Professional Documents
Culture Documents
Impact of Removable Partial Denture Prosthesis On Chewing Efficiency
Uploaded by
Mădălina ConstantinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Impact of Removable Partial Denture Prosthesis On Chewing Efficiency
Uploaded by
Mădălina ConstantinCopyright:
Available Formats
www.scielo.
br/jaos
http://dx.doi.org/10.1590/1679-775720130046
Impact of removable partial denture prosthesis
on chewing efficiency
Marion BESSADET, Emmanuel NICOLAS, Marine SOCHAT, Martine HENNEQUIN, Jean-Luc VEYRUNE
Clermont Université, Université d'Auvergne, Centre de Recherche en Odontologie Clinique; CHU Clermont-Ferrand, Service d'Odontologie, Hôtel-Dieu France,
Clermont-Ferrand, France.
Corresponding address: Dr. Emmanuel Nicolas - UFR Odontologie, CROC - 11 bd Charles de Gaulle - 630000 Clermont - Ferrand, France - Phone: 04 73
17 73 82 - Fax: 04 73 17 73 88 - e-mail: emmanuel.nicolas@udamail.fr
Submitted: January 16,2016
2013 - Modification: June 3,2016
2013 - Accepted: July 4,2016
2016 2013
2016
abstract
R emovable partial denture prostheses are still being used for anatomic, medical and
economic reasons. However, the impact on chewing parameters is poorly described.
Objectives: The objective of this study was to estimate the impact of removable partial
denture prosthesis on masticatory parameters. Material and Methods: Nineteen removable
partial denture prosthesis (RPDP) wearers participated in the study. Among them, 10
subjects were Kennedy Class III partially edentulous and 9 with posterior edentulism
(Class I). All presented a complete and full dentate opposing arch. The subjects chewed
samples of carrots and peanuts with and without their prosthesis. The granulometry of
the expectorated boluses from carrot and peanuts was characterized by median particle
size (D50), determined at the natural point of swallowing. Number of chewing cycles (CC),
chewing time (CT) and chewing frequency (CF=CC/CT) were video recorded. Results: With
RPDP, the mean D50 values for carrot and peanuts were lower [Repeated Model Procedures
(RMP), F=15, p<0.001] regardless of the type of Kennedy Class. For each food, mean CC, CT
and CF values recorded decreased (RMP, F=18, F=9, and F=20 respectively, p<0.01). With
or without RPD, the boluses’ granulometry values were above the masticatory normative
index (MNI) determined as 4,000 μm. Conclusion: RPDP rehabilitation improves the ability
to reduce the bolus particle size, but does not reestablish fully the masticatory function.
Clinical relevance: This study encourages the clinical improvement of oral rehabilitation
procedure.
Keywords: Rehabilitation. Removable partial denture. Mastication.
Introduction masticatory surface is not the only argument for
absent tooth replacement: esthetics and wedging
According to some studies, dentists often of opposing and neighboring teeth are also
overestimate the functional consequences of important, and thus reasons that lead both patients
edentulous areas. In 1974, Levin8 described the and practitioners to replace missing teeth. It also
“28 teeth syndrome”, which led to systematically raises the question about preserving the integrity
replacing any missing teeth. Subsequently, studies of temporomandibular joints.
tended to emphasize the shortened arch concept, In the case of partial edentulism, and based
which corresponds to a denture comprising 3 to 5 on clinical examination, rehabilitation of the oral
functional units (a functional unit being established function can be obtained with fixed or removable
by a pair of premolars or molars in occlusion) and prosthodontics. The removable partial denture
some authors still tend to defend this concept6,17. prosthesis (RPDP) must be able to restore the
According to Käyser, 12 anterior teeth and 8 chewing function, esthetics and phonetics. It
premolars would be necessary and sufficient to compensates for partial edentulism6. Understanding
ensure the mandibular stability required for secure of the biomechanics involved (appreciation of the
deglutition without aspiration, provided that these tissue’s double nature – teeth and oral tissue – and
teeth are efficient6,17. However, increasing the thus of different behaviors) allows the practitioner
J Appl Oral Sci. 392 2013;21(5):392-6
Impact of removable partial denture prosthesis on chewing efficiency
to design a removable partial denture prosthesis MATERIAL AND Methods
satisfying the requirement of balance during
the function, or in other words establishing and Study design
maintaining lift, stabilization and retention (the The study was prospective and observational,
Housset triad). With these imperatives taken into and the subjects functioned as their own controls.
account, and depending on the number of teeth Recruitment extended over 12 months in the Dental
lost and the type of edentulous areas (bounded Department of the University Hospital of Clermont-
by remaining teeth or without posterior tooth Ferrand, France. The study included voluntary
support), the constraints on the prosthesis will patients and was approved by the local ethics
be different and functional rehabilitation altered. committee (CECIC, 2010/06; IRB number 5044).
Effectively, during mastication, natural or artificial Each subject attended two times for mastication
teeth are not simple tools that mechanically reduce evaluation. The first evaluation was organized
the food to particles and mix saliva and the food without any rehabilitation and the second with
to produce a bolus, easy to swallow. They also are RPDP.
essential to the neuromotor control of chewing and
swallowing, through the sensory receptors10. Any Subjects
oral disease that affects the numbers, the structure The required sample size was estimated from
or the position of the teeth is supposed to have a previous study that measured the carrot bolus
an impact on chewing and, in turn, on nutrition. A granulometry in a group of edentulous subjects
physiological approach is thus necessary to measure rehabilitated with implants procedure 16 . The
to what limits the edentulous status and their oral mean D50 values of the carrot bolus decreased
rehabilitation could affect the chewing function. from 4,800±1,013 μm (without rehabilitation) to
Calculating food bolus granulometry collected 3,292±1,335 μm (with implant rehabilitation).
before swallowing, associated with analysis of Calculations with the epiR package 0.9-30 were
the kinematic parameters developed to produce based on a difference of 1600 μm and a common
this bolus, could help to distinguish patients with standard deviation value of 1,100 μm. That indicated
normal mastication from those with seriously the need for at least 9 subjects with Kennedy Class
impaired mastication1,18. Impaired chewing function I and 9 patients with Kennedy Class III (α=5%,
leads to an increase of food bolus particle size, β=20%). Thus, in 2010, 19 subjects from 24 to
measured by the median particle size of the food 79 years old; 6 men (mean age=50.8±8.1 years)
bolus at swallowing. It has been shown that adults and 13 women (mean age=60.7±11.3 years)
with impaired mastication could be distinguished participated in the study. Their prostheses had been
from those with normal function if the median in place for at least 2 months and they were able to
particle size of the bolus that they produced when eat without difficulty. Among them, 10 were wearing
chewing raw carrot reached a cut-off value of 4 removable partial dentures prosthesis bounded
mm, called the masticatory normative indicator by remaining teeth replacing at most 4 posterior
(MNI)19. The adaptation of chewing behavior to food teeth (maxillary or mandibulary, Kennedy Class III)
hardness can also characterize healthy mastication. and 9 were wearing posterior removable partial
Adaptation to increasing food hardness results in denture prostheses (Kennedy Class I). All subjects
an augmented number of chewing cycles and an presented a complete, full dentate opposing arch.
increase in the chewing sequence duration, with Two prosthodontics experts (calibrated to the
no modification of the chewing frequency (number evaluation) checked the conformity of the prosthetic
of cycles per second) in healthy subjects3,7,13. The design.
mean chewing frequency is slowed down in subjects
with chewing deficiencies while eating any type of Experimental procedure
resistant food. Previous studies on the chewing Two natural foods commonly used in mastication
ability of dentally impaired subjects showed that a studies were used. Subjects were asked to chew
decrease in the number of functionally paired teeth with their prostheses three standardized samples of
and oral rehabilitation with removable dentures carrot (cylinders of 2 cm diameter adjusted in height
were linked to a decrease in CT and CC values to reach a weight of 4.0±0.5 g) and non-salted draw
and to an increased D50 value9,14. Nevertheless, peanuts (selected to reach a weight of 4.0±0.5 g).
the physiological impact of RPDM rehabilitation Afterwards, the subjects were asked to repeat the
has been seldom studied. Also, the objective of operation without wearing their prostheses.
this work was to estimate the impact of partial Video recording was used for evaluation of
edentulous areas rehabilitation by removable partial kinematic parameters12. A digital camera positioned
denture prosthesis with a metallic frame on chewing in front of the subject (face-on) recorded a video
parameters4. of the face. All subjects were asked to close their
eyes while the experimenter placed the food sample
J Appl Oral Sci. 393 2013;21(5):392-6
BESSADET M, NICOLAS E, SOCHAT M, HENNEQUIN M, VEYRUNE JL
on the tongue so as to prevent recognition of the time and 0.92-0.97 for chewing cycles (p<0.01).
food sample. The subjects then had to close the Calculation of external reliability gave an ICC index
mouth and teeth without contracting their muscles, ranging between 0.97-0.98 for chewing time and
keeping the food sample between the tongue and from 0.90 to 0.97 for number of cycles. The method
palate. When prompted by the experimenter, the has previously been validated for healthy, fully
subjects began chewing as naturally as possible. dentate patients and for denture wearers5,12.
The subjects were then asked to chew three
replicates of carrots and peanuts. The first replicate Statistical analysis
was completely masticated and swallowed for Statistical analysis was performed using IBM
training. During this sequence, the chewing time SPSS®20 software. Statistical significance was
was monitored by an investigator and was the set at p<0.05. To evaluate the impact of RPDP
baseline time for the following measurements. For rehabilitation on mastication parameters, the mean
the two other replicates, the patient was instructed values of CC, CT, CF and D50 measured during
to spit out each bolus when they thought it was mastication of carrot and peanuts were compared
ready to be swallowed. If there was a difference with and without RPDP by four repeated model
of more than ±5 s between the chewing times of procedures (RMP) (dependent factor: CC, CT, CF,
the swallowed and the two expectorated replicates, D50; fixed factor: type of food; type of Kennedy
the patient was asked to chew a new piece of the Class). Values were expressed as mean±SD.
test food.
Results
Bolus granulometry analysis
Each chewed bolus (masticate) was collected in Bolus granulometry
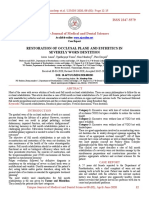
a container, rinsed with water in a 100-μm sieve With RPDP, the mean D50s were significantly
to eliminate saliva, and dried at 80°C for 30 min. decreased for carrot and peanuts (RMP, F=15,
The bolus was then spread onto a transparent A4 p<0.001). These variations were independent of
sheet. The sheet was scanned to produce a 600-dpi the type of Kennedy Class and type of food (Figure
image (Epson Perfection 4990 photo, Seiko Epson 1). With and without RPDP, the mean D50 values
Corporation, Nagano, Japan). The images were then for carrot are above the MNI value of 4,000 μm.
software-processed to evaluate food particle size
and distribution (Powdershape® version 4.3.6 for
Windows, 2005, Innovative Sintering Technologies,
Vilters, Switzerland). For each masticate, the
results were expressed in terms of the D50 value,
characterizing the theoretical sieve size that would
let through 50% of the particle weights14,19. Data
were saved directly in an Excel™ file. Thus, D50
value decreased as food boluses contained more
small particles. According to a previous study, the
two D50 values recorded for each subject and each
natural food were averaged, and D50 values for
carrots above 4 mm were considered as coming
from a subject with impaired mastication19.
Kinematic parameters of mastication
The recorded variables were chewing time (CT:
the time in seconds between the moment the
subject started to chew and swallowing, identified
by the immediate swallow after the end of rhythm
micro-rotary movements) and number of chewing
cycles (CC: number of chewing actions during the
CT period; this included all the rotary patterns, with
and without lip closure). Chewing frequency (CF)
was calculated as the ratio CC/CT. The evaluations of Figure 1- Mean variation ± standard deviation of the
each kinematic parameter required an independent granulometry of the carrot and peanut preswallowed bolus
reading of each video recording by a calibrated (D50, median size of bolus particle) whether a removable
observer who watched the recordings in random prosthesis was worn or not, and according to the type
order15. The internal reliability gave an ICC index of edentulous areas. Repeated measure procedure was
ranging between 0.86-0.98 (p<0.01) for chewing
used for intergroup comparisons (***p<0.001, **p<0.01)
J Appl Oral Sci. 394 2013;21(5):392-6
Impact of removable partial denture prosthesis on chewing efficiency
Table 1- Mean values ± standard deviation of the kinematics parameters of the carrot and peanut mastication (CC, number
of chewing cycles; CT, chewing time; CF, chewing frequency with CF=CC/CT) with and without removable partial denture
(RPD) rehabilitation and for each type of Kennedy class
Kennedy Class I Kennedy Class III
Without RPD With RPD Without RPD With RPD
Carrot CC 44.2±26.9 38.5±19.6 52.7±24.1 44.3±15.3
CT (s) 27.3±15.6 25.9±12.4 33.0±16.1 31.3±10.9
CF (s−1) 1.59±0.21 1.48±0.20 1.63±0.29 1.44±0.3
Peanut CC 44.6±23.0 39.5±20.5 57.0±24.0 48.7±12.6
CT (s) 28.1±13.4 25.5±12.1 38.9±16.4 32.5±9.9
CF (s−1) 1.60±0.35 1.56±0.20 1.56±0.20 1.53±0.27
Discussion
This study aimed at evaluating the impact
of rehabilitation with removable partial denture
prosthesis on chewing parameters. The mastication
variables used in this study were chewing frequency
and the granulometry measured during the
mastication of two test foods: carrots and peanuts.
A decrease in the median particle size of the test
foods boluses and an increase in the chewing
frequency were shown. These results were not
dependent of the type of Kennedy Class.
Some limits of this study could be outlined. In
particular, the participants had their prostheses in
place for at least 2 months and reported no difficulty
for eating. However, the experiment was not strictly
standardized for the time of prosthesis use. It is
possible that a person using oral prosthesis for a
longer period could be more adapted, performing
oral function better than a person with a recent
prosthesis placement. This aspect should be
Figure 2- Mean chewing frequency ± standard deviation explored in further clinical studies. Furthermore,
of the carrot and peanut with and without removable partial chewing adaptation to food hardness was not
assessed in this experiment. According to previous
denture prostheses according to the edentulous areas
studies, three viscoelastic model foods, differing in
(Kennedy Class). Repeated measure procedure was
hardness, could be used to explore if RPDP improves
used for intergroup comparisons (***p<0.001, **p<0.01)
adaptability of mastication7,9.
Kinematic parameters of mastication Granulometry measurement consists in
The mean CC, CT, and CF values measured for comparing median particle size or D50. In this
carrot and peanuts with and without RPDP are study, the D50 value remained above the MNI
presented in Table 1. When comparing mean values value, regardless of the type of edentulous areas,
of CC, CT, and CF, controlling for subject with or or the presence or not of prosthesis. As showed
without RPDP, significant decreases in CC, CT and in preceding studies, this value improved with
CF mean values were shown (RMP procedure, F=18 prostheses rehabilitation but insufficiently11,16. Thus,
for CC, F=9 for CT, and F=20 for CF; p<0.001). it was confirmed, as previously demonstrated in
These variations were independent of the type of other populations, that the number of functional
Kennedy Class and type of food with one exception: units control chewing efficiency2,14. Effectively,
the decrease in the chewing frequency with RPDP feedback controls are necessary for the formation
was dependent of the type of food (F=7, p<0.05) of the food bolus, allowing modulation of muscular
(Figure 2). activity. The involvement of these feedback controls
varies as a function of the loss of periodontal
sensitivity due to edentulous areas. Nonetheless,
a completely edentulous patient will retain their
J Appl Oral Sci. 395 2013;21(5):392-6
BESSADET M, NICOLAS E, SOCHAT M, HENNEQUIN M, VEYRUNE JL
sensing ability through mucosal, muscular and 3- Grigoriadis A, Johansson RS, Trulsson M. Adaptability of
mastication in people with implant-supported bridges. J Clin
temporomandibular joint sensitivity. A previous
Periodontol. 2011;38(4):395‑404.
study showed that wearers of removable dentures
4- Hatch JP, Shinkai RS, Sakai S, Rugh JD, Paunovich ED.
were losing precision in the control force needed Determinants of masticatory performance in dentate adults. Arch
to crush food, a loss directly correlated to the need Oral Biol. 2001;46(7):641‑8.
for a prosthesis9. In an intermediate situation, 5- Hennequin M, Allison PJ, Veyrune JL, Faye M, Peyron M.
partial edentulous subjects with an impaired dental Clinical evaluation of mastication: validation of video versus
electromyography. Clin Nutr. 2005;24(2):314‑20.
status could not produce a food bolus with the
6- Kanno T, Carlsson GE. A review of the shortened dental arch
same particle size distribution as the fully dented concept focusing on the work by the Käyser/Nijmegen group. J
patients7. The reduction in proprioception due to Oral Rehabil. 2006;33(11):850-62.
the lack of dental functional units could not be fully 7- Lassauzay C, Peyron MA, Albuisson E, Dransfield E, Woda A.
compensated by mucosal sensitivity re-attained Variability of the masticatory process during chewing of elastic
model foods. Eur J Oral Sci. 2000;108(6):484‑92.
when wearing prostheses. However, previous
8- Levin B. Editorial: The 28-tooth syndrome - or should all teeth
studies showed that implant-related proprioception be replaced? Dent Surv. 1974;50(7):47.
helped maintaining chewing efficiency3,16. 9- Mishellany-Dutour A, Renaud J, Peyron MA, Rimek F, Woda A. Is
A second variable contributed to the hypothesis the goal of mastication reached in young dentates, aged dentates
that complete chewing function rehabilitation and aged denture wearers? Br J Nutr. 2008;99(1):121‑8.
10- N’gom PI, Woda A. Influence of impaired mastication on
cannot be obtained when using RPDP. The chewing
nutrition. J Prosthet Dent. 2002;87(6):667‑73.
frequency of the food samples in both groups of 11- Nicolas E, Veyrune J, Lassauzay C. A six-month assessment of
edentulous subjects (posterior or bounded by oral health-related quality of life of complete denture wearers using
remaining teeth) decreased significantly (p<0.001) denture adhesive: a pilot study. J Prosthodont. 2010;19(6):443‑8.
when subjects wore removable partial denture 12- Nicolas E, Veyrune JL, Lassauzay C, Peyron MA, Hennequin
M. Validation of video versus electromyography for chewing
prosthesis. Chewing frequency is the mastication
evaluation of the elderly wearing a complete denture. J Oral
rhythm linked to a particular food. Some authors Rehabil. 2007;34(8):566‑71.
specified that chewing frequency is the most 13- Peyron MA, Lassauzay C, Woda A. Effects of increased hardness
reproducible masticatory parameter between tests on jaw movement and muscle activity during chewing of visco-
on the same individual15. Consequently, chewing elastic model foods. Exp Brain Res. 2002;142(1):41‑51.
14- Veyrune JL, Miller CC, Czernichow S, Ciangura CA, Nicolas E,
frequency is often used as one of two parameters
Hennequin M. Impact of morbid obesity on chewing ability. Obes
used to detect chewing deficiency. A lower chewing Surg. 2008;18(11):1467‑72.
frequency is therefore a sign of a disturbed 15- Veyrune JL, Mioche L. Complete denture wearers:
mastication function. The results of this study are in electromyography of mastication and texture perception whilst
agreement with these facts, highlighting a decrease eating meat. Eur J Oral Sci. 2000;108(2):83‑92.
16- Veyrune JL, Opé S, Nicolas E, Woda A, Hennequin M. Changes
in chewing frequency when missing teeth are
in mastication after an immediate loading implantation with
replaced by removable partial denture prosthesis. complete fixed rehabilitation. Clin Oral Investig. 2013;17(4):1127-
The prosthesis constitutes an artificial element that 34.
is more or less stable depending on the type of 17- Witter DJ, van Elteren P, Käyser AF, van Rossum MJ. The effect
edentulous areas and the number of missing teeth, of removable partial dentures on the oral function in shortened
dental arches. J Oral Rehabil. 1989;16(1):27‑33.
as this modifies jaw kinematics.
18- Woda A, Foster K, Mishellany A, Peyron MA. Adaptation of
healthy mastication to factors pertaining to the individual or to
Conclusion the food. Physiol Behav. 2006;89(1):28‑35.
19- Woda A, Nicolas E, Mishellany-Dutour A, Hennequin M, Mazille
This study showed that RPDP rehabilitation does M-N, Veyrune J-L, et al. The masticatory normative indicator. J
Dent Res. 2010;89(3):281‑5.
improve the ability to reduce the bolus particle
size, but is not able to fully restore the masticatory
function. The median bolus granulometry values
measured without or with prostheses remained
above the normative values but the chewing
frequency continues to be impaired.
References
1- Aras K, Hasanreisoğlu U, Shinogaya T. Masticatory performance,
maximum occlusal force, and occlusal contact area in patients with
bilaterally missing molars and distal extension removable partial
dentures. Int J Prosthodont. 2009;22(2):204‑9.
2- Decerle N, Nicolas E, Hennequin M. Chewing deficiencies
in adults with multiple untreated carious lesions. Caries Res.
2013;47(4):330‑7.
J Appl Oral Sci. 396 2013;21(5):392-6
You might also like
- Marcello Machadoetal JPR2017Document9 pagesMarcello Machadoetal JPR2017vivi alfiyani noorNo ratings yet
- Surgical Reconstruction of Interdental PDocument11 pagesSurgical Reconstruction of Interdental PMaria Jose GodoyNo ratings yet
- Gon Alves 2014Document6 pagesGon Alves 2014saulNo ratings yet
- Implant-Supported Removable Partial Dentures in The Mandible A 3-16 Year Retrospective StudyDocument8 pagesImplant-Supported Removable Partial Dentures in The Mandible A 3-16 Year Retrospective StudyMohammad Fadyl YunizarNo ratings yet
- Analysis of Masticatory Cycle EfficiencyDocument4 pagesAnalysis of Masticatory Cycle EfficiencyAndreeaSinNo ratings yet
- 10 1067@mpr 2000 107113Document7 pages10 1067@mpr 2000 107113gbaez.88No ratings yet
- Premium Day Poster COIR 2013Document28 pagesPremium Day Poster COIR 2013juanNo ratings yet
- Clin Implant Dent Rel Res - 2021 - ELsyad - Masseter Muscle Activity of Conventional Denture Fixed Prosthesis and MilledDocument9 pagesClin Implant Dent Rel Res - 2021 - ELsyad - Masseter Muscle Activity of Conventional Denture Fixed Prosthesis and MilledDanielle SoleyNo ratings yet
- Survival of Restored Endodontically Treated Teeth in Relation To Periodontal StatusDocument4 pagesSurvival of Restored Endodontically Treated Teeth in Relation To Periodontal StatusJing XueNo ratings yet
- A Withinpatient Comparative Study of The Influence of Number and Distribution of Ball Attachment Retained Mandibular Overdenture 1011Document6 pagesA Withinpatient Comparative Study of The Influence of Number and Distribution of Ball Attachment Retained Mandibular Overdenture 1011dentureNo ratings yet
- The Retention Characteristics of Hawley and Vacuum-FormedDocument8 pagesThe Retention Characteristics of Hawley and Vacuum-FormedYayis LondoñoNo ratings yet
- Art 2Document6 pagesArt 2Joyce Stefania Posada MauricioNo ratings yet
- Comparative Evaluation of Postoperative Pain and Success Rate A 2017 JournalDocument10 pagesComparative Evaluation of Postoperative Pain and Success Rate A 2017 JournalAlbertoNo ratings yet
- Primary Canine Auto-Transplantation: A New Surgical TechniqueDocument16 pagesPrimary Canine Auto-Transplantation: A New Surgical TechniqueMaryGonzalesʚïɞNo ratings yet
- Implant 1Document8 pagesImplant 1phungNo ratings yet
- MTA Pulpotomy As An Alternative To Root Canal Treatment in Children's Permanent Teeth in A Dental Public Health Setting.Document6 pagesMTA Pulpotomy As An Alternative To Root Canal Treatment in Children's Permanent Teeth in A Dental Public Health Setting.Abdul Rahman AlmishhdanyNo ratings yet
- FMR OcclusionDocument10 pagesFMR OcclusionSkAliHassanNo ratings yet
- 9205 PDFDocument10 pages9205 PDFAlexandraNo ratings yet
- Cekic Nagas2016 PDFDocument8 pagesCekic Nagas2016 PDFAkanksha MahajanNo ratings yet
- Roll Man 2013Document6 pagesRoll Man 2013SergioNo ratings yet
- Esposito2017.PDF Vertical Osseodistraction With A New Intraosseous Alveolar Distractor Prototype For Dental Implant RehabilitationDocument11 pagesEsposito2017.PDF Vertical Osseodistraction With A New Intraosseous Alveolar Distractor Prototype For Dental Implant Rehabilitationdrmezzo68No ratings yet
- Cast Partial Denture Improving Emergence and Masticatory Function - A Case ReportDocument6 pagesCast Partial Denture Improving Emergence and Masticatory Function - A Case ReportIOSRjournalNo ratings yet
- Full Mouth Rehabilitation Using Hobo Twin-Stage TechniqueDocument5 pagesFull Mouth Rehabilitation Using Hobo Twin-Stage TechniqueswagataNo ratings yet
- CCR3 8 1932Document5 pagesCCR3 8 1932Alice EmailsNo ratings yet
- Sedacion Oral Dental OfficeDocument22 pagesSedacion Oral Dental OfficeAngélica Valenzuela AndrighiNo ratings yet
- BIODENTINE EndovitalDocument8 pagesBIODENTINE EndovitalLupu SebastianNo ratings yet
- Long-Term Survival of Indirect Pulp Treatment Performed in Primary and Permanent Teeth With Clinically Diagnosed Deep Carious LesionsDocument4 pagesLong-Term Survival of Indirect Pulp Treatment Performed in Primary and Permanent Teeth With Clinically Diagnosed Deep Carious LesionsBAHAMON TRUJILLO MAYRA ALEJANDRANo ratings yet
- Jensen2016 PDFDocument7 pagesJensen2016 PDFchetna yogeshNo ratings yet
- Cju 005Document5 pagesCju 005gifar ihsanNo ratings yet
- Complications in The Use of The Mandibular Body, Ramus and Symphysis As Donor Sites in Bone Graft Surgery. A Systematic ReviewDocument9 pagesComplications in The Use of The Mandibular Body, Ramus and Symphysis As Donor Sites in Bone Graft Surgery. A Systematic ReviewBrenda Carolina Pattigno ForeroNo ratings yet
- Impact of Mandibular Conventional Denture and Overdenture On Quality of Life and Masticatory EfficiencyDocument7 pagesImpact of Mandibular Conventional Denture and Overdenture On Quality of Life and Masticatory EfficiencyDiego Ignacio Puerto GodoyNo ratings yet
- Abi Nader S, - Plaque Accumulation Beneath Maxillary All-On-4™ Implant-Supported ProsthesesDocument6 pagesAbi Nader S, - Plaque Accumulation Beneath Maxillary All-On-4™ Implant-Supported ProsthesesAnsaquilo AnsaquiloNo ratings yet
- Rehab of Severley Worn Dentition-Using Fixed and RemovableDocument0 pagesRehab of Severley Worn Dentition-Using Fixed and RemovableFaheemuddin MuhammadNo ratings yet
- Artigo 5Document9 pagesArtigo 5joao pauloNo ratings yet
- Función Masticatoria en Pacientes Con Deformidades Dentofaciales Antes y Después Del Tratamiento Ortognático - Un Estudio Prospectivo, Longitudinal y ControladoDocument6 pagesFunción Masticatoria en Pacientes Con Deformidades Dentofaciales Antes y Después Del Tratamiento Ortognático - Un Estudio Prospectivo, Longitudinal y Controladocd.brendasotofloresNo ratings yet
- Comparative Evaluation of Effect of Denture Adhesives On Retention ofDocument6 pagesComparative Evaluation of Effect of Denture Adhesives On Retention ofdentureNo ratings yet
- A One Year Pilot Prospective Multicenter StudyDocument10 pagesA One Year Pilot Prospective Multicenter StudyEly Valentina Contreras ArceoNo ratings yet
- A Review On Chewing Efficiency of Completely Edentulous Patients With Various DenturesDocument11 pagesA Review On Chewing Efficiency of Completely Edentulous Patients With Various DenturesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Restoration of Occlusal Plane and Esthetics in Severely Worn DentitionDocument4 pagesRestoration of Occlusal Plane and Esthetics in Severely Worn DentitionUJ CommunicationNo ratings yet
- Complications Associated With The Ball, Bar and Locator Attachments For Implant-Supported OverdenturesDocument7 pagesComplications Associated With The Ball, Bar and Locator Attachments For Implant-Supported OverdenturesDr FarhatNo ratings yet
- Fixed Versus Removable Orthodontic Appliances To Correct Anterior Crossbite in The Mixed Dentition-A Randomized Controlled Trial PDFDocument6 pagesFixed Versus Removable Orthodontic Appliances To Correct Anterior Crossbite in The Mixed Dentition-A Randomized Controlled Trial PDFJejeNo ratings yet
- Maxillary Dentoalveolar Assessment Following Retraction of Maxillary Incisors: A Preliminary StudyDocument8 pagesMaxillary Dentoalveolar Assessment Following Retraction of Maxillary Incisors: A Preliminary StudyAndrea TokumotoNo ratings yet
- Bone Augmentation of The Edentulous Maxilla For Implant Placement: A Systematic ReviewDocument12 pagesBone Augmentation of The Edentulous Maxilla For Implant Placement: A Systematic ReviewJarvin Miguel Buitrago GalindezNo ratings yet
- Patient Satisfaction With Implant Overdentures and ConventionalDocument7 pagesPatient Satisfaction With Implant Overdentures and ConventionalSandrinaPufinaNo ratings yet
- 1 s2.0 S0022391321004947 Main 2Document7 pages1 s2.0 S0022391321004947 Main 2Daniela Calderón CélleriNo ratings yet
- Responsiveness of Methods To Evaluate Chewing Ability After Removable Partial Denture TreatmentsDocument21 pagesResponsiveness of Methods To Evaluate Chewing Ability After Removable Partial Denture Treatmentsdrg Triani UmaiyahNo ratings yet
- Removable Prosthodontics: Denture AdhesivesDocument2 pagesRemovable Prosthodontics: Denture AdhesivespaulinaNo ratings yet
- Various Concepts of Occlusion in Full MouthDocument5 pagesVarious Concepts of Occlusion in Full Mouthdea swastikaNo ratings yet
- Submergence of Vital Root For Preservation of Residual RidgeDocument0 pagesSubmergence of Vital Root For Preservation of Residual RidgeFaheemuddin MuhammadNo ratings yet
- Long Term Ao4 ReviewDocument13 pagesLong Term Ao4 ReviewjosfranNo ratings yet
- Prosthodontic Rehabilitation of Cleft Lip and Palate Patients Using Conventional Methods: A Case SeriesDocument6 pagesProsthodontic Rehabilitation of Cleft Lip and Palate Patients Using Conventional Methods: A Case SeriesAkanksha MahajanNo ratings yet
- Implant Supported Dentures and Masticatory PerformanceDocument1 pageImplant Supported Dentures and Masticatory PerformanceSandrinaPufinaNo ratings yet
- Effect of Occlusal SplintDocument6 pagesEffect of Occlusal SplintDr. Zardasht N. BradostyNo ratings yet
- Socket Shield Otto Zuhr Hurzeler PDFDocument12 pagesSocket Shield Otto Zuhr Hurzeler PDFLozovan GregoryNo ratings yet
- Over Sem EsplintarDocument9 pagesOver Sem EsplintarClaudia BrilhanteNo ratings yet
- Preservação AlveolarDocument14 pagesPreservação AlveolarMarcela ResendeNo ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMI PDFDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMI PDFAlla MushkeyNo ratings yet
- Schropp Et Al (2005) Immediate Vs Delayed IJOMIDocument9 pagesSchropp Et Al (2005) Immediate Vs Delayed IJOMIAlla MushkeyNo ratings yet
- Stability of Orthodontic Treatment Outcome in Relation To Retention Status: An 8-Year Follow-UpDocument7 pagesStability of Orthodontic Treatment Outcome in Relation To Retention Status: An 8-Year Follow-UpNeeraj AroraNo ratings yet
- 02 Digestive SystemDocument18 pages02 Digestive Systemnaseer alfahdNo ratings yet
- Dysphagia From A Neurogeriatric Point of ViewDocument6 pagesDysphagia From A Neurogeriatric Point of ViewVanessaCarrilloNo ratings yet
- Effects of Resistive Jaw-Opening Exercise With Elastic Bands On Suprahyoid Muscle Activation in Normal SubjectsDocument8 pagesEffects of Resistive Jaw-Opening Exercise With Elastic Bands On Suprahyoid Muscle Activation in Normal Subjectsximena MarchantNo ratings yet
- Muscles OinaDocument3 pagesMuscles Oinageldevera100% (2)
- Mewing Script - Feb8 PDFDocument14 pagesMewing Script - Feb8 PDFRicardo Vallejo0% (3)
- Digestive SystemDocument60 pagesDigestive SystemdrynwhylNo ratings yet
- UW - Fluoro ProtocolDocument57 pagesUW - Fluoro ProtocolIbrahim Mohammed Mohammed MorshedNo ratings yet
- Anatomy & Physiology Outlines - Finals (Chapter 16: Digestive)Document15 pagesAnatomy & Physiology Outlines - Finals (Chapter 16: Digestive)Dahrell Lopez BautistaNo ratings yet
- Dysphagia Diagnosis 1and Treatment (Olle Ekberg) (Z-Lib - Org) (1) - 83-284Document202 pagesDysphagia Diagnosis 1and Treatment (Olle Ekberg) (Z-Lib - Org) (1) - 83-284Macarena Paz ÁlvarezNo ratings yet
- 2019 CIS - 1 Dysphagia - Odynaphagia - Atypical CPDocument22 pages2019 CIS - 1 Dysphagia - Odynaphagia - Atypical CPorangenarwhalNo ratings yet
- PAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaDocument5 pagesPAPER (ENG) - Swallowing Disturbance Questionnaire For Detecting DysphagiaAldo Hip NaranjoNo ratings yet
- Pharynx Lecture 8Document7 pagesPharynx Lecture 8Amy KochNo ratings yet
- Disfagia JPGN 2023Document8 pagesDisfagia JPGN 2023monicarodriguezsalas82No ratings yet
- Swallowing Analyses of Neonates and Infants in Breastfeeding and Bottle-Feeding: Impact On Video Uoroscopy Swallow StudiesDocument11 pagesSwallowing Analyses of Neonates and Infants in Breastfeeding and Bottle-Feeding: Impact On Video Uoroscopy Swallow Studiesantonio gabriel egea castilloNo ratings yet
- Digestive System Anatomy and Physiology - NurseslabsDocument33 pagesDigestive System Anatomy and Physiology - NurseslabsMari FeNo ratings yet
- Yano Et Al. (2014)Document11 pagesYano Et Al. (2014)Paula Acuña UrrutiaNo ratings yet
- 2012 Digestive System in ManDocument52 pages2012 Digestive System in ManhueymeyNo ratings yet
- Chapter 7 - The Digestive SystemDocument65 pagesChapter 7 - The Digestive SystemLama AlqarniNo ratings yet
- Tongue Strength in Children With and Without Speech Sound DisordersDocument12 pagesTongue Strength in Children With and Without Speech Sound DisordersJuliza Tatiana Suárez PatarroyoNo ratings yet
- Effect of Swallowing Rehabilitation Protocol On Swallowing Function in Patients With Esophageal Atresia Andor Tracheoesophageal Fistula.Document6 pagesEffect of Swallowing Rehabilitation Protocol On Swallowing Function in Patients With Esophageal Atresia Andor Tracheoesophageal Fistula.Anonymous xvlg4m5xLXNo ratings yet
- Digestion and AbsorptionDocument38 pagesDigestion and Absorptionapi-226664928No ratings yet
- NCP On SahDocument21 pagesNCP On SahDr-Sanjay SinghaniaNo ratings yet
- Anatomy & Physiology of PharynxDocument22 pagesAnatomy & Physiology of PharynxArvind SangaviNo ratings yet
- Digestive Physiology-LectureDocument58 pagesDigestive Physiology-Lectureisabella brantonNo ratings yet
- Schussler's Tissue Salts (Cell Salts)Document269 pagesSchussler's Tissue Salts (Cell Salts)poiuytrewqNo ratings yet
- FDA Industry Guidance For Size Shape PhysicalDocument11 pagesFDA Industry Guidance For Size Shape PhysicalAhmed AliNo ratings yet
- Treatment of Oropharyngeal Dysphagia CarolMcKee (1) DPNS StudyDocument23 pagesTreatment of Oropharyngeal Dysphagia CarolMcKee (1) DPNS Studyconstantineelia100% (1)
- Progressive Balbar Palsy: Dr. Mohamed Ali 3 Year MD IM ResidentDocument15 pagesProgressive Balbar Palsy: Dr. Mohamed Ali 3 Year MD IM ResidentMohamed AliNo ratings yet
- Speech Therapy RehabilitationDocument5 pagesSpeech Therapy RehabilitationMian Imran IqbalNo ratings yet
- Barium StudiesDocument16 pagesBarium StudiesRuby Dela RamaNo ratings yet