Professional Documents
Culture Documents
A Comparative Study of Different Doses of Ephedrine On Intubating Conditions and Hemodynamics Using Propofol and Low Dos
Uploaded by
nadaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Comparative Study of Different Doses of Ephedrine On Intubating Conditions and Hemodynamics Using Propofol and Low Dos
Uploaded by
nadaCopyright:
Available Formats
esia & Cli
sth n
Journal of Anesthesia & Clinical Sharma et al., J Anesth Clin Res 2019, 10:11
urn f Ane
ica
l Research
al o
Research
Jo
ISSN: 2155-6148
Research Article Open Access
A Comparative Study of Different Doses of Ephedrine on Intubating
Conditions and Hemodynamics Using Propofol and Low Dose
Rocuronium
Manju Sharma*, Anju Jamwal, Anjali Mehta and Ruchika Jyoti
Department of Anesthesiology and Critical Care, Government Medical Collage, Jammu, India
*Corresponding author: Dr Manju Sharma, Department of Anesthesiology and Critical Care, Government Medical Collage, Jammu, India, Tel: +917006241526; E-mail:
drmanjusharma7@gmail.com
Received date: October 29, 2019; Accepted date: November 11, 2019; Published date: November 18, 2019
Copyright: © 2019 Sharma M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,
distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Succinylcholine as muscle relaxant is a norm in emergency department even though it is
associated with a multitude of adverse effects. We used low dose rocuronium with ephedrine so as to shorten the
onset of rocuronium in accordance with RSI without prolonging the duration as seen with the usual dose used for
RSI. Increase in cardiac output caused by Ephedrine can reduce the onset time of Rocuronium. Hypotension
associated with bolus dose of Propofol can also be prevented by Ephedrine. Appropriate dose of Ephedrine is
advised to achieve the aforementioned benefits without undue side effects such as hypertension and tachycardia.
Because of variation in doses and side effects of Ephedrine in various studies, we compared the influence of
Ephedrine 30, 70 and 110 mcg/kg on intubating conditions and hemodynamics using Propofol and low dose
Rocuronium
Methods: 90 patients of either sex, ranging from 18-50 years belonging to ASA grade 1 and 2 undergoing
elective surgeries under general anesthesia were taken up for study. Patients were randomly allocated to one of the
three groups of 30 patients each.
Group 1: Rocuronium 0.6 mg/kg and Ephedrine 30 mcg/kg
Group 2: Rocuronium 0.6 mg/kg and Ephedrine 70 mcg/kg
Group 3: Rocuronium 0.6 mg/kg and Ephedrine 110 mcg/kg
Results: It was found that intubating conditions were most favorable in group 2 followed by group 3 and least
favorable in group 1. Group 3 was associated with adverse hemodynamic effects such as tachycardia and increased
blood pressure. Such effects being least in group 1 and intermediate in group 2.
Conclusion: Ephedrine pre-treatment in the dose of 70 mcg/kg with similar doses of Rocuronium and Propofol
provides ideal intubating conditions with acceptable hemodynamic changes. So, the combination of Propofol 2.5
mg/kg, Rocuronium 0.6 mg/kg and ephedrine 70 mcg/kg may be of value when use of Succinylcholine is
contraindicated for RSI.
Keywords: Hemoglobin; Intravenous; Propofol; Rocuronium; Introduction
Succinylcholine
Rapid sequence intubation is almost a norm in emergency
departments where full stomach patients are commonly encountered.
Abbreviations: I/V: Intravenous; Mg: Milligram; Mcg: Microgram; Succinylcholine is the most common neuromuscular blocking agent
Kg: Kilogram; Inj.: Injection; ASA: American Society of used owing to its short onset as well as duration. Though
Anesthesiologist; GMC: Government Medical College; MPG: Mallam succinylcholine is the most favored neuromuscular blocking agent for
Patti Grade; BMI: Body Mass Index; BP: Blood Pressure; HR: Heart rapid sequence intubation, its use is not without several adverse
Rate; HB: Hemoglobin; BT: Bleeding Time; CT: Clotting Time; TLC: reactions ranging from myalgia to hyperkalemia, masseter spasm and
Total Lymphocyte Count; DLC: Differential Lymphocyte Count; RFT: even death. To avoid these adverse reactions, non-depolarizing muscle
Renal Function Test; RSI: Rapid Sequence Induction; LFT: Liver relaxants have come in favor.
Function Test; R/E: Routine Examination; ECG: Electrocardiogram;
SPO2: Saturation of Oxygen; ETCO2: End Tidal Carbon dioxide. Rocuronium in appropriate doses has a speed of onset only
marginally slower than that of Succinylcholine. It has an intermediate
duration of action and depends on the kidney and liver for
elimination. Rocuronium by the virtue of its low potency and thereby a
J Anesth Clin Res, an open access journal Volume 10 • Issue 11 • 1000920
ISSN: 2155-6148
Citation: Sharma M, Jamwal A, Mehta A, Jyoti R (2019) A Comparative Study of Different Doses of Ephedrine on Intubating Conditions and
Hemodynamics Using Propofol and Low Dose Rocuronium. J Anesth Clin Res 10: 920.
Page 2 of 5
rapid onset of action may be used in place of Succinylcholine. 90 patients of either sex, ranging in age from 18-50 years belonging
However, the onset of Rocuronium is dose dependent and duration of to ASA grade 1 and 2 undergoing elective surgeries under general
action is longer as compared to Succinylcholine which limits its use in anesthesia were taken up for study. Patients were randomly allocated to
Rapid Sequence Induction. one of the three groups of 30 patients each.
Most of the general anesthetic procedures require laryngoscopy and Group 1: Patient received Rocuronium 0.6 mg/kg and Ephedrine 30
endotracheal intubation. Risk of hypoxia and pulmonary aspiration is mcg/kg
highest in the period ranging from loss of consciousness to tracheal
Group 2: Patient received Rocuronium 0.6 mg/kg and Ephedrine 70
intubation. Therefore, it becomes important to use a neuromuscular
mcg/kg
blocking agent with short onset so as to prevent life threatening
hypoxia or aspiration. Group 3: Patient received Rocuronium 0.6 mg/kg and Ephedrine
110 mcg/kg
The onset time of Rocuronium depends on the rate at which a
pharmacologically effective concentration is achieved in the Bio phase
that is the neuromuscular cleft. In turn, this rate is influenced by Exclusion criteria
certain factors, such as the potency of the drug, the dose administered • Patient refusal to participate in the study.
and the cardiovascular status namely cardiac output and muscle blood • Hypersensitivity to study drugs.
flow. Moreover, the onset time of drugs with rapid onset such as • Haemodynamically unstable patient.
Rocuronium, chiefly depends on the circulation time to the muscle [1]. • Any cardiovascular or neuromuscular disease.
• Intake of drugs known to interact with neuromuscular junction or
It has been reported that Rocuronium is only comparable to Ephedrine such as Aminoglycosides, Tetracyclins, Bacitracin,
Succinylcholine during Rapid Sequence Induction and Intubation in a Polymyxin B, Colistin, Sodium Colistimethate, MAO inhibitors and
dose of 0.9-1.2 mg/kg body weight, but a dose of 0.9-1.2 mg/kg lead to Tri Cyclic antidepressants.
increased duration of action up to 50-60 minutes [2]. Rocuronium in a • Anticipated difficult airway (MPG grade 3 or 4).
dose of 0.6 mg/kg produced moving vocal cords on direct • Cormack Lehane grade 3 or 4 on direct laryngoscopy.
laryngoscopy and diaphragmatic response to intubation in 20%-25% of • Patients on chronic preoperative Beta-Adrenergic Blocker treatment.
patients [3]. • Pregnancy
Ephedrine is an indirect acting sympathomimetic agent that • Obesity (BMI>30 Kg/m)
stimulates both alpha and beta receptors, and hence increases systolic • History of long term Diuretic or vasoactive medication.
blood pressure, diastolic blood pressure, heart rate, cardiac output and • 30% or more increase in BP or HR above baseline during procedure
venous return. Intravenous Ephedrine is used for hypotension were excluded from the study.
associated with regional anesthesia in a dosage of 2.5-10 mg I/v stat.
Ephedrine by increasing the cardiac output and tissue perfusion could Pre-anesthetic evaluation
reduce the onset time of Rocuronium and improve the intubating
conditions [4]. It can also prevent hypotension associated with bolus 1. Each patient underwent a detailed pre-anesthetic check up one
doses of Propofol during induction of general anesthesia [5]. The peak day prior to surgery. Informed written consent was taken from all the
effect of Ephedrine on cardiac output is reached at about 2-3 minutes patients to be enrolled in the study.
after the injection [6]. 2. Detailed history, thorough clinical examination (physical and
It is advisable to use an appropriate dose of Ephedrine to achieve systemic) was done.
both these benefits without undue side effects such as hypertension or 3. Routine investigations like Hb, BT, CT, TLC, DLC, RFT, serum
tachycardia. Because of variation in doses and side effects of Ephedrine electrolytes, LFT, blood sugar(F), urine R/E, ECG and chest X-ray (PA
in various studies, we compared the influence of Ephedrine 30, 70 and view) was noted.
110 mcg/kg on intubating conditions and hemodynamics using
Propofol and low dose Rocuronium. 4. Any other investigation as deemed necessary for the patient was
carried out.
Aims and Objectives 5. All patients were prepared by overnight fasting. Patients received
tab Alprazolam 0.25 mg and tab Ranitidine 150 mg orally at bed time
To compare the effect of various doses of Ephedrine on the night before surgery.
intubating conditions with low dose Rocuronium.
To compare the effect of these doses of Ephedrine on 6. After arrival in pre-operative room, I/V line with 20 G cannula
hemodynamic parameters with low dose Rocuronium. was established and all patients received 2 ml/kg/hr. of ringer lactate
and Inj Diclofenac Sodium was given in the dose of 1.5 mg/kg body
weight intra muscularly.
Patients and Methods
The present randomized open labeled prospective study was Anesthetic procedure
conducted in the Post Graduate department of Anesthesiology and
In the operating room, standard monitors such as ECG, SPO2,
critical care GMC, Jammu.
ETCO2 and automated blood pressure was attached, and baseline
This study was approved by the University's Institutional Ethics measurements were recorded. Patients were pre-oxygenated for 3
Committee (IEC/Thesis/Research/T5B/2016/294) dated 07-10-2016 minutes. Fentanyl 2 mcg/kg body weight was given one minute after
and written informed consent was obtained from all subjects start of pre-oxygenation. Then one minute afterwards, Ephedrine was
participating in the trial. administered in the dosage of 30, 70 or 110 mcg/kg body weight in the
J Anesth Clin Res, an open access journal Volume 10 • Issue 11 • 1000920
ISSN: 2155-6148
Citation: Sharma M, Jamwal A, Mehta A, Jyoti R (2019) A Comparative Study of Different Doses of Ephedrine on Intubating Conditions and
Hemodynamics Using Propofol and Low Dose Rocuronium. J Anesth Clin Res 10: 920.
Page 3 of 5
groups 1, 2 and 3 respectively diluted in 5 ml of saline. Three minutes patients enrolled in the study 4 patients were excluded from the study.
after pre-oxygenation with 100% Oxygen, anesthesia was induced with Endotracheal intubation caused significant increase in systolic and
Propofol 2.5 mg/kg over 20 seconds. After loss of verbal contact with diastolic blood pressure (systolic/diastolic blood pressure: >200/100) at
the patient and confirmation that ventilation via the facemask is 1 minute in 4 patients of group 3 (110 mcg/kg) with no patients in
possible, all the patients received 0.6 mg/kg of inj. Rocuronium over 5 other study group. This exaggerated response may be because lighter
seconds. Patients were not ventilated unless SPO2 fell below 90%. planes of anesthesia, prolonged laryngoscopy or higher dose of
Laryngoscopy was done with an appropriately sized Macintosh blade Ephedrine (110 mcg/kg).
60 seconds after administration of Rocuronium. And tracheal
intubation was attempted after that. Oral endotracheal tubes 7.0 and Groups N Mean age SD Range p-value
8.0 internal diameter was used for females and males respectively. The Group 1 30 34.3 7.89 21-49
cuff was inflated with air until the disappearance of a leak on positive
pressure ventilation. Group 2 30 35.8 7.93 19-50 0.727
Intubation time was recorded as the number of seconds from end of Group 3 30 34.4 7.97 20-48
administration of neuromuscular blocking agent to insertion of tube
into trachea, as measured by a stopwatch. Table 1: Showing mean age of study patients among various groups.
Intubating conditions were assessed using the criteria of Cooper and
colleagues [7]. Criteria for jaw relaxation, vocal cord position and
intubating response were used to assess intubation condition. Jaw
relaxation: 0=poor, 1=minimal, 2=moderate and 3=good; vocal cords
position: 0=closed, 1=closing, 2=moving and 3=open; response to
intubation: 0=severe coughing or bucking, 1=mild coughing, 2=light
diaphragmatic movement and 3=none. A total score of 8-9 was
considered excellent; 6-7 was considered good, 3-5 as fair and 0-2 as
poor.
Patient’s mean arterial pressure, heart rate, and oxygen saturation
was recorded before induction (baseline), just before intubation, and 1,
3, and 5 minutes after the intubation and then every 10 minutes
throughout surgery.
30% or more increase in BP or HR above baseline was excluded
from the study. 20%-30% increase in HR or BP above baseline was
managed by esmolol 0.3 mg/kg.
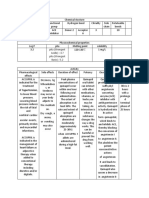
Anesthesia was maintained with oxygen 40%, Nitrous Oxide 60% Figure 1: Intubating conditions amongst various groups.
and Halothane with intermittent positive pressure ventilation
maintaining normocapnia. Top-up of Rocuronium in the dosage of
0.15 mg/kg was given if required.
All patients were reversed with inj Glycopyrrolate 10 mcg/kg and inj
Neostigmine 50 mcg/kg after completion of surgical procedure. Inj
ondansetron in the dose of 0.1 mg per kg was given prior to reversal.
Statistical analysis
The recorded data was compiled and entered in a spreadsheet
(Microsoft Excel) and then exported to data editor of SPSS Version
20.0 (SPSS Inc., Chicago, Illinois, USA). Continuous variables were
summarized in the form of means and standard deviations and
categorical variables were expressed as frequencies and percentages.
Graphically the data was presented by bar and lie diagrams. Analysis of
variance (ANOVA) with least significant difference (LSD) test was
employed for comparing continuous variables. Chi-square test or
Fisher’s exact test, whichever appropriate, was applied for comparing
categorical variables. A p-value of less than 0.05 was considered
statistically significant.
Results Figure 2: Changes in heart rate (beats/min) among various groups
during induction.
The demographic parameters of the patients including age, weight,
sex, ASA status and intubating time was statistically insignificant
between the groups (p-value>0.05) (Tables 1 and 2). Among the 90
J Anesth Clin Res, an open access journal Volume 10 • Issue 11 • 1000920
ISSN: 2155-6148
Citation: Sharma M, Jamwal A, Mehta A, Jyoti R (2019) A Comparative Study of Different Doses of Ephedrine on Intubating Conditions and
Hemodynamics Using Propofol and Low Dose Rocuronium. J Anesth Clin Res 10: 920.
Page 4 of 5
Discussion
In patients where Succinylcholine could be avoided because of
conditions like recent burns, open globe injury, increased intracranial
pressure etc., Rocuronium was successfully used in higher doses of
0.9-1.2 mg/kg to decrease the onset time of neuromuscular blockade.
When a large dose of Rocuronium is used, its duration of action is
prolonged, making it unsuitable for short procedures and difficult
ventilation situations. Several anesthesiologists used Rocuronium in
the lower dose of 0.6 mg/kg for rapid tracheal intubation which lead to
suboptimal intubating conditions in 20-25% of patients [8].
Ephedrine as an adjuvant with Rocuronium and Propofol has
various effects. A larger dose of Rocuronium 0.9 ± 1.2 mg/kg can be
avoided by administering ephedrine. Another advantage being that it’s
theoretically safer for haemodynamically unstable patients. Induction
with Propofol, Ephedrine and low dose Rocuronium produces good
intubating conditions in a timescale appropriate for rapid sequence
induction. The use of the Propofol-Ephedrine combination will also
avoid the unwanted side-effects of Ketamine and Etomidate, which
although shortens the onset of Rocuronium but produces
hallucinations and adrenal suppression [9].
Figure 3: Changes in MAP (mm Hg) among various groups during
induction. The better intubating conditions in Group 2 and Group 3 are most
likely due to the effects of Ephedrine resulting in an increased cardiac
output and tissue perfusion and therefore a faster delivery of
Mean Intubating
Rocuronium to the laryngeal and diaphragmatic muscles. The factors
Groups N SD Range p-value affecting the onset of neuromuscular blockers have been extensively
time
reviewed by Donati, 1981 [1] and includes access of the neuromuscular
Group 1 30 120.1 19.73 90-150 blocker to the muscle and its interaction with muscle nicotinic
Group 2 30 119.4 16.97 93-146 0.667
receptors. The speed of a drug's access to these receptors appears to be
proportional to cardiac output, circulation time and muscle perfusion.
Group 3 30 123.4 17.66 95-150
Development of neuromuscular blockade was not monitored as
there is a poor correlation between onset time of neuromuscular
Table 2: Comparison based on intubating time among various groups. blockade measured at the adductor pollicis muscle and the quality of
intubating conditions [10]. Agoston in 1951 [11] has declared that
It was found that intubating conditions were most favorable in neuromuscular transmission monitoring is probably obsolete in this
group 2 (Ephedrine 70 mcg/kg) followed by group 3 (Ephedrine 110 context. Furthermore, we considered it more important to adhere to a
mcg/kg) and least favorable in group 1 (Ephedrine 30 mcg/kg) (Table rapid sequence protocol rather than delay tracheal intubation during
3, Figure 1)). Group 3 was associated with adverse hemodynamic the calibration period of a neuromuscular transmission monitor.
effects such as tachycardia and increased blood pressure. Such effects
being least in group 1 (Ephedrine 30 mcg/kg) and intermediate in In present study, the difference in heart rate from the baseline was
group 2 (Ephedrine 70 mcg/kg). However, group 2 (Ephedrine 30 greatest in group 3 followed by group 2 and group 1 in that order. This
mcg/kg) had best patient profile in terms of favorable intubating can be explained by the fact that in group 1 we used lowest dose of
conditions and hemodynamic conditions (Figures 2 and 3). Ephedrine and hence patients ’ laryngeal and diaphragmatic
musculature could not be completely paralyzed during laryngoscopy
Intubating
Group 1 [n=30] Group 2 [n=30] Group 3 [n=30] and intubation. As lower dose of Ephedrine has minimal effect on
Conditions cardiac output, therefore decreased amount of the muscle relaxant will
No. %age No. %age No. %age
be present in the bio phase leading to poor relaxation of laryngeal
Excellent 2 6.7 8 26.7 6 20 musculature during intubation and hence the aforementioned effects.
Good 15 50 19 63.3 19 63.3 No statistically significant difference in Systolic blood pressure,
diastolic blood pressure and mean arterial pressure was found amongst
Fair 13 43.3 3 10 5 16.7 the groups on intergroup comparison (p value>0.05). On intragroup
comparison, statistically significant increase in systolic blood pressure,
Group 2 vs. Group 3 Group 1 vs. Group 3
Group 1 vs. Group 2 diastolic blood pressure and mean arterial pressure from baseline was
p-value
seen after intubation and 1 minute after intubation in all the three
0.006* 0.675 0.039* groups. The difference in blood pressure from the baseline was greatest
*Statistically significant difference from baseline (p-value<0.05)
in group 3 followed by group 2 and group 1 in that order.
The increase in heart rate and blood pressure after Ephedrine is
Table 3: Comparison based on intubating conditions among various expected as it is a sympathomimetic drug which stimulates both alpha
groups. and beta receptors, and also releases Noradrenaline from the storage
J Anesth Clin Res, an open access journal Volume 10 • Issue 11 • 1000920
ISSN: 2155-6148
Citation: Sharma M, Jamwal A, Mehta A, Jyoti R (2019) A Comparative Study of Different Doses of Ephedrine on Intubating Conditions and
Hemodynamics Using Propofol and Low Dose Rocuronium. J Anesth Clin Res 10: 920.
Page 5 of 5
sites. This sympathomimetic action is responsible for the Associate Professor of Psychiatry at Vanderbilt School of Medicine for
hemodynamic changes. However, the heart rate returned to baseline at his valuable input after reviewing the manuscript and for the insightful
5 minutes after intubation and the systolic blood pressure, diastolic suggestions he contributed.
blood pressure and mean arterial pressure returned to baseline at 3
minutes after intubation. References
Finally, to sum up, ephedrine 70 mcg/kg given 60 seconds before 1. Donati F (1988) Onset of action of relaxants. Can J Anaesth 35: 52–58.
Rocuronium improved intubating conditions and facilitated the onset
2. McCourt KC, Salmela L, Mirakhur RK, Carroll M, Mäkinen MT, et al.
of Rocuronium without adverse hemodynamic effects. It was found (1998) Comparison of Rocuronium and Suxamethonium for use during
that intubating conditions were most favorable in group 2 (Ephedrine rapid sequence induction of anesthesia. Anaesthesia 53: 867-871.
70 mcg/kg) followed by group 3 (Ephedrine 110 mcg/kg) and least 3. Sparr HJ, Giesinger S, Ulmer H, Hollenstein-Zacke M, Luger TJ (1996)
favorable in group 1 (Ephedrine 30 mcg/kg). Group 3 was associated Influence of induction technique on intubating conditions after
with adverse hemodynamic effects such as tachycardia and increased rocuronium in adults: comparison with rapid sequence induction using
blood pressure. Such effects being least in group 1 (Ephedrine 30 thiopentone and suxamethonium. Br J Anaesth 77: 339-342.
mcg/kg) and intermediate in group 2 (Ephedrine 70 mcg/kg). 4. Tan CH, Onisong MK, Chiu WK (2002) The influence of induction
However, group 2 (Ephedrine 30 mcg/kg) had best patient profile in technique on intubating conditions 1 min after rocuronium
terms of favorable intubating conditions and hemodynamic administration: a comparison of a propofol-ephedrine combination and
propofol. Anaesthesia 57: 223-226.
conditions.
5. Michelsen I, Helbo-Hansen HS, Kohler F, Lorenzen AG, Rydlund E, et al.
(1998) Prophylactic ephedrine attenuates the hemodynamic response to
Conclusion propofol in elderly female patients. Anesth Analg 86: 477-481.
We conclude that pre-treatment with ephedrine 30 mcg/kg one 6. Rådström M, Bengtsson J, Ederberg S, Bengtsson A, Loswick AC, et al.
(1995) Effects of ephedrine on oxygen consumption and cardiac output.
minute before administration of low dose Rocuronium (0.6 mg/kg) on Acta Anaesthesiol Scand 39: 1084-1087.
induction with Propofol (2.5 mg/kg) provides poor intubating
7. Cooper R, Mirakhur RK, Clarke RSJ, Boules Z (1992) Comparison of
conditions with stable hemodynamics, while pre-treatment with intubating conditions after administration of org 9426(rocuronium) and
ephedrine 110 mcg/kg with the same doses of Rocuronium and Suxamethonium. Br J Anaesth 69: 269-273.
Propofol provides acceptable intubating conditions but with 8. Magorain T, Flannery KB, Miller RD (1993) Comparison of rocuronium,
exaggerated and unacceptable hemodynamic response. Ephedrine pre- succinylcholine, and vecuronium for rapid sequence induction of
treatment in the dose of 70 mcg/kg with similar doses of Rocuronium anesthesia in adult patients. Anesthesiology 79: 913-918.
and Propofol provides ideal intubating conditions with acceptable 9. Muñoz HR, González AG, Dagnino JA, González JA, Pérez AE (1997)
hemodynamic changes. So, the combination of Propofol 2.5 mg/kg, The effect of ephedrine on the onset time of Rocuronium. Anesth Analg
Rocuronium 0.6 mg/kg and ephedrine 70 mcg/kg may be of value 85: 437-440.
when use of Succinylcholine is contraindicated for Rapid Sequence 10. Huizinga ACT, Vandenbrom RHG, Wierda JMKH, Hommes FDM,
Induction. Hennis PJ (1992) Intubating conditions and onset of neuromuscular
block of rocuronium (Org 9426); a comparison with suxamethonium.
Acta Anaesthesiol Scand 36: 463–468.
Acknowledgements 11. Agoston S (1995) Onset time and evaluation of intubating conditions:
rocuronium in perspective. Eur J Anaesthesiol 12: 31–37.
The authors would like to thank Dr Harry Gwirtsman, Staff
Psychiatrist, Tennessee Valley Healthcare System, VA Hospitals and
J Anesth Clin Res, an open access journal Volume 10 • Issue 11 • 1000920
ISSN: 2155-6148
You might also like
- Personal Care Attendant TestDocument16 pagesPersonal Care Attendant Testtugurlan50% (2)
- CHCPAL001 Assessment 1Document14 pagesCHCPAL001 Assessment 1dev kumar75% (4)
- Form Sop SampleDocument12 pagesForm Sop SampleAlka AzzwarsNo ratings yet
- Clinical Case in Neurology by SlidesgoDocument46 pagesClinical Case in Neurology by SlidesgonadaNo ratings yet
- Kundu - Pearls in Medicine For Students@helpmedico PDFDocument303 pagesKundu - Pearls in Medicine For Students@helpmedico PDFSwarnadeep Mani100% (1)
- Bahasa Inggris AskepDocument4 pagesBahasa Inggris AskepMona Indah100% (2)
- Raphael Rettner - Your Healing Hands - The Polarity ExperienceDocument42 pagesRaphael Rettner - Your Healing Hands - The Polarity ExperienceYuldash100% (2)
- Pharmacologic Therapy For Acute PainDocument11 pagesPharmacologic Therapy For Acute PainDiana Florez100% (1)
- UEG Journal - 2018 - Nishizawa - Propofol For Gastrointestinal EndosDocument5 pagesUEG Journal - 2018 - Nishizawa - Propofol For Gastrointestinal Endosmax medinaNo ratings yet
- RocuroniumbromideinjDocument14 pagesRocuroniumbromideinjagnes hutabaratNo ratings yet
- Ağrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Document4 pagesAğrısız Gastroskopi Sırasında Anestezi Indüksiyonunda Bireyselleştirilmiş Optimal Hedef Konsantrasyonu Hesaplamak Için Bir Gösterge Olarak Kirpik Refleksini Kullanmanın Uygulanabilirliğini Araştırmak.Ali ÖzdemirNo ratings yet
- Anesthesia and Procedural MonitoringDocument5 pagesAnesthesia and Procedural MonitoringVanesa Michelle Estrella ObregonNo ratings yet
- Critical Care CasesDocument7 pagesCritical Care CasesJude Micko Bunyi AlipitNo ratings yet
- A Case Report and Overview of Organophosphate (OP) PoisoningDocument5 pagesA Case Report and Overview of Organophosphate (OP) PoisoningDhruva PatelNo ratings yet
- Jurnal GenerghjfgjyjhvjhgjfjdjmhfjmDocument5 pagesJurnal GenerghjfgjyjhvjhgjfjdjmhfjmH'Cham AchmadNo ratings yet
- Experimental Models of Impaired Hypoglycaemia As - 2020 - Trends in EndocrinologDocument13 pagesExperimental Models of Impaired Hypoglycaemia As - 2020 - Trends in EndocrinologJOSE ARTURO LOZANO CRUZNo ratings yet
- haloperidol combined with dexamethasoneDocument6 pageshaloperidol combined with dexamethasoneapi-741687858No ratings yet
- RSI Pharmacology For The Emergency Medicine PhysicianDocument2 pagesRSI Pharmacology For The Emergency Medicine PhysicianGuide LPNo ratings yet
- Pharmacology Viva Manual Prefinal PDFDocument112 pagesPharmacology Viva Manual Prefinal PDF9821699080100% (1)
- Jurnal 9Document5 pagesJurnal 9Widi MarsandaNo ratings yet
- Articulo 3Document6 pagesArticulo 3Raul Soto FigueroaNo ratings yet
- FarmaciaGheldiu Vlase 453-459Document8 pagesFarmaciaGheldiu Vlase 453-459Pablo AndrésNo ratings yet
- Independent Predictors of Delay in Emergence From General AnesthesiaDocument6 pagesIndependent Predictors of Delay in Emergence From General AnesthesiaDwi WahyudiNo ratings yet
- Outcome of Treatment of OPC Poisoning Patients With Atropine or Atropine Plus PralidoximeDocument5 pagesOutcome of Treatment of OPC Poisoning Patients With Atropine or Atropine Plus Pralidoximeshaker al baharNo ratings yet
- IOT Rapid Sequence Induction and Intubation 2010Document8 pagesIOT Rapid Sequence Induction and Intubation 2010fe53No ratings yet
- Jurnal Kelompok AnestesiDocument44 pagesJurnal Kelompok AnestesiAndrean MartinNo ratings yet
- The Effect of Acebrophylline Vs Sustained Release Theophylline in Pati...Document4 pagesThe Effect of Acebrophylline Vs Sustained Release Theophylline in Pati...Agencia FaroNo ratings yet
- RoculaxDocument4 pagesRoculaxvannyanoyNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument7 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Insulin Autoimmune Syndrome Induced by Exogenous Insulin Injection: A Four-Case SeriesDocument6 pagesInsulin Autoimmune Syndrome Induced by Exogenous Insulin Injection: A Four-Case SeriesFeni Nurmia PutriNo ratings yet
- Acta Anaesthesiol Scand - 2023 - SJ en - Hemodynamic Effects of A Low Versus A High Dose of Propofol During Induction ofDocument9 pagesActa Anaesthesiol Scand - 2023 - SJ en - Hemodynamic Effects of A Low Versus A High Dose of Propofol During Induction ofGunnar Helge SjøenNo ratings yet
- Choice of General Anesthetics For Trauma PatientsDocument8 pagesChoice of General Anesthetics For Trauma PatientsAngel IbarraNo ratings yet
- Anesthesiology Pain MedicineDocument4 pagesAnesthesiology Pain MedicinemarinarizkyutamiNo ratings yet
- Perioperative Glucocorticoid ManagementDocument8 pagesPerioperative Glucocorticoid ManagementjuanpbagurNo ratings yet
- Anesthesiology Pain MedicineDocument4 pagesAnesthesiology Pain MedicineagnessupangkatNo ratings yet
- Dr. Koduri's Review of Anesthesia for Eye SurgeryDocument20 pagesDr. Koduri's Review of Anesthesia for Eye SurgeryKamal MohamedNo ratings yet
- Iavt 03 I 2 PDocument3 pagesIavt 03 I 2 PAnastasia Lilian SuryajayaNo ratings yet
- Are Antimalarials Effective and Safe for Rheumatic DiseasesDocument10 pagesAre Antimalarials Effective and Safe for Rheumatic DiseasesYahya RizkiNo ratings yet
- Propofol: Present by The StudentDocument7 pagesPropofol: Present by The StudentAli dhyaaNo ratings yet
- Research Article: International Journal OfcurrentresearchDocument4 pagesResearch Article: International Journal OfcurrentresearchkasimNo ratings yet
- K Etorolac Tormethamine PDFDocument19 pagesK Etorolac Tormethamine PDFMuhammad Khairun NNo ratings yet
- FodaleDocument11 pagesFodaleAlexandra CojocaruNo ratings yet
- Flolan Drug Monograph - Munoz-3Document3 pagesFlolan Drug Monograph - Munoz-3Muhammad Muneeb KhawarNo ratings yet
- Drug Presentation ON Bronchodilato R: AminophyllineDocument16 pagesDrug Presentation ON Bronchodilato R: AminophyllineAnn_Antony_8717No ratings yet
- Pharmacology Muscle Relaxants and AnestheticsDocument15 pagesPharmacology Muscle Relaxants and AnestheticsDr IqraNo ratings yet
- Pleasant: 90 Letters TO Editors Br. J. Pharinac. (1 9 78), 5Document2 pagesPleasant: 90 Letters TO Editors Br. J. Pharinac. (1 9 78), 5DesalegnNo ratings yet
- 1 s2.0 S1550830716301665 MainDocument7 pages1 s2.0 S1550830716301665 MainAwadAyoubNo ratings yet
- 1 s2.0 S1550830716301665 MainDocument7 pages1 s2.0 S1550830716301665 MainAwadAyoubNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument5 pagesRevista Brasileira DE AnestesiologiaAngie OrtizNo ratings yet
- Rocuronium Versus Succinylcholine Are They.9Document4 pagesRocuronium Versus Succinylcholine Are They.9Kian PrakashNo ratings yet
- Clozapin RisperidonDocument7 pagesClozapin RisperidonAnonymous 2LcGdsRNo ratings yet
- Kleinberg l020715Document7 pagesKleinberg l020715hasanahNo ratings yet
- Research ArticleDocument7 pagesResearch Articlenaljnaby9No ratings yet
- JAnaesthClinPharmacol293394-8554992 234549 PDFDocument3 pagesJAnaesthClinPharmacol293394-8554992 234549 PDFAle ZuveNo ratings yet
- La Eficacia Del Sulfato de Magnesio para El Estado Asmático Fuera Del Entorno de Cuidados IntensivosDocument6 pagesLa Eficacia Del Sulfato de Magnesio para El Estado Asmático Fuera Del Entorno de Cuidados IntensivosCesar Jesus Jara VargasNo ratings yet
- Brufen Sustained Release (SR) : Data SheetDocument11 pagesBrufen Sustained Release (SR) : Data SheetPrince Ali100% (1)
- ABC of Oxygen Therapy in Acute CareDocument4 pagesABC of Oxygen Therapy in Acute CarefujiNo ratings yet
- Comparison of Two Drug Combinations in Total Intravenous Anesthesia: Propofol - Ketamine and Propofol-FentanylDocument12 pagesComparison of Two Drug Combinations in Total Intravenous Anesthesia: Propofol - Ketamine and Propofol-FentanylArya ArgamandaNo ratings yet
- Comparative Study of A Low-Dose With Standard Dose Propofol in Electroconvulsive Therapy (ECT) in Federal Neuropsychiatric Hospital, KadunaDocument5 pagesComparative Study of A Low-Dose With Standard Dose Propofol in Electroconvulsive Therapy (ECT) in Federal Neuropsychiatric Hospital, KadunaAdeyemi OlusolaNo ratings yet
- Riltrava Aerosphere Epar Product Information enDocument42 pagesRiltrava Aerosphere Epar Product Information enshihyanghuangNo ratings yet
- PropofolDocument27 pagesPropofolRoberto Carlos Castillo LopezNo ratings yet
- Besok HuluqDocument7 pagesBesok Huluqagustiawan28No ratings yet
- Opiodes de Corta DuraciónDocument9 pagesOpiodes de Corta DuraciónJuan Carlos Mandujano GuajardoNo ratings yet
- Effects of Olanzapine and Haloperidol On The Metabolic Status of Healthy MenDocument8 pagesEffects of Olanzapine and Haloperidol On The Metabolic Status of Healthy MenBenjamin paulNo ratings yet
- Evaluation of Propofol Anesthesia in Morbidly Obese Children and AdolescentsDocument9 pagesEvaluation of Propofol Anesthesia in Morbidly Obese Children and AdolescentsDebi SumarliNo ratings yet
- Hyperbaric Oxygenation Therapy: Molecular Mechanisms and Clinical ApplicationsFrom EverandHyperbaric Oxygenation Therapy: Molecular Mechanisms and Clinical ApplicationsNariyoshi ShinomiyaNo ratings yet
- [14374331 - Clinical Chemistry and Laboratory Medicine (CCLM)] Comparison of throat swabs and sputum specimens for viral nucleic acid detection in 52 cases of novel coronavirus (SARS-Cov-2)-infected pneumonia (COVID-19)Document6 pages[14374331 - Clinical Chemistry and Laboratory Medicine (CCLM)] Comparison of throat swabs and sputum specimens for viral nucleic acid detection in 52 cases of novel coronavirus (SARS-Cov-2)-infected pneumonia (COVID-19)nadaNo ratings yet
- Health Research AllianceDocument14 pagesHealth Research AlliancenadaNo ratings yet
- Biology Thesis by SlidesgoDocument39 pagesBiology Thesis by SlidesgozahraNo ratings yet
- KRS 03011281419129 Semester 1 2014-2015Document4 pagesKRS 03011281419129 Semester 1 2014-2015Wahyudi Permana DarlisNo ratings yet
- SalerioDocument28 pagesSalerioRizqaFebrilianyNo ratings yet
- Strokeaha 118 024172Document7 pagesStrokeaha 118 024172nadaNo ratings yet
- Strokeaha 118 024172Document7 pagesStrokeaha 118 024172nadaNo ratings yet
- Optimizing Red Blood Cell Transfusion Practice: S. D. Surgenor, M. Hampers, and H. L. CorwinDocument10 pagesOptimizing Red Blood Cell Transfusion Practice: S. D. Surgenor, M. Hampers, and H. L. CorwinnadaNo ratings yet
- Regional Center by SlidesgoDocument52 pagesRegional Center by SlidesgoPham PhamIoNo ratings yet
- Buvanendran2009 PDFDocument6 pagesBuvanendran2009 PDFnadaNo ratings yet
- Andi Rahmat PDFDocument7 pagesAndi Rahmat PDFyuyunNo ratings yet
- Regional Center by SlidesgoDocument52 pagesRegional Center by SlidesgoPham PhamIoNo ratings yet
- SalerioDocument28 pagesSalerioRizqaFebrilianyNo ratings yet
- Manajemen Transfusi Perioperatif Pada Pasien Bedah Jantung Dewasa DenganDocument18 pagesManajemen Transfusi Perioperatif Pada Pasien Bedah Jantung Dewasa DenganGambar DoangNo ratings yet
- Biology Thesis by SlidesgoDocument39 pagesBiology Thesis by SlidesgozahraNo ratings yet
- Emergency Cricothyrotomy Performed by Surgical Airway-Naive Medical PersonnelDocument9 pagesEmergency Cricothyrotomy Performed by Surgical Airway-Naive Medical PersonnelnadaNo ratings yet
- 29 82 1 PBDocument9 pages29 82 1 PBAlmuizzu NurjannahNo ratings yet
- Anesthetics and Anesthesiology: ClinmedDocument6 pagesAnesthetics and Anesthesiology: ClinmednadaNo ratings yet
- Bmri2015 465465Document5 pagesBmri2015 465465nadaNo ratings yet
- Fsurg 05 00059Document10 pagesFsurg 05 00059nadaNo ratings yet
- A Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationDocument10 pagesA Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationnadaNo ratings yet
- Journal PDFDocument6 pagesJournal PDFmuhammadfahmanNo ratings yet
- A Comparison Study of The Effect of Different Doses of Ephedrine On Prevention of Hemodynamic Changes Associated With Induction of General Anesthesia by Propofol and FentanylDocument10 pagesA Comparison Study of The Effect of Different Doses of Ephedrine On Prevention of Hemodynamic Changes Associated With Induction of General Anesthesia by Propofol and FentanylseruniallisaaslimNo ratings yet
- A Comparison Study of The Effect of Different Doses of Ephedrine On Prevention of Hemodynamic Changes Associated With Induction of General Anesthesia by Propofol and FentanylDocument10 pagesA Comparison Study of The Effect of Different Doses of Ephedrine On Prevention of Hemodynamic Changes Associated With Induction of General Anesthesia by Propofol and FentanylseruniallisaaslimNo ratings yet
- Anesthetics and Anesthesiology: Effect of Opioid-Free Anaesthesia On Perioperative Period: A ReviewDocument11 pagesAnesthetics and Anesthesiology: Effect of Opioid-Free Anaesthesia On Perioperative Period: A Reviewveranisa suciaNo ratings yet
- Joseph 2016Document1 pageJoseph 2016nadaNo ratings yet
- Introduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlDocument6 pagesIntroduction: Intravenous Ibuprofen May Offer Advantages Over Ketorolac For Postoperative Pain ControlnadaNo ratings yet
- Tracheal Intubation in Critically Ill PatientDocument9 pagesTracheal Intubation in Critically Ill PatientArdi FkuiNo ratings yet
- Tracheoesophageal Fistula (TEF) Is Commonly A Birth DefectDocument18 pagesTracheoesophageal Fistula (TEF) Is Commonly A Birth Defectboni_paguiganNo ratings yet
- QUINAPRILDocument2 pagesQUINAPRILTazkiaNo ratings yet
- Manual of Clinical Nutrition2013Document458 pagesManual of Clinical Nutrition2013Jeffrey Wheeler100% (9)
- Cashew Apple Report FinalDocument138 pagesCashew Apple Report FinalAbhijeet Singh50% (2)
- Know Your Magnetic FieldDocument75 pagesKnow Your Magnetic FieldAtma Jnani100% (5)
- The Effect of Massage Therapy On Chemotherapy-Induced Nausea and Vomiting in Pediatric CancerDocument7 pagesThe Effect of Massage Therapy On Chemotherapy-Induced Nausea and Vomiting in Pediatric CancerAgito Dedi100% (2)
- Atow 448 00Document10 pagesAtow 448 00Pandhu SuproboNo ratings yet
- Pterygium: Surgical Techniques and ChoicesDocument2 pagesPterygium: Surgical Techniques and ChoicesJohny Marquez TrochezNo ratings yet
- OGTT Recruitment Call Script For Individual Adult English V3 29nov10Document2 pagesOGTT Recruitment Call Script For Individual Adult English V3 29nov10rebklineNo ratings yet
- NCP For Rapid Shallow BreathingDocument1 pageNCP For Rapid Shallow Breathingbamboo2dNo ratings yet
- Complementary and Alternative TherapyDocument16 pagesComplementary and Alternative TherapyDevangi Bhorsat100% (1)
- Anger ManagementDocument4 pagesAnger ManagementAmron Azman100% (1)
- NCP&SOAPIEDocument4 pagesNCP&SOAPIEMica OmotsosircNo ratings yet
- Chest Trauma: Prof. Anjum Sohail Ansari H.O.D Surgery Cims, BahawalpurDocument37 pagesChest Trauma: Prof. Anjum Sohail Ansari H.O.D Surgery Cims, BahawalpurAmnaNo ratings yet
- Peace Corps Mefloquine Policy March 2015 Letter To DirectorDocument7 pagesPeace Corps Mefloquine Policy March 2015 Letter To DirectorAccessible Journal Media: Peace Corps DocumentsNo ratings yet
- Complete Thesis of HypertensionDocument79 pagesComplete Thesis of HypertensionFaisal Khan100% (6)
- The Association Between Hyponatremia and Psychotropic: An Observational Study in Chronic Forensic Rehabilitation Ward at Mental Health Hospital, Taif, Saudi ArabiaDocument5 pagesThe Association Between Hyponatremia and Psychotropic: An Observational Study in Chronic Forensic Rehabilitation Ward at Mental Health Hospital, Taif, Saudi ArabiaJAVED ATHER SIDDIQUINo ratings yet
- Basic EKG RefresherDocument210 pagesBasic EKG RefresherAaron D. Phoenix100% (6)
- Environmental SanitationDocument3 pagesEnvironmental SanitationChristopher MaNo ratings yet
- File 79 PDFDocument159 pagesFile 79 PDFSuzanne Le100% (1)
- Dengue DHFDocument14 pagesDengue DHFSandesh RaiNo ratings yet
- SJDS 412562 572Document11 pagesSJDS 412562 572habeebNo ratings yet
- Patient Education and CounselingDocument10 pagesPatient Education and CounselingRizky KaruniawatiNo ratings yet



































































![[14374331 - Clinical Chemistry and Laboratory Medicine (CCLM)] Comparison of throat swabs and sputum specimens for viral nucleic acid detection in 52 cases of novel coronavirus (SARS-Cov-2)-infected pneumonia (COVID-19)](https://imgv2-2-f.scribdassets.com/img/document/469431258/149x198/2a26953226/1710590182?v=1)