Professional Documents
Culture Documents
16 Abdominal Tuberculosis - Un Diagnóstico Dilema
Uploaded by
jhon_4548Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
16 Abdominal Tuberculosis - Un Diagnóstico Dilema
Uploaded by
jhon_4548Copyright:
Available Formats
DOI: 10.7860/JCDR/2015/13350.
5887
Original Article
Abdominal Tuberculosis: A Diagnostic
Pathology Section
Dilemma
Seema Awasthi1, Manoj Saxena2, Faiyaz Ahmad3, Ashutosh Kumar4, Shyamoli Dutta5
ABSTRACT / excised specimens was done and Ziehl-Neelsen (ZN)
Background: Abdominal tuberculosis (TB) is the sixth staining to detect the tubercular bacilli and Periodic acid-
most common form of extra-pulmonary site of infection Schiff (PAS) stain to rule out fungal infection was done in
after lymphatic, genitourinary, bone and joint, miliary and all the cases.
meningeal TB with a rising incidence in recent years. Results: Out of 48 cases with abdominal tuberculosis, the
TB can affect any part of the gastro-intestinal (GI) tract average age of presentation was 27.4 years with a slight
including anus, peritoneum and hepato-biliary system. The male predominance (Male:Female=1.4:1). Abdominal pain
clinical manifestations of abdominal tuberculosis are non- (100%) was the most common presenting symptom followed
specific and mimic various GI disorders and cause delay by anorexia (98%), fever (88%) and intestinal obstruction
in diagnosis and management. (88%). The ileum was the most common site of involvement.
Aim: To evaluate the various clinical, radiological and All the 45 resected / excised tissue specimens (34 cases of
microbiological findings of abdominal tuberculosis and intestinal resection and 11 cases of intesinal, omental and
to define the role of histopathological examination in lymph nodes biopsies) showed epithelioid granulomas along
establishing the diagnosis in resource poor settings and with necrosis (in 38 cases) and Langhans giant cells (in 42
to analyze the compliance and response to anti-tubercular cases). Acid Fast Bacilli (AFB) positivity was seen in 5 tissue
treatment. specimens only. All patients were put on anti-tubercular
treatment and majority showed good response to therapy.
Materials and Methods: A five year retrospective study
(January 2010 to December 2014) was done in a tertiary Conclusion: Abdominal tuberculosis should be considered as
teaching hospital in Northern India and all the cases a differential diagnosis in patients with vague GI symptoms.
diagnosed as abdominal tuberculosis during the study period, Study of histopathological findings can aid in the diagnosis
were included. The relevant clinical informations, laboratory in the settings where advanced molecular methods of
results, microbiological and radiological investigations were diagnosis are not available, leading to early diagnosis and
recorded. Histopathological examination of all the resected management.
Keywords: Gastrointestinal, Histopathology, Intestinal obstruction, Langhans
Introduction Peritoneal involvement may occur due to spread of the bacilli
Tuberculosis is a chronic granulomatous disease caused by from mesenteric lymph node, contiguous spread from intestinal
an aerobic bacteria Mycobacterium tuberculosis. It remains lesion or from tubercular salpingitis in women. However, one
the world-wide problem despite the discovery of the causative third of the cases show abdominal lymph node and peritoneal
organism for more than a century ago. Pulmonary tuberculosis tuberculosis without any evidence of gastrointestinal involvement
is the most common form and it primarily involves the lung [12].
but any part of the body can be involved by the disease Grossly the abdominal tuberculosis presents in 3 morphological
[1, 2]. Abdominal tuberculosis (TB) although less common in forms- ulcerative, hypertrophic and combination of both ulcero-
western countries, constitutes a major public health problem in hypertrophic [6,11,13,14]. Most common complication of intestinal
developing countries and associated with significant morbidity tuberculosis is intestinal obstruction attributed to strictures or
and mortality [3,4]. It is the 6th most frequent site for the extra by adhesions and in India approximately 3-20% of all cases
pulmonary involvement and it can involve any part of the of bowel obstruction are due to the tuberculosis [8,15,16].
gastrointestinal tract , peritoneum and hepatobiliary system. One of the serious complication of abdominal tuberculosis is
perforation, causing high morbidity and mortality [6,8,17] and
The mycobacterium reaches the gastrointestinal tract via
it accounts for 5-9% of small intestinal perforations in India.
hematogenous spread, ingestion of infected sputum or direct
It is the 2nd most common cause of intestinal perforation in
spread from infected contiguous lymph nodes and fallopian
India after typhoid fever [2]. Perforations due to tuberculosis are
tubes [5-9]. usually single and occurs proximal to the stricture site [6].
The clinical manifestations of abdominal tuberculosis are protean Scant literature is available on the extra-pulmonary tuberculosis
and can mimic many other disease process, causing delay in in reference to its incidence and bacteria positivity [18].
diagnosis [10].
We emphasize here to suspect the abdominal tuberculosis
The most common site of predilection is the ileocaecal region, clinically and also on the role and importance of the
attributed to the minimal digestive activity, relatively increased histopathological examination in resource poor settings where
physiological stasis, higher rate of fluid and electrolyte study of tissue biopsy can aid in diagnosis and ultimately in
absorption and more lymphoid tissue at this site [5,8,11]. proper and early management of affected cases.
Journal of Clinical and Diagnostic Research. 2015 May, Vol-9(5): EC01-EC03 1
Seema Awasthi et al., Abdominal Tuberculosis in a Tertiary Teaching Hospital: Review of 48 Cases www.jcdr.net
Materials and Methods In 19 cases ascitic fluid was available for further analysis
A retrospective study was conducted in a tertiary teaching with Acid Fast Stain (AFS) and mycobacterium culture. Ascitic
hospital in North India. All the cases diagnosed as abdominal fluid was exudates in nature in all the cases and showed
tuberculosis, including gastrointestinal tract, peritoneum, AFB positivity in only 8 patients. On culture, tubercular colony
mesenteric lymph nodes or other intra-abdominal solid organs growth was seen in only 2 cases with Lowenstein Jensen
were retrieved. The detailed patient information in form of media.
demographic data, clinical details, laboratory results and All patients received plain film chest radiographs (CXR) and 10
treatment outcome were recorded. Ziehl-Neelsen (ZN) staining cases had abnormal radiological findings including cavitatory
was done to identify the tubercular bacilli and Periodic acid- lesions, pleural effusion and lymphadenopathies.
Schiff (PAS) stain was used to rule out the fungal etiology of Pathological examination was performed on 45 patients and
granuloma formation. Intestinal resection was the most common surgical procedure
The diagnosis of abdominal tuberculosis was made in all performed in the cases of abdominal tuberculosis followed by
the cases fulfilling following criterias: lymph node and intestinal biopsy (intestinal resection in 34
1) Acid fast stain positivity for M. tuberculosis in ascitic/biopsy cases and 11 cases of intesinal, omental and lymph nodes
specimens. biopsies). Tubercular enteritis was seen in 39 cases with most
common involvement of the ileocaecal region. Perforations
2) Identification of caseating granulomas on histological
were present in 31 cases out of total 39 cases of intestinal
examination of excised/ resected specimens from
enteritis (in 28 cases of 34 intestinal segment resection) and
abdomen.
was most commonly present in ileum. Microscopically all 45
3) Response to anti-tubercular treatment cases revealed characteristic pathological findings consistent
HIV ( Human Immunodeficiency Virus) screening was done in all with tuberculosis including granulomatous inflammation (n =45),
the cases and cases with positive HIV status were excluded Langhans giant cells (n =38), caseous necrosis (n= 22) and AFB
from the study. positivity (n=5) [Table /Fig-3-5]. None of the case showed PAS
Total 48 cases were diagnosed as abdominal tuberculosis stain positivity.
between January 2010 and December 2014 and the follow- The anti tubercular treatment was started in all the 48 cases.
up record was analyzed along with response to anti-tubercular All the cases responded well to therapy except one case
agents. that developed osteomyelitis of ankle during the course of
treatment.
Results
During the study period total 48 patients were diagnosed Discussion
as a case of abdominal tuberculosis with a slight male Though pulmonary tuberculosis is the most common form of
predominance of 28 males and 20 females (Male:Female=1.4:1). tuberculosis, extra-pulmonary TB is also a significant cause
The demographic characteristics of all these patients are of morbidity and mortality and affect lymph nodes, intestine,
summarized in [Table/Fig-1]. bone, joints, meninges, genitourinary tract, etc [1]. Abdominal
These patients presented a wide age group of distribution of tuberculosis is the sixth most common form of extra-pulmonary
11 to 58 years with maximum number of cases (n=27, 56 %) site of infection after lymphatic, genitourinary, bone and joints,
presenting between 21-40 years. Only 9 cases (19%) had the miliary and meningeal TB [11]. The incidence of abdominal
past history of pulmonary tuberculosis while family history of tuberculosis is rising all over the world however very scant
tuberculosis was present in only 5 cases. literature and knowledge has been updated.
The clinical manifestations of the patients are summarized Abdominal TB can affect any age group. In a study conducted by
in [Table/Fig- 2] which shows abdominal pain as the most Sharma MP et al., [19] most affected patients were between
common presentation followed by anorexia, fever, intestinal 21-45 years of age. Our study also showed maximum number
obstruction, perforation peritonitis, ascitis and nausea/vomiting. of cases (n=27) in this age group (56%). This finding of
involvement of slight younger population was also seen in
The laboratory findings revealed elevated ESR in 34 patients
many other studies [20,21]. Our study showed a slight male
and anaemia in 22 patients as most common laboratory
predominance than females with abdominal tuberculosis and
abnormalities. Mantoux skin test was performed in 31 cases
a similar results were seen in a study conducted by Rajput
and was found positive in 9 cases only.
MJ et al., [21]. Although Indian studies have suggested a slight
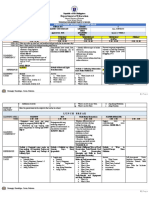
S. no. Age group (years) No. of cases (Male + Female) % female predominance [6].
1. 0-20 9 (4 Male + 5 Female ) 19 The clinical manifestations of abdominal tuberculosis are quite
2. 21-40 27 (16 Male + 11Female) 56 protean. Similar to the previous reports abdominal pain (100%)
3. 41-60 12 (8 Male + 4 Female) 25 was the most common clinical presentation in this study also,
Total 48 (28 Male + 20 Female) 100
followed by anorexia (98%) [19]. In a study by Sharma MP
et al., [19] fever was recorded in half of the patients while in
[Table/Fig-1]: Distribution of cases according to age
present study higher no of cases 88% presented with fever.
Clinical presentation Number of cases % Routine laboratory tests have limited value in the diagnosis of
Abdominal pain 48 100 Abdominal TB [22]. In present study 10 cases were found to
Anorexia 47 98 have abnormal findings on chest X-ray (CXR). Arif Au et al.,
[20] and Rajput MJ et al., [21] observed preexisting pulmonary
Fever 42 88
tuberculosis in 20% and 33.95% of their patients respectively.
Intestinal obstruction 42 88
In this study we found ileocaecal region as the most frequent
Perforation 31 65
involved site in cases of abdominal tuberculosis and the
Ascitis 19 40 most common manifestation was presence of strictures. These
Nausea/ vomiting 12 25 findings were in accordance with the previously published
[Table/Fig-2]: Clinical presentations of patients literature [20].
2 Journal of Clinical and Diagnostic Research. 2015 May, Vol-9(5): EC01-EC03
www.jcdr.net Seema Awasthi et al., Abdominal Tuberculosis in a Tertiary Teaching Hospital: Review of 48 Cases
[Table/Fig-3]: Photomicrograph showing Epithelioid granulomas with numerous giant cells (x100, H&E) [Table/Fig-4]: Photomicrograph showing central caseous necrosis in a
granuloma (x100, H&E) [Table/Fig-5]: High power photomicrograph showing numerous Acid fast bacilli (x1000, ZN stain)
[2] Kapoor VK. Abdominal tuberculosis: The Indian contribution. Indian J
Very low incidence of perforation (0-11% in adults, 3-4% in
Gastroenterol. 1998;17:141-47.
children, 2.5-6% at autopsy and 20% of all non-appendiceal [3] Global tuberculosis control 2012. [Internet]: World Health Organization. (Online)
perforations) has been reported in literature [8,17] because of http://www.who.int/tb/publications/global_report/en/index.html Cited 2011 April
reactive fibrosis of the peritoneum and formation of adhesions 11.
[4] Wadhwa N, Agarwal S, Mishra K. Reappraisal of abdominal tuberculosis. J
with adjacent tissues. In contrast however in the present study, Indian Med Assoc. 2004;102:31-32.
perforation was more common than that reported previously [5] Marshall JB. Tuberculosis of the gastrointestinal tract and peritoneum. Am
(65% of all cases and 82% of resected intestinal segment speci- J Gastroenterol. 1993;88:989-99.
mens). In the present study we aimed to investigate the relative [6] Kapoor VK. Abdominal tuberculosis. Postgrad Med J. 1998;74:459-67.
[7] Das P, Shukla HS. Clinical diagnosis of abdominal tuberculosis. Br J Surg.
reliability of different tools for the diagnosis of abdominal tuber- 1976;63:941-46.
culosis which present with nonspecific and vague symptoms. [8] Bhansali SK. Abdominal tuberculosis: Experiences with 300 cases. Am J
We conclude that clinical and laboratory results are usually Gastroenterol. 1977;67:324-37.
[9] Prakash A. Ulcero-constrictive tuberculosis of the bowel. Int Surg.1978;63:
nonspecific and lead to diagnosis of a chronic disease only.
23-29.
To differentiate the ileocaecal TB from Crohn's disease is indeed [10] Peda Veerraju E. Abdominal tuberculosis. In: Satya Sri S, editor. Textbook of
difficult and classically the diagnosis of abdominal tuberculosis Pulmonary and Extrapulmonary Tuberculosis. 3rd ed. New Delhi: Interprint; 1998.
pp.250-52.
requires microbiological and culture confirmation of Mycobac- [11] Paustian FF, Marshall JB. Intestinal tuberculosis. In: Berk JE, editor. Bockus
terium tuberculosis, many studies established the diagnosis on Gastroenterology. 4th ed. Philadelphia: WB Saunders: 1985. p. 2018-36.
histopathological examination only [13,18]. Sharma et al., [19] [12] Hoon JR, Dockerty MB, Pemberton J. Ileocaecal tuberculosis including
a comparison of this disease with non-specific regional enterocolitis and
found very low yield of organisms on smear and culture (acid fast
noncaseous tuberculated enterocolitis. Int Abstr Surg. 1950;91: 417-40.
bacilli is positive in less than 3 per cent of cases and positive culture [13] Tandon HD, Prakash A. Pathology of intestinal tuberculosis and its distinction
in less than 20 per cent of cases). In our study also the diagnosis from Crohn's disease. Gut. 1972;13:260-69.
could be reached histopathologically in majority of the cases [14] Prakash A, Tandon HD, Nirmala L, Wadhwa SN, Prakash O, Kapur M.
Chronic ulcerative lesions of the bowel. Indian J Surg. 1970;32;1-14.
(93%). Polymerase chain reaction (PCR) although has emerged [15] Bhansali SK, Sethna JR. Intestinal obstruction: a clinical analysis of 348 cases.
as a promising tools for diagnosing extra-pulmonary TB, is not Indian J Surg. 1970; 32:57-70.
cost-effective in resource poor setting . [16] Tandon RK, Sarin SK, Bose SL, Berry M, Tandon BN. A clinico-radiological
reappraisal of intestinal tuberculosis – changing profile? Gastroenterol Jpn.
1986; 21:17-22.
Conclusion [17] Talwar S, Talwar R, Prasad P. Tuberculous perforations of the small
Since the clinical presentations of abdominal tuberculosis are intestine. Int J Clin Pract. 1999;53:514-18.
very non-specific and vague and the diagnostic criteria’s are [18] Yoon HJ, Song YG, Park IW, Choi JP, Chang KH, Kim JM. Clinical
Manifestations and Diagnosis of Extrapulmonary Tuberculosis. Yonsei Med J.
limited, hence diagnosis has to be supported by additional 2004;45:453–61.
tests and by retrospective analysis with reference to clinical [19] Sharma MP, Bhatia V. Abdominal tuberculosis. Indian J Med Res.
patterns, underlying diseases and X-ray findings. We also 2004;120:305-15.
[20] Arif AU, Shah LA, Ullah A, Sadiq Mu D. The frequency and management
emphasize the importance of histopathological examination in
of intestinal tuberculosis; a hospital based study. J Postgrad Med Instit.
establishing the diagnosis in poor resource settings. 2008;22(2):152-56.
[21] Rajput MJ, Memon AS, Rani S, Memon AH. Clinicopathological profile
References and surgical management outcomes in patients suffering from intestinal
tuberculosis. JLUMHS. 2005;4:113-18.
[1] Park K, editor. Park’s textbook of Preventive & Social Medicine. 19th ed.
India: M/S Banarasidas Bhanot; 2007. pp.768. [22] Underwood MJ, Thompson MM, Sayers RD, Hall AW. Presentation of abdominal
tuberculosis to general surgeons. Br J Surg. 1992;79:1077-79.
PARTICULARS OF CONTRIBUTORS:
1. Associate Professor, Department of Pathology, Teerthanker Mahaveer Medical College & Research Centre, Moradabad, India.
2. Assistant Professor, Department of Pathology, Teerthanker Mahaveer Medical College & Research Centre, Moradabad, India.
3. Assistant Professor, Department of Pathology, Teerthanker Mahaveer Medical College & Research Centre, Moradabad, India.
4. Assistant Professor, Department of Pathology, Teerthanker Mahaveer Medical College & Research Centre, Moradabad, India.
5. Professor, Department of Pathology, Teerthanker Mahaveer Medical College & Research Centre, Moradabad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Seema Awasthi,
Associate Professor, Department of Pathology, Faculty Block-B, 201, TMU Campus, Moradabad, India. Date of Submission: Feb 05, 2015
E-mail : dr.seemaabhishek@yahoo.com Date of Peer Review: Feb 23, 2015
Date of Acceptance: Mar 30, 2015
Financial OR OTHER COMPETING INTERESTS: None. Date of Publishing: May 01, 2015
Journal of Clinical and Diagnostic Research. 2015 May, Vol-9(5): EC01-EC03 3
You might also like
- Abdominal Tuberculosis: A Diagnostic Dilemma - PMCDocument9 pagesAbdominal Tuberculosis: A Diagnostic Dilemma - PMCDiptanshu ShekharNo ratings yet
- Jurnal TB AbdomenDocument4 pagesJurnal TB AbdomenbelaNo ratings yet
- Abdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduDocument4 pagesAbdominal Tuberculosis in Nepal Medical College Teaching Hospital, KathmanduSavitri Maharani BudimanNo ratings yet
- Gastritis - Facts and Doubts: Original PaperDocument10 pagesGastritis - Facts and Doubts: Original Paperindah setiyaniNo ratings yet
- Multimodal Imaging of Fibrosing Mesenteric TuberculosisDocument6 pagesMultimodal Imaging of Fibrosing Mesenteric Tuberculosisdanielito1990No ratings yet
- Clinical, Imaging, and Endoscopic Profile of Patients With Abdominal TuberculosisDocument6 pagesClinical, Imaging, and Endoscopic Profile of Patients With Abdominal TuberculosisINDRINo ratings yet
- Pancreatic Tuberculosis Diagnosis UpdateDocument24 pagesPancreatic Tuberculosis Diagnosis UpdatesamudraandiNo ratings yet
- Infectious IleoceicitisDocument2 pagesInfectious IleoceicitisYandiNo ratings yet
- Jurnal DigesDocument9 pagesJurnal DigesRendy SusantoNo ratings yet
- Clinical Predictors of Ileocecal Tuberculosis: A Case SeriesDocument14 pagesClinical Predictors of Ileocecal Tuberculosis: A Case SeriesChristopher AsisNo ratings yet
- July 1991 B PDFDocument4 pagesJuly 1991 B PDFRhenofkunair0% (1)
- Intestinal Tuberculosis: A Diagnostic Challenge: Open Access Case DOI: 10.7759/cureus.13058Document4 pagesIntestinal Tuberculosis: A Diagnostic Challenge: Open Access Case DOI: 10.7759/cureus.13058ATIKA INDAH SARINo ratings yet
- Gill 2011Document4 pagesGill 2011qwerNo ratings yet
- Abd TBReviewDocument4 pagesAbd TBReviewdrelvNo ratings yet
- Systematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmentDocument16 pagesSystematic Review: Tuberculous Peritonitis - Presenting Features, Diagnostic Strategies and TreatmenthendraNo ratings yet
- Gallbladder Tuberculosis Mimicking Cholecystitis A Case Report 9712Document3 pagesGallbladder Tuberculosis Mimicking Cholecystitis A Case Report 9712cowok10blablablaNo ratings yet
- Adult Intussusception ReviewDocument6 pagesAdult Intussusception ReviewnurfitriaNo ratings yet
- Manuscript Info: International Journal of Advanced ResearchDocument5 pagesManuscript Info: International Journal of Advanced Researchadil2050No ratings yet
- Intestinal Tuberculosis: A Diagnostic Challenge: © 2017 John Wiley & Sons LTDDocument6 pagesIntestinal Tuberculosis: A Diagnostic Challenge: © 2017 John Wiley & Sons LTDLily SmithNo ratings yet
- Peritoneal Dialysis-Related Peritonitis Caused by Pseudomonas Species: Insight From A Post-Millennial Case SeriesDocument9 pagesPeritoneal Dialysis-Related Peritonitis Caused by Pseudomonas Species: Insight From A Post-Millennial Case SeriesDesi HutapeaNo ratings yet
- Ungaro2016 PDFDocument15 pagesUngaro2016 PDFAbraham SalvadorNo ratings yet
- 1 s2.0 S0140673623009662 MainDocument14 pages1 s2.0 S0140673623009662 MainKesia MaldonadoNo ratings yet
- Abcesele FicatuluiDocument4 pagesAbcesele FicatuluiMihaela AlinaNo ratings yet
- Sampling and Reporting of Inflammatory Bowel DiseaseDocument12 pagesSampling and Reporting of Inflammatory Bowel DiseaseDiego Fernando Ortiz TenorioNo ratings yet
- Clinical Presentation of Abdominal TuberculosisDocument4 pagesClinical Presentation of Abdominal TuberculosisRizky AmaliahNo ratings yet
- H. pylori gastritis and ulcer diseaseDocument6 pagesH. pylori gastritis and ulcer diseasetambamanuellaNo ratings yet
- Abdominal Tuberculosis Research ReviewDocument12 pagesAbdominal Tuberculosis Research ReviewrikarikaNo ratings yet
- Colitis: A Practical Approach to Colon and Ileum Biopsy InterpretationFrom EverandColitis: A Practical Approach to Colon and Ileum Biopsy InterpretationAnne Jouret-MourinNo ratings yet
- Gastritis and Carditis: University of British Columbia, Vancouver, British Columbia, CanadaDocument17 pagesGastritis and Carditis: University of British Columbia, Vancouver, British Columbia, CanadaJose SirittNo ratings yet
- Peritoneal Tuberculosis Mimiking Gastrointestinal Stromal TumorDocument3 pagesPeritoneal Tuberculosis Mimiking Gastrointestinal Stromal TumorIJAR JOURNALNo ratings yet
- Alternation of Gut Microbiota in Patients With Pulmonary TuberculosisDocument10 pagesAlternation of Gut Microbiota in Patients With Pulmonary TuberculosisNurul Hildayanti ILyasNo ratings yet
- Laroche 1998Document9 pagesLaroche 1998takechi takechiNo ratings yet
- 37poflee EtalDocument3 pages37poflee EtaleditorijmrhsNo ratings yet
- Surgical Interventions in Abdominal Tuberculosis: A Clinico-Pathological StudyDocument5 pagesSurgical Interventions in Abdominal Tuberculosis: A Clinico-Pathological StudySatwinder KaurNo ratings yet
- 1 s2.0 S0268960X22000182 MainDocument10 pages1 s2.0 S0268960X22000182 Mainafg_19No ratings yet
- Incidence of Tuberculosis in Cervical LymphadenopathyDocument4 pagesIncidence of Tuberculosis in Cervical Lymphadenopathyedy belajar572No ratings yet
- Tuberculous Peritonitis The Effectiveness of Diagnostic Laparoscopy and The Perioperative Infectious Prevention - A Case ReportDocument4 pagesTuberculous Peritonitis The Effectiveness of Diagnostic Laparoscopy and The Perioperative Infectious Prevention - A Case ReportDumitru RadulescuNo ratings yet
- Update Sydney SystemDocument16 pagesUpdate Sydney SystemMohammad IrfanNo ratings yet
- JCDR 8 NC07 PDFDocument3 pagesJCDR 8 NC07 PDFdr.deyshieNo ratings yet
- Abdominal Tuberculosis With An Acute Abdomen: Our Clinical ExperienceDocument3 pagesAbdominal Tuberculosis With An Acute Abdomen: Our Clinical Experiencedr.deyshieNo ratings yet
- Clinical presentation and management of abdominal tuberculosisDocument5 pagesClinical presentation and management of abdominal tuberculosisVic KeyNo ratings yet
- Helicobacter Pylori Infection in Gastritis and UlcersDocument25 pagesHelicobacter Pylori Infection in Gastritis and UlcersAri AldopiNo ratings yet
- Intestinal Tuberculosis With Abdominal ComplicationsDocument7 pagesIntestinal Tuberculosis With Abdominal ComplicationsTheodelinda Andreea DumitriuNo ratings yet
- Caz Bun 3Document7 pagesCaz Bun 3Dumitru RadulescuNo ratings yet
- Abdominal TBCDocument11 pagesAbdominal TBCNitin SainiNo ratings yet
- Tuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeDocument3 pagesTuberculous Ileal Perforation in Post-Appendicectomy PeriOperative Period: A Diagnostic ChallengeIOSRjournalNo ratings yet
- Rare Primary Tuberculosis in TonsilsDocument3 pagesRare Primary Tuberculosis in Tonsilsmanish agrawalNo ratings yet
- Gastritis and Gastropathy Perspectives From The EndoscopistDocument4 pagesGastritis and Gastropathy Perspectives From The Endoscopisthenrique.uouNo ratings yet
- JGH 13174Document9 pagesJGH 13174samudraandiNo ratings yet
- A Comprehensive Study of Intestinal ObstructionDocument9 pagesA Comprehensive Study of Intestinal ObstructionRoxana ElenaNo ratings yet
- Enterocolitis Neutropénica en Pacientes Pediátricos Con Leucemia Tratados Con QuimioterapiaDocument6 pagesEnterocolitis Neutropénica en Pacientes Pediátricos Con Leucemia Tratados Con QuimioterapiaIRINA SULEY TIRADO PEREZNo ratings yet
- Jurnal AppendiksDocument6 pagesJurnal AppendiksSiti anasya CahyaNo ratings yet
- Animals 12 02489 With CoverDocument17 pagesAnimals 12 02489 With Coverpalsantanu8837276365No ratings yet
- Wound Infection-LaparoscopicDocument4 pagesWound Infection-LaparoscopicIvan InkovNo ratings yet
- Practical Approach To Diagnosis of GastritisDocument9 pagesPractical Approach To Diagnosis of GastritisYao RaNo ratings yet
- Acute PyelonephritisDocument13 pagesAcute Pyelonephritiskevin maulandaNo ratings yet
- CASE REPORT Colitis TuberculosisDocument3 pagesCASE REPORT Colitis TuberculosisIfan RizkyNo ratings yet
- Diagnosis of Abdominal Tuberculosis: Lessons Learned Over 30 Years: Pectoral AssayDocument7 pagesDiagnosis of Abdominal Tuberculosis: Lessons Learned Over 30 Years: Pectoral AssayKusuma IntanNo ratings yet
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- Diseases of the Liver and Biliary TreeFrom EverandDiseases of the Liver and Biliary TreeAnnarosa FloreaniNo ratings yet
- Popular Telugu Novel "Prema DeepikaDocument2 pagesPopular Telugu Novel "Prema Deepikasindhu60% (5)
- 250 - Windows ShellcodingDocument116 pages250 - Windows ShellcodingSaw GyiNo ratings yet
- Keerai BenefitsDocument3 pagesKeerai BenefitsjnaguNo ratings yet
- DocxDocument5 pagesDocxFelicya Angel Ivy LynnNo ratings yet
- 12th English Elec Lyp 2013 DelhiDocument10 pages12th English Elec Lyp 2013 DelhiKanishkha SivasankarNo ratings yet
- Power2 Leading The Way in Two-Stage TurbochargingDocument4 pagesPower2 Leading The Way in Two-Stage TurbochargingМаксим АгеевNo ratings yet
- Hatch-Slack PathwayDocument10 pagesHatch-Slack Pathwaychurail khanNo ratings yet
- September/News/Septiembre 2013: P.O. Box 44 WWW - Hecatomberecords.esDocument7 pagesSeptember/News/Septiembre 2013: P.O. Box 44 WWW - Hecatomberecords.eshecatomberecordsNo ratings yet
- How To Comp For A Vocalist - Singer - The Jazz Piano SiteDocument5 pagesHow To Comp For A Vocalist - Singer - The Jazz Piano SiteMbolafab RbjNo ratings yet
- IEC 61850 Configuration of A Phoenix Contact IED: User ManualDocument68 pagesIEC 61850 Configuration of A Phoenix Contact IED: User ManualHarold PuinNo ratings yet
- Sun Temple, Modhera: Gudhamandapa, The Shrine Hall Sabhamandapa, The AssemblyDocument11 pagesSun Temple, Modhera: Gudhamandapa, The Shrine Hall Sabhamandapa, The AssemblyShah PrachiNo ratings yet
- Everyman A Structural Analysis Thomas F. Van LaanDocument12 pagesEveryman A Structural Analysis Thomas F. Van LaanRodrigoCarrilloLopezNo ratings yet
- The Story of A Seagull and The Cat Who Taught Her To Fly PDFDocument46 pagesThe Story of A Seagull and The Cat Who Taught Her To Fly PDFYo Seven67% (3)
- Indigenous Peoples SyllabusDocument9 pagesIndigenous Peoples Syllabusapi-263787560No ratings yet
- Laws On Banks-A4Document16 pagesLaws On Banks-A4Steven OrtizNo ratings yet
- TRW WHP PDFDocument20 pagesTRW WHP PDFmonica_codNo ratings yet
- Forming Plurals of NounsDocument5 pagesForming Plurals of NounsCathy GalNo ratings yet
- Grade 6 Quarter 3 WHLP WEEK 4Document3 pagesGrade 6 Quarter 3 WHLP WEEK 4JaneDandanNo ratings yet
- Wonder Woman: Directed byDocument4 pagesWonder Woman: Directed byRoxana Ioana DumitruNo ratings yet
- Underwater Cutting and Welding Equipment - 89250054 - AbDocument38 pagesUnderwater Cutting and Welding Equipment - 89250054 - AbAhmed Adel100% (1)
- Birla Institute of Technology and Science, Pilani: Pilani Campus AUGS/ AGSR DivisionDocument5 pagesBirla Institute of Technology and Science, Pilani: Pilani Campus AUGS/ AGSR DivisionDeep PandyaNo ratings yet
- Multimedia ExerciseDocument1 pageMultimedia ExercisemskgghNo ratings yet
- Jha 2018Document4 pagesJha 2018AditiNo ratings yet
- Sales Confirmation: Alpha Trading S.P.A. Compagnie Tunisienne de NavigationDocument1 pageSales Confirmation: Alpha Trading S.P.A. Compagnie Tunisienne de NavigationimedNo ratings yet
- MGT211 RecruitmentDocument16 pagesMGT211 RecruitmentEdward N MichealNo ratings yet
- Guide to Preparing STEM Fellowship ApplicationsDocument14 pagesGuide to Preparing STEM Fellowship ApplicationsNurrahmiNo ratings yet
- Race, Gender, and the Politics of Visible IdentityDocument21 pagesRace, Gender, and the Politics of Visible IdentityrebenaqueNo ratings yet
- + or Cryptopotato - Com or U.today-Domain Domains-UsDocument128 pages+ or Cryptopotato - Com or U.today-Domain Domains-UsMalkeet SinghNo ratings yet
- Lucid Dreaming Fast TrackDocument3 pagesLucid Dreaming Fast TrackWulan Funblogger50% (2)
- MMRP Narrative Report FormatDocument3 pagesMMRP Narrative Report FormatClarence Dave TolentinoNo ratings yet