Professional Documents
Culture Documents
Collins Et Al. 2018 - Prescribing FHD in Complex Patients, Highlights From EDTA
Uploaded by
ShareDialysisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Collins Et Al. 2018 - Prescribing FHD in Complex Patients, Highlights From EDTA
Uploaded by
ShareDialysisCopyright:
Available Formats
Prescribing Frequent Haemodialysis
in Complex Patients: Highlights from
the 55th ERA–EDTA Congress
This symposium took place on 26th May 2018, as part of the 55th
European Renal Association–European Dialysis and Transplant
Association (ERA–EDTA) Congress in Copenhagen, Denmark
Chairperson: Mari Vilpakka1
Speakers: Allan Collins,2,3 Natalie Borman,4 Maxence Ficheux,5 Sunita Nair6
1. Päijät-Häme Central Hospital, Lahti, Finland
2. NxStage Medical, Lawrence, Massachusetts, USA
3. Department of Medicine, University of Minnesota, Minneapolis, Minnesota, USA
4. Queen Alexandra Hospital, Wessex Kidney Centre, Portsmouth, England
5. CHR Clémenceau, Service Néphrologie-Hémodialyse-Transplantation, Caen, France
6. Shrewsbury and Telford Hospital NHS Trust, Shrewsbury, England
Disclosure: Dr Vilpakka, Dr Borman, Dr Ficheux, and Dr Nair are members of the NxStage
European Medical Board and have received speaker honoraria. Prof Collins is
employed by NxStage Medical as Chief Medical Officer.
Acknowledgements: Writing assistance was provided by Ms Kristine Kubisiak and Dr Eric Weinhandl,
NxStage Medical, Lawrence, Massachusetts, USA.
Support: The publication of this article was supported by NxStage Medical. The opinions and
views expressed in this manuscript are those of the authors and do not necessarily
represent the opinions and/or recommendations of NxStage Medical.
Disclaimer: The reader should check the package insert of all drugs and devices for indications,
dosage, warnings, and precautions.
Citation: EMJ Nephrol. 2018;6[1]:34-41.
Meeting Summary
At the 55th European Renal Association–European Dialysis and Transplant Association (ERA–EDTA)
Congress in Copenhagen, Denmark, physicians from the USA, UK, and France presented an educational
symposium entitled ‘Complex Patients May Be Better Treated with Frequent Hemodialysis: A Review
and Comparison of Published Evidence and Recent European Experience’. During this symposium,
leading physicians discussed the concepts underlying the prescription of frequent haemodialysis
(>3 sessions per week), the role of frequent haemodialysis in managing haemodynamic instability, treating
patients who require larger volume clearance due to pregnancy or obesity, and utilising frequent home
haemodialysis in the palliative care setting. This report briefly summarises the symposium.
34 NEPHROLOGY • July 2018 EMJ EUROPEAN MEDICAL JOURNAL
Prescribing Frequent Prescriptions that prioritise fluid removal can be
derived in the following manner. First, an upper
Haemodialysis limit of UFR (e.g., 10 mL/hour/kg) is selected
Professor Allan Collins and multiplied by body weight. Second, weekly
fluid intake (minus cumulative urine volume)
Haemodialysis, as it is widely prescribed today, is divided by the weight-scaled UFR limit to
has created a new and unique chronic disease identify the minimum number of ultrafiltration
state in patients with end-stage renal disease hours per week. Third, the minimum number of
who previously would not have survived. ultrafiltration hours per week is divided by the
This disease state is characterised by chronic number of treatments (e.g., 4, 5, or 6) that are
fluid overload,1,2 intense ultrafiltration during desired during the week to target symptom-free
dialysis,3 and persistent hyperphosphataemia,4,5 haemodialysis and control blood pressure, ideally
all of which impact the heart and vessels and with minimal use of antihypertensive medication.
eventually induce cardiovascular disease.1-5 With a UFR limit of 10 mL/hour/kg in a 70 kg
male patient, for example, the maximum rate
To address chronic disease, a dialysis prescription of fluid removal is 700 mL/hour. With a weekly
must extend beyond clearance of small solutes fluid intake of 10.5 L, ≥15 hours per week of
(e.g., urea) to target the health of organ systems. ultrafiltration are required; these could be
This shift in focus to monitoring a patient’s divided among five sessions of 3 hours each or
tolerance of therapy and slowing the decline six sessions of 2 hours each. Since the uremic
of cardiovascular health represents a new milieu is different during the first 90 minutes of
paradigm in dialysis delivery; this is particularly treatment, a conventional schedule comprising
important when dealing with complex patients, three sessions of 5 hours each does not provide
including those with uncontrolled hypertension, the same amount of clearance, despite equal
left ventricular hypertrophy, heart failure, hours of ultrafiltration.
hyperphosphataemia (despite prescription
of phosphate binders), recurrent intradialytic After addressing fluid volume, the haemodialysis
hypotension, and excessive post-treatment prescription must also maintain adequate
fatigue, as well as pregnant or obese patients, solute clearance, a task largely determined by
and frail patients in need of supportive care. dialysate saturation. High dialysate saturation
maximises the removal of small, middle,
The haemodialysis prescription can be and large molecular weight solutes, even in
conceptualised as a two-step approach that a system that utilises low-volume dialysate
focusses primarily on managing fluid, thereby (e.g., NxStage® System One™, NxStage Medical,
addressing blood pressure and cardiac geometry, Lawrence, Massachusetts, USA). Moreover, a
and secondarily on managing solute removal.6 system that utilises low-volume dialysate that is
This model begins with setting the weekly fluid highly saturated during treatment will improve
removal requirement and then the ultrafiltration clearance of phosphorus, a molecule that is
rate (UFR), by way of both treatment frequency otherwise difficult to remove. Conventional
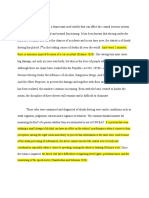
and session duration, to a rate that minimises systems with a flow rate of 500 mL/min, for
cardiac stunning, improves stability during example, achieve 55% urea saturation and 35%
treatment, and minimises post-treatment phosphorus saturation (in vivo).10 In contrast,
fatigue. Though a conventional UFR threshold low-volume dialysate systems with a flow rate of
is 10 mL/hour/kg, studies have suggested that 200 mL/min achieve >90% urea saturation and
limiting UFR as much as possible may reduce roughly 70% phosphorus saturation (Figure 1).
all-cause and cardiovascular mortality.3,6-9 With On nocturnal treatment with a flow rate of merely
frequent diurnal therapy for 2–3 hours per 100 mL/min, nearly 99% urea saturation and
session, UFR can be lowered to 6 mL/hour/kg, 95% phosphorus saturation can be achieved.10
and with nocturnal therapy, UFR can be lowered Dialysate saturation is coupled with the amount
to 2–3 mL/hour/kg. Only after managing fluid of weekly total body water clearance, which
should the haemodialysis prescription address varies on different modalities (Figure 2), to
solute removal with standardised Kt/V as a provide adequate clearance of solutes, including
guiding metric. middle molecules between urea and phosphorus.
Creative Commons Attribution-Non Commercial 4.0 July 2018 • NEPHROLOGY 35
Urea saturation at Qb: 400 mL/min
Low dialysate volume system
Dialysate-to-plasma concentration of urea
1.0
0.9
0.8
0.7
0.6
Conventional haemodialysis
0.5
0.4
0.3
0.2
0.1
0.0
0 50 100 150 200 250 300 350 400 450 500 550 600 650 700 750 800
Dialysate flow rate
Urea KoA in vivo 851 mL/min
Figure 1: Dialysate-to-plasma concentration of urea as a function of dialysate flow rate.
KoA: dialyser mass transfer-area coefficient; Qb: blood flow rate.
Adapted from Leypoldt K et al.10
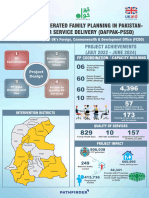
Nocturnal haemodialysis maximises solute fluid overload is a key contributing factor to
removal and minimises UFR, likely leading to the development of heart failure on dialysis
improved cardiovascular outcomes. (Figure 3).1,2 Firstly, within the constraints
of thrice-weekly in-centre haemodialysis,
A haemodialysis prescription reflecting the a higher UFR is needed to remove excess fluid
paradigm shift to maintaining cardiovascular in an overloaded patient; higher UFR can lead
health will focus first on fluid volume to cardiac and other organ system stunning
management, thereby minimising UFR and during dialysis, as well as to intradialytic
lowering blood pressure. Solute removal is hypotension.12 Notably, between 5% and 15%
considered next; the adequacy of removal is of patients on conventional haemodialysis
determined by dialysate saturation. These aims experience symptomatic hypotension, which is
may be best achieved by a frequent treatment characterised by cramps, dizziness, and nausea.13,14
regimen with low-volume dialysate, which limits Organ system stunning and symptomatic
UFR and maximises solute clearance, thus hypotension both contribute to longer post-
maintaining dialysis patient health. treatment recovery time, reducing quality of life
and potentially leading patients to sign-off early
or skip sessions entirely.15 Incomplete sessions
lead to more fluid overload, thus creating a cycle
Managing Haemodynamic of poor patient outcomes and adverse events.
Instability with Frequent Secondly, chronic fluid overload contributes
to uncontrolled hypertension, left ventricular
Haemodialysis hypertrophy, and heart failure, ultimately leading
to increased risk of hospitalisation and death.16
Doctor Natalie Borman
The thrice-weekly haemodialysis prescription
Cardiovascular disease remains the leading became the dominant regimen because of
cause of death in dialysis patients.1,11 feasibility, logistics, and cost, rather than the
Through multiple physiological pathways, achievement of optimal health outcomes.
36 NEPHROLOGY • July 2018 EMJ EUROPEAN MEDICAL JOURNAL
Normal 1,000 L/week
I
90
eGFR stage continuous clearance
Transplant 605 L/week
II
60
III HDx6† 342 L/week
30 nocturnal
IV HDx5* 128 L/week
diurnal
15 HDx3 PDx7
80–90 L/week
V 80–90 L/week
eGFR (mL/min) STD L/week urea
Figure 2: Volumes cleared per week among renal replacement therapies.
*30 L/session of dialysate. †60 L/session of dialysate.
eGFR: estimated glomerular filtration rate; HD: home dialysis; PD: peritoneal dialysis; STD: standard.
Adapted from Leypoldt K et al.10
The 2-day gap that is inherent in this schedule dialysis duration, permitting the therapy to meet
is strongly associated with increased risks weekly ultrafiltration requirements with low UFR,
of death, hospitalisation, and cardiovascular even in the case of fluid overload.
events.17-19 High UFR, which has been linked to
an increased risk of all-cause and cardiovascular The KIHDNEy22 study collected data from 182 home
mortality, is prevalent in patients on conventional haemodialysis patients using the NxStage System
haemodialysis.3,7-9 Moreover, the prevalence One at nine centres throughout Europe. This
of persistent hypertension on dialysis has retrospective study followed patients for 12 months
not changed during the past 10 years, after initiating frequent home haemodialysis.
despite considerable improvements in small Patients in the KIHDNEy cohort had a mean UFR
solute removal and extensive application of of 6.8 mL/hour/kg at 6 and 12 months follow-up
antihypertensive medications.2 after initiating frequent therapy, with 82% of
patients having UFR <10 mL/hour/kg.22 The cohort
More frequent therapy has the potential to also exhibited a statistically significant decline in
ameliorate these symptoms and improve antihypertensive use, averaging 1.51 agents per
patients’ outcomes. Data from the Frequent day at baseline and 0.91 agents per day after
Hemodialysis Network (FHN) Daily Trial show that 12 months of frequent therapy (p<0.001).22
patients prescribed more frequent haemodialysis The number of participants requiring no
for 1.50–2.75 hours per session have favourable antihypertensive medication increased from 27%
outcomes for left ventricular mass, systolic blood to 42% (p<0.001), and the number requiring at
pressure, physical health, and even death.21 least two antihypertensive agents concurrently
Eliminating the 2-day gap not only lowers the decreased from 43% to 25% (p<0.001).22
associated risks of adverse events but also
substantially reduces the likelihood of patients In a subset of 86 patients dialysing at home
accumulating excess fluid between consecutive for ≥5 sessions per week, under the care of the
dialysis sessions.21 Furthermore, tailoring the Wessex Kidney Centre, Portsmouth, UK, 75%
frequency of therapy also allows for increased reported immediate recovery after dialysis.
Creative Commons Attribution-Non Commercial 4.0 July 2018 • NEPHROLOGY 37
Left
Uncontrolled Heart Hospitalisation
ventricular
hypertension failure and death
hypertrophy
Fluid
overload
High Cramping,
Intradialytic 'Early sign-offs'
ultrafiltration dizziness,
hypotension and 'no-shows'
rate nausea, etc.
Cardiac and Long
Poor quality
organ system post-dialysis
of life
stunning recovery time
Figure 3: Causal diagram of the clinical pathophysiology of chronic fluid overload.
Across these 7,600 consecutive sessions on Frequent Home Haemodialysis
frequent therapy, a greater change in intradialytic
systolic blood pressure was associated with
in Complex Patients
increased number of symptoms reported
Doctor Maxence Ficheux
(p<0.0001) and longer post-treatment recovery
time (p<0.0001). Maintaining stable blood Managing patients who are either pregnant or
pressure reduces the likelihood of symptoms obese is uniquely challenging. Each of these
on dialysis, leading to fewer early sign-offs and patient types requires more volume clearance
less perpetuation of chronic fluid overload.15 than the typical haemodialysis patient and
presents unique physiological challenges
An ageing multicomorbid dialysis population
and potentially poor health outcomes.26,27
has resulted in a patient cohort that is, on
More frequent haemodialysis in the home
average, more susceptible to fluid overload and
setting may improve outcomes in both pregnant
haemodynamic instability than it was in the
patients and obese patients, as well as provide
past.23,24 These patients are extremely sensitive to
individualised and convenient therapy for these
fluid shifts and are at a high risk of hospitalisation complex cases.
due to recurrent episodes of fluid overload,
particularly after a 2-day gap in therapy.2 Women on haemodialysis are likely to experience
Furthermore, their haemodynamic instability decreased fertility due to both sexual dysfunction
compounds the difficulty in removing fluid.25 and reproductive hormonal dysfunction, including
Providing patients with shorter, more frequent amenorrhea.28,29 Specifically, lack of oestradiol-
haemodialysis sessions and minimising UFR has stimulated cyclic luteinising hormone secretion
been shown, in many cases, to engender fewer leads to ovarian failure (i.e., anovulation),
symptoms on dialysis, stabilise blood pressure, and an elevated prolactin concentration
improve fluid balance, and reduce the risk of contributes to abnormal uterine bleeding.30
hospitalisation.21,22 The above data suggest that These physiological obstacles have historically
by directly addressing chronic fluid overload, contributed to a low likelihood of successful
frequent haemodialysis can meaningfully improve pregnancy. Survey data from multiple continents
both cardiovascular outcomes and quality of life. have shown few pregnancies on dialysis
and a <50% probability of live birth among
pregnant patients.31-33
38 NEPHROLOGY • July 2018 EMJ EUROPEAN MEDICAL JOURNAL
Intensive haemodialysis may help improve poor patients who wish to conceive but are unable to
pregnancy outcomes. One meta-analysis that wait for a transplant.
assessed dialysis schedules and pregnancy
outcomes reported a negative correlation
between weekly haemodialysis duration and the
percentage of pregnancies ending in preterm Frequent Home Haemodialysis
(i.e., <37 weeks) delivery (R2=0.22; p=0.044).34 as Palliative Care
The same meta-analysis also reported negative
correlations between the percentage of small Doctor Sunita Nair
for gestational age infants and both weekly
haemodialysis duration (R2=0.54; p=0.017) Since the first successful dialysis treatment
and weekly haemodialysis frequency (R2=0.84; in 1945, the goal of dialysis therapy has
p=0.003).34 Recent survey results have suggested shifted from saving lives to sustaining lives,
that although prenatal complications and and subsequently to rehabilitation, with more
preterm delivery are still frequent, neonatal frequent haemodialysis prescribed to improve
survival has improved in the last 30 years, health-related quality of life. However, patients
which may be linked to the rise of more frequent still experience a high burden of symptoms,
and longer haemodialysis sessions.35 including pain, itching, lethargy, and restless legs.
Dialysis patients also have substantial functional
Obesity, which is prevalent in approximately limitations, which place a heavy burden on
1 in 4 dialysis patients in both the USA and family members and care partners.
France, is a common challenge.36,37 Patients with
a BMI >30 kg/m2 require more volume clearance The current dialysis delivery system focusses
than patients with a normal BMI.27 Frequent on achieving fluid volume and biochemical
haemodialysis in the home setting may address targets, aiming to reduce cardiovascular risk.
this challenge. Thirty-three (18%) patients in When these targets can no longer be achieved,
the KIHDNEy cohort had a BMI ≥30 kg/m2.22 the common practice is to withdraw dialysis
One year after initiating haemodialysis for ≥5 and assist patients embarking on end-of-life
sessions per week, these patients maintained journeys. However, some dialysis patients with
a mean standardised Kt/V of 2.53 (standard significant symptom burden and coexisting
deviation: 0.31) and mean UFR of 4.49 mL/hour/kg. terminal illness may wish to continue dialysis.
Concurrently, mean serum phosphorus among These patients’ goals do not align well with the
these patients decreased by 4%, despite a current interpretation of palliative care, which
24% reduction in mean phosphate binder pill is offered only to patients with a predictably
count. Furthermore, the use of antihypertensive short life expectancy and a desire to forgo
agents declined by 41%.22 life-prolonging treatment. In the UK, for instance,
patients are expected to withdraw from dialysis
These data, along with multiple case studies, before entering hospice care. A new palliative
provide compelling evidence that frequent home dialysis care model may address these currently
haemodialysis with low-volume dialysate not only unmet needs.
maintains adequate small solute clearance, but
also leads to improved outcomes and provides Merging renal care and palliative care is a
patients with a convenient and individualised dynamic process aimed at offering specialised
therapy. In a pregnant patient, increased care for people with chronic or serious illnesses.
frequency and duration of haemodialysis may This care model may be appropriate at any
increase the likelihood of live birth and permit the age and at any stage in a serious illness and
mother and neonate to return home more rapidly. can be provided alongside curative and life-
In obese patients, increased frequency and prolonging treatment. Comprehensive palliative
duration of haemodialysis may lessen the need care in patients with end-stage renal disease
for oral medications and lower the incidence focusses on providing patients with symptom
of dialysis-related side effects. Frequent home relief, supporting decision-making, and aligning
haemodialysis represents a practical and efficient treatment plans with patients’ goals. By adopting
method of therapy for complex patients and a multidisciplinary approach between the renal
gives new hope to end-stage renal disease and palliative care teams, the model provides
Creative Commons Attribution-Non Commercial 4.0 July 2018 • NEPHROLOGY 39
truly holistic care by integrating psychosocial without a requirement of costly remodelling
and spiritual needs with medical needs, of the site. Furthermore, this modality
and co-ordinating both medical and social requires less training time, is financially viable,
services, thereby providing an extra layer of and allows ongoing palliative input through its
support for patients and their families. monitoring system.39
Frequent haemodialysis in the home setting is This paradigm shift in providing palliative
arguably the most straightforward method of dialysis to patients with coexisting terminal
implementing this new paradigm of palliative illness resets the treatment goals of dialysis,
dialysis care. Frequent therapy has been focussing almost entirely on controlling
shown to reduce symptom burden, reduce symptoms and individualising treatment targets.
morbidity, and improve quality of life, particularly Palliative care should be part of the continuum
in patients with multiple comorbidities.38 of holistic, quality care for renal patients.
Home haemodialysis also allows patients to In this way, we will continue to extend the
dialyse in their preferred setting, which is dialysis paradigm from one that rehabilitates
especially important during a vulnerable time in patients when life expectancy is long to one that
life. The NxStage System One enables dialysis comforts patients when life expectancy is short.
delivery in both home and hospice settings
References
1. Ahmadmehrabi S, Tang WHW. risk in home hemodialysis patients. with the long interdialytic gap in
Hemodialysis-induced cardiovascular Abstract SaO042. ERA-EDTA thrice-weekly hemodialysis patients.
disease. Semin Dial. 2018;31(3): Congress, 24-27 May, 2018. Kidney Int. 2015;88(3):569-75.
258-67.
10. Leypoldt K et al. Urea clearance 19. Slinin Y et al. Ultrafiltration rate in
2. Kim EJ et al. Extracellular fluid/ modelling using 300 mL/min of conventional hemodialysis: Where
intracellular fluid volume ratio as dialysate flow. Abstract FR-PO824. are the limits and what are the
a novel risk indicator for all-cause American Society of Nephrology consequences? Semin Dial. 2018.
mortality and cardiovascular disease (ASN) Kidney Week, 31 October-5 [Epub ahead of print].
in hemodialysis patients. PLoS One. November, 2017.
2017;12(1):e0170272. 20. US-DOPPS Practice Monitor. Feature
11. Hill NR et al. Global prevalence of Data. 2016. Available at: http://www.
3. Flythe JE et al. Rapid fluid removal chronic kidney disease - A systematic dopps.org/DPM. Last accessed:
during dialysis is associated with review and meta analysis. PLoS One. 22 June 2018.
cardiovascular morbidity and 2016;11(7):e0158765.
mortality. Kidney Int. 2011;79(2):250-7. 21. Daugirdas JT et al. Effect of frequent
12. Burton JO et al. Hemodialysis- hemodialysis on residual kidney
4. Noori N et al. Dietary potassium induced cardiac injury: Determinants function. Kidney Int. 2013;
intake and mortality in long-term and associated outcomes. Clin J Am 83(5):949-58.
hemodialysis patients. Am J Kidney Soc Nephrol. 2009;4(5):914-20.
Dis. 2010;56(2):338-47. 22. Nair S et al. More frequent
13. MacEwen C et al. Relationship haemodialysis improved outcomes:
5. Tentori F et al. Mortality risk for between hypotension and cerebral The wish comes true at home.
dialysis patients with different levels ischemia during hemodialysis. J Am EMJ Nephrol. 2017;5(1):36-42.
of serum calcium, phosphorus, and Soc Nephrol. 2017;28(8):2511-20.
PTH: The Dialysis Outcomes and 23. Tonelli M, Riella M. Chronic kidney
Practice Patterns Study (DOPPS). Am 14. Sands JJ et al. Intradialytic disease and the aging population.
J Kidney Dis. 2008;52(3):519-30. hypotension: Frequency, sources Indian J Nephrol. 2014;24(2):71-4.
of variation and correlation with
6. Agar JW. Personal viewpoint: clinical outcome. Hemodial Int. 24. Thomas B et al. Maintenance dialysis
Limiting maximum ultrafiltration 2014;18(2):415-22. throughout the world in years
rate as a potential new measure of 1990 and 2010. J Am Soc Nephrol.
dialysis adequacy. Hemodial Int. 15. Rocco MV, Burkart JM. Prevalence of 2015;26(11):2621-33.
2016;20(1):15-21. missed treatments and early sign-offs
in hemodialysis patients. J Am Soc 25. Chirakarnjanakorn S et al.
7. Chazot C et al. Even a moderate fluid Nephrol. 1993;4(5):1178-83. Cardiovascular impact in patients
removal rate during individualised undergoing maintenance
haemodialysis session times is 16. Zipes DP et al., Braunwald’s heart hemodialysis: Clinical management
associated with decreased patient disease: A textbook of cardiovascular considerations. Int J Cardiol.
survival. Blood Purif. 2017; medicine (2018) 10th edition, 2017;232:12-23.
44(2):89-97. Philadelphia: Elsevier.
26. Manisco G et al. Pregnancy in end-
8. Assimon MM et al. Ultrafiltration 17. Foley R et al. Long interdialytic stage renal disease patients on
rate and mortality in maintenance interval and mortality among patients dialysis: How to achieve a successful
hemodialysis patients. Am J Kidney receiving hemodialysis. N Engl J Med. delivery. Clin Kidney J.
Dis. 2016;68(6):911-22. 2011;365(12):1099-107. 2015;8(3):293-9.
9. Kubisiak K et al. Ultrafiltration rate is 18. Fotheringham J et al. The mortality 27. Feezor R. Approach to permanent
positively associated with mortality and hospitalization rates associated hemodialysis access in obese
40 NEPHROLOGY • July 2018 EMJ EUROPEAN MEDICAL JOURNAL
patients. Semin Vasc Surg. Association. Br J Obstet Gynaecol. 36. Doshi M et al. Examining the
2011;24(2):96-101. 1980;87(10):839-45. robustness of the obesity paradox in
maintenance hemodialysis patients:
28. Strippoli et al. Sexual dysfunction 32. Okundaye I et al. Registry of A marginal structural model analysis.
in women with ESRD requiring pregnancy in dialysis patients. Nephrol Dial Transplant.
hemodialysis. Clin J Am Soc Nephrol. Am J Kidney Dis. 1998;31(5):766-73. 2016;31:1310-9.
2012;7(6):974-81.
33. Toma et al. Pregnancy in 37. Agence de la Biomédecine. Réseau
29. Holley et al. Changes in fertility and women receiving renal dialysis Epidémiologie, Information,
hormone replacement therapy in or transplantation in Japan: Néphrologie (REIN) Annual Report
kidney disease. Adv Chronic Kidney A nationwide survey. Nephrol Dial 2016. Available at: https://www.
Dis. 2013;20(3):240-5. Transplant. 1999;14(6):1511-6. agence-biomedecine.fr/IMG/pdf/
30. Matuszkiewicz-Rowińska J et al. 34. Piccoli GB et al. Pregnancy in dialysis rapportrein2016.compressed.pdf.
Endometrial morphology and patients in the new millennium: Last accessed: 25 June 2018.
pituitary-gonadal axis dysfunction A systematic review and meta- 38. Morrison RS, Meier DE. Clinical
in women of reproductive age regression analysis correlating practice. Palliative care. N Engl J Med.
undergoing chronic haemodialysis dialysis schedules and pregnancy 2004;350(25):2582-90.
- A multicentre study. Nephrol Dial outcomes. Nephrol Dial Transplant.
Transplant. 2004;19(8):2074-7. 2016;31(11):1915-34. 39. Benain JP. et al. Economic
assessment of home and in-centre
31. Successful pregnancies in women 35. Nadeau-Fredette AC et al. End-stage haemodialysis from a dialysis centre
treated by dialysis and kidney renal disease and pregnancy. perspective in the UK. British Journal
transplantation. Report from the Adv Chronic Kidney Dis. of Renal Medicine. 2018;23(1):27-31.
Registration Committee of the 2013;20(3):246-52.
European Dialysis and Transplant
Creative Commons Attribution-Non Commercial 4.0 July 2018 • NEPHROLOGY 41
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Biological Warfare Agents - AgronDocument129 pagesBiological Warfare Agents - AgronMARK ARQUE LACANARIANo ratings yet
- Your Grief Youre Not GoingDocument50 pagesYour Grief Youre Not GoingalexcostelaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- RN MedSurgDocument685 pagesRN MedSurgArgyll Baye Ansuas100% (4)
- Benefits of Autophagy, Plus How To Induce ItDocument4 pagesBenefits of Autophagy, Plus How To Induce ItОля Явор100% (1)
- Test Bank For Medical Assisting Administrative and Clinical Competencies 8th Edition by BlesiDocument18 pagesTest Bank For Medical Assisting Administrative and Clinical Competencies 8th Edition by BlesiMary Lawson100% (33)
- Sultan Ali Akbar Sinenggayan High School: Program of Activities Activity Target Date Resources Need Expected OutputDocument5 pagesSultan Ali Akbar Sinenggayan High School: Program of Activities Activity Target Date Resources Need Expected OutputRAHIB SAMAYATINNo ratings yet
- The Nursing Council of Hong KongDocument11 pagesThe Nursing Council of Hong KongbienNo ratings yet
- DM No. 2022-0287 Updated Moa and Tor PRDPDocument8 pagesDM No. 2022-0287 Updated Moa and Tor PRDPDRMC Infirmary100% (1)
- CHC33015-Sub 1 AssessmentDocument102 pagesCHC33015-Sub 1 AssessmentMaimuna100% (8)
- Artis User Manual ENG SP00105 Revision 0Document924 pagesArtis User Manual ENG SP00105 Revision 0ShareDialysis88% (17)
- Risk Assessment - Working Ship SideDocument3 pagesRisk Assessment - Working Ship SideSatya SatishNo ratings yet
- Impaired Physical MobilityDocument11 pagesImpaired Physical MobilityAgronaSlaughter100% (1)
- Report 2013Document340 pagesReport 2013ShareDialysisNo ratings yet
- Report2017 For CommissionersDocument422 pagesReport2017 For CommissionersShareDialysisNo ratings yet
- Report2014 PDFDocument332 pagesReport2014 PDFShareDialysis100% (1)
- Report2015 PDFDocument380 pagesReport2015 PDFShareDialysisNo ratings yet
- Rapportrein2017 PDFDocument382 pagesRapportrein2017 PDFShareDialysisNo ratings yet
- Borman Et Al. 2019 - Survival After End-Stage Renal Failure, Preventing Cardiac Death in ESRDDocument3 pagesBorman Et Al. 2019 - Survival After End-Stage Renal Failure, Preventing Cardiac Death in ESRDShareDialysisNo ratings yet
- Nair Et Al. 2016 - Frequent Home Haemodialysis, A Review of The EvidenceDocument8 pagesNair Et Al. 2016 - Frequent Home Haemodialysis, A Review of The EvidenceShareDialysisNo ratings yet
- Cherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyDocument10 pagesCherukuri Et Al. 2018 - Home Haemodialysis Treatment and Outcomes, Retrospective Analysis of KIHDNEyShareDialysisNo ratings yet
- Nair, Goffin Et Al. 2017 - More Frequent Haemodialysis Improved OutcomesDocument7 pagesNair, Goffin Et Al. 2017 - More Frequent Haemodialysis Improved OutcomesShareDialysisNo ratings yet
- 2008K Operator's Manual 490042 Rev NDocument239 pages2008K Operator's Manual 490042 Rev NShareDialysis100% (2)
- Timing of Umbilical Cord Clamping and Neonatal Jaundice in Singleton TermDocument5 pagesTiming of Umbilical Cord Clamping and Neonatal Jaundice in Singleton TerminesNo ratings yet
- Minimal Invasive Dentistry: Review ArticleDocument4 pagesMinimal Invasive Dentistry: Review ArticleKarissa NavitaNo ratings yet
- PE 2112 Week 1-19 OedDocument5 pagesPE 2112 Week 1-19 OedEury Marc Suhi-anNo ratings yet
- Breast Imagingand InterventionalDocument353 pagesBreast Imagingand Interventionalservice iyadMedicalNo ratings yet
- Meperidine Hydro ChlorideDocument4 pagesMeperidine Hydro Chlorideapi-3797941No ratings yet
- Allotment List Medical r1 26.04.2020 For WebDocument29 pagesAllotment List Medical r1 26.04.2020 For WebManu PaliwalNo ratings yet
- Vital Signs: Nursing Assessment Techniques ModuleDocument24 pagesVital Signs: Nursing Assessment Techniques ModuleSHELLAH MARIE MAMAWAGNo ratings yet
- For Partial Fulfilment of The Requirement For TheDocument45 pagesFor Partial Fulfilment of The Requirement For ThesalmanNo ratings yet
- Piriformis Syndrome: DefinitionDocument3 pagesPiriformis Syndrome: DefinitionMd Sherajul HaqueNo ratings yet
- LESSON 1 Occupational Health and Safety Policies and ProceduresDocument11 pagesLESSON 1 Occupational Health and Safety Policies and Procedurescky yarteNo ratings yet
- Medina, Joanna BN3C - NCP FormatDocument7 pagesMedina, Joanna BN3C - NCP FormatJOANNA MARIE MEDINANo ratings yet
- RRL ExhalyzerDocument5 pagesRRL ExhalyzerKimberleigh MetrioNo ratings yet
- GL3655EDocument0 pagesGL3655EandyhrNo ratings yet
- Requisite Skills and Abilities: Becoming A Licensed Practical Nurse in CanadaDocument12 pagesRequisite Skills and Abilities: Becoming A Licensed Practical Nurse in CanadaneoclintNo ratings yet
- Addisons DiseaseDocument1 pageAddisons DiseaseAndreia Palade100% (1)
- ZXXZDocument6 pagesZXXZfei cuaNo ratings yet
- RH BillDocument23 pagesRH BillArah Obias CopeNo ratings yet
- Distinguishes Aerobic From MuscleDocument2 pagesDistinguishes Aerobic From MuscleVolley PilgrimsNo ratings yet
- Poster Sindh 2-01-2024Document11 pagesPoster Sindh 2-01-2024FM Printers111No ratings yet