Professional Documents
Culture Documents
Executive Summary: Standards of Medical Care in Diabetesd2012
Uploaded by
Paula Rojas ROriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Executive Summary: Standards of Medical Care in Diabetesd2012
Uploaded by
Paula Rojas RCopyright:
Available Formats
E X E C U T I V E S U M M A R Y
Executive Summary: Standards of
Medical Care in Diabetesd2012
Current criteria for the c In those identified with increased risk those with IGT (A), IFG (E), or an A1C of
diagnosis of diabetes for future diabetes, identify and, if ap- 5.7–6.4% (E), especially for those with
c A1C $6.5%. The test should be per- propriate, treat other cardiovascular dis- BMI .35 kg/m2, those aged ,60 years,
formed in a laboratory using a method ease (CVD) risk factors. (B) and those with prior GDM. (A)
that is National Glycohemoglobin Stan- c At least annual monitoring for the de-
dardization Program (NGSP)-certified Detection and diagnosis of velopment of diabetes in those with
and standardized to the Diabetes Con- gestational diabetes prediabetes is suggested. (E)
trol and Complications Trial (DCCT) mellitus (GDM)
assay; or c Screen for undiagnosed type 2 diabetes Glucose monitoring
c fasting plasma glucose (FPG) $126 at the first prenatal visit in those with c Self-monitoring of blood glucose (SMBG)
mg/dL (7.0 mmol/l). Fasting is de- risk factors, using standard diagnostic should be carried out three or more
fined as no caloric intake for at least criteria. (B) times daily for patients using multiple
8 h; or c In pregnant women not previously insulin injections or insulin pump ther-
c 2-h plasma glucose $200 mg/dL (11.1 known to have diabetes, screen for apy. (B)
mmol/l) during an oral glucose toler- GDM at 24-28 weeks gestation, using a c For patients using less frequent insulin
ance test (OGTT). The test should be 75-g 2-h OGTT and the diagnostic injections, noninsulin therapies, or med-
performed as described by the World cutpoints in Table 6 of the “Standards ical nutrition therapy (MNT) alone,
Health Organization, using a glucose of Medical Care in Diabetesd2012”. SMBG may be useful as a guide to man-
load containing the equivalent of 75 g (B) agement. (E)
anhydrous glucose dissolved in wa- c Screen women with GDM for persistent c To achieve postprandial glucose tar-
ter; or diabetes at 6–12 weeks postpartum, gets, postprandial SMBG may be ap-
c in a patient with classic symptoms of using a test other than A1C. (E) propriate. (E)
hyperglycemia or hyperglycemic crisis, c Women with a history of GDM should c When prescribing SMBG, ensure that
a random plasma glucose $200 mg/dL have lifelong screening for the devel- patients receive initial instruction in,
(11.1 mmol/l); opment of diabetes or prediabetes at and routine follow-up evaluation of,
c in the absence of unequivocal hypergly- least every 3 years. (B) SMBG technique and their ability to
cemia, the result should be confirmed by c Women with a history of GDM found use data to adjust therapy. (E)
repeat testing. to have prediabetes should receive c Continuous glucose monitoring (CGM)
lifestyle interventions or metformin to in conjunction with intensive insulin
prevent diabetes. (A) regimens can be a useful tool to lower
Testing for diabetes in A1C in selected adults (age $25 years)
asymptomatic patients Prevention/delay of type 2 with type 1 diabetes. (A)
c Testing to detect type 2 diabetes and to diabetes c Although the evidence for A1C-lowering
assess risk for future diabetes in asymp- c Patients with IGT (A), IFG (E), or an is less strong in children, teens, and
tomatic people should be considered in A1C of 5.7–6.4% (E) should be re- younger adults, CGM may be helpful in
adults of any age who are overweight or ferred to an effective ongoing sup- these groups. Success correlates with
obese (BMI $25 kg/m2) and who have port program targeting weight loss of adherence to ongoing use of the de-
one or more additional risk factors for 7% of body weight and increasing vice. (C)
diabetes (see Table 4 of the “Standards physical activity to at least 150 min c CGM may be a supplemental tool to
of Medical Care in Diabetesd2012”). In per week of moderate activity such as SMBG in those with hypoglycemia un-
those without these risk factors, testing walking. awareness and/or frequent hypoglyce-
should begin at age 45 years. (B) c Follow-up counseling appears to be mic episodes. (E)
c If tests are normal, repeat testing at important for success. (B)
least at 3-year intervals is reasonable. c Based on the cost-effectiveness of dia- A1C
(E) betes prevention, such programs should c Perform the A1C test at least two times
c To test for diabetes or to assess risk of be covered by third-party payers. (B) a year in patients who are meeting treat-
future diabetes, A1C, FPG, or 2-h 75-g c Metformin therapy for prevention of ment goals (and who have stable glyce-
OGTT are appropriate. (B) type 2 diabetes may be considered in mic control). (E)
c Perform the A1C test quarterly in pa-
c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c c tients whose therapy has changed or
who are not meeting glycemic goals. (E)
DOI: 10.2337/dc12-s004
c Use of point-of-care testing for A1C
© 2012 by the American Diabetes Association. Readers may use this article as long as the work is properly
cited, the use is educational and not for profit, and the work is not altered. See http://creativecommons.org/ provides the opportunity for more timely
licenses/by-nc-nd/3.0/ for details. treatment changes. (E)
S4 DIABETES CARE, VOLUME 35, SUPPLEMENT 1, JANUARY 2012 care.diabetesjournals.org
Executive Summary
Glycemic goals in adults Recommendations for energy moderate amount (one drink per day or
c Lowering A1C to below or around 7% balance, overweight, and obesity less for adult women and two drinks per
has been shown to reduce microvascular c Weight loss is recommended for all day or less for adult men) and should
complications of diabetes, and if im- overweight or obese individuals who take extra precautions to prevent hypo-
plemented soon after the diagnosis of have or are at risk for diabetes. (A) glycemia. (E)
diabetes is associated with long-term c For weight loss, either low-carbohydrate, c Routine supplementation with anti-
reduction in macrovascular disease. low-fat calorie-restricted, or Mediterra- oxidants, such as vitamins E and C and
Therefore, a reasonable A1C goal for nean diets may be effective in the short carotene, is not advised because of lack
many nonpregnant adults is ,7%. (B) term (up to 2 years). (A) of evidence of efficacy and concern re-
c Providers might reasonably suggest more c For patients on low-carbohydrate di- lated to long-term safety. (A)
stringent A1C goals (such as ,6.5%) for ets, monitor lipid profiles, renal func- c It is recommended that individualized
selected individual patients, if this can tion, and protein intake (in those with meal planning include optimization of
be achieved without significant hypo- nephropathy) and adjust hypoglyce- food choices to meet recommended
glycemia or other adverse effects of mic therapy as needed. (E) daily allowance (RDA)/dietary reference
treatment. Appropriate patients might c Physical activity and behavior modi- intake (DRI) for all micronutrients. (E)
include those with short duration of fication are important components of
diabetes, long life expectancy, and no weight loss programs and are most help- Diabetes self-management
significant CVD. (C) ful in maintenance of weight loss. (B) education (DSME)
c Less stringent A1C goals (such as c People with diabetes should receive
,8%) may be appropriate for patients Recommendations for primary DSME according to national standards
with a history of severe hypoglycemia, prevention of diabetes and diabetes self-management support
limited life expectancy, advanced micro- c Among individuals at high risk for de- at the time their diabetes is diagnosed
vascular or macrovascular complications, veloping type 2 diabetes, structured pro- and as needed thereafter. (B)
and extensive comorbid conditions and grams that emphasize lifestyle changes c Effective self-management and quality
for those with longstanding diabetes that include moderate weight loss (7% of life are the key outcomes of DSME
in whom the general goal is difficult to body weight) and regular physical ac- and should be measured and moni-
attain despite diabetes self-management tivity (150 min/week), with dietary tored as part of care. (C)
education, appropriate glucose moni- strategies that include reduced calories c DSME should address psychosocial is-
toring, and effective doses of multiple and reduced intake of dietary fat, can sues, since emotional wellbeing is associ-
glucose-lowering agents including in- reduce the risk for developing diabetes ated with positive diabetes outcomes. (C)
sulin. (B) and are therefore recommended. (A) c Because DSME can result in cost-savings
c Individuals at risk for type 2 diabetes and improved outcomes (B), DSME
Therapy for type 2 diabetes should be encouraged to achieve the U.S. should be adequately reimbursed by
c At the time of type 2 diabetes diagnosis, Department of Agriculture (USDA) rec- third-party payers. (E)
initiate metformin therapy along with ommendation for dietary fiber (14 g fiber/
lifestyle interventions, unless metformin 1,000 kcal) and foods containing whole Physical activity
is contraindicated. (A) grains (one-half of grain intake). (B) c People with diabetes should be advised
c In newly diagnosed type 2 diabetic c Individuals at risk for type 2 diabetes to perform at least 150 min/week of
patients with markedly symptomatic should be encouraged to limit their moderate-intensity aerobic physical ac-
and/or elevated blood glucose levels or intake of sugar-sweetened beverages. (B) tivity (50–70% of maximum heart rate),
A1C, consider insulin therapy, with or spread over at least 3 days per week with
without additional agents, from the out- Recommendations for management no more than 2 consecutive days with-
set. (E) of diabetes out exercise. (A)
c If noninsulin monotherapy at maxi- Macronutrients in diabetes management c In the absence of contraindications,
mal tolerated dose does not achieve c The mix of carbohydrate, protein, and people with type 2 diabetes should be
or maintain the A1C target over 3–6 fat may be adjusted to meet the meta- encouraged to perform resistance train-
months, add a second oral agent, a GLP-1 bolic goals and individual preferences ing at least twice per week. (A)
receptor agonist, or insulin. (E) of the person with diabetes. (C)
c Monitoring carbohydrate intake, whether Psychosocial assessment
Medical nutrition therapy by carbohydrate counting, choices, or and care
(MNT) experience-based estimation, remains a c It is reasonable to include assessment
General Recommendations key strategy in achieving glycemic con- of the patient’s psychological and so-
c Individuals who have prediabetes or trol. (B) cial situation as an ongoing part of the
diabetes should receive individualized c Saturated fat intake should be ,7% of medical management of diabetes. (E)
MNT as needed to achieve treatment total calories. (B) c Psychosocial screening and follow-up
goals, preferably provided by a regis- c Reducing intake of trans fat lowers LDL may include, but is not limited to, atti-
tered dietitian familiar with the com- cholesterol and increases HDL choles- tudes about the illness, expectations for
ponents of diabetes MNT. (A) terol (A); therefore intake of trans fat medical management and outcomes,
c Because MNT can result in cost-savings should be minimized. (E) affect/mood, general and diabetes-related
and improved outcomes (B), MNT should Other nutrition recommendations. quality of life, resources (financial, so-
be adequately covered by insurance c If adults with diabetes choose to use cial, and emotional), and psychiatric
and other payers. (E) alcohol, they should limit intake to a history. (E)
care.diabetesjournals.org DIABETES CARE, VOLUME 35, SUPPLEMENT 1, JANUARY 2012 S5
Executive Summary
c Consider screening for psychosocial prob- c Administer pneumococcal polysaccharide c Patients with diabetes and hypertension
lems such as depression and diabetes- vaccine to all diabetic patients $2 years should be treated with a pharmacologic
related distress, anxiety, eating disorders, of age. A one-time revaccination is rec- therapy regimen that includes either an
and cognitive impairment when self- ommended for individuals .64 years of ACE inhibitor or an ARB). If one class is
management is poor. (C) age previously immunized when they not tolerated, the other should be
were ,65 years of age if the vaccine substituted. (C)
Hypoglycemia was administered .5 years ago. Other c Multiple drug therapy (two or more
c Glucose (15–20 g) is the preferred treat- indications for repeat vaccination in- agents at maximal doses) is generally
ment for the conscious individual with clude nephrotic syndrome, chronic renal required to achieve blood pressure tar-
hypoglycemia, although any form of car- disease, and other immunocompro- gets. (B)
bohydrate that contains glucose may be mised states, such as after transplan- c Administer one or more antihyperten-
used. If SMBG 15 min after treatment tation. (C) sive medications at bedtime. (A)
shows continued hypoglycemia, the treat- c Administer hepatitis B vaccination to c If ACE inhibitors, ARBs, or diuretics are
ment should be repeated. Once SMBG adults with diabetes as per Centers for used, kidney function and serum potas-
glucose returns to normal, the individual Disease Control and Prevention (CDC) sium levels should be monitored. (E)
should consume a meal or snack to pre- recommendations. (C) c In pregnant patients with diabetes and
vent recurrence of hypoglycemia. (E) chronic hypertension, blood pressure tar-
c Glucagon should be prescribed for all Hypertension/blood get goals of 110–129/65–79 mmHg are
individuals at significant risk of severe pressure control suggested in the interest of long-term
hypoglycemia, and caregivers or family Screening and diagnosis maternal health and minimizing impaired
members of these individuals should be c Blood pressure should be measured at fetal growth. ACE inhibitors and ARBs
instructed in its administration. Gluca- every routine diabetes visit. Patients found are contraindicated during pregnancy. (E)
gon administration is not limited to to have systolic blood pressure $130
health care professionals. (E) mmHg or diastolic blood pressure $80 Dyslipidemia/lipid
c Individuals with hypoglycemia un- mmHg should have blood pressure management
awareness or one or more episodes of confirmed on a separate day. Repeat Screening
severe hypoglycemia should be advised systolic blood pressure $130 mmHg or c In most adult patients, measure fasting
to raise their glycemic targets to strictly diastolic blood pressure $80 mmHg lipid profile at least annually. In adults
avoid further hypoglycemia for at least confirms a diagnosis of hypertension. (C) with low-risk lipid values (LDL choles-
several weeks, to partially reverse hy- terol ,100 mg/dL, HDL cholesterol .50
poglycemia unawareness and reduce Goals mg/dL, and triglycerides ,150 mg/dL),
risk of future episodes. (B) c A goal systolic blood pressure ,130 lipid assessments may be repeated every
mmHg is appropriate for most patients 2 years. (E)
Bariatric surgery with diabetes. (C)
c Bariatric surgery may be considered for c Based on patient characteristics and Treatment recommendations
adults with BMI .35 kg/m2 and type 2 response to therapy, higher or lower and goals
diabetes, especially if the diabetes or systolic blood pressure targets may be c Lifestyle modification focusing on the
associated comorbidities are difficult to appropriate. (B) reduction of saturated fat, trans fat, and
control with lifestyle and pharmaco- c Patients with diabetes should be trea- cholesterol intake; increase of n-3 fatty
logic therapy. (B) ted to a diastolic blood pressure ,80 acids, viscous fiber and plant stanols/
c Patients with type 2 diabetes who have mmHg. (B) sterols; weight loss (if indicated); and
undergone bariatric surgery need life- increased physical activity should be
long lifestyle support and medical mon- Treatment recommended to improve the lipid
itoring. (B) c Patients with a systolic blood pressure profile in patients with diabetes. (A)
c Although small trials have shown glyce- of 130–139 mmHg or a diastolic blood c Statin therapy should be added to life-
mic benefit of bariatric surgery in patients pressure of 80–89 mmHg may be given style therapy, regardless of baseline lipid
with type 2 diabetes and BMI of 30– lifestyle therapy alone for a maximum levels, for diabetic patients:
35 kg/m2, there is currently insufficient of 3 months and then, if targets are not
c with overt CVD. (A)
evidence to generally recommend sur- achieved, may be treated with the ad-
c without CVD who are over the age of
gery in patients with BMI ,35 kg/m2 dition of pharmacological agents. (E)
40 years and have one or more other
outside of a research protocol. (E) c Patients with more severe hypertension
CVD risk factors. (A)
c The long-term benefits, cost-effectiveness, (systolic blood pressure $140 or di-
and risks of bariatric surgery in indi- astolic blood pressure $90 mmHg) at c For lower-risk patients than the above
viduals with type 2 diabetes should be diagnosis or follow-up should receive (e.g., without overt CVD and under the
studied in well-designed controlled trials pharmacologic therapy in addition to age of 40 years), statin therapy should
with optimal medical and lifestyle ther- lifestyle therapy. (A) be considered in addition to lifestyle
apy as the comparator. (E) c Lifestyle therapy for hypertension con- therapy if LDL cholesterol remains .100
sists of weight loss, if overweight; DASH- mg/dL or in those with multiple CVD
Immunization style dietary pattern, including reducing risk factors. (E)
c Annually provide an influenza vaccine sodium and increasing potassium in- c In individuals without overt CVD, the
to all diabetic patients $6 months of take; moderation of alcohol intake; and primary goal is LDL cholesterol ,100
age. (C) increased physical activity. (B) mg/dL (2.6 mmol/l). (A)
S6 DIABETES CARE, VOLUME 35, SUPPLEMENT 1, JANUARY 2012 care.diabetesjournals.org
Executive Summary
c In individuals with overt CVD, a lower c Include smoking cessation counsel- either ACE inhibitors or ARBs should be
LDL cholesterol goal of ,70 mg/dL ing and other forms of treatment as used. (A)
(1.8 mmol/l), using a high dose of a a routine component of diabetes care. c If one class is not tolerated, the other
statin, is an option. (B) (B) should be substituted. (E)
c If drug-treated patients do not reach c Reduction of protein intake to 0.8–1.0
the above targets on maximal tolerated Coronary heart disease (CHD) g z kg body wt21 z day21 in individuals
statin therapy, a reduction in LDL cho- screening and treatment with diabetes and the earlier stages of
lesterol of ;30–40% from baseline is an Screening CKD and to 0.8 g z kg body wt21 z day21
alternative therapeutic goal. (A) c In asymptomatic patients, routine screen- in the later stages of CKD may improve
c Triglycerides levels ,150 mg/dL (1.7 ing for coronary artery disease (CAD) is measures of renal function (UAE rate,
mmol/l) and HDL cholesterol .40 mg/ not recommended, as it does not im- GFR) and is recommended. (B)
dL (1.0 mmol/l) in men and .50 mg/dL prove outcomes as long as CVD risk c When ACE inhibitors, ARBs, or diuretics
(1.3 mmol/l) in women, are desirable. factors are treated. (A) are used, monitor serum creatinine
However, LDL cholesterol–targeted statin and potassium levels for the develop-
therapy remains the preferred strategy. (C) Treatment ment of increased creatinine and hy-
c If targets are not reached on maximally c In patients with known CVD, consider perkalemia. (E)
tolerated doses of statins, combination ACE inhibitor therapy (C) and use as- c Continued monitoring of UAE to assess
therapy using statins and other lipid- pirin and statin therapy (A) (if not both response to therapy and pro-
lowering agents may be considered to contraindicated) to reduce the risk of gression of disease is reasonable. (E)
achieve lipid targets but has not been cardiovascular events. In patients with a c When estimated GFR (eGFR) is ,60
evaluated in outcome studies for either prior myocardial infarction, b-blockers ml z min/1.73 m2, evaluate and manage
CVD outcomes or safety. (E) should be continued for at least 2 years potential complications of CKD. (E)
c Statin therapy is contraindicated in after the event. (B) c Consider referral to a physician ex-
pregnancy. (B) c Longer-term use of b-blockers in the perienced in the care of kidney dis-
absence of hypertension is reasonable if ease for uncertainty about the etiology
Antiplatelet agents well tolerated, but data are lacking. (E) of kidney disease, difficult manage-
c Consider aspirin therapy (75–162 mg/ c Avoid TZD treatment in patients with ment issues, or advanced kidney dis-
day) as a primary prevention strategy in symptomatic heart failure. (C) ease. (B)
those with type 1 or type 2 diabetes at c Metformin may be used in patients with
increased cardiovascular risk (10-year stable congestive heart failure (CHF) if
risk .10%). This includes most men renal function is normal. It should be Retinopathy screening and
.50 years of age or women .60 years avoided in unstable or hospitalized pa- treatment
of age who have at least one additional tients with CHF. (C) General recommendations
major risk factor (family history of c To reduce the risk or slow the pro-
CVD, hypertension, smoking, dyslipi- Nephropathy screening gression of retinopathy, optimize gly-
demia, or albuminuria). (C) and treatment cemic control. (A)
c Aspirin should not be recommended c To reduce the risk or slow the progres-
General recommendations
for CVD prevention for adults with c To reduce the risk or slow the progres-
sion of retinopathy, optimize blood pres-
diabetes at low CVD risk (10-year CVD sion of nephropathy, optimize glucose sure control. (A)
risk ,5%, such as in men ,50 years control. (A)
and women ,60 years of age with no c To reduce the risk or slow the progres- Screening
major additional CVD risk factors), sion of nephropathy, optimize blood c Adults and children aged 10 years or
since the potential adverse effects from pressure control. (A) older with type 1 diabetes should have
bleeding likely offset the potential an initial dilated and comprehensive
benefits. (C) eye examination by an ophthalmologist
c In patients in these age-groups with
Screening or optometrist within 5 years after the
c Perform an annual test to assess urine
multiple other risk factors (e.g., 10-year onset of diabetes. (B)
risk 5–10%), clinical judgment is re- albumin excretion (UAE) in type 1 di- c Patients with type 2 diabetes should
quired. (E) abetic patients with diabetes duration have an initial dilated and comprehen-
c Use aspirin therapy (75–162 mg/day) as a
of $5 years and in all type 2 diabetic sive eye examination by an ophthalmol-
secondary prevention strategy in those patients starting at diagnosis. (B) ogist or optometrist shortly after the
c Measure serum creatinine at least annu-
with diabetes with a history of CVD. (A) diagnosis of diabetes. (B)
c For patients with CVD and documented
ally in all adults with diabetes regardless c Subsequent examinations for type 1
aspirin allergy, clopidogrel (75 mg/day) of the degree of UAE. The serum creati- and type 2 diabetic patients should be
should be used. (B) nine should be used to estimate glo- repeated annually by an ophthalmolo-
c Combination therapy with ASA (75–
merular filtration rate (GFR) and stage gist or optometrist. Less-frequent exams
162 mg/day) and clopidogrel (75 mg/ the level of chronic kidney disease (every 2–3 years) may be considered
day) is reasonable for up to a year after (CKD), if present. (E) following one or more normal eye exams.
an acute coronary syndrome. (B) Examinations will be required more fre-
Treatment quently if retinopathy is progressing. (B)
Smoking cessation c In the treatment of the nonpregnant pa- c High-quality fundus photographs can de-
c Advise all patients not to smoke. (A) tient with micro- or macroalbuminuria, tect most clinically significant diabetic
care.diabetesjournals.org DIABETES CARE, VOLUME 35, SUPPLEMENT 1, JANUARY 2012 S7
Executive Summary
retinopathy. Interpretation of the im- Foot care years of age and has had diabetes for 5
ages should be performed by a trained eye c For all patients with diabetes, perform years. (B)
care provider. While retinal photogra- an annual comprehensive foot exami- c Treatment with an ACE inhibitor, titrated
phy may serve as a screening tool for nation to identify risk factors predictive to normalization of albumin excretion,
retinopathy, it is not a substitute for a of ulcers and amputations. The foot should be considered when elevated
comprehensive eye exam, which should examination should include inspec- ACR is subsequently confirmed on
be performed at least initially and at in- tion, assessment of foot pulses, and two additional specimens from differ-
tervals thereafter as recommended by testing for loss of protective sensation ent days. (E)
an eye care professional. (E) (10-g monofilament plus testing any
c Women with preexisting diabetes who one of the following: vibration using Hypertension
are planning pregnancy or who have 128-Hz tuning fork, pinprick sensa- c Initial treatment of high-normal blood
become pregnant should have a com- tion, ankle reflexes, or vibration per- pressure (systolic or diastolic blood
prehensive eye examination and should ception threshold). (B) pressure consistently above the 90th per-
be counseled on the risk of development c Provide general foot self-care education centile for age, sex, and height) includes
and/or progression of diabetic retinopa- to all patients with diabetes. (B) dietary intervention and exercise, aimed
thy. Eye examination should occur in c A multidisciplinary approach is rec- at weight control and increased phys-
the first trimester with close follow-up ommended for individuals with foot ical activity, if appropriate. If target
throughout pregnancy and for 1 year ulcers and high-risk feet, especially blood pressure is not reached with 3–6
postpartum. (B) those with a history of prior ulcer or months of lifestyle intervention, phar-
amputation. (B) macologic treatment should be consid-
c Refer patients who smoke, have loss of ered. (E)
Treatment
c Promptly refer patients with any level
protective sensation and structural ab- c Pharmacologic treatment of hyper-
normalities, or have history of prior tension (systolic or diastolic blood
of macular edema, severe nonproli-
lower-extremity complications to foot pressure consistently above the 95th
ferative diabetic retinopathy (NPDR),
care specialists for ongoing preventive percentile for age, sex, and height or
or any PDR to an ophthalmologist
who is knowledgeable and experienced
care and life-long surveillance. (C) consistently .130/80 mmHg, if 95%
c Initial screening for peripheral arterial exceeds that value) should be consid-
in the management and treatment of
disease (PAD) should include a history ered as soon as the diagnosis is con-
diabetic retinopathy. (A)
c Laser photocoagulation therapy is in-
for claudication and an assessment of firmed. (E)
the pedal pulses. Consider obtaining c ACE inhibitors should be considered
dicated to reduce the risk of vision loss
an ankle-brachial index (ABI), as many for the initial treatment of hyperten-
in patients with high-risk PDR, clini-
cally significant macular edema, and patients with PAD are asymptomatic. (C) sion, following appropriate reproduc-
c Refer patients with significant claudi- tive counseling due to the potential
some cases of severe NPDR. (A)
cation or a positive ABI for further vas- teratogenic effects. (E)
c The presence of retinopathy is not a
contraindication to aspirin therapy for cular assessment and consider exercise, c The goal of treatment is a blood pres-
cardioprotection, as this therapy does
medications, and surgical options. (C) sure consistently ,130/80 or below the
not increase the risk of retinal hemor- 90th percentile for age, sex, and height,
rhage. (A) Assessment of common whichever is lower. (E)
comorbid conditions
Neuropathy screening and Dyslipidemia
c For patients with risk factors, signs or
treatement Screening
c All patients should be screened for
symptoms, consider assessment and treat- c If there is a family history of hyper-
ment for common diabetes-associated
distal symmetric polyneuropathy (DPN) cholesterolemia or a cardiovascular
conditions (see Table 15 of the “Stand-
starting at diagnosis of type 2 diabetes event before age 55 years, or if family
ards of Medical Care in Diabetesd
and 5 years after the diagnosis of type 1 history is unknown, then consider
2012”). (B)
diabetes and at least annually thereafter, obtaining a fasting lipid profile on
using simple clinical tests. (B) children .2 years of age soon after
c Electrophysiological testing is rarely Children and adolescents diagnosis (after glucose control has
needed, except in situations where the Glycemic control been established). If family history is
clinical features are atypical. (E) c Consider age when setting glycemic goals not of concern, then consider the first
c Screening for signs and symptoms of in children and adolescents with type 1 lipid screening at puberty ($10 years).
cardiovascular autonomic neuropathy diabetes. (E) For children diagnosed with diabetes
should be instituted at diagnosis of type at or after puberty, consider obtaining
2 diabetes and 5 years after the diagnosis Screening and management a fasting lipid profile soon after dia-
of type 1 diabetes. Special testing is of chronic complications in gnosis (after glucose control has been
rarely needed and may not affect man- children and adolescents established). (E)
agement or outcomes. (E) with type 1 diabetes c For both age-groups, if lipids are abnor-
c Medications for the relief of specific Nephropathy mal, annual monitoring is reasonable. If
symptoms related to painful DPN and c Annual screening for microalbuminuria, LDL cholesterol values are within the
autonomic neuropathy are recom- with a random spot urine sample for accepted risk levels (,100 mg/dL [2.6
mended, as they improve the quality of albumin-to-creatinine ratio (ACR), should mmol/l]), a lipid profile repeated every
life of the patient. (E) be considered once the child is 10 5 years is reasonable. (E)
S8 DIABETES CARE, VOLUME 35, SUPPLEMENT 1, JANUARY 2012 care.diabetesjournals.org
Executive Summary
Treatment if the patient develops symptoms of may benefit those with life expectancy at
c Initial therapy may consist of optimi- thyroid dysfunction, thyromegaly, or least equal to the time frame of primary or
zation of glucose control and MNT an abnormal growth rate. (E) secondary prevention trials. (E)
using a Step 2 American Heart Associ- c Screening for diabetes complications
ation Diet aimed at a decrease in the Transition from pediatric to adult care should be individualized in older adults,
amount of saturated fat in the diet. (E) c As teens transition into emerging adult- but particular attention should be paid to
c After the age of 10 years, the addition hood, health care providers and families complications that would lead to func-
of a statin in patients who, after MNT must recognize their many vulnerabi- tional impairment. (E)
and lifestyle changes, have LDL cho- lities (B) and prepare the developing
lesterol .160 mg/dL (4.1 mmol/l), or teen, beginning in early to mid adoles- Cystic fibrosis–related
LDL cholesterol . 30 mg/dL (3.4 cence and at least one year prior to the diabetes (CFRD)
mmol/l) and one or more CVD risk transition. (E) c Annual screening for CFRD with OGTT
factors, is reasonable. (E) c Both pediatricians and adult health care should begin by age 10 years in all pa-
c The goal of therapy is an LDL choles- providers should assist in providing sup- tients with CF who do not have CFRD
terol value ,100 mg/dL (2.6 mmol/l). (E) port and links to resources for the teen (B). Use of A1C as a screening test for
and emerging adult. (B) CFRD is not recommended. (B)
Retinopathy c During a period of stable health the
c The first ophthalmologic examination Preconception care diagnosis of CFRD can be made in CF
should be obtained once the child is c A1C levels should be as close to normal as patients according to usual diagnostic
$10 years of age and has had diabetes possible (,7%) in an individual patient criteria. (E)
for 3–5 years. (B) before conception is attempted. (B) c Patients with CFRD should be treated
c After the initial examination, annual c Starting at puberty, preconception coun- with insulin to attain individualized gly-
routine follow-up is generally recom- seling should be incorporated in the cemic goals. (A)
mended. Less-frequent examinations routine diabetes clinic visit for all women c Annual monitoring for complications
may be acceptable on the advice of an of childbearing potential. (C) of diabetes is recommended, beginning
eye care professional. (E) c Women with diabetes who are contem- 5 years after the diagnosis of CFRD. (E)
plating pregnancy should be evaluated
Celiac disease and, if indicated, treated for diabetic
c Consider screening children with type 1 retinopathy, nephropathy, neuropathy, Diabetes care in the hospital
c All patients with diabetes admitted to the
diabetes for celiac disease by measur- and CVD. (B)
ing tissue transglutaminase or antiendo- c Medications used by such women should
hospital should have their diabetes clearly
mysial antibodies, with documentation be evaluated prior to conception, since identified in the medical record. (E)
c All patients with diabetes should have
of normal total serum IgA levels, soon drugs commonly used to treat diabetes
after the diagnosis of diabetes. (E) and its complications may be contra- an order for blood glucose monitoring,
c Testing should be considered in chil- indicated or not recommended in preg- with results available to all members
dren with growth failure, failure to gain nancy, including statins, ACE inhibitors, of the health care team. (E)
c Goals for blood glucose levels:
weight, weight loss, diarrhea, flatulence, ARBs, and most noninsulin therapies. (E)
abdominal pain, or signs of malabsorp- c Since many pregnancies are unplanned, ○ Critically ill patients: Insulin ther-
tion, or in children with frequent un- consider the potential risks and benefits apy should be initiated for treatment
explained hypoglycemia or deterioration of medications that are contraindicated of persistent hyperglycemia starting
in glycemic control. (E) in pregnancy in all women of childbear- at a threshold of no greater than 180
c Consider referral to a gastroenterolo- ing potential, and counsel women using mg/dL (10 mmol/L). Once insulin
gist for evaluation with endoscopy and such medications accordingly. (E) therapy is started, a glucose range of
biopsy for confirmation of celiac disease 140–180 mg/dL (7.8 to 10 mmol/L) is
in asymptomatic children with positive Older adults recommended for the majority of
antibodies. (E) c Older adults who are functional, cog- critically ill patients. (A)
c Children with biopsy-confirmed celiac nitively intact, and have significant life ○ More stringent goals, such as 110–
disease should be placed on a gluten- expectancy should receive diabetes care 140 mg/dL (6.1–7.8 mmol/l) may be
free diet and have consultation with a using goals developed for younger appropriate for selected patients, as
dietitian experienced in managing both adults. (E) long as this can be achieved without
diabetes and celiac disease. (B) c Glycemic goals for older adults not significant hypoglycemia. (C)
meeting the above criteria may be re- ○ Critically ill patients require an in-
Hypothyroidism laxed using individual criteria, but hy- travenous insulin protocol that has
c Consider screening children with type 1 perglycemia leading to symptoms or risk demonstrated efficacy and safety in
diabetes for thyroid disease using thyroid of acute hyperglycemic complications achieving the desired glucose range
peroxidase and thyroglobulin antibodies should be avoided in all patients. (E) without increasing risk for severe
soon after diagnosis. (E) c Other cardiovascular risk factors should hypoglycemia. (E)
c Measuring TSH concentrations soon be treated in older adults with consid- ○ Non–critically ill patients: There is
after diagnosis of type 1 diabetes, after eration of the time frame of benefit and no clear evidence for specific blood
metabolic control has been established, the individual patient. Treatment of hy- glucose goals. If treated with in-
is reasonable. If normal, consider re- pertension is indicated in virtually all sulin, premeal blood glucose targets
checking every 1–2 years, especially older adults, and lipid and aspirin therapy generally ,140 mg/dL (7.8 mmol/l)
care.diabetesjournals.org DIABETES CARE, VOLUME 35, SUPPLEMENT 1, JANUARY 2012 S9
Executive Summary
with random blood glucose ,180 octreotide or immunosuppressive medi- Strategies for improving care
mg/dL (10.0 mmol/l) are reasonable, cations. (B) If hyperglycemia is docu- c Care should be aligned with compo-
provided these targets can be safely mented and persistent, consider treating nents of the Chronic Care Model to
achieved. More stringent targets such patients to the same glycemic goals ensure productive interactions be-
may be appropriate in stable pa- as patients with known diabetes. (E) tween a prepared proactive practice
tients with previous tight glycemic c A hypoglycemia management protocol team and an informed activated pa-
control. Less stringent targets may be should be adopted and implemented tient. (A)
appropriate in those with severe co- by each hospital or hospital system. A c When feasible, care systems should
morbidites. (E) plan for preventing and treating hy- support team-based care, community
poglycemia should be established for involvement, patient registries, and
c Scheduled subcutaneous insulin with each patient. Episodes of hypoglycemia embedded decision support tools to
basal, nutritional, and correction com- in the hospital should be documented meet patient needs. (B)
ponents is the preferred method for in the medial record and tracked. (E) c Treatment decisions should be timely
achieving and maintaining glucose con- c Consider obtaining an A1C on patients and based on evidence-based guidelines
trol in noncritically ill patients. with diabetes admitted to the hospital that are tailored to individual patient
c Glucose monitoring should be initi- if the result of testing in the previous preferences, prognoses, and comorbid-
ated in any patient not known to be 2–3 months is not available. (E) ities. (B)
diabetic who receives therapy associ- c Patients with hyperglycemia in the c A patient centered communication style
ated with high-risk for hyperglycemia, hospital who do not have a prior di- should be employed that incorporates
including high-dose glucocorticoid agnosis of diabetes should have ap- patient preferences, assesses literacy and
therapy, initiation of enteral or parenteral propriate plans for follow-up testing numeracy, and addresses cultural bar-
nutrition, or other medications such as and care documented at discharge. (E) riers to care. (B)
S10 DIABETES CARE, VOLUME 35, SUPPLEMENT 1, JANUARY 2012 care.diabetesjournals.org
Copyright of Diabetes Care is the property of American Diabetes Association and its content may not be copied
or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission.
However, users may print, download, or email articles for individual use.
You might also like
- DM 2Document11 pagesDM 2Karen QuezadaNo ratings yet
- ADA 2013 Resumen EjecutivoDocument7 pagesADA 2013 Resumen EjecutivoNatalia SánchezNo ratings yet
- Executive Summary: Standards of Medical Care in Diabetesd2014Document9 pagesExecutive Summary: Standards of Medical Care in Diabetesd2014Karen QuezadaNo ratings yet
- Executive Summary: Standards of Medical Care in Diabetes-2010Document7 pagesExecutive Summary: Standards of Medical Care in Diabetes-2010mir-medicinaNo ratings yet
- ADA STD of DM Care 2009 Exe SummaryDocument7 pagesADA STD of DM Care 2009 Exe SummaryAbuHumayraNo ratings yet
- Executive Summary: Standards of Medical Care in Diabetesd2014Document9 pagesExecutive Summary: Standards of Medical Care in Diabetesd2014Juan Carlos Plácido OlivosNo ratings yet
- Diabetes Care Guidelines - ADA 2014Document9 pagesDiabetes Care Guidelines - ADA 2014Manish Chandra PrabhakarNo ratings yet
- Resumen Guias ADA 11Document7 pagesResumen Guias ADA 11Yolpa Figueroa PorrasNo ratings yet
- Glycemic Control Targets A ISPADDocument10 pagesGlycemic Control Targets A ISPADIuliana TarceaNo ratings yet
- Metas GlicémicasDocument14 pagesMetas Glicémicasmaria suarezNo ratings yet
- Glycemic Targets. Standards of Medical Care in DiabetesDocument14 pagesGlycemic Targets. Standards of Medical Care in DiabeteslauraNo ratings yet
- Diabetes (6. Metas Glucémicas - Estándares de Atención Médica en Diabetes-2022)Document14 pagesDiabetes (6. Metas Glucémicas - Estándares de Atención Médica en Diabetes-2022)Antony Yamid Bolaños VillarrealNo ratings yet
- Description: C C C C C C C CDocument1 pageDescription: C C C C C C C CEndah budi ArsihNo ratings yet
- Ada Glycemic Targets - Metas de GlicemiaDocument14 pagesAda Glycemic Targets - Metas de GlicemiaMedicina UnisimonNo ratings yet
- Ada 2022 GlicemiaDocument14 pagesAda 2022 GlicemiaBelén MigalaNo ratings yet
- Limitations of Conventional Methods of Self-Monitoring of Blood GlucoseDocument5 pagesLimitations of Conventional Methods of Self-Monitoring of Blood GlucoseMohammed ElnaggarNo ratings yet
- Standards of Medical Care in Diabetesd2018: 6. Glycemic TargetsDocument2 pagesStandards of Medical Care in Diabetesd2018: 6. Glycemic TargetsJimmy GrefaNo ratings yet
- Standards of Medical Care in Diabetesd2018: 6. Glycemic TargetsDocument10 pagesStandards of Medical Care in Diabetesd2018: 6. Glycemic TargetsJimmy GrefaNo ratings yet
- Glycemic Targets 2022Document14 pagesGlycemic Targets 2022Tom BiusoNo ratings yet
- Glycemic Target ADA 2018Document10 pagesGlycemic Target ADA 2018Selly DamayantiNo ratings yet
- In Range StudyDocument11 pagesIn Range Studyhssdj2hfdmNo ratings yet
- Standards of Medical Care in Diabetesd2018: 6. Glycemic TargetsDocument10 pagesStandards of Medical Care in Diabetesd2018: 6. Glycemic TargetsjeanetteNo ratings yet
- Glycemic Targets: American Diabetes AssociationDocument8 pagesGlycemic Targets: American Diabetes AssociationHelenaNo ratings yet
- Does Continuous Glucose Monitoring Really Improve Diabetes ManagementDocument3 pagesDoes Continuous Glucose Monitoring Really Improve Diabetes ManagementjohnNo ratings yet
- Diabetes ValuesDocument67 pagesDiabetes Valuesluckytung07100% (1)
- Continuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic OutcomesDocument13 pagesContinuous Glucose Monitoring: A Review of Recent Studies Demonstrating Improved Glycemic OutcomesguillermocochaNo ratings yet
- Use of Glycosylated HbA1c and Random Blood Sugar As A Screening Tool For Gestational Diabetes Mellitus in First Trimester (Amreen, 2018)Document5 pagesUse of Glycosylated HbA1c and Random Blood Sugar As A Screening Tool For Gestational Diabetes Mellitus in First Trimester (Amreen, 2018)dvefrandaNo ratings yet
- Standards of Medical Care in Diabetesd2021: 6. Glycemic TargetsDocument12 pagesStandards of Medical Care in Diabetesd2021: 6. Glycemic TargetsFajar NugrahantoNo ratings yet
- Jurnal Uji Diagnosis (PD 1)Document8 pagesJurnal Uji Diagnosis (PD 1)nirmala apriziaNo ratings yet
- A1c Glycemic ControlDocument12 pagesA1c Glycemic ControlShanaz NovriandinaNo ratings yet
- March 2019 1551446825 124Document3 pagesMarch 2019 1551446825 124Anjali Rahul AjmeriNo ratings yet
- Diabetes - Dia Care 2016Document10 pagesDiabetes - Dia Care 2016titagilNo ratings yet
- Standar Medical TreatmentDocument17 pagesStandar Medical TreatmentIba SuprasabaNo ratings yet
- A1C Vs CTOGDocument6 pagesA1C Vs CTOGDiego MartinezNo ratings yet
- Celiac Disease - Inter 1Document7 pagesCeliac Disease - Inter 1Yuly Asih WidiyaningrumNo ratings yet
- Dm:Improving Outcomes: A. Consensus RecommendationsDocument21 pagesDm:Improving Outcomes: A. Consensus RecommendationsNarayananNo ratings yet
- DIABETES MCQsDocument82 pagesDIABETES MCQsFatima Zuhra100% (1)
- DM in CKD Core Curriculum 2022Document9 pagesDM in CKD Core Curriculum 2022Di KlauNo ratings yet
- Dung An 2008Document11 pagesDung An 2008EmmanuelPauloR.DiancoNo ratings yet
- VildagliptinDocument7 pagesVildagliptinwanburyNo ratings yet
- Abridged Standards of Care 2021: 7. Diabetes TechnologyDocument1 pageAbridged Standards of Care 2021: 7. Diabetes TechnologyShefira TashaNo ratings yet
- Gestational Diabetes Mellitus, Diagnostic Approaches and Maternal Offspring ComplicationsDocument12 pagesGestational Diabetes Mellitus, Diagnostic Approaches and Maternal Offspring ComplicationsSaraid RuizNo ratings yet
- Intensive Glycemic Control in The ACCORD and ADVANCE Trials: EditorialsDocument4 pagesIntensive Glycemic Control in The ACCORD and ADVANCE Trials: EditorialsMarco CarvajalNo ratings yet
- Clinical Practice Guidelines For Diabetes ManagementDocument5 pagesClinical Practice Guidelines For Diabetes ManagementIqbal Fida MaulanaNo ratings yet
- Office-Based Point of Care Testing (Iga/Igg-Deamidated Gliadin Peptide) For Celiac DiseaseDocument9 pagesOffice-Based Point of Care Testing (Iga/Igg-Deamidated Gliadin Peptide) For Celiac DiseasemarcosNo ratings yet
- Dexcom G6 CGM System Performance in Pregnant WomenDocument5 pagesDexcom G6 CGM System Performance in Pregnant WomenRizqi Fauzi Nurul AwalinNo ratings yet
- Sec2 Clinical2 (CKD + Answers)Document82 pagesSec2 Clinical2 (CKD + Answers)ahmedmohamed01153159469No ratings yet
- Clasificacion y Diagnostico de La Diabetes Guias Ada 2015Document9 pagesClasificacion y Diagnostico de La Diabetes Guias Ada 2015elizabeth salanNo ratings yet
- Diabetes LectureDocument65 pagesDiabetes LecturebailovinaflorNo ratings yet
- Comparison of Hba1C and Ogtt For The Diagnosis of Type 2 Diabetes in Children at Risk of DiabetesDocument7 pagesComparison of Hba1C and Ogtt For The Diagnosis of Type 2 Diabetes in Children at Risk of DiabetesAnnisa FujiantiNo ratings yet
- How Should You Assess Glycemic Control If The Hemoglobin A1c Is Inaccurate or Uninterpretable?Document5 pagesHow Should You Assess Glycemic Control If The Hemoglobin A1c Is Inaccurate or Uninterpretable?Jassiel AzisNo ratings yet
- 134 2021 Article 6526Document13 pages134 2021 Article 6526Eyal RobinsonNo ratings yet
- Ada 2 PDFDocument21 pagesAda 2 PDFdepy oktaNo ratings yet
- Update On: Diabetes MellitusDocument37 pagesUpdate On: Diabetes MellitusDr. Mamunul Abedin100% (1)
- Curr Opin Pediatr 2018 - Neonatal Hypoglycemia, Continuous Glucose MonitoringDocument5 pagesCurr Opin Pediatr 2018 - Neonatal Hypoglycemia, Continuous Glucose MonitoringCharlie CharcapeNo ratings yet
- Vitamin Dand HB A1 CDocument4 pagesVitamin Dand HB A1 CArizal GhazaliNo ratings yet
- Continuous Glucose MonitoringFrom EverandContinuous Glucose MonitoringWeiping JiaNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderFrom EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Resume Patricia HunterDocument2 pagesResume Patricia Hunterapi-315423763No ratings yet
- Genital Ulcer DiseaseDocument29 pagesGenital Ulcer DiseaseFu' BudhyNo ratings yet
- Cleaning Guidelines For The Prevention of Covid-19 Infections - Finnish Institute of Occupational HealthDocument8 pagesCleaning Guidelines For The Prevention of Covid-19 Infections - Finnish Institute of Occupational HealthMeng WaiNo ratings yet
- Visual AidDocument3 pagesVisual Aidapi-499098722No ratings yet
- Dementia Staging - CDR Sum of Boxes - 2008Document5 pagesDementia Staging - CDR Sum of Boxes - 2008Lee Sin YiNo ratings yet
- Tips On Applying For PCSO Medical AssistanceDocument1 pageTips On Applying For PCSO Medical AssistanceNyx100% (1)
- Effect of COVID-19 Pandemic on Livelihood of Common People in IndiaDocument2 pagesEffect of COVID-19 Pandemic on Livelihood of Common People in IndiaMUSKAN DUBEYNo ratings yet
- ConditionalsDocument7 pagesConditionalsquynhnnp234101eNo ratings yet
- Jodie Rininger ResumeDocument1 pageJodie Rininger Resumeapi-354743017No ratings yet
- Gordon'S Functional Health Pattern I. Health Perceptual PatternDocument2 pagesGordon'S Functional Health Pattern I. Health Perceptual Patternjoyrena ochondraNo ratings yet
- Review Question Week 4 StudentsDocument2 pagesReview Question Week 4 StudentsScribdNo ratings yet
- Amniotic Fluid Embolism (AFE)Document27 pagesAmniotic Fluid Embolism (AFE)ThenewaaSitumorangNo ratings yet
- Flagellates (New Version) PDFDocument91 pagesFlagellates (New Version) PDFjan9paeiamsubNo ratings yet
- Fitopanacea, LLC: Commercial ProposalDocument2 pagesFitopanacea, LLC: Commercial Proposalmadison7000No ratings yet
- There Is No Glory For Our Profession - The Experiences of Surgeons and Nurses in The American Civil WarDocument126 pagesThere Is No Glory For Our Profession - The Experiences of Surgeons and Nurses in The American Civil WarMike Wilburn100% (1)
- Abstract Book FinalDocument45 pagesAbstract Book Finalapi-200029530No ratings yet
- Breast Cancer TreatmentDocument13 pagesBreast Cancer TreatmentRissa AlmiraNo ratings yet
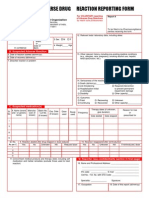
- Reporting Suspected Adverse Drug ReactionsDocument2 pagesReporting Suspected Adverse Drug ReactionsRaúl Haimerich MoncadaNo ratings yet
- PPBCC Waiver Form - GillageDocument2 pagesPPBCC Waiver Form - GillageShie MinimoNo ratings yet
- Mahatma Gandhi UniversityDocument11 pagesMahatma Gandhi UniversityMukesh BishtNo ratings yet
- Quality Improvement in Pharmacy Using PDCA ModelDocument21 pagesQuality Improvement in Pharmacy Using PDCA ModelKyte100% (2)
- 50 Facts Global Health Situation and Trends 1955-2025Document4 pages50 Facts Global Health Situation and Trends 1955-2025ClydeNo ratings yet
- Surgical Hand PreparationDocument28 pagesSurgical Hand PreparationyafetNo ratings yet
- Pediatric AcupunctureDocument11 pagesPediatric AcupunctureAli ElHadi MarmarNo ratings yet
- Laparoscopic AdrenalectomyDocument21 pagesLaparoscopic AdrenalectomyHu EyongNo ratings yet
- Male Urethritis With or Without Discharge A ClinicDocument5 pagesMale Urethritis With or Without Discharge A ClinicDian FitriNo ratings yet
- Guidelines For Management of Endometrial CarcinomaDocument41 pagesGuidelines For Management of Endometrial CarcinomaVeenaNo ratings yet
- Assessment of satisfaction among complete denture wearersDocument7 pagesAssessment of satisfaction among complete denture wearersVinod ViswanathanNo ratings yet
- Anemia Acute Blood LossDocument2 pagesAnemia Acute Blood LossCatharinaNoviaNo ratings yet