to prepare ourselves for dying is
care of any unfinished business in our
ss. Most of us have unresolved relationships—
ne that go back quite far—that we may want
gp work out or perhaps just make a final state-
int on. We can seek out people with whom we
ive unfinished business and see to it that some
unforgiven hurts are healed—and recognize
some can't ever be healed. Those who have
de the effort to do this say tis very important.
efore her death my sister asked to see each of her five
thers and sisters. We talked about the ways we had
en close and trusting with each other, and we also
tlked about some of our long-standing fights and
dges. I know thatthe hour that she and I spent going
dr our times together was very important to me. [twas
‘way to say good-bye. And I think it was important
healing for her, as well. [a forty-seven-yearold
oman)
Ej:tcan remember the day my grandfather died, in a tractor
‘accident on the farm. The men brought him in from the
field to the house, and my grandmother, my mother, and
‘my aunt bathed and dressed him. I was a loving act, and
f ritual, and J was terribly impressed. I was eight at the
time, My own father went from the hospital bed where he
F< died to a funeral kome, and I know my mother doestt?
feel like she was a part of his dying. I'm tying 10 wnder-
stand that difference, and what I myself want to do in
‘that regard. fa sixty-seven-yearold woman}
In some cultures, death is understood to be a
natural transition at the end oflife. Among some
Native American tribes, for instance, each life is
seen as a road that is expected to come to an end,
The healers in those societies see themselves as
“keepers of the road,” guardians of health for as
& Jong as the journey goes on—not as persons who
‘work to prevent the journey from ending in its
‘expected transition,
But in our contemporary culture, we invest
j heavily in science and want to believe that
through it we can control all the events of our
lives. We have hope that the discoveries of science
will allow us to prolong life and prevent “death,
These attitudes make it hard to look on death as
the natural, expected end of life, and make it
harder to accept the inevitability of death.
Physicians often use every possible means to
protong life without regard for its quality. The
result can be feelings of anguish and heipless-
ness on the part of the dying person, relatives,
and friends.
When my husband had his heart attack I thought 1
should rush him to the hospital. The ambulance came
right away but by the time they resuscitated him he
already had a lot of brain damage, He never recovered
consciousness. Everyone in the ICU [Intensive Care
Unit] worked very hard to save his life, and he did live for
‘another two weeks, but as faras I'm concemed he wasn't
realy alive—just a body attached to a lot of tubes and
machinery. Lwish now that Thad just held him, cradled
his head, when he first fell! could have said good-bye
that way. [a sixty-five-year-old woman]
As some medical professionals are beginning
to recognize, focus on the inappropriate pursuit
of a cure when the situation is clearly beyond
hope can lead medical personnel to make a per-
son's last days more painful and difficult than
necessary. Of course, there are situations of
acute emergency in which one cannot be sure
whether recovery is possible; it is very hard to
know the right thing to do in such a case. But
some medical treatments designed to cure, such
as chemotherapy and radiotherapy, may increase
the dying person's discomfort.
‘Many of us may feel more secure in a hospi-
tal when we are very ill. Or we may feel we want
to try, or should continue to try, medical reme-
dies on the chance that one may heal us.
My daughter died of breast cancer at age foty-swo. We
‘thought she wanted to deat home and we were ready to
‘ake care of her there. But inthe end the doctors urged her
to try one more round of treatment with chemotherapy
‘and she went back into the hospital. She never came
hhome again, and forthe fast week she was so sick and in
such pain tha she di even ware her teenage children
‘als her [a snty-efght-year-old woman]
Discomforts such as pain, shortness of
breath, weakness, nausea, and vomiting often
precede death. The last days of living can be
eased by concentrating on comfort rather than
eure. (See Dealing with Pain in the chapter
aan
+ THe New Ourseives, Growine OLDER +
Habits Worth Changing, pages 35-36.) Occa-
sionally, treatments such as radiotherapy or even
surgery may be used to bring relief of pain and
discomfort, though it is more common to use
high doses of pain-relieving drugs.
We were lucky enough to find a doctor who was willing 10
come to the house and could prescribe drugs for Grand-
rma’s pain and also for the nausea. We heard about the
doctor because she had performed the same service for a
neighbor down the street, and she made a hard time
‘much easier than it might have been. (a thirty-six-year-
‘ld woman]
‘TAKING CONTROL OF OUR
OWN DEATHS
Many of us would prefer not to be subjected to
machines and tubes and complex technological
procedures that may extend life a few extra days,
weeks, or months at the expense of whatever
quality it may be possible to achieve. Some of us
who have such thoughts, however, will surely die
in the very circumstances we deplore. How does
this happen?
‘We tend to forget experiences that most of us
have had as patients, like being moved from one
treatment to another with little explanation of
what is really thought to be wrong, how the
treatment is supposed to work, and what to
expect next, as if once we become patients we
have given over the right or desire to make
choices. The physician often doesn't present
alternatives from which we can choose; the alter-
natives of no treatment or of treatments such as
acupuncture or herbal remedies are rarely dis-
cussed. This failure to present alternatives
makes it difficult for the ill person to make
informed decisions. Being a patient can feel like
‘being ona slippery slide you cant easily get off.
My daughter spent the last months of he life going tothe
hospital for outpatient treatments, and feeling terrible.
wortt ever do that, Tm not saying it’s any better to be sick
{rom the cancer, but at least you'd fel like its your bod
dnd your life. Ti want to have some tne to myself live
ait fT thought f was going to die soon. (a ifty-nine-
yearold woman] :
Here are some things to remember about
doctors and dying:
* Physicians cannot actually predict recovery,
death, or future disability for any single
; they can only make broad, educated
guesses based on statistics for large popula.
tions. They deal in group probabilities.”
* Many people whose death was predicted with
firm certainty by medical experts have recov-
ered: this happens with sufficient regularity to
remind us that iliness is not fully understood
byscience.
+ Each individual has a right to say how she or
he will live out the last days of a soon-to-be.
ended life. If living outside a hospital or with-
out the discomfort of medical treatment is
what you want, your right to do so ought to be
honored.
Ten years ago, when 1 was fortyfive, I was told I had
breast cancer. For the next year I had chemotherapy and
radiation—I was sick and worried the whole year. But
now I feel that when the cancer comes back I just want to
live with it, except for painkillers when I need them. 1 feel
that ifm going olive on, or die, I want to be able to expe-
rience each day as my day. I've written letters (0 each of
‘my children to let them know how important this is ome.
Even when we try to stay in control, an ill-
ness can become overwhelming and may deplete
our energy reserves, especially if we do not have
a dependable support system. Though we may
aspire to a serene death for ourselves or a loved
one, surrounded by familiar faces, we must rec-
‘ognize that humans have never been able to con-
twolor predict death.
I felt like I was in a dream. had promised my husband
wouldnt send him back to the hospital, but I was up for
twenty hours each day taking care of him and I just
‘couldnt go on. He agreed to go back because I promised
him that I would live there with him. The last ten days he
didn’ talk but he seemed t0 be comfortable. They were
giving him morphine intravenously. The doctor woke me
at 3 Ast 10 tell me he had died while I was sleeping. It
bothered me that 1 was sleeping when he died because 1
+had promised him that Twould be with him. Idon’ know
if he would have said anything if 1 had been awake. No
‘matter how hard you try, it doesn? always work out the
‘way you want, (a woman in her sixties)
Advance Medical Directives
IE you ‘decide thlatiin some circumstances you
‘would prefer to have no treatment, or treatment
for comfort only, you have a right to refuse treat-
ment. In every state, constitutional and common
Jaw support the right of any competent adult to
refuse medical treatment in any situation.* How-
ever, writing your wishes in an advance medical
422
Girective can protect your right to refuse treat-
Bent, make it clear to your family members and
Pealth-care providers what you want, and help
em to comply with your wishes,
» Anew federal law requires hospitals, nursing
nes, HMOs, and home health agencies serv
g persons covered by Medicaid or Medicare to
de Information ‘upon admission about
directives and to explain your legal
and choices. If they will not honor your
they must tell you, so that you can select
er institution. State laws vary on this, and
have provisions for doctors who, for rea-
of conscience, will not comply with certain
es. Check with your state attorney generals
They may be able to provide you with
‘ate forms as well.
‘Advance medical directives can be stated ina
ng will or in a durable power of attorney for
alth care. In a living will you give directions
‘your future medical care, stating what you
fant and don't want. A durable power of attor-
éy for health care is a document in which you
‘Appoint a health-care agent or proxy to represent
pu in the event you become unable to commu
te your wishes. If possible, discuss your
‘with your health-care proxy or represen-
and give her or him copies of all relevant
iments,
‘As of June 1993, all fifty states and the Dis-
trict of Columbia authorize either living wills or
B the appointment of a health-care agent. Three
, Massachusetts, Michigan, and New York,
paiithorize only the appointment of a health-care
gent, and two states, Alabama and Alaska, a
B thorize only living wills?
F Living wills are valid only in cases of termi-
pal illness—that is, when a person is expected to
lic in the near future, usually within six months,
a direct consequence of injury or illness. They
‘not honored in situations when a person has
slow degenerative disease or when a very old
firson has “muliplo systems flue” In these
ations, appointing a health-care proxy throug!
durable power of attorney may be more effec-
> Another drawback of the living will is that it
: Operates primarily for treatment refusal. If you
{Want all possible treatments tried, a durable
Bower of attorney is more useful” and may serve
for treatment refusal aswel, a
Assuring that you get adequate medical treat-
E ment if you are severely ill may take more than
‘writing out your wishes. The cost-containment
‘emphasis in medical care has resulted in people
F
+ DEATH AND Dyine +
being discharged from hospitals when they still
hope for recovery and want treatment. Older
persons, especially those with limited funds, are
at-an especially high risk of being discharged
prematurely agains: their wishes.
Dying at Home
At one time, almost everybody could have
expected to die in their own homes—even in
their own beds. Now, death more often occurs in
a hospital or nursing home. Recently, however,
"pore people are insisting that they be allowed t0
die outside of these institutions.
Idon' want anyone to tell me what to do. I ived all these
‘years with my eight children, and made decisions, right
orvsrong, about how we'd live. I want to decide for myself
now: I've no need for medicine, drugs, or hospitals, never
have, and 1 don't want to start now. I want to die with
dignity. I'm comfortable in my home among my own
‘things and with my family around me. They'l care for
‘me. They" respect my wishes. Ican see who [want in my
‘own home. Ican eat what I want to eat. know my own
body and what it needs or can handle. Iv a private per-
son. There's no privacy in the hospital. I want my chit-
dren around me. 1 need their touch, their love. [a
seventy.six-year-old woman}
‘Mom needed to be hostess and be in charge in her home
even while dying. She continued to direct and guide her
children about her care. While we held a cup to her
‘mouth, she would urge, “Eat with me.” When she needed
‘more care, we hired hospice workers. When I introduced
my mom to the new worker, Mom was already in her
“withdrawal from the world stage." But she drew herself
‘together from her fetal position under the blankets to peek
at this new person, and, in her weak, raspy voice, said,
“Welcome to my home.” These were her final words to the
world. What a magnificens, feisty, independent woman
this mother of mine was. She showed us how to live and
‘how to die. Mom passed on as peacefully as possible con-
sidering her pain and weakness. [a filty-seven-yearold
woman, the daughter of the wornan quoted above]
A.woman who is a midwife wrote the follow-
ing account of her mother’s death:
‘This past year brotight serious illness to my mother, Mar-
ion Cunningham. We sought conventional medical
attention, plus an array of alternative healing practition-
ers. Afier months of misdiagnosis, Marion diagnosed her-
self as dying. We admitted her to the hospital and, alas,
the diagnosis of lung cancer was finally acknowledged.
My brother, my sister, and I stood in disbelief at her side,
423
+ THe New OURSELVES, GRowiNe OLDER +
Marion Cunningham Roxanne Cummings Pore
A pioneer in natural childbirth and in single parenting,
she had always been our source of strength and inspira-
tion. Weall ried together that day. Then Marion spoke to
ime, words which would affect our caring of one another
in the months to follow: "Why dont they have midwives
for what I've got?” We decided tocar for her at home.
‘One night at midnight 1 received a call from my
brother... "Mom says she will die today and that you all
should come.”
dnd thus i was thar we gathered round. My brother
requested that I sing “The Goodbye Song,” which I had
‘written just a month before.
th see you in the babies’ faces
I feel you in the wind
hear you in the quietest places
Tihold you in my friend.
I played on my guitar and sang to Marion, and in the
hnidst of the song I could hear her breaching relax and
knew she would die. We watched one tear roll down her
face and then she took her last breath."
Hospices
A relatively new institution called the hospice
hhas developed in response to the growing inter-
est in dying at home. The hospice is modeled
after medieval way stations that accommodated
both travelers and those who were dying (death
being, metaphorically, another forni of travel).
‘Contemporary hospice agencies started out
as coalitions of volunteers who were trained to
visit and offer help to dying people in their own
homes. Most hospice agencies now also have
specially designed inpatient buildings where
people can get short-term help managing un-
comfortable symptoms and then go back hor
‘The services of medical professionals are a rele.
tively minor part of the care offered by hospices,
‘They also provide trained volunteer visitor, vis:
ing nurses, nurses” aides, homemakers, and
bereavement counseling for family and frends,
‘One of the major goals of a hospice program
is to maintain the quality of life through spiritual
and emotional support, medication, and meth-
fds such as meditation and visualization for
pain control. They will also provide temporary
relief for caregivers.
(Our son died of Hodgkin's disease two years ago. Toward
the end he said he didn't want to go back into the hospi-
tal, no matter what. We called the hospice and they sent a
volunteer who came to vist John two days a week a frst
and then, at the end, every day. He was almost like a
‘member ofthe family, and the help he gave made a bi df-
ference to all of us—especially 10 Jolin [a seventy-six-
year-old woman}
Some of these services have always been
available from visiting-nurse and home-care
agencies, clergy, church-visitation committees,
and other local sources. But a hospice program
coordinates all these services. Medicare, Medic-
aid, and some other insurance plans may pay
part of the bill. Not all communities have hos-
pice agencies, however. If you want to locate the
hospice nearest you, call a visiting-nurse agency
or a local hospital's social service department.
(See Resources for this chapter for the two
national hospice organizations.) A local Social
Security office can also tell you which hospice
programs are Medicare certified.
Choosing the Time of Our Death
Two years ago my mother, who was then eighty-three, told
‘me that she planned to end her life by taking an overdose
of pills. Her health was failing rapidly and she was going
blind. She didn't want to become weak and dependent.
She had always been a fierce and active woman, She
wrote her intentions ia fetter to me—I was her only close
family member—and she told two friends and her doctor.
We all cold her that we would not help her accumulate
enough pills do the job. And I think we all worked very
‘hard to help her find new reasons 16 be happy to be alive.
But finally I understood that she really wanted to do what
she had planned. and in the end, offer she gathered
together enough pills and took them, sat with her for the
last thrtysix hours as she slipped away, I cant tell you
show many of her friends and acquaintances told me how
‘graceful my mother was it her life to the very end. For my
424
+ DEATH AND Dytne +
‘mother, given her personality, staying in control of her
own life made her graceful. [a forty-one-yearold woman]
There is a great difference between someone,
terminally ill and in pain, who says, “Tve lived 4
j Gull, long life and I think this is may time to die,”
, and someone who is viewing life through the fog
(of depression and says, “Idon't want to go on Ine
eR mS der ogame,
ing.” For a depressed person, a suicide attempt
fy may be a call for help in finding resources 10
p Tegain pleasure in living. You can get help for
such a person through a suicide-prevention
p organization like the Samaritans (see Resources
for this chapter),
tis very difficult to know what to do when a
cone wants to end her or his life. Talking
with this person can help us distinguish tempo-
rary feelings of discouragement from the convie-
tion that a life of pain and deterioration would
be unbearable,
Laws vary from state to state, but nearly
everywhere, a person who helps a dying family
member or friend commit suicide risks prosecu-
tion as an accessory to a crime. To protect their
loved ones, some dying persons have chosen t0
g0 off by themselves and take a fatal substance.
They have had to do without the loving support
and the talking and planning that would have
eased the transition for everybody.
Claiming the right to control the end of our
lives in no way minimizes the seriousness or the
finality of the decision, nor the pain and grief of
those we leave behind. A number of organiza-
tions, such as Choice In Dying, now publicize
issues and can help us deal with them per-
sonally (see Resources for this chapter)
Practical Matters
Before we die, some of us may want to arrange to
donate vitally needed organs, such as kidneys
and corneas, for transplant Purposes, We can
also plan the kind of funeral or memorial service
‘we want. Helpful, practical information on these
matters is available from the Older Womens
League as part of their “Living Will Packet” (see
Resgurossforthis chap a
A growing number of people today want to
keep ‘matters relating to death under the control
of the ic i
‘mation itself, and last rites and memorial ser-
vices can all, within broad limits, be designed to
suit the wishes of the person who has died and
her or his survivors.
The person I talked ro about renting a place forthe memo-
rial service told me sharply that I had no business plan
fring a memorial while my mother was stillalive. But lam
ery thant thas we did plan it when we did. First of all,
as amazed fied thaeFwasin absolutely mo condbeon
‘0 make sensible plans after she ded... Planning the
forms of the memorial beforehand helped mie face the real,
{ty of my mothers death. Thinking about and writing
what ! would say brought the love we had shared back
‘me once more. Petcipating in the memorial gave me a
ind of peace and acceptance t hardly dared hope for!™
If you have preferences about your burial, it
will be much easier for your family and friends
to carry out your wishes if
known ‘in writing. This will also Protect your
loved ones from having feelings of guilt, because
they will be assured they ate following your
wishes,
Remember that the funeral business is just
that-—a profitable business, There are some reg.
ulations, from state to state, that govern
this industry. You can leam about them by call-
ing your state attorney general’ office.
1 foundout later thatthe funeral director lied to me when
the said stare law required a cement lining for my hus.
bands grave, contrary to our personal and religious
belief. [a fifty-ive-year-old woman}
Those of us who are struggling to come to a
better understanding ofthe great, universal ran.
sition at the end of life have many opportunities
to ponder the matter: Experiences such as watch.
ing persons we are close to approach death, be.
‘coming aware of symptoms that might signal the
inning of life-threatening ilIness putting ne
affairs in order in a written will, working as avo.
unter in a hospice agency, or being part of a
‘supportive network for a dying friend or relative,
all can help us come to a peaceful, personal un.
derstanding of death.
Notes
1. Tish Sommers, Death—A Feminist View, Paper
presented at Drake Uuiversity Law School, Des Moines,
Towa. March 271976, *
2, Phyllis R. Silverman, Helping Women Cope with
Gri Bere i: Saget
3. Carolyn Ruth Swift unpublished manuscript
4 Sty Spencer lag Read Broom Vl 7,
‘No.6 (November-Decamber 1988), pp. 40-42,
5.3. W. Wordes and Willam Proctor, Personal Death
Awareness. Englewood Clifs, I: Prentice Hall, 1976
425
+ THe New Ourseives, Growinc O1pen +
6. Swift, op.cit.
7. See Stephen Jay Gould, “The Median Isn't the
Message.” Discover, Vol. 6, No.6 une 1985), pp, 40-42.
8. George Annas and Joan Dennsberger, "Compe-
tence to Refuse Medical Treatment: Autonomy vs. Pater
‘alistn.” University of Toledo Law Review, Vol. 15 (1988),
p. 561-96,
9. Choice in Dying, Inc., (see Resources for this
chapter), State Statutes Govemiing Living Wills and
Appointment of Health Care Agents, June 1993,
10. Barbara Mishkin, ‘Making Decisions for the Ter.
‘minally IL” Business and Health, ne 1985, pp. 13-16.
41. Roxanne Curamings Potter, “To Lite—To Death.”
alfornia Association of Midwives Newsletter. Syeing
1984, p.7.
12, Spencer, op.clt.
426
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Some Reflections On Violence Against Women by Radhika Coomaraswamy IndiaDocument5 pagesSome Reflections On Violence Against Women by Radhika Coomaraswamy IndiaVedant TapadiaNo ratings yet
- Case List (KK Luthara Memorial Moot Court Competition) Memo For DianaDocument1 pageCase List (KK Luthara Memorial Moot Court Competition) Memo For DianaVedant TapadiaNo ratings yet
- CH 4 Adolescence Change VulnerabilityDocument28 pagesCH 4 Adolescence Change VulnerabilityVedant TapadiaNo ratings yet
- Subordination and Sexual Control A Comparative View of The Control of Women by Gita SenDocument6 pagesSubordination and Sexual Control A Comparative View of The Control of Women by Gita SenVedant TapadiaNo ratings yet
- Refugee Definitions Source: United States Association For UNHCRDocument2 pagesRefugee Definitions Source: United States Association For UNHCRVedant TapadiaNo ratings yet
- Sumangala's Mother, India, Pali Language, 13 CenturyDocument27 pagesSumangala's Mother, India, Pali Language, 13 CenturyVedant TapadiaNo ratings yet
- Yosano Akiko, "Labour Pains," Japan, 1878-1942Document30 pagesYosano Akiko, "Labour Pains," Japan, 1878-1942Vedant TapadiaNo ratings yet
- Female Genital Mutilation: Key FactsDocument4 pagesFemale Genital Mutilation: Key FactsVedant TapadiaNo ratings yet
- Mridushi FactsDocument1 pageMridushi FactsVedant TapadiaNo ratings yet
- In The Hon'Ble High Court of Judicature at Allahabad, Lucknow Bench, LucknowDocument12 pagesIn The Hon'Ble High Court of Judicature at Allahabad, Lucknow Bench, LucknowVedant TapadiaNo ratings yet
- In The Hon'Ble Supreme Court of IndiaDocument18 pagesIn The Hon'Ble Supreme Court of IndiaVedant TapadiaNo ratings yet
- SemIV - Labour. Arpit Parakh .33Document15 pagesSemIV - Labour. Arpit Parakh .33Vedant TapadiaNo ratings yet
- In The Hon'Ble High Court of Judicature at Allahabad, Lucknow Bench, LucknowDocument12 pagesIn The Hon'Ble High Court of Judicature at Allahabad, Lucknow Bench, LucknowVedant TapadiaNo ratings yet
- Legal Notice: Notice From The Buyer To The VendorDocument7 pagesLegal Notice: Notice From The Buyer To The VendorVedant TapadiaNo ratings yet
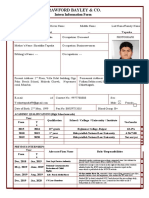
- Crawford Bayley & Co.: Intern Information FormDocument2 pagesCrawford Bayley & Co.: Intern Information FormVedant TapadiaNo ratings yet
- Consumer PlaintDocument5 pagesConsumer PlaintVedant TapadiaNo ratings yet
- Bail Application U/S 438 Cr.P.C. For Grant of Anticipatory Bail On Behalf of The Accused (Mr. V)Document4 pagesBail Application U/S 438 Cr.P.C. For Grant of Anticipatory Bail On Behalf of The Accused (Mr. V)Vedant TapadiaNo ratings yet
- Assignment of IghtsDocument7 pagesAssignment of IghtsVedant TapadiaNo ratings yet