Professional Documents
Culture Documents
ECP - Immulite 1000
Uploaded by
Hida KurticCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ECP - Immulite 1000
Uploaded by
Hida KurticCopyright:
Available Formats
ECP
For use on the IMMULITE®
and IMMULITE® 1000 systems
IMMULITE /IMMULITE 1000 ECP
® ®
1,10
airway responsiveness, and spirometry.
English Atopic serum samples have higher ECP
levels than nonatopic control samples,
even when the circulating eosinophil count
9
Intended Use: For research use only with remains within the normal range. In
the IMMULITE and IMMULITE 1000 seasonal asthmatic patients, ECP
Analyzers. Not for use in diagnostic measurements reflect changes in disease
1,9
procedures. activity throughout the year. Roquet,
Catalog Number: LKEOZ (50 tests) et al. reported significant correlations
between ECP levels and bronchial
Test Code: ECP Color: Aqua hyperreactivity in mildly asthmatic
6
CDC Analyte Identifier Code: 1616 patients. Tomassini, et al. showed that
CDC Test System Identifier Code: 10418 serum ECP concentrations exceed
CLIA Complexity Category: Moderate normal, control levels in both IgE-
mediated and non-IgE-mediated atopic
conditions. Serum ECP measurements
Summary and Explanation avoid inconsistencies inherent in
Eosinophils, originating from bone-marrow subjective asthma assessments.
stem cells, appear in large numbers at
inflammation sites and in response to Serum ECP concentrations can indicate
2,3
certain parasitic infections. These the severity of certain skin disorders.
leukocytes, when mature, reside mostly in ECP's neuronal toxicity might contribute to
tissues, but about 1% of the eosinophil itching disorders; patients with certain skin
population circulates in the blood. disorders, such as papular erythematous
Activated eosinophils degranulate to eruptions and prurigo nodularis, displayed
release four highly basic proteins into the increased serum ECP levels, which
8,3
surrounding tissue. The granular proteins, normalized when the conditions healed.
which can kill parasites and some Several groups found that serum ECP
mammalian cells, might cause the tissue concentrations reflect atopic dermatitis
2,3
damage associated with asthma and other (AD) activity. The commonly used
inflammatory diseases. Eosinophil clinical scoring system for atopic
activation accompanies a wide range of dermatitis records lichenification, loss of
inflammatory conditions, including sleep, erythema, papules, pruritus, and
bronchial asthma, atopic dermatitis, excoriations. Czech, et al. showed that
rhinitis, allergic eye inflammation, allergic ECP correlates with each of these
middle ear effusion, parasitic and bacterial symptoms and most highly correlates with
infections, autoimmune diseases, and the total clinical score. Although altered
chronic fatigue syndrome.
11 immunological parameters accompany
atopic dermatitis, measured serum IgE
Among the four basic granule proteins, concentrations did not correlate with some
eosinophil cationic protein (ECP) has of the clinical symptoms.
2
proven a useful monitor for many active
11
inflammatory diseases. ECP
concentrations in plasma and certain other
Principle of the Procedure
body fluids increase during inflammatory IMMULITE/IMMULITE 1000 ECP is a
reactions marked by activated eosinophils. solid-phase, two-site chemiluminescent
Produced by eosinophils exclusively, ECP immunometric assay.
is toxic to neurons, some epithelial cell Incubation Cycles: 1 × 30 minutes.
lines, and isolated myocardial cells. The
positively charged protein binds to heparin
and inhibits blood coagulation.
Specimen Collection
13
Collect blood by venipuncture into
Several studies report high individual and Becton Dickinson SST vacutainer
group correlations between ECP levels tubes, noting the time of collection. Fill
and clinical asthma symptoms, such as collection tubes completely, gently invert,
increases in peak expiratory flow (PEF), and let the blood clot for 60–120 minutes
prn ("as needed") inhaled β2-agonist,
2 IMMULITE/IMMULITE 1000 ECP (PILKEO-6, 2005-03-14)
at room temperature (15–28°C). potentially explosive metal azides in lead
Centrifuge at 1,000–1,300×g for 10 and copper plumbing.
minutes at room temperature, and
Chemiluminescent Substrate: Avoid
separate the serum from the cells. Please
contamination and exposure to direct
note that blood sample processing sunlight. (See insert.)
parameters, including time and
temperature of blood clotting, Water: Use distilled or deionized water.
centrifugation, and sample storage, may
7
impact measured ECP concentration. Materials Supplied
Variations in blood processing parameters Components are a matched set. The
between sampling may cause inconsistent barcode labels are needed for the assay.
ECP measurements.
Plasma or hemolyzed samples should ECP Test Units (LEO1)
not be used. Each barcode-labeled unit contains one
The use of an ultracentrifuge is bead coated with monoclonal murine anti-
recommended to clear lipemic samples. ECP antibody. Stable at 2–8°C until
expiration date.
Centrifuging serum samples before a LKEOZ: 50 units.
complete clot forms may result in the
presence of fibrin. Allow the Test Unit bags to come to room
temperature before opening. Open by
Blood collection tubes from different cutting along the top edge, leaving the
manufacturers may yield differing values, ziplock ridge intact. Reseal the bags to
depending on materials and additives, protect from moisture.
including gel or physical barriers, clot
activators and/or anticoagulants. ECP Reagent Wedge (LEO2)
Volume Required: 5 µL serum. (Sample With barcode. 6.5 mL alkaline
cup must contain at least 100 µL more phosphatase (bovine calf intestine)
than the total volume required.) conjugated to polyclonal rabbit anti-ECP
antibody in buffer, with preservative. Store
Storage: 7 days at 2–8°C or up to 3 capped and refrigerated: stable at 2–8°C
12
months at –20°C. until expiration date. Recommended
Store the serum samples in polystyrene or usage is within 30 days after opening
polypropylene rather than glass tubes, to when stored as indicated.
avoid a decrease in ECP values. Do not LKEOZ: 1 wedge.
attempt to thaw frozen specimens by
heating them in a waterbath. Avoid ECP Adjustors (LEOL, LEOH)
repeated freeze/thaw cycles. Two vials containing lyophilized (Low and
High) ECP in an ECP-free nonhuman
Warnings and Precautions serum/buffer matrix, with preservative.
Reconstitute each vial with 2.0 mL distilled
For research use only. Not for use in
or deionized water. Mix by gentle swirling
diagnostic procedures.
or inversion until the lyophilized material is
Reagents: Store at 2–8°C. Dispose of in fully dissolved. Aliquot and freeze
accordance with applicable laws. immediately after reconstitution. Stable at
Follow universal precautions, and handle –20°C for 6 months after reconstitution.
all components as if capable of LKEOZ: 1 set.
transmitting infectious agents. Source
materials derived from human blood were ECP Controls (LEOC1, LEOC2)
tested and found nonreactive for syphilis; Two vials containing lyophilized ECP in an
for antibodies to HIV 1 and 2; for hepatitis ECP-free nonhuman serum/buffer matrix,
B surface antigen; and for antibodies to with preservative. Reconstitute each vial
hepatitis C. with 2.0 mL distilled or deionized water.
Mix by gentle, intermittent swirling. Aliquot
Sodium azide, at concentrations less than and freeze immediately after
0.1 g/dL, has been added as a reconstitution. Stable at –20°C for
preservative. On disposal, flush with large 6 months after reconstitution.
volumes of water to prevent the buildup of LKEOZ: 1 set.
IMMULITE/IMMULITE 1000 ECP (PILKEO-6, 2005-03-14) 3
Refer to the control insert for [See Boscato LM, Stuart MC. Heterophilic
concentration levels. antibodies: a problem for all
immunoassays. Clin Chem 1988:34:27-
Kit Components 33.]
Supplied Separately
Performance Data
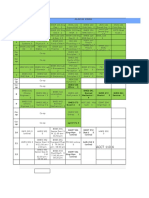
ECP Sample Diluent (LEOZ) See Tables and Graphs for data
For the manual dilution of patient samples. representative of the assay's performance.
One vial 25 mL of processed, ECP-free Results are expressed in ng/mL. (Unless
nonhuman serum/buffer, with otherwise specified, all results were
preservative. Stable at 2–8°C for 30 days generated on serum samples collected in
after opening, or for 6 months (aliquotted) Becton Dickinson SST vacutainer tubes.)
at –20°C.
Calibration Range: up to 200 ng/mL.
LSUBX: Chemiluminescent Substrate
Analytical Sensitivity: 0.2 ng/mL.
LPWS2: Probe Wash Module
LKPM : Probe Cleaning Kit High-dose Hook Effect:
LCHx-y: Sample Cup Holders (barcoded) None up to 8,000 ng/mL
LSCP: Sample Cups (disposable) Linearity: Samples were assayed under
LSCC: Sample Cup Caps (optional) various dilutions. (See "Linearity" table for
Also Required representative data.)
Sample transfer pipets, distilled or Recovery: Samples spiked 1 to 19 with
deionized water. three ECP solutions (100, 600 and
1,680 ng/mL) were assayed. (See
Assay Procedure "Recovery" table for representative data.)
Note that for optimal performance, it is
important to perform all routine References
maintenance procedures as defined in the
1) D'Amato G, Liccardi G, et al. Measurement of
IMMULITE or IMMULITE 1000 Operator's serum levels of eosinophil cationic protein to
Manual. monitor patients with seasonal respiratory
See the IMMULITE or IMMULITE 1000 allergy induced by Parietaria pollen (treated and
untreated with specific immunotherapy). Allergy
Operator's Manual for: preparation, setup,
1996;51:245-50. 2) Czech W, Krutmann J, et al.
dilutions, adjustment, assay and quality Serum eosinophil cationic protein (ECP) is a
control procedures. sensitive measure for disease activity in atopic
Visually inspect each Test Unit for the dermatitis. Br J Dermatol 1992;126:351-5. 3)
Juhlin L, Venge P. Eosinophilic Cationic Protein
presence of a bead before loading it onto (ECP) in skin disorders. Acta Derm Venereol
the system. 1991;71:495-501. 4) Peterson CG, Enander I, et
Recommended Adjustment Interval: al. Radioimmunoassay of human eosinophil
cationic protein (ECP) by an improved method.
2 weeks.
Establishment of normal levels in serum and
Quality Control Samples: Use the turnover in vivo. Clin Exper Allerg 1991;21:561-
control(s) supplied with the kit. 7. 5) Reimert CM, Poulsen LK, et al.
Measurement of eosinophil cationic protein
(ECP) and eosinophil protein X/eosinophil-
Expected Values derived neurotoxin (EPX/EDN). Time and
Each laboratory should establish its own temperature dependent spontaneous release in
vitro demands standardized sample processing.
reference ranges.
J Immun Meth 1993;166:183-90. 6) Roquet A,
Hallden G, et al. Eosinophil activity markers in
Limitations peripheral blood have high predictive value for
bronchial hyperreactivity in patients with
Variations in blood processing parameters suspected mild asthma. Allergy 1996;51:482-8.
could cause inconsistent ECP 7) Rubira N, Rodrigo MJ, et al. Blood sample
7
measurements. processing affect on cationic protein
concentraion. Ann Allergy Asthma Immunol
Heterophilic antibodies in human serum
1997;78:394-8. 8) Sunohara N, Furukawa S, et
can react with the immunoglobulins al. Neurotoxicity of human eosinophils towards
included in the assay components causing periperal nerves. J Neurolog Sci 1989;92:1-7. 9)
interference with in vitro immunoassays. Tomassini M, Magrini L, et al. Serum levels of
4 IMMULITE/IMMULITE 1000 ECP (PILKEO-6, 2005-03-14)
eosinophil cationic protein in allergic diseases Linearity (ng/mL)
and natural allergen exposure. J Allerg Clin
Immun 1996;97:1350-5. 10) Vatrella A, Dilution1 Observed2 Expected3 %O/E4
Ponticiello A, et al. Serum eosinophil cationic
1 8 in 85 19.1 — —
protein (ECP) as a marker of disease activity
and treatment efficacy in seasonal asthma. 4 in 8 9.6 9.6 100%
Allergy 1996;51:547-55. 11) Wardlaw AJ.
2 in 8 4.7 4.8 98%
Eosinophils in the 1990s: new perspectives on
their role in health and disease. Postgrad Med J 1 in 8 2.0 2.4 83%
1994;70:536-552. 12) Data on file. 13) National
2 32 in 32 45 — —
Committee for Clinical Laboratory Standards,
Procedures for the collection of diagnostic blood 16 in 32 21 23 91%
specimens by venipuncture, 3rd ed, NCCLS
8 in 32 11.0 11.3 97%
Document H3-A3, 1991.
4 in 32 5.0 5.6 89%
Technical Assistance 2 in 32 2.5 2.8 89%
In the United States, available for 1 in 32 1.2 1.4 86%
research use only. Contact DPC's 3 32 in 32 86 — —
Technical Services department. 16 in 32 42 43 98%
Tel: 800.372.1782 or 973.927.2828
Fax: 973.927.4101. Outside the United 8 in 32 20 22 91%
States, contact your National Distributor. 4 in 32 9.0 10.8 83%
The Quality System of Diagnostic Products 2 in 32 4.8 5.4 89%
Corporation is registered to ISO 13485:2003.
1 in 32 2.2 2.7 81%
4 32 in 32 93 — —
Tables and Graphs 16 in 32 48 47 102%
8 in 32 23 23 100%
4 in 32 12.0 11.6 103%
Recovery (ng/mL) 2 in 32 5.7 5.8 98%
Solution1 Observed2 Expected3 %O/E4 1 in 32 2.7 2.9 93%
1 — 9.8 — —
A 13 14 93%
B 33 39 85%
C 84 93 90%
2 — 11 — — Diagnostic Products Corporation
Corporate Offices
A 15 15 100%
5210 Pacific Concourse Drive
B 35 40 88% Los Angeles, CA 90045-6900
C 82 94 87% USA
3 — 22 — — 2005-03-14
A 28 26 108% PILKEO – 6
B 48 51 94%
C 114 105 109%
IMMULITE/IMMULITE 1000 ECP (PILKEO-6, 2005-03-14) 5
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- Case History 33Document4 pagesCase History 33Hida KurticNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Il 943Document14 pagesIl 943Hida KurticNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hitachi 902 MoreDocument2 pagesHitachi 902 MoreHida KurticNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Erasmus+ International Credit MobilityDocument34 pagesErasmus+ International Credit MobilityHida KurticNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Practical Mix Design of Concrete2Document3 pagesPractical Mix Design of Concrete2Jiabin LiNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- 2 PassivetransportDocument8 pages2 PassivetransportFayeNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Joseph Brazier, Ltd. Et Al v. Specialty Bar Products Company - Document No. 7Document3 pagesJoseph Brazier, Ltd. Et Al v. Specialty Bar Products Company - Document No. 7Justia.comNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Tle q4 l5 Quiz Google FormsDocument5 pagesTle q4 l5 Quiz Google FormsEdilbert Bonifacio GayoNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- PolicySchedule PDFDocument1 pagePolicySchedule PDFSandeep Borse100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Ombw003a Five Inch BwsDocument39 pagesOmbw003a Five Inch BwsNavaneethan NatarajanNo ratings yet
- Data Mining ToolsDocument9 pagesData Mining Toolspuneet0303No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Holmstrom1982 Moral Hazard in TeamsDocument18 pagesHolmstrom1982 Moral Hazard in TeamsfaqeveaNo ratings yet
- Table of Specifications With Test in Science - Quarter 4 - (Week 3 and Week 4)Document4 pagesTable of Specifications With Test in Science - Quarter 4 - (Week 3 and Week 4)Sarah Jane Lagura Rele50% (2)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Adime 2Document13 pagesAdime 2api-496164982No ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Dokumen - Tips Strength of Materials 5691845f3ea8eDocument13 pagesDokumen - Tips Strength of Materials 5691845f3ea8eJay GeeNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Ucla Dissertation Filing DatesDocument7 pagesUcla Dissertation Filing DatesBestOnlinePaperWritingServiceCanada100% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- BSMS Drexel ScheduleDocument4 pagesBSMS Drexel ScheduleAmy ZhiNo ratings yet
- Companies in KeralaDocument14 pagesCompanies in KeralasumeshmhrNo ratings yet
- Practical 9: Enthalpy Change of ReactionDocument4 pagesPractical 9: Enthalpy Change of ReactionJulia QistinaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Esp-English For Tour GuidesDocument13 pagesEsp-English For Tour GuidestijehNo ratings yet
- Essay 1 DraftDocument1 pageEssay 1 Draftgdx3100% (3)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Protein MetabolismDocument78 pagesProtein MetabolismU2002862 STUDENTNo ratings yet
- Special Theory of RelativityDocument16 pagesSpecial Theory of RelativityBrigita SteffyNo ratings yet
- De Quervains TenosynovitisDocument2 pagesDe Quervains TenosynovitisomboNo ratings yet
- Measurement of Hardness of Rubber CompoundsDocument8 pagesMeasurement of Hardness of Rubber CompoundsDarshan VariaNo ratings yet
- Sachet MarketingDocument7 pagesSachet MarketingTom JohnNo ratings yet
- 119 - Circular - 2021 - 211124 - 165700 (1) - 1Document3 pages119 - Circular - 2021 - 211124 - 165700 (1) - 1manoj jainNo ratings yet
- Valley Line LRT Preliminary DesignDocument26 pagesValley Line LRT Preliminary DesigncaleyramsayNo ratings yet
- USEFUL TIPS For Repairing LAPTOPDocument17 pagesUSEFUL TIPS For Repairing LAPTOPGeronJosephusLofrancoManaiz100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Cut Pieces: From Flat Plates, Strips and Coil Stock. A. Shearing B. Bend Allowance C. Forming Dies D. Spring BackDocument100 pagesCut Pieces: From Flat Plates, Strips and Coil Stock. A. Shearing B. Bend Allowance C. Forming Dies D. Spring BackJade DigNo ratings yet
- UNIT 2 - LESSON 1 - Overview To Qualitative ResearchDocument31 pagesUNIT 2 - LESSON 1 - Overview To Qualitative ResearchmikkaellaNo ratings yet
- Hotels Review Classification FinalDocument34 pagesHotels Review Classification FinalPurvaNo ratings yet
- Arch MLCDocument471 pagesArch MLCJoseNo ratings yet
- Banking Financial InstitutionsDocument252 pagesBanking Financial Institutionspraise ferrerNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)