Professional Documents
Culture Documents
Providing Care For Infants Born at Home: Policy Statement
Uploaded by
KenMOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Providing Care For Infants Born at Home: Policy Statement
Uploaded by
KenMCopyright:
Available Formats
POLICY STATEMENT Organizational Principles to Guide and Define the Child Health
Care System and/or Improve the Health of all Children
Providing Care for Infants Born
at Home
Kristi Watterberg, MD, FAAP, COMMITTEE ON FETUS AND NEWBORN
The American Academy of Pediatrics (AAP) believes that current data show abstract
that hospitals and accredited birth centers are the safest settings for birth in
the United States. The AAP does not recommend planned home birth, which
Department of Pediatrics, The University of New Mexico, Albuquerque,
has been reported to be associated with a twofold to threefold increase in New Mexico
infant mortality in the United States. The AAP recognizes that women may
Policy statements from the American Academy of Pediatrics benefit
choose to plan a home birth. This statement is intended to help pediatricians from expertise and resources of liaisons and internal (AAP) and
external reviewers. However, policy statements from the American
provide constructive, informed counsel to women considering home birth Academy of Pediatrics may not reflect the views of the liaisons or the
while retaining their role as child advocates and to summarize appropriate organizations or government agencies that they represent.
care for newborn infants born at home that is consistent with care provided Dr Watterberg was responsible for revising and updating the draft
and responding to all suggestions from internal and external
for infants born in a medical care facility. Regardless of the circumstances of reviewers as well as the Board of Directors; and she approved the
his or her birth, including location, every newborn infant deserves health care final manuscript as submitted.
consistent with that highlighted in this statement, which is more completely The guidance in this statement does not indicate an exclusive course
of treatment or serve as a standard of medical care. Variations, taking
described in other publications from the AAP, including Guidelines for into account individual circumstances, may be appropriate.
Perinatal Care and the Textbook of Neonatal Resuscitation. All health care
All policy statements from the American Academy of Pediatrics
clinicians and institutions should promote communications and automatically expire 5 years after publication unless reaffirmed,
revised, or retired at or before that time.
understanding on the basis of professional interaction and mutual respect.
This document is copyrighted and is property of the American
Academy of Pediatrics and its Board of Directors. All authors have filed
conflict of interest statements with the American Academy of
Pediatrics. Any conflicts have been resolved through a process
INTRODUCTION approved by the Board of Directors. The American Academy of
Pediatrics has neither solicited nor accepted any commercial
Women and their families may desire a home birth for a variety of reasons, involvement in the development of the content of this publication.
including cultural or religious beliefs and traditions, hopes for a more DOI: https://doi.org/10.1542/peds.2020-0626
family-friendly setting, increased control of the process, and decreased Address correspondence to Kristi Watterberg, MD, FAAP. E-mail:
obstetric intervention.1 The incidence of home birth has increased over kwatterberg@salud.unm.edu
the past decade, with the largest increase occurring in white, non-Hispanic PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
women; more than 2% of births to these women now occur at home, with
Copyright © 2020 by the American Academy of Pediatrics
wide variation in incidence among states.2 However, a woman’s choice to
FINANCIAL DISCLOSURE: The author has indicated she has no financial
plan a home birth is not well supported in the United States. Problems relationships relevant to this article to disclose.
with home birth include wide variation in state laws and regulations, lack
FUNDING: No external funding.
of appropriately trained and willing providers, and lack of supporting
systems to ensure the availability of specialty consultation and timely
transport to a hospital. Geography also may adversely affect the safety of To cite: Watterberg K, AAP COMMITTEE ON FETUS AND
planned home birth because travel times longer than 15 to 20 minutes to NEWBORN. Providing Care for Infants Born at Home.
Pediatrics. 2020;145(5):e20200626
a medical facility have been associated with increased risk for adverse
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
PEDIATRICS Volume 145, number 5, May 2020:e20200626 FROM THE AMERICAN ACADEMY OF PEDIATRICS
neonatal outcomes, including and Gynecologists stated, “Although home birth should make her aware
mortality.3,4 the College believes that hospitals that some women who plan to deliver
and accredited birth centers are the at home will need transfer to
Planned home birth in the
safest settings for birth, each woman a hospital before birth because of
United States has previously been
has the right to make a medically unanticipated complications. This
reported to be associated with
informed decision about delivery.”11 percentage varies widely among
a twofold to threefold increase in
In addition, “Women inquiring about reports, from approximately 10% to
perinatal (fetal or newborn) death
planned home birth should be 40%, with a higher transfer rate for
or an absolute risk increase of
informed of its risks and benefits primiparous women.10,13 The mother
approximately 1 to 2 deaths per
based on recent evidence.”11 In the should be encouraged to see transfer
1000 live births.5–7 These findings
statement, the authors reviewed to a hospital not as a failure of the
were recently confirmed in
appropriate candidates for home home birth but rather as a success of
a population-based study by using
birth and health care system the system to provide a healthy
birth certificates with information
components “critical to reducing outcome for both mother and infant.
on intended place of birth as well as
perinatal mortality rates and
actual place of birth, permitting Care of the newborn infant born at
achieving favorable home birth
analysis of birth outcomes after home is a particularly important topic
outcomes” (Table 1).
intrapartum transfer to the hospital.8 because infants born at home are
This study also confirmed previous If requested, pediatric health care cared for outside the safeguards of
findings that infants born at home providers in the United States should the systems-based protocols required
in the United States have an be prepared to provide constructive, of hospitals and birthing centers,
increased incidence of low Apgar informed counsel to women placing a larger burden on health care
scores and of neonatal seizures.5,6 considering home birth while providers attending home births to
There may be an irreducible retaining their role as child advocates remember and perform all
minimum increase in adverse in assessing whether the situation is components of assessment and care
outcomes with planned home births, appropriate to support a planned of the newborn infant. To assist
even in a well-integrated health care home birth (Table 1). In addition to providers, this policy statement
system such as that in England. For apprising the expectant mother of the addresses the following specific
example, the English National increase in neonatal mortality and areas: resuscitation and evaluation of
Institute for Health and Care other neonatal complications with the newborn infant immediately after
Excellence recommends that planned home birth (Table 1), the birth and essential elements of care
practitioners “advise low-risk health care provider counseling and follow-up for the healthy term
nulliparous women that planning a pregnant woman about planned newborn infant.
to give birth in a midwifery-led unit
(freestanding or alongside) is
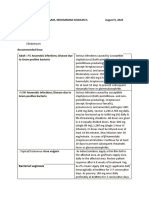
particularly suitable for them TABLE 1 Planned Home Birth Considerations
because the rate of interventions is Potential candidate for home birth
lower and the outcome for the • Absence of preexisting maternal disease
• Absence of significant disease arising during the pregnancy
baby is no different compared with
• A gestation of 37 1 0/7 to 41 1 6/7 weeks
an obstetric unit. Explain that if • A singleton fetus estimated to be appropriate for gestational age
they plan birth at home there is • A cephalic presentation
a small increase in the risk of an • Labor that is spontaneous or induced as an outpatient
adverse outcome for the baby.”9 Reported risks to the newborn associated with planned home birth in the United States
• Increased fetal and/or neonatal mortality5–8
This advice is based on the
• Increased incidence of neonatal seizures5,6,8
Birthplace in England study, which • Higher incidence of an Apgar score ,4 at 5 min5,6,8
revealed an increase in composite Systems needed to support planned home birth
adverse outcomes of intrapartum • The availability of a physician or a midwife certified by the American Midwifery Certification Board
stillbirths and early neonatal deaths, (or its predecessor organizations) or whose education and licensure meet the International
Confederation of Midwives Global Standards for Midwifery Education practicing within an
neonatal encephalopathy, meconium
integrated and regulated health system
aspiration syndrome, brachial plexus • Attendance by at least 2 care providers, one of whom is an appropriately trained individual (see
injury, and fractured humerus or text) whose primary responsibility is the care of the newborn infant
clavicle.10 • Availability of appropriate equipment for neonatal resuscitation12
• Ready access to medical consultation
In a recent position statement, the • Access to safe and timely transport to a nearby hospital with a preexisting arrangement
Committee on Obstetric Practice of As stated in Guidelines for Perinatal Care, fetal malpresentation, multiple gestation, and previous cesarean delivery are
the American College of Obstetricians considered absolute contraindications to planned home birth.
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
2 FROM THE AMERICAN ACADEMY OF PEDIATRICS
ASSESSMENT, RESUSCITATION, AND be monitored closely in the conditions associated with
CARE OF THE NEWBORN INFANT transitional period. Temperature, prematurity, including respiratory
IMMEDIATELY AFTER BIRTH heart rate, skin color, peripheral distress, poor feeding,
As recommended by the American circulation, respiration, level of hypoglycemia, and
Academy of Pediatrics (AAP) and consciousness, tone, and activity hyperbilirubinemia.
the American Heart Association, should be monitored and recorded at • Monitoring for early-onset sepsis:
there should be 2 care providers least once every 30 minutes until the As recommended by the Centers
present at every birth, at least 1 of infant’s condition has remained stable for Disease Control and
whom has the primary for 2 hours. Infants who receive Prevention and the AAP, all
responsibility to care for the extensive resuscitation (eg, positive- pregnant women should be
newborn infant.12 Situations in pressure ventilation for more than 30 screened for group B
which both the mother and the to 60 seconds12) should be Streptococcus colonization at 35
newborn infant simultaneously transferred to a medical facility for to 37 weeks’ gestation.19 Women
require urgent attention are close monitoring and evaluation. who are colonized should be
infrequent but will, nonetheless, Additionally, any infant who has given an intrapartum antibiotic
occur. Thus, of the 2 care providers respiratory distress, continued (penicillin, ampicillin, or
who should attend each birth, at least cyanosis, or other signs of illness cefazolin) at least 4 hours before
1 should have the appropriate should be immediately transferred to delivery. If the mother has received
training, skills, and equipment to a medical facility. this intrapartum treatment and
perform a full resuscitation of the both she and her newborn infant
infant in accordance with the CARE OF THE NEWBORN INFANT remain asymptomatic, they can
principles of the Neonatal remain at home if the infant can be
Subsequent newborn care should
Resuscitation Program.12,14 To observed frequently by an
adhere to that described in Guidelines
facilitate obtaining emergency experienced and knowledgeable
for Perinatal Care as well as the AAP
assistance when needed, the health care provider.20 If the
statement regarding care of the well
operational integrity of the telephone mother shows signs of
newborn infant.15–17 Although
or other communication system intraamniotic infection
a comprehensive review of these
should be tested before the delivery (chorioamnionitis) but the infant
guidelines would be far too lengthy to
(as should every other piece of appears completely well, the
include in this statement, a few
medical equipment), and the weather infant also can remain at home as
practice points are worthy of specific
should be monitored. In addition, long as he or she is observed
mention.
access to safe and timely transport to frequently by an experienced and
a medical facility should be available, • Transitional care (first 4–8 hours): knowledgeable health care
and a previous arrangement with that The infant should be kept warm provider. A quantitative estimate
facility should be in place. Examples and should undergo a detailed of the risk of newborn infection
of guidelines and forms for maternal physical examination that includes (as can be obtained from use of
and infant transport, developed by an assessment of gestational age the sepsis risk calculator at https://
the Home Birth Summit organization, and intrauterine growth status as neonatalsepsiscalculator.
can be found at http://www. well as a comprehensive risk kaiserpermanente.org) may help
homebirthsummit.org. assessment for neonatal conditions guide the decision to transfer the
that require additional monitoring infant to a medical facility.21 If the
Care of the newborn infant or intervention. Temperature, heart infant does not appear completely
immediately after delivery should and respiratory rates, skin color, well, the infant should be
adhere to practices described in peripheral circulation, respiration, transferred rapidly to a medical
Guidelines for Perinatal Care15,16 and level of consciousness, tone, and facility for further evaluation and
should include provision of warmth, activity should be monitored and monitoring in accordance with
initiation of appropriate resuscitation recorded at least once every AAP guidelines.20
measures, and assignment of Apgar 30 minutes until the infant’s
• Glucose screening: Infants who
scores. Although skin-to-skin contact condition is considered normal and
have intrauterine growth
with the mother is the most effective has remained stable for 2 hours. A
restriction or whose mothers
way to provide warmth, portable newborn infant who is determined
warming pads should be available in to be ,37 weeks’ gestational age have diabetes should be delivered
case a newborn infant requires by physical assessment18 should be in a hospital or birthing center
resuscitation and cannot be placed on transferred to a medical facility for because of the increased risk of
the mother’s chest. The infant should continuing observation for hypoglycemia and other neonatal
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
PEDIATRICS Volume 145, number 5, May 2020 3
complications. If, after birth, an early days of breastfeeding. found at https://wisconsinshine.
infant is discovered to be small or Nomograms providing hour- org/home-births/.25,26
large for gestational age or an specific expected weight loss in the • Provision of follow-up care:
infant has required resuscitation, first postnatal week can be found at Documentation of prenatal care,
he or she should be screened for https://www.newbornweight.org/. delivery, and immediate postnatal
hypoglycemia, as outlined in the • Screening for hyperbilirubinemia: course, in addition to prompt,
AAP statement.22 If hypoglycemia Infants whose mothers are Rh- comprehensive communication
(glucose level ,45 mg/dL) is negative should have cord blood with the follow-up care provider, is
identified and persists after sent for a Coombs direct antibody essential. Completion of forms such
feeding, the infant should be test; if the mother’s blood type is O as those found on the AAP Bright
transferred promptly to a medical and she is Rh-positive, the cord Futures Web site (https://
facility for continuing evaluation blood may be tested for the infant’s brightfutures.aap.org) can help
and treatment. blood type and sent for a direct provide such communication. A
• Eye prophylaxis: every newborn antibody test, but it is not required, knowledgeable and experienced
infant should receive prophylaxis provided that there is appropriate health care professional should
against gonococcal ophthalmia surveillance, risk assessment, and examine all infants within 24 hours
neonatorum, as directed by local follow-up.24 All newborn infants of birth and subsequently within
laws and regulations. should be assessed for risk of 48 hours of that first evaluation.
• Vitamin K: Every newborn infant hyperbilirubinemia and undergo The initial follow-up visit should
should receive a single parenteral bilirubin screening between 24 and include infant weight and physical
dose of vitamin K1 oxide 48 hours after birth. The bilirubin examination, especially for jaundice
(phytonadione [0.5–1 mg]) to value should be plotted on the and hydration. If the mother is
prevent vitamin K–dependent hour-specific nomogram to breastfeeding, the visit should
hemorrhagic disease of the determine the risk of severe include evaluation of any maternal
newborn. Oral administration of hyperbilirubinemia and the need history of breast problems (eg, pain
vitamin K has not been shown to be for repeat determinations.24 or engorgement), infant elimination
as efficacious as parenteral • Universal newborn screening: patterns, and a formal observed
administration for the prevention Every newborn infant should evaluation of breastfeeding,
of late hemorrhagic disease. undergo universal newborn including position, latch, and milk
screening in accordance with transfer. Results of maternal and
• Hepatitis B vaccination: For all
individual state mandates. A list of neonatal laboratory tests should be
medically stable infants weighing
conditions for which screening is reviewed; clinically indicated tests,
.2000 g at birth who are born to
performed in each state is such as serum bilirubin, should be
hepatitis B surface antigen
maintained online by the National performed; and screening tests
(HBsAg)–negative mothers, the first
Newborn Screening and Genetic should be completed in accordance
dose of vaccine should be
Resource Center (available at with state regulations. The
administered within 24 hours of
http://genes-r-us.uthscsa.edu/ documentation provided by the
birth. Only single-antigen hepatitis
resources/consumer/statemap. health care professional attending
B vaccine should be used for the
htm). the birth should include whether
birth dose, following proper
tests and vaccinations usually
storage and handling requirements • Hearing screening: the newborn
performed as part of hospital
for immunizations. Infants born to infant’s initial caregiver should
protocols have been completed or
mothers who are HBsAg-positive or document arrangements for
scheduled.
whose HBsAg status is unknown screening the infant’s hearing.
should also receive hepatitis B • Pulse oximetry screening:
immune globulin, as guided by Screening for congenital heart CONCLUSIONS
current recommendations.23 disease should be performed by The AAP does not recommend
• Assessment of feeding: A trained using oxygen saturation testing, planned home birth. However, the
caregiver should evaluate at least 1 ideally between 24 and 48 hours’ AAP recognizes that women may
session of breastfeeding, including postnatal age. Earlier screening can choose to plan a home birth. The AAP
observation of position, latch, and be performed, although the concurs with the American College of
milk transfer. The mother should be incidence of false-positive screen Obstetricians and Gynecologists
encouraged to record the time and results may be increased. Helpful statement that “for quality and safety
duration of each feeding, as well as information for oximetry screening reasons, the College specifically
urine and stool output, during the for planned home births can be supports the provision of care by
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
4 FROM THE AMERICAN ACADEMY OF PEDIATRICS
midwives who are certified by the Regardless of the circumstances of his Karen Marie Puopolo, MD, PhD, FAAP
American Midwifery Certification or her birth, including location, every Dan L. Stewart, MD, FAAP
RADM Wanda D. Barfield, MD, MPH, FAAP
Board (or its predecessor newborn infant deserves health care
organizations) or whose education that adheres to the guidelines
and licensure meet the International highlighted in this statement and LIAISONS
Confederation of Midwives Global more completely described in other Yasser El-Sayed, MD – American College of
Standards for Midwifery Education. AAP publications.15–17 Continuing Obstetricians and Gynecologists
The College does not support efforts by all health care clinicians Erin L. Keels, DNP, APRN, NNP-BC – National
Association of Neonatal Nurses
provision of care by midwives who do and institutions should promote
Meredith Mowitz, MD, MS, FAAP – Section on
not meet these standards.”11 communications and understanding Neonatal Perinatal Medicine Trainees and
on the basis of professional Early Career Neonatologists
In the case of a home birth, as interaction and mutual respect. Michael Ryan Narvey, MD, FAAP – Canadian
advocates for children, the AAP Paediatric Society
recommends that provisions for the Tonse N.K. Raju, MD, DCH, FAAP – National
Institutes of Health
potential resuscitation of a depressed Kasper S. Wang, MD, FACS, FAAP – Section on
newborn infant and immediate LEAD AUTHOR Surgery
neonatal care be optimized in the Kristi Watterberg, MD, FAAP
home setting. Thus, each delivery
STAFF
should be attended by 2 care
providers, at least 1 of whom has the COMMITTEE ON FETUS AND NEWBORN, Jim Couto, MA
primary responsibility for the 2018–2019
newborn and has the appropriate James J. Cummings, MD, FAAP, Chairperson
training, skills, and equipment to Ira S. Adams-Chapman, MD, FAAP ABBREVIATIONS
perform a full resuscitation of the Susan Wright Aucott, MD, FAAP
AAP: American Academy of
Jay P. Goldsmith, MD, FAAP
infant in accordance with the Ivan L. Hand, MD, FAAP Pediatrics
principles of the Neonatal Sandra E. Juul, MD, PhD, FAAP HBsAg: hepatitis B surface antigen
Resuscitation Program.12,14 Brenda Bradley Poindexter, MD, MS, FAAP
POTENTIAL CONFLICT OF INTEREST: The author has indicated she has no potential conflicts of interest to disclose.
REFERENCES
1. Zielinski R, Ackerson K, Kane Low L. United States 2000 to 2004. J Perinatol. Available at: https://www.nice.org.uk/
Planned home birth: benefits, risks, and 2010;30(9):622–627 guidance/cg190. Accessed December 2,
opportunities. Int J Womens Health. 2018
6. Cheng YW, Snowden JM, King TL,
2015;7:361–377
Caughey AB. Selected perinatal 10. Brocklehurst P, Hardy P, Hollowell J,
2. MacDorman MF, Declercq E. Trends and outcomes associated with planned et al; Birthplace in England
characteristics of United States out-of- home births in the United States. Am Collaborative Group. Perinatal and
hospital births 2004-2014: new J Obstet Gynecol. 2013;209(4):325.e1- maternal outcomes by planned place of
information on risk status and access 325.e8 birth for healthy women with low risk
to care. Birth. 2016;43(2):116–124 7. Chang JJ, Macones GA. Birth outcomes pregnancies: the Birthplace in England
of planned home births in Missouri: national prospective cohort study. BMJ.
3. Ravelli AC, Jager KJ, de Groot MH, et al. 2011;343:d7400
a population-based study. Am
Travel time from home to hospital and
J Perinatol. 2011;28(7):529–536 11. American College of Obstetricians and
adverse perinatal outcomes in women
at term in the Netherlands. BJOG. 2011; 8. Snowden JM, Tilden EL, Snyder J, Gynecologists’ Committee on Obstetric
118(4):457–465 Quigley B, Caughey AB, Cheng YW. Practice. Committee opinion No. 669:
Planned out-of-hospital birth and birth planned home birth. Obstet Gynecol.
4. Paranjothy S, Watkins WJ, Rolfe K, et al. outcomes. N Engl J Med. 2015;373(27): 2016;128(2):e26–e31
Perinatal outcomes and travel time 2642–2653
from home to hospital: Welsh data from 12. Wyckoff MH, Aziz K, Escobedo MB, et al.
1995 to 2009. Acta Paediatr. 2014; 9. National Institute for Health and Care Part 13: neonatal resuscitation: 2015
Excellence. Intrapartum Care for American Heart Association guidelines
103(12):e522–e527
Healthy Women and Babies. London, update for cardiopulmonary
5. Malloy MH. Infant outcomes of certified United Kingdom: National Institute for resuscitation and emergency
nurse midwife attended home births: Health and Care Excellence; 2014. cardiovascular care (reprint).
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
PEDIATRICS Volume 145, number 5, May 2020 5
Pediatrics. 2015;136(suppl 2): Watterberg K, eds. Guidelines for 22. Adamkin DH; Committee on Fetus and
S196–S218 Perinatal Care, 8th ed. Elk Grove Village, Newborn. Postnatal glucose
13. Lindgren HE, Rådestad IJ, Hildingsson IL: American Academy of Pediatrics; homeostasis in late-preterm and term
IM. Transfer in planned home births in 2017:409–478 infants. Pediatrics. 2011;127(3):575–579.
Sweden–effects on the experience of Reaffirmed June 2015
17. Benitz WE; Committee on Fetus and
birth: a nationwide population-based Newborn, American Academy of 23. Committee on Infectious Diseases;
study. Sex Reprod Healthc. 2011;2(3): Pediatrics. Hospital stay for healthy Committee on Fetus and Newborn.
101–105 term newborn infants. Pediatrics. 2015; Elimination of perinatal hepatitis B:
14. American Academy of Pediatrics; 135(5):948–953 providing the first vaccine dose within
American Heart Association. Preparing 18. Ballard JL, Khoury JC, Wedig K, Wang L, 24 hours of birth. Pediatrics. 2017;
for Resuscitation. In: Wiener GM, Eilers-Walsman BL, Lipp R. New Ballard 140(3):e20171870
Zaichkin J, eds. Textbook of Neonatal Score, expanded to include extremely 24. American Academy of Pediatrics
Resuscitation, 7th ed. Elk Grove Village, premature infants. J Pediatr. 1991; Subcommittee on Hyperbilirubinemia.
IL: American Academy of Pediatrics; 119(3):417–423 Management of hyperbilirubinemia in
2016:17–32
19. Baker CJ, Byington CL, Polin RA; the newborn infant 35 or more weeks
15. American Academy of Pediatrics Committee on Infectious Diseases; of gestation [published correction
Committee on Fetus and Newborn; Committee on Fetus and Newborn. appears in Pediatrics. 2004;114(4):
American College of Obstetricians and Policy statement—recommendations 1138]. Pediatrics. 2004;114(1):297–316
Gynecologists Committee on Obstetric for the prevention of perinatal group B
Practice. Care of the Newborn. In: 25. Oster ME, Aucott SW, Glidewell J, et al.
streptococcal (GBS) disease. Pediatrics. Lessons learned from newborn
Kilpatrick SJ, Papile LA, Macones GA, 2011;128(3):611–616
Watterberg KL, eds. Guidelines for screening for critical congenital heart
Perinatal Care, 8th ed. Elk Grove Village, 20. Benitz WE, Wynn JL, Polin RA. defects. Pediatrics. 2016;137(5):
IL: American Academy of Pediatrics; Reappraisal of guidelines for e20154573
2017:347–408 management of neonates with
26. Miller KK, Vig KS, Goetz EM, Spicer G,
suspected early-onset sepsis. J Pediatr.
16. American Academy of Pediatrics Yang AJ, Hokanson JS. Pulse oximetry
2015;166(4):1070–1074
Committee on Fetus and Newborn; screening for critical congenital heart
American College of Obstetricians and 21. Kuzniewicz MW, Puopolo KM, Fischer A, disease in planned out of hospital
Gynecologists Committee on Obstetric et al. A quantitative, risk-based births and the incidence of critical
Practice. Neonatal Complications and approach to the management of congenital heart disease in the Plain
Management of High-Risk Infants. In: neonatal early-onset sepsis. JAMA community. J Perinatol. 2016;36(12):
Kilpatrick S, Papile LA, Macones G, Pediatr. 2017;171(4):365–371 1088–1091
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
6 FROM THE AMERICAN ACADEMY OF PEDIATRICS
Providing Care for Infants Born at Home
Kristi Watterberg and COMMITTEE ON FETUS AND NEWBORN
Pediatrics 2020;145;
DOI: 10.1542/peds.2020-0626 originally published online April 20, 2020;
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/145/5/e20200626
References This article cites 22 articles, 8 of which you can access for free at:
http://pediatrics.aappublications.org/content/145/5/e20200626#BIBL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Current Policy
http://www.aappublications.org/cgi/collection/current_policy
Committee on Fetus & Newborn
http://www.aappublications.org/cgi/collection/committee_on_fetus_
_newborn
Fetus/Newborn Infant
http://www.aappublications.org/cgi/collection/fetus:newborn_infant_
sub
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
Providing Care for Infants Born at Home
Kristi Watterberg and COMMITTEE ON FETUS AND NEWBORN
Pediatrics 2020;145;
DOI: 10.1542/peds.2020-0626 originally published online April 20, 2020;
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/145/5/e20200626
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 345 Park Avenue, Itasca, Illinois, 60143. Copyright © 2020
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.
Downloaded from www.aappublications.org/news at Philippines:AAP Sponsored on August 6, 2020
You might also like
- Diagnosis & ManagementDocument36 pagesDiagnosis & ManagementKenMNo ratings yet
- Cholelith MGT - 2Document33 pagesCholelith MGT - 2KenMNo ratings yet
- D-6-12 Sanaani, Mohammad Khaisar H. August 9, 2020: Bacterial VaginosisDocument4 pagesD-6-12 Sanaani, Mohammad Khaisar H. August 9, 2020: Bacterial VaginosisKenMNo ratings yet
- 5J 569 - Boarding PassDocument1 page5J 569 - Boarding PassKenMNo ratings yet
- Liver CirrhosisDocument86 pagesLiver CirrhosisKenMNo ratings yet
- Heart FailureDocument78 pagesHeart FailureKenMNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Gestational AgeDocument22 pagesGestational AgeAnushya JayendranNo ratings yet
- 2018 Non-Clinical Interventions For Reducing Unnecessary Caesarean Chen - Et - Al-2018-Cochrane - Database - of - Systematic - ReviewsDocument130 pages2018 Non-Clinical Interventions For Reducing Unnecessary Caesarean Chen - Et - Al-2018-Cochrane - Database - of - Systematic - ReviewsAli BahadırlıNo ratings yet
- Immediate Drying: Essential Intrapartum and Newborn Care (Einc)Document1 pageImmediate Drying: Essential Intrapartum and Newborn Care (Einc)Kaycee JoyNo ratings yet
- RDL Introduction STEM SarmientoDocument3 pagesRDL Introduction STEM SarmientoErik Maximus SarmientoNo ratings yet
- 12 Biology - Reproductive HealthDocument4 pages12 Biology - Reproductive HealthTanya Mishra100% (1)
- Birth PlanDocument7 pagesBirth PlanaishahakidzandraNo ratings yet
- Factors Affecting Labor.Document2 pagesFactors Affecting Labor.Salman KhanNo ratings yet
- Destiny Blevins AbortionDocument5 pagesDestiny Blevins Abortionapi-241253097No ratings yet
- Planning For Healthy PregnancyDocument31 pagesPlanning For Healthy Pregnancyafiani qonitaNo ratings yet
- DEMONSTRATION On Care of BreastDocument12 pagesDEMONSTRATION On Care of BreastRaja100% (3)
- Practice Bulletin Multifetal GestationDocument16 pagesPractice Bulletin Multifetal GestationSusana Torres0% (1)
- Indah Nurmala Sari 27 33Document8 pagesIndah Nurmala Sari 27 33Arbianus SurbaktiNo ratings yet
- PT Resp OutcomesDocument6 pagesPT Resp OutcomesHarish SudarsananNo ratings yet
- DIABETES in Pregnancy With NotesDocument84 pagesDIABETES in Pregnancy With NotesNeill CelesteNo ratings yet
- YÖKDİL Sağlık Cloze Test Soru TipiDocument6 pagesYÖKDİL Sağlık Cloze Test Soru Tipipinaryildizli01No ratings yet
- 1: Preparation For The DeliveryDocument3 pages1: Preparation For The DeliveryAngelika Padawan100% (1)
- Maternal Health and Its Influences On Child HealthDocument83 pagesMaternal Health and Its Influences On Child HealthSangpuii HmarNo ratings yet
- Breast FeedingDocument28 pagesBreast FeedingAnadh PatelNo ratings yet
- PP Bahasa Inggris Vika (Ziziphus)Document9 pagesPP Bahasa Inggris Vika (Ziziphus)Dini TaluNo ratings yet
- Leopold's ManeuverDocument3 pagesLeopold's ManeuverPekabuNo ratings yet
- Post Test - CHNDocument13 pagesPost Test - CHNNaomi VirtudazoNo ratings yet
- Copy3-Obgyn Final Base LvivtechDocument3,466 pagesCopy3-Obgyn Final Base LvivtechHart ElettNo ratings yet
- Lecture-13 Transeverse LieDocument15 pagesLecture-13 Transeverse LieMadhu Sudhan PandeyaNo ratings yet
- INTRAPARTUMDocument18 pagesINTRAPARTUMMICHELLE FACTONo ratings yet
- Breastfeeding "A Gift That Lasts A Lifetime"Document2 pagesBreastfeeding "A Gift That Lasts A Lifetime"Janine Mae MacaraigNo ratings yet
- Nursing Care During Labor and BirthDocument7 pagesNursing Care During Labor and BirthRegine VillanuevaNo ratings yet
- Prenatal Factors Influencing Growth and Development of FetusDocument15 pagesPrenatal Factors Influencing Growth and Development of FetusSrd Rch100% (1)
- Breast Pumps Flyer EN 1819-Single-Pages-A4Document6 pagesBreast Pumps Flyer EN 1819-Single-Pages-A4Rigoberto Leigue OrdoñezNo ratings yet
- Employment Form NMBI SGHDocument6 pagesEmployment Form NMBI SGHJoel GijiNo ratings yet
- 9 - Postterm PregnancyDocument22 pages9 - Postterm PregnancyMara Medina - BorleoNo ratings yet