Professional Documents
Culture Documents
Pleomorphic Carcinoma of The Lung: Relationship Between CT Findings and Prognosis
Uploaded by
Yuriansyah Dwi Rahma PutraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pleomorphic Carcinoma of The Lung: Relationship Between CT Findings and Prognosis
Uploaded by
Yuriansyah Dwi Rahma PutraCopyright:
Available Formats
Cardiopulmonar y Imaging • Original Research
Fujisaki et al.
CT of Pleomorphic Carcinoma of the Lung
Cardiopulmonary Imaging
Original Research
Downloaded from www.ajronline.org by 103.125.234.201 on 10/01/20 from IP address 103.125.234.201. Copyright ARRS. For personal use only; all rights reserved
Pleomorphic Carcinoma of the
Lung: Relationship Between CT
Findings and Prognosis
Akitaka Fujisaki1 OBJECTIVE. The objective of our study was to assess the radiologic and clinical findings
Takatoshi Aoki1 of pleomorphic carcinoma (PC) of the lung and to evaluate whether there are any character-
Takahiko Kasai2,3 istic features that can be used to predict prognosis.
Shunsuke Kinoshita1 MATERIALS AND METHODS. Forty-four consecutive patients whose diagnosis of
Yoshinori Tomoda4 PC was histologically confirmed through resection of the lung tumor were included in this
study. The clinical and CT findings of these patients were retrospectively reviewed. Two tho-
Fumihiro Tanaka5
racic radiologists evaluated the CT findings including the size, location, internal character-
Kazuhiro Yatera6 istics, and margin characteristics of the tumors and the presence of chest wall invasion, me-
Hiroshi Mukae 6 diastinal invasion, and surrounding lung abnormalities. A multivariate analysis by the Cox
Yukunori Korogi1 proportional hazards regression model was used to identify variables that can be used to pre-
dict overall survival and disease-free survival.
Fujisaki A, Aoki T, Kasai T, et al.
RESULTS. In the patients with PC, a central low-attenuation area or cavity (40/44, 91%),
chest wall invasion (19/44, 43%), and pulmonary emphysema (30/44, 68%) were frequently
observed on CT. On multivariate analysis, a massive central low-attenuation area or cavity
Keywords: CT, lung cancer, pleomorphic carcinoma,
prognosis
(> 25% of the lesion) on CT indicating necrosis was the only significant independent factor for
overall survival and disease-free survival (p < 0.05). Clinical findings, the presence of lymph
DOI:10.2214/AJR.15.15542 node metastasis at surgery, and postoperative pathologic stage were not significant predictors
of overall survival and disease-free survival.
Received August 30, 2015; accepted after revision
CONCLUSION. A massive central low-attenuation area or cavity on CT was the only
February 1, 2016.
predictor of overall survival and disease-free survival in patients with lung PC.
1
Department of Radiology, University of Occupational
leomorphic carcinoma (PC) is a and showed that the 5-year survival rate of
P
and Environmental Health School of Medicine,
1-1 Iseigaoka, Yahatanishi-ku, Kitakyushu 807-8555,
subtype of sarcomatoid carcino- the sarcomatoid lung tumor patients (24.5%)
Japan. Address correspondence to T. Aoki
(a-taka@med.uoeh-u.ac.jp). ma that contains a component of was significantly less than that of the patients
sarcoma or sarcomalike (spindle with other types of NSCLC (46.3%).
2
Department of Pathology, National Hospital Organization cells, giant cells, or both) differentiation. Ac- Although several clinicopathologic studies
Kinki-Chuo Chest Medical Center, Sakai, Japan. cording to the criteria of the World Health of lung PC have been reported in the litera-
3
Department of Pathology and Oncology, University of
Organization classification [1], PC of the lung ture, there are few studies about its radiologic
Occupational and Environmental Health School of is defined as a poorly differentiated non– features [7, 8]. Moreover, to our knowledge,
Medicine, Kitakyushu, Japan. small cell lung carcinoma (NSCLC) contain- the correlation of CT findings with prognosis
4
ing spindle cells, giant cells, or both or a car- has not been described to date. The purpose
Cancer Therapy Center, Tobata Kyoritsu Hospital,
cinoma consisting of only spindle and giant of our study was to assess the radiologic and
Kitakyushu, Japan.
cells. At least 10% of the carcinoma should be clinical findings of lung PC and to evaluate
5
Second Department of Surgery, University of composed of spindle cells, giant cells, or both whether there are any characteristic features
Occupational and Environmental Health School of for it to be classified as a PC. This tumor is that predict the prognosis.
Medicine, Kitakyushu, Japan. rare, and its incidence has been reported to be
6
Department of Respiratory Medicine, University of
0.1–0.4% of all lung malignancies [2, 3]. Pa- Materials and Methods
Occupational and Environmental Health School of tients with PC tend to present at a more ad- Our institutional review board approved this
Medicine, Kitakyushu, Japan. vanced stage and to have a poorer prognosis study, and informed consent was waived for ret-
than those with a common type of NSCLC rospective review of patient records and images.
AJR 2016; 207:289–294 [3–5]. Martin et al. [6] compared the 5-year
0361–803X/16/2072–289
survival rate of 63 sarcomatoid lung tumor Patients and Clinical Findings
patients with that of propensity score– The medical records of 59 Asian patients with
© American Roentgen Ray Society matched patients with other types of NSCLC a diagnosis of lung PC at our hospital between
AJR:207, August 2016 289
Fujisaki et al.
June 1995 and December 2013 were retrospective- resection (n = 1), segmentectomy (n = 5), lobecto- gle-detector helical CT unit. For the MDCT ex-
ly reviewed, and patients who had undergone sur- my (n = 35), or pneumonectomy (n = 3) was per- aminations, the following parameters were used:
gical resection of the lung tumor, had undergone formed. Eight patients had undergone CT more 2.0-mm section width with 2.0-mm reconstruc-
contrast-enhanced CT before surgery, and had than 2 months before surgery in addition to the tion interval, pitch (ratio of table travel per rota-
not been given any anticancer drugs before sur- preoperative CT study; therefore, tumor growth tion to total beam width) of 15, 120 kVp, and 300
gery were included in this study. PET/CT was per- could be evaluated using the previous CT exami- mA. For the single-detector CT examinations, the
Downloaded from www.ajronline.org by 103.125.234.201 on 10/01/20 from IP address 103.125.234.201. Copyright ARRS. For personal use only; all rights reserved
formed in 27 of the 59 patients and detected occult nation and the preoperative CT examination. CT following parameters were used: 10-mm section
metastasis in five patients. Fifteen patients were observation periods of the eight patients ranged thickness, 120 kVp, 150 mA, and a table speed
excluded from the study for the following reasons: from 70 to 329 days. The medical record of each of 10 mm/s. For additional scanning of the tumor
11 patients received neoadjuvant chemotherapy patient was reviewed by two of the authors for the using the single-detector CT unit, the following
before CT, two patients underwent needle biopsy following: age, sex, smoking habits, treatment, and parameters were used: 2.0-mm section thickness,
without surgical resection for PC diagnosis, and long-term clinical status after surgery (i.e., recur- 120 kVp, and 250 mA. All images were reviewed
two patients did not undergo contrast-enhanced rence, metastasis, or survival). on an ultra-high-resolution gray-scale monitor
CT. Thus, 44 patients were included in this study. (20.8 inches [27.4 cm], 2048 × 1560 pixels; Coro-
The time interval between the final preopera- CT Analysis nis 3MP, BARCO Display Systems) using stan-
tive CT examination and surgery ranged from 2 to Scanning of the whole lungs was performed dard lung window settings (window width, 1600
26 days. Surgical resection in the form of a wedge on a 4-, 16-, 32-, or 64-MDCT unit or on a sin- HU; window level, –600 HU) and mediastinal
A B
C D
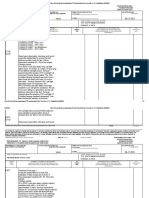
Fig. 1—63-year-old man with pleomorphic carcinoma (PC) of lung. Liver metastasis was detected 7 months after surgery, and patient died of disease
9 months after surgery.
A, CT image obtained before surgery shows grossly irregular nodule and centrilobular emphysema.
B, CT image obtained before surgery shows central low-attenuation area; this finding indicates necrosis is present within tumor.
C, Low-power photomicrograph of histologic specimen shows extensive necrosis in central portion of tumor.
D, High-power photomicrograph shows predominantly atypical multinucleated giant cells (arrows).
290 AJR:207, August 2016
CT of Pleomorphic Carcinoma of the Lung
window settings (window width, 350 HU; win- TABLE 1: Thin-Section CT Findings of 44 Patients With Lung
dow level, 50 HU). Pleomorphic Carcinoma
Two radiologists with 24 and 10 years of ex-
CT Findings No. (%) of Patients
perience in interpreting thoracic CT, respectively,
evaluated the CT examinations for the size, loca- Tumor size
tion, internal characteristics (i.e., central low-atten- ≤ 30 mm 18 (40.9)
Downloaded from www.ajronline.org by 103.125.234.201 on 10/01/20 from IP address 103.125.234.201. Copyright ARRS. For personal use only; all rights reserved
uation area or cavity and calcification), and margin
> 30 mm 26 (59.1)
characteristics of the tumors and for the presence
of chest wall invasion, mediastinal invasion, and Internal characteristics
surrounding lung abnormalities (i.e., emphysema Central low-attenuation area or cavity 40 (90.9)
or interstitial pneumonia). A central low-attenua- > 25% of the lesion 27 (61.4)
tion area or cavity was defined as an internal area
Calcification 0 (0)
with low attenuation relative to the attenuation of
the surrounding musculature. We used unenhanced Margin characteristics
CT images for differentiating a tumor with a cen- Sharp and smooth 0 (0)
tral low-attenuation area or cavity from a tumor Some irregular undulations 27 (61.4)
with rim enhancement. The percentage of the cen-
Grossly irregular with spiculations 17 (38.6)
tral low-attenuation area or cavity was semiquanti-
tatively calculated by dividing the area of the low- Chest wall invasion 19 (43.2)
attenuation area or cavity by the total tumor area Mediastinal invasion 11 (25.0)
in the transaxial plane and was classified into two Pulmonary emphysema 30 (68.2)
groups: 0–25% of the lesion and more than 25% of
Interstitial pneumonia 3 (6.8)
the lesion. The reviewers interpreted the images
separately, and a final decision was reached by con-
sensus if their interpretations differed. In the eight ings, vessel invasion, lymph node metastasis, and (40/44, 91%), tumor margin with some irreg-
patients who had undergone a previous CT exami- pathologic stage. Variables with p values < 0.05 by ular undulations (27/44, 61%), chest wall in-
nation before the preoperative CT examination, the univariate analyses were chosen as the variables vasion (19/44, 43%), and pulmonary emphy-
method originally described by Schwartz [9] was for the multivariate logistic regression analysis. A sema (30/44, 68%) were frequently observed
used to calculate tumor doubling time: multivariate analysis by the Cox proportional haz- on CT (Figs. 1–3). In the majority of cases
ards regression model was used to identify vari- with a central low-attenuation area or cavity,
Tdt = tlog2 / 3log(Dt / D0), ables that can be used to predict prognosis. In- the low-attenuation area or cavity was greater
terobserver agreement for the CT findings was than 25% of the lesion (27/44, 61%). Interob-
where Tdt is the tumor doubling time, t is the time analyzed by computing the intraclass correlation server agreement (kappa value) for the CT
lapse between the two measurements, Dt is the coefficient (ICC). The strength of agreement was findings was excellent (0.86–1.00). The tumor
mean tumor diameter at the final measurement, considered slight for an ICC of 0.40 or less, fair for doubling times (n = 8) based on CT ranged
and D0 is the mean tumor diameter at the ini- an ICC of 0.41–0.60, moderate for an ICC of 0.61– from 53 to 139 days, with a mean of 86.7 days.
tial measurement. 0.80, and excellent for an ICC of 0.81 or greater.
Histopathologic Findings
Histopathologic Analysis Results The pathologic stage of the PC was IA in
All surgical specimens were fixed in the inflated Clinical Features five patients, IB in nine, IIB in 10, IIIA in 11,
state by transpleural and transbronchial infusion of Of the 44 patients in this study, 36 were IIIB in six, and IV in three. Vessel invasion
formalin. The specimens were stained with H and men and eight were women. The age of the was observed in 26 (59%), and lymph node
E. Histopathologic findings (i.e., vessel invasion, patients at the time of PC diagnosis ranged metastasis was seen in 17 (39%) patients.
lymph node metastasis, and pathologic stage) were from 36 to 91 years, with an average of 67.1 Pathologic analysis showed that the areas of
reviewed in the surgical specimens by a lung pa- years. Thirty-nine patients (89%) were smok- tumor necrosis with hemorrhagic foci corre-
thologist for this study. Pathologic staging was per- ers, and 34 (77%) were heavy smokers (> 20 sponded to the massive central low-attenua-
formed according to the classification of the Union pack-years). Twenty-two of the 44 patients tion area or cavity on CT in most patients and
for International Cancer Control [10]. The internal died 3–120 months (mean, 27.5 months) af- that the areas of myxoid degeneration also
characteristics of the tumors seen on CT scans were ter surgery, and 22 patients were alive 5–80 corresponded to the low-attenuation area or
compared with those seen at pathologic examination months (mean, 31.5 months) at the time of cavity on CT in two patients.
of the specimens. The correlations were decided by the most recent follow-up. Fourteen of the 22
consensus of the pathologist and one radiologist. surviving patients were disease-free, and the Correlation Clinical and CT Features
remaining eight had disease progression. With Prognosis
Statistical Method A univariate analysis of the prognostic
Overall survival and disease-free survival were CT Findings factors influencing overall survival and dis-
calculated according to the Kaplan-Meier method. The results of the CT findings in all pa- ease-free survival is summarized in Table
Univariate analyses were performed to determine tients with lung PC are summarized in Ta- 2. A massive central low-attenuation area or
the influence of age, sex, smoking habits, CT find- ble 1. A central low-attenuation area or cavity cavity on CT and advanced pathologic stage
AJR:207, August 2016 291
Fujisaki et al.
TABLE 2: Univariate Analysis of Prognostic Factors Influencing O verall (stage III–IV) predicted poorer overall sur-
Survival and Disease-Free Survival of Patients With Lung vival (p < 0.05; Fig. 4). A massive central
Pleomorphic Carcinoma low-attenuation area or cavity on CT, lymph
p
node metastasis, and advanced stage (stage
III–IV) predicted poorer disease-free surviv-
Disease-Free al (p < 0.05; Fig. 5). A multivariate analysis
Downloaded from www.ajronline.org by 103.125.234.201 on 10/01/20 from IP address 103.125.234.201. Copyright ARRS. For personal use only; all rights reserved
Prognostic Factors Overall Survival Survival of the prognostic factors influencing overall
Age 0.4752 0.4097 survival and disease-free survival is summa-
Sex 0.8856 0.1113 rized in Table 3. A massive central low-at-
tenuation area or cavity on CT indicating ne-
Smoking index > 20 pack-years 0.6352 0.7959
crosis was the only significant independent
Tumor size > 30 mm 0.2706 0.1980 factor for predicting prognosis (p < 0.05).
Central low-attenuation area or cavity > 25% of the lesion 0.0038 0.0133
Margins grossly irregular with spiculations 0.1586 0.7580 Discussion
The results of our study showed that a
Chest wall invasion 0.2836 0.2931
massive central low-attenuation area or cav-
Mediastinal invasion 0.2922 0.6088 ity on CT was the only significant indepen-
Pulmonary emphysema or interstitial pneumonia 0.1648 0.1231 dent factor for predicting prognosis (p <
Vessel invasion 0.1007 0.2317 0.05); pathologic stage was not a significant
predictor. Surgical resection alone is there-
Lymph node metastasis 0.0637 0.0232
fore insufficient in patients with this find-
Stage (I–II vs III–IV) 0.0184 0.0266 ing on CT even if the pathologic stage is not
advanced, and the combination of extensive
TABLE 3: Multivariate Analysis of Prognostic Factors Influencing O
verall surgical intervention with aggressive postop-
Survival and Disease-Free Survival of Patients With Lung erative chemotherapy, radiotherapy, or both
Pleomorphic Carcinoma needs to be explored. Given that CT is rou-
tinely performed of most patients with lung
Prognostic Factors Relative Risk 95% CI p
PC, this imaging study is readily available
Overall survival and requires no additional cost. A massive
Central low-attenuation area or cavity > 25% of the lesion 4.739 0.060–0.738 0.0149 central low-attenuation area or cavity on CT
Lymph node metastasis 1.815 0.197–1.546 0.2578 may help in selecting a therapeutic strategy
for patients with lung PC.
Stage (I–II vs III–IV) 1.916 0.180–1.513 0.2312
In most cases in our study, the massive
Disease-free survival central low-attenuation area or cavity seen
Central low-attenuation area or cavity > 25% of the lesion 2.475 0.164–0.994 0.0484 on contrast-enhanced CT scans correspond-
Lymph node metastasis 1.923 0.214–1.262 0.1480
ed to areas of tumor necrosis in pathologic
specimens. Tumor necrosis represents a para-
Stage (I–II vs III–IV) 1.357 0.294–1.848 0.5153
doxical relationship whereby evidence of in-
A B
Fig. 2—36-year-old man with pleomorphic carcinoma of lung. Patient was alive without evidence of recurrence Fig. 3—76-year-old woman with pleomorphic
at 3-year follow-up. carcinoma of lung. Lung metastasis was detected
A and B, CT images obtained before surgery show mass with some irregular undulations (A) and chest wall and 7 months after surgery, and patient died of disease
mediastinal invasion (B). 19 months after surgery. CT image obtained before
surgery shows necrotic cavity within mass.
292 AJR:207, August 2016
CT of Pleomorphic Carcinoma of the Lung
Central low-attenuation area or
1.0 cavity that is greater than 25% 1.0
of lesion (–)
0.8 0.8 Central low-attenuation area or
cavity that is greater than 25%
Cumulative Survival
Cumulative Survival
of lesion (–)
Downloaded from www.ajronline.org by 103.125.234.201 on 10/01/20 from IP address 103.125.234.201. Copyright ARRS. For personal use only; all rights reserved
0.6 p = 0.0038 0.6 p = 0.0133
Central low-attenuation area or
0.4 cavity that is greater than 25% 0.4 Central low-attenuation area or
of lesion (+) cavity that is greater than 25%
of lesion (+)
0.2 0.2
0 0
0 20 40 60 80 100 120 0 20 40 60 80 100 120
Survival (mo) Survival (mo)
Fig. 4—Graph shows overall survival according to CT finding of central low- Fig. 5—Graph shows disease-free survival according to CT finding of central low-
attenuation area or cavity that is greater than 25% of lesion. attenuation area or cavity that is greater than 25% of lesion.
creased tumor cell death indicates that the PC in our study may be explained by these giogenesis through unregulation of vascular
tumor is a more aggressive tumor. This re- unique clinical features. endothelial growth factor, are significantly
lationship can be explained by rapid tumor The imaging findings of lung PC have been greater in lung PC than in lung adenocarci-
growth to a size at which the tumor has out- reported in only a few articles to date. Kim et noma [19]. Because angiogenesis is essential
grown its blood supply [11]. Hypoxia is a char- al. [7] retrospectively evaluated the CT fea- for tumor growth, the overexpression of HIF-
acteristic of invasive cancers that can lead to tures of 10 patients with lung PC and reported 1α and the increase of MVD of lung PC are
the development of an aggressive phenotype that lung PCs preferentially manifest as large also considered causes of rapid growth.
through a mechanism that is mediated mainly peripheral lung neoplasms with a central low- The current study has several limitations.
by hypoxia-inducible factor (HIF)–1 and that attenuation area (80%) and frequently invade First, this study included a relatively small
includes cell immortalization and dedifferen- the pleura or chest wall (70%). Another group number of Asian patients because lung PC
tiation, pH regulation, autocrine growth and of researchers, Kim et al. [8], also assessed is rare. An additional prospective study in a
survival, angiogenesis, invasion and metasta- the CT features of surgically resected lung broader population would yield more com-
sis, and resistance to chemotherapy [12–14]. PC in 30 patients, and a central low-attenua- prehensive results. Second, our study popu-
We speculate that rapid tumor growth leads to tion area or cavity was observed in 50% of the lation did not reflect the entire spectrum of
inadequate blood supply to the central area of patients in their series. In our larger series, a lung PC because we could include only pa-
the tumor, which results in ischemic changes. low-attenuation area or cavity and chest wall tients with surgically resected lung PC and
Extensive necrosis due to ischemic changes invasion were observed in 91% and 43% of because we excluded patients who were
was the most prevalent cause of cavity forma- patients, respectively, and these results con- treated with neoadjuvant chemotherapy.
tion and has been reported to be an indepen- cur with those of previous reports. These re- These factors may have given rise to selec-
dent histologic factor in predicting prognosis sults suggest that lung PC tends to be necrot- tion bias. Third, the difference in surgical
of patients with lung PC [4, 15]. ic, cavitary, and locally invasive. management and the progression of chemo-
Because lung PC is a rare type of lung Rapid growth of lung PC has been sporad- therapy over a relatively long study period
tumor, the studies in the peer-reviewed lit- ically reported [3, 15, 17]; in some cases that may have had an impact on survival. Fourth,
erature on its clinical features are relatively were measurable on CT using the Schwartz in the eight patients who had undergone a
limited. However, several clinical features method, the tumor doubling times were less previous CT examination before the preop-
that are unique to lung PC have been report- than 30 days [3, 15, 17]. In our cases, most erative CT examination, we assessed the CT
ed: PC shows prevalence in male smokers of the tumors grew as rapidly as those in the findings on the preoperative CT examina-
who have a history of heavy tobacco con- past reports, and the tumor doubling times tion (i.e., the later CT examination) because
sumption, and the average age at presenta- were shorter than those of the common types we correlated CT features and postopera-
tion is 60 years [3, 4, 16]. Similar to these of NSCLC [18]. Although the characteristic tive prognosis. Given the aggressive nature
results, our results also showed a male pre- of rapid growth has not fully been explained, of lung PC, the use of the preoperative (later)
dominance (male-female ratio, 4.5:1) and the sarcomatoid elements of lung PC have a images may have biased the CT findings. De-
a clear association with a smoking habit high proliferative activity (MIB1 cell prolif- spite these limitations, we believed that it is
(89% had a history of smoking, the majority eration marker index) and may be related to important to determine the CT findings that
whom were heavy smokers [i.e., > 20 pack- the rapid growth [15]. From another point of can be used to predict prognosis in patients
years]). The high prevalence of pulmonary view, the expression of HIF-1α and microves- with lung PC. Finally, CT software was not
emphysema (68%) surrounding the lung sel density (MVD), which strongly affect an- used in this study for the calculation of tu-
AJR:207, August 2016 293
Fujisaki et al.
mor doubling time because of the retrospec- dle/giant cell) carcinoma of the lung: a clinico- Taylor SG 4th. Tumor necrosis is a prognostic pre-
tive nature of this study. Further study of a pathologic correlation of 78 cases. Cancer 1994; dictor for early recurrence and death in lymph
greater number of cases of lung PC with CT 73:2936–2945 node-positive breast cancer: a 10-year follow-up
software that can perform 3D volume mea- 4. Rossi G, Cavazza A, Sturm N, et al. Pulmonary study of 728 Eastern Cooperative Oncology
surements is likely necessary to characterize carcinomas with pleomorphic, sarcomatoid, or Group patients. J Clin Oncol 1993; 11:1929–1935
tumor growth of lung PC. sarcomatous elements: a clinicopathologic and 13. Semenza GL. HIF-1 inhibitors for cancer therapy:
Downloaded from www.ajronline.org by 103.125.234.201 on 10/01/20 from IP address 103.125.234.201. Copyright ARRS. For personal use only; all rights reserved
In conclusion, a central low-attenuation immunohistochemical study of 75 cases. Am J from gene expression to drug discovery. Curr
area or cavity in PC that occupies greater Surg Pathol 2003; 27:311–324 Pharm Des 2009; 15:3839–3843
than 25% of the tumor is associated with de- 5. Nakajima M, Kasai T, Hashimoto H, Iwata Y, 14. Hiraoka N, Ino Y, Sekine S, et al. Tumour necrosis
creased overall survival and decreased dis- Manabe H. Sarcomatoid carcinoma of the lung: a is a postoperative prognostic marker for pancre-
ease free-survival, more so than pathologic clinicopathologic study of 37 cases. Cancer 1999; atic cancer patients with a high interobserver re-
stage and lymph node metastases of NSCLC. 86:608–616 producibility in histological evaluation. Br J
Recognition of this prognostic factor may 6. Martin LW, Correa AM, Ordonez NG, et al. Sarco- Cancer 2010; 103:1057–1065
have important clinical implications, and fur- matoid carcinoma of the lung: a predictor of poor 15. Fujioka S, Nakamura H, Adachi Y, et al. Pleomor-
ther large-scale study is encouraged to deter- prognosis. Ann Thorac Surg 2007; 84:973–980 phic carcinoma of the lung in which the sarcoma-
mine the appropriate treatment strategy based 7. Kim TH, Kim SJ, Ryu YH, et al. Pleomorphic car- tous element grew rapidly: a case report. Ann Tho-
on CT findings for patients with lung PC. cinoma of lung: comparison of CT features and rac Cardiovasc Surg 2009; 15:111–114
pathologic findings. Radiology 2004; 232:554–559 16. Mochizuki T, Ishii G, Nagai K, et al. Pleomorphic
References 8. Kim TS, Han J, Lee KS, et al. CT finding of surgi- carcinoma of the lung: clinicopathologic charac-
1. Corrin B, Chang YL, Rossi G, et al. Sarcomatoid cally resected pleomorphic carcinoma of the lung teristics of 70 cases. Am J Surg Pathol 2008;
carcinoma. In: Travis WD, Brambilla E, Müller- in 30 patients. AJR 2005; 185:120–125 32:1727–1735
Hermelink HK, Harris CC, eds. World Health 9. Schwartz M. A biomathematical approach to clin- 17. Ito K, Oizumi S, Fukumoto S, et al. Clinical char-
Organization classification of tumors: pathology ical tumor growth. Cancer 1961; 14:1272–1294 acteristics of pleomorphic carcinoma of the lung.
and genetics of tumours of the lung, pleura, thymus 10. Sobin LH, Gospodarowicz MK, Wittekind C, eds. Lung Cancer 2010; 68:204–210
and heart. Lyon, France: IARC Press, 2004:53–58 International Union Against Cancer (UICC) 18. Detterbeck FC, Gibson CJ. Turning gray: the nat-
2. Chang YL, Lee YC, Shih JY, Wu CT. Pulmonary TNM classification of malignant tumours, 7th ed. ural history of lung cancer over time. J Thorac
pleomorphic (spindle) cell carcinoma: peculiar New York, NY: Wiley-Blackwell, 2010 Oncol 2008; 3:781–792
clinicopathologic manifestations different from 11. Swinson DE, Jones JL, Richradson D, et al. Tumour 19. Tsubata Y, Sutani A, Okimoto T, et al. Compara-
ordinary non–small cell carcinoma. Lung Cancer necrosis is an independent prognostic marker in tive analysis of tumor angiogenesis and clinical
2001; 34:91–97 non–small cell lung cancer: correlation with bio- features of 55 cases of pleomorphic carcinoma
3. Fishback NF, Travis WD, Moran CA, Guinee DG logical variables. Lung Cancer 2002; 37:235–240 and adenocarcinoma of the lung. Anticancer Res
Jr, McCarthy WF, Koss MN. Pleomorphic (spin- 12. Gilchrist KW, Gray R, Fowble B, Tormey DC, 2015; 35:389–394
294 AJR:207, August 2016
You might also like
- Jurnal Radio 3Document9 pagesJurnal Radio 3Zakii MuhammadNo ratings yet
- Clear Cell Renal Cell Carcinoma: Associations Between CT Features and Patient SurvivalDocument8 pagesClear Cell Renal Cell Carcinoma: Associations Between CT Features and Patient SurvivalBastian VizcarraNo ratings yet
- Jurnal CT ScanDocument12 pagesJurnal CT ScanJefri Rudolf WomsiworNo ratings yet
- Atlas of Spectral Endoscopic ImagesDocument32 pagesAtlas of Spectral Endoscopic ImagesChargerNo ratings yet
- Tanimura Et Al 2016 Quantitative Assessment of Erector Spinae Muscles in Patients With Chronic Obstructive PulmonaryDocument8 pagesTanimura Et Al 2016 Quantitative Assessment of Erector Spinae Muscles in Patients With Chronic Obstructive Pulmonarysasan.zamani.sasanNo ratings yet
- Linical Eat Res Pri Ar L NG Cancer Presenting As P L Nar Cnsliatin Iicingpne NiaDocument5 pagesLinical Eat Res Pri Ar L NG Cancer Presenting As P L Nar Cnsliatin Iicingpne NiaYusi RizkyNo ratings yet
- CT-Guided Core Biopsy of Lung Lesions: A PrimerDocument11 pagesCT-Guided Core Biopsy of Lung Lesions: A PrimerCristian O. Saavedra RodriguezNo ratings yet
- Oral-Maxillary Sinus Fistula (Oroantral Fistula) :: Clinical Features and Findings On Multiplanar CTDocument4 pagesOral-Maxillary Sinus Fistula (Oroantral Fistula) :: Clinical Features and Findings On Multiplanar CTnataliayobeantoNo ratings yet
- Evaluation of The Relationship Between Age And.4Document4 pagesEvaluation of The Relationship Between Age And.4denizNo ratings yet
- Colorectal Cancer Screening With Odour Material by Canine Scent DetectionDocument7 pagesColorectal Cancer Screening With Odour Material by Canine Scent DetectionJorge RuizNo ratings yet
- Radiology of Chest Wall MassesDocument11 pagesRadiology of Chest Wall MassesDevina BumiNo ratings yet
- 920 FullDocument17 pages920 FullHeru SigitNo ratings yet
- Ajr 17 18384Document10 pagesAjr 17 18384storyofmylife600No ratings yet
- WwasDocument6 pagesWwasChandan SkNo ratings yet
- Appearance of Enhanced Tissue Features in Narrow-Band Endoscopic ImagingDocument10 pagesAppearance of Enhanced Tissue Features in Narrow-Band Endoscopic ImagingAnders AguilarNo ratings yet
- Ajr 09 2463Document7 pagesAjr 09 2463fitriNo ratings yet
- 2022 Article 3346Document5 pages2022 Article 3346فرجني موغNo ratings yet
- Arakawa2016 Article AsbestosisAndOtherPulmonaryFibDocument8 pagesArakawa2016 Article AsbestosisAndOtherPulmonaryFibandres pinillaNo ratings yet
- Unexpectedly High Incidence of VenousDocument3 pagesUnexpectedly High Incidence of VenousfranciscoNo ratings yet
- Evaluation of Lung Ultrasound For The Diagnosis of Pneumonia in The EDDocument7 pagesEvaluation of Lung Ultrasound For The Diagnosis of Pneumonia in The EDAsclepioNo ratings yet
- Diagnostic Accuracy of Oblique Chest Radiograph For Occult Pneumothorax: Comparison With UltrasonographyDocument7 pagesDiagnostic Accuracy of Oblique Chest Radiograph For Occult Pneumothorax: Comparison With UltrasonographyVirni AprieliaNo ratings yet
- Acodaduras Ureterales (Kinking)Document7 pagesAcodaduras Ureterales (Kinking)Clínica CIPRONo ratings yet
- Comparative Analysis of Radiation Dose and Image Quality BetweenDocument5 pagesComparative Analysis of Radiation Dose and Image Quality BetweenIshani Anushika JayakodyNo ratings yet
- Cta Cardiac After CabgDocument6 pagesCta Cardiac After Cabgmirza alfariziNo ratings yet
- Subchondroplasty What TheDocument6 pagesSubchondroplasty What TheikhsanNo ratings yet
- Ajr 1921168Document10 pagesAjr 1921168Arnesh kumar issarNo ratings yet
- Ajr Pulmonary MucorDocument6 pagesAjr Pulmonary MucorNicky ChhajwaniNo ratings yet
- Three-Dimensional Morphology of The Masseter Muscle in Patients With Mandibular PrognathismDocument7 pagesThree-Dimensional Morphology of The Masseter Muscle in Patients With Mandibular PrognathismChavdarNo ratings yet
- Purysko Et Al 2012 Characteristics and Distinguishing Features of Hepatocellular Adenoma and Focal Nodular HyperplasiaDocument9 pagesPurysko Et Al 2012 Characteristics and Distinguishing Features of Hepatocellular Adenoma and Focal Nodular HyperplasiaPatricia Peñaflor GrimaldoNo ratings yet
- CV Ajr.19.22578Document10 pagesCV Ajr.19.22578Andi Wetenri PadaulengNo ratings yet
- Evaluation of Maxillary Sinus Dimensions in GenderDocument8 pagesEvaluation of Maxillary Sinus Dimensions in Gendersignacc362No ratings yet
- CT Predictors of Unfavorable Clinical Outcomes of Acute Right Colonic DiverticulitisDocument10 pagesCT Predictors of Unfavorable Clinical Outcomes of Acute Right Colonic DiverticulitisDiego Andres VasquezNo ratings yet
- What Are The Indications For The Use of Computed Tomography Before Septoplasty?Document3 pagesWhat Are The Indications For The Use of Computed Tomography Before Septoplasty?Putri HakimNo ratings yet
- Optimal Timing of The First Barium Swallow Examination For Diagnosis of Pyriform Sinus FistulaDocument7 pagesOptimal Timing of The First Barium Swallow Examination For Diagnosis of Pyriform Sinus Fistulaflorentulis91No ratings yet
- Jurnal B 1Document10 pagesJurnal B 1Nasayu Nadia Santika AyuNo ratings yet
- CT of Globe Rupture: Analysis and Frequency of FindingsDocument8 pagesCT of Globe Rupture: Analysis and Frequency of FindingsdrmgroaNo ratings yet
- Kim Et Al 2009 Phase II Trial of Concurrent Radiation and Weekly Cisplatin Followed by Vipd Chemotherapy in NewlyDocument6 pagesKim Et Al 2009 Phase II Trial of Concurrent Radiation and Weekly Cisplatin Followed by Vipd Chemotherapy in Newly2512505993No ratings yet
- Pola Cco 2013Document3 pagesPola Cco 2013akivaNo ratings yet
- Art BiopsiasDocument6 pagesArt BiopsiasLinda DávilaNo ratings yet
- Fusion 9.2.3.1 PDFDocument6 pagesFusion 9.2.3.1 PDFGowri ShankarNo ratings yet
- Clinical Analysis of The Short-Term Outcome of Papillary Thyroid Microcarcinoma After I-131 TreatmentDocument8 pagesClinical Analysis of The Short-Term Outcome of Papillary Thyroid Microcarcinoma After I-131 TreatmentĐỗThanhTuấnNo ratings yet
- Recurrence in The Thyroidectomy Bed Sonographic FindingsDocument7 pagesRecurrence in The Thyroidectomy Bed Sonographic Findingspunct_org3256No ratings yet
- Isd 48 121Document5 pagesIsd 48 121kalixinNo ratings yet
- Ajr 2Document10 pagesAjr 2Fika FathiaNo ratings yet
- MRI of Small Hepatocellular Carcinoma: Typical Features Are Less Frequent Below A Size Cutoff of 1.5 CMDocument8 pagesMRI of Small Hepatocellular Carcinoma: Typical Features Are Less Frequent Below A Size Cutoff of 1.5 CMTaffy GultomNo ratings yet
- Lin 2017Document11 pagesLin 2017Ibnu CaesarNo ratings yet
- Scanning Techniques in Computed Body Tomography: Contrast AgentsDocument7 pagesScanning Techniques in Computed Body Tomography: Contrast AgentsNidaa MubarakNo ratings yet
- Computed Tomography in The Diagnosis of Subcapsular and Perirenal HematomaDocument6 pagesComputed Tomography in The Diagnosis of Subcapsular and Perirenal HematomaGordana PuzovicNo ratings yet
- Can Malignant and Benign Pulmonary Nodules Be Differentiated With Diffusion-Weighted MRI?Document7 pagesCan Malignant and Benign Pulmonary Nodules Be Differentiated With Diffusion-Weighted MRI?Patta DaengNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Ahmad Fari Arief LopaNo ratings yet
- Haga 2017Document9 pagesHaga 2017tsania nkdNo ratings yet
- 344 FullDocument7 pages344 Fulleric22hkNo ratings yet
- Matulanya - Applications of Nuclear TechnologyDocument75 pagesMatulanya - Applications of Nuclear TechnologyFlavioMuhaleNo ratings yet
- Anatomical Variationsofthe Foramen MagnumDocument11 pagesAnatomical Variationsofthe Foramen MagnumChavdarNo ratings yet
- Aspecto Linfonodal Fujiwara 2010Document7 pagesAspecto Linfonodal Fujiwara 2010VickNo ratings yet
- IMRT: A Review and Preview: Physics in Medicine & BiologyDocument18 pagesIMRT: A Review and Preview: Physics in Medicine & BiologychatsashNo ratings yet
- Intrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationDocument13 pagesIntrahepatic Biloma Formation (Bile Duct Necrosis) After Transcatheter Arterial ChemoembolizationIndra PrimaNo ratings yet
- Kashima 2011Document5 pagesKashima 2011eric suNo ratings yet
- Needle Tract Implantation Following Fine-Needle Aspiration of Thyroid CancerDocument7 pagesNeedle Tract Implantation Following Fine-Needle Aspiration of Thyroid Cancersalman khanNo ratings yet
- Lab AdarahDocument2 pagesLab AdarahYuriansyah Dwi Rahma PutraNo ratings yet
- Template Pemeriksaan PenunjangDocument4 pagesTemplate Pemeriksaan PenunjangYuriansyah Dwi Rahma PutraNo ratings yet
- Identifying Pulmonary Nodules or Masses On Chest Radiography Using Deep Learning: External Validation and Strategies To Improve Clinical PracticeDocument8 pagesIdentifying Pulmonary Nodules or Masses On Chest Radiography Using Deep Learning: External Validation and Strategies To Improve Clinical PracticeYuriansyah Dwi Rahma PutraNo ratings yet
- Worksheet JournalDocument4 pagesWorksheet JournalrikarikaNo ratings yet
- Pulmonary Embolism in Children: Paul G. Thacker Edward Y. LeeDocument11 pagesPulmonary Embolism in Children: Paul G. Thacker Edward Y. LeeYuriansyah Dwi Rahma PutraNo ratings yet
- Ajr 15 14445Document8 pagesAjr 15 14445Yuriansyah Dwi Rahma PutraNo ratings yet
- InfoDatin Situasi Demam Berdarah DengueDocument8 pagesInfoDatin Situasi Demam Berdarah DengueYuriansyah Dwi Rahma PutraNo ratings yet
- Scottish Dental April 2018Document108 pagesScottish Dental April 2018valentinanlNo ratings yet
- College of Nursing: Labor WatchDocument3 pagesCollege of Nursing: Labor WatchRS BuenavistaNo ratings yet
- Warren Barr South LoopDocument7 pagesWarren Barr South LoopBeth LawrenceNo ratings yet
- Myusdoctor 150414122940 Conversion Gate01Document15 pagesMyusdoctor 150414122940 Conversion Gate01shipletNo ratings yet
- ARW1 - Final Exam - Virtual 202211 Avanzado 10 17 - 45-19 - 15Document7 pagesARW1 - Final Exam - Virtual 202211 Avanzado 10 17 - 45-19 - 15Rosa Milagros Mostorino PiconNo ratings yet
- استبيان سوء التغذية جامعة عمرانDocument7 pagesاستبيان سوء التغذية جامعة عمرانAkram ZayedNo ratings yet
- Barangay Nutrition Committe: Project ProposalDocument3 pagesBarangay Nutrition Committe: Project ProposalDesiree OngNo ratings yet
- Bronchiolitis Case StudyDocument14 pagesBronchiolitis Case StudyTey Herrera0% (1)
- Ryans World Squad GoalsDocument1 pageRyans World Squad GoalsMelindaNo ratings yet
- The Estrogen Elixir - A History of Hormone Replacement Therapy in America 2007 Edited by Elizabeth Siegel WatkinsDocument364 pagesThe Estrogen Elixir - A History of Hormone Replacement Therapy in America 2007 Edited by Elizabeth Siegel WatkinsAlonso Rodriguez EscobedoNo ratings yet
- Skripsi Tanpa Bab Pembahasan PDFDocument112 pagesSkripsi Tanpa Bab Pembahasan PDFMaudiaazhara RaisaNo ratings yet
- Genetic Counselling: Lecturer Dept. of Psychiatric Nursing Sajjalashree Institute of Nursing Sciences, Navanagar-BagalkotDocument14 pagesGenetic Counselling: Lecturer Dept. of Psychiatric Nursing Sajjalashree Institute of Nursing Sciences, Navanagar-Bagalkottuppadb50% (2)
- Retrospective Drug Use Evaluation of Gentamycin Use in Ambo Hospital, Oromia Region State, West Showa, EthiopiaDocument12 pagesRetrospective Drug Use Evaluation of Gentamycin Use in Ambo Hospital, Oromia Region State, West Showa, EthiopiaIjupbs IjupbsNo ratings yet
- Drug Study (Schizo)Document5 pagesDrug Study (Schizo)aliannaNo ratings yet
- Head Nursing Evaluation ToolDocument2 pagesHead Nursing Evaluation ToolDharline Abbygale Garvida Agullana100% (5)
- PDFDocument11 pagesPDFNico IonaşcuNo ratings yet
- Sedation Record: Patient Selection Criteria DateDocument2 pagesSedation Record: Patient Selection Criteria Datenona aryanNo ratings yet
- Abid Hussain: ARAR Group of Companies, Lahore - Assistant ManagerDocument2 pagesAbid Hussain: ARAR Group of Companies, Lahore - Assistant ManagerAbid HussainNo ratings yet
- Clinical Practice From Bench To Bedside - Is There A Great Divide by DR Marceliano T Aquino JRDocument25 pagesClinical Practice From Bench To Bedside - Is There A Great Divide by DR Marceliano T Aquino JRChristian ErelNo ratings yet
- Neclex Questions Test 3Document16 pagesNeclex Questions Test 3Brittany Worrall100% (13)
- Nurs FPX 4060 Assessment 4 Health Promotion PlanDocument8 pagesNurs FPX 4060 Assessment 4 Health Promotion Planjoohnsmith070No ratings yet
- Brooks Cole Empowerment Series Understanding Human Behavior and The Social Environment 9th Edition by Zastrow and Ashman ISBN Test BankDocument11 pagesBrooks Cole Empowerment Series Understanding Human Behavior and The Social Environment 9th Edition by Zastrow and Ashman ISBN Test Bankwilliam100% (24)
- Ikam Bau TahiDocument17 pagesIkam Bau TahiAndre PrasetyooNo ratings yet
- Postpartum HemorrhageDocument30 pagesPostpartum HemorrhageMusekhirNo ratings yet
- Venipuncture 1Document57 pagesVenipuncture 1Pearce Gabrielle PinlacNo ratings yet
- Heart Disease and Cancer: CirculationDocument4 pagesHeart Disease and Cancer: CirculationDewi AyuNo ratings yet
- First Year PBBSC Master Rotation Plan by DelDocument1 pageFirst Year PBBSC Master Rotation Plan by DelDelphy VargheseNo ratings yet
- Treating The Post-LVAD Patient in An Acute Inpatient Rehab SettingDocument7 pagesTreating The Post-LVAD Patient in An Acute Inpatient Rehab Settingkori holubNo ratings yet
- Hyperemesis GravidarumDocument37 pagesHyperemesis GravidarumRamadhan GhaffarNo ratings yet
- Diklat Rekam MedikDocument196 pagesDiklat Rekam MedikMulyono Aba AthiyaNo ratings yet