Professional Documents
Culture Documents
HHS Public Access: Origin and Functions of Tissue Macrophages
Uploaded by
Brandi MichelleOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HHS Public Access: Origin and Functions of Tissue Macrophages
Uploaded by
Brandi MichelleCopyright:
Available Formats
HHS Public Access
Author manuscript
Immunity. Author manuscript; available in PMC 2015 June 17.
Author Manuscript
Published in final edited form as:
Immunity. 2014 July 17; 41(1): 21–35. doi:10.1016/j.immuni.2014.06.013.
Origin and Functions of Tissue Macrophages
Slava Epelman1,*, Kory J. Lavine1, and Gwendalyn J. Randolph1,2,*
1Centerfor Cardiovascular Research, Division of Cardiology, Department of Medicine,
Washington University School of Medicine, St. Louis, MO 63110, USA
2Departmentof Pathology and Immunology, Washington University School of Medicine, St. Louis,
MO 63110, USA
Author Manuscript
Abstract
Macrophages are distributed in tissues throughout the body and contribute to both homeostasis and
disease. Recently, it has become evident that most adult tissue macrophages originate during
embryonic development and not from circulating monocytes. Each tissue has its own composition
of embryonically derived and adult-derived macrophages, but it is unclear whether macrophages
of distinct origins are functionally interchangeable or have unique roles at steady state. This new
understanding also prompts reconsideration of the function of circulating monocytes. Classical
Ly6chi monocytes patrol the extravascular space in resting organs, and Ly6clo nonclassical
monocytes patrol the vasculature. Inflammation triggers monocytes to differentiate into
macrophages, but whether resident and newly recruited macrophages possess similar functions
during inflammation is unclear. Here, we define the tools used for identifying the complex origin
Author Manuscript
of tissue macrophages and discuss the relative contributions of tissue niche versus ontological
origin to the regulation of macrophage functions during steady state and inflammation.
Introduction
The Phagocyte: Ilya Metchnikoff and the Historical Perspective
Macrophages were first discovered late in the 19th century by Ilya Metchnikoff and are
evolutionary conserved phagocytes that evolved more than 500 million years ago (Cooper
and Alder, 2006; Tauber, 2003). Metchnikoff combined both evolutionary and ontological
perspectives, which is particularly relevant in light of recent findings that have
revolutionized the macrophage field. In the 1960s, van Furth proposed that all tissue
macrophages originate from circulating adult blood monocytes, which has been the
Author Manuscript
prevailing view for the last 40 years despite evidence that tissue macrophages are
independent of circulating monocytes (van Furth and Cohn, 1968; Volkman et al., 1983;
Sawyer et al., 1982). However, in the last few years, a series of more definitive publications
have drastically revised our understanding of macrophage origin by demonstrating that
many resident tissue macrophages are in fact established during embryonic development and
persist into adulthood independently of blood monocyte input in the steady state (Ginhoux et
©2014 Elsevier Inc.
*
Correspondence: sepelman@dom.wustl.edu (S.E.), grandolph@path.wustl.edu (G.J.R.).
Epelman et al. Page 2
al., 2010; Schulz et al., 2012; Yona et al., 2013; Hashimoto et al., 2013; Epelman et al.,
Author Manuscript
2014; Guilliams et al., 2013; Jakubzick et al., 2013). Metchnikoff defined the embryonic
establishment of macrophages in the starfish, which has no formal vascular system.
Accordingly, he argued for inflammation independent of blood vessels, countering Julius
Cohnheim’s duly influential claims that “there is no inflammation without blood vessels.”
Thus, in the 21st century, we have come full circle to these debates with the reality that
inflammation, even in organisms anatomically more complex than starfish, centrally
involves macrophages but can occur through mechanisms that are both dependent and
independent of monocyte recruitment from the vasculature. Self-sustaining resident
macrophages already present in the tissue make this possible.
As our tools develop, we continue to refine our understanding of tissue macrophages and
can now further delineate multiple distinct embryonically derived macrophage lineages.
Several detailed review articles describing different aspects of macrophage ontogeny and
Author Manuscript
function have been published (Sieweke and Allen, 2013; Davies et al., 2013a; Wynn et al.,
2013). Although a novel concept in and of itself, the dichotomy between embryonically
derived and adult-derived macrophage populations does not fully encapsulate the entire
complexity and diversity found among tissue macrophages. Intriguingly, tissue macrophages
of differing ontological origins coexist, and when assessed as a group, they perform
specialized, organ-specific functions. The goal of this review is to highlight emerging
questions in the field, such as to what extent macrophage ontogeny versus the tissue niche
dictates a macrophage’s function. Are we missing critical insight by not parsing macrophage
function on the basis of origin? To what extent is there redundancy between adult-
monocyte-derived macrophages and different resident macrophage subsets? We will utilize
this framework to discuss how subsets of tissue macrophages and circulating monocytes
originate, how expansion of tissue macrophages is regulated when homeostasis is disrupted,
Author Manuscript
and what functions can be ascribed to individual subsets and lineages.
Understanding the Tools Used for Defining Macrophage Ontogeny
During early gestation (embryonic day 6.5 [E6.5]–E8.5), macrophages are first observed and
expand in the extraembryonic yolk sac during what is termed primitive hematopoiesis
(Samokhvalov, 2014) (see Figure 1). At this stage in development, macrophages are the only
“white blood cell” produced, because restricted progenitors in the yolk sac give rise only to
macrophages and red blood cells. This limited hematopoietic cell diversity is reminiscent of
the Drosophila immune system (Makhijani and Bruückner, 2012) and indicative of the
conserved origin of the yolk-sac-derived macrophage lineage. Subsequently (E8.5–E10.5),
definitive hematopoietic stem cells (HSCs) emerge from the aorta-gonad-mesonephros and
Author Manuscript
give rise to all immune lineages. Beginning at E10.5, HSCs migrate to the fetal liver, which
then serves as the major hematopoietic organ during the remainder of embryonic
development. Only in the perinatal period do traditional bone marrow HSCs become the
primary site of hematopoiesis and produce the full complement of immune lineages (Orkin
and Zon, 2008).
During embryonic development, transcription factor usage and surface-marker expression
differ between yolk-sac-derived and definitive-HSC-derived macrophages. Definitive HSCs
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 3
are completely dependent on the transcription factor MYB, whereas yolk-sac-derived
Author Manuscript
progenitors develop independently of MYB (Schulz et al., 2012). Furthermore, during
embryogenesis, yolk-sac-derived macrophages have a characteristic CX3CR1hi
F4/80hiCD11blo expression pattern (Schulz et al., 2012; Yona et al., 2013; Hashimoto et al.,
2013; Epelman et al., 2014). Unfortunately, many adult resident tissue macrophages that
originate during embryonic development alter the expression of cell-surface markers as the
animal matures, hindering the ability to precisely track macrophage populations. Clear
examples include embryonically established tissue macrophages that express CX3CR1
during development (lung and peritoneal macrophages and liver Kupffer cells) but lose
expression after birth (Yona et al., 2013).
Genetic fate-mapping techniques give us the ability to precisely identify and track different
embryonic macrophage populations into adulthood, and when combined with parabiotic and
adoptive-transplant studies, they give us the ability to discern the relationship between
Author Manuscript
macrophages and circulating blood monocytes. Fate-mapping studies utilize the principle of
genetic recombination to permanently label cells (and all subsequent progeny) on the basis
of the recombination-induced expression of a reporter gene that is under the control of a
constitutive promoter (typically Rosa26). Genetic techniques have evolved to include
inducible systems, where temporally controlling recombination facilitates precise labeling of
embryonic populations and tracking into adulthood. Below, we will discuss in detail
experimental evidence that undergirds the recently revised view of macrophage origins and
identify both the strengths and the limitations of each approach (see a summary of tools used
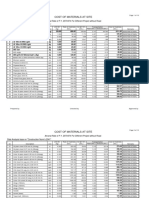
for defining macrophage origin in Table 1).
The inducible runt-related transcription factor 1 (Runx1CreER)-based system takes advantage
of the early expression of Runx1 in the yolk sac at ~E7.0, which occurs prior to the
Author Manuscript
development of definitive HSCs (Samokhvalov et al., 2007). Labeling of E7.0 Runx1-
expressing yolk-sac-derived macrophages demonstrates that they persist faithfully into
adulthood as microglia. Skin Langerhans cells contain both yolk-sac-derived and fetal-
monocyte-derived populations, but fetal-monocyte-derived macrophages have become the
dominant lineage over time (Hoeffel et al., 2012; Ginhoux et al., 2010). Whereas early
labeling techniques (prior to E7.5) enable specific tracking of yolk-sac-derived macrophages
(such as microglia), labeling between E8.0 and E10.5 leads to recombination in both yolk-
sac-derived macrophages and early definitive HSCs, which migrate to the fetal liver and
give rise to blood monocytes and lymphocytes (Ginhoux et al., 2010; Samokhvalov et al.,
2007). As a result, the ability of Runx1CreER to differentiate between tissue macrophages and
blood monocytes during later developmental stages becomes obscured.
The inducible Csf1rCreER has also been used for fate-mapping approaches. Initially, it was
Author Manuscript
observed that E8.5-labeled (yolk-sac-derived macrophages) seed virtually all developing
tissues in the embryo and show variable persistence into adulthood (Schulz et al., 2012).
Similar to Runx1CreER, Csf1rCreER used at E8.5 in a separate study achieved ~30% labeling
of yolk-sac-derived macrophages in the embryo and persistent labeling of microglia at the
same rate in adults, confirming the near exclusive yolk sac origin of these cells (Epelman et
al., 2014). The only other adult organs that retained significant numbers of yolk-sac-derived
macrophages that originated from E8.5 were the heart and liver, suggesting that the
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 4
persistence of early yolk-sac-derived macrophages might be more restricted than currently
Author Manuscript
appreciated. However, given that yolk sac progenitors migrate to the fetal liver at later
stages of development, the possibility exists that these progenitors can continue to give rise
to adult tissue macrophages. Unlike using Runx1CreER, using Csf1rCreER to label at E8.5 did
not result in labeling of adult circulating blood monocytes, suggesting that a longer window
for fate-mapping studies might exist. Two important caveats should be highlighted. First,
unlike Runx1CreER, Csf1rCreER is a transgene and might not report native gene expression in
all conditions. Second, the precision of any tamoxifen-inducible system that requires
temporal activation is limited because of the half-life of tamoxifen. For example, labeling
early yolk sac progenitors at E8.5 could be confounded by the persistence of tamoxifen in
tissue and labeling at later developmental stages, which underscores the importance of
monitoring recombination not only in tissue macrophages but also in later HSC-derived
cells.
Author Manuscript
Adult definitive HSCs transiently pass through a FLT3+ stage during differentiation into all
lineages (myeloid, lymphoid, megakarocyte, and erythroid cells), which can be exploited
genetically (Flt3Cre) for labeling adult-definitive-HSC-derived cells (Boyer et al., 2011).
What is clear is that Flt3-Cre+ blood monocytes do not replace Flt3-Cre− tissue macrophage
populations, even over extended periods of time (Epelman et al., 2014; Hashimoto et al.,
2013; Schulz et al., 2012). Interpreting the ontological origin of Flt3-Cre− macrophages
must be handled with care because it might be tempting to assume that the entire population
developed from yolk-sac-derived progenitors, but this remains unclear. During situations
where there is high demand (after macrophage depletion), the efficiency of Flt3Cre-
dependent recombination within myeloid cells is reduced in comparison to the steady state.
This represents a general limitation of Cre-dependent lineage-tracing systems. For example,
after adoptive transplant of E14.5 fetal-liver definitive HSCs into sublethally irradiated adult
Author Manuscript
animals, it takes ~8 weeks for Flt3Cre recombination to reach steady state in circulating
blood monocytes. Prior to 8 weeks posttransplant, large numbers of Flt3-Cre− blood
monocytes differentiate into long-lasting resident tissue macrophages (Epelman et al., 2014).
Therefore, during times of high monocyte demand, HSC-derived monocytes appear to
originate in a FLT3-independent fashion (Flt3-Cre−).
Additional complexity surrounds the observation that during early embryonic development,
<5% of phenotypically MYB-dependent macrophages (HSC derived) display Flt3Cre-
dependent recombination (Epelman et al., 2014). On the basis of available data, these cells
might be derived from fetal-liver monocytes. Therefore, it is possible that Flt3-Cre− tissue
macrophages in the adult consist of a mixed population containing macrophages derived
from both the yolk sac and fetal monocytes (Epelman et al., 2014) (see Figure 1). The
Author Manuscript
ontological and functional relationship between Flt3-Cre+ versus Flt3-Cre− fetal monocytes
and adult-monocyte-derived macrophages is undefined. Conversely, it might be tempting to
assume that Flt3-Cre+ tissue macrophages are continually replenished by Flt3-Cre+
circulating blood monocytes. Adoptive transplant and parabiotic studies suggest that in the
majority of organs, HSC-derived macrophages—except for gut CX3CR1hi macrophages,
cardiac CCR2+ macrophages, and dermal macrophage populations—also exist
autonomously from circulating blood monocytes (Hashimoto et al., 2013; Epelman et al.,
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 5
2014; Yona et al., 2013; Jakubzick et al., 2013). Consistent with these observations, lung
Author Manuscript
macrophages that reside in the alveolus develop shortly after birth from HSC-derived fetal
monocytes but are not replaced by circulating adult monocytes during parabiosis studies
(Guilliams et al., 2013; Jakubzick et al., 2013).
A limitation of current fate-mapping strategies is that during embryonic development,
incomplete labeling of monocyte and macrophage populations is invariably obtained. In
part, this represents a technical limitation related to both the duration and levels of CRE
expression—rapidly dividing progenitors might be too short-lived to permit recombination.
However, an intriguing alternative interpretation is that in addition to incomplete labeling,
embryonic macrophage lineages other than those derived from fetal monocytes and yolk sac
progenitors might exist. In support of this possibility, Rag1Cre lineage tracing has identified
a novel lymphomyeloid progenitor population that precedes the development of definitive
HSCs (Böiers et al., 2013). As the name implies, lymphomyeloid cells give rise to only
Author Manuscript
lymphocytes and monocytes, but not megakaroycoytes or erythrocytes. Lymphomyeloid
progenitors develop at E8.5–E9.5 through a RAG1+ progenitor and migrate to the fetal liver.
Detailed analysis of fetal-liver-derived macrophages suggests that this subset is outcompeted
over time by RAG1-independent macrophages (derived from fetal monocytes and/or the
yolk sac). At E14.5 microglia, skin and liver macrophages were not labeled, suggesting that
RAG-1-derived macrophages were significantly lost by this time point (Böiers et al., 2013;
Schulz et al., 2012). It would be interesting to determine whether RAG1-dependent
macrophages persist into adulthood as long-lived tissue macrophages.
Monocyte-Specific Origins and Functions
In the adult, monocytes originate from definitive HSCs through a characterized
differentiation program involving progressively further committed progenitors. The
Author Manuscript
identification of the monocyte-macrophage dendritic cell (DC) progenitor (MDP) provided a
developmental link between both DCs and monocytes within a common differentiation
pathway (Fogg et al., 2006). Recently, a Ly6c+ monocyte-specific progenitor downstream of
MDPs has been identified in the bone marrow and spleen. Although this progenitor displays
proliferative capacity, unlike mature monocytes, it lacks phagocytic activity (Hettinger et al.,
2013). Our current understanding of monocytes suggests that there are two principle subsets:
(1) classical Ly6chi monocytes, which appear to be directly descendent from Ly6c+
monocyte progenitors, and (2) Ly6clo nonclassical monocytes, which differentiate from
Ly6chi monocytes through an Nr4a1-dependent transcriptional program (Hanna et al., 2011;
Hettinger et al., 2013; Yona et al., 2013) (Figure 2). These monocyte subsets are highly
conserved and transcriptionally closely match human monocyte subsets (Ingersoll et al.,
2010). In both humans and mice, a third monocyte subset has also been suggested; it
Author Manuscript
resembles an intermediate population between classical and nonclassical monocytes on the
basis of cell-surface markers and transcriptional analysis. However, the function of this
subset has not been well investigated (Schmidl et al., 2014).
The biology of the nonclassical subset of monocytes is unusual in that these cells appear
primarily to function within the vasculature itself. They “patrol” the vasculature by slowly
crawling over the endothelium, even moving against the flow of blood, in a manner
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 6
dependent upon LFA-1 integrin (Auffray et al., 2007). The purpose of this behavior has
Author Manuscript
recently been elucidated. Patrolling, nonclassical monocytes have a key role in clearing
damaged endothelial cells, thereby maintaining integrity of the vasculature (Carlin et al.,
2013). Although some investigators have considered these monocytes to be vascular
“macrophages,” they closely cluster with other monocytes and do not express the core,
mature macrophage signature of mRNA transcripts, including Mer tyrosine kinase (Gautier
et al., 2012b; Jakubzick et al., 2013).
Although they are often referred to as “inflammatory monocytes,” recent work indicates that
Ly6chi monocytes can enter resting tissues. In this capacity, they patrol extravascular tissues
to pick up antigens for transport to draining lymph nodes, all the while remaining relatively
undifferentiated rather than committing to macrophages or DCs (Jakubzick et al., 2013).
However, in the context of inflammation, recruited monocytes differentiate to macrophages
(Jakubzick et al., 2013). Thus, monocytes of both subsets carry out a patrolling function in
Author Manuscript
resting mice—the classical monocyte subset patrols extravascular tissues, and the
nonclassical subset patrols the intravascular space (Figure 2). This patrolling feature
distinguishes monocytes from macrophages, which have a limited ability to emigrate in
comparison to monocytes. Once in tissue, Ly6Chi monocytes can take on many
characteristics of Ly6Clo monocytes (Arnold et al., 2007; Hilgendorf et al., 2014) and enter
the lymphatics after such conversion (Qu et al., 2004) (Figure 2).
In summary, a combination of approaches have greatly informed our understanding of the
diversity and complex ontological origins of resident tissue macrophages (see Figure 1).
Each organ has its own particular composition of embryonically derived and adult-derived
macrophage subsets, and each organ dictates the degree to which circulating monocytes
replace resident macrophages after birth. As we continually refine our understanding of
Author Manuscript
macrophage lineage, an important new goal is to determine the functions of these cells, both
through direct targeting of individual macrophage subsets and through reflecting on prior
studies and putting into context observations that were made prior to the revelation that
embryonically derived macrophages exist.
The Developing Embryo and Macrophage Function
Perhaps the simplest way to learn what functions embryonically derived macrophages might
possess in the adult is to first examine what these cells do during embryonic development. In
this way, we can determine whether macrophage functions executed in the embryo are “hard
wired” and specifically retained by these subsets in the adult. Mice deficient in PU.1,
CSF1R, or M-CSF (CSF1) lack many tissue macrophages from the earliest stages of
development beginning at the time of yolk sac hematopoiesis. These animals display
Author Manuscript
increased perinatal mortality, reduced postnatal survival, and stunted growth (Dai et al.,
2002; McKercher et al., 1996; Wiktor-Jedrzejczak et al., 1990). Careful examination of
macrophage-deficient embryos has revealed defects in embryonic vascular development.
Spi1−/− and Csf1op/op animals demonstrate reduced CNS vascular complexity and branching
as early as E11.5 (Nucera et al., 2011; Fantin et al., 2010; Arnold and Betsholtz, 2013).
Elegant experiments utilizing zebrafish and genetic mouse models have revealed that
macrophages orchestrate CNS vascular development by acting as endothelial cell
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 7
chaperones promoting endothelial tip cell fusion in a VEGF-A-independent manner (Fantin
Author Manuscript
et al., 2010). Intriguingly, macrophages found in the developing retina are required for blood
vessel regression through a noncanonical WNT- and FLT1-dependent mechanism (Lobov et
al., 2005), indicating that macrophages might interact with the developing vasculature in
distinct ways depending on the tissue context.
In addition to regulating embryonic vascular growth and patterning, macrophages participate
in other important processes during development. In the developing brain, microglia mediate
neuronal patterning through regulation of neuronal survival and programmed cell death
(Wake et al., 2013; Nayak et al., 2014). With respect to neuronal survival, microglia are
essential for cortical layer V formation, where they release multiple growth factors,
including IGF-1 (Ueno et al., 2013). Conversely, microglia pattern the developing
hippocampus and cerebellum by triggering the death of excess neurons through DAP12
signaling and the release of reactive oxygen species (Marín-Teva et al., 2004; Wakselman et
Author Manuscript
al., 2008). Microglia-induced neuronal cell death is accompanied by minimal inflammation
and rapid phagocytosis of apoptotic neurons. Similarly, microglia play essential roles in
synaptic patterning by using DAP12-, CX3CR1-, and complement-dependent mechanisms
(Paolicelli et al., 2011; Roumier et al., 2004; Stevens et al., 2007). Recently, a more general
role for embryonic macrophages in the clearance of senescent cells during embryonic
development was described (Munñoz-Espín et al., 2013; Storer et al., 2013).
A common feature of Csf1op/op, Csf1r−/−, and Spi1−/− mice is defective long-bone
formation, tooth eruption, and osteopetrosis (Dai et al., 2002; Wiktor-Jedrzejczak et al.,
1990; Tondravi et al., 1997). Each of these phenotypes is a consequence of failed osteoclast
development. Osteoclasts are terminally differentiated macrophage-derived cells with
specialized functions in bone remodeling. With respect to long-bone formation,
Author Manuscript
macrophage-deficient embryos display defects in growth-plate dynamics, fail to undergo
timely endochondrial ossification, and contain increased numbers of hypertrophic
chondrocytes (Ortega et al., 2010). Failed tooth eruption and osteopetrosis are a direct result
of deficiencies in osteoclast-mediated bone demineralization and remodeling (Kodama et al.,
1991). It is not entirely known from what macrophage lineage(s) osteoclasts are derived. In
the adult mouse, parabiosis studies have revealed that monocytes can be recruited to the
bone and differentiate to osteoclasts. By using a transgenic mouse expressing a
photoconvertable GFP molecule (Kikume Green-Red), Kotani et al. (2013) identified a
contribution of splenic monocytes to osteoclasts. This study did not employ genetic lineage-
tracing techniques, and although adult monocytes can contribute to the osteoclast pool, it
remains unclear to what degree and whether embryonically derived macrophages do as well.
Moreover, the ontogeny of osteoclasts during embryonic and postnatal development remains
Author Manuscript
unresolved.
Consistent with a role in tissue repair during development, a recent manuscript reported that
neonatal macrophages are required for cardiac repair after neonatal myocardial infarction
(Aurora et al., 2014). After cardiac injury, neonatal macrophages were required for
angiogenesis and were associated with a less vigorous inflammatory response when
compared to macrophages in the injured adult heart. Unfortunately, this study did not
include a detailed characterization of monocyte and macrophage subsets or lineages. Prior
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 8
studies in humans have also described differences in inflammatory potential between fetal
Author Manuscript
and adult mononuclear phagocytes after LPS stimulation (Caron et al., 2010; De Wit et al.,
2003; Levy et al., 2004; Weatherstone and Rich, 1989). Together, these findings suggest that
embryonic and neonatal macrophages play important roles in tissue remodeling during
development, and compared to adult-monocyte-derived macrophages, they have a reduced
capacity to generate inflammatory responses.
Monocyte and Macrophage Dynamics and Function in Tissues
Comprehensive transcriptional analysis of resident macrophages through the ImmGen
Consortium suggests that transcriptionally, resident macrophages isolated from various
organs are as different from each other as they are from circulating blood monocytes during
steady state (Gautier et al., 2012b), suggesting that the tissue niche provides instructive
signals orchestrating macrophage differentiation. However, because many resident
Author Manuscript
macrophage populations consist of a mixture of embryonic- and adult-HSC-derived
macrophages and because fate-mapping studies were not employed, we must view the
ImmGen data with the understanding that lineage-specific functions among tissue
macrophages were not strictly assessed (Epelman et al., 2014; Hoeffel et al., 2012; Schulz et
al., 2012; Hashimoto et al., 2013). In this section, we will highlight the relevant studies that
allow us to discern how different tissue macrophage populations change during times of
stress, whether functions possessed by macrophages during embryonic development are
“hard wired” and therefore retained by their adult progeny, and how macrophages are
conditioned by the tissue in which they reside.
Brain Microglia and the Synapse—A Dynamic Bidirectional Relationship
As mentioned previously, unlike other macrophage pools, brain microglia are derived
Author Manuscript
entirely from yolk sac macrophages; therefore, in the steady state, functions can be directly
attributable to this lineage. After birth, a massive expansion of microglia cell numbers is
driven exclusively through in situ proliferation via M-CSF and interleukin-34 (IL-34)
without monocyte input (Wegiel et al., 1998; Wang et al., 2012; Ginhoux et al., 2010; Ajami
et al., 2007). As in the embryo, microglia retain their ability to alter neuronal circuitry
during the postnatal period, where they are critical for synaptic pruning through engulfment
of neuronal synapses, in addition to phagocytosis of apoptotic neurons (Paolicelli et al.,
2011). Specifically, Cx3cr1−/− mice have a transient reduction in microglia numbers during
the early postnatal period, incomplete synaptic pruning, and decreased functional brain
connectivity, resulting in neurodevelopmental abnormalities related to social interaction and
repetitive behaviors (Zhan et al., 2014).
Author Manuscript
Microglia dynamically interact with neurons at both pre- and postsynaptic sites through the
extension of microglial processes, where prolonged contact leads to elimination (Miyamoto
et al., 2013). During normal visual stimulation, microglia respond to light-dark cycles by
changing the frequency and duration of contacts with multiple synapse-associated elements
(Tremblay et al., 2010). Interestingly, contact (and envelopment) by microglia is correlated
with subsequent changes in synaptic connec- tions, suggesting that sensory experiences
manipulate microglia activity acutely, and microglia are involved in the modulation of
sensory processing by regulating synapses. Their role in the steady-state adult brain can be
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 9
ascertained through novel genetic techniques that now allow for specific deletion of brain
Author Manuscript
microglia in the absence of the confounding effects of surgical trauma with the use of the
Cx3cr1CreER system. Specific microglia deletion results in decreased synaptic formation and
learning (Parkhurst et al., 2013). Loss of microglia-specific brain-derived neurotrophic
factor produces a similar phenotype, suggesting that a key steady-state function of microglia
is promoting synaptic plasticity of neurons in response to learning cues secondary to the
release of soluble mediators. During brain ischemia, microglia significantly increase the
duration of their interactions with synapses, which correlates with the loss of dysfunctional
synaptic structures and suggests that microglia serve an early protective role after brain
injury (Wake et al., 2009).
Microglia and Recruited Monocytes during Brain Injury
Autoimmune experimental encephalitis (EAE) in the mouse is similar to human multiple
Author Manuscript
sclerosis and is believed to depend on the activation of myelin-specific T cells that trigger
resident microglia and monocyte-derived macrophages, inflammatory demyelination, and a
relapsing and remitting motor paralysis. Although this has been well investigated, we
highlight two studies in which the roles of resident microglia and recruited monocytes were
separated. Through the elegant use of mixed parabiotic and bone-marrow-transplant studies,
specific infiltration of monocyte-derived macrophages was both correlated to and required
for progression of neurological disease, indicating a critical role for infiltrating monocytes in
the pathogenesis of EAE (Ajami et al., 2011). Utilizing the Cx3cr1CreER system, a recent
study has demonstrated that specific deletion of the kinase TAK1 in microglia (and not
infiltrating monocytes) prevents both initial and relapsing paralysis, as well as inhibition of
cellular expansion and disease progression (Goldmann et al., 2013). Together, these data
suggest that both lineages are required for EAE progression and that early microglia
Author Manuscript
activation via TAK1 is necessary for disease initiation, whereas the latter monocyte infiltrate
(which is dependent on microglia activation) drives neurological damage through
demyelization and progression of paralysis. As in EAE, if monocytes are prevented from
infiltrating the brain after ischemic injury, the permeability of the blood-brain barrier is
reduced and infarct size is reduced, suggesting a pathological role for monocyte-derived
macrophages during ischemia (Dimitrijevic et al., 2007).
Whether or not monocytes enter the CNS is a difficult question to address because it
depends on the techniques utilized. For example, with parabiosis, acute motor nerve damage
leads to microglia expansion that occurs without chimeric monocyte input. However, if
peripheral chimerism is achieved through irradiation and intravenous injection of large
numbers of bone marrow cells (standard bone-marrow-transplant studies), chimeric blood
monocytes are recruited to the sites of neuronal injury (Ajami et al., 2007). Use of
Author Manuscript
irradiation is a key confounder in microglia dynamics, given that there is disruption of the
bloodbrain barrier and entry of monocytes that would otherwise not enter into the brain in
the setting of adoptive transplant (Mildner et al., 2011). During EAE, the microglia
population expands locally through proliferation, whereas recruited monocytes are
eliminated over time, suggesting that even during intense inflammation, monocyte-derived
macrophages do not have the capacity to become self-sustaining microglia and have little
long-term access to the CNS (Ajami et al., 2011). Although many homeostatic functions of
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 10
yolk-sac-derived microglia are under intense investigation, what has not been specifically
Author Manuscript
addressed is the relative ability of monocyte-derived macrophages to perform highly
specialized functions typically associated with microglia, such as synaptic pruning.
Monocyte-derived macrophages are found in the CNS several months after EAE induction,
and it would be interesting to observe whether these cells, even though their presence is
temporary, are able to take over homeostatic functions in brain areas in which they reside.
Neurodegenerative diseases are chronic disorders often associated with aging and numerical
expansion of microglia. During the aging process, microglia acquire an irregular shape,
occupy smaller territories, and form inclusions containing apparent synaptic elements,
suggesting that dysfunction develops in macrophage degradative pathways with age
(Tremblay et al., 2012; Wake et al., 2013). Similarly, in animal models of Alzheimer’s
disease, microglia numerically expand and progressively accumulate beta amyloid plaques,
which is believed to impair phagocytic function and allow beta amyloid plaques to
Author Manuscript
accumulate in the brain, suggesting that phagocytosis of plaques could be protective. SNPs
in genes encoding CD33 (a phagocytosis inhibitor) or TREM2 (which mediates neuronal
uptake) are associated with Alzheimer’s disease, lending clinical credence to the idea that
impaired phagocytotic clearance of plaque promotes disease progression (Griciuc et al.,
2013; Guerreiro et al., 2013). Multiple studies have suggested that recruitment of CCR2+
(Ly6chi) monocytes improves clearance of plaque depositions, improves cognitive function,
and decreases mortality in animal models of Alzheimer’s disease, suggesting a clear
protective role for infiltrating monocytes (Naert and Rivest, 2011; El Khoury et al., 2007).
However, the use of irradiation and bone-marrow-transplantation models to localize CCR2
deficiency to the bone marrow compartment, which, as stated above, might allow circulating
monocytes access to the brain, suggests that formal proof that monocytes enter the CNS in
Alzheimer’s models is currently lacking. In fact, there is strong evidence that circulating
Author Manuscript
monocytes do not enter the brains of other neurodegenerative disorders (such as
Huntington’s disease), but as of yet, the role of microglia in Huntington’s disease is not clear
(Ajami et al., 2007). Understanding the role of monocytes and microglia in neurocognitive
dysfunction is challenging because subtle dysfunctions might not be readily detectable. For
example, Cx3cr1−/− mice have been widely utilized over the last decade in multiple fields,
and as mentioned above, we have only recently identified neurocognitive deficits related to
microglia in this strain (Zhan et al., 2014). Together, these data demonstrate that resident
microglia have important homeostatic functions in regulating synaptic development, and the
diseased state (e.g., Alzheimer’s disease) might be insufficient to prevent chronic
neurodegeneration. Taking advantage of macrophage plasticity in the setting of
dysfunctional brain microglia by promoting monocyte entry could lead to novel therapeutic
approaches for neurocognitive disorders.
Author Manuscript
Cardiac Macrophages—Ontologically and Functionally Distinct Subsets
Unlike the brain, which exclusively contains yolk-sac-derived microglia, the heart contains
several discrete macrophage populations with mixed ontological origins (Epelman et al.,
2014). CCR2− macrophages are largely derived from embryonic progenitors, including
contributions from yolk sac macrophages, and are primarily autonomous from blood
monocytes. In contrast, resident cardiac CCR2+ macrophages are derived entirely from
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 11
definitive HSCs and are replaced slowly by blood monocytes. In the setting of acute
Author Manuscript
hypertensive stress, both resident embryonically derived macrophage populations and
recruited populations expand by proliferation in a manner analogous to that of peritoneal
macrophages during sterile inflammation (Davies et al., 2013b). Functionally, when all
cardiac macrophages are depleted after ischemic injury, a net beneficial role in scar
formation is revealed, given that macrophage-depleted mice demonstrate poor infarct
healing and myocardial rupture (van Amerongen et al., 2007; Nahrendorf et al., 2007).
Subset-specific transcriptional profiling indicates that CCR2+ macrophages differentially
express multiple components of the NLRP3 inflammasome and are required for IL-1β
production, suggesting that adult-derived macrophage lineages within the myocardium
might be primed to generate inflammatory responses (Epelman et al., 2014). These data
could help explain why targeting CCR2+ macrophages is beneficial after ischemic injury
(Frangogiannis et al., 2007). Whether reparative and proangiogenic responses are mediated
Author Manuscript
by adult and/or embryonically established macrophage populations remains unknown.
Depletion, Plasticity, and Function of Tissue Macrophages
After depletion of cardiac macrophages, circulating Ly6chi monocytes take up permanent
residence within cardiac tissue and give rise to the dominant population of resident tissue
macrophages. After repopulation is complete, autonomy of tissue macrophages is restored,
albeit with a large complement of adult-monocyte-derived macrophages as the new resident
macrophage population (Epelman et al., 2014). If Ly6chi monocytes are absent from
circulation (such as in Ccr2−/− mice), resident macrophages are fully capable of repopulating
the tissue niche (see Figure 3). Careful examination of the repopulation of tissue
macrophages after depletion has revealed that multiple mechanisms are at play. As a result,
a universally applied repopulation strategy does not exist, because both organ- and
Author Manuscript
depletion-specific factors apply. For example, similar to depletion of cardiac macrophages,
clodronate-liposome-mediated depletion results in profound and permanent loss of
embryonically established resident tissue macrophages, including liver Kupffer cells and
splenic red-pulp macrophages. Both Kupffer cells and splenic red-pulp macrophages are
subsequently replacement by adult-derived (FLT3-dependent) monocytes, indicating that
circulating monocytes have a competitive advantage over the remaining resident tissue
macrophages (Epelman et al., 2014). These data indicate that forced “ontological
reprogramming” of tissue macrophages can be easily achieved with clodronate-liposome-
mediated depletion strategies in these organs. The functional significance of ontological
reprogramming is unknown, and defining whether distinct macrophage lineages harbor
unique or overlapping functions will require tissue-specific investigations.
Alveolar macrophages reside on the epithelial surface of the lung, and in contrast to other
Author Manuscript
resident macrophage populations, they are in direct contact with the environment, which
includes commensal bacteria, inhaled particulates, and host-epithelial-derived factors, such
as surfactants. Embryonically derived fetal monocytes appear to colonize the lung shortly
after birth and differentiate into alveolar macrophages in a GM-CSF-dependent process
(Guilliams et al., 2013). GM-CSF signaling drives expression of PPAR-γ, a characteristic
feature of alveolar macrophages (Malur et al., 2011), which contributes to the unique gene-
expression profile of lung macrophages (Gautier et al., 2012a). Alveolar macrophages
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 12
normally live independently of blood monocyte input; however, an interesting competition
Author Manuscript
takes place if alveolar macrophages are depleted. CD163-DTR-mediated depletion results in
repopulation by in situ proliferation independently of blood monocyte input (Hashimoto et
al., 2013) (see Figure 3). However, if alveolar macrophages are depleted by genotoxic injury
via lethal irradiation, recruited monocytes now gain the competitive advantage and
repopulate the alveolar macrophage niche. Intriguingly, despite genotoxic injury, irradiated
resident alveolar macrophages can re-expand if recruited monocytes cannot receive GM-
CSF signals. Use of sublethal irradiation seems to level the playing field such that both
resident macrophages and blood monocytes contribute to repopulation. Functionally, similar
observations have also been seen in the heart (Epelman et al., 2014). These data indicate that
most resident tissue macrophages maintain themselves indefinitely without monocyte input,
but if an acute and profound depletion occurs, circulating monocytes can readily repopulate
the macrophage niche.
Author Manuscript
Pulmonary surfactant is produced by alveolar epithelial cells, and together with other
pathways, it acts to suppress alveolar macrophage activation during resting conditions
(Hussell and Bell, 2014). An essential role of alveolar macrophages is the ability to
phagocytose excessive surfactant proteins and prevent alveolar proteinosis (Dranoff et al.,
1994; Guilliams et al., 2013). After alveolar macrophage depletion, local production of GM-
CSF is essential for both alveolar macrophages and recruited monocytes to reverse alveolar
proteinosis (Hashimoto et al., 2013), again highlighting the ability of the tissue niche to
govern macrophage differentiation independently of developmental lineage.
Splenic red-pulp macrophages are required to take up senescent red blood cells and
specifically utilize the transcription factor SPI-C to drive the genes necessary for iron uptake
(Kohyama et al., 2009). Unlike other embryonically derived macrophages, splenic red-pulp
Author Manuscript
macrophages receive instructive signals from the spleen to express SPI-C, highlighting clear
tissue-specific steady-state functions. In the setting of hemolysis, excessive heme induces
the loss of resident red-pulp macrophages. Circulating monocytes enter the spleen and
upregulate SpiC, leading to macrophage differentiation, reestablishment of the splenic red-
pulp macrophage compartment, and restoration of iron homeostasis. These data provide
further evidence that local signaling within tissues might be sufficient to promote the
acquisition of specialized macrophage functions irrespective of the ontological lineage
(Haldar et al., 2014).
Splenic marginal-zone macrophage development is dependent on the nuclear receptor LXR
and functions to limit bloodborne infections (A-Gonzalez et al., 2013). Although the precise
origin of marginal-zone macrophages is not known, these cells proliferate in the first weeks
Author Manuscript
of life. LXR-deficient mice have normal monocyte numbers, and adoptive transfer of wild-
type monocytes into LXR-deficient mice leads to functional reestablishment of the splenic
marginal-zone macrophage niche, indicating that monocytes are instructed within the spleen
in a LXR-dependent manner to acquire marginal-zone macrophage fate. Together, these data
highlight the ability of the spleen to drive monocyte-to-macrophage differentiation and
compartmentalize monocyte fate to specific splenic macrophage subsets (red pulp verses
marginal zone).
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 13
However, it remains unclear whether the tissue microenvironment is sufficient to induce
Author Manuscript
tissue-specific macrophage mRNA transcripts in organs beyond the spleen. GATA6 is a
transcription factor that selectively regulates peritoneal macrophage transcripts (Gautier et
al., 2014; Gautier et al., 2012b; Okabe and Medzhitov, 2014; Rosas et al., 2014). In the
absence of GATA6, the major resident macrophage population in the peritoneum is greatly
contracted, but a second, smaller population that normally lacks GATA6 expression remains
at normal frequency (Gautier et al., 2014; Okabe and Medzhitov, 2014; Rosas et al., 2014).
Enhanced apoptosis in the resting state (Gautier et al., 2014) and a failure to proliferate in
states of inflammation (Rosas et al., 2014) explain the loss of macrophages. GATA6 can be
induced by vitamin A signaling, but addition of vitamin A to cultured macrophages will
induce GATA6 only when sources of fetal macrophages, such as fetal-liver macrophages,
are used (Okabe and Medzhitov, 2014). A working model is that mature macrophages have
undergone epigenetic changes that prevent such induction, such that GATA6 has not yet
Author Manuscript
been demonstrated to be induced in monocytes or other macrophages from adult mice. In
line with this model, GATA6 is not induced in monocyte-derived macrophages recruited to
the peritoneum during thioglycollate-elicited inflammation. These elicited macrophages
upregulate canonical, universal macrophage differentiation transcripts, but they induce only
some peritoneal-cavity-selective transcripts (Gautier et al., 2012b). It will be important to
determine in the future whether the ablation of resident peritoneal macrophages provides a
niche in which recruited monocytes can replace them with induction of the full panoply of
local resident macrophage transcripts, including GATA6 and its targets.
Macrophages and Tissue Regeneration
One of the most interesting aspects of macrophage function is their involvement in tissue
repair and regeneration. Model organisms, including salamanders, zebrafish, and neonatal
Author Manuscript
mice, all require macrophages for tissue regeneration; however, no studies have addressed
the contribution of distinct macrophage subtypes and/or lineages in this process (Godwin et
al., 2013; Aurora et al., 2014; Huang et al., 2013). The liver is the best characterized adult
organ capable of regeneration in mammals after injury or resection. Macrophage expansion
occurs in the setting of injury, and a significant component occurs through monocyte
recruitment, although specifics regarding the contribution of resident versus recruited cells
are lacking. After injury, liver macrophages engulf hepatocyte debris and activate a program
leading to the secretion of WNT ligands, which direct hepatocyte differentiation from
progenitors (You et al., 2013; Boulter et al., 2012). Although macrophage depletion impairs
hepatocyte differentiation, bile duct regeneration is not affected, highlighting the potential
specificity of macrophage-mediated regeneration. In the absence of circulating monocytes
(such as in CCR2- or MCP-1-deficient mice), fibrosis after acute liver injury or diet-induced
Author Manuscript
nonalcoholic liver disease is reduced, suggesting that monocyte-derived macrophages rather
than Kupffer cells promote liver fibrosis (Kassel et al., 2010; Karlmark et al., 2009). The
ability to induce fibrosis at the site of injury appears to be a common function of recently
recruited monocytes, not only in the liver but also in the heart and kidney, suggesting a
conserved transcriptional program (Kaikita et al., 2004; Kitagawa et al., 2004). Studies that
focus on the role of monocyte-derived macrophages invariably target the CCR2 pathway,
which also limits monocyte egress from the bone marrow during steady state. CCR2
deficiency serves as our best model of peripheral monocyte ablation, but several important
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 14
caveats must be taken into account. CCR2 is also required for HSCs to traffic to sites of
Author Manuscript
injury (such as the liver), and CCR2 signaling in nonimmune cells might also promote injury
(Si et al., 2010; Zhou et al., 2006).
Given recent advances in our understanding of macrophage ontogeny, novel genetic tools
for and approaches to separating out functions of infiltrating monocytes from resident
embryonically derived and adult-derived macrophages are being developed. Future studies
will focus on deciphering the function of individual pathways (such as TAK1 in microglia)
within distinct macrophage lineages. Common macrophage functions, such as phagocytosis,
could be easily complemented by nonresident monocyte-derived macrophages. Whether
specialized macrophage functions are specific to resident macrophage lineages or can be
fully acquired by recruited, monocyte-derived macrophages remains an important question
and will require careful examination.
Author Manuscript
Monocyte and Macrophage Proliferation in Tissues
Macrophage expansion in tissues during disease is common and critically modulates injury
versus healing. However, the contribution of monocyte recruitment and local proliferation is
only now coming to light. Until the demonstration that proliferation of macrophages could
solely account for macrophage expansion at sites of nematode infection, macrophage
proliferation was not recognized as a powerful modifier of macrophage numbers within
organs. IL-4 signals serve in this context as a major driver of proliferation, raising the initial
idea that macrophage proliferation is a particularly specialized feature of T helper 2 (Th2)-
cell-oriented immunity (Jenkins et al., 2011; Jenkins et al., 2013). Cardiac injury and sterile
peritonitis induce monocyte recruitment and subsequent proliferation in tissues of resident
macrophages, recruited monocytes, and monocyte-derived macrophages (Davies et al.,
2013b; Epelman et al., 2014). Recent studies of adipose tissue and atherosclerosis suggest
Author Manuscript
that macrophage proliferation contributes to inflammation in contexts beyond Th2 cell
immunity. Understanding whether monocyte recruitment or proliferation of resident and
recruited macrophages drives expansion is critical if therapies targeting macrophages are to
move forward. For example, if local macrophage expansion is sufficient to mediate
pathology, blockade of monocyte recruitment would be expected to only modestly affect
disease progression.
Recruitment and proliferation appear to be intertwined. Macrophage proliferation in adipose
tissue has been reported to be dependent on MCP-1, as is monocyte emigration from bone
marrow and entry into circulation and peripheral tissue (Serbina and Pamer, 2006; Amano et
al., 2014). As opposed to the idea that MCP-1-CCR2 signaling in adipose tissue
macrophages drives proliferation directly, it seems more likely that proliferation of
Author Manuscript
macrophages is coupled to signals downstream of CCR2-mediated monocyte recruitment.
The concept of coupled proliferation and recruitment also extends to atherosclerosis. There
is significant evidence that early in disease progression, recruited monocytes enter into
plaque, take up cholesterol, and become dysfunctional foam cells. Blockade of monocyte
recruitment prevents disease progression (Randolph, 2014). However, recent data also
generate a compelling case for proliferation as a major determinant for macrophage burden
within plaques (Robbins et al., 2013).
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 15
What is clear is that recruited monocytes, monocyte-derived macrophages, and resident
Author Manuscript
macrophages utilize proliferation as a strategy to control cell numbers within tissue. Given
that monocyte numbers can be augmented simply through additional recruitment, the reader
might ask, why do monocytes and monocyte-derived macrophages proliferate in tissues?
One possibility is that local expansion and contraction could be a more efficient and tightly
regulated process. If local expansion (of resident macrophages) is insufficient, increased
production and release of monocytes from bone marrow and splenic stores could be utilized
(Swirski et al., 2009). However, as a generalized mechanism, increased peripheral monocyte
production and release in the hopes that those short-lived cells rapidly and specifically enter
an inflamed tissue appears less efficient. The very recent identification of proliferating
Ly6c+ monocyte progenitors in the spleen and bone marrow might reveal another nuanced
mechanism in which injured tissue recruits monocyte progenitors that locally proliferate and
thus give the tissue an opportunity to control monocyte numbers in situ rather than through
Author Manuscript
recruitment. Monocyte recruitment and local proliferation are unlikely to be independent
mechanisms. In fact, the currently available evidence supports a model in which recruitment
of monocytes is linked to proliferation of previously recruited monocyte-derived
macrophages (Randolph, 2013).
Human Correlates to Ontologically Distinct Tissue Macrophage Subsets
Few studies have examined whether human tissue macrophages are similarly composed of
resident embryonically derived and monocyte-derived macrophage subsets. Instead,
designation of macrophage populations in humans has largely been focused on defining cell
types on the basis of the M1 (interferon-γ-mediated) versus M2 (IL-4-mediated) macrophage
phenotype. The M1 versus M2 designation is a widely utilized paradigm in mice and
appears to be conserved to some degree in humans (Martinez et al., 2013). However, a
Author Manuscript
recent study has demonstrated that treatment of human blood monocytes with a variety of
stimuli results in acquisition of a spectrum of macrophage phenotypes that span between
classic M1 and M2 definitions, casting doubt on the concept that M1 versus M2 behavior
can be used for defining macrophage subsets (Xue et al., 2014; Murray et al., 2014, in this
issue of Immunity).
Studies focusing on human skin after HSC transplantation have revealed indirect evidence
that tissue macrophages are long lived and might exist independently of circulating
progenitors. Careful examination of skin HLA-DR+ myeloid cells from patients receiving
sex-mismatched bone marrow transplants demonstrated that DC populations reached nearly
100% chimerism within 40 days posttransplant, indicating a clear dependency on circulating
cells (Haniffa et al., 2009). However, ~25% of skin macrophages were not replaced, even
Author Manuscript
after 1 year posttransplant, suggesting that some human skin resident macrophages might
persist independently of circulating monocyte input, which is similar to what has been
observed in mice (Jakubzick et al., 2013; Tamoutounour et al., 2013).
Because genetic lineage tracing is not feasible in humans, the optimal strategy for
identifying and defining distinct macrophage lineages in human tissue is not immediately
obvious. Identification of conserved gene-expression signatures represents one potential
solution to this problem. Systematic analysis of the ImmGen data set from C57Bl/6 mice has
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 16
yielded the discovery of a core macrophage gene-expression signature, allowing the
Author Manuscript
distinction of monocytes, macrophages, and DCs (Gautier et al., 2012b). Major surface
proteins found in the core signature include Mer tyrosine kinase and FcgRI, molecules that
themselves highlight the specialized function that macrophages have in engulfing apoptotic
cells and responding to immunoglobulins made during adaptive immunity to coordinate
tissue responses, respectively. Importantly, Mer tyrosine kinase and FcgRI were recently
shown to also be conserved in human monocyte-derived macrophages (Xue et al., 2014).
With this methodology, it is conceivable that by defining the core signatures of
embryonically derived and monocyte-derived macrophage subsets in mice, it might be
possible to identify corresponding macrophage populations in humans.
Summary
There are clear examples in which tissue-specific factors drive highly specialized
Author Manuscript
macrophage functions irrespective of their ontological origin, suggesting tremendous
plasticity and redundancy in the mononuclear phagocyte system. Whether embryonic and
adult macrophages possess specialized roles has yet to be formally tested. However, our
conceptual understanding and genetic tools are now sufficiently developed to precisely
follow both embryonic and adult macrophage subsets in health and disease, which should
allow important and unanswered questions in the field to be addressed (see Table 2). In
order to develop novel therapies, a critical future goal is to harness this newfound
understanding that different macrophage lineages exist within tissues and clarify whether
these distinct lineages differentially contribute to tissue damage and repair.
REFERENCES
A-Gonzalez N, Guillen JA, Gallardo G, Diaz M, de la Rosa JV, Hernandez IH, Casanova-Acebes M,
Author Manuscript
Lopez F, Tabraue C, Beceiro S, et al. The nuclear receptor LXRα controls the functional
specialization of splenic macrophages. Nat. Immunol. 2013; 14:831–839. [PubMed: 23770640]
Ajami B, Bennett JL, Krieger C, Tetzlaff W, Rossi FM. Local self-renewal can sustain CNS microglia
maintenance and function throughout adult life. Nat. Neurosci. 2007; 10:1538–1543. [PubMed:
18026097]
Ajami B, Bennett JL, Krieger C, McNagny KM, Rossi FM. Infiltrating monocytes trigger EAE
progression, but do not contribute to the resident microglia pool. Nat. Neurosci. 2011; 14:1142–
1149. [PubMed: 21804537]
Amano SU, Cohen JL, Vangala P, Tencerova M, Nicoloro SM, Yawe JC, Shen Y, Czech MP, Aouadi
M. Local proliferation of macrophages contributes to obesity-associated adipose tissue
inflammation. Cell Metab. 2014; 19:162–171. [PubMed: 24374218]
Arnold T, Betsholtz C. The importance of microglia in the development of the vasculature in the
central nervous system. Vascular Cell. 2013; 5:4. [PubMed: 23422217]
Arnold L, Henry A, Poron F, Baba-Amer Y, van Rooijen N, Plonquet A, Gherardi RK, Chazaud B.
Author Manuscript
Inflammatory monocytes recruited after skeletal muscle injury switch into antiinflammatory
macrophages to support myogenesis. J. Exp. Med. 2007; 204:1057–1069. [PubMed: 17485518]
Auffray C, Fogg D, Garfa M, Elain G, Join-Lambert O, Kayal S, Sarnacki S, Cumano A, Lauvau G,
Geissmann F. Monitoring of blood vessels and tissues by a population of monocytes with patrolling
behavior. Science. 2007; 317:666–670. [PubMed: 17673663]
Aurora AB, Porrello ER, Tan W, Mahmoud AI, Hill JA, Bassel-Duby R, Sadek HA, Olson EN.
Macrophages are required for neonatal heart regeneration. J. Clin. Invest. 2014; 124:1382–1392.
[PubMed: 24569380]
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 17
Böiers C, Carrelha J, Lutteropp M, Luc S, Green JC, Azzoni E, Woll PS, Mead AJ, Hultquist A,
Swiers G, et al. Lymphomyeloid contribution of an immune-restricted progenitor emerging prior to
Author Manuscript
definitive hematopoietic stem cells. Cell Stem Cell. 2013; 13:535–548. [PubMed: 24054998]
Boulter L, Govaere O, Bird TG, Radulescu S, Ramachandran P, Pellicoro A, Ridgway RA, Seo SS,
Spee B, Van Rooijen N, et al. Macrophage-derived Wnt opposes Notch signaling to specify
hepatic progenitor cell fate in chronic liver disease. Nat. Med. 2012; 18:572–579. [PubMed:
22388089]
Boyer SW, Schroeder AV, Smith-Berdan S, Forsberg EC. All hematopoietic cells develop from
hematopoietic stem cells through Flk2/Flt3-positive progenitor cells. Cell Stem Cell. 2011; 9:64–
73. [PubMed: 21726834]
Carlin LM, Stamatiades EG, Auffray C, Hanna RN, Glover L, Vizcay-Barrena G, Hedrick CC, Cook
HT, Diebold S, Geissmann F. Nr4a1-dependent Ly6C(low) monocytes monitor endothelial cells
and orchestrate their disposal. Cell. 2013; 153:362–375. [PubMed: 23582326]
Caron JE, La Pine TR, Augustine NH, Martins TB, Hill HR. Multiplex analysis of toll-like receptor-
stimulated neonatal cytokine response. Neonatology. 2010; 97:266–273. [PubMed: 19955831]
Cooper MD, Alder MN. The evolution of adaptive immune systems. Cell. 2006; 124:815–822.
Author Manuscript
[PubMed: 16497590]
Dai XM, Ryan GR, Hapel AJ, Dominguez MG, Russell RG, Kapp S, Sylvestre V, Stanley ER.
Targeted disruption of the mouse colony-stimulating factor 1 receptor gene results in
osteopetrosis, mononuclear phagocyte deficiency, increased primitive progenitor cell frequencies,
and reproductive defects. Blood. 2002; 99:111–120. [PubMed: 11756160]
Davies LC, Jenkins SJ, Allen JE, Taylor PR. Tissue-resident macrophages. Nat. Immunol. 2013a;
14:986–995. [PubMed: 24048120]
Davies LC, Rosas M, Jenkins SJ, Liao CT, Scurr MJ, Brombacher F, Fraser DJ, Allen JE, Jones SA,
Taylor PR. Distinct bone marrow-derived and tissue-resident macrophage lineages proliferate at
key stages during inflammation. Nat Commun. 2013b; 4:1886. [PubMed: 23695680]
De Wit D, Tonon S, Olislagers V, Goriely S, Boutriaux M, Goldman M, Willems F. Impaired
responses to toll-like receptor 4 and toll-like receptor 3 ligands in human cord blood. J.
Autoimmun. 2003; 21:277–281. [PubMed: 14599853]
Dimitrijevic OB, Stamatovic SM, Keep RF, Andjelkovic AV. Absence of the chemokine receptor
CCR2 protects against cerebral ischemia/reperfusion injury in mice. Stroke. 2007; 38:1345–1353.
Author Manuscript
[PubMed: 17332467]
Dranoff G, Crawford AD, Sadelain M, Ream B, Rashid A, Bronson RT, Dickersin GR, Bachurski CJ,
Mark EL, Whitsett JA, et al. Involvement of granulocyte-macrophage colony-stimulating factor in
pulmonary homeostasis. Science. 1994; 264:713–716. [PubMed: 8171324]
El Khoury J, Toft M, Hickman SE, Means TK, Terada K, Geula C, Luster AD. Ccr2 deficiency
impairs microglial accumulation and accelerates progression of Alzheimer-like disease. Nat. Med.
2007; 13:432–438. [PubMed: 17351623]
Epelman S, Lavine KJ, Beaudin AE, Sojka DK, Carrero JA, Calderon B, Brija T, Gautier EL, Ivanov
S, Satpathy AT, et al. Embryonic and adult-derived resident cardiac macrophages are maintained
through distinct mechanisms at steady state and during inflammation. Immunity. 2014; 40:91–104.
[PubMed: 24439267]
Fantin A, Vieira JM, Gestri G, Denti L, Schwarz Q, Prykhozhij S, Peri F, Wilson SW, Ruhrberg C.
Tissue macrophages act as cellular chaperones for vascular anastomosis downstream of VEGF-
mediated endothelial tip cell induction. Blood. 2010; 116:829–840. [PubMed: 20404134]
Author Manuscript
Fogg DK, Sibon C, Miled C, Jung S, Aucouturier P, Littman DR, Cumano A, Geissmann F. A
clonogenic bone marrow progenitor specific for macrophages and dendritic cells. Science. 2006;
311:83–87. [PubMed: 16322423]
Frangogiannis NG, Dewald O, Xia Y, Ren G, Haudek S, Leucker T, Kraemer D, Taffet G, Rollins BJ,
Entman ML. Critical role of monocyte chemoattractant protein-1/CC chemokine ligand 2 in the
pathogenesis of ischemic cardiomyopathy. Circulation. 2007; 115:584–592. [PubMed: 17283277]
Gautier EL, Chow A, Spanbroek R, Marcelin G, Greter M, Jakubzick C, Bogunovic M, Leboeuf M,
van Rooijen N, Habenicht AJ, et al. Systemic analysis of PPARγ in mouse macrophage
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 18
populations reveals marked diversity in expression with critical roles in resolution of inflammation
and airway immunity. J. Immunol. 2012a; 189:2614–2624. [PubMed: 22855714]
Author Manuscript
Gautier EL, Shay T, Miller J, Greter M, Jakubzick C, Ivanov S, Helft J, Chow A, Elpek KG, Gordonov
S, et al. Immunological Genome Consortium. Gene-expression profiles and transcriptional
regulatory pathways that underlie the identity and diversity of mouse tissue macrophages. Nat.
Immunol. 2012b; 13:1118–1128. [PubMed: 23023392]
Gautier EL, Ivanov S, Williams JW, Huang SC, Marcelin G, Fairfax K, Wang PL, Francis JS, Leone
P, Wilson DB, et al. Gata6 regulates aspartoacylase expression in resident peritoneal macrophages
and controls their survival. J. Exp. Med. 2014 in press.
Ginhoux F, Greter M, Leboeuf M, Nandi S, See P, Gokhan S, Mehler MF, Conway SJ, Ng LG,
Stanley ER, et al. Fate mapping analysis reveals that adult microglia derive from primitive
macrophages. Science. 2010; 330:841–845. [PubMed: 20966214]
Godwin JW, Pinto AR, Rosenthal NA. Macrophages are required for adult salamander limb
regeneration. Proc. Natl. Acad. Sci. USA. 2013; 110:9415–9420. [PubMed: 23690624]
Goldmann T, Wieghofer P, Müller PF, Wolf Y, Varol D, Yona S, Brendecke SM, Kierdorf K,
Staszewski O, Datta M, et al. A new type of microglia gene targeting shows TAK1 to be pivotal in
Author Manuscript
CNS autoimmune inflammation. Nat. Neurosci. 2013; 16:1618–1626. [PubMed: 24077561]
Griciuc A, Serrano-Pozo A, Parrado AR, Lesinski AN, Asselin CN, Mullin K, Hooli B, Choi SH,
Hyman BT, Tanzi RE. Alzheimer’s disease risk gene CD33 inhibits microglial uptake of amyloid
beta. Neuron. 2013; 78:631–643. [PubMed: 23623698]
Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, Cruchaga C, Sassi C, Kauwe
JS, Younkin S, et al. Alzheimer Genetic Analysis Group. TREM2 variants in Alzheimer’s disease.
N. Engl. J. Med. 2013; 368:117–127. [PubMed: 23150934]
Guilliams M, De Kleer I, Henri S, Post S, Vanhoutte L, De Prijck S, Deswarte K, Malissen B,
Hammad H, Lambrecht BN. Alveolar macrophages develop from fetal monocytes that
differentiate into long-lived cells in the first week of life via GM-CSF. J. Exp. Med. 2013;
210:1977–1992. [PubMed: 24043763]
Haldar M, Kohyama M, So AY, Kc W, Wu X, Briseño CG, Satpathy AT, Kretzer NM, Arase H,
Rajasekaran NS, et al. Heme-mediated SPI-C induction promotes monocyte differentiation into
iron-recycling macrophages. Cell. 2014; 156:1223–1234. [PubMed: 24630724]
Haniffa M, Ginhoux F, Wang XN, Bigley V, Abel M, Dimmick I, Bullock S, Grisotto M, Booth T,
Author Manuscript
Taub P, et al. Differential rates of replacement of human dermal dendritic cells and macrophages
during hematopoietic stem cell transplantation. J. Exp. Med. 2009; 206:371–385. [PubMed:
19171766]
Hanna RN, Carlin LM, Hubbeling HG, Nackiewicz D, Green AM, Punt JA, Geissmann F, Hedrick
CC. The transcription factor NR4A1 (Nur77) controls bone marrow differentiation and the
survival of Ly6C- mono- cytes. Nat. Immunol. 2011; 12:778–785. [PubMed: 21725321]
Hashimoto D, Chow A, Noizat C, Teo P, Beasley MB, Leboeuf M, Becker CD, See P, Price J, Lucas
D, et al. Tissue-resident macrophages self-maintain locally throughout adult life with minimal
contribution from circulating monocytes. Immunity. 2013; 38:792–804. [PubMed: 23601688]
Hettinger J, Richards DM, Hansson J, Barra MM, Joschko AC, Krijgsveld J, Feuerer M. Origin of
monocytes and macrophages in a committed progenitor. Nat. Immunol. 2013; 14:821–830.
[PubMed: 23812096]
Hilgendorf I, Gerhardt LM, Tan TC, Winter C, Holderried TA, Chousterman BG, Iwamoto Y, Liao R,
Zirlik A, Scherer-Crosbie M, et al. Ly-6Chigh monocytes depend on Nr4a1 to balance both
Author Manuscript
inflammatory and reparative phases in the infarcted myocardium. Circ. Res. 2014; 114:1611–
1622. [PubMed: 24625784]
Hoeffel G, Wang Y, Greter M, See P, Teo P, Malleret B, Leboeuf M, Low D, Oller G, Almeida F, et
al. Adult Langerhans cells derive predominantly from embryonic fetal liver monocytes with a
minor contribution of yolk sac-derived macrophages. J. Exp. Med. 2012; 209:1167–1181.
[PubMed: 22565823]
Huang WC, Yang CC, Chen IH, Liu YM, Chang SJ, Chuang YJ. Treatment of Glucocorticoids
Inhibited Early Immune Responses and Impaired Cardiac Repair in Adult Zebrafish. PLoS ONE.
2013; 8:e66613. [PubMed: 23805247]
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 19
Hussell T, Bell TJ. Alveolar macrophages: plasticity in a tissue-specific context. Nat. Rev. Immunol.
2014; 14:81–93. [PubMed: 24445666]
Author Manuscript
Ingersoll MA, Spanbroek R, Lottaz C, Gautier EL, Frankenberger M, Hoffmann R, Lang R, Haniffa
M, Collin M, Tacke F, et al. Comparison of gene expression profiles between human and mouse
monocyte subsets. Blood. 2010; 115:e10–e19. [PubMed: 19965649]
Jakubzick C, Gautier EL, Gibbings SL, Sojka DK, Schlitzer A, Johnson TE, Ivanov S, Duan Q, Bala S,
Condon T, et al. Minimal differentiation of classical monocytes as they survey steady-state tissues
and transport antigen to lymph nodes. Immunity. 2013; 39:599–610. [PubMed: 24012416]
Jenkins SJ, Ruckerl D, Cook PC, Jones LH, Finkelman FD, van Rooijen N, MacDonald AS, Allen JE.
Local macrophage proliferation, rather than recruitment from the blood, is a signature of TH2
inflammation. Science. 2011; 332:1284–1288. [PubMed: 21566158]
Jenkins SJ, Ruckerl D, Thomas GD, Hewitson JP, Duncan S, Brombacher F, Maizels RM, Hume DA,
Allen JE. IL-4 directly signals tissue-resident macrophages to proliferate beyond homeostatic
levels controlled by CSF-1. J. Exp. Med. 2013; 210:2477–2491. [PubMed: 24101381]
Jung S, Aliberti J, Graemmel P, Sunshine MJ, Kreutzberg GW, Sher A, Littman DR. Analysis of
fractalkine receptor CX(3)CR1 function by targeted deletion and green fluorescent protein reporter
Author Manuscript
gene insertion. Mol. Cell. Biol. 2000; 20:4106–4114. [PubMed: 10805752]
Kaikita K, Hayasaki T, Okuma T, Kuziel WA, Ogawa H, Takeya M. Targeted deletion of CC
chemokine receptor 2 attenuates left ventricular remodeling after experimental myocardial
infarction. Am. J. Pathol. 2004; 165:439–447. [PubMed: 15277218]
Karlmark KR, Weiskirchen R, Zimmermann HW, Gassler N, Ginhoux F, Weber C, Merad M, Luedde
T, Trautwein C, Tacke F. Hepatic recruitment of the inflammatory Gr1+ monocyte subset upon
liver injury promotes hepatic fibrosis. Hepatology. 2009; 50:261–274. [PubMed: 19554540]
Kassel KM, Guo GL, Tawfik O, Luyendyk JP. Monocyte chemoattractant protein-1 deficiency does
not affect steatosis or inflammation in livers of mice fed a methionine-choline-deficient diet. Lab.
Invest. 2010; 90:1794–1804. [PubMed: 20697377]
Kitagawa K, Wada T, Furuichi K, Hashimoto H, Ishiwata Y, Asano M, Takeya M, Kuziel WA,
Matsushima K, Mukaida N, Yokoyama H. Blockade of CCR2 ameliorates progressive fibrosis in
kidney. Am. J. Pathol. 2004; 165:237–246. [PubMed: 15215179]
Kodama H, Nose M, Niida S, Yamasaki A. Essential role of macrophage colony-stimulating factor in
the osteoclast differentiation supported by stromal cells. J. Exp. Med. 1991; 173:1291–1294.
Author Manuscript
[PubMed: 2022928]
Kohyama M, Ise W, Edelson BT, Wilker PR, Hildner K, Mejia C, Frazier WA, Murphy TL, Murphy
KM. Role for Spi-C in the development of red pulp macrophages and splenic iron homeostasis.
Nature. 2009; 457:318–321. [PubMed: 19037245]
Kotani M, Kikuta J, Klauschen F, Chino T, Kobayashi Y, Yasuda H, Tamai K, Miyawaki A,
Kanagawa O, Tomura M, Ishii M. Systemic circulation and bone recruitment of osteoclast
precursors tracked by using fluorescent imaging techniques. J. Immunol. 2013; 190:605–612.
[PubMed: 23241888]
Levy O, Zarember KA, Roy RM, Cywes C, Godowski PJ, Wessels MR. Selective impairment of TLR-
mediated innate immunity in human newborns: neonatal blood plasma reduces monocyte TNF-
alpha induction by bacterial lipopeptides, lipopolysaccharide, and imiquimod, but preserves the
response to R-848. J. Immunol. 2004; 173:4627–4634. [PubMed: 15383597]
Lobov IB, Rao S, Carroll TJ, Vallance JE, Ito M, Ondr JK, Kurup S, Glass DA, Patel MS, Shu W, et
al. WNT7b mediates macrophage-induced programmed cell death in patterning of the vasculature.
Author Manuscript
Nature. 2005; 437:417–421. [PubMed: 16163358]
Makhijani K, Brückner K. Of blood cells and the nervous system: hematopoiesis in the Drosophila
larva. Fly (Austin). 2012; 6:254–260. [PubMed: 23022764]
Malur A, Baker AD, McCoy AJ, Wells G, Barna BP, Kavuru MS, Malur AG, Thomassen MJ.
Restoration of PPARg reverses lipid accumulation in alveolar macrophages of GM-CSF knockout
mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 2011; 300:L73–L80. [PubMed: 21036914]
Marín-Teva JL, Dusart I, Colin C, Gervais A, van Rooijen N, Mallat M. Microglia promote the death
of developing Purkinje cells. Neuron. 2004; 41:535–547. [PubMed: 14980203]
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 20
Martinez FO, Helming L, Milde R, Varin A, Melgert BN, Draijer C, Thomas B, Fabbri M, Crawshaw
A, Ho LP, et al. Genetic programs expressed in resting and IL-4 alternatively activated mouse and
Author Manuscript
human macrophages: similarities and differences. Blood. 2013; 121:e57–e69. [PubMed:
23293084]
McKercher SR, Torbett BE, Anderson KL, Henkel GW, Vestal DJ, Baribault H, Klemsz M, Feeney
AJ, Wu GE, Paige CJ, Maki RA. Targeted disruption of the PU.1 gene results in multiple
hematopoietic abnormalities. EMBO J. 1996; 15:5647–5658. [PubMed: 8896458]
Mildner A, Schlevogt B, Kierdorf K, Böttcher C, Erny D, Kummer MP, Quinn M, Brück W,
Bechmann I, Heneka MT, et al. Distinct and non-redundant roles of microglia and myeloid subsets
in mouse models of Alzheimer’s disease. J. Neurosci. 2011; 31:11159–11171. [PubMed:
21813677]
Miyamoto A, Wake H, Moorhouse AJ, Nabekura J. Microglia and synapse interactions: fine tuning
neural circuits and candidate molecules. Front Cell Neurosci. 2013; 7:70. [PubMed: 23720611]
Muñoz-Espín D, Cañamero M, Maraver A, Gómez-López G, Contreras J, Murillo-Cuesta S,
Rodríguez-Baeza A, Varela-Nieto I, Ruberte J, Collado M, Serrano M. Programmed cell
senescence during mammalian embryonic development. Cell. 2013; 155:1104–1118. [PubMed:
Author Manuscript
24238962]
Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, Gordon S, Hamilton JA, Ivashkiv
LB, Lawrence T, et al. Macrophage Activation and Polarization: Nomenclature and Experimental
Guidelines. Immunity. 2014; 41(this issue):14–20. [PubMed: 25035950]
Naert G, Rivest S. CC chemokine receptor 2 deficiency aggravates cognitive impairments and amyloid
pathology in a transgenic mouse model of Alzheimer’s disease. J. Neurosci. 2011; 31:6208–6220.
[PubMed: 21508244]
Nahrendorf M, Swirski FK, Aikawa E, Stangenberg L, Wurdinger T, Figueiredo JL, Libby P,
Weissleder R, Pittet MJ. The healing myocardium sequentially mobilizes two monocyte subsets
with divergent and complementary functions. J. Exp. Med. 2007; 204:3037–3047. [PubMed:
18025128]
Nayak D, Roth TL, McGavern DB. Microglia development and function. Annu. Rev. Immunol. 2014;
32:367–402. [PubMed: 24471431]
Nucera S, Biziato D, De Palma M. The interplay between macrophages and angiogenesis in
development, tissue injury and regeneration. Int. J. Dev. Biol. 2011; 55:495–503. [PubMed:
Author Manuscript
21732273]
Okabe Y, Medzhitov R. Tissue-specific signals control reversible program of localization and
functional polarization of macrophages. Cell. 2014; 157:832–844. [PubMed: 24792964]
Orkin SH, Zon LI. Hematopoiesis: an evolving paradigm for stem cell biology. Cell. 2008; 132:631–
644. [PubMed: 18295580]
Ortega N, Wang K, Ferrara N, Werb Z, Vu TH. Complementary interplay between matrix
metalloproteinase-9, vascular endothelial growth factor and osteoclast function drives
endochondral bone formation. Dis. Model. Mech. 2010; 3:224–235. [PubMed: 20142327]
Paolicelli RC, Bolasco G, Pagani F, Maggi L, Scianni M, Panzanelli P, Giustetto M, Ferreira TA,
Guiducci E, Dumas L, et al. Synaptic pruning by microglia is necessary for normal brain
development. Science. 2011; 333:1456–1458. [PubMed: 21778362]
Parkhurst CN, Yang G, Ninan I, Savas JN, Yates JR 3rd, Lafaille JJ, Hempstead BL, Littman DR, Gan
WB. Microglia promote learning-dependent synapse formation through brain-derived neurotrophic
factor. Cell. 2013; 155:1596–1609. [PubMed: 24360280]
Author Manuscript
Qu C, Edwards EW, Tacke F, Angeli V, Llodrá J, Sanchez-Schmitz G, Garin A, Haque NS, Peters W,
van Rooijen N, et al. Role of CCR8 and other chemokine pathways in the migration of monocyte-
derived dendritic cells to lymph nodes. J. Exp. Med. 2004; 200:1231–1241. [PubMed: 15534368]
Randolph GJ. Proliferating macrophages prevail in atherosclerosis. Nat. Med. 2013; 19:1094–1095.
[PubMed: 24013746]
Randolph GJ. Mechanisms that regulate macrophage burden in atherosclerosis. Circ. Res. 2014;
114:1757–1771. [PubMed: 24855200]
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 21
Robbins CS, Hilgendorf I, Weber GF, Theurl I, Iwamoto Y, Figueiredo JL, Gorbatov R, Sukhova GK,
Gerhardt LM, Smyth D, et al. Local proliferation dominates lesional macrophage accumulation in
Author Manuscript
atherosclerosis. Nat. Med. 2013; 19:1166–1172. [PubMed: 23933982]
Rosas M, Davies LC, Giles PJ, Liao CT, Kharfan B, Stone TC, O’Donnell VB, Fraser DJ, Jones SA,
Taylor PR. The transcription factor Gata6 links tissue macrophage phenotype and proliferative
renewal. Science. 2014; 344:645–648. [PubMed: 24762537]
Roumier A, Béchade C, Poncer JC, Smalla KH, Tomasello E, Vivier E, Gundelfinger ED, Triller A,
Bessis A. Impaired synaptic function in the microglial KARAP/DAP12-deficient mouse. J.
Neurosci. 2004; 24:11421–11428. [PubMed: 15601948]
Samokhvalov IM. Deconvoluting the ontogeny of hematopoietic stem cells. Cell. Mol. Life Sci. 2014;
71:957–978. [PubMed: 23708646]
Samokhvalov IM, Samokhvalova NI, Nishikawa S. Cell tracing shows the contribution of the yolk sac
to adult haematopoiesis. Nature. 2007; 446:1056–1061. [PubMed: 17377529]
Sawyer RT, Strausbauch PH, Volkman A. Resident macrophage proliferation in mice depleted of
blood monocytes by strontium-89. Lab. Invest. 1982; 46:165–170. [PubMed: 6174824]
Schmidl C, Renner K, Peter K, Eder R, Lassmann T, Balwierz PJ, Itoh M, Nagao-Sato S, Kawaji H,
Author Manuscript
Carninci P, et al. FANTOM consortium. Transcription and enhancer profiling in human monocyte
subsets. Blood. 2014; 123:e90–e99. [PubMed: 24671955]
Schulz C, Gomez Perdiguero E, Chorro L, Szabo-Rogers H, Cagnard N, Kierdorf K, Prinz M, Wu B,
Jacobsen SE, Pollard JW, et al. A lineage of myeloid cells independent of Myb and hematopoietic
stem cells. Science. 2012; 336:86–90. [PubMed: 22442384]
Serbina, N.V., and Pamer, E.G. Monocyte emigration from bone marrow during bacterial infection
requires signals mediated by chemokine receptor CCR2. Nat. Immunol. 2006; 7:311–317.
[PubMed: 16462739]
Si Y, Tsou CL, Croft K., and Charo, I.F. CCR2 mediates hematopoietic stem and progenitor cell
trafficking to sites of inflammation in mice. J. Clin. Invest. 2010; 120:1192–1203. [PubMed:
20234092]
Sieweke, M.H., and Allen, J.E. Beyond stem cells: self-renewal of differentiated macrophages.
Science. 2013; 342:1242974. [PubMed: 24264994]
Stevens B, Allen NJ, Vazquez LE, Howell GR, Christopherson KS, Nouri N, Micheva KD, Mehalow
Author Manuscript
AK, Huberman AD, Stafford B, et al. The classical complement cascade mediates CNS synapse
elimination. Cell. 2007; 131:1164–1178. [PubMed: 18083105]
Storer M, Mas A, Robert-Moreno A, Pecoraro M, Ortells MC, Di Giacomo V, Yosef R, Pilpel N,
Krizhanovsky V, Sharpe J, Keyes WM. Senescence is a developmental mechanism that
contributes to embryonic growth and patterning. Cell. 2013; 155:1119–1130. [PubMed: 24238961]
Swirski FK, Nahrendorf M, Etzrodt M, Wildgruber M, Cortez-Retamozo V, Panizzi P, Figueiredo JL,
Kohler RH, Chudnovskiy A, Waterman P, et al. Identification of splenic reservoir monocytes and
their deployment to inflammatory sites. Science. 2009; 325:612–616. [PubMed: 19644120]
Tamoutounour S, Guilliams M, Montanana Sanchis F, Liu H, Terhorst D, Malosse C, Pollet E,
Ardouin L, Luche H, Sanchez C, et al. Origins and functional specialization of macrophages and
of conventional and monocyte-derived dendritic cells in mouse skin. Immunity. 2013; 39:925–938.
[PubMed: 24184057]
Tauber AI. Metchnikoff and the phagocytosis theory. Nat. Rev. Mol. Cell Biol. 2003; 4:897–901.
[PubMed: 14625539]
Tondravi MM, McKercher SR, Anderson K, Erdmann JM, Quiroz M, Maki R, Teitelbaum SL.
Author Manuscript
Osteopetrosis in mice lacking haematopoietic transcription factor PU.1. Nature. 1997; 386:81–84.
[PubMed: 9052784]
Tremblay ME, Lowery RL, Majewska AK. Microglial interactions with synapses are modulated by
visual experience. PLoS Biol. 2010; 8:e1000527. [PubMed: 21072242]
Tremblay ME, Zettel ML, Ison JR, Allen PD, Majewska AK. Effects of aging and sensory loss on glial
cells in mouse visual and auditory cortices. Glia. 2012; 60:541–558. [PubMed: 22223464]
Ueno M, Fujita Y, Tanaka T, Nakamura Y, Kikuta J, Ishii M, Yamashita T. Layer V cortical neurons
require microglial support for survival during postnatal development. Nat. Neurosci. 2013;
16:543–551. [PubMed: 23525041]
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 22
van Amerongen MJ, Harmsen MC, van Rooijen N, Petersen AH, van Luyn MJ. Macrophage depletion
impairs wound healing and increases left ventricular remodeling after myocardial injury in mice.
Author Manuscript
Am. J. Pathol. 2007; 170:818–829. [PubMed: 17322368]
van Furth R, Cohn ZA. The origin and kinetics of mononuclear phagocytes. J. Exp. Med. 1968;
128:415–435. [PubMed: 5666958]
Volkman A, Chang NC, Strausbauch PH, Morahan PS. Differential effects of chronic monocyte
depletion on macrophage populations. Lab. Invest. 1983; 49:291–298. [PubMed: 6887784]
Wake H, Moorhouse AJ, Jinno S, Kohsaka S, Nabekura J. Resting microglia directly monitor the
functional state of synapses in vivo and determine the fate of ischemic terminals. J. Neurosci.
2009; 29:3974–3980. [PubMed: 19339593]
Wake H, Moorhouse AJ, Miyamoto A, Nabekura J. Microglia: actively surveying and shaping
neuronal circuit structure and function. Trends Neurosci. 2013; 36:209–217. [PubMed:
23260014]
Wakselman S, Béchade C, Roumier A, Bernard D, Triller A, Bessis A. Developmental neuronal death
in hippocampus requires the microglial CD11b integrin and DAP12 immunoreceptor. J.
Neurosci. 2008; 28:8138–8143. [PubMed: 18685038]
Author Manuscript
Wang Y, Szretter KJ, Vermi W, Gilfillan S, Rossini C, Cella M, Barrow AD, Diamond MS, Colonna
M. IL-34 is a tissue-restricted ligand of CSF1R required for the development of Langerhans cells
and microglia. Nat. Immunol. 2012; 13:753–760. [PubMed: 22729249]
Weatherstone KB, Rich EA. Tumor necrosis factor/cachectin and interleukin-1 secretion by cord blood
monocytes from premature and term neonates. Pediatr. Res. 1989; 25:342–346. [PubMed:
2786182]
Wegiel J, Wiśniewski HM, Dziewiatkowski J, Tarnawski M, Kozielski R, Trenkner E, Wiktor-
Jedrzejczak W. Reduced number and altered morphology of microglial cells in colony
stimulating factor-1-deficient osteopetrotic op/op mice. Brain Res. 1998; 804:135–139.
[PubMed: 9729335]
Wiktor-Jedrzejczak W, Bartocci A, Ferrante AW Jr. Ahmed-Ansari A, Sell KW, Pollard JW, Stanley
ER. Total absence of colony-stimulating factor 1 in the macrophage-deficient osteopetrotic
(op/op) mouse. Proc. Natl. Acad. Sci. USA. 1990; 87:4828–4832. [PubMed: 2191302]
Wynn TA, Chawla A, Pollard JW. Macrophage biology in development, homeostasis and disease.
Nature. 2013; 496:445–455. [PubMed: 23619691]
Author Manuscript
Xue J, Schmidt SV, Sander J, Draffehn A, Krebs W, Quester I, De Nardo D, Gohel TD, Emde M,
Schmidleithner L, et al. Transcriptome-based network analysis reveals a spectrum model of
human macrophage activation. Immunity. 2014; 40:274–288. [PubMed: 24530056]
Yona S, Kim KW, Wolf Y, Mildner A, Varol D, Breker M, Strauss-Ayali D, Viukov S, Guilliams M,
Misharin A, et al. Fate mapping reveals origins and dynamics of monocytes and tissue
macrophages under homeostasis. Immunity. 2013; 38:79–91. [PubMed: 23273845]
You Q, Holt M, Yin H, Li G, Hu CJ, Ju C. Role of hepatic resident and infiltrating macrophages in
liver repair after acute injury. Biochem. Pharmacol. 2013; 86:836–843. [PubMed: 23876342]
Zhan Y, Paolicelli RC, Sforazzini F, Weinhard L, Bolasco G, Pagani F, Vyssotski AL, Bifone A,
Gozzi A, Ragozzino D, Gross CT. Deficient neuron-microglia signaling results in impaired
functional brain connectivity and social behavior. Nat. Neurosci. 2014; 17:400–406. [PubMed:
24487234]
Zhou L, Azfer A, Niu J, Graham S, Choudhury M, Adamski FM, Younce C, Binkley PF, Kolattukudy
PE. Monocyte chemoattractant protein-1 induces a novel transcription factor that causes cardiac
Author Manuscript
myocyte apoptosis and ventricular dysfunction. Circ. Res. 2006; 98:1177–1185. [PubMed:
16574901]
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 23
Author Manuscript
Author Manuscript
Figure 1. Macrophage Lineages, Ontogeny, and Contribution to Populations of Resident Tissue
Macrophages
(A) Schematic depicting the origins of embryonic and adult macrophage lineages. Genetic
lineage tracing using Flt3Cre and direct labeling techniques, including Csf1rCreER and
Runx1CreER, allow identification of adult-monocyte-derived and yolk-sac-derived
macrophages. There are no available tools for lineage tracing of fetal-liver-monocyte-
derived macrophages only.
(B) Contribution of macrophage lineages to populations of adult resident macrophages.
HSC-derived populations include embryonic populations and no definitive evidence of yolk
sac origin (embryonic), whereas HSCs (adult) have passed through a FLT3+ stage (Flt3-
Author Manuscript
Cre+) and are continually replaced by circulating adult monocytes.
Author Manuscript
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 24
Author Manuscript
Figure 2. The Life Cycle of Monocyte Subsets and Macrophages in Resting and Inflamed Tissues
In the vasculature, classical Ly6ChiCD43− monocytes give rise to nonclassical
Ly6CloCD43+ monocytes through an NR4A1-dependent manner (dashed black arrow).
Nonclassical monocytes go on to patrol the intravascular endothelial cell surface to clear
dying endothelial cells. Classical monocytes can exit the bloodstream and have the capacity
to patrol extravascular tissues. These tissue monocytes can transport antigens to lymph
Author Manuscript
nodes with minimal differentiation changes from their state in blood, although a proportion
can convert to Ly6Clo monocytes. However, in the context of inflammation, classical
monocytes readily differentiate to macrophages. These monocyte-derived macrophages are
distinct from resident macrophages, which in many organs are embryonically derived and
capable of sustaining themselves by local proliferation. Both recruited and resident
macrophages share the capacity for proliferation in tissue during inflammation.
Author Manuscript
Author Manuscript
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 25
Author Manuscript
Author Manuscript
Figure 3. Schematic Representation of Repopulation Strategies Used by Tissues to Replenish
Macrophage Numbers via Different Depletions Methods
(A) Cardiac macrophages. In the steady state, the majority of cardiac macrophages are
embryonically derived (red, Flt3-Cre−), and a smaller contribution is derived from HSCs
(green, Flt3-Cre+). After depletion, Ly6chi monocytes enter into tissue, proliferate, and
Author Manuscript
compete with proliferating resident cardiac macrophages to reestablish the steady-state
macrophage pool. After repopulation is complete, autonomy between tissue macrophages
and monocytes is restored. The pool of resident cardiac macrophages has undergone
“ontological reprogramming” and is now primarily composed of adult-derived macrophages.
In the absence of circulating blood monocytes (such as in Ccr2−/− mice), resident cardiac
macrophages are fully capable of reestablishing steady-state levels solely through in situ
proliferation.
(B) Alveolar macrophages. In the steady state, the majority of alveolar macrophages are
derived from embryonic progenitors, and a smaller contribution is derived from HSCs.
Alveolar macrophages are instructed by GM-CSF to differentiate into functional alveolar
macrophages that prevent alveolar proteinosis. After depletion (CD163-DTR), numbers of
resident macrophages are reduced, and repopulation occurs solely through in situ
Author Manuscript
proliferation of resident lung macrophages. If resident macrophages receive significant
genotoxic injury (lethal irradiation) as a depletion strategy, recruited monocytes gain a
competitive advantage and replace resident, embryonically derived lung macrophages. If
recruited monocytes cannot receive GM-CSF signals, then alveolar macrophages, despite
genotoxic injury, are capable of repopulating the lung macrophage niche.
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 26
Table 1
Tools Used for Defining Macrophage Lineages
Author Manuscript
Strategy Result Strength Limitation References
Runx1 CreER identifies yolk-sac- is expressed very early has a very limited Hoeffel et al. (2012);
derived macrophages during development window; results in Ginhoux et al. (2010)
incomplete labeling
during development
Csf1r CreER identifies yolk-sac- is expressed very early results in incomplete Epelman et al. (2014);
derived macrophages during development; labeling during Schulz et al. (2012)
has a longer window development
than Runx1CreER
Flt3 Cre defines cells that pass has strong reporter does not differentiate Epelman et al. (2014);
through definitive induction in circulating well between embryonic Schulz et al. (2012);
hematopoiesis (HSCs) monocytes in adult lineages (yolk sac versus Hashimoto et al. (2013);
animals; differentiates fetal monocytes); might Boyer et al. (2011)
well between embryonic not label some HSC-
and adult macrophages; derived macrophages
Author Manuscript
is excellent at following during times of rapid
population dynamics expansion (i.e., in early
during stress development or after
adoptive transplant)
Cx3cr1 GFP/+ identifies cells currently CX3CR1hi macrophages is not reliable for Yona et al. (2013);
expressing CX3CR1 correspond well to differentiating lineages Jung et al. (2000)
yolk-sac-derived in the adult
F4/80hiCD11blo
macrophages during
development only
Cx3cr1 Cre labels all cells that pass identifies traditionally is less useful for Yona et al. (2013)
through a CX3CR1+ CX3CR1− populations as differentiating between
stage having passed through recruited and resident
the CX3CR1+ stage macrophages in the adult
Cx3cr1 CreER has the potential to label identifies very strong is limited to tissue Yona et al. (2013);
embryonic macrophages reporter expression in macrophages that Goldmann et al. (2013);
Author Manuscript
at different stages of tissue macrophages express CX3CR1 Parkhurst et al. (2013)
development expressing high levels of at the time of induction
CX3CR1; only transiently
labels monocytes, which
allows for differential
targeting
Rag1 Cre identifies lymphomyeloid is the only technique for it is unclear whether Böiers et al. (2013)
progenitors specifically labeling progeny persist into
lymphomyeloid adulthood
progenitors
Parabiosis demonstrates tissue- does not use irradiation; typically demonstrates Hashimoto et al. (2013);
specific replacement of turnover is dependent on only 30% chimerism in Epelman et al. (2014);
resident macrophages the steady state rather wild-type mice; surgery Ajami et al. (2011);
by chimeric monocytes than tissue injury; use might alter steady-state Ajami et al. (2007)
of Ccr2−/− recipients trafficking
increases chimerism
to >90%
Author Manuscript
Sublethal irradiation induces chimerism in demonstrates blood radiation might alter Epelman et al. (2014)
and bone marrow blood monocytes without monocyte dependence steady dynamics (i.e.,
transplant eradicating resident of tissue macrophages injured tissue recruits
macrophages over long periods of time; monocytes)
tissue shielding can
minimize local radiation
injury
Immunity. Author manuscript; available in PMC 2015 June 17.
Epelman et al. Page 27
Table 2
Future Directions
Author Manuscript
Do tissue macrophages that live in mixed ontological lineages differ
transcriptionally?
Does targeting tissue macrophages on the basis of ontological
lineage reveal differential functions?
What is the extent of tissue macrophage plasticity?
Why do tissue macrophages proliferate during inflammation?
Author Manuscript
Author Manuscript
Author Manuscript
Immunity. Author manuscript; available in PMC 2015 June 17.
You might also like
- Airway Management in The Critically Ill: ReviewDocument9 pagesAirway Management in The Critically Ill: ReviewQuarmina HesseNo ratings yet
- Tissue-Specific Macrophages: How They Develop and Choreograph Tissue BiologyDocument17 pagesTissue-Specific Macrophages: How They Develop and Choreograph Tissue BiologyLinlinNo ratings yet
- Grupo 1Document7 pagesGrupo 1Jhon BarraNo ratings yet
- Developmental Control of Macrophage FunctionDocument11 pagesDevelopmental Control of Macrophage FunctionMaria SunflowerNo ratings yet
- Memoranda: Classification of Macrophages, CellsDocument8 pagesMemoranda: Classification of Macrophages, CellsRusu LauraNo ratings yet
- 2021 Munoz-Garcia et al. TheranosticsDocument26 pages2021 Munoz-Garcia et al. Theranosticsphilippe.lacroix38490No ratings yet
- The Serial Endosymbiosis Theory of Eukaryotic EvolutionDocument6 pagesThe Serial Endosymbiosis Theory of Eukaryotic EvolutionAmanda KhoirunisaNo ratings yet
- Intercellular Communication in The Cumulus - Oocyte Complex During Folliculogenesis: A ReviewDocument13 pagesIntercellular Communication in The Cumulus - Oocyte Complex During Folliculogenesis: A ReviewJohn XIENo ratings yet
- Cell Interactions Guide FateDocument25 pagesCell Interactions Guide Fatekaladhar reddyNo ratings yet
- ExosomesinfectiousdiseaseDocument10 pagesExosomesinfectiousdiseaseTaniaNo ratings yet
- 1644 FullDocument5 pages1644 FullhermannNo ratings yet
- Origins of multicellularityDocument4 pagesOrigins of multicellularityKylie TuguinayNo ratings yet
- HHS Public Access: Live Imaging Revolutionizes Understanding of Drosophila OogenesisDocument13 pagesHHS Public Access: Live Imaging Revolutionizes Understanding of Drosophila Oogenesis奕蓁陳No ratings yet
- 1 s2.0 S0022202X15447736 MainDocument7 pages1 s2.0 S0022202X15447736 MainKhan FatemaNo ratings yet
- Stem CellsDocument20 pagesStem CellsalibrownNo ratings yet
- Epithelial-Mesenchymal Crosstalk in Wolffian Duct and FetalDocument15 pagesEpithelial-Mesenchymal Crosstalk in Wolffian Duct and FetalEletícia SousaNo ratings yet
- Exosomas Vladimir EmilioDocument8 pagesExosomas Vladimir EmilioChente BookNo ratings yet
- Ellismar - 1802101010003 - Kelas 01Document17 pagesEllismar - 1802101010003 - Kelas 01EllismarNo ratings yet
- Adult Stem CellDocument13 pagesAdult Stem CellDipti BagdeNo ratings yet
- The Bone Marrow Niche For Haematopoietic Stem CellsDocument21 pagesThe Bone Marrow Niche For Haematopoietic Stem CellsHitomi-No ratings yet
- Jurnal Biosel Serial Endosymbiosis TheoryDocument4 pagesJurnal Biosel Serial Endosymbiosis TheoryHeny SinagaNo ratings yet
- Lepra2 Revista CellDocument2 pagesLepra2 Revista CellTavo CabañasNo ratings yet
- 2articulo_(2023) Genetic control of meiosis surveillance mechanisms in mammals (1)Document22 pages2articulo_(2023) Genetic control of meiosis surveillance mechanisms in mammals (1)mauricio yucumaNo ratings yet
- Developmental Biology ReferencesDocument79 pagesDevelopmental Biology ReferencesNeenu PrasannanNo ratings yet
- Adult Stem CellDocument9 pagesAdult Stem CellMeloveshop DropNo ratings yet
- Exosomes in Cancer Development, Metastasis, and ImmunityDocument33 pagesExosomes in Cancer Development, Metastasis, and ImmunityAlexa ReinkeNo ratings yet
- Trager 1963Document6 pagesTrager 1963IñigoGaitanSalvatellaNo ratings yet
- Leukocytes: (White Blood Cells)Document41 pagesLeukocytes: (White Blood Cells)syed nomanshahNo ratings yet
- Hemopoiesis1Document17 pagesHemopoiesis1Octafiani Trikartika DarimanNo ratings yet
- A5 Innate ImmunityDocument18 pagesA5 Innate ImmunityRizkia Milladina HidayatullohNo ratings yet
- Genetic Models of Macrophage Depletion: Li Hua, Jiayuan Shi, Leonard D. Shultz, and Guangwen RenDocument11 pagesGenetic Models of Macrophage Depletion: Li Hua, Jiayuan Shi, Leonard D. Shultz, and Guangwen RenFahad Hassan ShahNo ratings yet
- Cell Potency: Cell Potency Is A Cell's Ability To Differentiate Into Other Cell TypesDocument9 pagesCell Potency: Cell Potency Is A Cell's Ability To Differentiate Into Other Cell TypesAlmasidesNo ratings yet
- NIH Public Access: Author ManuscriptDocument42 pagesNIH Public Access: Author ManuscriptEletícia SousaNo ratings yet
- Shamir 2014 - Review organoid 3DDocument40 pagesShamir 2014 - Review organoid 3DDaniela PatricioNo ratings yet
- InTech-Stem Cells Ethical and Religious Issues PDFDocument17 pagesInTech-Stem Cells Ethical and Religious Issues PDFFionna PohanNo ratings yet
- Ok Stratification of Yeast Cells During Chronological Aging by Size Points To The Role of Trehalose in Cell VitalityDocument20 pagesOk Stratification of Yeast Cells During Chronological Aging by Size Points To The Role of Trehalose in Cell VitalityRoberto Emmanuel Bolaños RosalesNo ratings yet
- Emperipolesis Entosis and Cell Cannibalism DemystiDocument7 pagesEmperipolesis Entosis and Cell Cannibalism DemystiDiego Fernando Ortiz TenorioNo ratings yet
- Artigo 1Document7 pagesArtigo 1GUSTAVO DOS SANTOS CARDOSONo ratings yet
- Stem Cell ThesisDocument62 pagesStem Cell ThesisShradha SharmaNo ratings yet
- Cell Potency: TotipotencyDocument4 pagesCell Potency: TotipotencyMuhammad ZairulfikriNo ratings yet
- Exosomes Communicate Between CellsDocument8 pagesExosomes Communicate Between CellsGlauce L TrevisanNo ratings yet
- Macrophage Biology in Development, Homeostasis and DiseaseDocument11 pagesMacrophage Biology in Development, Homeostasis and DiseaseCristian Gutiérrez VeraNo ratings yet
- 1 s2.0 S001216061400579X MainDocument10 pages1 s2.0 S001216061400579X MainOnall SebsNo ratings yet
- GENERAL BIOLOGYDocument5 pagesGENERAL BIOLOGYFern Nicole TagatacNo ratings yet
- mitosis-WPS OfficeDocument5 pagesmitosis-WPS OfficeSheila Mae AramanNo ratings yet
- (Review) (Biomolecular Concepts) Kazuyuki Ohbo Et Shin-Ichi Tomizawa-2015Document9 pages(Review) (Biomolecular Concepts) Kazuyuki Ohbo Et Shin-Ichi Tomizawa-2015Priscilla FreschuNo ratings yet
- Cell BiologyDocument10 pagesCell BiologySaadNo ratings yet
- Building The Mammalian Testis: Origins, Differentiation, and Assembly of The Component Cell PopulationsDocument19 pagesBuilding The Mammalian Testis: Origins, Differentiation, and Assembly of The Component Cell Populationssendy ali baehaqiNo ratings yet
- Stem Cells in Gynecology 2012 American Journal of Obstetrics and GynecologyDocument8 pagesStem Cells in Gynecology 2012 American Journal of Obstetrics and GynecologyfujimeisterNo ratings yet
- The Origins of Cellular LifeDocument15 pagesThe Origins of Cellular LifeSIGIFREDO LOPEZNo ratings yet
- Development and differentiation of white blood cellsDocument12 pagesDevelopment and differentiation of white blood cellsHelenaNo ratings yet
- Stem CellDocument16 pagesStem Celltanishq groverNo ratings yet
- Newman&Müller 2010Document9 pagesNewman&Müller 2010Isolda Alanna RlNo ratings yet
- Developmental Biology H. 277 - Gillbert BarresiDocument57 pagesDevelopmental Biology H. 277 - Gillbert BarresiAndini M RNo ratings yet
- Formation and Types of Multinucleated Giant CellsDocument3 pagesFormation and Types of Multinucleated Giant CellsmarianekmeidNo ratings yet
- Stem CellDocument4 pagesStem CellZeth VargasNo ratings yet
- Modularity in Development and Evolution: Cite This PaperDocument4 pagesModularity in Development and Evolution: Cite This PaperKristy Veyna BautistaNo ratings yet
- HHS Public Access: Macrophage Epithelial Reprogramming Underlies Mycobacterial Granuloma Formation and Promotes InfectionDocument30 pagesHHS Public Access: Macrophage Epithelial Reprogramming Underlies Mycobacterial Granuloma Formation and Promotes InfectionEdgar DíazNo ratings yet
- The Use of Zygotic Embryos As Explants For in Vitro Propagation: An OverviewDocument27 pagesThe Use of Zygotic Embryos As Explants For in Vitro Propagation: An OverviewCesarRamNo ratings yet
- Scaffolds For Stem CellsDocument8 pagesScaffolds For Stem Cellscubed3No ratings yet
- Teachers Guide to Combating Misinformation About Autism TreatmentsDocument8 pagesTeachers Guide to Combating Misinformation About Autism TreatmentsBrandi MichelleNo ratings yet
- MainDocument3 pagesMainBrandi MichelleNo ratings yet
- Aluminium: Reason For Not Establishing A Guideline ValueDocument2 pagesAluminium: Reason For Not Establishing A Guideline ValueBrandi MichelleNo ratings yet
- Chelation Therapy - Guidance For The General PublicDocument4 pagesChelation Therapy - Guidance For The General PublicBrandi MichelleNo ratings yet
- Angle of Depression Lesson for Grade 9 MathDocument6 pagesAngle of Depression Lesson for Grade 9 MathPatrick Guerra100% (1)
- Edema Paru Kardiogenik Akut Kak TiaraDocument8 pagesEdema Paru Kardiogenik Akut Kak TiaraTyara LarisaNo ratings yet
- Bathymetry and Its Applications PDFDocument158 pagesBathymetry and Its Applications PDFArseni MaximNo ratings yet
- Effect of Water Immersion On Mechanical Properties of Polyurethane ...Document8 pagesEffect of Water Immersion On Mechanical Properties of Polyurethane ...konshoeNo ratings yet
- Aam April 2023Document198 pagesAam April 2023Adhitya DewantaraNo ratings yet
- CHAPTER-9, Respiration in Organisms.Document3 pagesCHAPTER-9, Respiration in Organisms.HarshitAhelani2379ScribdNo ratings yet
- Science: Pure Substances Vs MixturesDocument33 pagesScience: Pure Substances Vs MixturesElle Ma Rie100% (1)
- MSDS 442 BulkDocument2 pagesMSDS 442 BulkEliasNo ratings yet
- Water Quality Notes: Alkalinity and Hardness: P. Chris WilsonDocument6 pagesWater Quality Notes: Alkalinity and Hardness: P. Chris WilsonrishabhNo ratings yet
- How To Attract Love and Powerful Soul ConnectionsDocument5 pagesHow To Attract Love and Powerful Soul Connectionskinzaali71916No ratings yet
- 6kW V2G EV Charger Module Datasheet (2018)Document2 pages6kW V2G EV Charger Module Datasheet (2018)pysogaNo ratings yet
- Separation and Purification TechnologyDocument10 pagesSeparation and Purification TechnologyPedro Henrique MagachoNo ratings yet
- Resume Curt JerromeDocument5 pagesResume Curt JerromeAashish MuraliNo ratings yet
- Rate Analysis-Norms 1Document10 pagesRate Analysis-Norms 1yamanta_rajNo ratings yet
- Discover Over 70 Player Classes and RacesDocument1 pageDiscover Over 70 Player Classes and RacesFred FrançaNo ratings yet
- Entrepreneurship Macro Environment ForcesDocument26 pagesEntrepreneurship Macro Environment ForcesSivaNo ratings yet
- Kant On Religion and ScienceDocument21 pagesKant On Religion and ScienceEduardo CharpenelNo ratings yet
- Assignment in English Plus Core 11 Full CircleDocument76 pagesAssignment in English Plus Core 11 Full CircleRitu Maan68% (38)
- GypsumDocument79 pagesGypsumMansi GirotraNo ratings yet
- Bronchiolitis A Practical Approach For The General RadiologistDocument42 pagesBronchiolitis A Practical Approach For The General RadiologistTara NareswariNo ratings yet
- Measurement of Level in A Tank Using Capacitive Type Level ProbeDocument13 pagesMeasurement of Level in A Tank Using Capacitive Type Level ProbeChandra Sekar100% (1)
- AstigmatismDocument1 pageAstigmatismAmmellya PutriNo ratings yet
- Fundamental Calculations To Convert Intensities Into Concentrations in Optical Emission Spectrochemical AnalysisDocument14 pagesFundamental Calculations To Convert Intensities Into Concentrations in Optical Emission Spectrochemical AnalysisPYDNo ratings yet
- Caelus TT - Caelus Product TrainingDocument93 pagesCaelus TT - Caelus Product TrainingYader Daniel Ortiz CerdaNo ratings yet
- Beneficiation of Cassiterite From Primary Tin OresDocument11 pagesBeneficiation of Cassiterite From Primary Tin OresSULMAGNo ratings yet
- ON Code (Aci 318-77) : Commentary Building Requirements For Reinforced ConcreteDocument132 pagesON Code (Aci 318-77) : Commentary Building Requirements For Reinforced ConcreteAzmi BazazouNo ratings yet
- Steel Grid StructureDocument2 pagesSteel Grid StructureKusum RawatNo ratings yet
- Interfacial Phenomena in Pharmaceutical FormulationDocument21 pagesInterfacial Phenomena in Pharmaceutical FormulationNickson DrabeNo ratings yet
- Financing of New EnterpriseDocument8 pagesFinancing of New EnterpriseSunil BhamuNo ratings yet