Professional Documents
Culture Documents
Journal of Anesthesia & Clinical Research
Journal of Anesthesia & Clinical Research
Uploaded by
Teshome AssefaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Journal of Anesthesia & Clinical Research
Journal of Anesthesia & Clinical Research
Uploaded by
Teshome AssefaCopyright:
Available Formats
Journal of Anesthesia & Clinical
Research Kassa et al., J Anesth Clin Res 2015, 6:6
http://dx.doi.org/10.4172/2155-6148.1000536
Research Article Open Access
Post Dural Puncture Headache (PDPH) and Associated Factors after Spinal
Anesthesia among Patients in University of Gondar Referral and Teaching
Hospital, Gondar, North West Ethiopia
Adugna Aregawi Kassa1*, Teresa Kisi Beyen2 and Zewditu Abdissa Denu1
1Department of Medical Anesthesiology, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
2Department of Epidemiology and Biostatistics, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
*Corresponding author: Kassa AA, Department of Medical Anesthesiology, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia. E-mail:
adugenet2007@yahoo.com
Received date: April 30, 2015; Accepted date: June 15, 2015; Published date: June 22, 2015
Copyright: © 2015 Kassa AA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Post dural puncture headache (PDPH) has been a problem for patients after dural puncture. It is
one of the most frequently occurring complications following spinal anesthesia (SA). It is believed to originate from
persistent leakage of cerebrospinal fluid (CSF) through the punctured Dura, greater than the CSF production after
lumbar puncture. Although the problem has been widely reported, its magnitude and associated factors has never
been studied in our country. Thus, the aim of this study is to assess the magnitude of post dural puncture headache
(PDPH) and associated factors after spinal anesthesia among patients in university of Gondar referral and teaching
hospital.
Methods: An institution based cross sectional study was conducted from February 25-April 10, 2013 in University
of Gondar teaching and referral hospital, Gondar, Ethiopia. A total of 116 patients aged 17-74 years were included in
the study. Data was collected by interviewing patients using structured and pre-tested questionnaire and reviewing
chart. Both bivariable and multivariable logistic regressions were used to determine the association between post
dural puncture headache and independent variables.
Results: Out of 116 patients who have undergone spinal anesthesia 45 (38.8%) patients developed post dural
puncture headache. Sex [AOR=0.2; 95% CI: 0.058, 0.67], repeated attempts [AOR=0.22; 95% CI: 0.09, 0.54], and
needle sizes [AOR=5.3; 95% CI: 1.66, 16.93] were found to be significantly associated with Post Dural puncture
headache.
Conclusion: Prevalence of post dural puncture headache was found to be high among patients in the University
of Gondar teaching and referral hospital after spinal anesthesia (SA). The hospital management and the
anesthetists of University of Gondar teaching and referal hospital should minimize the incidence of post dural
puncture headache by avoiding use of big needles and repeated attempt especially on female patients.
Keywords: PDPH; Gondar; Ethiopia IHS reported this, recent studies indicated the latency period to be
within 3 days [4-6,8-12], and another study conducted in 2012 to
Introduction evaluate the validity of the diagnostic criteria for Post-Dural puncture
headache showed that some patients can suffer from PDPH in the
Since August Bier reported the first case in 1898, post-dural absence of the associated symptoms [4].
puncture headache (PDPH) has been a problem for patients following
dural puncture. PDPH is an important iatrogenic cause of patient Factors predisposing for PDPH can be patient or equipment
morbidity in modern anesthesia [1,2]. (needle). Women, particularly during pregnancy, are considered at
increased risk for PDPH [1,2,4]. High levels of estrogens in women
Post-dural puncture headache typically presents as a postural can influence the tone of the cerebral vessels, thus increasing the
headache that worsens when a patient is in the upright position and vascular distension response to CSF hypotension [1-4].
lessens to some extent when a patient is in the recumbent position
[1-6]. PDPH is believed to originate from persistent leakage of The incidence of PDPH is highest in young individuals [1,2,4,5] and
cerebrospinal fluid (CSF) greater than the cerebrospinal fluid lean patients [1-4]. Women who are obese or morbidly obese may
production after lumbar puncture [3]. According to the diagnostic have a decreased incidence of PDPH as a result of the increased in
criteria of the International Headache Society (IHS) in 2004, the intra-abdominal pressure which acts as an abdominal binder helping
headache can appear up to the fifth day after puncture and disappears to seal the defect in the dura and decreasing the loss of CSF [1].
spontaneously within a week, or up to 48 hours after an epidural blood The incidence of PDPH is also directly related to the needle
patch (EBP) and accompanied by neck stiffness, tinnitus, hypoacusia diameter that pierces the Dura mater. The incidence is significantly
(partial loss of hearing), photophobia, and nausea [7]. Even though the higher when large bore needles greater than 22 G than when smaller
J Anesth Clin Res Volume 6 • Issue 7 • 1000536
ISSN:2155-6148 JACR, an open access journal
Citation: Kassa AA, Beyen TK, Denu ZA (2015) Post Dural Puncture Headache (PDPH) and Associated Factors after Spinal Anesthesia among
Patients in University of Gondar Referral and Teaching Hospital, Gondar, North West Ethiopia. J Anesth Clin Res 6: 536. doi:
10.4172/2155-6148.1000536
Page 2 of 6
needles (<25 G) were used [1,2,4,5]. Although smaller diameter needle severity of pain was determined using visual analogue scale (VAS) and
punctures used for spinal block decrease the risk of PDPH, these verbal rating scale. To ensure quality of data pre-test of the
needles are technically difficult to use and are associated with a lower questionnaire was done on 20 patients from Bahirdar Felege Hiwot
success rate in spinal anesthesia [1-4]. Not only the size of the needle hospital to check for accuracy and clarity of information and
affects the incidence of PDPH, but also the type of needle tips [1,2,4]. anesthetist who had an experience was collected the data after training
The cutting needle bevels are more common to cause PDPH than the had been given. Data collection procedure was also supervised by a
less traumatic pencil point needle bevels. The direction of the needle consultant anesthesiologist and investigators.
bevel during insertion also contributes to the occurrence of PDPH. If
the bevel of the spinal needle is inserted perpendicular to the fibres of Data analysis procedures
the Dura (which are believed to run longitudinally) an increased
incidence of PDPH is expected [1,2,4-6,13,14]. The collected data were cleaned, coded, and entered in to EPI info 7
and then exported to SPSS version 20 for further analysis. The patients
Another factor is a past history of PDPH [1,2,4,15,16]. Patients with were identified as having PDPH if Headache develops within three
previous history of PDPH have a significantly more probability of days after dural puncture and a headache that worsens within 15
developing PDPH on the subsequent lumbar punctures. Repeated minutes after sitting or standing and/or improves within 15 minutes
Dural puncture due to inexperience of the procedure performer or after lying. Once patients diagnosed as having PDPH, the severity of
technical difficulty also increases the chance of PDPH on patients this pain was assessed using VAS and NAS (for those who can read
[1,2,5]. and write) or verbal rating scale (for those who can’t read or write).
Different studies have reported widely different incidence of PDPH. Both descriptive and analytic statistics were computed and data
In our country we could not find published research done on this were presented by tables, graphs, percentile and texts. All independent
topic, so the prevalence of PDPH is not known in our situation. variables were analyzed using binary logistic regression with the
Knowing the prevalence of PDPH and its associated factors in our dependent variable PDPH using SPSS version 20 and those which were
situation helps to recognize the magnitude of the problem and may significant at a p-value of <0.2 were fitted to a multivariate logistic
help to facilitate actions to reduce its occurrence. This research can regression to check their association with the outcome variable, PDPH
also help as a baseline for future researches on related topics by at a p-value of <0.05. Hosmer-Lemeshow (0.82) test of goodness of fit
indicating the prevalence rate and associated risk factors of PDPH in was performed to check the appropriateness of the model for analysis.
this area.
Ethical considerations
Methods
Before actual data collection ethical clearance was obtained from
the ethical review board of University of Gondar. Formal letter of
Study design, setting and period cooperation was written to Hospital administrators. The objectives of
An institution based cross sectional study was conducted among the study were explained and written consent was obtained from each
patients in the University of Gondar teaching and referral hospital participant. Confidentiality was maintained at all levels of the study by
from February 25-April 10, 2013. Gondar town, which is the capital of avoiding identifiers, using codes to identify patients, keeping privacy
North Gondar zone, is one of the historical towns in the country and of the study participants during data collection and locking the
located at about 727 Km Northwest of Addis Ababa. According to the questionnaires securely. For seriously ill patients advice has been given
2007 Ethiopian census report, Gondar has a total population of to revisit health institution.
206,987 and more than half (108,902) of them were females [17].
Results
Sample size and sampling technique
All patients (124) who have undergone their surgical procedure Socio-demographic and physical characteristics
under spinal anesthesia between February 25 and April 10, 2013 were A total of 116 patients were included in the analysis making the
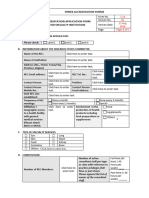
included in the study. The study has included all surgical and obstetric response rate of 93.35%. The majority of patients included in this
patients of Gondar teaching and referral hospital who have undergone study were female patients (78.4%). The age of study participants
their surgical procedure under spinal anesthesia by excluding patients range from 17 to 74 years with mean age of 33.8 year and a standard
with impaired cognitive ability. deviation of 14.2 year and majority (93.1%) of them were ASA I (Table
1 and Figure 1).
Data collection procedure
A structured and pretested questionnaire was prepared to collect Spinal anesthesia related history of patients
data both from the chart and patient interview. Socio demographic Ten patients (8.6%) had a previous history of spinal anesthesia (SA)
data like the patient’s age and sex, the American Society of exposure and three (37.5%) of them complained a PDPH like
Anesthesiologists (ASA) status, patient position, size of the needle and headache after the procedure. Almost all patients (99.1%) had been
number of attempts were collected from the chart. The data for the given SA on a sitting position. 20 G was the most frequently used
outcome variable was collected by interviewing the patients using spinal needle to administer SA (42.5% of patients) whereas 25 G was
questionnaire at least 12 hours after the dural puncture had been used only in one patient. There were 5 cases (4.3%) of failed block that
performed and those who didn’t complain headache at the first visit were converted to general anesthesia (GA) and two of these patients
were followed up each day until the 3rd day to see if they develop have developed PDPH (Table 2).
headache in the consecutive days. For patients who experienced PDPH
J Anesth Clin Res Volume 6 • Issue 7 • 1000536
ISSN:2155-6148 JACR, an open access journal
Citation: Kassa AA, Beyen TK, Denu ZA (2015) Post Dural Puncture Headache (PDPH) and Associated Factors after Spinal Anesthesia among
Patients in University of Gondar Referral and Teaching Hospital, Gondar, North West Ethiopia. J Anesth Clin Res 6: 536. doi:
10.4172/2155-6148.1000536
Page 3 of 6
Variable Frequency: n (%) Yes 10 (8.6%)
15-29 76 (65.5%) Previous SA No 106 (91.4%)
Age (years) 30-59 34 (29.3%) Yes 3 (2.6%)
>60 6 (5.2%) Previous history of PDPH No 113 (97.4%)
Female 91 (78.4%) Sitting 115 (99.1%)
Sex
Male 25 (21.6%) Position Lateral 1 (0.9%)
<18.5 Single attempt 64 (55.2%)
18 (15.5%)
(underweight)
Twice attempt 36 (31%)
18.5-24.9
BMI 91 (78.4%)
(normal) Number of attempts >2 attempts 16 (13.8%)
25-29.9 18 Gauge 11 (9.5%)
7 (6%)
(overweight)
20 Gauge 49 (42.5%)
ASA I 108 (93.1%)
ASA 22 Gauge 29 (25%)
ASA II 8 (6.9%)
24 Gauge 15 (12.9%)
Table 1: Socio-demographic and physical characteristics of the study 25 Gauge 1 (0.9%)
participants in GUH from February 25-April 10, 2013.
Size of SA needle 26 Gauge 5 (4.3%)
27 Gauge 6 (5.2%)
Yes 111 (95.7%)
A successful block No 5 (4.3%)
Neck stiffness 34 (29.3%)
Tinnitus 2 (1.7%)
Photophobia 1 (0.9%)
Nausea 10 (8.6%)
Associated symptoms None 69 (59.5%)
Figure 1: Distribution of the study participants’ age in GUH when Table 2: Spinal anesthesia related parameters of the study participants
expressed by categorizing into groups. Most of patients were in the in GUH from February 25-April 10, 2013.
age group of 15-29 years.
Prevalence of PDPH
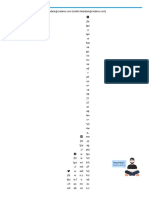
In this study PDPH was observed on 45 patients (38.8%) whereas 11
patients (9.5%) complained headache but they didn’t fulfill the criteria
to be classified as patients with PDPH (Figure 2).
The proportion of PDPH varies greatly when different needle sizes
were used. For instance the proportion of PDPH was very high
(63.6%) when 18G spinal needles were used, whereas the proportion
was low (8.3%) when small needles were used (Table 3).
Figure 2: Magnitude of post dural puncture headache (PDPH)
among patients who have had spinal anesthesia in university of
Severity of PDPH
Gondar referral and teaching hospital, Gondar, North West
Among 45 patients who developed PDPH, majority of them have Ethiopia, April 10, 2013 (n=116).
developed mild (42.2%) followed by moderate (31.1%) pain (Figure 3).
On 80% of patients with PDPH either of neck stiffness, nausea, or
photophobia was observed (Figure 4).
Needle size used PDPH % of patients with PDPH
Variable Frequency: n (%)
J Anesth Clin Res Volume 6 • Issue 7 • 1000536
ISSN:2155-6148 JACR, an open access journal
Citation: Kassa AA, Beyen TK, Denu ZA (2015) Post Dural Puncture Headache (PDPH) and Associated Factors after Spinal Anesthesia among
Patients in University of Gondar Referral and Teaching Hospital, Gondar, North West Ethiopia. J Anesth Clin Res 6: 536. doi:
10.4172/2155-6148.1000536
Page 4 of 6
Yes No
18G 7 4 63.60%
20G 24 25 49%
22G 9 20 31%
24G 4 11 26.60%
<24 G (25, 26 and 27) 1 11 8.30%
Table 3: percentage of PDPH developed when specific needle sizes
were used among the study participants of GUH who developed
PDPH, February 25-April 10, 2013.
Figure 4: Associated symptoms complained by patients who had
PDPH after spinal anesthesia in university of Gondar referral and
teaching hospital, Gondar, North West Ethiopia, April 10, 2013.
Factors associated with PDPH
The result of bivariate logistic regression indicated that sex, BMI,
needle size and number of attempts were significantly associated with
PDPH of patients. However, by multivariate logistic regression
analysis only sex, needle size and number of attempts were found to be
Figure 3: Severity of headache among patients who developed statistically significant at p-value<0.05 (Table 4).
PDPH in GUH from February 25-April 10, 2013. In this study sex was significantly associated with the outcome
variable PDPH. Male patients are 80% less likely to develop PDPH
than female patients (AOR=0.2, 95% CI: 0.058, 0.67).
Variables PDPH COR (95% CI) AOR (95% CI) P-value
Yes No
Sex Male 4 21 0.23 (0.074, 0.731) 0.2 (0.058, 0.67) 0.009
Female 41 50 1 1
Spinal needles Large needles* 40 49 3.6 (1.25, 10.34) 5.3 (1.66, 16.93) 0.005
Small needles** 5 22 1 1
Attempt Single 17 47 0.31 (0.14, 0.67) 0.22 (0.09, 0.54) 0.001
Multiple 28 24 1 1
Table 4: Factors associated with PDPH of patients who had SA in GUH, February 25-April 10, 2013. *needle sizes larger than 24 G; **needle
sizes<24 G.
Size of the needle used to administer SA is also significantly Discussion
associated with the development of PDPH. Patients received SA using
bigger spinal needles were more than 5 times more likely to develop Different researches showed different values of the prevalence of
PDPH than patients who received SA using smaller needles (AOR=5.3, PDPH. In this study the overall prevalence of PDPH was 38.8%. This
95% CI: 1.66,16.93). result is found to be higher than the usual figures reported by most
studies [4,6,8,13]. The possible cause for this could be because most
Another significant association was found between number of (77%) of the study participants in our study were received SA using big
attempts and PDPH. Patients who received SA on the first attempt spinal needles. The study participants in this study were also prone to
were 78% less likely to develop PDPH than their counter part patients repeated number of attempts. The other possible cause for this higher
who had a repeated attempt (AOR=0.22, 95% CI: 0.09, 0.54). figure could be again most (78%) of participants were female.
These factors were found to be significantly associated with the
development of PDPH in our study and many other literatures.
J Anesth Clin Res Volume 6 • Issue 7 • 1000536
ISSN:2155-6148 JACR, an open access journal
Citation: Kassa AA, Beyen TK, Denu ZA (2015) Post Dural Puncture Headache (PDPH) and Associated Factors after Spinal Anesthesia among
Patients in University of Gondar Referral and Teaching Hospital, Gondar, North West Ethiopia. J Anesth Clin Res 6: 536. doi:
10.4172/2155-6148.1000536
Page 5 of 6
In our study the majority of patients have experienced mild (42.2) some of the limitations of the study. In addition the study is not out of
and moderate (31.1%) PDPH pain, which is the same as studies the effect of cross sectional study design whish unable to indicate the
conducted in Ghana [18], Australia [19] and Pakistan [12]. On the temporal relationship.
other hand 26.7% of patients with PDPH complained as having severe
pain. This figure in line with studies conducted in Australia on Conclusions
obstetric patients, which has reported as 27.7% [19] and Pakistan
which has reported as 28.6% severe headache [12]. Unlike the figures The study revealed that prevalence of PDPH was too high when
reported in the above studies, a study conducted in Denmark to grade compared to other studies out of which majority of the patients have
the severity of PDPH reported that 60% of patients rated their pain as been suffered from severe headache. The study also showed that being
severe [20]. The reason behind the discrepancy in severity of pain female, big spinal needles and repeated number of attempts were
could be the cultural effect. Because pain has psychological, social, and factors significantly associated with PDPH.
spiritual as well as physical dimensions, it is greatly influenced by
cultural factors. People of different cultures respond differently to Recommendations
pain. For instance, people who passed through a lot of pain and
sufferings, like people in Africa, are less likely to complain a severe The hospital management and the anesthetists of University of
pain for a given intensity of pain than people who didn’t pass through Gondar teaching and referal hospital should minimize the incidence of
such pain and suffering like people in Scandinavia [21]. Post Dural puncture headache by avoiding use of big needles and
repeated attempt especially on female patients.
In this study we found out that being male is a protective factor for
PDPH. Male patients are 80% less likely to develop PDPH than female
Competing Interests
patients [AOR=0.2; 95% CI: 0.058, 0.67]. The reason for an increased
risk of PDPH for females could be the high level of estrogens in The authors of this study declare that there were no conflicts of
women. High levels of estrogens in women can influence the tone of interests.
the cerebral vessels, increasing the vascular distension response to CSF
hypotension [1-4]. This finding was similar with different studies Authors' Contributions
[1,2,4-6,22-25]. But in some studies no significant association was
reported between gender and the incidence of PDPH [26,27]. AA, wrote the proposal, participated in data collection, analyzed the
data and drafted the paper. TK and ZA approved the proposal with
Size of the spinal needle used was significantly associated with the some revisions, participated in data analysis and revised subsequent
development of PDPH in this study. Patients who received SA using drafts of the paper. All authors read and approved the final
big needles were about five times more likely to develop PDPH than manuscript.
those patients who received SA using small needles [AOR=5.3; 95%
CI:1.66, 16.93]. The reason behind this is bigger needles leave bigger
opening on the Dura, so more CSF leak than smaller opening caused Acknowledgements
by smaller needles. Many studies support our finding We would like to acknowledge University of Gondar for providing
[1,2,5,21,23,28-30]. us financial aid to conduct the study. Our special gratitude also goes to
Another significant association was found between the number of all study participants for their patience and providing us full
attempts and the development of PDPH. Patients for whom SA was information.
successful at the first attempt were 78% less likely to develop PDPH
than those patients for whom attempt was repeated [AOR=0.22; 95% References
CI: 0.09, 0.54]. This could be due to as the number of attempt increase
1. Ghaleb A (2010) Post-dural puncture headache, Review Article.
the probability of piercing the Dura matter repeatedly will increase, International Journal of Medicine 45-52.
which increases the volume of CSF leak, thereby increasing the
2. Kuczkowski KM (2004) Post-dural puncture headache in the obstetric
probability of development of CSF hypotension & PDPH. This finding patient: an old problem. New solutions. Minerva Anestesiol 70: 823-830.
in lines with findings of different studies [1,2,5,23] even if some other 3. Liu H, Kalarickal PL, Rosinia F (2011) A case of paradoxical presentation
studies couldn’t find significant association between the number of of postural post dural puncture headache. J Clin Anesth 24: 255-256.
attempts and PDPH development [26,30,31]. 4. Amorim JA, Gomes de Barros MV, Valença MM (2012) Post-dural
(post-lumbar) puncture headache: risk factors and clinical features.
On the other hand BMI, age of the patients and previous history of
Cephalalgia 32: 916-923.
PDPH were not associated with the development of PDPH even
5. Lybecker H, Møller JT, May O, Nielsen HK. (1990) Incidence and
though these variables (lower BMI, younger age, and previous history Prediction of Post dural Puncture Headache. A prospective Study of 1021
of PDPH) have reported as risk factors for PDPH in different studies Spinal Anesthesia. Anesth Analg 70: 389-394.
[1,2,4,5,15,27]. This could be most likely due to the small sample size 6. Douglas MJ, Ward ME, Campbell DC, Bright SB, Merrick PM (1997)
to compare different categories of BMI, age, and patients with and Factors involved in the incidence of post-dural puncture headache with
without previous history of PDPH in our study. the 25 gauge Whitacre needle for obstetric anesthesia. Int J Obstet Anesth
6: 220-223.
Even though this study indicated very important results, using small
7. Oleson J, Steiner T (2004) The International Classification of Headache
sample size, not including very important variables like level of the Disorders, 2nd edition. The Lancet Neurology 2:720.
anesthetist performing the SA, the effect of needle tip on the
8. Frenkel C, Altscher T, Groben V, Hörnchen U (1992) [The incidence of
prevalence of PDPH, and direction of the needle bevel during post spinal headache in a group of young patients]. Anaesthesist 41:
insertion and only following patients for three days since some 142-145.
patients may develop PDPH till the 7th day after Dural puncture are
J Anesth Clin Res Volume 6 • Issue 7 • 1000536
ISSN:2155-6148 JACR, an open access journal
Citation: Kassa AA, Beyen TK, Denu ZA (2015) Post Dural Puncture Headache (PDPH) and Associated Factors after Spinal Anesthesia among
Patients in University of Gondar Referral and Teaching Hospital, Gondar, North West Ethiopia. J Anesth Clin Res 6: 536. doi:
10.4172/2155-6148.1000536
Page 6 of 6
9. L'ubuský M, Berta E, Procházka M, Marek O, Kudela M (2006) 20. Corbey MP, Bach AB, Lech K, Frørup AM (1997) Grading of severity of
Development of incidence of post-dural puncture headache in patients postdural puncture headache after 27-gauge Quincke and Whitacre
undergoing caesarean section in spinal anaesthesia at the Department of needles. Acta Anaesthesiol Scand 41: 779-784.
Obstetrics and Gynecology in Olomouc during 2003-2004. Cas Lek Cesk, 21. Hall JK, Boswell MV (2009) Ethics, law, and pain management as a
Czech 145: 204-208. patient right. Pain Physician 12: 499-506.
10. Dakka Y, Warra N, Albadareen RJ, Jankowski M, Silver B (2011) 22. Hwang JJ, Ho ST, Wang JJ, Kuo WS, Liu HS (1997) The incidence of post
Headache rate and cost of care following lumbar puncture at a single dural puncture headache in Taiwanese patients undergoing cesarean
tertiary care hospital. Neurology 77: 71-74. section. Acta Anaesthesiol Sin 35: 1-6.
11. Van de Velde M, Schepers R, Berends N, Vandermeersch E, De Buck F 23. M Kuczkowski (2006) Post-dural puncture headache in pregnant women:
(2008) Ten years of experience with accidental dural puncture and post- What have we learned? Revista Colombiana de Anestesiología 34: 267-72.
dural puncture headache in a tertiary obstetric anaesthesia department. 24. Kang SB, Goodnough DE, Lee YK, Olson RA, Borshoff JA, et al. (1992)
Int J Obstet Anesth 17: 329-335. Comparison of 26- and 27-G needles for spinal anesthesia for ambulatory
12. Malik MA, Khan BH (2008) To Compare the Frequency and Severity of surgery patients. Anesthesiology 76: 734-738.
Post-dural Puncture Headache (PDPH) in Parturients given Spinal 25. Wadud R, Laiq N, Qureshi FA, Jan AS (2006) The frequency of postdural
Anaesthesia with 25G Quincke with that of 25G Whitacre Needle. puncture headache in different age groups. J Coll Physicians Surg Pak 16:
Department of Anesthesia, Shalamar Hospital, Lahore, Pakistan 42-47. 389-392.
13. Chan L, Delilkan AE (1992) Incidence of postdural puncture headache. A 26. Jeanjean P, Montpellier D, Carnec J, Crasquin O, Koral E, et al. (1997)
prospective study of 101 spinal anaesthetics in orthopaedic patients. Med [Headaches after spinal anesthesia: prospective multicenter study of a
J Malaysia 47: 20-26. young adult population]. Ann Fr Anesth Reanim 16: 350-353.
14. Richman JM, Joe EM, Cohen SR, Rowlingson AJ, Michaels RK, et al. 27. de Almeida SM, Shumaker SD, LeBlanc SK, Delaney P, Marquie-Beck J,
(2006) Bevel direction and postdural puncture headache: a meta-analysis. et al. (2011) Incidence of post-dural puncture headache in research
Neurologist 12: 224-228. volunteers. Headache 51: 1503-1510.
15. Amorim JA, Valença MM (2008) Postdural puncture headache is a risk 28. Coahan U, Hamdani GA (2003) Post dural puncture headache. Journal of
factor for new postdural puncture headache. Cephalalgia 28: 5-8. Pakistan Medical Association 53:272-281.
16. Kuczkowski KM, Benumof JL (2003) Once a post-dural puncture 29. Frank RL1 (2008) Lumbar puncture and post-dural puncture headaches:
headache patient always post-dural puncture headache patient? Acta implications for the emergency physician. J Emerg Med 35: 149-157.
Anaesthesiol Belg 54: 167-168.
30. Bezov D, Ashina S, Lipton R (2010) Post-dural puncture headache: Part
17. Central Statistical Agency (2008) Summary and statistical report of the II--prevention, management, and prognosis. Headache 50: 1482-1498.
2007 population and housing census: population size by age and sex.
Ethiopia AA. In. UNFPA.
31. Imarengiaye C, Ekwere I (2006) Postdural puncture headache: a cross-
sectional study of incidence and severity in a new obstetric anaesthesia
18. Nafiu OO, Salam RA, Elegbe EO (2007) Post dural puncture headache in unit. Afr J Med Med Sci 35: 47-51.
obstetric patients: experience from a West African teaching hospital. Int J
Obstet Anesth 16: 4-7.
19. Ross AW, Greenhalgh C, McGlade DP, Balson IG, Chester SC, et al.
(1993) The Sprotte needle and post dural puncture headache following
caesarean section. Anaesth Intensive Care 21: 280-283.
J Anesth Clin Res Volume 6 • Issue 7 • 1000536
ISSN:2155-6148 JACR, an open access journal
You might also like
- Decree 4725 de 2005Document3 pagesDecree 4725 de 2005api-594576766No ratings yet
- 10 1016@j JHT 2017 02 001 PDFDocument10 pages10 1016@j JHT 2017 02 001 PDFGusti Ayu KrisnayantiNo ratings yet
- Jaccoa 08 00330Document5 pagesJaccoa 08 00330Teshome AssefaNo ratings yet
- Postdural Puncture Headache: Kyung-Hwa KwakDocument8 pagesPostdural Puncture Headache: Kyung-Hwa KwakRakha FahrezaNo ratings yet
- Deambulacion Vs Reposo en CPPDocument10 pagesDeambulacion Vs Reposo en CPPNoé Alejandro SánchezNo ratings yet
- Postdural Puncture Headache and Epidural Blood Patch Use in Elderly PatientsDocument5 pagesPostdural Puncture Headache and Epidural Blood Patch Use in Elderly PatientsJunwei XingNo ratings yet
- PDPH MeruDocument6 pagesPDPH MeruTeshome AssefaNo ratings yet
- Management Practices For Postdural Puncture Headache in Obstetrics: A Prospective, International, Cohort StudyDocument11 pagesManagement Practices For Postdural Puncture Headache in Obstetrics: A Prospective, International, Cohort StudyAlexisNo ratings yet
- Post Dural Puncture Headache - UpToDateDocument17 pagesPost Dural Puncture Headache - UpToDateBarbarita Alvarado CamposNo ratings yet
- Stroke - Severity - Modified - The - Effect - of - Chronic.66 TromboliziraniDocument5 pagesStroke - Severity - Modified - The - Effect - of - Chronic.66 TromboliziraniM StojanovskaNo ratings yet
- Panic Disorder in Patients Presenting To The Emergency Department With Chest Pain: Prevalence and Presenting SymptomsDocument7 pagesPanic Disorder in Patients Presenting To The Emergency Department With Chest Pain: Prevalence and Presenting SymptomsNasriNo ratings yet
- International Journal of Surgery Case Reports: Mekuanint Asmare, Liyew Ewnetu, Kumlachew GetaDocument3 pagesInternational Journal of Surgery Case Reports: Mekuanint Asmare, Liyew Ewnetu, Kumlachew GetanukeNo ratings yet
- HypertensiDocument7 pagesHypertensizazaNo ratings yet
- Jurnal UtamaDocument8 pagesJurnal UtamaUhti JahrotunisaNo ratings yet
- Neshige 2015Document5 pagesNeshige 2015belleswanNo ratings yet
- A Study On Assessment of Frequency, Intensity, Disability and Severity Associated With Primary HeadachesDocument7 pagesA Study On Assessment of Frequency, Intensity, Disability and Severity Associated With Primary HeadachesDhEg LieShh WowhNo ratings yet
- Pain Agitation DeliriumDocument10 pagesPain Agitation DeliriumMelati HasnailNo ratings yet
- 22 Ajner 7 1 2017Document8 pages22 Ajner 7 1 2017Aqnha AulyaNo ratings yet
- BallDocument8 pagesBallAllan Alejandro SevillaNo ratings yet
- Thailand Anest,+02-Raviwan-FinalDocument8 pagesThailand Anest,+02-Raviwan-FinalAldaherlen BangunNo ratings yet
- The Effectiveness of Early Position Change Postcardiac Catheterization On Patient's Outcomes A Randomized Controlled TrialDocument9 pagesThe Effectiveness of Early Position Change Postcardiac Catheterization On Patient's Outcomes A Randomized Controlled TrialAdelia putriNo ratings yet
- Content ServerDocument8 pagesContent ServerG. Araya MoraNo ratings yet
- Medi 97 E10919Document4 pagesMedi 97 E10919oktaviaNo ratings yet
- 21 Iajps21072017Document4 pages21 Iajps21072017Baru Chandrasekhar RaoNo ratings yet
- StudyDocument23 pagesStudyJose Paul RaderNo ratings yet
- Cefalea PospuncionDocument31 pagesCefalea Pospuncionmanolo.mendozavNo ratings yet
- 26 PDFDocument5 pages26 PDFBaru Chandrasekhar RaoNo ratings yet
- A Comprehensive Update On The Treatment and Management of Postdural Puncture HeadacheDocument9 pagesA Comprehensive Update On The Treatment and Management of Postdural Puncture HeadacheFirjatullahNo ratings yet
- Korea Video ProgramDocument12 pagesKorea Video Programmaya permata sariNo ratings yet
- Comparision Between Provisional Diagnosis Made in Emergency Department VS Final Discharge Diagnosis at Ramkrishna Care Hospital, Raipur C.GDocument14 pagesComparision Between Provisional Diagnosis Made in Emergency Department VS Final Discharge Diagnosis at Ramkrishna Care Hospital, Raipur C.GIJAR JOURNALNo ratings yet
- Treatment Options For Patellar Tendinopathy: A Systematic ReviewDocument12 pagesTreatment Options For Patellar Tendinopathy: A Systematic ReviewEstefa Roldan RoldanNo ratings yet
- Effectiveness of Chinese Hand Massage On Anxiety Among Patients Awaitng Coronary AngiographyDocument8 pagesEffectiveness of Chinese Hand Massage On Anxiety Among Patients Awaitng Coronary AngiographyLia AgustinNo ratings yet
- Research Article Published in Plose One - Manish Chandra PrabhakarDocument6 pagesResearch Article Published in Plose One - Manish Chandra PrabhakarManish Chandra Prabhakar100% (1)
- Treatment Options For Patellar Tendinopathy A Systematic ReviewDocument12 pagesTreatment Options For Patellar Tendinopathy A Systematic ReviewRonny Araya AbarcaNo ratings yet
- Postdural Puncture Headache A Headache ARTICULO 1Document8 pagesPostdural Puncture Headache A Headache ARTICULO 1alejandro rodriguezNo ratings yet
- HHS Public AccessDocument14 pagesHHS Public AccessPepe OcaNo ratings yet
- Swallowing Rehabilitation Following Spinal Injury A Case SeriesDocument12 pagesSwallowing Rehabilitation Following Spinal Injury A Case SeriesniekoNo ratings yet
- Quotes On ESIsDocument2 pagesQuotes On ESIsArt Levine, Mental Health Inc.No ratings yet
- Study To Determine The Role of Platelet Rich Plasma Injection in Treatment of Frozen Shoulder in Terms of Improvement in PainDocument5 pagesStudy To Determine The Role of Platelet Rich Plasma Injection in Treatment of Frozen Shoulder in Terms of Improvement in PainEditor IJETBSNo ratings yet
- Precedex Delirium Spine - AA2023Document9 pagesPrecedex Delirium Spine - AA2023Ahida VelazquezNo ratings yet
- Plan of Thesis VishalDocument24 pagesPlan of Thesis Vishalvishaljha86No ratings yet
- DrugDocument7 pagesDrugIhdina Hanifa Hasanal IbrahimNo ratings yet
- Rooij Et Al-2016-Arthritis Care & ResearchDocument12 pagesRooij Et Al-2016-Arthritis Care & ResearchJennifer JaneNo ratings yet
- The Outcomes of Serial Cerebrospinal Fluid Removal in Elderly Patients With Idiopathic Normal Pressure HydrocephalusDocument7 pagesThe Outcomes of Serial Cerebrospinal Fluid Removal in Elderly Patients With Idiopathic Normal Pressure Hydrocephalusmutia nur rahmiNo ratings yet
- Investigating The Impact of Foot Reflexology On SeDocument6 pagesInvestigating The Impact of Foot Reflexology On Segitha noviaNo ratings yet
- IJTPR, Vol 13, Issue 10, Article 8Document4 pagesIJTPR, Vol 13, Issue 10, Article 8Jaldeep PatelNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofnaufal12345No ratings yet
- Giovannetti (2019) - Cognition and Cerebral Infarction in Older Adults After Surgical Aortic Valve ReplacementDocument8 pagesGiovannetti (2019) - Cognition and Cerebral Infarction in Older Adults After Surgical Aortic Valve ReplacementVanessaNo ratings yet
- 2020 Invasive Electrical Neuromodulation For The Treatment of Painful Diabetic Neuropathy Systematic Review and Meta-AnalysisDocument9 pages2020 Invasive Electrical Neuromodulation For The Treatment of Painful Diabetic Neuropathy Systematic Review and Meta-AnalysisSafitri MuhlisaNo ratings yet
- Pulsed Radiofrequency ofDocument8 pagesPulsed Radiofrequency ofDiego Pinto PatroniNo ratings yet
- Assessment of The Effect of Epidural Steroid Injection in Patient Having Lumbar RadiculopathyDocument5 pagesAssessment of The Effect of Epidural Steroid Injection in Patient Having Lumbar RadiculopathyIJAR JOURNALNo ratings yet
- Acute LBP ScreenDocument6 pagesAcute LBP ScreenIsnaenyEraKartikaNo ratings yet
- Murottal Al-Qur'An Stimulation For Reducing Anxiety Level On Acute Coronary Syndrome Patient: A Practice Based On EvidenceDocument9 pagesMurottal Al-Qur'An Stimulation For Reducing Anxiety Level On Acute Coronary Syndrome Patient: A Practice Based On EvidenceDesi Ratna SariNo ratings yet
- Chen 2017Document7 pagesChen 2017Miranti Dea DoraNo ratings yet
- Extubation Success Prediction in A Multicentric Cohort of Patients With Severe Brain InjuryDocument9 pagesExtubation Success Prediction in A Multicentric Cohort of Patients With Severe Brain InjuryEdison LucioNo ratings yet
- Efects of Splinting in EpicondylitisDocument8 pagesEfects of Splinting in EpicondylitisMaria Jesus GonzalezNo ratings yet
- Post Swallowing DysfunctionDocument7 pagesPost Swallowing DysfunctionfitrianisyaNo ratings yet
- Patient Safety During Sedation by Anesthesia ProfeDocument8 pagesPatient Safety During Sedation by Anesthesia ProfeIsmar MorenoNo ratings yet
- Content ServerDocument13 pagesContent ServerTisna WennyNo ratings yet
- Assessment of The Effects of Dysphagia Therapy in Patients in The Early Post-Stroke Period: A Randomised Controlled TrialDocument7 pagesAssessment of The Effects of Dysphagia Therapy in Patients in The Early Post-Stroke Period: A Randomised Controlled TrialAlba Fernández GonzálezNo ratings yet
- Kidney Transplant Management: A Guide to Evaluation and ComorbiditiesFrom EverandKidney Transplant Management: A Guide to Evaluation and ComorbiditiesNo ratings yet
- PHREB Form No. 1.1a Application For Accreditationof Specialty ClinicsDocument5 pagesPHREB Form No. 1.1a Application For Accreditationof Specialty ClinicsDawn CasuncadNo ratings yet
- Marketing Authorization Procedure For Pharmaceuticals in Europe - Credevo ArticlesDocument12 pagesMarketing Authorization Procedure For Pharmaceuticals in Europe - Credevo ArticlesvinayNo ratings yet
- Historical SupplyDocument5 pagesHistorical Supplylara torricoNo ratings yet
- You - Stop When You See That Sign. You - Eat in Class. You - Keep Off The Grass! You - Take A Cough Syrup Once A Day. You - Tell My Secret To AnybodyDocument3 pagesYou - Stop When You See That Sign. You - Eat in Class. You - Keep Off The Grass! You - Take A Cough Syrup Once A Day. You - Tell My Secret To AnybodyDaniel D'AlessandroNo ratings yet
- Diagnosis For ParkinsonDocument7 pagesDiagnosis For ParkinsonAnna Mae SuminguitNo ratings yet
- The Status of PPFP in Bangladesh - WP 20 244 - D4I 1 1Document9 pagesThe Status of PPFP in Bangladesh - WP 20 244 - D4I 1 1Ridwanul MosrurNo ratings yet
- Research Note: K. Kumar, Debra Kemmler, and E. Riley HolmanDocument8 pagesResearch Note: K. Kumar, Debra Kemmler, and E. Riley HolmanHandoyo RianNo ratings yet
- Instructions On How To Properly Fill in The WAIRDocument17 pagesInstructions On How To Properly Fill in The WAIRRudy BancoroNo ratings yet
- Towards A Grand Convergence For Child Survival and HealthDocument78 pagesTowards A Grand Convergence For Child Survival and HealthNicholasNo ratings yet
- Personality Disorders in The Icd-11: Spanish Validation of The Picd and The Saspd in A Mixed Community and Clinical SampleDocument33 pagesPersonality Disorders in The Icd-11: Spanish Validation of The Picd and The Saspd in A Mixed Community and Clinical SampleBoskoBuhaNo ratings yet
- IRMA Pediatric Palliative CommunicationDocument40 pagesIRMA Pediatric Palliative CommunicationHelmi IrmawantyNo ratings yet
- Exam CDI 313Document4 pagesExam CDI 313Arianne FarnazoNo ratings yet
- BIO210 Chapter Summary 8Document6 pagesBIO210 Chapter Summary 8Rex BrazilNo ratings yet
- Boost Your Brainpower: Sistema Integrado de Gestión Procedimiento Ejecución de La Formación Profesional IntegralDocument7 pagesBoost Your Brainpower: Sistema Integrado de Gestión Procedimiento Ejecución de La Formación Profesional IntegralDiego Andres Pasachoa AmayaNo ratings yet
- Case Study 1Document6 pagesCase Study 1api-542345721No ratings yet
- Friendly House v. WhitingDocument27 pagesFriendly House v. WhitingLegal MomentumNo ratings yet
- Chapter I: Assessment: Comprehensive Nursing Process RubricDocument4 pagesChapter I: Assessment: Comprehensive Nursing Process RubricErika Cadawan100% (1)
- ClozapineDocument5 pagesClozapineANDREWNo ratings yet
- Dci 230030Document14 pagesDci 230030MARIA LEIVANo ratings yet
- Mukinge College of Nursing PHN JAN 2018: Port HealthDocument39 pagesMukinge College of Nursing PHN JAN 2018: Port HealthBa Mulenga100% (3)
- Safety Panelty Matrix For Contractor: SR - No Type of Safety Violation 1 Warning 2 Warning 3 WarningDocument2 pagesSafety Panelty Matrix For Contractor: SR - No Type of Safety Violation 1 Warning 2 Warning 3 WarningAejaz MujawarNo ratings yet
- General Hazards Tools and Equipment AHADocument1 pageGeneral Hazards Tools and Equipment AHAVijayakumarVageesanNo ratings yet
- Soal UTS Bahasa InggrisDocument3 pagesSoal UTS Bahasa InggrisPutri NayNo ratings yet
- Tamir Hands of ClitroidectomyDocument5 pagesTamir Hands of ClitroidectomyTechnic RealityNo ratings yet
- Annals of Tourism Research: Neil Carr (Associate Professor)Document2 pagesAnnals of Tourism Research: Neil Carr (Associate Professor)Alessandra Tarazona HiromotoNo ratings yet
- 1662725026318-1662725013173-Student Reg Form - BlankDocument4 pages1662725026318-1662725013173-Student Reg Form - BlankRuvarasheNo ratings yet
- Effects of Using Smartphones in Relation To Grade 12 Students Research of Estipona National High SchoolDocument2 pagesEffects of Using Smartphones in Relation To Grade 12 Students Research of Estipona National High SchoolTeacher GHENo ratings yet
- Professional EducationDocument54 pagesProfessional EducationJoshua AlibanNo ratings yet
- Module 2, Section 3 Reflection: The Sugar Film (2014) by Damon GarneauDocument3 pagesModule 2, Section 3 Reflection: The Sugar Film (2014) by Damon GarneauNicole Milan100% (3)