Professional Documents
Culture Documents
Lancet Hematology 2020-07-06-E447-E455
Lancet Hematology 2020-07-06-E447-E455
Uploaded by
bhat LibraryOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lancet Hematology 2020-07-06-E447-E455
Lancet Hematology 2020-07-06-E447-E455
Uploaded by
bhat LibraryCopyright:
Available Formats
Articles
Daratumumab monotherapy in patients with heavily
pretreated relapsed or refractory multiple myeloma:
final results from the phase 2 GEN501 and SIRIUS trials
Saad Z Usmani, Hareth Nahi, Torben Plesner, Brendan M Weiss, Nizar J Bahlis, Andrew Belch, Peter M Voorhees, Jacob P Laubach,
Niels W C J van de Donk, Tahamtan Ahmadi, Clarissa M Uhlar, Jianping Wang, Huaibao Feng, Ming Qi, Paul G Richardson, Sagar Lonial
Summary
Background Daratumumab showed encouraging efficacy as monotherapy in patients with heavily pretreated multiple Lancet Haematol 2020;
myeloma in the GEN501 and SIRIUS studies. Here we report a pooled, post-hoc final analysis of these two studies. 7: e447–55
See Comment page e426
Methods GEN501 was an open-label, multicentre, phase 1–2, dose escalation and expansion study done in the Levine Cancer Institute/Atrium
Netherlands, the USA, Sweden, and Denmark. Eligible patients had multiple myeloma and had relapsed or were Health, Charlotte, NC, USA
(S Z Usmani MD,
refractory to 2 or more previous lines of treatment that included a proteasome inhibitor or an immunomodulatory Prof P M Voorhees MD);
drug. SIRIUS was an open-label, multicentre, phase 2 study done in Canada, Spain, and the USA, in which eligible Karolinska Institute, Karolinska
patients with multiple myeloma had received 3 or more previous lines of therapy, including a proteasome inhibitor or University Hospital at
Huddinge, Stockholm, Sweden
an immunomodulatory drug, or were double refractory. In both studies, eligible patients were aged 18 years or older
(H Nahi MD); Vejle Hospital and
and had an Eastern Cooperative Oncology Group performance status of 2 or less. In part 2 of GEN501, patients were University of Southern
given intravenous daratumumab 16 mg/kg once per week for 8 weeks, twice per month for 8 doses, and then once per Denmark, Vejle, Denmark
month until disease progression. In part 2 of SIRIUS, patients received intravenous daratumumab 16 mg/kg once (Prof T Plesner MD); Janssen
Research & Development,
per week for 8 weeks, twice per month for 16 weeks, and once per month until disease progression. The primary
Spring House, PA, USA
endpoints (safety in GEN501 and overall response rate in SIRIUS) have previously been reported. These trials are (B M Weiss MD, C M Uhlar PhD,
registered on ClinicalTrials.gov, NCT00574288 (GEN501) and NCT01985126 (SIRIUS). J Wang PhD, H Feng PhD,
M Qi MD); Arnie Charbonneau
Cancer Research Institute,
Findings Patients were enrolled in GEN501 from March 27, 2008, until May 30, 2014, and in SIRIUS from Sept 30, 2013,
University of Calgary, Calgary,
until May 5, 2014. The combined analysis included 148 patients who received daratumumab 16 mg/kg (42 patients in AB, Canada (Prof N J Bahlis MD);
GEN501 part 2; 106 patients in SIRIUS), with a median follow-up of 36·6 months (IQR 34·5–38·2). Patients had Cross Cancer Institute,
received a median of 5 previous lines of therapy (IQR 4–7), and 128 (87%) of 148 patients were double refractory. The Edmonton, AB, Canada
(Prof A Belch MD); Dana Farber
overall response rate was 30·4% (95% CI 23·1–38·5), including 20 (14%) of 148 patients with very good partial
Cancer Institute, Harvard
response or better (8·5–20·1) and seven (5%) patients reporting complete response or better (1·9–9·5). Among Medical School, Boston, MA,
45 responders, the median duration of response was 8·0 months (95% CI 6·5–14·7). Median overall survival was USA (J P Laubach MD,
20·5 months (95% CI 16·6–28·1), with a 3-year overall survival rate of 36·5% (28·4–44·6). The most common Prof P G Richardson MD); VU
University Medical Center,
grade 3–4 treatment-emergent adverse events (TEAEs) were anaemia (grade 3, 26 [18%] of 148 patients; no grade 4 Amsterdam, Netherlands
events) and thrombocytopenia (grade 3, 13 [9%] of 148 patients; grade 4, 8 [5%] of 148 patients). Serious drug-related (N W C J van de Donk MD);
TEAEs occurred in 13 (9%) of 148 patients. There were no treatment-related deaths. Genmab A/S, Princeton, NJ,
USA (T Ahmadi MD); Winship
Cancer Institute, Emory
Interpretation In this analysis, daratumumab 16 mg/kg monotherapy showed durable responses and there were no University, Atlanta, GA, USA
new safety concerns with longer follow-up. (Prof S Lonial MD)
Correspondence to:
Funding Janssen Research & Development. Dr Saad Z Usmani, Levine Cancer
Institute, Charlotte, NC 28204,
USA
Copyright © 2020 Elsevier Ltd. All rights reserved. saad.usmani@atriumhealth.
org
Introduction heavily pretreated patients, including those refractory to
Outcomes for patients with multiple myeloma have treatment with both a proteasome inhibitor and an
improved as a result of an increase in treatment options, immunomodulatory drug.2–4 Patients with successive
including the introduction of proteasome inhibitors such relapses and those who are refractory to treatment have
as bortezomib, and immunomodulatory drugs such as poor survival.5 In a real-world analysis, overall survival
lenalidomide.1 However, most patients have disease was worse for patients with disease that was triple or
relapse, and the duration and depth of response decreases quadruple refractory to proteasome inhibitors and
with each successive line of therapy. Regimens containing immunomodulatory drugs (median overall survival
the second-generation proteasome inhibitors carfilzomib 5·1 months, 95% CI 2·6–8·7) than for those who were
and ixazomib have shown favourable response rates and double refractory to these classes of therapies (7·8 months,
prolonged survival in patients with previously treated 6·0–8·9).6 Effective therapies for patients with relapsed or
multiple myeloma, but outcomes remain poor for more refractory multiple myeloma remain a high unmet need.
www.thelancet.com/haematology Vol 7 June 2020 e447
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
Research in context
Evidence before this study Added value of this study
We searched PubMed on June 6, 2019, with no date This study presents the combined analysis for patients receiving
restriction using the keywords “progression risk”, “overall daratumumab 16 mg/kg in monotherapy studies GEN501 and
survival”, “multiple myeloma”, “relapsed”, and “refractory” SIRIUS at a median follow-up of approximately 3 years.
and identified 111 articles. Evidence suggests that, although Daratumumab monotherapy in heavily pretreated patients with
new agents have prolonged survival for patients with multiple myeloma continues to show impressive efficacy, with
previously treated multiple myeloma, outcomes remain poor rapid and durable responses observed. More than one third of
for most patients. Almost all patients have disease patients were still alive 3 years after initiation of the two trials.
progression, and treatments are also frequently associated The safety profile of daratumumab has remained consistent
with substantial adverse events. Daratumumab is a human after extended follow-up, with no new concerns identified.
CD38-targeting monoclonal antibody that gained initial
Implications of all the available evidence
US Food and Drug Administration approval as monotherapy
These findings highlight the efficacy of daratumumab
for patients with multiple myeloma in 2015 on the basis of
monotherapy in patients with heavily pretreated multiple
the results of early-phase studies GEN501 and SIRIUS.
myeloma. The rapid and durable responses and the manageable
Subsequent studies have shown significant improvement in
safety profile of daratumumab support its use alone or in
progression-free survival and response rates for patients
combination with other therapies for patients with relapsed or
treated with daratumumab in combination with standard-of-
refractory multiple myeloma.
care therapy in several treatment settings.
Daratumumab is a human IgG1 kappa (IgG1κ) (95% CI 23·7–39·2) and a median duration of response of
monoclonal antibody that binds with high affinity and 7·6 months (95% CI 5·6 to not evaluable), after a median
selectivity to CD38, inducing antitumour activity through follow-up of 20·7 months (range 0·5–27·1).13 Median
immunomodulation and directly targeting the tumour overall survival for the combined data was 20·1 months
cells.7 Following binding of daratumumab to CD38, (95% CI 16·6 to not evaluable), which could be attributed
tumour cell death is induced by numerous mechanisms, in part to the immunomodulatory mechanism of action of
including complement-dependent cyto toxicity, antibody- daratumumab or the inhibition of growth and survival
dependent cellular cytotoxicity, antibody-dependent phago factor transfer from bone marrow stromal cells.
cytosis, induction of apoptosis, and modulation of CD38 Daratumumab monotherapy is associated with a manage
enzymatic activity.7 The immuno modulatory actions of able safety profile and a low proportion of treatment
daratumumab include modulation of the tumour discontinuations due to adverse events.13 We present the
microenvironment, clonal expansion of cytotoxic T cells, final safety and efficacy findings for patients receiving
increase in helper T cells, depletion of CD38+ immuno daratumumab 16 mg/kg in GEN501 and SIRIUS in a
suppressive cells, and increase in granzyme B-positive combined analysis, after a median follow-up of
CD8+ T cells.8,9 Moreover, increase in myeloma cell survival approximately 3 years.
and proliferation via mitochondrial transfer from stromal
cells in the bone marrow microenvironment are inhibited Methods
by a CD38-blocking antibody.10 Study design and participants
The efficacy and safety of daratumumab monotherapy at The study design and patient populations for GEN501
16 mg/kg in patients with heavily pretreated relapsed or and SIRIUS have been described previously.11–13 GEN501
refractory multiple myeloma was investigated in two early- was an open-label, multicentre, phase 1–2, dose escalation
phase open-label studies.11,12 Results of the first-in-human and expansion study done in the Netherlands, the USA,
phase 1–2 study GEN50111 showed a proportion of patients Sweden, and Denmark. SIRIUS was an open-label,
receiving daratumumab 16 mg/kg with an objective multicentre, phase 2 study done in Canada, Spain, and
response rate (hereafter referred to as overall response the USA. Study sites information is included in the
See Online for appendix rate) of 36% (95% CI 22–52) and a median progression- appendix (pp 6–7) In both studies eligible patients were
free survival of 5·6 months (95% CI 4·2–8·1) at a median adults aged 18 years or older, with documented secretory
follow-up of 10·2 months (range 1·2–16·0). In SIRIUS, a multiple myeloma requiring systemic therapy, and an
phase 2 study,12 overall response rate was 29% (95% CI Eastern Cooperative Oncology Group (ECOG) perfor
20·8–38·9) and median progression-free survival was mance status of 2 or less. In GEN501, eligible patients
3·7 months (95% CI 2·8–4·6) at a median follow-up of were relapsed or refractory to at least 2 previous lines of
9·3 months (range 0·5–14·4). In both studies, the depth of treatment, including proteasome inhibitors, immuno
responses improved for many patients. Responses were modulatory drugs, chemotherapy, and autologous stem-
also durable, with an analysis of pooled data from these cell trans
plantation (ASCT). In SIRIUS, patients had
two studies showing an overall response rate of 31% received an alkylating agent (alone or as part of
e448 www.thelancet.com/haematology Vol 7 June 2020
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
combination therapy) and at least 3 previous lines of progression-free survival, time to disease progression, and
treatment that included a proteasome inhibitor and an duration of response. We report a combined analysis of
immunomodulatory drug, or had disease confirmed as the GEN501 and SIRIUS studies including updated data
double refractory to the most recent proteasome inhibitor for response, overall survival, subsequent therapy, and
and immunomodulatory treatment. Evidence of disease safety. There is no update on overall progression-free
progression (on or within 60 days of the last dose of their survival, as these data were mature at the previously
most recent treatment regimen) per International published analysis.13 Complete definitions of primary and
Myeloma Working Group (IMWG) criteria was required.14 secondary endpoints can be found in the appendix (pp 3–4);
Eligible patients in GEN501 (but not SIRIUS) had a life although this is a post-hoc analysis, all endpoints were
expectancy longer than 3 months. Additional eligibility defined as in the original study protocols.
criteria are in the appendix (p 2).
All study participants provided written informed Statistical analysis
consent before study entry. The studies were approved by Data from GEN501 and SIRIUS for patients who received
institutional review boards or ethics committees at all daratumumab monotherapy 16 mg/kg were pooled. All
participating institutions and were done in accordance patients who had received at least one dose of daratumumab
with the Declaration of Helsinki, the International were included in the efficacy and safety analyses. No
Conference on Harmonisation, and the guidelines for formal statistical hypotheses were formulated or tested,
Good Clinical Practice. and no statistical power calculations were done. In both
studies, if patients developed progressive disease and
Procedures subsequently discontinued daratumumab treatment, their
GEN501 included a dose escalation phase (part 1) and a subsequent therapies and best clinical responses to those
dose expansion phase (part 2). In part 1, patients received therapies were captured, when possible.
intravenous daratumumab at doses of 0·005 to 24 mg/kg. Responses were defined as per the IMWG criteria,14
After evaluation of safety and response at these doses, evaluated with the use of a computerised algorithm,
patients in part 2 received daratumumab at 8 mg/kg or and presented with two-sided exact 95% CIs. Previously
16 mg/kg. Daratumumab 16 mg/kg was administered reported response results from SIRIUS were based on
once per week for the first seven doses after the initial assessment by the Independent Review Committee,
dose, which had a 3-week washout period to collect showing excellent agreement with the results of the
pharmacokinetic data, twice per month for the subsequent computerised algorithm (kappa coefficient 0·98).12
eight doses, and once per month thereafter until disease Time-to-event endpoints were analysed using the
progression. In SIRIUS, patients were randomly assigned Kaplan-Meier method. Adverse events were reported by
1:1 to receive intravenous daratumumab 8 mg/kg or the patients at each study visit from informed content
16 mg/kg in part 1 and, after interim analysis that assessed to 30 days after the last dose of study drug for SIRIUS,
the responses of patients in each treatment group, and from the first infusion to the end-of-treatment visit
additional patients were enrolled into the 16 mg/kg for GEN501, and were defined as per National Cancer
cohort. Patients in part 2 of the SIRIUS study received Institute Common Terminology Criteria for Adverse
daratumumab 16 mg/kg once per week for 8 weeks, twice Events version 4.03.15
per month for 16 weeks, and then once per month These trials are registered on ClinicalTrials.gov,
thereafter. No daratumumab dose modifications were NCT00574288 (GEN501) and NCT01985126 (SIRIUS).
permitted. To prevent or mitigate infusion-related
reactions, patients in both the GEN501 and SIRIUS Role of the funding source
studies were given preinfusion and post-infusion Janssen Research & Development. The study design and
medications. Study treatment was discontinued for analyses were devised by the investigators and sponsor.
unacceptable toxic effects, patient withdrawal, predefined Study data were collected by the investigators and their
protocol deviation, disease progression, or if research teams. Final data analysis and verification of
daratumumab became commercially available (for accuracy was done by the sponsor. The investigators were
SIRIUS). Patients in GEN501 also discontinued treat not restricted by confidentiality agreements and had full
ment if they started a new antimyeloma therapy or had access to all the data. Medical writing and editorial
low platelet count. Reasons for study withdrawal were assistance were funded by Janssen Global Services.
loss to follow-up, patient withdrawal, study termination
by sponsor, or if daratumumab became commercially Results
available (for SIRIUS). Patients were enrolled in GEN501 between March 27, 2008,
and May 30, 2014; the 72 patients included in part 2 were
Outcomes followed up until the final clinical cutoff date of
The primary endpoint of GEN501 was safety. In SIRIUS, March 31, 2017. 124 patients were enrolled in SIRIUS
the primary endpoint was overall response rate. Other between Sept 30, 2013, and May 5, 2014, who were
endpoints of both studies included overall survival, followed up until the final clinical cutoff date of
www.thelancet.com/haematology Vol 7 June 2020 e449
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
Pooled analysis Response, n (%) 95% CI*
(n=148)
sCR 2 (1%) 0·2–4·8
Sex CR 5 (3%) 1·1–7·7
Male 69 (47%) VGPR 13 (9%) 4·8–14·6
Female 79 (53%) PR 25 (17%) 11·2–23·9
Age Minimal response 9 (6%) 2·8–11·2
Median age, years 64 (58–70) Stable disease 70 (47%) 39·0–55·7
65 to <75 years 52 (35%) Progressive disease 18 (12%) 7·4–18·5
≥75 years 16 (11%) Not evaluable 6 (4%) 1·5–8·6
ECOG performance status OR (sCR + CR + VGPR + PR) 45 (30%) 23·1–38·5
0 41 (28%) VGPR or better (sCR + CR + VGPR) 20 (14%) 8·5–20·1
1 97 (66%) CR or better (sCR + CR) 7 (5%) 1·9–9·5
2 10 (7%)
All patients received daratumumab 16 mg/kg. CR=complete response. OR=overall
Years since diagnosis 5·1 (3·9–7·8) response. PR=partial response. sCR=stringent complete response. VGPR=very
≥1 extramedullary plasmacytomas 18 (12%) good partial response. *Calculated by use of an exact CI.
Creatinine clearance
Table 2: Best responses in 148 patients combined from GEN501 part 2
≥60 mL/min 89 (60%) and SIRIUS
≥30 to <60 mL/min 54 (37%)
<30 mL/min 5 (3%)
Bone marrow plasma cells (%) follow-up of 36·6 months (IQR 34·5–38·24). All patients
≤30 85 (57%) who received 16 mg/kg daratumumab from the primary
>30 to ≤60 26 (18%) analyses11,12 are included in this pooled analysis with
>60 35 (24%) longer follow-up.
Number of previous lines of therapy 5 (4–7) Patient demographics and baseline characteristics for
>3 previous lines of therapy 113 (76%) 148 patients receiving daratumumab 16 mg/kg in the
Previous ASCT 116 (78%) combined analysis are presented in table 1. Patients were
Previous proteasome inhibitor* heavily pretreated, with a median of 5 (IQR 4–7) previous
Any 148 (100%) lines of therapy, and 113 (76%) of 148 patients having
Bortezomib 147 (99%) received more than 3 previous lines of therapy. 128 (87%)
Carfilzomib 61 (41%) of 148 patients were refractory to both a proteasome
Previous immunomodulatory drug* inhibitor and an immunomodulatory drug; 124 (84%)
Any 146 (99%) patients were refractory to lenalidomide, 82 (55%) patients
Lenalidomide 145 (98%) were refractory to pomalidomide, and 58 (39%) patients
Pomalidomide 82 (55%) were refractory to carfilzomib (table 1).
Thalidomide 66 (45%)
In GEN501, median duration of treatment was
Refractory to treatment
5·4 months (IQR 1·6–13·6), and patients received a
Last line of therapy 135 (91%)
median of 14·5 infusions (6–23). In SIRIUS, median
duration of treatment was 2·8 months (1·7–6·7), and
Both a proteasome inhibitor and 128 (87%)
an immunomodulatory drug patients received a median of 11·0 infusions (8–18). At
Proteasome inhibitor and immunomodulatory 100 (68%) clinical cutoff for both studies, most patients had
drug and alkylating agent discontinued treatment with daratumumab because of
Bortezomib 125 (85%) progressive disease (32 [76%] of 42 patients in GEN501
Carfilzomib 58 (39%) part 2; 96 [91%] of 106 patients in SIRIUS). Discon
Lenalidomide 124 (84%) tinuations as a result of adverse events were infrequent,
Pomalidomide 82 (55%) with only one (2%) of 42 patients in GEN501 and five (5%)
Thalidomide 41 (28%) of 106 patients in SIRIUS discontinuing treatment
Alkylating agent only 107 (72%) because of adverse events, none of which were considered
Data are n (%) or median (IQR). ASCT=autologous stem-cell transplantation.
related to daratumumab. Among the 148 patients from
ECOG=Eastern Cooperative Oncology Group. *Patients could have received more GEN501 and SIRIUS, 14 (9%) died within 30 days of the
than one of these therapies. last daratumumab dose: 11 (7%) because of progressive
Table 1: Patient characteristics at baseline
disease and three (2%) because of adverse events (not
considered related to daratumumab).
In the combined analysis, the overall response rate
May 30, 2017. The combined analysis included 148 patients was 30·4% (95% CI 23·1–38·5), with 20 (14%) of
who received daratumumab 16 mg/kg (42 patients in 148 patients reporting a very good partial response
GEN501 part 2; 106 patients in SIRIUS), with a median (8·5–20·1) or better and seven (5%) patients reporting
e450 www.thelancet.com/haematology Vol 7 June 2020
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
complete response or better (1·9–9·5; table 2). Responses
PR
improved with continued daratumumab treatment for PR CR
VGPR CR
14 (31%) of 45 patients with a response across both PR sCR
PR
studies (figure 1). Of the 45 patients with a response, VGPR CR
PR VGPR
34 (76%) had an initial partial response. Seven (21%) of VGPR
VGPR
CR
34 patients went on to have very good partial response, PR
VGPR sCR
VGPR CR
one (3%) to complete response, and one (3%) to stringent PR
PR
complete response. Five (46%) of 11 patients with an PR VGPR
PR VGPR
initial response of VGPR had responses deepen, four PR
PR
(36%) to complete response and one (9%) to stringent PR
VGPR
VGPR
complete response. The median duration of response PR
PR
Patient
was 8·0 months (95% CI 6·5–14·7) for the combined PR
PR VGPR
VGPR
population of 45 responders. PR
PR
In patients with a partial response or better, the PR
VGPR
proportion of patients with progression-free survival at PR
VGPR
36 months was 19·6% (95% CI 9·0–33·2), 19·6% at PR
PR
24 months (9·0–33·2), and 40·6% at 12 months PR VGPR
PR
(26·1–54·6). For all patients, median overall survival was PR
PR
PR
20·5 months (95% CI 16·6–28·1) with a 3-year overall PR
PR
survival of 36·5% (28·4–44·6; figure 2A) at clinical cutoff. PR
PR VGPR
An analysis of median overall survival by response status VGPR SIRIUS
PR
is presented in figure 2B. The median overall survival for PR GEN501 part 2
responders (partial response or better) was not reached 0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 42
(95% CI 29·2–not estimable), and 36-month overall Time from first dosing date (months)
survival was 60·2% (43·9–73·2). Patients with a minimal
response or stable disease had a median overall survival Figure 1: Swim-lane plot of responders in 148 patients who received daratumumab at 16 mg/kg from
GEN501 part 2 and SIRIUS
of 18·5 months (95% CI 15·1–22·4) and 36-month overall CR=complete response. PR=partial response. sCR=stringent complete response. VGPR=very good partial response.
survival of 29·5% (19·1–40·6). Patients with progressive
disease or without an evaluable response had median
overall survival of 3·5 months (95% CI 1·5–6·6) and of 148 patients. Three patients died during the studies
36-month overall survival of 12·5 % (3·1–28·7). because of TEAEs, which were not considered to be drug-
119 (80%) of 148 patients received subsequent therapy related (one each of viral H1N1 infection, pneumonia,
for multiple myeloma. The most common (given to and aspiration pneumonia). Infusion-related reactions
>20% of patients) subsequent therapies included occurred in 71 (48%) of 148 patients. 68 (96%) of
dexamethasone (96 [65%] patients), pomalidomide 71 patients with an infusion-related reaction had an event
(62 [42%]), cyclophosphamide (54 [36%]), carfilzomib occur during the first infusion, five (7%) patients had an
(48 [32%]), bortezomib (44 [30%]), and lenalidomide event during the second infusion, and five (7%) patients
(31 [21%]). 28 (19%) of 148 patients received daratumumab had an event during subsequent infusions. The most
as subsequent therapy. Of the 119 patients receiving common infusion-related reactions included nasal
subsequent therapy, 44 (37%) had a partial response or congestion (17 [11%] of 148 patients), cough (12 [8%]),
better on their first subsequent line of therapy, including allergic rhinitis (10 [7%]), chills (10 [7%]), throat irritation
14 (12%) patients with a very good partial response, (9 [6%]), dyspnoea (8 [5%]), and nausea (8 [5%]).
three (3%) patients with a complete response, and Immunoparesis (defined as uninvolved immunoglobulin
three (3%) patients with a stringent complete response. <lower limit of normal) at baseline occurred among
147 (99%) of 148 patients had at least one treatment- 37 (88%) of 42 patients in GEN501 and 103 (97%) of
emergent adverse event (TEAE; table 3). The most 106 patients in SIRIUS. Within 30 days of last study
frequently reported any-grade TEAEs were fatigue treatment, immunoparesis was seen in 41 (98%) of
(62 [42%] of 148 patients), nausea (44 [30%]), anaemia 42 patients in GEN501 part 2, including among all
(42 [28%]), back pain (40 [27%]), and cough (38 [26%]). 15 responders. For SIRIUS, postbaseline immunoglobulins
Infections of any grade occurred in 87 (59%) of were not available.
148 patients, with a grade 3 event in 13 (9%) of 148 patients Patient samples to evaluate the potential immuno
and a grade 4 event in two (1%) patients. TEAEs were genicity of daratumumab were collected predose, during
generally mild (grade 1–2); anaemia (26 [18%] patients) study treatment, and after completion of therapy.11,12 In
was the only grade 3 TEAE reported in more than 10% of both studies, none of the patients with samples appropriate
patients, and the only grade 4 TEAE occurring in 5% or for analysis (39 patients in GEN501 part 2 and 95 patients
more of patients was thrombocytopenia (8 [5%] patients). in SIRIUS) were positive for antidaratumumab antibodies,
Serious drug-related adverse events occurred in 13 (9%) suggesting a low risk for immunogenicity.
www.thelancet.com/haematology Vol 7 June 2020 e451
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
A
100
80
Overall survival (%)
60
Median overall survival 20·5 months
(95% CI 16·6–28·1)
40
20
0
0 2 4 6 8 10 12 14 16 18 20 22 24 26 28 30 32 34 36 38 40 42 44
Number at risk 148 136 125 119 108 103 96 90 82 77 70 64 60 58 55 52 50 43 30 14 9 2 0
(number censored) (0) (0) (4) (5) (6) (6) (7) (7) (8) (9) (9) (11) (12) (12) (12) (12) (13) (19) (30) (44) (49) (56) (58)
B
100 Patients with PR or better
Patients with minimal response
or stable disease
Patients with progressive disease
80
Median overall survival NR
(95% CI 29·2–not estimable)
Overall survival (%)
60
40 Median overall survival 18·5 months
(95% CI 15·1–22·4)
20 Median overall survival 3·5 months
(95% CI 1·5–6·6)
0
0 3 6 9 12 15 18 21 24 27 30 33 36 39 42 45
Time from start of treatment (months)
Number at risk
(number censored)
Patients with PR 45 45 44 42 42 40 39 34 33 30 28 26 18 7 2 0
or better (0) (0) (1) (1) (1) (1) (1) (2) (2) (2) (2) (3) (10) (20) (25) (27)
Patients with minimal 79 73 65 58 50 45 35 28 24 23 21 18 10 4 0 0
response or stable disease (0) (1) (4) (5) (6) (6) (8) (8) (10) (10) (10) (12) (19) (24) (28) (28)
Patients with 24 14 10 5 4 3 3 3 3 3 3 3 2 0 0 0
progressive disease (0) (0) (0) (0) (0) (0) (0) (0) (0) (0) (0) (0) (1) (3) (3) (3)
Figure 2: Overall survival in 148 patients who received daratumumab at 16 mg/kg from GEN501 part 2 and SIRIUS
(A) All patients. (B) Patients stratified by response. Patients with progressive disease include those whose response was not evaluable. NR=not reached. PR=partial
response.
Discussion clinical trials, daratumumab-based regimens were
This pooled, final analysis among patients with refractory associated with significant reductions in the risk of
multiple myeloma shows that daratumumab 16 mg/kg progression or death by 44–63% and increased minimal
monotherapy provides durable responses; no new safety residual disease negativity, such as in the CASTOR and
concerns were identified with longer follow-up. POLLUX studies (patients with ≥1 previous lines of
Daratumumab was initially approved as a monotherapy treatment),17,18 and the ALCYONE and MAIA studies
in heavily treated patients on the basis of the GEN501 and (ASCT-ineligible, newly diagnosed patients).19,20 Therefore,
SIRIUS phase 2 studies.16 Across a series of phase 3 in many regions, patients treated with daratumumab are
e452 www.thelancet.com/haematology Vol 7 June 2020
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
likely to receive the drug as a component of a combination
Any grade Grade 1–2 Grade 3 Grade 4
regimen with standard-of-care therapies.7,21 However,
understanding the effects of long-term treatment with Fatigue 62 (42%) 59 (40%) 3 (2%) 0
daratumumab monotherapy is of value, as daratumumab- Nausea 44 (30%) 44 (30%) 0 0
based combinations are not available to many patients Anaemia 42 (28%) 16 (11%) 26 (18%) 0
and single-agent therapy is often the only option for Back pain 40 (27%) 36 (24%) 4 (3%) 0
disease refractory to multiple drug classes. Cough 38 (26%) 38 (26%) 0 0
Survival outcomes in similarly heavily pretreated patients Upper respiratory tract infection 33 (22%) 32 (22%) 1 (1%) 0
have typically been poor.5 Here, we report a median overall Thrombocytopenia 31 (21%) 10 (7%) 13 (9%) 8 (5%)
survival of 20·5 months (95% CI 16·6–28·1) for dara Neutropenia 31 (21%) 16 (11%) 11 (7%) 4 (3%)
tumumab monotherapy after median follow-up of Pyrexia 29 (20%) 28 (19%) 1 (1%) 0
36·6 months (IQR 34·5–38·24). The median overall Nasal congestion 29 (20%) 29 (20%) 0 0
survival and differences in overall survival observed when Arthralgia 28 (19%) 28 (19%) 0 0
stratified by response status are consistent with an earlier Diarrhoea 28 (19%) 27 (18%) 1 (1%) 0
pooled analysis of these studies.13 The progression-free Pain in extremity 26 (18%) 25 (17%) 1 (1%) 0
survival data were mature at the earlier pooled analysis, Dyspnoea 25 (17%) 24 (16%) 1 (1%) 0
with median progression-free survival of 4·0 months Nasopharyngitis 24 (16%) 24 (16%) 0 0
(95% CI 2·8–5·6), and median progression-free survival Constipation 23 (16%) 23 (16%) 0 0
data remain unchanged in this updated analysis.13 Decreased appetite 23 (16%) 22 (15%) 1 (1%) 0
In studies of other single-agent therapies (eg, without Vomiting 21 (14%) 21 (14%) 0 0
the addition of dexamethasone), similar or lower Musculoskeletal chest pain 19 (13%) 17 (11%) 2 (1%) 0
proportions of patients with overall response have been Hypercalcaemia 18 (12%) 13 (9%) 3 (2%) 2 (1%)
reported, with varying effects on overall survival. Headache 18 (12%) 16 (11%) 2 (1%) 0
Isatuximab, a CD38 monoclonal antibody in clinical Musculoskeletal pain 16 (11%) 15 (10%) 1 (1%) 0
development, showed an overall response of 21% in a Bone pain 15 (10%) 14 (9%) 1 (1%) 0
phase 1 study at a dose of 20 mg/kg (every 1 or 2 weeks).22 Chills 15 (10%) 15 (10%) 0 0
In a larger phase 2 study23 of 20 mg/kg isatuximab every Hypertension 15 (10%) 8 (5%) 7 (5%) 0
2 weeks in patients with a median of 4 previous lines of
Data are n (%). All patients received daratumumab 16 mg/kg.
therapy, the proportion of patients with overall response
was 26%, median progression-free survival was 4·9 months Table 3: Treatment-emergent adverse events reported in 10% or more of 148 patients combined from
(95% CI 3·8–7·7), and 16-month overall survival was 57% GEN501 part 2 and SIRIUS
(median not reached, 95% CI 14·7–not estimable).23
Treatment with a different CD38 monoclonal antibody,
MOR202, as monotherapy in a phase 1–2a study24 resulted response at 56 days, and further deepened to stringent
in an overall response of 31% in patients with heavily complete response at 194 days. Approximately 2 years
pretreated relapsed or refractory multiple myeloma. after enrolment, the patient showed no minimal residual
Monotherapy studies have also been done with next- disease, and after more than 3 years had not had disease
generation proteasome inhibitors. In a population of relapse.27 Three patients enrolled in GEN501 who had a
266 patients,25 in whom 82% had received 4 or more best response of stringent complete response remained
lines of previous therapy, patients given single-agent on daratumumab monotherapy for more than 4·5 years
carfilzomib had an overall response of 24% (95% CI (durations of 54 months, 56 months, and 59 months); all
18·7–29·4), with median overall survival of 15·6 months remain minimal residual disease negative at a 10–⁶
(13·0–19·2).25 A phase 1 study26 of ixazomib monotherapy sensitivity threshold.28 High proportions of minimal
in patients with a median of 4 lines of previous residual disease negativity have been shown in multiple
treatment resulted in an overall response of just 15% studies of daratumumab-based combinations.17–20 Analysis
(95% CI 6–27). Although many new therapies are under of minimal residual disease negativity in this pooled
investigation, the efficacy and favourable tolerability population would be of interest, but minimal residual
profile make single-agent daratumumab a useful disease data were not routinely evaluated in GEN501 and
treatment option for patients with heavily pretreated SIRIUS.
disease, particularly in patients who cannot tolerate Deep responses driven by daratumumab could be
combination therapy or where combination therapy is associated with changes in immune cell phenotype and
not available. function. Rapid and sustained decreases in immuno
In this analysis, responses continued to improve in suppressive CD38+ regulatory B and T cells were observed
some patients. A case report27 of a patient enrolled in in GEN501 and SIRIUS.9 Of note, a shift in T-cell
SIRIUS who was triple refractory (including bortezomib, phenotype in blood samples obtained after eight infusions
lenalidomide, and pomalidomide) described a partial of daratumumab occurred, with an increased proportion
response at 28 days, which improved to very good partial of CD8+ cells associated with an increase in granzyme B
www.thelancet.com/haematology Vol 7 June 2020 e453
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
positivity; this was most pronounced in patients who status (ECOG 3 and 4), and 10% had severe renal
responded to treatment.9 Inhibition of CD38 has been impairment. An additional limitation of GEN501 and
shown to prevent the transfer of mitochondria through SIRIUS is that the sample size did not allow for
nanotubes from bone marrow stromal cells to myeloma comparisons of patient subgroups, such as by cytogenetic
cells, thereby interfering with myeloma cell survival and risk status or those with a sustained response (>2 years). In
proliferation.10 a previous report of patients in SIRIUS, subgroup analysis
Although daratumumab is increasingly administered of overall response by baseline characteristics showed that
as part of combination therapy, this analysis showed that responses were observed across all subgroups regardless
long-term use as a monotherapy is well tolerated. In of the number or type of previous lines of therapy,
addition to its use as a monotherapy in heavily pretreated refractory status, renal function, or baseline percentage of
patients, daratumumab is used as a single-agent plasma cells in the bone marrow (appendix p 5).12
maintenance treatment after a period of combination After a median 3 years of follow-up, daratumumab
therapy, on the basis of the CASTOR and ALCYONE monotherapy continued to show a favourable safety profile
studies.17,19 with no new safety concerns. Meaningful responses were
No new safety concerns were identified relative to the observed in patients with a median of 5 previous lines of
initial reports for the two individual studies (at approxi therapy, suggesting that daratumumab could address an
mately 10 months of follow-up),11,12 or the previously unmet need in patients for whom other available treatment
published pooled analysis (at approximately 20 months of options have been exhausted. The encouraging efficacy
follow-up).13 The rate of infusion-related reactions was results observed with daratumumab monotherapy in
similar to previous publications, and these reactions were heavily pretreated patients, in addition to its manageable
well managed with preinfusion and postinfusion safety profile, support its use for patients with relapsed or
medications.11–13,29 Cytopenias were among the most refractory multiple myeloma. Ongoing studies are
common TEAEs, as were infections of any grade, addressing the efficacy and safety of daratumumab in
consistent with other daratumumab studies.11–13,19,20,30–32 combination regimens across lines of therapy, and
Immunoparesis was observed in nearly all patients, both at potential re-treatment, as daratumumab becomes more
baseline and post-treatment, consistent with the nature of frequently used in newly diagnosed patients.
advanced disease in this patient population. Daratumumab Contributors
can deplete natural killer (NK) cells, but there is no All authors drafted and reviewed the manuscript, approved the final
relationship between the safety profile and NK cell count version, and decided to publish this report, and vouch for data accuracy
and completeness. SL, HN, TP, NJB, TA, and PGR participated in the
reduction.33 The safety results reported here are also conception and design of the work being described in the publication,
consistent with those observed in an early access acquisition or collection of data, and analysis or interpretation of data.
programme in the USA for daratumumab in heavily SZU, BMW, AB, PMV, NWCJvdD, CMU, and JW participated in the
pretreated patients with relapsed or refractory multiple acquisition or collection of data and analysis or interpretation of data.
JPL participated in the conception and design of the work being
myeloma.34 Results from this early access programme also described in the publication. HF and MQ participated in analysis or
showed consistent health-related quality of life based on interpretation of data.
patient-reported outcomes after initiation of daratumumab Declaration of interests
treatment, further supporting the good tolerability of SZU served in a consulting or advisory role for Onyx, Sanofi, Takeda,
daratumumab monotherapy. That there does not seem to Celgene, Skyline, Millennium, Amgen, and Janssen; served on a speakers’
be cumulative or progressive toxicity with long-term bureau for Takeda, Celgene, and Amgen; and received research funding
from Onyx, Sanofi, Array BioPharma, Pharmacyclics, Takeda, Celgene,
daratumumab monotherapy is encouraging. and Bristol-Myers Squibb. TP received honoraria from Janssen; served in
A limitation of this analysis is that clinical trials might a consulting or advisory role for Janssen, Celgene, Takeda, and AbbVie;
not reflect real-world populations and outcomes can differ. received research funding from Janssen, Genmab, Amgen, Takeda,
Daratumumab monotherapy was less efficacious in a Roche, and Celgene; and had travel, accommodations, or other expenses
paid or reimbursed by Janssen. BMW received research funding and
study of 41 patients from a single centre in a real-world honoraria from and is an employee of Janssen. NJB received honoraria
study than in clinical trial data.35 Patients were treated per from Celgene, Janssen, AbbVie, and Amgen; served in a consulting or
the approved indication, namely 3 previous treatment advisory role for Celgene, Janssen, and AbbVie; received research funding
from Celgene; and had travel, accommodations, or other expenses paid or
lines including a proteasome inhibitor and an immuno
reimbursed by Celgene and Janssen. PMV served in a consulting or
modulatory drug, or were double refractory. An overall advisory role for Adaptive Biotechnologies, Bristol-Myers Squibb, Celgene,
response of 24% was associated with median progression- Janssen, Novartis, and Oncopeptides; and received research funding from
free survival of 1·9 months (95% CI 1·4–2·5) and median Amgen, Celgene, GlaxoSmithKline, and Janssen. JPL received research
funding from Bristol-Myers Squibb, Takeda, and Celgene. NWCJvdD
overall survival of 6·5 months (3·1–10·0). However, 44% of
served in a consulting or advisory role for Celgene, Janssen, Bristol-Myers
these patients did not receive subsequent therapy after Squibb, Bayer, Servier, and Novartis; and received research funding from
daratumumab. In GEN501 and SIRIUS, 119 (80%) of Celgene, Janssen, and Bristol-Myers Squibb. TA is an employee of and
148 patients received subsequent therapy, of whom owns stocks or has other ownership in Genmab. CMU, JW, HF, and MQ
are employees of Janssen. PGR received honoraria from and served in a
44 (37%) had a response (partial response or better). The
consulting or advisory role for Karyopharm, Oncopeptides, Celgene,
authors also noted that compared with GEN501 and Takeda, Amgen, and Janssen; and received research funding from
SIRIUS, the patients were older, 20% had worse functional Oncopeptides, Celgene, Takeda, and Bristol-Myers Squibb. SL received
e454 www.thelancet.com/haematology Vol 7 June 2020
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
Articles
consulting fees or honoraria from Celgene, Novartis, Bristol-Myers 16 McKeage K. Daratumumab: first global approval. Drugs 2016;
Squibb, Amgen, Janssen, GlaxoSmithKline, Merck, Karyopharm, and 76: 275–81.
Takeda; and received grants from or has pending grants with Celgene, 17 Spencer A, Lentzsch S, Weisel K, et al. Daratumumab plus
Janssen, and Takeda. HN and AB declare no competing interests. bortezomib and dexamethasone versus bortezomib and
dexamethasone in relapsed or refractory multiple myeloma:
Data sharing updated analysis of CASTOR. Haematologica 2018; 103: 2079–87.
The data sharing policy of Janssen Pharmaceutical Companies of Johnson 18 Dimopoulos M, San Miguel J, Belch A, et al. Daratumumab plus For more on the data sharing
& Johnson is available online. Requests for access to the study data can be lenalidomide and dexamethasone versus lenalidomide and policy of Janssen
submitted through the Yale Open Data Access (YODA) Project site. dexamethasone in relapsed or refractory multiple myeloma: Pharmaceutical Companies of
updated analysis of POLLUX. Haematologica 2018; 103: 2088–96. Johnson & Johnson see
Acknowledgments
19 Mateos MV, Dimopoulos MA, Cavo M, et al. Daratumumab plus https://www.janssen.com/
This study was sponsored by Janssen Research & Development.
bortezomib, melphalan, and prednisone for untreated myeloma. clinical-trials/transparency
The authors thank the patients who participated in the GEN501 and
N Engl J Med 2018; 378: 518–28.
SIRIUS (MMY2002) studies and their families; and the study co- For requests for access to the
20 Facon T, Kumar S, Plesner T, et al. Daratumumab plus study data see
investigators, research nurses, and coordinators at each of the clinical sites.
lenalidomide and dexamethasone for untreated myeloma.
Medical writing and editorial support were provided by Elise Blankenship, http://yoda.yale.edu
N Engl J Med 2019; 380: 2104–15.
PhD, of MedErgy, and were funded by Janssen Global Services.
21 Blair HA. Daratumumab: a review in relapsed and/or refractory
References multiple myeloma. Drugs 2017; 77: 2013–24.
1 Costa LJ, Brill IK, Omel J, Godby K, Kumar SK, Brown EE. 22 Martin T, Strickland S, Glenn M, et al. Phase I trial of isatuximab
Recent trends in multiple myeloma incidence and survival by age, monotherapy in the treatment of refractory multiple myeloma.
race, and ethnicity in the United States. Blood Adv 2017; 1: 282–87. Blood Cancer J 2019; 9: 41.
2 Siegel DS, Dimopoulos MA, Ludwig H, et al. Improvement in 23 Dimopoulos M, Bringhen S, Anttila P, et al. Results from a phase II
overall survival with carfilzomib, lenalidomide, and dexamethasone study of isatuximab as a single agent and in combination with
in patients with relapsed or refractory multiple myeloma. dexamethasone in patients with relapsed/refractory multiple
J Clin Oncol 2018; 36: 728–34. myeloma. Blood 2018; 132 (suppl 1): 155 (abstr).
3 Dimopoulos MA, Goldschmidt H, Niesvizky R, et al. Carfilzomib 24 Raab MS, Chatterjee M, Goldschmidt H, et al. A phase I/IIa study
or bortezomib in relapsed or refractory multiple myeloma of the CD38 antibody MOR202 alone and in combination with
(ENDEAVOR): an interim overall survival analysis of an open-label, pomalidomide or lenalidomide in patients with relapsed or
randomised, phase 3 trial. Lancet Oncol 2017; 18: 1327–37. refractory multiple myeloma. Blood 2016; 128 (suppl): 1152 (abstr).
4 Moreau P, Masszi T, Grzasko N, et al. Oral ixazomib, lenalidomide, 25 Siegel DS, Martin T, Wang M, et al. A phase 2 study of single-agent
and dexamethasone for multiple myeloma. N Engl J Med 2016; carfilzomib (PX-171-003-A1) in patients with relapsed and refractory
374: 1621–34. multiple myeloma. Blood 2012; 120: 2817–25.
5 Kumar SK, Lee JH, Lahuerta JJ, et al. Risk of progression and survival 26 Richardson PG, Baz R, Wang M, et al. Phase 1 study of twice-weekly
in multiple myeloma relapsing after therapy with IMiDs and ixazomib, an oral proteasome inhibitor, in relapsed/refractory
bortezomib: a multicenter international myeloma working group multiple myeloma patients. Blood 2014; 124: 1038–46.
study. Leukemia 2012; 26: 149–57. 27 Usmani SZ, Khan I, Chiu C, et al. Deep sustained response to
6 Usmani S, Ahmadi T, Ng Y, et al. Analysis of real-world data on daratumumab monotherapy associated with T-cell expansion in
overall survival in multiple myeloma patients with ≥3 prior lines triple refractory myeloma. Exp Hematol Oncol 2018; 7: 3.
of therapy including a proteasome inhibitor (PI) and an 28 Szabo AG, Minnema MC, Nahi H, Plesner T. Long-lasting
immunomodulatory drug (IMiD), or double refractory to a PI remissions for myeloma patients on daratumumab therapy from
and an IMiD. Oncologist 2016; 21: 1355–61. the GEN501 and GEN503 trials. Blood 2018;
7 Syed YY. Daratumumab: a review in combination therapy for 132 (suppl 1): 3308 (abstr).
transplant-ineligible newly diagnosed multiple myeloma. Drugs 29 Voorhees PM, Weiss B, Usmani S, et al. Management of infusion-
2019; 79: 447–54. related reactions following daratumumab monotherapy in patients
8 Krejcik J, Casneuf T, Nijhof IS, et al. Daratumumab depletes with at least 3 lines of prior therapy or double refractory multiple
CD38+ immune-regulatory cells, promotes T-cell expansion, and myeloma (MM): 54767414MMY2002 (Sirius). Blood 2015;
skews T-cell repertoire in multiple myeloma. Blood 2016; 128: 384–94. 126 (suppl): 1829 (abstr).
9 Adams HC 3rd, Stevenaert F, Krejcik J, et al. High-parameter mass 30 Dimopoulos MA, Oriol A, Nahi H, et al. Daratumumab,
cytometry evaluation of relapsed/refractory multiple myeloma lenalidomide, and dexamethasone for multiple myeloma.
patients treated with daratumumab demonstrates immune N Engl J Med 2016; 375: 1319–31.
modulation as a novel mechanism of action. Cytometry A 2019; 31 Palumbo A, Chanan-Khan A, Weisel K, et al. Daratumumab,
95: 279–89. bortezomib, and dexamethasone for multiple myeloma.
10 Marlein CR, Piddock RE, Mistry JJ, et al. CD38-driven N Engl J Med 2016; 375: 754–66.
mitochondrial trafficking promotes bioenergetic plasticity in 32 Moreau P, Attal M, Hulin C, et al. Bortezomib, thalidomide, and
multiple myeloma. Cancer Res 2019; 79: 2285–97. dexamethasone with or without daratumumab before and after
11 Lokhorst HM, Plesner T, Laubach JP, et al. Targeting CD38 with autologous stem-cell transplantation for newly diagnosed multiple
daratumumab monotherapy in multiple myeloma. N Engl J Med myeloma (CASSIOPEIA): a randomised, open-label, phase 3 study.
2015; 373: 1207–19. Lancet 2019; 394: 29–38.
12 Lonial S, Weiss BM, Usmani S, et al. Daratumumab monotherapy 33 Casneuf T, Xu XS, Adams HC 3rd, et al. Effects of daratumumab on
in patients with treatment-refractory multiple myeloma (SIRIUS): natural killer cells and impact on clinical outcomes in relapsed
an open-label, randomised, phase 2 trial. Lancet 2016; 387: 1551–60. refractory multiple myeloma. Blood Advances 2017; 1: 2105–14.
13 Usmani SZ, Weiss BM, Plesner T, et al. Clinical efficacy of 34 Chari A, Lonial S, Mark TM, et al. Results of an early access
daratumumab monotherapy in patients with heavily pretreated treatment protocol of daratumumab in United States patients with
relapsed or refractory multiple myeloma. Blood 2016; 128: 37–44. relapsed or refractory multiple myeloma. Cancer 2018; 124: 4342–49.
14 Rajkumar SV, Harousseau JL, Durie B, et al. Consensus 35 Jullien M, Trudel S, Tessoulin B, et al. Single-agent daratumumab
recommendations for the uniform reporting of clinical trials: report in very advanced relapsed and refractory multiple myeloma
of the International Myeloma Workshop Consensus Panel 1. patients: a real-life single-center retrospective study. Ann Hematol
Blood 2011; 117: 4691–95. 2019; 98: 1435–40.
15 US Department of Health and Human Services, National Institutes
of Health, National Cancer Institute. Common Terminology Criteria
for Adverse Events (CTCAE). Version 4.036/14/2010, 2010.
http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_
QuickReference_5x7.pdf (accessed May 11, 2014).
www.thelancet.com/haematology Vol 7 June 2020 e455
Downloaded for Anonymous User (n/a) at Cadila Pharmaceuticals Ltd from ClinicalKey.com by Elsevier on August 07, 2020.
For personal use only. No other uses without permission. Copyright ©2020. Elsevier Inc. All rights reserved.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pharmacology IDocument197 pagesPharmacology IHampson Malekano50% (2)
- COVID-19 Control in China During Mass PopulationDocument3 pagesCOVID-19 Control in China During Mass Populationbhat LibraryNo ratings yet
- Coronavirus: A New Coronavirus Associated With Human Respiratory Disease in ChinaDocument23 pagesCoronavirus: A New Coronavirus Associated With Human Respiratory Disease in Chinabhat LibraryNo ratings yet
- Nursery GradenDocument36 pagesNursery Gradenbhat LibraryNo ratings yet
- Iron Deficiency Anemia PDFDocument61 pagesIron Deficiency Anemia PDFbhat Library100% (1)
- Koha PresentationDocument36 pagesKoha Presentationbhat LibraryNo ratings yet
- KohaManual GOOD PDFDocument949 pagesKohaManual GOOD PDFbhat LibraryNo ratings yet
- 03-KOHA Overview & FeaturesDocument34 pages03-KOHA Overview & Featuresnitika gargNo ratings yet
- Over Sweat or DiaphoresisDocument5 pagesOver Sweat or DiaphoresisSiddiqur RahmanNo ratings yet
- Pharmacology TerminologyDocument4 pagesPharmacology TerminologyNjeodo VignyNo ratings yet
- Rekap Obat Bulan November 2022Document20 pagesRekap Obat Bulan November 2022nevy.kartikaNo ratings yet
- Aim and ObjectivesDocument3 pagesAim and ObjectivesDevvrat DubeyNo ratings yet
- Pharmacology in Rehabilitation 4th Edition Ciccone Test BankDocument35 pagesPharmacology in Rehabilitation 4th Edition Ciccone Test Bankalomancyheriot.o7m4100% (26)
- Pharmacognosy Assignment StarchDocument3 pagesPharmacognosy Assignment StarchAbdul BasitNo ratings yet
- Population Pharmacokinetics of Cyclosporine in Chinese Cardiac Transplant RecipientsDocument8 pagesPopulation Pharmacokinetics of Cyclosporine in Chinese Cardiac Transplant RecipientsGifari Muhammad SyabaNo ratings yet
- Data Barang Masuk 2019Document37 pagesData Barang Masuk 2019Uci AfrinaNo ratings yet
- Latihan Analisis Abc No Nama Obat Jumlah Obat Harga Satuan (RP)Document7 pagesLatihan Analisis Abc No Nama Obat Jumlah Obat Harga Satuan (RP)Nur FadliahNo ratings yet
- Introduction To Pharmaceutics: Rashid Ali Arbani Pharm-D, Mphil (Pharmaceutics) Lecturer SALUDocument14 pagesIntroduction To Pharmaceutics: Rashid Ali Arbani Pharm-D, Mphil (Pharmaceutics) Lecturer SALUSimmiNo ratings yet
- Biology Kondez 3-4pmDocument3 pagesBiology Kondez 3-4pmQuezanda OndezNo ratings yet
- Regulatory Bodies in USA, Europe, India, China and AustraliaDocument9 pagesRegulatory Bodies in USA, Europe, India, China and AustraliapriyadarshNo ratings yet
- KAPS CourseDocument12 pagesKAPS CourseUbaid Ur RehmanNo ratings yet
- Liposomal Amphotericin B Injection I.P.: AmphonexDocument5 pagesLiposomal Amphotericin B Injection I.P.: Amphonexprashant_rmlnluNo ratings yet
- Nystatinniosomes PDFDocument7 pagesNystatinniosomes PDFEufrasia Willis PakadangNo ratings yet
- E PrescribingDocument2 pagesE PrescribingDakota SimbsNo ratings yet
- Elisabeth Johanne Rook: Curriculum VitaeDocument2 pagesElisabeth Johanne Rook: Curriculum VitaeAbdullah TheNo ratings yet
- Draft Reflection Paper Dissolution Specification Generic Oral Immediate Release Products First enDocument9 pagesDraft Reflection Paper Dissolution Specification Generic Oral Immediate Release Products First enkutluuNo ratings yet
- Formulation Development of Solid Dosage FormsDocument23 pagesFormulation Development of Solid Dosage FormsRifael Satrio AdinugrohoNo ratings yet
- Unit 2 Pharmacology NotesDocument3 pagesUnit 2 Pharmacology Notessalted fishNo ratings yet
- Siap Print Untuk SimulasiDocument3 pagesSiap Print Untuk SimulasiRossa patria NandaNo ratings yet
- Pharmacokinetics - DrdhritiDocument83 pagesPharmacokinetics - Drdhritidbrahma100% (1)
- 7 - DS SATK - Zonal Change in Address 1.2Document2 pages7 - DS SATK - Zonal Change in Address 1.2MCBI AuditorNo ratings yet
- Top 200 Pharmaceuticals 2021V2Document1 pageTop 200 Pharmaceuticals 2021V2Amin AminiradNo ratings yet
- Formularium RSBD 2022 Fix EditedDocument152 pagesFormularium RSBD 2022 Fix EditedInstalasi Farmasi RSBDNo ratings yet
- Algesia: 37.5 MG / 325 MG Film-Coated TABLET AnalgesicDocument1 pageAlgesia: 37.5 MG / 325 MG Film-Coated TABLET AnalgesicEsel WazowskiNo ratings yet
- HPL PharmaDocument70 pagesHPL PharmaDipali ManjuchaNo ratings yet
- Question Bank of Pharmaceutics I: Multiple Choice Questions (1 Marks Each)Document6 pagesQuestion Bank of Pharmaceutics I: Multiple Choice Questions (1 Marks Each)Khushboo Dhaval KatharotiyaNo ratings yet
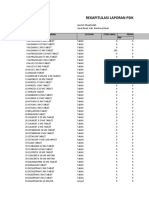
- Rekapitulasi Laporan Psikotropika: NO Nama Satuan Stok Awal Pemasukan PBFDocument8 pagesRekapitulasi Laporan Psikotropika: NO Nama Satuan Stok Awal Pemasukan PBFFajarRachmadiNo ratings yet