Professional Documents
Culture Documents
Hipopituitarismo Lectura Motivadora1) PDF
Hipopituitarismo Lectura Motivadora1) PDF
Uploaded by
Dávalos M. MayteOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hipopituitarismo Lectura Motivadora1) PDF
Hipopituitarismo Lectura Motivadora1) PDF
Uploaded by
Dávalos M. MayteCopyright:
Available Formats
Seminar
Hypopituitarism
Claire E Higham, Gudmundur Johannsson, Stephen M Shalet
Hypopituitarism refers to deficiency of one or more hormones produced by the anterior pituitary or released from the Lancet 2016; 388: 2403–15
posterior pituitary. Hypopituitarism is associated with excess mortality, a key risk factor being cortisol deficiency due to Published Online
adrenocorticotropic hormone (ACTH) deficiency. Onset can be acute or insidious, and the most common cause in March 31, 2016
http://dx.doi.org/10.1016/
adulthood is a pituitary adenoma, or treatment with pituitary surgery or radiotherapy. Hypopituitarism is diagnosed
S0140-6736(16)30053-8
based on baseline blood sampling for thyroid stimulating hormone, gonadotropin, and prolactin deficiencies, whereas
Department of Endocrinology,
for ACTH, growth hormone, and antidiuretic hormone deficiency dynamic stimulation tests are usually needed. Christie Hospital NHS
Repeated pituitary function assessment at regular intervals is needed for diagnosis of the predictable but slowly Foundation Trust, Manchester,
evolving forms of hypopituitarism. Replacement treatment exists in the form of thyroxine, hydrocortisone, sex steroids, UK (C E Higham DPhil,
Prof S M Shalet MD); Centre for
growth hormone, and desmopressin. If onset is acute, cortisol deficiency should be replaced first. Modifications in
Endocrinology and Diabetes,
replacement treatment are needed during the transition from paediatric to adult endocrine care, and during pregnancy. Institute of Human
Development, Faculty of
Introduction adenomas is low in childhood and peaks at age Medical and Human Sciences,
University of Manchester,
Hypopituitarism is deficiency of one or more pituitary 60–65 years.3,4 The combined results from these studies
Manchester Academic Health
hormones. The pituitary gland has two lobes. Within the suggest an increase in the prevalence of hypopituitarism, Science Centre, Manchester, UK
anterior lobe, six hormones are produced: growth which might be a result of increased use of high- (C E Higham, Prof S M Shalet);
hormone, the gonadotropins follicle stimulating resolution imaging. Department of Internal
Medicine and Clinical
hormone (FSH) and luteinising hormone, adreno-
Nutrition, Sahlgrenska
corticotropic hormone (ACTH), thyroid stimulating Mortality Academy, University
hormone (TSH), and prolactin. The posterior pituitary Findings from several studies have shown excess of Gothenburg,
lobe contains two hormones, oxytocin and antidiuretic mortality in patients with hypopituitarism,5 with higher Gothenburg, Sweden
(Prof G Johannsson MD); and
hormone (ADH), which are produced in the supraoptic mortality in women than in men.6 This excess mortality Department of Endocrinology,
and paraventricular nuclei of the hypothalamus and was mainly attributable to cardiovascular and respiratory Sahlgrenska University
transported axonally via the pituitary stalk to be stored diseases. This reported increased mortality was most Hospital, Gothenburg, Sweden
and released from the posterior lobe. likely multifactorial and related to young age at diagnosis, (Prof G Johannsson)
In this Seminar, we describe the range of mechanisms the underlying cause of the hypopituitarism (eg, cranio- Correspondence to:
Prof Stephen M Shalet, Endocrine
underlying hypopituitarism, geographic variations both pharyngioma), tumour treatment using transcranial
Department, Christie Hospital
in terms of causation and treatments, and future surgery or radiotherapy, and presence of diabetes NHS Foundation Trust,
therapeutic options. insipidus.6–8 In other studies, increased mortality in Manchester M20 4BX, UK
patients with cortisol deficiency has been reported.9 In a stephen.m.shalet@manchester.
ac.uk
Epidemiology nationwide study of patients with non-functioning
The incidence and prevalence of anterior pituitary pituitary adenoma,3 excess mortality was noted in women
hormone deficiency, including growth hormone with hypopituitarism, but not in men, suggesting the
deficiency (GHD), has only been reported in one study,1 importance of sex on outcome in patients with
which comprised a mean population sample of hypothalamic–pituitary disorders.
146 000 adult inhabitants in South Galicia, Spain, and Findings from prospective studies in patients with
showed an increase in the prevalence of hypopituitarism hypopituitarism who were receiving growth hormone
from 29·0 per 100 000 people to 45·5 per 100 000 people have shown an excess mortality of 13–42%7–9 or no excess
between 1992 and 1999, with a mean annual incidence of mortality.10 Excess cardiovascular mortality was not
4·21 cases per 100 000 population, which remained stable found, although increased mortality from stroke was
during this period. In other studies, the epidemiology of reported among women and those who received
the underlying causes of hypopituitarism has been radiotherapy.8 The varying pattern of mortality might be a
reported, such as pituitary adenomas, a common cause result of improved care of patients, but could also be due
of hypopituitarism in adults. In Sweden, the national to heterogeneity of patient selection.
incidence of non-functioning pituitary adenomas
increased from 0·6 cases per 100 000 people to 1·1 cases
per 100 000 people between 1975 and 1991.2 Between Search strategy and selection criteria
2002 and 2011, the annual incidence was 2·03 cases We searched PubMed, Embase, and Cochrane Databases (last
per 100 000 people, suggesting a further increase.3 search done Sept 29, 2015) using the search terms “hypopit*”
In a regional Finnish study,4 the annual incidence AND “epidemiology” OR “presentation” OR “signs and
of non-functioning pituitary adenomas was 1·0 per symptoms” OR “investigations” OR “management”. Relevant
100 000 people between 1992 and 2007, with occurrences articles written in English were reviewed for inclusion, with
of incidentally discovered masses tripling during this the emphasis on those published in the past 5 years.
time period. The incidence of non-functioning pituitary
www.thelancet.com Vol 388 November 12, 2016 2403
Seminar
Causes for pituitary tumours, nasopharyngeal carcinoma, retino-
In adults, the most common cause of hypopituitarism is blastoma, and other tumours in the hypothalamic–
a pituitary adenoma or treatment with pituitary surgery pituitary area and in those who receive whole head
or radiotherapy.11 The profile of pituitary hormone irradiation for brain tumours. Additionally, children who
deficiencies varies depending on the site within the receive prophylactic cranial irradiation for acute
hypothalamic–pituitary axis and the nature of the lymphatic leukaemia or total body irradiation for various
underlying pathological process. For example, diabetes malignant diseases are at risk of hypopituitarism, and, in
insipidus can occur in patients with lesions affecting the particular, GHD, many years later.19
pituitary stalk, but not with lesions confined to the Newer methods of delivery of radiation to pituitary
pituitary fossa. tumours have been introduced, such as proton beam
therapy, and radiosurgery involving stereotactic irradiation
Pituitary and hypothalamic mass lesions with the Leksell gamma knife or a stereotactic linear
Benign pituitary tumours account for most pituitary accelerator. The principal advantage of these methods is
mass lesions, although secondary tumours do occur, the consistent dose delivery to the tumour, which is
with metastasis to the pituitary gland reported from associated with less irradiation outside the targeted
carcinomas of the breast, lung, colon, and prostate. At volume. Findings from reports20–22 suggest that hypo-
presentation, macroadenomas (≥1 cm) are commonly pituitarism occurs even after these newer methods of
associated with deficiencies in anterior pituitary irradiation, but the prevalence of this complication might
hormones.12,13 Evidence suggests that the causative be reduced;23 however, lengthy follow-up is needed before
mechanism is compression of the portal vessels in the this finding can be proved conclusively, in view of the
pituitary stalk, either secondary to direct expansion of the known relation between radiation dose and speed of onset
tumour mass or due to raised intrasellar pressure.14 Non- of hypopituitarism.24
functioning pituitary microadenomas (<1 cm) are more
common than macroadenomas, being found in between Trauma and vascular injury
1·5% and 27% of autopsies in the general population; Traumatic brain injury (TBI) is a long-recognised cause
these tumours are rarely associated with hypopituitarism. of hypopituitarism.25–27 The extent of hypopituitarism
Craniopharyngiomas are the third most common ranges from isolated deficiency to panhypopituitarism,
intracranial tumour and account for most parasellar and the prevalence of reported hypopituitarism after TBI
tumours; 35% occur in patients younger than 18 years.15 varies widely (15–90%).25–27 A possible relation between
Other mass lesions in the parapituitary area capable the severity of TBI and the prevalence of hypopituitarism
of causing hypopituitarism include chondromas, has not been shown, and is complicated by reports of
chordomas, germinomas, suprasellar meningiomas, hypopituitarism after low-intensity repeated trauma25 in
astrocytomas of the optic nerve, and other primary participants of some sports (eg, kickboxing) and
tumours of the third ventricle. uncertainty regarding the ideal diagnostic strategy and
the optimum timing after TBI for detection of permanent
Pituitary surgery hypopituitarism.25–27
Hypopituitarism is a common consequence of pituitary Pituitary apoplexy is the abrupt destruction of pituitary
surgery. The risk and extent of hypopituitarism depends tissue, resulting from infarction or haemorrhage into the
on several factors, including the original tumour size and pituitary, usually into an underlying pituitary adenoma.
amount of tumour infiltration. The experience and Severe headache accompanies a variable amount of
volume load of the pituitary surgeon also has a substantial visual loss or cranial nerve palsies, or both. Pituitary
effect on the chance of a surgical cure for the pituitary hormone deficiencies can develop rapidly.28,29
adenoma and the mortality and morbidity associated In Sheehan’s syndrome, pituitary infarction occurs
with surgery.16,17 Prompt postoperative assessment of secondary to severe post-partum haemorrhage and
pituitary function is mandatory; however, a decrease in ensuing circulatory failure.30,31 In a normal pregnancy, the
pituitary function is not universal. Paradoxically, surgery pituitary gland can double or treble in volume; a small
for non-functioning pituitary adenomas is sometimes fall in blood pressure can precipitate pituitary infarction.
associated with substantial recovery of pituitary Aneurysmal subarachnoid haemorrhage can cause
function.12,18 hypopituitarism, but there is no agreement on the
precise incidence, clinical course, and effect on overall
Radiotherapy quality of life in long-term survivors.32–34
Hypopituitarism can occur after treatment with
conventional external beam radiotherapy if the Infiltrative
hypothalamic–pituitary axis lies within the radiation Granulomatous diseases including sarcoidosis, tuber-
fields.19 The extent of hypopituitarism and the speed of culosis, and histiocytosis X can involve the hypothalamic–
onset are dose dependent. Radiation-induced hypo- pituitary axis, and, in particular, the pituitary stalk,
pituitarism occurs in patients who receive radiotherapy causing hypopituitarism. Diabetes insipidus is a
2404 www.thelancet.com Vol 388 November 12, 2016
Seminar
common complication of neurosarcoidosis (25–33%) Genetic
and histiocytosis X.35 The development of the pituitary gland depends on the
Iron overload states, which occur in patients with sequential temporal and spatial expression of tran-
haemochromatosis36 and in those who need several blood scription factors and signalling molecules; these include
transfusions for disorders such as β thalassaemia, can the transcription factors HESX1, PROP1, POUF1, LHX3,
cause hypopituitarism. Gonadotropin secretion seems to LHX4, PITX1, OTX2, SOX2, and SOX3. Genetic
be especially affected, but other pituitary hormone mutations in any of these factors can lead to congenital
deficiencies can occur. hypopituitarism in association with a wide spectrum of
craniofacial and midline defects (table).40 Congenital
Immunological hypopituitarism can present with non-specific symptoms
Lymphocytic hypophysitis is caused by an immune- in neonates, but in some instances the full expression of
mediated diffuse infiltration of the anterior pituitary with the hypopituitarism evolves over time, with the last
lymphocytes and plasma cells. It occurs predominantly deficiency presenting in adolescence or young adult-
in women and is often first evident in pregnancy or after hood.41,42 Isolated pituitary hormone deficiency can be
delivery.37 Classic presentation is hypopituitarism in the caused by a mutation in genes involved in the
peripartum, often with a pituitary mass, visual failure, development and functional activity of that specific
and headaches. pituitary cell line.41
Increasing use of immunologically based treatments in
patients with cancer has resulted in a growing number of International variation
reports of hypophysitis.38,39 Ipilimumab is a humanised In most countries, the main cause of hypopituitarism
monoclonal antibody that blocks cytotoxic T-lymphocyte that presents in adult life is a benign pituitary tumour or
antigen 4 and enhances T-cell activation. In a large series its treatment by surgery or radiotherapy, or both. The
of patients with metastatic melanoma treated with prevalence of some of the less common causes is greater
ipilimumab, more than 10% developed hypophysitis, in countries situated in the tropics than in developed
particular risk factors being male sex and older age.38 countries,43 and not just because of very rare causes, such
Hypopituitarism only involved anterior pituitary as acute pituitary infarction caused by snakebite.44 In
function, was persistent in most patients, and was countries situated within the tropics, hypopituitarism
associated with pituitary enlargement that often resolved due to infective causes, such as pituitary abscess, HIV
rapidly.38,39 infection, and tuberculosis, is more common than in
Inheritance Types Endocrinopathies Phenotypes
GLI2 Haploinsufficiency Missense or frameshift CPHD (GH, TSH, LH, FSH, or ACTH) Holoprosencephaly, craniofacial abnormalities, polydactyly, HH, and
partial agenesis of the corpus callosum
FGF8 AR and AD Missense or chromosome deletion LH, FSH, or diabetes insipidus HH, anosmia, holoprosencephaly, Moebius syndrome, and SOD
LHX3 AR Missense, non-sense, frameshift, or CPHD (GH, TSH, LH, FSH, prolactin, or Limited neck rotation, short cervical spine, and sensorineural
splicing ACTH) deafness
LHX4 AD Missense or frameshift CPHD (GH, TSH, and ACTH) or Cerebellar abnormalities
variable gonadotropin deficiency
HESX1 AR and AD Missense or frameshift IGHD or CPHD SOD
SOX2 AD Missense, non-sense, or frameshift LH, FSH, or variable GHD Anophthalmia or microphthalmia, oesophageal atresia, genital tract
abnormalities, hypothalamic hamartoma, sensorineural hearing loss,
or diplegia
SOX3 X linked Variations in polyalanine tract IGHD or CPHD Mental retardation, infundibular hypoplasia, EPP, or midline
length, or chromosome duplication abnormalities
OTX2 AD Missense, non-sense, or IGHD or CPHD Anophthalmia or microphthalmia, coloboma, or developmental
microdeletion delay
PROP1 AR Missense, non-sense, frameshift, or CPHD (GH, TSH, LH, FSH, or prolactin) Transient anterior pituitary hyperplasia
splicing or evolving ACTH deficiency
POU1F1 AR or AD Missense, non-sense, frameshift, or CPHD (GH, TSH, or prolactin) Variable anterior pituitary hypoplasia
splicing
TBX19 AR Missense, non-sense, frameshift, or ACTH Neonatal hypoglycaemia or neonatal cholestatic jaundice
splicing
ACTH=adenocorticotropic hormone. AD=autosomal dominant. AR=autosomal recessive. CPHD=combined pituitary hormone deficit. EPP=ectopic posterior pituitary. FSH=follicle stimulating hormone.
GH=growth hormone. GHD=growth hormone deficiency. HH=hypogonadotropic hypogonadism. IGHD=isolated growth hormone deficiency. LH=luteinising hormone. SOD=septo-optic dysplasia. TSH=thyroid
stimulating hormone. Reproduced from McCabe and Dattani,40 by permission of Elsevier.
Table: Mutational characteristics of transcription factors mediating pituitary development
www.thelancet.com Vol 388 November 12, 2016 2405
Seminar
developed countries.43 Sheehan’s syndrome is more symptoms and signs depends on the order and extent of
common in countries situated in the tropics43 and in hormonal loss. The typical symptoms and signs
Turkey31 than in other developed countries because of associated with each hormonal deficiency are described
less well developed obstetric care. in the following sections that relate to hormone
measurements and dynamic testing.
Clinical presentation and diagnosis
The clinical presentation of hypopituitarism is varied and Hormone measurements and dynamic testing
depends on the nature and acuity of the damage to the Methods for hormonal measurement need to be
hypothalamic–pituitary region and the resultant order harmonised, international standards need to be used,
and amount of hormonal loss. and units of reporting need to be consistent to eliminate
the need for conversion factors.47 Binding globulins can
Acute be affected by many disorders and drugs, most
Pituitary apoplexy, acute pituitary inflammation, and commonly oral forms of oestrogen, leading to variability
Sheehan’s syndrome can all cause acute hypopituitarism, in total hormone concentrations. Measurement of
which, if untreated, have a high risk of mortality, usually concentrations of free hormone using salivary methods
secondary to loss of ACTH and subsequent hypo- and mass spectrometry has been advocated to avoid
adrenalism. This presentation is rare but crucial to these issues.48,49 Knowledge of local laboratory methods
recognise. and potential interferences is vital in the assessment of
Sudden onset of acute severe headache, usually retro- pituitary function. Robust normative data are also
orbital in nature, should alert clinicians to the possibility needed to provide meaningful reference ranges.50
of acute pituitary damage. Increased intrasellar pressure Ideally, reference ranges and cutoffs for stimulation
in the pituitary as a result of haemorrhage, infarct, or tests should be derived locally, and the suggested values
inflammation generates pain, and is also associated with provided in this Seminar need to be interpreted with
neuro-ophthalmic signs in up to 70% of patients45 These this in mind.51
symptoms and signs can constitute a surgical
emergency.45,46 Clinicians should also recognise these GHD in childhood
symptoms as suggestive of a possible association with In childhood, the most prominent feature of GHD is
acute hypopituitarism, and many patients will have reduced growth. The Growth Hormone Research Society
coincident nausea, vomiting, hypotension, and hypo- suggest a combination of convincing auxology, bio-
natraemia caused by an acute loss of ACTH and chemical assessment of the growth hormone–IGF-1 axis,
subsequent hypocortisolism. and pituitary imaging is needed for a diagnosis of GHD
Diabetes insipidus can also be a presenting feature of in children.52 Growth hormone is secreted in a pulsatile
acute pituitary damage and should be suspected if fashion and therefore a random growth hormone
polyuria and polydipsia are present. Hypocortisolism estimation is rarely helpful in excluding GHD unless the
can mask diabetes insipidus, and therefore the sample coincides with a growth hormone secretory peak.
symptoms of diabetes insipidus might not manifest Stimulation of growth hormone using, for example,
until cortisol is replaced. insulin-induced hypoglycaemia, arginine, or glucagon, is
In acute hypopituitarism, rapid replacement with the usual method of diagnosis, and diagnosis is more
hydrocortisone is crucial. Before urgent administration likely in the presence of several hormone deficiencies,
of hydrocortisone, measurements of cortisol and ACTH low serum IGF-1 concentration, and a structural lesion.
concentrations are needed to confirm the diagnosis. In In the case of isolated GHD, two dynamic tests should be
an acute setting, serum cortisol concentrations of less done to confirm a diagnosis.
than 500 nmol/L would be regarded as subnormal for
this setting. A short Synacthen test in this setting can be GHD in adulthood
falsely reassuring because adrenal atrophy would Adults with GHD have increased fat mass and reduced
probably be absent and therefore the adrenal glands muscle mass, low energy, and reduced quality of life,
would respond appropriately to ACTH.45,46 which is ideally assessed clinically and by a validated
Other pituitary hormone defects occur with acute questionnaire. Although GHD exists as a continuum of
hypopituitarism but rarely result in acute symptoms. deficiency, strict diagnostic criteria exist for severe
Measurement of insulin-like growth factor 1 (IGF-1), GHD in adults, which determines replacement
luteinising hormone and FSH, testosterone or oestradiol, strategies in many countries. Guidance from inter-
TSH, and thyroxine and prolactin are also useful for the national and national societies is largely followed.53 In
diagnosis of hypopituitarism. the presence of a known structural pituitary lesion and
several other pituitary hormone deficiencies, severe
Chronic GHD is probable. In this situation, the presence of
The onset of hypopituitarism is usually insidious, and three other pituitary hormone deficiencies and a low
the clinical presentation non-specific. The pattern of serum IGF-1 concentration is conclusive of diagnosis
2406 www.thelancet.com Vol 388 November 12, 2016
Seminar
and justifies no further testing.54 In less clear-cut ACTH deficiency
situations, dynamic pituitary function tests are Chronic ACTH deficiency causes lethargy, tiredness, and
necessary. The insulin tolerance test is the gold weight loss. However, it can be asymptomatic when only
standard55 for diagnosis in adults, although the growth partial, such as when there is sufficient ACTH to
hormone releasing hormone (GHRH)–arginine maintain cortisol concentrations for day-to-day activity
stimulation test has similar sensitivity and specificity.56 but not at times of intermittent stress or illness. Patients
Thought must be given to the choice of stimulation in with a low cortisol concentration (<80 nmol/L) at 0900 h
patients with a probable hypothalamic contribution to can be diagnosed with complete ACTH deficiency, but a
pituitary failure (eg, after irradiation), because direct stimulation test is needed to elucidate the cortisol reserve
pituitary stimulation with drugs such as GHRH can in those with intermediate cortisol results (>80 and
give a false negative diagnosis.57 Other pituitary <400 nmol/L) at 0900 h.59 The gold standard for testing
hormones must be replaced adequately before under- pituitary ACTH deficiency is the insulin tolerance
taking growth hormone stimulation tests. The insulin test. Stimulated concentrations of cortisol less than
tolerance test has many contraindications, and GHRH 500 nmol/L suggest an inability to respond adequately to
is no longer available in some countries, making other stress, and hydrocortisone replacement should be
stimulation tests necessary. Recommendations are for a considered. Insulin tolerance tests are contraindicated in
glucagon stimulation test in this situation.55 patients with ischaemic heart disease and those with
The growth hormone cutoff values for diagnosis of epilepsy.60,61
severe GHD are arbitrary. In the UK, the cutoff value for A short Synacthen test (250 μg ACTH[1–24]) is a less
growth hormone during an insulin tolerance test to labour intensive alternative to the insulin tolerance test;
diagnose severe GHD and allow growth hormone it has been validated for the detection of ACTH deficiency,
treatment under National Institute for Health and using the peak cortisol concentration.60,61 However, the
Clinical Excellence approval is less than 3 μg/L; this short Synacthen test can be less sensitive in some
concentration has been translated across all dynamic situations and can provide a false negative result,
tests in most UK centres. However, the accuracy of this including when the pituitary damage occurred less than
threshold is questionable and some recommend a cutoff 6 weeks before the test. Caution must be taken when
of less than 5 μg/L for the insulin tolerance test.55 using the short Synacthen test in patients with a history
Cutoffs for GHRH–arginine testing should be of asthma and anaphylaxis.62 Controversy exists regarding
dependent on body-mass index (BMI; 11·5 μg/L for whether to use a 30 min or 60 min cutoff for diagnosis
patients with a BMI <25 kg/m²; 8·0 μg/L if and the usefulness of the low dose, 1 μg short Synacthen
BMI is ≥25 kg/m² and <30 kg/m²; and 4·2 μg/L if BMI test.61 Other tests to detect ACTH status include the
is ≥30 kg/m²), and evidence suggests that the cutoff
should be reduced to 1 μg/L in a glucagon stimulation
test for those with an increased BMI above 25 kg/m² to Panel: Symptoms and signs suggestive of androgen deficiency in men
avoid overdiagnosis.58 More specific signs and symptoms
• Incomplete or delayed sexual development (ie, eunuchoidism)
Gonadotropin deficiency • Reduced sexual desire (ie, libido) and activity
Gonadotropin deficiency in premenopausal women • Decreased spontaneous erections
can present with menstrual irregularities, ameno- • Breast discomfort or gynaecomastia
rrhoea, or difficulty with conception. A low serum • Loss of body (axillary and pubic) hair or reduced shaving
oestradiol concentration with coincidentally low • Reduced volume (especially <5 mL; normal adult male testicular volume 15 mL) or
luteinising hormone and FSH is the diagnostic key, shrinking testes
but must be interpreted in the context of the menstrual • Inability to father children, or low or zero sperm count
cycle phase. • Height loss, low trauma fracture, or low bone mineral density
In men, hypogonadotropic hypogonadism can • Hot flushes or sweats
present with testosterone deficiency or infertility, or
both (panel). The presence of low (<10·4 nmol/L) Other less specific symptoms and signs
morning serum total testosterone concentrations with • Decreased energy, motivation, initiative, and self-confidence
non-raised gonadotropin concentrations on two • Feeling sad or blue, depressed mood, or dysthymia
occasions is needed for diagnosis.51 Total testosterone • Poor concentration and memory
measurements represent testosterone bound to sex • Sleep disturbance or increased sleepiness
hormone binding globulin and therefore if results • Mild anaemia (normochromic, normocytic, or in the female range for assay used)
are borderline, sex hormone binding globulin • Reduced muscle bulk and strength
concentrations and measurement of free or bioavailable • Increased body fat or body-mass index
testosterone should be considered.51 In adolescents, • Diminished physical or work performance
failure to progress through puberty is usually the Adapted from Bhasin and colleagues,51 by permission of Endocrine Society.
presenting symptom.
www.thelancet.com Vol 388 November 12, 2016 2407
Seminar
glucagon stimulation test, measurement of overnight Prolactin deficiency
metyrapone stimulation, and corticotropin-releasing Hypoprolactinaemia prevents adequate lactation in
hormone testing.63 women. Severe hypoprolactinaemia (serum prolactin
concentrations <100 pmol/L) is rare, but has been
TSH deficiency suggested to be a reliable marker of severe hypo-
TSH deficiency leads to central hypothyroidism. pituitarism,68 independently associated with low serum
Presenting symptoms are similar to those for primary IGF-1,69 and in that context low serum IGF-1 might be
hypothyroidism. Differences include absence of goitre associated with specific humoral immune dysfunction.70
and reduced severity of symptoms. Central hypo-
thyroidism nearly always presents alongside other ADH deficiency
pituitary hormonal deficiencies, and as a result the The classic presentation of complete central diabetes
phenotype is difficult to define.64 insipidus due to ADH deficiency is polyuria (>3 L per day)
Measurement of both serum TSH and free thyroxine and concomitant polydipsia. Providing thirst sensation is
concentrations is needed for diagnosis. Low thyroxine intact, normal serum sodium concentrations and
and low or normal TSH concentrations confirms the osmolality are maintained through increased fluid intake.
diagnosis in the absence of non-thyroidal illness.64 An initial finding of hypotonic polyuria is needed for
Reference ranges for TSH and thyroxine for healthy diagnosis. No diagnostic gold standard exists.71 A water
individuals (ie, set points) are narrower than those for deprivation test should be done in the first instance,
the general population. Many patients with deficiency although when this test was used in isolation only 70% of
who have TSH and free thyroxine concentrations that are patients were classified in the correct diagnostic
within the reference range but have substantially reduced category.72 A urine osmolality of more than 800 mOsm/kg
over time from their individual set point will probably after fluid deprivation excludes diabetes insipidus. A
not be classed as TSH deficient according to these urine osmolality of less than 300 mOsm/kg in the
criteria.65 Models of individual TSH and thyroxine indices presence of fluid deprivation and subsequent response to
might be useful in this context, but clinical usefulness arginine vasopressin (AVP) is suggestive of central
has not been validated.66,67 diabetes insipidus. The use of 3% saline stimulation and
measurement of AVP concentrations are alternative
options, but are limited by difficulties in accurate AVP
A B measurement73,74 and uncertainty regarding the normal
range for AVP in relation to plasma osmolality.72
Copeptin, the C-terminal moiety of AVP, is a stable
marker of AVP concentrations, and the combination of a
fluid deprivation test with hypertonic saline challenge
using copeptin measurements recently provided an
accurate diagnosis in 96% of patients presenting with
polyuria and polydipsia.75 Radiologically, in diabetes
insipidus the normal high-intensity posterior pituitary
signal might be absent on MRI (figure).
In symptomatic patients with a clear underlying cause
for diabetes insipidus, a therapeutic trial of desmopressin
can be warranted in lieu of clear-cut diagnostics.
C D
Diabetes insipidus in patients with altered thirst
perception is more difficult to diagnose and manage.
Adipsic diabetes insipidus is rare, but has a substantially
increased morbidity and mortality compared with
patients with diabetes insipidus with intact thirst
perception. Thirst perception must be assessed in all
patients who present with signs and symptoms of
central diabetes insipidus.77,78
Management
Included in the management of a patient with hypo-
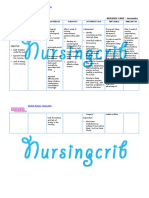
Figure: MRI of the pituitary gland pituitarism are replacement of hormone deficiencies,
(A) T1-weighted and (B) T2-weighted MRI of normal pituitary gland in sagittal planes before contrast regular screening for the development of new pituitary
administration. The high signal intensity of the posterior lobe is visible. (C) T1-weighted and (D) T2-weighted
MRI in sagittal planes before contrast administration in a 36-year-old man with central diabetes insipidus. The
hormone deficiencies, surveillance of the underlying
high signal intensity of the posterior lobe is not visible. Reproduced from Bladowska and Sąsiadek,76 under cause (usually a tumour), and monitoring and
CC BY 3.0 licence. management of other consequences of hypopituitarism,
2408 www.thelancet.com Vol 388 November 12, 2016
Seminar
such as cardiometabolic risk factors, bone health, and provides information for the patient regarding the
wellbeing of the patient. intercurrent illness regimen and information for health-
care personnel on how to manage adrenal crisis. Patients
ACTH deficiency should also have an emergency kit for self-administration
Most patients with secondary adrenal insufficiency have of parenteral hydrocortisone in case of a sudden severe
other pituitary hormone deficiencies.6,79 Replacement disease, such as gastroenteritis, when extra doses of oral
treatment for cortisol deficiency must meet the day-to-day hydrocortisone are less likely to be efficacious. Parenteral
basic maintenance needs and include rescue treatment administration is needed if the patient requires general
when patients increase their dose during physical and anaesthesia or when oral administration is not possible.
mental stress to prevent an adrenal crisis. The aim of Patients with hypopituitarism who have untreated
replacement treatment is to achieve a physiological daily severe GHD have increased local 11β-hydroxysteroid
dose for each patient and to mimic the circadian serum dehydrogenase type 1 activity in adipose tissues, resulting
cortisol profile. Hydrocortisone or cortisone acetate are in increased local cortisol exposure.91,92 Therefore, when
most commonly used for replacement treatment.80 The growth hormone replacement is started, tissue exposure
recommended mean daily dose of hydrocortisone should of cortisol is reduced; this can push some patients with
be lower than 30 mg,81 on the basis of findings from partial cortisol insufficiency into overt deficiency.93 To
studies that showed a cortisol production rate of avoid the occurrence of problems with cortisol deficiency,
15·5–19 mg/day in healthy adults82 and adverse metabolic the hydrocortisone dose might need to be increased in
risk in patients with hypopituitarism who received doses those on a low replacement dose at the start of growth
greater than 20 mg/day.83 hormone replacement.
In patients with partial cortisol insufficiency, use of ACTH deficiency also leads to androgen deficiency,
conventional doses of hydrocortisone will result in overly including dehydroepiandrosterone (DHEA) deficiency.94
high cortisol exposure.84 Clinical judgment should be Studies on DHEA replacement have been done in women
used to decide whether to start with lower than with secondary adrenal insufficiency, and findings from
conventional doses for replacement (5–10 mg/day) or to some, but not all, showed beneficial effects on wellbeing
use only rescue treatment when needed. and sexuality.95,96 DHEA replacement might also be of
Commonly used doses are hydrocortisone 10 mg in the some benefit in men.97 Addition of 20–50 mg DHEA can
morning in the fasting state together with 5 mg at 1200 h, be considered in women with hypopituitarism and low
often with an additional 5 mg later in the day (before serum concentrations of DHEA who report reduced
1800 h). This regimen attempts to simulate the normal wellbeing and libido,95 which might also reduce the need
physiological exposure to cortisol, higher in the morning for growth hormone.98 Side-effects that can occur are
and lower in the afternoon and evening. A dose increased sweating, acne, and undesired hair growth.
administered too late during the day results in higher
cortisol exposure during late evening, which might affect TSH deficiency
sleepiness and have a more adverse metabolic effect.85,86 In patients with central hypothyroidism, the extent of
New products for the treatment of adrenal insufficiency insufficiency cannot be defined as well as in patients with
have been developed and provide a more physiological primary hypothyroidism, in whom the magnitude of
cortisol profile,87–89 which might have some beneficial increase in TSH is associated with the severity of the
effects over conventional replacement treatment with insufficiency. Therefore, the starting dose and dose titration
hydrocortisone.89 should be chosen with caution in all elderly patients and
Adrenal crisis occurs when cortisol availability is those with known ischaemic heart disease. In patients with
reduced or low at a time of increased need for cortisol, hypopituitarism with central hypothyroidism, the status of
such as during a severe infection. During adrenal crisis, the hypothalamic–pituitary–adrenal axis should always be
patients develop fever, abdominal pain, nausea and assessed and cortisol insufficiency corrected before starting
vomiting, diarrhoea, reduced blood pressure, and treatment with L-thyroxine. Otherwise, overt cortisol
eventually circulatory failure, with a risk of death unless insufficiency or even adrenal crisis can occur because of
treated promptly with cortisol and saline infusion. the accelerated metabolic clearance of cortisol and
Common precipitating disorders that cause adrenal increased cortisol need as a result of an increased basal
crisis are gastroenteritis, other infections, and mental metabolic rate after thyroxine replacement.
stress.90 Therefore, to prevent adrenal crisis patients are Growth hormone replacement increases the conversion
instructed to immediately double or triple their daily of thyroxine to triiodothyronine.99 Therefore, careful
dose of hydrocortisone during an illness, whereas the monitoring of thyroid function is mandatory during
dose adjustment during a stress not related to illness, growth hormone treatment because it might uncover
such as mental stress and physical exercise, is less and central hypothyroidism or suggest the need for changes
needs to be tailored more individually to prevent excess in the dose of L-thyroxine.
cortisol exposure. All patients with hypopituitarism and Finding the appropriate L-thyroxine replacement dose
cortisol insufficiency should carry a steroid card that in central hypothyroidism is based on measurement of
www.thelancet.com Vol 388 November 12, 2016 2409
Seminar
the free thyroxine concentration before the daily intake Well-documented effects of growth hormone replacement
of L-thyroxine. Serum free thyroxine concentrations in adults include reductions in total and LDL cholesterol
should be in the upper normal range for the assay and diastolic blood pressure,113 and changes in body
used.100–103 This suggestion is supported by findings from composition, with increases in lean body mass and
two large trials104,105 of adults with hypopituitarism that reductions in fat mass, particularly abdominal
showed more prevalent cardiometabolic risk factors adiposity.113,114 Findings from randomised controlled trials
among patients with free thyroxine concentrations in have also shown improvements in quality of life,
the lower normal range and that BMI and total and LDL wellbeing, and cognitive function,115,116 although these
cholesterol improved with an increased dose of were not found in all studies.117
L-thyroxine. Findings from other prospective dose- Recombinant human growth hormone is available for
titration studies have suggested that an adult replace- daily subcutaneous injections. In adults, the treatment
ment dose of L-thyroxine should be 1·6 μg/kg per dose needs to be low initially and then titrated gradually
day,101,102,105 with a dose of 1·1–1·4 μg/kg per day in patients against serum IGF-1 concentration and clinical response
older than 60 years and 1·41–1·7 μg/kg per day in those every 2–4 weeks.118,119 Effects on wellbeing, with increased
younger than 60 years.106 energy, are usually reported after 3–12 months of
treatment and are sustained by continued treatment.120
Gonadotropin deficiency The growth hormone dose should be titrated towards a
Oral oestrogen with cyclic addition of progestin to mimic normal serum IGF-1 concentration against proper age-
the normal menstrual cycle is the most common adjusted reference values. Using a larger initial dose of
replacement regimen in women with hypopituitarism. growth hormone and undertaking dose titration too fast
Younger women need higher oestrogen doses and places patients at risk of side-effects related to fluid
women approaching the age of menopause might need a retention, such as muscle and joint stiffness and pain,
lower dose. After age 50 years (ie, the mean age of peripheral oedema, and carpal tunnel syndrome.10
menopause), oestrogen treatment is usually withdrawn. Dose adjustment of growth hormone needs to be done
Oral, by contrast with transdermal, oestrogen has in women who change their oestrogen replacement
clinically significant effects on lipid metabolism, treatment. Since oral oestrogen replacement attenuates
coagulation factors, systemic inflammation, and various the serum IGF-1 response to growth hormone, a dose
circulating binding globulins important for carrying reduction is needed when withdrawing oestrogen
hormones.107 Oral oestrogen during its first passage replacement or switching to a transdermal route of
through the liver suppresses the hepatic IGF-1 response replacement. Thyroid and adrenal function need to be
to growth hormone and might also attenuate other monitored before and after the start of growth hormone
metabolic responses to growth hormone.107 replacement because this treatment can unmask central
Ovulation and fertility can be achieved in women hypothyroidism and secondary adrenal insufficiency,
with hypopituitarism by gonadotropin treatment. The which would result in the need for dose adjustments in
outcome of such treatment in general is not known, but those receiving replacement treatment with L-thyroxine
in some patients, pregnancy and successful births have and glucocorticoid.93,99
been achieved.108,109 Adults with hypopituitarism and untreated GHD are
For men with hypopituitarism, testosterone can be insulin resistant.121,122 Growth hormone directly reduces
replaced using depot formulation for intramuscular insulin sensitivity and therefore the possibility that
injections or transdermal or oral preparations. The oral growth hormone replacement might induce diabetes
formulations are often less effective and are more likely mellitus in adults with hypopituitarism is concerning.
to induce hepatic toxicity than are other formulations Findings from two large prospective surveillance studies
that are likely to be otherwise similar in terms of safety showed either no change123 or an increase124 in the
and efficacy. Before initiation of testosterone replacement, incidence and prevalence of diabetes mellitus among
and on a regular basis during treatment, patients need to adults who underwent growth hormone replacement.
be screened for prostate cancer, polycythaemia, and Available data do not suggest an increased risk of de-novo
sleep apnoea. malignancies125 or recurrence or regrowth of pituitary
Spermatogenesis can be induced in men with hypo- tumour during long-term growth hormone replacement
pituitarism using human chorionic gonadotropin or treatment.121,126,127
recombinant FSH, or both,110 but this takes months and
in some cases 2–3 years. Small testicular volumes at the Diabetes insipidus
start of treatment is a negative predictor of success.111 Desmopressin is a modified form of the normal human
hormone AVP. For maintenance, desmopressin tablets
Growth hormone deficiency divided into two or three daily doses, or nasal preparations
In adults, the goal of growth hormone replacement is to administered one to two times daily are used. The
improve wellbeing, reduce cardiovascular risk, increase parenteral form is available for emergency use and when
bone density, and normalise body composition.112 oral or nasal administration is not possible.
2410 www.thelancet.com Vol 388 November 12, 2016
Seminar
Patients with central diabetes insipidus who are dose is gradually reduced and then discontinued around
conscious can compensate for the excess loss of free gestational week 20.108
water from the kidney by drinking more fluids. However, Data on the outcome of pregnancy in women with
in decompensated patients with increased serum sodium hypopituitarism are limited;108,109,128 however, there is no
concentrations, slow correction of serum sodium should evidence to suggest that appropriately treated hypo-
be done to avoid cerebral oedema. In patients who are pituitarism is associated with decreased frequency of
unconscious, management of diabetes insipidus needs livebirths, increased risk of malformation, or variation in
to be monitored carefully, with assessment of fluid gestational week of delivery or birthweight.
balance, serum sodium concentrations, and appropriate
replacement of AVP. Controversies, uncertainties, and future needs
The aim of replacement treatment in diabetes Pathology
insipidus is to reduce the daily urinary production of The varying sensitivity of the different anterior pituitary
free water to prevent excessive thirst, persistent hormones to pathological damage remains unexplained.
polyuria, and nocturia. Ideally, treatment with Thus, the reason why growth hormone secretion is
desmopressin should be started with a dose at bedtime adversely affected early and TSH later after pathological
to prevent nocturia. Thereafter, the most appropriate changes such as radiation or increased sellar pressure
morning and, sometimes, midday dose should be from a pituitary tumour is unknown. Equally unknown
added. The duration of antidiuresis after nasal is the explanation for why radiation-induced damage,
administration varies from 6 h to 12 h, whereas the oral primarily hypothalamic in most instances, does not
dose can have a shorter duration. Most patients need cause diabetes insipidus. Similarly, the specific
twice daily dosing, but a third oral dose might be vulnerability of gonadotropin secretion to iron deposition
needed. Patients should learn to sense signs and in the pituitary and ACTH secretion to lymphocytic
symptoms suggestive of reduced efficacy, such as hypophysitis are unexplained. Without an explanation
increased thirst and increased urinary output, and also for these findings, new hypopituitarism-avoidance
signs suggestive of overdose such as headache, fatigue strategies cannot be developed.
(caused by hyponatraemia), and low urinary output.
Biochemical monitoring consists of measurement of Treatment
serum sodium and urea concentrations. Different strategies exist for endocrine replacement in
Patients with diabetes insipidus and hypothalamic adults. In the UK, growth hormone treatment is offered
lesions that have resulted in loss of thirst sensation are at to adults with severe GHD on the basis of a single
risk of developing severe hypertonic hypernatraemia. biological endpoint: impaired quality of life. Elsewhere in
This can be managed by a constant intake of the world, growth hormone replacement is offered on
desmopressin each day and calculation of variable daily holistic grounds in the belief that it improves adverse
fluid intake to balance renal and insensible losses. Daily markers of vascular risk, reduces the risk of fractures,
weighing and frequent monitoring of serum sodium and offers metabolic benefit, and improves quality of life.129
urea is needed in these patients, in particular in the early In general, the enthusiasm of the endocrinologist for
stages of treatment. starting thyroxine and hydrocortisone replacement
diminishes for lesser amounts of TSH and ACTH
Pregnancy deficiency, whereas partial GHD does not warrant growth
Before conception, endocrine replacement treatment in hormone replacement in adults.127 Furthermore, the
women with hypopituitarism should be optimised, replacement dose (eg, thyroxine for TSH deficiency) is
including growth hormone replacement and adjustment less frequently optimised than it is when used for
of the L-thyroxine dose to obtain high normal free treatment of failure of the primary target gland.130
thyroxine concentrations. The hypothalamic–pituitary– In the future, modified-release forms of growth
adrenal axis should be assessed carefully before hormone administered about once weekly or even less
pregnancy, because this is difficult during pregnancy frequently might replace once daily preparations.
owing to the marked increase in cortisol binding globulin. Similarly, in selected patients, sustained-release forms of
During pregnancy, the L-thyroxine dose needs to be hydrocortisone might replace thrice daily conventional
increased in the first trimester and regular and careful hydrocortisone to improve quality of life through a more
clinical assessment of glucocorticoid status should be physiological cortisol profile.
done because an increase in the dose might be needed in
some women during the last trimester. In many women, Continuation of care
growth hormone treatment is discontinued when Care of patients with childhood-onset hypopituitarism,
pregnancy is confirmed, whereas in others treatment is once growth is completed, varies substantially. Attempts
continued until placental production of variant growth to offer transitional care involving shared management
hormone is clinically evident (usually around the between paediatric and adult endocrinologists have had
12th week of gestation), after which the growth hormone mixed success, depending on the health-care system of
www.thelancet.com Vol 388 November 12, 2016 2411
Seminar
the country and the local circumstances of endocrine 14 Arafah BM, Prunty D, Ybarra J, Hlavin ML, Selman WR.
practice in the vicinity of the patient. Thus, although The dominant role of increased intrasellar pressure in the
pathogenesis of hypopituitarism, hyperprolactinemia, and
guidelines are clear in their recommendations for the headaches in patients with pituitary adenomas.
management of this period in life,131 the success of the J Clin Endocrinol Metab 2000; 85: 1789–93.
integration of the adult and paediatric contributions is 15 Olsson DS, Andersson E, Bryngelsson I-L, Nilsson AG,
Johannsson G. Excess mortality and morbidity in patients with
often dependent on the beliefs and personalities of the craniopharyngioma, especially in patients with childhood onset:
local adult and paediatric endocrinologists. a population-based study in Sweden. J Clin Endocrinol Metab 2015;
100: 467–74.
Finally, the strategy for repeated assessment over the
16 Swearingen B. Update on pituitary surgery. J Clin Endocrinol Metab
long term in patients with predictable slowly evolving 2012; 97: 1073–81.
hypopituitarism also needs more thought regarding who 17 Barker FG, Klibanski A, Swearingen B. Transsphenoidal surgery for
to screen and how often, and which are the best screening pituitary tumors in the United States, 1996–2000: mortality,
morbidity, and the effects of hospital and surgeon volume.
instruments in terms of labour, cost, and endocrine yield. J Clin Endocrinol Metab 2003; 88: 4709–19.
However, in the meantime, many patients in the 18 Arafah BM, Kailani SH, Nekl KE, Gold RS, Selman WR.
community undoubtedly have untreated hypopituitarism Immediate recovery of pituitary function after transsphenoidal
resection of pituitary macroadenomas. J Clin Endocrinol Metab 1994;
and are suffering greatly because of this absence of a 79: 348–54.
process of follow-up.132 19 Darzy KH, Shalet SM. Hypopituitarism following radiotherapy
Contributors revisited. Endocr Dev 2009; 15: 1–24.
All authors contributed equally to this work. 20 Marek J, Jezková J, Hána V, et al. Is it possible to avoid
hypopituitarism after irradiation of pituitary adenomas by the
Declaration of interests Leksell gamma knife? Eur J Endocrinol 2011; 164: 169–78.
GJ has served as a consultant to Viropharma/Shire and AstraZeneca and 21 Roug S, Rasmussen AK, Juhler M, et al. Fractionated stereotactic
has received lecture fees from Merck Serono, Novartis, Novo Nordisk, radiotherapy in patients with acromegaly: an interim single-centre
Otsuka, Pfizer, and Shire. SMS has received fees for lecturing and audit. Eur J Endocrinol 2010; 162: 685–94.
ad-hoc advisory board consultancy from Pfizer, Novo Nordisk, Ipsen, 22 Schalin-Jäntti C, Valanne L, Tenhunen M, et al. Outcome of
Sandoz, Merck, and Eli Lilly. CEH declares no competing interests. fractionated stereotactic radiotherapy in patients with pituitary
adenomas resistant to conventional treatments: a 5.25-year
References follow-up study. Clin Endocrinol (Oxf) 2010; 73: 72–77.
1 Regal M, Páramo C, Sierra SM, Garcia-Mayor RV. Prevalence and
23 Xu Z, Lee Vance M, Schlesinger D, Sheehan JP.
incidence of hypopituitarism in an adult Caucasian population in
Hypopituitarism after stereotactic radiosurgery for pituitary
northwestern Spain. Clin Endocrinol (Oxf) 2001; 55: 735–40.
adenomas. Neurosurgery 2013; 72: 630–37.
2 Nilsson B, Gustavasson-Kadaka E, Bengtsson BA, Jonsson B.
24 Cohen-Inbar O, Ramesh A, Xu Z, Vance ML, Schlesinger D,
Pituitary adenomas in Sweden between 1958 and 1991: incidence,
Sheehan JP. Gamma knife radiosurgery in patients with persistent
survival, and mortality. J Clin Endocrinol Metab 2000; 85: 1420–25.
acromegaly or Cushing’s disease: long-term risk of hypopituitarism.
3 Olsson DS, Nilsson AG, Bryngelsson I-L, Trimpou P, Clin Endocrinol (Oxf) 2016; 84: 524–31.
Johannsson G, Andersson E. Excess mortality in women and young
25 Tanriverdi F, Schneider HJ, Aimaretti G, Masel BE, Casanueva FF,
adults with nonfunctioning pituitary adenoma: a Swedish
Kelestimur F. Pituitary dysfunction after traumatic brain injury:
nationwide study. J Clin Endocrinol Metab 2015; 100: 2651–58.
a clinical and pathophysiological approach. Endocr Rev 2015;
4 Raappana A, Koivukangas J, Ebeling T, Pirilä T. Incidence of 36: 305–42.
pituitary adenomas in northern Finland in 1992–2007.
26 Fernandez-Rodriguez E, Bernabeu I, Castro AI, Kelestimur F,
J Clin Endocrinol Metab 2010; 95: 4268–75.
Casanueva FF. Hypopituitarism following traumatic brain injury:
5 Tomlinson JW, Holden N, Hills RK, et al. Association between determining factors for diagnosis. Front Endocrinol (Lausanne)
premature mortality and hypopituitarism. West Midlands 2011; 2: 25.
Prospective Hypopituitary Study Group. Lancet 2001; 357: 425–31.
27 Schneider HJ, Aimaretti G, Kreitschmann-Andermahr I, Stalla G-K,
6 Sherlock M, Ayuk J, Tomlinson JW, et al. Mortality in patients with Ghigo E. Hypopituitarism. Lancet 2007; 369: 1461–70.
pituitary disease. Endocr Rev 2010; 31: 301–42.
28 Capatina C, Inder W, Karavitaki N, Wass JAH. Management of
7 Gaillard RC, Mattsson AF, Akerblad A-C, et al. Overall and endocrine disease: pituitary tumour apoplexy. Eur J Endocrinol 2015;
cause-specific mortality in GH-deficient adults on GH replacement. 172: R179–90.
Eur J Endocrinol 2012; 166: 1069–77.
29 Briet C, Salenave S, Chanson P. Pituitary apoplexy.
8 Van Bunderen CC, van Nieuwpoort IC, Arwert LI, et al. Endocrinol Metab Clin North Am 2015; 44: 199–209.
Does growth hormone replacement therapy reduce mortality in
30 Diri H, Tanriverdi F, Karaca Z, et al. Extensive investigation of
adults with growth hormone deficiency? Data from the Dutch
114 patients with Sheehan’s syndrome: a continuing disorder.
National Registry of Growth Hormone Treatment in adults.
Eur J Endocrinol 2014; 171: 311–18.
J Clin Endocrinol Metab 2011; 96: 3151–59.
31 Ramiandrasoa C, Castinetti F, Raingeard I, et al. Delayed diagnosis
9 Burman P, Mattsson AF, Johannsson G, et al. Deaths among adult
of Sheehan’s syndrome in a developed country: a retrospective
patients with hypopituitarism: hypocortisolism during acute stress,
cohort study. Eur J Endocrinol 2013; 169: 431–38.
and de novo malignant brain tumors contribute to an increased
mortality. J Clin Endocrinol Metab 2013; 98: 1466–75. 32 Khajeh L, Blijdorp K, Neggers SJ, Ribbers GM, Dippel DW,
van Kooten F. Hypopituitarism after subarachnoid haemorrhage,
10 Hartman ML, Xu R, Crowe BJ, et al. Prospective safety surveillance
do we know enough? BMC Neurol 2014; 14: 205.
of GH-deficient adults: comparison of GH-treated vs untreated
patients. J Clin Endocrinol Metab 2013; 98: 980–88. 33 Kronvall E, Valdemarsson S, Säveland H, Nilsson OG.
High prevalence of pituitary dysfunction after aneurysmal
11 Tanriverdi F, Dokmetas HS, Kebapcı N, et al. Etiology of
subarachnoid hemorrhage: a long-term prospective study using
hypopituitarism in tertiary care institutions in Turkish population:
dynamic endocrine testing. World Neurosurg 2015; 83: 574–82.
analysis of 773 patients from Pituitary Study Group database.
Endocrine 2014; 47: 198–205. 34 Hannon MJ, Behan LA, O’Brien MM, et al. Chronic
hypopituitarism is uncommon in survivors of aneurysmal
12 Nomikos P, Ladar C, Fahlbusch R, Buchfelder M. Impact of primary
subarachnoid haemorrhage. Clin Endocrinol (Oxf) 2015; 82: 115–21.
surgery on pituitary function in patients with non-functioning
pituitary adenomas—a study on 721 patients. Acta Neurochir (Wien) 35 Kaltsas GA, Powles TB, Evanson J, et al. Hypothalamo–pituitary
2004; 146: 27–35. abnormalities in adult patients with langerhans cell histiocytosis:
clinical, endocrinological, and radiological features and response to
13 Arafah BM. Reversible hypopituitarism in patients with large
treatment. J Clin Endocrinol Metab 2000; 85: 1370–76.
nonfunctioning pituitary adenomas. J Clin Endocrinol Metab 1986;
62: 1173–79.
2412 www.thelancet.com Vol 388 November 12, 2016
Seminar
36 Wilson V, Mallipedhi A, Stephens JW, Redfern RM, Price DE. 57 Darzy KH, Aimaretti G, Wieringa G, Gattamaneni HR, Ghigo E,
The causes of hypopituitarism in the absence of abnormal pituitary Shalet SM. The usefulness of the combined growth hormone
imaging. Q JM 2014; 107: 21–24. (GH)-releasing hormone and arginine stimulation test in the
37 Karaca Z, Tanriverdi F, Unluhizarci K, Kelestimur F. Pregnancy and diagnosis of radiation-induced GH deficiency is dependent on the
pituitary disorders. Eur J Endocrinol 2010; 162: 453–75. post-irradiation time interval. J Clin Endocrinol Metab 2003;
38 Faje AT, Sullivan R, Lawrence D, et al. Ipilimumab-induced 88: 95–102.
hypophysitis: a detailed longitudinal analysis in a large cohort of 58 Dichtel LE, Yuen KCJ, Bredella MA, et al. Overweight/obese adults
patients with metastatic melanoma. J Clin Endocrinol Metab 2014; with pituitary disorders require lower peak growth hormone cutoff
99: 4078–85. values on glucagon stimulation testing to avoid overdiagnosis of
39 Albarel F, Gaudy C, Castinetti F, et al. Long-term follow-up of growth hormone deficiency. J Clin Endocrinol Metab 2014;
ipilimumab-induced hypophysitis, a common adverse event of the 99: 4712–19.
anti-CTLA-4 antibody in melanoma. Eur J Endocrinol 2015; 59 Nieman LK. Dynamic evaluation of adrenal hypofunction.
172: 195–204. J Endocrinol Invest 2003; 26 (suppl 7): 74–82.
40 McCabe MJ, Dattani MT. Genetic aspects of hypothalamic and 60 Maghnie M, Uga E, Temporini F, et al. Evaluation of adrenal
pituitary gland development. Handb Clin Neurol 2014; 124: 3–15. function in patients with growth hormone deficiency and
41 Alatzoglou KS, Webb EA, Le Tissier P, Dattani MT. Isolated growth hypothalamic–pituitary disorders: comparison between insulin-
hormone deficiency (GHD) in childhood and adolescence: recent induced hypoglycemia, low-dose ACTH, standard ACTH and CRH
advances. Endocr Rev 2014; 35: 376–432. stimulation tests. Eur J Endocrinol 2005; 152: 735–41.
42 Bancalari RE, Gregory LC, McCabe MJ, Dattani MT. Pituitary gland 61 Chitale A, Musonda P, McGregor AM, Dhatariya KK. Determining
development: an update. Endocr Dev 2012; 23: 1–15. the utility of the 60 min cortisol measurement in the short
synacthen test. Clin Endocrinol (Oxf) 2013; 79: 14–19.
43 Kalra S, Dhanwal D, Khadilkar V. Hypopituitarism in the tropics.
Indian J Endocrinol Metab 2011; 15 (suppl 3): S151–53. 62 Society for Endocrinology. Position statement on the use of
synthetic ACTH (Synacthen) in patients with a history of asthma.
44 Golay V, Roychowdhary A, Dasgupta S, Pandey R. Hypopituitarism
http://www.endocrinology.org/policy/docs/11-09_syntheticACTH_
in patients with vasculotoxic snake bite envenomation related acute
in_patients_with_asthma.pdf (accessed March 12, 2016).
kidney injury: a prospective study on the prevalence and outcomes
of this complication. Pituitary 2014; 17: 125–31. 63 Crowley RK, Argese N, Tomlinson JW, Stewart PM. Central
hypoadrenalism. J Clin Endocrinol Metab 2014; 99: 4027–36.
45 Rajasekaran S, Vanderpump M, Baldeweg S, et al. UK guidelines
for the management of pituitary apoplexy. Clin Endocrinol (Oxf) 64 Persani L. Central hypothyroidism: pathogenic, diagnostic, and
2011; 74: 9–20. therapeutic challenges. J Clin Endocrinol Metab 2012; 97: 3068–78.
46 Capatina C, Inder W, Karavitaki N, Wass JA. Management of 65 Andersen S, Pedersen KM, Bruun NH, Laurberg P. Narrow
endocrine disease: pituitary tumour apoplexy. Eur J Endocrinol 2015; individual variations in serum T(4) and T(3) in normal subjects:
172: R179–90. a clue to the understanding of subclinical thyroid disease.
J Clin Endocrinol Metab 2002; 87: 1068–72.
47 Wieringa GE, Sturgeon CM, Trainer PJ. The harmonisation of
growth hormone measurements: taking the next steps. 66 Goede SL, Leow MK-S. General error analysis in the relationship
Clin Chim Acta 2014; 432: 68–71. between free thyroxine and thyrotropin and its clinical relevance.
Comput Math Methods Med 2013; 2013: 831275.
48 Monaghan PJ, Keevil BG, Stewart PM, Trainer PJ. Case for the
wider adoption of mass spectrometry-based adrenal steroid testing, 67 Jostel A, Ryder WDJ, Shalet SM. The use of thyroid function tests in
and beyond. J Clin Endocrinol Metab 2014; 99: 4434–37. the diagnosis of hypopituitarism: definition and evaluation of the
TSH Index. Clin Endocrinol (Oxf) 2009; 71: 529–34.
49 Handelsman DJ, Wartofsky L. Requirement for mass spectrometry
sex steroid assays in the Journal of Clinical Endocrinology and 68 Mukherjee A, Murray RD, Columb B, Gleeson HK, Shalet SM.
Metabolism. J Clin Endocrinol Metab 2013; 98: 3971–73. Acquired prolactin deficiency indicates severe hypopituitarism in
patients with disease of the hypothalamic–pituitary axis.
50 Bidlingmaier M, Friedrich N, Emeny RT, et al. Reference intervals
Clin Endocrinol (Oxf) 2003; 59: 743–48.
for insulin-like growth factor-1 (IGF-I) from birth to senescence:
results from a multicenter study using a new automated 69 Mukherjee A, Ryder WDJ, Jöstel A, Shalet SM. Prolactin deficiency
chemiluminescence IGF-I immunoassay conforming to recent is independently associated with reduced insulin-like growth
international recommendations. J Clin Endocrinol Metab 2014; factor I status in severely growth hormone-deficient adults.
99: 1712–21. J Clin Endocrinol Metab 2006; 91: 2520–25.
51 Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in 70 Mukherjee A, Helbert M, Davis J, Shalet S. Immune function in
men with androgen deficiency syndromes: an Endocrine Society hypopituitarism: time to reconsider? Clin Endocrinol (Oxf) 2010;
clinical practice guideline. J Clin Endocrinol Metab 2010; 73: 425–31.
95: 2536–59. 71 Fenske W, Allolio B. Current state and future perspectives in the
52 Kommunehospital A. Consensus guidelines for the diagnosis and diagnosis of diabetes insipidus: a clinical review.
treatment of growth hormone (GH) deficiency in childhood and J Clin Endocrinol Metab 2012; 97: 3426–37.
adolescence: summary statement of the GH Research Society. GH 72 Fenske W, Quinkler M, Lorenz D, et al. Copeptin in the differential
Research Society. J Clin Endocrinol Metab 2000; 85: 3990–93. diagnosis of the polydipsia-polyuria syndrome—revisiting the direct
53 Ho KKY. Consensus guidelines for the diagnosis and treatment of and indirect water deprivation tests. J Clin Endocrinol Metab 2011;
adults with GH deficiency II: a statement of the GH Research 96: 1506–15.
Society in association with the European Society for Pediatric 73 Morgenthaler NG, Struck J, Alonso C, Bergmann A. Assay for the
Endocrinology, Lawson Wilkins Society, European Society of measurement of copeptin, a stable peptide derived from the
Endocrinology, Japan Endocrine Society, and Endocrine Society of precursor of vasopressin. Clin Chem 2006; 52: 112–19.
Australia. Eur J Endocrinol 2007; 157: 695–700. 74 Robertson GL, Mahr EA, Athar S, Sinha T. Development and clinical
54 Hartman ML, Crowe BJ, Biller BMK, Ho KKY, Clemmons DR, application of a new method for the radioimmunoassay of arginine
Chipman JJ. Which patients do not require a GH stimulation test vasopressin in human plasma. J Clin Invest 1973; 52: 2340–52.
for the diagnosis of adult GH deficiency? J Clin Endocrinol Metab 75 Timper K, Fenske W, Kühn F, et al. Diagnostic accuracy of copeptin
2002; 87: 477–85. in the differential diagnosis of the polyuria-polydipsia syndrome:
55 Molitch ME, Clemmons DR, Malozowski S, Merriam GR, a prospective multicenter study. J Clin Endocrinol Metab 2015;
Vance ML. Evaluation and treatment of adult growth hormone 100: 2268–74.
deficiency: an Endocrine Society Clinical Practice Guideline. 76 Bladowska J, Sąsiadek M. Diagnostic imaging of the pituitary and
J Clin Endocrinol Metab 2011; 96: 1587–609. parasellar region. In: Rahimi-Movaghar V, ed. Pituitary adenomas.
56 Aimaretti G, Corneli G, Razzore P, et al. Comparison between Rijeka: InTech, 2012: 13–32.
insulin-induced hypoglycemia and growth hormone (GH)- 77 Cuesta M, Gupta S, Salehmohamed R, et al. Heterogenous patterns
releasing hormone + arginine as provocative tests for the diagnosis of recovery of thirst in adult patients with adipsic diabetes
of GH deficiency in adults. J Clin Endocrinol Metab 1998; insipidus. Q JM 2015; published online Sept 25. DOI: 10.1093/
83: 1615–18. qjmed/hcv175.
www.thelancet.com Vol 388 November 12, 2016 2413
Seminar
78 Eisenberg Y, Frohman LA. Adipsic diabetes insipidus: a review. 99 Jørgensen JOL, Pedersen SA, Laurberg P, Weeke J, Sakkebæk NE,
Endocr Pract 2016; 22: 76–83. Christiansen JS. Effects of growth hormone therapy on thyroid
79 Clayton PE, Shalet SM. Dose dependency of time of onset of radiation- function of growth hormone-deficient adults with and without
induced growth hormone deficiency. J Pediatr 1991; 118: 226–28. concomittant thyroxine-substituted central hypothyroidism.
80 Forss M, Batcheller G, Skrtic S, Johannsson G. Current practice of J Clin Endocrinol Metab 1989; 69: 1127–32.
glucocorticoid replacement therapy and patient-perceived health 100 Carrozza V, Csako G, Yanovski JA, et al. Levothyroxine replacement
outcomes in adrenal insufficiency—a worldwide patient survey. therapy in central hypothyroidism: a practice report.
BMC Endocr Disord 2012; 12: 8. Pharmacotherapy 1999; 19: 349–55.
81 Besser GM, Jeffcoate WJ. Endocrine and metabolic diseases. 101 Slawik M, Klawitter B, Meiser E, et al. Thyroid hormone
Adrenal diseases. Br Med J 1976; 1: 448–51. replacement for central hypothyroidism: a randomized controlled
82 Kraan GP, Dullaart RP, Pratt JJ, Wolthers BG, Drayer NM, trial comparing two doses of thyroxine (T4) with a combination of T4
De Bruin R. The daily cortisol production reinvestigated in healthy and triiodothyronine. J Clin Endocrinol Metab 2007; 92: 4115–22.
men. The serum and urinary cortisol production rates are not 102 Alexopoulou O, Beguin C, De Nayer P, Maiter D. Clinical and
significantly different. J Clin Endocrinol Metab 1998; 83: 1247–52. hormonal characteristics of central hypothyroidism at diagnosis and
83 Filipsson H, Monson JP, Koltowska-Haggstrom M, Mattsson A, during follow-up in adult patients. Eur J Endocrinol 2004; 150: 1–8.
Johannsson G. The impact of glucocorticoid replacement regimens 103 Shimon I, Cohen O, Lubetsky A, Olchovsky D. Thyrotropin
on metabolic outcome and comorbidity in hypopituitary patients. suppression by thyroid hormone replacement is correlated with
J Clin Endocrinol Metab 2006; 91: 3954–61. thyroxine level normalization in central hypothyroidism. Thyroid
84 Agha A, Liew A, Finucane F, et al. Conventional glucocorticoid 2002; 12: 823–27.
replacement overtreats adult hypopituitary patients with partial 104 Filipsson Nystrom H, Feldt-Rasmussen U, Kourides I, et al.
ACTH deficiency. Clin Endocrinol (Oxf) 2004; 60: 688–93. The metabolic consequences of thyroxine replacement in adult
85 Lamia KA, Papp SJ, Yu RT, et al. Cryptochromes mediate rhythmic hypopituitary patients. Pituitary 2012; 15: 495–504.
repression of the glucocorticoid receptor. Nature 2011; 480: 552–56. 105 Klose M, Marina D, Hartoft-Nielsen M-L, et al. Central
86 Plat L, Leproult R, L’Hermite-Baleriaux M, et al. Metabolic effects of hypothyroidism and its replacement have a significant influence on
short-term elevations of plasma cortisol are more pronounced in cardiovascular risk factors in adult hypopituitary patients.
the evening than in the morning. J Clin Endocrinol Metab 1999; J Clin Endocrinol Metab 2013; 98: 3802–10.
84: 3082–92. 106 Ferretti E, Persani L, Jaffrain-Rea ML, Giambona S, Tamburrano G,
87 Whitaker MJ, Debono M, Huatan H, Merke DP, Arlt W, Ross RJ. Beck-Peccoz P. Evaluation of the adequacy of levothyroxine
An oral multiparticulate, modified-release, hydrocortisone replacement therapy in patients with central hypothyroidism.
replacement therapy that provides physiological cortisol exposure. J Clin Endocrinol Metab 1999; 84: 924–29.
Clin Endocrinol 2014; 80: 554–61. 107 Leung KC, Johannsson G, Leong GM, Ho KK. Estrogen regulation
88 Oksnes M, Bjornsdottir S, Isaksson M, et al. of growth hormone action. Endocr Rev 2004; 25: 693–721.
Continuous subcutaneous hydrocortisone infusion versus oral 108 Wiren L, Boguszewski CL, Johannsson G. Growth hormone (GH)
hydrocortisone replacement for treatment of Addison’s disease: a replacement therapy in GH-deficient women during pregnancy.
randomized clinical trial. J Clin Endocrinol Metab 2014; 99: 1665–74. Clin Endocrinol (Oxf) 2002; 57: 235–39.
89 Johannsson G, Nilsson AG, Bergthorsdottir R, et al. Improved 109 Vila G, Akerblad AC, Mattsson AF, et al. Pregnancy outcomes in
cortisol exposure–time profile and outcome in patients with adrenal women with growth hormone deficiency. Fertil Steril 2015;
insufficiency: a prospective randomized trial of a novel 104: 1210–17.
hydrocortisone dual-release formulation. J Clin Endocrinol Metab 110 Depenbusch M, von Eckardstein S, Simoni M, Nieschlag E.
2012; 97: 473–81. Maintenance of spermatogenesis in hypogonadotropic hypogonadal
90 Hahner S, Spinnler C, Fassnacht M, et al. High incidence of men with human chorionic gonadotropin alone. Eur J Endocrinol
adrenal crisis in educated patients with chronic adrenal 2002; 147: 617–24.
insufficiency: a prospective study. J Clin Endocrinol Metab 2015; 111 Liu PY, Baker HW, Jayadev V, Zacharin M, Conway AJ,
100: 407–16. Handelsman DJ. Induction of spermatogenesis and fertility during
91 Swords FM, Carroll PV, Kisalu J, Wood PJ, Taylor NF, Monson JP. gonadotropin treatment of gonadotropin-deficient infertile men:
The effects of growth hormone deficiency and replacement on predictors of fertility outcome. J Clin Endocrinol Metab 2009;
glucocorticoid exposure in hypopituitary patients on cortisone 94: 801–08.
acetate and hydrocortisone replacement. Clin Endocrinol (Oxf) 112 Drake WM, Howell SJ, Monson JP, Shalet SM. Optimizing GH
2003; 59: 613–20. therapy in adults and children. Endocr Rev 2001; 22: 425–50.
92 Weaver JU, Thaventhiran L, Noonan K, et al. The effect of growth 113 Maison P, Griffin S, Nicoue-Beglah M, Haddad N, Balkau B,
hormone replacement on cortisol metabolism and glucocorticoid Chanson P. Impact of growth hormone (GH) treatment on
sensitivity in hypopituitary adults. Clin Endocrinol (Oxf) 1994; cardiovascular risk factors in GH-deficient adults: a meta analysis of
41: 639–48. blinded, randomized, placebo-controlled trials.
93 Giavoli C, Libe R, Corbetta S, et al. Effect of recombinant J Clin Endocrinol Metab 2004; 89: 2192–99.
human growth hormone (GH) replacement on the 114 Bengtsson BA, Eden S, Lonn L, et al. Treatment of adults with
hypothalamic–pituitary–adrenal axis in adult GH-deficient patients. growth hormone (GH) deficiency with recombinant human GH.
J Clin Endocrinol Metab 2004; 89: 5397–401. J Clin Endocrinol Metab 1993; 76: 309–17.
94 Miller KK, Sesmilo G, Schiller A, Schoenfeld D, Burton S, 115 Burman P, Broman JE, Hetta J, et al. Quality of life in adults with
Klibanski A. Androgen deficiency in women with hypopituitarism. growth hormone (GH) deficiency: response to treatment with
J Clin Endocrinol Metab 2001; 86: 561–67. recombinant human GH in a placebo-controlled 21-month trial.
95 Arlt W, Callies F, van Vlijmen JC, et al. Dehydroepiandrosterone J Clin Endocrinol Metab 1995; 80: 3585–90.
replacement in women with adrenal insufficiency. N Engl J Med 116 Arwert LI, Veltman DJ, Deijen JB, van Dam PS, Drent ML.
1999; 341: 1013–20. Effects of growth hormone substitution therapy on cognitive
96 Johannsson G, Sverrisdottir YB, Ellegard L, Lundberg PA, functioning in growth hormone deficient patients: a functional MRI
Herlitz H. GH increases extracellular volume by stimulating study. Neuroendocrinology 2006; 83: 12–19.
sodium reabsorption in the distal nephron and preventing pressure 117 Baum HB, Katznelson L, Sherman JC, et al. Effects of physiological
natriuresis. J Clin Endocrinol Metab 2002; 87: 1743–49. growth hormone (GH) therapy on cognition and quality of life in
97 Brooke AM, Kalingag LA, Miraki-Moud F, et al. patients with adult-onset GH deficiency. J Clin Endocrinol Metab
Dehydroepiandrosterone improves psychological well-being in male 1998; 83: 3184–89.
and female hypopituitary patients on maintenance growth hormone 118 Drake WM, Coyte D, Camacho-Hübner C, et al. Opimizing growth
replacement. J Clin Endocrinol Metab 2006; 91: 3773–79. hormone replacement therapy by dose titration in hypopituitary
98 Brooke AM, Kalingag LA, Miraki-Moud F, et al. adults. J Clin Endocrinol Metab 1998; 83: 3913–19.
Dehydroepiandrosterone (DHEA) replacement reduces growth 119 Johannsson G, Rosen T, Bengtsson BA. Individualized dose
hormone (GH) dose requirement in female hypopituitary patients titration of growth hormone (GH) during GH replacement in
on GH replacement. Clin Endocrinol (Oxf) 2006; 65: 673–80. hypopituitary adults. Clin Endocrinol (Oxf) 1997; 47: 571–81.
2414 www.thelancet.com Vol 388 November 12, 2016
Seminar
120 Wiren L, Bengtsson BA, Johannsson G. Beneficial effects of 127 Olsson DS, Buchfelder M, Wiendieck K, et al. Tumour recurrence
long-term GH replacement therapy on quality of life in adults with and enlargement in patients with craniopharyngioma with and
GH deficiency. Clin Endocrinol 1998; 48: 613–20. without GH replacement therapy during more than 10 years of
121 Stochholm K, Johannsson G. Reviewing the safety of GH follow-up. Eur J Endocrinol 2012; 166: 1061–68.
replacement therapy in adults. Growth Horm IGF Res 2015; 25: 149–57. 128 Curran AJ, Peacey SR, Shalet SM. Is maternal growth hormone
122 Johansson J-O, Fowelin J, Landin K, Lager I, Bengtsson B-Å. essential for a normal pregnancy? Eur J Endocrinol 1998; 139: 54–58.
Growth hormone-deficient adults are insulin-resistant. Metabolism 129 Shalet SM. Extensive expertise in endocrinology: UK stance on
1995; 44: 1126–29. adult GH replacement: the economist vs the endocrinologist.
123 Attanasio AF, Jung H, Mo D, et al. Prevalence and incidence of Eur J Endocrinol 2013; 169: R81–87.
diabetes mellitus in adult patients on growth hormone replacement 130 Koulouri O, Auldin MA, Agarwal R, et al. Diagnosis and treatment
for growth hormone deficiency: a surveillance database analysis. of hypothyroidism in TSH deficiency compared to primary thyroid
J Clin Endocrinol Metab 2011; 96: 2255–61. disease: pituitary patients are at risk of under-replacement with
124 Luger A, Mattsson AF, Koltowska-Haggstrom M, et al. Incidence of levothyroxine. Clin Endocrinol (Oxf) 2011; 74: 744–49.
diabetes mellitus and evolution of glucose parameters in growth 131 Clayton PE, Cuneo RC, Juul A, Monson JP, Shalet SM, Tauber M.
hormone-deficient subjects during growth hormone replacement Consensus statement on the management of the GH-treated
therapy: a long-term observational study. Diabetes Care 2012; adolescent in the transition to adult care. Eur J Endocrinol 2005;
35: 57–62. 152: 165–70.
125 Child CJ, Zimmermann AG, Woodmansee WW, et al. 132 Chemaitilly W, Li Z, Huang S, et al. Anterior hypopituitarism in
Assessment of primary cancers in GH-treated adult hypopituitary adult survivors of childhood cancers treated with cranial
patients: an analysis from the Hypopituitary Control and radiotherapy: a report from the St Jude Lifetime Cohort study.
Complications Study. Eur J Endocrinol 2011; 165: 217–23. J Clin Oncol 2015; 33: 492–500.
126 Olsson DS, Buchfelder M, Schlaffer S, et al. Comparing progression
of non-functioning pituitary adenomas in hypopituitarism patients
with and without long-term GH replacement therapy.
Eur J Endocrinol 2009; 161: 663–69.
www.thelancet.com Vol 388 November 12, 2016 2415
You might also like
- Project 1: Protinex: Market Opportunity Analysis Segmenting, Positioning and BrandingDocument6 pagesProject 1: Protinex: Market Opportunity Analysis Segmenting, Positioning and BrandingSwetaParija57% (7)
- Nursing Care Plan For Insomnia NCPDocument2 pagesNursing Care Plan For Insomnia NCPderic83% (24)
- Soap Notes - CroupDocument9 pagesSoap Notes - Croupkenata100% (1)
- Muscle Structure and FunctionsDocument59 pagesMuscle Structure and FunctionsThopu Umamaheswari100% (1)
- Pituitary Tumors: A Clinical CasebookFrom EverandPituitary Tumors: A Clinical CasebookLisa B. NachtigallNo ratings yet
- COVID 19 The Great Reset Klaus SchwabDocument213 pagesCOVID 19 The Great Reset Klaus SchwabКирилл Павлов75% (8)
- NeoCryl B-725 MsdsDocument3 pagesNeoCryl B-725 MsdsLeandro EsvizaNo ratings yet
- Serum Testosterone Levels in Male Hypogonadism - Why and When To Check-A Review 2017Document9 pagesSerum Testosterone Levels in Male Hypogonadism - Why and When To Check-A Review 2017Sara Velásquez JNo ratings yet
- 32 Saha EtalDocument3 pages32 Saha EtaleditorijmrhsNo ratings yet
- New Directions in The Treatment of HypoparathyroidismDocument6 pagesNew Directions in The Treatment of Hypoparathyroidismmiguel saba sabaNo ratings yet
- Turkish Journal Subclinical HypothyroidismDocument5 pagesTurkish Journal Subclinical HypothyroidismAminaNo ratings yet
- ART HtaDocument26 pagesART HtaClaudia IrimieNo ratings yet
- Pituitary Incidentalomas Best Practices and Looking AheadDocument9 pagesPituitary Incidentalomas Best Practices and Looking AheadJulieta LopezNo ratings yet
- Seminar Hypothyroidism - 2017 - Chaker Et AlDocument13 pagesSeminar Hypothyroidism - 2017 - Chaker Et AlIvan CardenasNo ratings yet
- Endokrin4 PDFDocument6 pagesEndokrin4 PDFAdelina Wahyuni LubisNo ratings yet
- International Journal of Pathology and Clinical Research Ijpcr 4 070Document3 pagesInternational Journal of Pathology and Clinical Research Ijpcr 4 070Psyryst AlladoNo ratings yet
- Cushing's Syndrome (Lancet)Document16 pagesCushing's Syndrome (Lancet)Irma OnofreNo ratings yet
- Hipofisis 3Document23 pagesHipofisis 3RafaelPetitNo ratings yet
- Aldrich2021 Article ComparisonOfHypothyroidismGrowDocument8 pagesAldrich2021 Article ComparisonOfHypothyroidismGrowMona ElsaudiNo ratings yet
- Newell Price2006Document13 pagesNewell Price2006fkia2013No ratings yet
- Pituitary Apoplexy Pathophysiology Diagnosis and MDocument6 pagesPituitary Apoplexy Pathophysiology Diagnosis and MlathifatulNo ratings yet
- Acromegaly PRIMERDocument17 pagesAcromegaly PRIMERtaagrettaaNo ratings yet
- NIH Public AccessDocument13 pagesNIH Public AccessYenifer Quispe PalominoNo ratings yet
- HipopituitarismoDocument34 pagesHipopituitarismoPaola De La CruzNo ratings yet
- Hormonal Therapies in Septic Shock: Review ArticleDocument8 pagesHormonal Therapies in Septic Shock: Review ArticleJhon3xNo ratings yet
- Nota 2Document8 pagesNota 2Hector GuzmanNo ratings yet
- Evaluation and Treatment of Women With HirsutismDocument8 pagesEvaluation and Treatment of Women With HirsutismDewi Puji AstutikNo ratings yet
- Unexpected Immunohistochemical Surprise of A Cushings Disease Macroadenoma Co-Expressing Acth and Prolactin: A Case ReportDocument5 pagesUnexpected Immunohistochemical Surprise of A Cushings Disease Macroadenoma Co-Expressing Acth and Prolactin: A Case ReportIJAR JOURNALNo ratings yet
- 2018 PHP ConsensusDocument25 pages2018 PHP ConsensusBianca ChiriacNo ratings yet
- Syaraf InterDocument7 pagesSyaraf Intersatria utamaNo ratings yet
- Sheehan Syndrom L. HaddockDocument9 pagesSheehan Syndrom L. Haddockfreddyop72No ratings yet
- A Clinical Case of A Primary Partial Empty Sella Presenting With Hypogonadotropic HypogonadismDocument4 pagesA Clinical Case of A Primary Partial Empty Sella Presenting With Hypogonadotropic HypogonadismIJAR JOURNALNo ratings yet
- Review: Maria Fleseriu, Fabienne Langlois, Dawn Shao Ting Lim, Elena V Varlamov, Shlomo MelmedDocument23 pagesReview: Maria Fleseriu, Fabienne Langlois, Dawn Shao Ting Lim, Elena V Varlamov, Shlomo MelmedAaron PeñaNo ratings yet
- 10.1515@jpem 2019 0075Document8 pages10.1515@jpem 2019 0075Ahmed BaghdadiNo ratings yet
- Iatrogenic Severe Hyperglycemia Due To Parenteral Administration of Glucose in Children - A Case Series PDFDocument7 pagesIatrogenic Severe Hyperglycemia Due To Parenteral Administration of Glucose in Children - A Case Series PDFSultan Rahmat SeptianNo ratings yet
- Jurnal 1 (2020)Document10 pagesJurnal 1 (2020)Inryuu ZenNo ratings yet
- Clinicopathological Correlates of HyperparathyroidismDocument18 pagesClinicopathological Correlates of HyperparathyroidismmaryNo ratings yet
- A Literature Review On Hypertensive Crisis: European Journal of Pharmaceutical and Medical ResearchDocument6 pagesA Literature Review On Hypertensive Crisis: European Journal of Pharmaceutical and Medical ResearchCindy MaslagNo ratings yet
- Meng Reli 2010Document8 pagesMeng Reli 2010abbhyasa5206No ratings yet
- Therapeutic Hypothermia in Children After Cardiac Arrest: Eview RticleDocument8 pagesTherapeutic Hypothermia in Children After Cardiac Arrest: Eview RticleIRINA SULEY TIRADO PEREZNo ratings yet
- Hulley 1998Document9 pagesHulley 1998junta.propietarios.1456No ratings yet
- Influence of Transfusions, Hemodialysis and Extracorporeal Life Support On Hyperferritinemia in Critically Ill PatientsDocument12 pagesInfluence of Transfusions, Hemodialysis and Extracorporeal Life Support On Hyperferritinemia in Critically Ill PatientsAmalNo ratings yet
- Macroprolactinemia Revisited A Study On 106 Patients JcemDocument8 pagesMacroprolactinemia Revisited A Study On 106 Patients JcemPaulo Eduardo CampanaNo ratings yet
- Management of Cushing Syndrome in Children and Adolescents Experience of A Single Tertiary CentreDocument10 pagesManagement of Cushing Syndrome in Children and Adolescents Experience of A Single Tertiary CentreTriratna FauziahNo ratings yet
- European Journal of Internal Medicine: Alon Grossman, Ilan Feldhamer, Joseph MeyerovitchDocument4 pagesEuropean Journal of Internal Medicine: Alon Grossman, Ilan Feldhamer, Joseph MeyerovitchlintangsrNo ratings yet
- Cardiovascular Manifestations in Hyperthyroidism: Research ArticleDocument7 pagesCardiovascular Manifestations in Hyperthyroidism: Research Articlenurharyanti darmaningtyasNo ratings yet
- Hypothyroidism and Atherosclerosis: Anne R. Cappola Paul W. LadensonDocument7 pagesHypothyroidism and Atherosclerosis: Anne R. Cappola Paul W. LadensonLock ThecodeNo ratings yet
- Delayed Onset of Hypopituitarism: Sequelae of Therapeutic Irradiation of Central Nervous System, Eye, and Middle Ear TumorsDocument7 pagesDelayed Onset of Hypopituitarism: Sequelae of Therapeutic Irradiation of Central Nervous System, Eye, and Middle Ear TumorsJade LoberianoNo ratings yet
- Thyroid Function and The Metabolic Syndrome in Older Persons: A Population-Based StudyDocument7 pagesThyroid Function and The Metabolic Syndrome in Older Persons: A Population-Based StudyAlifia RahmaNo ratings yet
- Thyroid Hormone Therapy For Older Adults With Subclinical HypothyroidismDocument11 pagesThyroid Hormone Therapy For Older Adults With Subclinical HypothyroidismAssifa RidzkiNo ratings yet
- LevothyroxineDocument12 pagesLevothyroxineYara Olalde CancinoNo ratings yet
- Pe 08044Document4 pagesPe 08044Ro KohnNo ratings yet
- Subclinical Hypothyroidism in Children With Down Syndrome: To Treat or Not To Treat???Document2 pagesSubclinical Hypothyroidism in Children With Down Syndrome: To Treat or Not To Treat???adkhiatul muslihatinNo ratings yet
- Depression The Homocysteine Hypothesis of DepressionDocument7 pagesDepression The Homocysteine Hypothesis of Depressionpb41No ratings yet
- 0120 2448 Amc 44 03 8Document8 pages0120 2448 Amc 44 03 8Lejla HusicNo ratings yet
- Ejhs2901 0887Document8 pagesEjhs2901 0887Syawal DragonballNo ratings yet
- Transient Ischemic Stroke Due To Hyperhomocysteinemia: A Rare Case ReportDocument2 pagesTransient Ischemic Stroke Due To Hyperhomocysteinemia: A Rare Case ReportInt Journal of Recent Surgical and Medical SciNo ratings yet
- Primary HyperparathyroidismDocument9 pagesPrimary HyperparathyroidismJamesNo ratings yet
- Nejmoa1603825 PDFDocument11 pagesNejmoa1603825 PDFPsikiatri KlenderNo ratings yet
- Polycystic Ovary SyndromeDocument11 pagesPolycystic Ovary SyndromeViridiana Briseño GarcíaNo ratings yet
- IndianJEndocrMetab177184-6475539 175915Document4 pagesIndianJEndocrMetab177184-6475539 175915Atika SugiartoNo ratings yet
- Polycystic Ovary Syndrome 2016 NEJMDocument11 pagesPolycystic Ovary Syndrome 2016 NEJMGabrielaNo ratings yet
- Sub Clinical Thyroid DiseaseDocument6 pagesSub Clinical Thyroid DiseaseYeon Ae NaritaNo ratings yet
- Arterial HypertensionDocument13 pagesArterial HypertensionZedodurex100% (1)
- Acromegaly Pathogenesis, Diagnosis, and ManagementDocument23 pagesAcromegaly Pathogenesis, Diagnosis, and ManagementPaolo MessinaNo ratings yet
- Testosterone: From Basic to Clinical AspectsFrom EverandTestosterone: From Basic to Clinical AspectsAlexandre HohlNo ratings yet
- Cromolyn Sodium Oral InhalationDocument2 pagesCromolyn Sodium Oral InhalationDeslita AjjahNo ratings yet
- Strengths For A Successful PracticumDocument3 pagesStrengths For A Successful PracticumRamon Chito S. PudelananNo ratings yet
- Nutrition Across The LifespanDocument25 pagesNutrition Across The Lifespaneinjjereu xxiNo ratings yet
- Peh 12 1ST Sem-1st Quarter ReviewerDocument15 pagesPeh 12 1ST Sem-1st Quarter ReviewerRalph Louis RosarioNo ratings yet
- Profile of Neil J. GajjarDocument247 pagesProfile of Neil J. GajjarNeil J. GajjarNo ratings yet
- Diagnosis Appraisal TipsDocument2 pagesDiagnosis Appraisal TipsSebastian SmytheNo ratings yet
- Evening Study Schedule Template Printable by Reverelia Nov21Document3 pagesEvening Study Schedule Template Printable by Reverelia Nov21Kiyah WiseNo ratings yet
- The Insider Guide To Invisalign TreatmentDocument293 pagesThe Insider Guide To Invisalign TreatmentSmit PatelNo ratings yet
- Chocoflan Cake (Impossible Cake) - Foxy FolksyDocument2 pagesChocoflan Cake (Impossible Cake) - Foxy Folksymishima.mqNo ratings yet
- Unit 4 Managing An Event LA - ADocument82 pagesUnit 4 Managing An Event LA - AMomo AbdulrasaqNo ratings yet
- OsteoDocument2 pagesOsteoJanelle MatamorosaNo ratings yet
- Ipsos Views Humanizing AI - 0Document9 pagesIpsos Views Humanizing AI - 0farzanaisadeborderNo ratings yet
- NCM 41118L Final Quiz 3Document13 pagesNCM 41118L Final Quiz 3Matelyn OargaNo ratings yet
- Kitten DevelopmentDocument6 pagesKitten DevelopmentKoren ShawNo ratings yet
- Occupational Therapy in Driving and Community Mobility: Position StatementDocument2 pagesOccupational Therapy in Driving and Community Mobility: Position StatementskinNo ratings yet
- Chakra 7Document10 pagesChakra 7amitgaursNo ratings yet
- Case-Study-PRD Test-KM Intern Associate Product OwnerDocument6 pagesCase-Study-PRD Test-KM Intern Associate Product OwnerDina MayaNo ratings yet
- Triticale Flours: Composition, Properties and Utilization: Alberto Edel León Gabriela T. Pérez Pablo D. RibottaDocument8 pagesTriticale Flours: Composition, Properties and Utilization: Alberto Edel León Gabriela T. Pérez Pablo D. RibottaMădălina ȘtefanNo ratings yet
- Chapter OneDocument29 pagesChapter OneAbebe ChekolNo ratings yet
- The Effect of Uterine Closure Technique On Cesarean Scar Niche Development After Multiple Cesarean DeliveriesDocument8 pagesThe Effect of Uterine Closure Technique On Cesarean Scar Niche Development After Multiple Cesarean DeliveriesWillans Eduardo Rosha HumerezNo ratings yet
- Middle and Late Adulthood StageDocument2 pagesMiddle and Late Adulthood StageSATOR DOMINICNo ratings yet
- TON Flyer 16th and 17th JulyDocument3 pagesTON Flyer 16th and 17th JulyManisha ThakurNo ratings yet
- Introduction ClinicalDocument4 pagesIntroduction ClinicaljzariziNo ratings yet
- User Manual: Our Family, Innovating Health, For YoursDocument16 pagesUser Manual: Our Family, Innovating Health, For YoursKelyNo ratings yet