Professional Documents
Culture Documents
Situations of Obstetric Violence From The Perspective of Puerperal Women
Uploaded by
IJAERS JOURNALOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Situations of Obstetric Violence From The Perspective of Puerperal Women
Uploaded by
IJAERS JOURNALCopyright:
Available Formats
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol-7, Issue-9, Sep- 2020]
https://dx.doi.org/10.22161/ijaers.79.14 ISSN: 2349-6495(P) | 2456-1908(O)
Situations of Obstetric Violence from the
Perspective of Puerperal Women
Genir Isidorio da Silva Santana1, Ana Catarina Torres de Lacerda2, Liniker
Scolfild Rodrigues da Silva3, Maria José dos Santos Monteiro4, Tatiane
Barbosa Soares Silva5, Gabriela Priscila Rodrigues da Silva6, Jozivalda
Venancio Caitano dos Santos7, Érika Sophia Gouveia da Silva8, Denise
Cesário de Sousa9, Anna Carollyne de Almeida Vasconcelos Silva10,
Fernanda Celiberti Soveral11
1,5,6,9ClinicalHospital (HC)/Federal University of Pernambuco (UFPE). Recife, Pernambuco, PE, Brazil.
2Nursing Department, Federal University of Pernambuco (UFPE). Recife, Pernambuco, PE, Brazil.
3Medical Sciences College (FCM)/University of Pernambuco (UPE). Recife, Pernambuco, PE, Brazil.
4,10Faculty of Human and Exact Sciences of the Sertão do São Francisco (FACESF). Recife, Pernambuco, PE, Brazil.
7Emergency Mobile Care Service (SAMU)/ Recife City Hall (PCR). Recife, Pernambuco, PE, Brazil.
8Faculty Redentor/Faculty IDE. Recife, Pernambuco, PE, Brazil. Recife, Pernambuco, PE, Brazil.
11Institute of Integral Medicine Prof. Fernando Figueiras (IMIP). Recife, Pernambuco, PE, Brazil.
Abstract— To investigate situations of obstetric violence in the perception of puerperal women in a
teaching hospital. Descriptive study, with a qualitative approach. Data collection used a semi-structured
interview with 17 puerperal women. The puerperal women’s statements were transcribed and analyzed
through content analysis in the thematic modality proposed by Bardin. From the analysis of the statements,
four thematic categories emerged: 1) Disrespect for the parturient, 2) Obstetric violence, 3) Violence
revealed, 4) Unknown violence. The study revealed the need for changes in childbirth care to make is more
welcoming, with pregnant women’s protagonism, respecting their rights constituted by laws, and using
good obstetric practices for a humanized childbirth free of violence.
Keywords— Gender-Based Violence, Midwifery, Nursing, Qualitative Research, Women’s Health.
I. INTRODUCTION subjected to seemingly safe norms and interventions,
The historical analysis of how women experienced their without her consent or oppression, fear, shame and because
deliveries shows that there were changes in the whole of the idea that the hospital environment would provide the
process, with records showing that, in ancient civilizations, best care for her and her baby. Assisted by unknown
women performed their deliveries alone, at most, people, away from their relatives and belongings, without
accompanied by a maternal figure who offered them the right of choices, contributing to maternal and neonatal
protection, which would later come to fruition as risks [1].
midwives. This fact culturally sedimented the delivery in To improve obstetric care, the World Health
the home itself, happening as a natural, private and family Organization (WHO) published a handbook in 1996, with
process in which the woman was the protagonist of the practices based on scientific evidence called good practices
parturition process [1]. for childbirth care. Ambulation, spray bath and immersion,
Since the 1940s, the institutionalization of childbirth lumbosacral massage, muscle relaxation, vertical positions,
intensified, aiming to reduce maternal and neonatal horse method or pelvic movement, aromatherapy, music
mortality and, at the end of the last century, more than 90% therapy, Swiss ball, breathing exercises and the presence of
of deliveries occurred in the hospital environment. The a companion chosen by the parturient act in reducing the
woman ceased to hold the lead role of her labor, being period of labor, effectively reduce pain and relieve anxiety,
www.ijaers.com Page | 109
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol-7, Issue-9, Sep- 2020]
https://dx.doi.org/10.22161/ijaers.79.14 ISSN: 2349-6495(P) | 2456-1908(O)
bringing a physical and psychological comfort to the II. METHODS
woman. Thus, they should be inserted in childbirth care This is a descriptive study with a qualitative approach,
[2,3]. conducted in a university hospital in Recife/PE, Brazil. The
On the other hand, procedures such as enema, participants were 17 puerperal women, aged over 18 years,
trichotomy, prophylactic venous catheterization, supine in the immediate postpartum period. Submitted to normal
and lithotomic position with or without stirrups, rectal delivery or cesarean section of the said hospital and
examination, routine uterine washing, prolonged and hospitalized in the rooming-in accommodation at the time
directed pull effort, massage and distension of the of research. Those with psychiatric disorders and who gave
perineum, parenteral ergomethrin and use of radiographic birth to stillborn fetuses were excluded. The number of
pelvimetry should not be used because they are harmful or interviewees was determined by theoretical saturation
ineffective. Early amniotomy, maneuvers related to during data collection and analysis. The theoretical
perineum protection and cephalic pole management, active saturation was identified from the non-occurrence of new
manipulation of the fetus, early clamping of the umbilical information, by the decreasing yield during the content
cord, fasting, routine episiotomy and active management of analysis performed [7].
oxytocin labor should be carefully used, since there is no For information collection, a semi-structured interview
scientific evidence for their use [4]. guide was used, containing the guiding questions: Can you
However, even with scientific evidence supporting the tell how your labor and delivery was? What did you find
implementation of good practices during labor and more difficult about your delivery? Have you ever felt
delivery, many women experience situations of violence. disrespected or mistreated? This guide also had
Exposed through negligence in care, social discrimination, sociodemographic and obstetric issues collected from
verbal aggression and physical violence, including the non- medical records. Data collection occurred between April
use of analgesia when indicated, inadequate use of and September 2015. An MP3 recorder was used to record
technology, with unnecessary interventions and procedures the interviews, simultaneously with data collection.
before the scientific evidence of the moment, causing The interviews were fully transcribed. Information was
interventions with potential risks and sequelae [5]. analyzed using the content analysis in the thematic
Although in Brazil there is no specific definition of modality, proposed by Bardin [8]. Constituting the
obstetric violence, it is characterized by the appropriation following thematic categories: disrespect for the parturient,
of the body and reproductive processes of women by health obstetric violence, violence revealed and unknown
professionals, through dehumanized treatment, abuse of violence. The thematic categories were analyzed and
medicalization and “pathologization” of natural processes, interpreted according to the theoretical framework of
causing the loss of autonomy and ability to freely decide childbirth care anchored in the World Health Organization
on their bodies and sexuality, negatively affecting the [WHO] (1996) [2]. Data related to sample characterization
empowerment of their life and their choices [6]. were typed and analyzed in the Software SPSS (Statistical
Thus, the woman has the right to choose the type of Package for the Social Sciences), version 21.0, using
delivery, intervention and procedure to be performed, to descriptive analysis techniques.
know their reasons, risks and benefits, to know the The research occurred after approval by the Research
possibilities of analgesia and to choose the place of Ethics Committee (CEP) at the Health Sciences Center
delivery and a companion. These measures should be taken (CCS) of the Federal University of Pernambuco (UFPE),
consciously, taking into account maternal and fetal well- (CAAE: 40024514.5.0000.5208) and signing of the
being and the autonomy of the parturient [4-6]. Informed Consent Form (ICF) by the interviewees. To
Due to the frequent discussions on the theme of social maintain anonymity, the interviews were identified by
relevance, as it constantly occurs, implying violation of the alphanumeric codes, using the letter P and subsequent
rights of parturients, evidencing the need for improvement interview number, from 1 to 17. The study respected the
in the attention given to delivery and birth, highlighting the formal requirements contained in national and international
importance of the active participation of women in this standards regulating researches involving human beings.
context. Thus, this study sought to investigate situations of
obstetric violence from the perspective of puerperal women III. RESULTS
at a teaching hospital.
The interviewees were between 18 and 44 years old,
with an average age of 26.29 years, 70.6% were from the
www.ijaers.com Page | 110
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol-7, Issue-9, Sep- 2020]
https://dx.doi.org/10.22161/ijaers.79.14 ISSN: 2349-6495(P) | 2456-1908(O)
Metropolitan Region of Recife and 29.4% from other cities migrating from one hospital to another, so I felt
in inland Recife. The majority lived in consensual union disrespected (P9).
(52.9%), only 29.4% were unmarried and 17.6% were The parturients’ statements showed that the non-respect
married. Regarding education, 17.6% had incomplete of the woman’s choice over her companion during labor
elementary school, 17.6% had complete elementary school, and delivery contributed negatively to the delivery process.
23.5% had incomplete high school, 11.8% had complete Only the female companion’s was allowed in some cases,
high school, 5.9% had incomplete higher education and and her presence was limited only to labor, in a few cases,
23.5% had complete higher education. About the during vaginal delivery. In cesarean section, this right was
profession/occupation, 58.8% were housewives and 41.2% denied to pregnant women, whose main argument was the
had paid activity. Regarding monthly family income, 5.9% lack of adequate clothing: One, I don’t know if she was a
lived with less than one minimum wage, 47.1% with a student too or a nurse, I don’t know, I just know I asked if
minimum wage, 35.3% with two minimum wages and she (mother) could get in, so she said, “There’s no cloth
11.8% with three minimum wages. for me and I work here, imagine for a companion.” Then
Obstetric data, number of pregnancies ranged from one my mother did not get in, I entered the delivery room alone
to five (mean=1.94), to one to four deliveries (mean= (P17). At no point did he (husband) come in to see me
1.71), abortions from zero to one (mean= 0.24). because they did not let him (P11). My mother wanted to
Gestational age ranged from 35 to 41 weeks (mean=39.12). watch the birth... The boy’s father also stayed outside
The number of normal deliveries was 76.5%, with the because he could not watch, because they had no clothes
remaining 23.5% submitted to cesarean section. The for either of them (P13).
university hospital was the first choice for 41.2% of The following statements reveal the disrespect to the
women. The presence of a companion was reported by woman’s right to have her privacy preserved in the place of
52.9% of the women, 52.9% walked during labor. All delivery, being subjected to several procedures with the
patients who gave birth by normal route stated that they presence of several people, without her prior consent,
were in lithotomy. without the right of refusal, exposing her, making her the
The use of oxytocin occurred in 76.5% of deliveries, object of learning, violating her intimacy: Two (students),
amniotomy was performed in 52.9% of the women, 70.6% the doctors were all near me, the boss and the doctors, they
of the interviewees remained fasting throughout the labor, were all over me (P2). .. Many academic doctors, interns,
17.6% used misoprostol and 52.9% received guidance on everyone around me, and we are already nervous (P15).
the procedures performed. The partogram was opened There were about ten people in the delivery room (P13).
during labor and delivery care of only 17.6% of the Many doctors came up to me, examined me and everything
women. Care was provided by obstetricians (94.1%) and (P8).
by obstetric nurses (5.9%). Although known as an effective method in relieving
From the speech analysis, four thematic categories pain and anxiety during labor, simple and low-cost therapy,
emerged: 1) Disrespect for the parturient, 2) Obstetric non-pharmacological practices were not used, or were
violence, 3) Violence revealed, 4) Unknown violence. inadequate, hindering labor, coping with pain, generating a
Disrespect for the parturient sense of death: They just told me to sit on the ball, there is
no professional... what to do on the ball? Do I sit down?
Good obstetric practices guide professionals to what
Do I jump? Do I walk? I was in so much pain that I do not
should and should not be done during labor. Some of these
even like to remember. (Crying) This was the whole night,
practices were not considered. Starting with the pilgrimage
the pain increasing and they only came to make the touch
while seeking a place that leads pregnant women feel
exam (P11). I do not ever want to have a child in my life
anxious and disrespected: First I went there, I thought it
again. Oh, my God! It was a terrible feeling! I thought I
was going to be there, the birth... Then they transferred me
was going to die there. There was so much pain, so much
to another hospital, then there was no duty, no, it was full,
pain. I did not know what that pain was like, first son. You
then I came back again... And they sent me to (another
do not know what it is like, you get lost. Because you think
maternity), so I was hospitalized there. Then the girl came
it is death, that pain, but I got it, I do not know how, but I
and said that I was going to be transferred to another
did it (P17).
hospital because there was no anesthesiologist, then they
sent me here (P5). I got there, they had no place for me Another practice reported was the restriction of food
there (P6). The hardest part was the uncertainty of and liquids imposed by professionals, a procedure that was
not questioned by pregnant women. Regardless of the
www.ijaers.com Page | 111
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol-7, Issue-9, Sep- 2020]
https://dx.doi.org/10.22161/ijaers.79.14 ISSN: 2349-6495(P) | 2456-1908(O)
delivery route, the woman’s desire and the labor stage, the several times this, suffering was immense, the physical
restriction still extended to the first two hours after vaginal pain was inexplicable, unforgettable (p15).
delivery: Very hungry, it was very difficult for me ... only Violence revealed
IV, it was very difficult. Here, I think that is where I had
In these discourses, the report of the excess of
the most accurate guidance that I could even eat, but
procedures configured as maltreatment and obstetric
eating could make me suffer more... Then I followed what
violence timidly begins to emerge. In this speech, we can
they told me (P9). Then I asked to drink water, she
perceive the team directed only to the care of the fetus, not
(professional) said I could not, then I put just a little bit of
taking into account the feelings and emotions of the
water on the lips and that was it (P12). I could not eat. I
parturient: The team that met me was terrible, because they
only ate two hours after delivery when I got to the
mistreated me, they were careless, because you’re out
infirmary (P14).
there screaming, bleeding and they’re just listening to your
Obstetric violence baby’s heart and you don’t count, don’t you?- cry -... I was
Vaginal touch is part of the obstetric evaluation, but so angry. You have to learn more, go back to school,
should not be performed repeatedly or frequently, because in addition to making money, you have to love
especially by more than one professional, being important what you do, because first of all I think you have to have
to guide the woman on the examination, request her love and compassion for the patients... You are inhumane.
authorization and perform in order to minimize the It was perverse, it is like you are nobody, that was my
discomfort of the procedure: They (professionals) always anguish... I was already calling him (husband): Look,
came to make the touch test (P1). There came another one come get me, because, if I have to die, I would rather die at
to make the touch. Then I said: Are you making the touch home (P11).
test, I cannot take it anymore... It was hurting. It is Taking the pregnant woman to the delivery room and
horrible. (P7). Finger has no camera, so they were in not waiting for the physiological time for birth entails a
doubt, one got in, got out, another got in, got out, one cascade of interventions, transforming the natural moment
passed to another three, it seems it is two, four: You are into something painful, the parturient has no autonomy
playing with my uterus! (P11). over her body, feels violated, with psychological sequelae
The use of the oxytocin synthetic hormone to correct or that need to be worked to reduce the damage in future
accelerate the pattern of uterine contractility during labor pregnancies: My problem was in the delivery room, which
was used deliberately, not respecting the physiology of characterized obstetric violence... let’ give her more IV...
childbirth, with absence of pain as the main justification Open my vagina and I force to see if the baby crowned and
for its indication: They gave me an IV, a medicine (P8). I nothing, then the obstetrician decided they would do the
was given an IV to speed up the pain. (P10). I was not in following: “I’m going to press your belly, it is going to
pain, then the girl gave me an IV, so I started to feel pain, open your vagina, you are going to push... Then the doctor
you know? (P7). They started putting medication on me to was pressing here, here in the belly... Then he pressed a
get to contractions (P3). They gave me an IV (P16). lot, and his physical condition so strong, a lot of force,
Routine amniotomy should not be performed in right?... Suffering this violence, all over my body, he did
obstetric practice, since there is no scientific evidence that that several times and nothing. Then the doctor grabbed
it improves outcomes, yet it is still a very common practice the forceps and gave me more IV ... For me, it was
in obstetrics as evidenced in the following reports: (The abnormal, it was not a normal delivery, my baby was
doctor) said I was five centimeters, then she broke my removed, like a caesarean... Feeling mistreated... I was
water (P13). The doctor said I was seven centimeters but scared. Now, I will never have a child through normal
the water had not broken, then she grabbed a thing delivery again, by god’s will, my next delivery will be a
(amniotomo), she broke herself (P8). They broke my water scheduled caesarean. So, it characterized an obstetric
in the delivery room (P3). violence for me (P15).
We can observe the use of perineum distension during This report unveils the woman’s dissatisfaction with the
the second stage of labor, a totally harmful practice that place of delivery, the procedures performed and the team’s
further increases the suffering and pain of the parturient unawareness that provided the care, even though she
and brings no benefit: They opened the vagina as much as accepted the interventions without questioning.
they could, because they were seeing the hair, “That’s the Professionals must introduce themselves, ask for the
hair.”, had not crowned yet,... tried, tried, tried, nothing, consent of pregnant women and give them the opportunity
to decide freely and consciously: They made the touch test,
www.ijaers.com Page | 112
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol-7, Issue-9, Sep- 2020]
https://dx.doi.org/10.22161/ijaers.79.14 ISSN: 2349-6495(P) | 2456-1908(O)
then they said I was going to be hospitalized, they put me However, in this hospital, the difference in care was not
in room two there, then I waited until the doctor came to perceived, given the excessive number of unnecessary
give the pill, I stayed there a long, long time. For me, I procedures, even being a high-complexity institution,
would not have even come here, but was already here nurses could better assist labor. All professionals who
right? Do what? I did not like it at all. They took too long assist women should have their behaviors supported by the
and some people had no idea about anything, they were updated scientific evidence. Encouraging pregnant women
interns I guess. They kept asking the doctor how to do or to have autonomy in the process of parturition, sharing care
not to do, I did not like it at all. I kept my mouth shut and respecting their choices. Starting with the right to give
because I was already feeling a lot of pain, so I let it go... birth in the place they want. However, we recognize that
They told me to lie on the bed there, then when she left, the guarantee of these rights is not only linked to the
they also used the speculum, it hurt so much, they kept professional who works in the delivery. The lack of
poking and poking ... A little disrespected, got it? (P6). structure and professionals in our maternity hospitals
Unknown violence results in closed shifts and overcrowding, increasing the
pilgrimage of pregnant women seeking a place to give
Although the puerperal women reported having
birth, generating feelings of disrespect and anxiety. This
experienced situations of disrespect to good practices of
violates what must be ensured, the right to know and have
childbirth care, some of them characterizing obstetric
access to the maternity where she will receive care at the
violence, it is evident the unawareness of the subject and
time of delivery. And when necessary, be referred, having
the lack of association of interventions suffered when
her transport and place guaranteed [1,5,10].
questioned about disrespect and maltreatment during their
labor and delivery: Not at all (P1). No, not at all (P2). No, Health services need to adapt to comply with what is
no (P3). No, never (P4). No (P5). No, I did not feel it, no exposed in Law n. 11,108 of April 7, 2005, which
(P7). I have nothing to say, no. (P8). No (P10). No, no, guarantees parturients the right to the presence of a
thank God, no (P13). No, never (P14). companion during labor, delivery and immediate
postpartum [4]. It is important to emphasize that the
companion is chosen by the woman and should be accepted
IV. DISCUSSION without distinction. His/her presence increases the chances
This study reveals that all women underwent some type of spontaneous vaginal delivery, decreases intrapartum
of intervention during labor, and, although most classified analgesia and dissatisfaction, promotes shorter labor time,
as being at usual obstetric risk, they did not experience a provides lower rate of cesarean section or instrumental
natural delivery. The use of technology when well vaginal delivery and decreases the chances that the baby
indicated improves obstetric indicators, but if used has a low Apgar score in the fifth minute of life [10,11].
unnecessarily implies greater risks for women and the This right needs to be respected by the institutions in an
conceptus [9]. For this reason, its use must be supported by integral way, denying because of the gender, restricting the
the updated scientific evidence. companion to labor, allowing permanence only in one type
of delivery, preventing access and permanence claiming
A factor that can contribute to reducing unnecessary
failure in the physical structure, lack of clothing or under
interventions is the work with greater autonomy of the
any pretext are violations of an acquired right, contributing
obstetric nurse in the delivery room, because he/she plays a
to obstetric violence.
more appropriate role, presenting a better cost-
effectiveness in the care of pregnancy and normal delivery, The parturient has the right to be assisted throughout
assessing risks and recognizing complications [3,9]. her labor and delivery, observing her physical and
Having been supported by the Ministry of Health through psychological well-being, including respect for her privacy
Ordinance N. 2815 of 05/29/1998, which included in the and the non-permission of unnecessary people in the
Hospital Information System (SIH/SUS) table the delivery room. Performing procedures for teaching
procedures for normal delivery without dystocia performed purposes without considering the integrity and intimacy of
by obstetric nurses and Ordinance GM N. 163 of the patient causes obstetric violence [5]. According to the
09/22/1998, which regulated the performance of normal reports of our study, pregnant women were seen by several
delivery without dystocia by an obstetric nurse in the different people during their hospitalization, but they still
Public Health Organizations of the Unified Health System spent most of their time alone, without adequate care.
(SUS). Making childbirth a painful event and an unpleasant
experience.
www.ijaers.com Page | 113
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol-7, Issue-9, Sep- 2020]
https://dx.doi.org/10.22161/ijaers.79.14 ISSN: 2349-6495(P) | 2456-1908(O)
Even though labor is generally painful, each woman childbirth, being a simple and effective tool that helps in
responds to pain differently, suffering cultural, family, taking appropriate behaviors. In developing countries, its
emotional influences, previous experiences and the social proper use is related to less indication of cesarean sections
group surrounding her. Some describe this pain as terrible, and early identification of complications [11-12]. It should
death-like pain, preferring not to remember. The be adopted in the follow-up of hospital deliveries
professional who assists the pregnant woman is responsible throughout the public network on the recommendation of
for providing conditions for her to support the discomforts the WHO and in the private network through Normative
of the parturition process [11]. This support can be offered Resolution n. 368/2015. We observed that professionals
through non-pharmacological pain relief techniques, such used techniques such as oxytocin and rupture of amniotic
as immersion bath, shower, massage and aromatherapy, membranes to accelerate labor in more than half of women,
techniques that have demonstrated decreased perception of which should not be routinely used. The use of oxytocin,
pain and anxiety. Freedom to take the most comfortable for example, in usual-risk women should be avoided, and
position and ambulation are practices that do not pose may lead to complications and the greater need for
risks, so they can be recommended [11]. Activities not surveillance of pregnant women [11]. The pain of labor is
performed with most participants since study, even with a already intrinsic for many women who do not question
multidisciplinary team present in the delivery room. these behaviors believing that their routine practice makes
The incentive and freedom of choice of women over them absolutely essential.
positioning during labor and delivery and the adoption of In the care of the second period of labor, the directed
vertical positions bring physical and psychological benefits pull was widely used in order to reduce the time of
and reveal greater satisfaction with the experience of delivery. Nonetheless, its practice is not recommended, as
childbirth [9]. Contrary to this recommendation, all the it is more likely to lead to instrumental delivery, and may
women interviewed reported not having chosen the injure the pelvic floor. Although parturients regarded it as
position and gave birth in a lithotomy position. It reveals something inherent in childbirth, it clearly causes physical
the preference of professionals for horizontalized delivery, wear and discomfort. On the other hand, practices such as
with technology in favor of their comfort, failing to perineal distension, which should not be performed,
consider what is best for women. episiotomy and forceps use, which should be observed
Another factor that should be considered is the supply regarding their need and cannot be routinely used, were
of liquids and soft diets during labor, as it contributes to reported by women within the context of violence. In
the replacement of spent energy sources, besides addition to the reports within the context of violence on
preventing dehydration and ketosis, ensuring the well- pressure at the bottom of the uterus (Kristeller maneuver),
being of the parturient and the conceptus [12]. However, for which there is insufficient evidence to recommend or
fasting is still a common practice, as justification for the not its use [12], but which made it clear that the way it was
risk of aspiration of gastric contents, if pregnant women applied should not be performed.
need the use of general anesthesia. To avoid this Obstetric violence revealed through the excess of
restriction, it is important to make an evaluation and, in unnecessary interventions, and practices not based on
case the pregnant woman is at usual risk, there is no need scientific evidence updated during labor, delivery and
to prescribe fasting [12]. However, considering that the postpartum is a matter of public health. In Brazil,
practice of offering food during labor is recent and many according to a national survey conducted in 2019, (12.6%)
professionals guide fasting fearing complications, we women reported having suffered obstetric violence [9]. In
understand why these pregnant women are afraid to eat, the present study, all women suffered some kind of
demonstrating that they are not being adequately oriented, disrespect, including procedures considered violence.
which prevents them from choosing consciously, without However, most of them showed no knowledge of the
fear or doubts according to their willingness to eat or not. It subject. In order to typify and reduce obstetric violence in
also reveals the failure in the care of women in the the country, law n. 7633/2014 is under process, which
pregnancy cycle, because this information should be provides for the humanization of care to women and
passed on during prenatal consultations, where there is newborns during the pregnancy-puerperal cycle and
continuous contact with the professional and reinforced provides other measures [13]. The urgency of dealing with
during their hospitalization. this issue is widely notorious, because, despite the efforts
A finding that deserves attention was the low use of of WHO and the Ministry of Health, with initiatives such
partogram in the deliveries investigated, which is a graphic as Rede Cegonha, there is still much to be done when it
instrument that allows monitoring the progress of comes to humanization of childbirth [14].
www.ijaers.com Page | 114
International Journal of Advanced Engineering Research and Science (IJAERS) [Vol-7, Issue-9, Sep- 2020]
https://dx.doi.org/10.22161/ijaers.79.14 ISSN: 2349-6495(P) | 2456-1908(O)
The participants of this study had a good level of in-normal-birth-a-practical-guide/
education, even though the majority did not recognize [3] Pereira, S. B., Diaz, C. M. G., Backes, M. T. S., Ferreira,
obstetric violence, situations of disrespect and the excess of C. L. L., & Backes D.S. (2018). Good practices of labor
and birth care from the perspective of health professionals.
procedures performed with them, all considered as
Rev Bras Enferm, 71(3), 1313-1319.
common to labor, making it necessarily laborious and
[4] Pauletti, J. M., Ribeiro, J. P., & Soares, M. C. (2020).
exhausting. The lack of information makes the woman Violência obstétrica: manifestações postadas em grupos
vulnerable, without autonomy to decide freely on her body. virtuais no facebook. Enfermería: Cuidados Humanizados,
The unequal relationship between the professionals who 9(1), 1-18.
assisted them is noticeable, not being asked to actively [5] Santos, R. C. S., & Souza, N. F. (2018). Violência
participate in the parturition process. This professional institucional obstétrica no Brasil: revisão sistemática.
attitude needs to be modified, however, it is necessary to Estação Científica, 5 (1), 57-68.
change the way in which these professionals learn to [6] Brasil, Ministério da Saúde. (2017). Diretrizes nacionais
de assistência ao parto normal: versão resumida.
approach women in the process of parturition. To eliminate
Recuperado em 8 agosto, 2020, de
violence, there must be a continuous educational process
http://bvsms.saude.gov.br/bvs/publicacoes/diretrizes_nacio
encompassing professionals who provide assistance nais_assistencia_parto_normal.pdf
directly and indirectly to women and family members. [7] Koerich, M. S., Backes, D. S., Sousa, F. G. M., Erdmann,
Institutions also must fulfill their role, adapting the A. L., & Alburquerque, G. L. (2016). Pesquisa-ação:
infrastructure and making the place of birth a welcoming ferramenta metodológica para a pesquisa qualitativa. Rev
environment. Eletr Enf, 11(3),717-23.
[8] Bardin, L. (2011). Análise de Conteúdo. Lisboa: Edições.
[9] Lansky, S., Souza, K. V. de, Peixoto, E. R. de M., Oliveira,
V. CONCLUSION B. J., Diniz, C. S. G., Vieira, N. F., Cunha, R. de O., &
Friche, A. A. de L. Violência obstétrica: influência da
This study showed that, although some women
exposição sentidos do nascer na vivência das
recognize that they were disrespected during their labor
gestantes. Ciência & Saúde Coletiva, 24(8), 2811-2824.
and delivery, they still do not associate this disrespect with [10] Leal, M. C., Pereira, A. P. E., Domingues, R. M. S. M.,
obstetric violence, believing those practices as common Theme, M. M., Filha, Dias, M. A. B., Pereira, M. N.,
during care, although they cause pain and anguish, Bastos, M. H., & Gama, S. G. N. da. (2015). Intervenções
supporting, not starring their deliveries. obstétricas durante o trabalho de parto em brasileiras de
risco habitual. Caderno Saúde Pública, 30(1), 17-47.
Despite the several initiatives seeking humanized care,
[11] Carvalho, I. S., & Brito, R. S. (2017). Formas de violência
without unnecessary interventions, respecting the intimacy
obstétrica vivenciadas por puérperas que tiveram parto
and autonomy of parturients, there is still need to move normal. Revista Electrónica trimestral de Enfermaría,
forward, with health education actions, policy creations, 47(16), 71-9.
laws, debates in the media, in academic centers, emphasis [12] Oliveira, M. J. de. (2019). Perspectivas Jurídicas Acerca
on prenatal care, to broaden the understanding of the da Violência Obstétrica no Brasil. Trabalho de Conclusão
importance of birth humanization. de Curso, Universidade Federal da Paraíba, Santa Rita,
Paraíba, Brasil.
This work is expected to raise reflections about the
[13] Brasil, Câmara dos Deputados. Projeto de Lei nº
need for broad discussions on obstetric care, directing care 7.633/2014. Dispõe sobre a humanização da assistência à
to women and their families in an integral way, making mulher e ao neonato durante o ciclo gravídico-puerperal e
them autonomous to actively participate in the parturition dá outras providências. Recuperado em 8 agosto, 2020, de
process, and that good practices be carried out during http://www.camara.gov.br/proposicoesWeb/fichadetramita
labor, eliminating obstetric violence. cao?idProposicao=617546<.
[14] Lima, S. S. de, Braga, M. C., Vanderlei, L. C. de M., Luna,
C. F., & Frias, P. G. (2020). Avaliação do impacto de
REFERENCES programas de assistência pré-natal, parto e ao recém-
[1] Zanardo, G. L. P., Calderón, M., Nadal, A. H. R., & nascido nas mortes neonatais evitáveis em Pernambuco,
Habigzang, L. F. (2017). Violência obstétrica no Brasil: Brasil: estudo de adequação. Cadernos de Saúde Pública,
uma revisão narrativa. Psicologia & Sociedade, 29, 36(2), e00039719.
e155043.
[2] World Health Organization. (1996). Maternal and
Newborn Health/Safe Motherhood Unit. Care in normal
birth: a practical guide. Recuperado em 8 agosto, 2020, de
https://portaldeboaspraticas.iff.fiocruz.br/biblioteca/care-
www.ijaers.com Page | 115
You might also like
- Pregnant Women's Knowledge of Obstetric Danger SignsDocument13 pagesPregnant Women's Knowledge of Obstetric Danger SignsDrPreeti Thakur ChouhanNo ratings yet
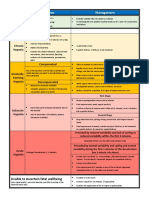
- Hypoxia Classification Table - Physiological-CTGDocument1 pageHypoxia Classification Table - Physiological-CTGKhánh Nguyễn NgọcNo ratings yet
- Humanized Delivery A Systematic ReviewDocument14 pagesHumanized Delivery A Systematic ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Research Priorities in Obstetrics SeminarDocument7 pagesResearch Priorities in Obstetrics SeminarSharmistha Debnath83% (6)
- The Daily Life of Pregnant Women: Nursing Promoting Being HealthyDocument8 pagesThe Daily Life of Pregnant Women: Nursing Promoting Being HealthyAlfina AlfianiNo ratings yet
- Brazilian Women's Use of Evidence-Based Practices in Childbirth After Participating in The Senses of Birth Intervention - A Mixed-Methods Study.Document29 pagesBrazilian Women's Use of Evidence-Based Practices in Childbirth After Participating in The Senses of Birth Intervention - A Mixed-Methods Study.Lúcia CostaNo ratings yet
- Obstetric Violence For Professionals Who Assist in ChildbirthDocument9 pagesObstetric Violence For Professionals Who Assist in ChildbirthBetsy Mirella Ramirez PrietoNo ratings yet
- Ijerph 17 08022Document11 pagesIjerph 17 08022PanegokuNo ratings yet
- Effectiveness of Antenatal Nursing Intervention On Childbirth's Fears, Psychological-Wellbeing and Pregnancy Outcomes in Primipara's WomenDocument9 pagesEffectiveness of Antenatal Nursing Intervention On Childbirth's Fears, Psychological-Wellbeing and Pregnancy Outcomes in Primipara's WomenHandayaniNo ratings yet
- Assessment of Factors That Affect Male Partner Involvement in Emergency Obstetric Care in Fortportal Regional Referral HospitalDocument16 pagesAssessment of Factors That Affect Male Partner Involvement in Emergency Obstetric Care in Fortportal Regional Referral HospitalKIU PUBLICATION AND EXTENSIONNo ratings yet
- Preconception Health and Care: A Life Course ApproachFrom EverandPreconception Health and Care: A Life Course ApproachJill ShaweNo ratings yet
- Taiwanese Journal of Obstetrics & Gynecology: Fatemeh Abdollahi, Sivosh Etemadinezhad, Munn-Sann LyeDocument5 pagesTaiwanese Journal of Obstetrics & Gynecology: Fatemeh Abdollahi, Sivosh Etemadinezhad, Munn-Sann LyePrima Wiwie'No ratings yet
- Moreau 2016Document11 pagesMoreau 2016heni bayu putriNo ratings yet
- Maternity Hospital Support SurveyDocument8 pagesMaternity Hospital Support SurveyNurul FadhilahNo ratings yet
- 1 Introduction - The Safety and Quality of Abortion Care in The United Sta172248Document20 pages1 Introduction - The Safety and Quality of Abortion Care in The United Sta172248Khrisha faith TayoNo ratings yet
- Artikel PICODocument6 pagesArtikel PICOanandaamellia0807No ratings yet
- BreastfeedDocument5 pagesBreastfeedBetHsy Pascua100% (1)
- A Survey Among Italian Pregnant Women and New-Mothers During The COVID-19 Pandemic LockdownDocument16 pagesA Survey Among Italian Pregnant Women and New-Mothers During The COVID-19 Pandemic LockdownesakkiammalNo ratings yet
- 20604-Article Text-65316-2-10-20180726 PDFDocument8 pages20604-Article Text-65316-2-10-20180726 PDFMALIK MANASRAHNo ratings yet
- Factors Influencing The Health Seeking Behaviors of Wo - 2021 - International JoDocument9 pagesFactors Influencing The Health Seeking Behaviors of Wo - 2021 - International JoRonald QuezadaNo ratings yet
- Assessment of The Factors Influencing Birth Preparedness and Complication Readiness Among Pregnant WomenDocument15 pagesAssessment of The Factors Influencing Birth Preparedness and Complication Readiness Among Pregnant WomenTwinkleNo ratings yet
- Literature Review On Uterine Prolapse in NepalDocument7 pagesLiterature Review On Uterine Prolapse in Nepaleyewhyvkg100% (1)
- Review of Literature Regarding Breast FeedingDocument6 pagesReview of Literature Regarding Breast Feedingfvhj1y00100% (1)
- DescargaDocument8 pagesDescargaMonse SantillánNo ratings yet
- Knowledge, Attitudes and Practice of Preconception Care Among Women Attending Maternal Health Clinic in KelantanDocument12 pagesKnowledge, Attitudes and Practice of Preconception Care Among Women Attending Maternal Health Clinic in Kelantandrillercz12zNo ratings yet
- 4 - Educación y GestaciónDocument5 pages4 - Educación y GestaciónSharon Lisbeth Ovalle MazoNo ratings yet
- Maternal Satisfaction Regarding Quality of Nursing Care During Labor & Delivery in Sulaimani Teaching HospitalDocument11 pagesMaternal Satisfaction Regarding Quality of Nursing Care During Labor & Delivery in Sulaimani Teaching HospitalElfira Bahar17No ratings yet
- Effect of health teaching on postpartum minor discomfortDocument6 pagesEffect of health teaching on postpartum minor discomfortSuci MaghfirahNo ratings yet
- Exploring Social and Health Care Representations About Home Birth: An Integrative Literature ReviewDocument17 pagesExploring Social and Health Care Representations About Home Birth: An Integrative Literature ReviewKrishna KoryNo ratings yet
- Abortion Literature ReviewDocument7 pagesAbortion Literature Reviewea8m12sm100% (1)
- Pharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoDocument7 pagesPharmaceutical Sciences: IAJPS 2018, 05 (04), 3075-3081 Aneeqa Ali RaoBaru Chandrasekhar RaoNo ratings yet
- Nonhuman Primates A Vital ModelDocument14 pagesNonhuman Primates A Vital ModelLídia SilveiraNo ratings yet
- Accouchement Naturel - en AnglaisDocument53 pagesAccouchement Naturel - en AnglaisDodieNo ratings yet
- Final Case Presentation Group 9 2nd RotationDocument105 pagesFinal Case Presentation Group 9 2nd Rotationjanaquintela58No ratings yet
- Perception of Child Bearing Women Towards Male Involvement in Midwifery Practice in Family Support Programme (FSP) Clinic Yenagoa, NigeriaDocument8 pagesPerception of Child Bearing Women Towards Male Involvement in Midwifery Practice in Family Support Programme (FSP) Clinic Yenagoa, NigeriaIOSRjournal100% (1)
- Lactation Induction in A Transgender WomanDocument6 pagesLactation Induction in A Transgender WomanM S de BarrosNo ratings yet
- Marwa 2Document16 pagesMarwa 2hanady shehataNo ratings yet
- Okolie Stephaine 1-3Document11 pagesOkolie Stephaine 1-3Confidence BlessingNo ratings yet
- Incidence of Mastitis in The Neonatal Period in A Traditional Breastfeeding Society: Results of A Cohort StudyDocument19 pagesIncidence of Mastitis in The Neonatal Period in A Traditional Breastfeeding Society: Results of A Cohort StudyFahrika Luthfi AfiqohNo ratings yet
- Healthcare Workers' Perspectives on Abortion MoralityDocument17 pagesHealthcare Workers' Perspectives on Abortion MoralityLinaMarcelaEcheverryBermudezNo ratings yet
- 10 1111@jog 143436777777Document17 pages10 1111@jog 143436777777Epiphany SonderNo ratings yet
- المصادر المعتمدة في فرع تمريض الام والوليدDocument6 pagesالمصادر المعتمدة في فرع تمريض الام والوليدمنتظر عبدالعظيم عبدالله حميدNo ratings yet
- The Mistreatment of Women During, Bohren 2015Document32 pagesThe Mistreatment of Women During, Bohren 2015Umratun Sirajuddin AhmadNo ratings yet
- Literature Review On Birth PreparednessDocument5 pagesLiterature Review On Birth Preparednessmgrekccnd100% (1)
- Gandhi University of Health Sciences, Karnataka Synopsis For Registration of Subject For DissertationDocument16 pagesGandhi University of Health Sciences, Karnataka Synopsis For Registration of Subject For DissertationNaman MishraNo ratings yet
- PJN Jan June 2021 Final Version CompleteDocument130 pagesPJN Jan June 2021 Final Version CompleteJohn Vincent LacuestaNo ratings yet
- Aquino 2018Document64 pagesAquino 2018Annisaa FitriNo ratings yet
- Ca MamaeDocument7 pagesCa MamaeAnonymous vkq7UwNo ratings yet
- Assess The Knowledge Regarding The Prevention and Management of Problems in Breastfeeding Among Antenatal Women in A Selected Hospital, ThrissurDocument7 pagesAssess The Knowledge Regarding The Prevention and Management of Problems in Breastfeeding Among Antenatal Women in A Selected Hospital, ThrissureditorbijnrNo ratings yet
- Journal Reading DELIVERY ROOMDocument16 pagesJournal Reading DELIVERY ROOMShyenNo ratings yet
- MLS 053 Group 10 Artificial Birth Control Case Study B8 FINALDocument15 pagesMLS 053 Group 10 Artificial Birth Control Case Study B8 FINALFrancine UriarteNo ratings yet
- 10 22034@apjcp 2018 19 4 875 PDFDocument10 pages10 22034@apjcp 2018 19 4 875 PDFClaudya TamaNo ratings yet
- Effect of Baby-Friendly Hospital Initiative Breast Feeding ProgramDocument10 pagesEffect of Baby-Friendly Hospital Initiative Breast Feeding ProgramAbi NairaNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument13 pagesJournal Homepage: - : Manuscript HistoryekaNo ratings yet
- Dean Hayden, Maria Esterlita Villanueva-Uy, Maria Katrina Mendoza, Dominic WilkinsonDocument4 pagesDean Hayden, Maria Esterlita Villanueva-Uy, Maria Katrina Mendoza, Dominic WilkinsonANONNo ratings yet
- Evaluation - KAY MAM LEAHDocument5 pagesEvaluation - KAY MAM LEAHaaron tabernaNo ratings yet
- Esplana - Nursing Research Vs Research in NursingDocument7 pagesEsplana - Nursing Research Vs Research in NursingLemuel EsplanaNo ratings yet
- Keywords: Midwifery, Qualitative Approaches, Communication, Patient Teaching, ParentingDocument9 pagesKeywords: Midwifery, Qualitative Approaches, Communication, Patient Teaching, ParentingkebsaribauamdNo ratings yet
- 95-Article Text-544-1-10-20151125Document8 pages95-Article Text-544-1-10-201511255m7m2c2kryNo ratings yet
- Social Science & Medicine: Anna L. Altshuler, Alison Ojanen-Goldsmith, Paul D. Blumenthal, Lori R. FreedmanDocument8 pagesSocial Science & Medicine: Anna L. Altshuler, Alison Ojanen-Goldsmith, Paul D. Blumenthal, Lori R. FreedmanCristina ToaderNo ratings yet
- Oup Accepted Manuscript 2018Document7 pagesOup Accepted Manuscript 2018FaidurrahmanNo ratings yet
- Beef Cattle Farmers' Economic Behavior in The Minahasa Tenggara Regency, IndonesiaDocument7 pagesBeef Cattle Farmers' Economic Behavior in The Minahasa Tenggara Regency, IndonesiaIJAERS JOURNALNo ratings yet
- Enhancing Cybersecurity: The Power of Artificial Intelligence in Threat Detection and PreventionDocument6 pagesEnhancing Cybersecurity: The Power of Artificial Intelligence in Threat Detection and PreventionIJAERS JOURNALNo ratings yet
- The Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaDocument4 pagesThe Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaIJAERS JOURNALNo ratings yet
- Climatic Rhythms and Prevalence of Malaria in The Municipality of Sinende in Northern BeninDocument8 pagesClimatic Rhythms and Prevalence of Malaria in The Municipality of Sinende in Northern BeninIJAERS JOURNALNo ratings yet
- Facing Dengue and Malaria As A Public Health Challenge in BrazilDocument6 pagesFacing Dengue and Malaria As A Public Health Challenge in BrazilIJAERS JOURNALNo ratings yet
- Business Logistics and The Relationship With Organizational SuccessDocument4 pagesBusiness Logistics and The Relationship With Organizational SuccessIJAERS JOURNALNo ratings yet
- Impacts On The Mental Health of Professionals in A Prisonal System in Alagoas During The Covid-19 PandemicDocument7 pagesImpacts On The Mental Health of Professionals in A Prisonal System in Alagoas During The Covid-19 PandemicIJAERS JOURNALNo ratings yet
- Breastfeeding and Factors Associated With The Prevention of Childhood Obesity: An Integrative Literature ReviewDocument16 pagesBreastfeeding and Factors Associated With The Prevention of Childhood Obesity: An Integrative Literature ReviewIJAERS JOURNALNo ratings yet
- Childhood/ Pediatric Cancer: Nursing Care in Oncopediatrics With A Central Focus On HumanizationDocument12 pagesChildhood/ Pediatric Cancer: Nursing Care in Oncopediatrics With A Central Focus On HumanizationIJAERS JOURNALNo ratings yet
- Constructed Wetlands: Technology For Removing Drug Concentration From WaterDocument12 pagesConstructed Wetlands: Technology For Removing Drug Concentration From WaterIJAERS JOURNALNo ratings yet
- Water Quality Assessment Using GIS Based Multi-Criteria Evaluation (MCE) and Analytical Hierarchy Process (AHP) Methods in Yenagoa Bayelsa State, NigeriaDocument11 pagesWater Quality Assessment Using GIS Based Multi-Criteria Evaluation (MCE) and Analytical Hierarchy Process (AHP) Methods in Yenagoa Bayelsa State, NigeriaIJAERS JOURNALNo ratings yet
- Associativism As Strategy of Reaching Territorial Rights, Programs, Projects and Public Policies of Rural Development: The Case of The São Francisco Do Mainã Community, Manaus, AMDocument9 pagesAssociativism As Strategy of Reaching Territorial Rights, Programs, Projects and Public Policies of Rural Development: The Case of The São Francisco Do Mainã Community, Manaus, AMIJAERS JOURNALNo ratings yet
- The Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaDocument4 pagesThe Economic Impact of Coronavirus Disease (COVID-19) : A Study On Tourism Indicators in The Kingdom of Saudi ArabiaIJAERS JOURNALNo ratings yet
- Analysis of The Thermal Behavior of Masonry Concrete Block With Internal Natural Element CoatingDocument11 pagesAnalysis of The Thermal Behavior of Masonry Concrete Block With Internal Natural Element CoatingIJAERS JOURNALNo ratings yet
- Morphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaDocument9 pagesMorphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaIJAERS JOURNALNo ratings yet
- Design and Building of Servo Motor Portable Coconut Peller MachineDocument5 pagesDesign and Building of Servo Motor Portable Coconut Peller MachineIJAERS JOURNALNo ratings yet
- Study of The Extraction Process of The Pleurotus Citrinopileatus Mushroom and Evaluation of The Biological Activity of The ExtractDocument8 pagesStudy of The Extraction Process of The Pleurotus Citrinopileatus Mushroom and Evaluation of The Biological Activity of The ExtractIJAERS JOURNALNo ratings yet
- Komla Uwolowudu Amegna: International Journal of Advanced Engineering Research and Science (IJAERS)Document9 pagesKomla Uwolowudu Amegna: International Journal of Advanced Engineering Research and Science (IJAERS)IJAERS JOURNALNo ratings yet
- Process Sequence Optimization and Structural Analysis of Nanoscale Heterostructure Using Compound Semiconductors AlAsSb/In0.59Ga0.41As/GaAs0.53Sb0.47Document5 pagesProcess Sequence Optimization and Structural Analysis of Nanoscale Heterostructure Using Compound Semiconductors AlAsSb/In0.59Ga0.41As/GaAs0.53Sb0.47IJAERS JOURNALNo ratings yet
- VCO Rancidity Analysis Refers To Fermentation Time That Produced by Gradual Heating MethodDocument6 pagesVCO Rancidity Analysis Refers To Fermentation Time That Produced by Gradual Heating MethodIJAERS JOURNAL100% (1)
- Morphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaDocument9 pagesMorphometric Analysis of The Ekole River As A Consequence of Climate Change: A Case Study in Yenagoa, Bayelsa State, NigeriaIJAERS JOURNALNo ratings yet
- Association of Bacterial Vaginosis To Atypia in Squamous Cells of The CervixDocument15 pagesAssociation of Bacterial Vaginosis To Atypia in Squamous Cells of The CervixIJAERS JOURNALNo ratings yet
- Sociodemographic and Clinical Profile of Women With Uterine Cervical Cancer Attended in An Oncological Hospital in The State of Acre, BrazilDocument9 pagesSociodemographic and Clinical Profile of Women With Uterine Cervical Cancer Attended in An Oncological Hospital in The State of Acre, BrazilIJAERS JOURNALNo ratings yet
- Modeling of Geological and Geophysical Data, Onshore Field of Potiguar Basin, Northeastern BrazilDocument5 pagesModeling of Geological and Geophysical Data, Onshore Field of Potiguar Basin, Northeastern BrazilIJAERS JOURNALNo ratings yet
- Mining and Its Impacts On Environment and Health With Special Reference To Ballari District, Karnataka, IndiaDocument7 pagesMining and Its Impacts On Environment and Health With Special Reference To Ballari District, Karnataka, IndiaIJAERS JOURNALNo ratings yet
- Humanization in Undergraduate Medical Education: The Brazilian Learner's PerspectiveDocument12 pagesHumanization in Undergraduate Medical Education: The Brazilian Learner's PerspectiveIJAERS JOURNALNo ratings yet
- Multiprofessional Care For A Patient With Gestational DiabetesDocument12 pagesMultiprofessional Care For A Patient With Gestational DiabetesIJAERS JOURNALNo ratings yet
- Does Blended Learning Approach Affect Madrasa Students English Writing Errors? A Comparative StudyDocument12 pagesDoes Blended Learning Approach Affect Madrasa Students English Writing Errors? A Comparative StudyIJAERS JOURNALNo ratings yet
- The Psychologist's Role in The Process of Listening To Children Victims of Sexual Violence in Legal ProceedingsDocument8 pagesThe Psychologist's Role in The Process of Listening To Children Victims of Sexual Violence in Legal ProceedingsIJAERS JOURNALNo ratings yet
- Assessment of The Risk of Cardiovascular Diseases and Its Relationship With Heart Rate Variability in Physically Active and Sedentary IndividualsDocument13 pagesAssessment of The Risk of Cardiovascular Diseases and Its Relationship With Heart Rate Variability in Physically Active and Sedentary IndividualsIJAERS JOURNALNo ratings yet
- Diabetes IN Pregnancy: Presenter: DR Leong Yuh Yang (MD Ukm) Supervisor: DR Noraza AzmeeraDocument45 pagesDiabetes IN Pregnancy: Presenter: DR Leong Yuh Yang (MD Ukm) Supervisor: DR Noraza AzmeeraLeong YuhyangNo ratings yet
- Journal Reading II - Dr. Yuda LutfiadiDocument13 pagesJournal Reading II - Dr. Yuda LutfiadiTegar Dwi Prakoso NurdionoNo ratings yet
- Obstetrics PDFDocument14 pagesObstetrics PDFKatheryn100% (1)
- Jurnal Reading PPT FixxeddDocument36 pagesJurnal Reading PPT Fixxeddiman prawiraNo ratings yet
- FHT, Frequency, Intensity and Duration of Contractions, Woman's Mood and BehaviourDocument2 pagesFHT, Frequency, Intensity and Duration of Contractions, Woman's Mood and BehaviourAnnrisa Layong AbainNo ratings yet
- Effects of The 2011 Flood in Thailand On Birth Outcomes and Perceived Social SupportDocument10 pagesEffects of The 2011 Flood in Thailand On Birth Outcomes and Perceived Social SupportSeptyana M ANo ratings yet
- Research On Oral Health During Pregnancy: Barriers and OpportunitiesDocument9 pagesResearch On Oral Health During Pregnancy: Barriers and OpportunitiescintaNo ratings yet
- Vaginal Oral Misoprostol-RafiqDocument29 pagesVaginal Oral Misoprostol-RafiqkhadzxNo ratings yet
- InVitroFertilization IVF KP AnalysisDocument14 pagesInVitroFertilization IVF KP AnalysisOvn Murthy100% (1)
- Preterm LaborDocument10 pagesPreterm Laborfathima AlfasNo ratings yet
- Understanding Normal Lochia Flow After ChildbirthDocument2 pagesUnderstanding Normal Lochia Flow After Childbirthbing bongNo ratings yet
- Magnesium SulfateDocument3 pagesMagnesium SulfateArabela TumbadoNo ratings yet
- Prenatal Care ReportDocument3 pagesPrenatal Care ReportczhuenaNo ratings yet
- Brochure - 'Wisdom 2010' 4th National Level PG CmeDocument6 pagesBrochure - 'Wisdom 2010' 4th National Level PG CmeSuyajna JoshiNo ratings yet
- Neonatal History and Physical ExamDocument2 pagesNeonatal History and Physical ExamMuhammad Farhan KhaliqNo ratings yet
- Fetal Death and Stillbirth - Incidence, Etiology, and Prevention - UpToDateDocument24 pagesFetal Death and Stillbirth - Incidence, Etiology, and Prevention - UpToDateChristian Yzaguirre AbantoNo ratings yet
- XAT Mock Test Paper Set BDocument8 pagesXAT Mock Test Paper Set BAli AgralNo ratings yet
- Antenatal Assessment of Fetal Well Being: DR - Abdulkarim Ahmed MohamudDocument46 pagesAntenatal Assessment of Fetal Well Being: DR - Abdulkarim Ahmed MohamudPeterNo ratings yet
- Obstetrics Hemorrhage: Khader Mohideen, Mohammed UmarDocument121 pagesObstetrics Hemorrhage: Khader Mohideen, Mohammed UmarUmar KhaderNo ratings yet
- Care and Management of Antepartal WomanDocument4 pagesCare and Management of Antepartal WomanGeuel PilapilNo ratings yet
- Komplikasi Kehamilan dan Diagnosa EktopikDocument24 pagesKomplikasi Kehamilan dan Diagnosa EktopikAldha S PutriiNo ratings yet
- OMS2 EngDocument64 pagesOMS2 EngsofiabloemNo ratings yet
- Abnormal Uterine ActionDocument20 pagesAbnormal Uterine ActionAly Badawy AgamyNo ratings yet
- Labuang Baji Hospital, Tuesday, August 29th, 2023 (Period August 23rd-August 27th, 2023) - 1Document4 pagesLabuang Baji Hospital, Tuesday, August 29th, 2023 (Period August 23rd-August 27th, 2023) - 1fadhil asyraqNo ratings yet
- Final 2014Document414 pagesFinal 2014Bhavesh Bhakodiya0% (1)
- Dampak Latihan Yoga Terhadap Kualitas Hidup Dan Psikologi Ibu NifasDocument9 pagesDampak Latihan Yoga Terhadap Kualitas Hidup Dan Psikologi Ibu NifasDella ApriliaNo ratings yet
- HOME vs HOSPITALDocument19 pagesHOME vs HOSPITALdevNo ratings yet
- Maternal & Child Health Situation in the PhilippinesDocument245 pagesMaternal & Child Health Situation in the Philippinesrhenier_ilado100% (3)
- MAPEH Third Periodical Exam for S.Y. 2019-2020Document7 pagesMAPEH Third Periodical Exam for S.Y. 2019-2020Maren PendonNo ratings yet