Professional Documents
Culture Documents
Articulo 4 PDF
Uploaded by
Andrea HermosaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articulo 4 PDF
Uploaded by
Andrea HermosaCopyright:
Available Formats
Journal of Geriatric Cardiology (2016) 13: 387390
©2016 JGC All rights reserved; www.jgc301.com
Perspective
Open Access
Nursing care in old patients with heart failure: current status and future
perspectives
Hong-Ying PI1,*, Xin HU2
1
Nursing Department, Chinese PLA General Hospital, Beijing, China
2
Vasculocardiology Department, Chinese PLA General Hospital, Beijing, China
J Geriatr Cardiol 2016; 13: 387390. doi:10.11909/j.issn.1671-5411.2016.05.019
Keywords: Heart failure; Nursing care; Tai Chi; The elderly
1 Introduction tioned to improve patient outcomes. There are several tasks
which nurses can take on to improve HF prognosis.[4] De-
The prognosis of heart failure (HF) patients has signifi-
velopment of patient education materials based on practice
cantly improved in the last 20 years, given the advent of
guidelines for old HF patients is a key component to ame-
therapies such as angiotensin-converting enzyme (ACE) in-
liorate patient outcomes. Assessment is another important
hibitors/angiotensin receptor blockers (ARBs), beta-block-
ers, and implantable cardioverter-defibrillator (ICD)/cardiac nursing tasks of improving patient outcomes.[4] Nurses also
resynchronization therapy devices (CRT). In addition to can aid the patient with HF by providing instructions for
these promising therapies, proper nursing-care is also im- patients, implementing tele-monitoring programs, and work-
portant. Here we summarize recent progress of nursing-care ing in quality improvement (QI) programs.[5]
strategies in older HF patients, including routine nursing Effective education includes many topics. Patient with
care, transitional care model, self-care, and role of exercise HF should be advised to strictly comply with a heart-healthy
training in old patients with HF. diet, including sodium control. They also should be taught
to follow fluid restrictions. Although the importance of
nursing in providing patient education is understood, at least
2 Epidemiology of HF
one study indicated that 55% of nurses involved in the study
HF is a progressive heart disease which affects a soaring spent only 15 min or less time to provide patient with re-
number of people worldwide. In America, over 5,000,000 lated education of medications, diet, and activity.
adults aged 20 and above live with HF, and this number is Nursing also should play a primary role in the ongoing
projected to increase by 46% in 2030.[1] Likewise, approxi- assessment of HF patient. The assessment of the patient
mately 4,000,000 people in China aged 35–74 years suf- with HF should be based on the patient’s need. Fluid status
fered from HF.[2] To fulfill that need of the dramatically is usually assessed with following indicators: orthopnea,
increasing patients with HF, we need to formalize nursing peripheral edema, weight gain and the need to increase
care in these patients as a manifestation of “patient-cen- baseline diuretic dose. Additionally, dietary behavior change,
tered” care for older adults who now constitute our domi-
decreased activity amount, worsening thirst, increases of
nant patient group. Although the concept is still in evolution
fluid intake, and adherence to medication should also be
and lacks a full armamentarium of precise tools and skill
evaluated for HF patients. If the patient is not well compli-
sets to define the field, the practice of nursing care in old
ant with the medication regimen, it should be carefully re-
patients with HF is developing toward a distinctive subspe-
cialty with specific skills and services to further advance the ferred to.[6]
care of older patients (Figure 1).[3] Some tradition exercises such as Tai Chi and Yoga are
known to be effective in lowering stress, lessening depres-
sion, and increasing physical fitness, which are used as an
3 Routine nursing care for old patients with HF adjuvant management program for patients with HF. Yoga
The nurses caring for patients with HF are perfectly posi- also may be helpful for routine disease management, pre-
vention of fluid retention, and improve the quality of life for
*Correspondence to: pihongying@301hospital.com.cn patients with HF. Nurses can integrate yoga into HF care.[7,8]
http://www.jgc301.com; jgc@jgc301.com | Journal of Geriatric Cardiology
388 PI HY & HU X. Nursing care in the elderly HF patients
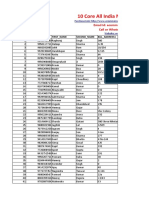
Figure 1. Proposed care model and skill needed for geriatric patients with heart failure.
4 Special issues in nursing care of old pa- lated factors, patient education, and telemonitoring are three
tients with HF major themes of self-care. In the patient-related factors,
age-related symptoms, cognitive factors, and social issues
4.1 Transitional care model for old patients with HF in were barriers to self-care. The interventions promoting self-
China care include adequate patient education and telemonitor-
Because of the complexity of HF, it’s still difficult for ing. Telemonitoring is an appropriate self-care enhancement
patients, even those discharged patients in stable condition tool for selected older adults. More emphasis should be
to self care, so continued specialized guidance and support placed to assist older adults with HF in symptom recogni-
are required. Transitional care is an effective approach to tion.[12]
improve quality of life, ease the tension of relatively less In addition, it is reported that type of self-care behaviors
hospital beds, and reduce national health expenditure. is another important factor influencing the prognosis of old
Therefore, to develop transitional care model for HF pa- HF patients. Cao, et al.[13] found type D personality could
tients in China has important practical significance.[9] Chen, affect HF self-care maintenance behaviors. While the self-
et al.[10] construct an effective transitional care model of HF care management behaviors of these patients may be as-
old patients in Beijing district. This health care include hos- cribed to HF knowledge level, self-care confidence, time of
pitals providing services to patients, community health cen- diagnosed with HF. Overall, 1.6% and 3.9% of HF patients
ter institutions (CHSI) providing services to patients and performed adequate self-care maintenance and self-care
services jointly provided by hospitals and CHSI. management behaviors, respectively, while 12.6% for ade-
quate self-care confidence. For self-care maintenance be-
4.2 Self-care in Chinese older adults with HF haviors, patients performed good adherence to medication,
In addition to nursing-care of old patients with HF in while poor adherence to weight control regularly. More
hospital, self-care is also important for patients’ recovery. importantly, up to 80.3% of patients would not comply with
According to medicare administrative statistics, 30-day rule of restricted intake of sodium. In self-care confidence,
risk-standardized readmission rates of HF patients were patients showed more confidence for following doctors’
24.6% in 2010. Approaches to promoting self-care behav- advice than taking measures to control HF symptoms them-
iors can decrease HF readmission rates. Currently, support- selves.
ing and promoting self-care behaviors focus on improving
4.3 Exercise training in old patients with HF
hospital and post-discharge care, including pre-discharge
planning, home-based follow-up, medication management Regular aerobic training is reported to increase exercises
and risk behavior and symptom management.[11] Patient-re- capacity and cardiac systolic function of patients with HF,
Journal of Geriatric Cardiology | jgc@jgc301.com; http://www.jgc301.com
PI HY & HU X. Nursing care in the elderly HF patients 389
which is strongly recommended in patients with HF. It is phones ‘Application’, from which can download computer
reported to improve left ventricular ejection fraction and program or softwares. It can help provide an opportunity to
attenuate symptoms and quality of life. Moderate-intensity overcome traditional barriers to receive primary or secon-
aerobic exercise is the best choice for HF patients at one dary prevention information and measures. Data from na-
time.[14] However, another high-intensity aerobic interval tionwide online surveys suggest that more than 50% of
exercise (HIIE) has aroused more interest in cardiac rehabi- smartphone users acquire health-related information from
litation recently. HIIE consists of repeated high-intensity their mobile phone, and 19% have downloaded a health-re-
exercise interspersed with recovery periods. The rationale of lated app to their device. As can be seen, health-related App
HIIE is to increase high-intensity of exercise, thereby in- is beneficial for HF prevention education.[19]
creasing the training stimulus.[15] Several recent studies have However, not all App is useful for HF prevention infor-
demonstrated that HIIE is more effective than moderate mation sharing. More than 43,000 health-related Apps exist
intensity aerobic exercise, especially for improving exercise in the Apple iTunes App Store, and only half the Apps have
capacity in patients with HF. In patients with chronic HF, been downloaded > 500 times. All these indicate a low uti-
dyspnea and fatigue limit their exercise ability, which lead lization rate of majority Apps. Therefore, FDA regulates
to progressive deconditioning and exercise intolerance, and only those Apps that transform the smartphone or tablet into
a vicious cycle of worsening dyspnea and fatigue. Therefore, a medical device, or are intended to be used as an accessory
it is necessary to improve exercise capacity especially in to a regulated medical device, for example blood-glucose
elder with chronic HF, regardless of age.[16] and blood-pressure monitors.[20]
In recent decades, Tai Chi, a form of low-intensity To date, only limited studies have focused on nursing-
physical activity originating from China, has become popu- care in older patients with HF. Interventions that specifically
lar in Western countries as a priority selection of exercise. considering age-related factors can improve self-care prac-
Studies have found positive effects of Tai Chi on balance tices. Modifications to current self-care strategies should be
control, flexibility, cardiovascular fitness, pain, fatigue, and implemented for older adults. Addressing patients’ and
insomnia, as well as on psychological well-being—includ- caregivers’ unique learning needs is an important considera-
ing enhanced mood and reduction of stress, anxiety, and de- tion. Strategies that help older patients and caregivers to
pression—in both community-dwelling healthy participants identify and attribute meaning to early symptoms of de-
and patients with chronic conditions.[17] compensating HF should be instituted. Frailty, a barrier or
contributing factor to self-care, needs to be researched.
5 Future perspectives in nursing care of old
patients with HF References
1 McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guide-
An initiative that has recently begun to be studied is tele-
lines for the diagnosis and treatment of acute and chronic
monitoring. Readmission rates do show improved outcomes
heart failure 2012: The Task Force for the Diagnosis and
with the implementation of telemonitoring. It has been sug- Treatment of Acute and Chronic Heart Failure 2012 of the
gested that most HF readmissions are a result of noncom- European Society of Cardiology. Developed in collaboration
pliance. Therefore, patient education and assessments per- with the Heart Failure Association (HFA) of the ESC. Eur
formed via telemonitoring should revolve around diet, exer- Heart J 2012; 33: 1787–1847.
cise, and medication adherence.[18] A telephonic interaction 2 Wang W, Hu SS, Kong LZ, et al. Summary of report on car-
that assesses the patient’s weight, exacerbation signs and diovascular diseases in China, 2012. Biomed Environ Sci 2014;
symptoms, dietary regimen, medication adherence, activi- 27: 552–558.
ties, and social supports can be effective in decreasing com- 3 Ariely R, Evans K, Mills T. Heart failure in China: a review
plications in patients with HF. This telephonic interaction of the literature. Drugs 2013; 73: 689–701.
4 Prasun MA. New heart failure treatment and nursing care.
should stress to patients the importance of compliance to
Heart Lung 2015; 44: 367.
medication regimen, the importance of maintaining their
5 Wan H, Yang Y, Zhu J, et al. Prognostic value of ventricular
activity level, and the importance of social supports.[19]
heart rate in patients with permanent atrial fibrillation and
Mobile phone technology might help to increase the cog- heart failure. Int J Cardiol 2015; 182: 70–71.
nition of old HF patients for cardiac vascular disease pre- 6 Ogunneye O, Rothberg MB, Friderici J, et al. The association
vention. According to statistics, almost 2 billion people (ap- between skilled nursing facility care quality and 30-day read-
proximately 28% of all world population) currently use mission rates after hospitalization for heart failure. Am J Med
smartphones. The term ‘App’ is an abbreviation of smart- Qual 2015; 30: 205–213.
http://www.jgc301.com; jgc@mail.sciencep.com | Journal of Geriatric Cardiology
390 PI HY & HU X. Nursing care in the elderly HF patients
7 Davidson PM, Cockburn J, Newton PJ, et al. Can a heart fail- training in heart failure: impact on sympathetic hyperactivity
ure-specific cardiac rehabilitation program decrease hospitali- and cardiac and skeletal muscle function. Braz J Med Biol Res
zations and improve outcomes in high-risk patients? Eur J 2011; 44: 827–835.
Cardiovasc Prev Rehabil 2010; 17: 393–402. 15 Chrysohoou C, Angelis A, Tsitsinakis G, et al. Cardiovascular
8 Conner D, Barnes C, Harrison-Felix C, Reznickova N. Reha- effects of high-intensity interval aerobic training combined
bilitation outcomes in a population of nonagenarians and with strength exercise in patients with chronic heart failure. A
younger seniors with hip fracture, heart failure, or cerebral vas- randomized phase III clinical trial. Int J Cardiol 2015; 179:
cular accident. Arch Phys Med Rehabil 2010; 91: 1505–1510. 269–274.
9 Chiang LC, Chen WC, Dai YT, Ho YL. The effectiveness of 16 Meyer P, Gayda M, Juneau M, Nigam A. High-intensity
telehealth care on caregiver burden, mastery of stress, and aerobic interval exercise in chronic heart failure. Curr Heart
family function among family caregivers of heart failure pa- Fail Rep 2013; 10: 130–138.
tients: a quasi-experimental study. Int J Nurs Stud 2012; 49: 17 Pan L, Yan J, Guo Y, Yan J. Effects of Tai Chi training on
1230–1242. exercise capacity and quality of life in patients with chronic
10 Chen YH, Ho YL, Huang HC, et al. Assessment of the clini- heart failure: a meta-analysis. Eur J Heart Fail 2013; 15:
cal outcomes and cost-effectiveness of the management of 316–323.
systolic heart failure in Chinese patients using a home-based 18 Riley JP, Gabe JP, Cowie MR. Does telemonitoring in heart
intervention. J Int Med Res 2010; 38: 242–252. failure empower patients for self-care? A qualitative study. J
11 Dickson VV, Melkus GD, Katz S, et al. Building skill in heart Clin Nurs 2013; 22: 2444–2455.
failure self-care among community dwelling older adults: re- 19 Schwarz KA, Mion LC, Hudock D, Litman G. Telemonitor-
sults of a pilot study. Patient Educ Couns 2014; 96: 188–196. ing of heart failure patients and their caregivers: a pilot ran-
12 Zavertnik JE. Self-care in older adults with heart failure: an domized controlled trial. Prog Cardiovasc Nurs 2008; 23:
integrative review. Clin Nurse Spec 2014; 28: 19–32. 18–26.
13 Cao XS, Chen J, Zou JZ, et al. Association of indoxyl sulfate 20 Vuorinen AL, Leppanen J, Kaijanranta H, et al. Use of home
with heart failure among patients on hemodialysis. Clin J Am telemonitoring to support multidisciplinary care of heart fail-
Soc Nephrol 2015; 10: 111–119. ure patients in Finland: randomized controlled trial. J Med In-
14 Brum PC, Bacurau AV, Medeiros A, et al. Aerobic exercise ternet Res 2014; 16: e282.
Journal of Geriatric Cardiology | jgc@jgc301.com; http://www.jgc301.com
You might also like
- Clinician's Guide to Chronic Disease Management of Long Term Conditions, TheFrom EverandClinician's Guide to Chronic Disease Management of Long Term Conditions, TheNo ratings yet
- Effect of Supportive Education on HF Patient Self-CareDocument7 pagesEffect of Supportive Education on HF Patient Self-CareJomer GonzalesNo ratings yet
- 1 s2.0 S2213076418300654 MainDocument5 pages1 s2.0 S2213076418300654 MaindaytdeenNo ratings yet
- Gheorghiu V Et Al 2017Document9 pagesGheorghiu V Et Al 2017Margarida ReisNo ratings yet
- Jurnal PD 4Document11 pagesJurnal PD 4Jay MNo ratings yet
- Bibliography 9thDocument2 pagesBibliography 9thMakki MarcosNo ratings yet
- ijcem0089201Document8 pagesijcem0089201ahmadalipoland25No ratings yet
- JHPN 24 E151Document8 pagesJHPN 24 E151MentiEndah dwi SeptianiNo ratings yet
- Nursing Care for Patients with Acute and Chronic Health ProblemsDocument5 pagesNursing Care for Patients with Acute and Chronic Health ProblemsJhevey ValdezNo ratings yet
- AGA Clinical Practice Update On Palliative Care ManagementDocument14 pagesAGA Clinical Practice Update On Palliative Care ManagementRicardo FernandesNo ratings yet
- Mathew 2017Document6 pagesMathew 2017GodlipNo ratings yet
- Running Head: HYPERTENSION 1Document9 pagesRunning Head: HYPERTENSION 1Peter Saka JagitaNo ratings yet
- 2020 Integrated Model PRIME-PkDocument11 pages2020 Integrated Model PRIME-PkSM199021No ratings yet
- Wu 2022Document9 pagesWu 2022Anindya Laksmi LarasatiNo ratings yet
- archivev3i3MDIwMTMxMDIy PDFDocument9 pagesarchivev3i3MDIwMTMxMDIy PDFLatasha WilderNo ratings yet
- Treating Alcoholism As A Chronic Disease: Approaches To Long Term Continuing CareDocument15 pagesTreating Alcoholism As A Chronic Disease: Approaches To Long Term Continuing Careesbat07No ratings yet
- Acute Care For The Elderly: A Literature Review: Mary Ann Liebert, IncDocument9 pagesAcute Care For The Elderly: A Literature Review: Mary Ann Liebert, IncWatson AbatNo ratings yet
- ObesityDocument9 pagesObesityTaoreed AdegokeNo ratings yet
- Patient Centric Oral Dosage Form.Document13 pagesPatient Centric Oral Dosage Form.Snehal Suresh100% (1)
- Improving End of Life CareDocument9 pagesImproving End of Life CareM_LXNo ratings yet
- Internet Based TreatmentDocument10 pagesInternet Based TreatmentnaveedNo ratings yet
- IPE Program in My InstitutionDocument11 pagesIPE Program in My InstitutionLOGESWARRY K.VESUPATHYNo ratings yet
- Guideline: Physical Therapist Clinical Practice Guideline For The Management of Individuals With Heart FailureDocument30 pagesGuideline: Physical Therapist Clinical Practice Guideline For The Management of Individuals With Heart FailureNindy Yantika MciNo ratings yet
- Effectiveness of Discharge Instruction in The Management of Hypertension Among Hospital PatientsDocument3 pagesEffectiveness of Discharge Instruction in The Management of Hypertension Among Hospital PatientsLance SilvaNo ratings yet
- Chen 2016Document11 pagesChen 2016Febian AlfiansyahNo ratings yet
- Impact of Diabetes Education and Self-Management Support On The 4D Series of Diabetes Patients PDFDocument7 pagesImpact of Diabetes Education and Self-Management Support On The 4D Series of Diabetes Patients PDFCris BañadosNo ratings yet
- Nurses' Activities and Time Management During Home Healthcare VisitsDocument10 pagesNurses' Activities and Time Management During Home Healthcare VisitsEli LNo ratings yet
- Appropriate Titration of Basal Insulin in Type 2 Diabetes and The Potential Role of The PharmacistDocument21 pagesAppropriate Titration of Basal Insulin in Type 2 Diabetes and The Potential Role of The PharmacistOlesiaNo ratings yet
- Integrating Care AcrossDocument11 pagesIntegrating Care AcrossKarina CabayNo ratings yet
- Cardiac RehabilitationDocument4 pagesCardiac RehabilitationBhaskar DhyaniNo ratings yet
- 11 3 23 Tonya Project Themes PapenotesDocument32 pages11 3 23 Tonya Project Themes PapenotesGeoffrey OdhiamboNo ratings yet
- Effect of A New Health Education Model On Continuous Nursing in Elderly Patients With Diabetes MellitusDocument6 pagesEffect of A New Health Education Model On Continuous Nursing in Elderly Patients With Diabetes Mellitusmochamad fahadNo ratings yet
- Self-Management Enhancement Programme PDFDocument18 pagesSelf-Management Enhancement Programme PDFSriMathi Kasi Malini ArmugamNo ratings yet
- ESRD Secondary To Diabetic Nephropathy CASE STUDYDocument42 pagesESRD Secondary To Diabetic Nephropathy CASE STUDYRalph Pelegrino75% (4)
- Research Article: Xijuan Cui, Tao Shan, and Lina QiaoDocument7 pagesResearch Article: Xijuan Cui, Tao Shan, and Lina QiaoitaNo ratings yet
- Evaluation of A Continuous Quality Improvement Initiative For End-of-Life Care For Older Noncancer PatientsDocument9 pagesEvaluation of A Continuous Quality Improvement Initiative For End-of-Life Care For Older Noncancer PatientsSERGIO ANDRES CESPEDES GUERRERONo ratings yet
- Physical Therapist Clinical Practice Guideline For The Management of Individuals With Heart FailureDocument30 pagesPhysical Therapist Clinical Practice Guideline For The Management of Individuals With Heart FailureSyahriadin SyamNo ratings yet
- Impact of A Designed Self-Care Program On Selected Outcomes Among Patients Undergoing HemodialysisDocument18 pagesImpact of A Designed Self-Care Program On Selected Outcomes Among Patients Undergoing HemodialysisImpact JournalsNo ratings yet
- Knowledge of Palliative and End-of-Life Care by Student Registered Nurse AnesthetistsDocument6 pagesKnowledge of Palliative and End-of-Life Care by Student Registered Nurse AnesthetistsRafi ramdhanNo ratings yet
- Nursing Diagnoses and Interventions For Cardiological Patients in Palliative Care Original ArticleDocument9 pagesNursing Diagnoses and Interventions For Cardiological Patients in Palliative Care Original ArticleMaginta Resy DianaNo ratings yet
- LI Famed HypertensionDocument3 pagesLI Famed HypertensionYolanda Dwi OktaviyaniNo ratings yet
- Connecting With Chronically Ill Patients To Improve Treatment AdherenceDocument2 pagesConnecting With Chronically Ill Patients To Improve Treatment AdherenceIdi FaithNo ratings yet
- Supportive Care: Integration of Patient-Centered Kidney Care To Manage Symptoms and Geriatric SyndromesDocument10 pagesSupportive Care: Integration of Patient-Centered Kidney Care To Manage Symptoms and Geriatric Syndromesyanuar esthoNo ratings yet
- PT in CanadaDocument27 pagesPT in CanadaAna CáceresNo ratings yet
- Final Care Coordination Plan - EditedDocument9 pagesFinal Care Coordination Plan - EditedElizabeth GithinjiNo ratings yet
- Jurnal Internasional 7Document13 pagesJurnal Internasional 7Mutiara Anak NegeriNo ratings yet
- Bahan 2-DikonversiDocument11 pagesBahan 2-DikonversiMaya ismayaNo ratings yet
- Jurnal Icha Periop 4Document14 pagesJurnal Icha Periop 4ichamarichaNo ratings yet
- Pneumonia Recovery: A Plan Can Help: Continuous Quality ImprovementDocument7 pagesPneumonia Recovery: A Plan Can Help: Continuous Quality ImprovementNestia RismindaNo ratings yet
- Reduce Modifiable Cardiac Risk Factors in AdultsDocument4 pagesReduce Modifiable Cardiac Risk Factors in AdultsevangelinaNo ratings yet
- Lifestyle Choices and Chronic Kidney Disease:: Dietary Habits and Nutritional ManagementDocument6 pagesLifestyle Choices and Chronic Kidney Disease:: Dietary Habits and Nutritional ManagementBalwayan, January DwayneNo ratings yet
- Case Study Orientation SlidesDocument88 pagesCase Study Orientation SlidesJoseph Emmanuel CandaNo ratings yet
- 13.the Effect of A Comprehensive Dementia Care Management Program On End-of-Life CareDocument6 pages13.the Effect of A Comprehensive Dementia Care Management Program On End-of-Life CareBadRahnaNo ratings yet
- NEUK 1464 (Revised) 1 (Updated)Document21 pagesNEUK 1464 (Revised) 1 (Updated)Sameen ShafaatNo ratings yet
- Arun ArticleDocument8 pagesArun Articleslacker77725No ratings yet
- Jurnal Masalah Prioritas 5 - Pranda 1Document7 pagesJurnal Masalah Prioritas 5 - Pranda 1Pranda Anas AzizahNo ratings yet
- Comfort nursing relieves pain and improves ability after spine surgeryDocument8 pagesComfort nursing relieves pain and improves ability after spine surgeryBella FebriantiNo ratings yet
- Reiss Sandborn 2015 Role of Psychosocial CareDocument6 pagesReiss Sandborn 2015 Role of Psychosocial CareAgata AgniNo ratings yet
- Family Physicians & Hypertension: Moving ForwardDocument4 pagesFamily Physicians & Hypertension: Moving ForwardSusi DesmaryaniNo ratings yet
- Improving Adherence and Biomedical Markers in Hemodialysis Patients: The Effects of Relaxation TherapyDocument9 pagesImproving Adherence and Biomedical Markers in Hemodialysis Patients: The Effects of Relaxation TherapyheriNo ratings yet
- Articulo 1Document15 pagesArticulo 1Andrea HermosaNo ratings yet
- Mental Health Problems in SchoolsDocument9 pagesMental Health Problems in SchoolsRezky PutriNo ratings yet
- ADocument7 pagesAAndrea HermosaNo ratings yet
- Articulo 1 PDFDocument23 pagesArticulo 1 PDFAndrea HermosaNo ratings yet
- Diarrheal Diseases Among Children in India: Current Scenario and Future PerspectivesDocument6 pagesDiarrheal Diseases Among Children in India: Current Scenario and Future PerspectivesAndrea HermosaNo ratings yet
- Diarrheal Diseases Among Children in India: Current Scenario and Future PerspectivesDocument6 pagesDiarrheal Diseases Among Children in India: Current Scenario and Future PerspectivesAndrea HermosaNo ratings yet
- Articulo 1 PDFDocument23 pagesArticulo 1 PDFAndrea HermosaNo ratings yet
- Leiter-3 Appendix D New 2014Document6 pagesLeiter-3 Appendix D New 2014Didenko MarinaNo ratings yet
- Microsoft Certificate Lifecycle Manager Quick Start GuideDocument8 pagesMicrosoft Certificate Lifecycle Manager Quick Start GuidevicogeoNo ratings yet
- Acts that may or may not be delegated to agentsDocument1 pageActs that may or may not be delegated to agentsEarl Vincent VistaNo ratings yet
- Status Signalling and Conspicuous Consumption: The Demand For Counterfeit Status GoodDocument5 pagesStatus Signalling and Conspicuous Consumption: The Demand For Counterfeit Status GoodMarliezel CaballeroNo ratings yet
- (Appendix C-02) COT-RPMS Rating Sheet For T I-III For SY 2022-2023Document1 page(Appendix C-02) COT-RPMS Rating Sheet For T I-III For SY 2022-2023Michelle Tamayo TimadoNo ratings yet
- Test Tenses en AnswersDocument4 pagesTest Tenses en AnswersAmit Kumar LalNo ratings yet
- 10 Study Hacks For Better Grades - EGBDocument41 pages10 Study Hacks For Better Grades - EGBNarimeneKahloulaNo ratings yet
- Sample OMR Sheet Marking PDFDocument1 pageSample OMR Sheet Marking PDFMuraliNo ratings yet
- The Snouters - Form and Life of - Harald StumpkeDocument126 pagesThe Snouters - Form and Life of - Harald StumpkeAlberto Humanes MuñozNo ratings yet
- GCC Students-IN Unit 5 Travel and TourismDocument3 pagesGCC Students-IN Unit 5 Travel and TourismMuhammad IrzanNo ratings yet
- Highway Construction Production Rates and Estimated Contracct TimesDocument95 pagesHighway Construction Production Rates and Estimated Contracct TimesLTE002No ratings yet
- Background Surya NepalDocument11 pagesBackground Surya NepalUjibpradhan67% (3)
- Workbook Answer Key SEODocument2 pagesWorkbook Answer Key SEOlabNo ratings yet
- Guardian Reading - Avon Cosmetics Sellers Prosper in AfricaDocument4 pagesGuardian Reading - Avon Cosmetics Sellers Prosper in Africamiguelillo84eireNo ratings yet
- MEDHERB - Volume 8 - Issue 2 - Pages 71-78Document8 pagesMEDHERB - Volume 8 - Issue 2 - Pages 71-78Andreea RoxanaNo ratings yet
- Pasyon and RevolutionDocument2 pagesPasyon and RevolutionBilly JoeNo ratings yet
- Classroom Management and DisciplineDocument2 pagesClassroom Management and DisciplineMonaida Umpar IbrahimNo ratings yet
- Fetal Mummification in CowsDocument22 pagesFetal Mummification in CowsTahseen AlamNo ratings yet
- Brown Creative Vintage Rustic Motivational Quote PosterDocument1 pageBrown Creative Vintage Rustic Motivational Quote PosterRafunzel Pe BandoquilloNo ratings yet
- LS Spanish Year 7 POS-1Document9 pagesLS Spanish Year 7 POS-1NEHALL GOYALNo ratings yet
- Leopoldo Jeremias Vs Estate of MarianoDocument1 pageLeopoldo Jeremias Vs Estate of MarianoGee LorinNo ratings yet
- 117cherished MomentsDocument32 pages117cherished MomentsPilar Martín Zamora100% (1)
- Pityriasis Versicolor: Avoiding Pitfalls in Disease Diagnosis and TherapyDocument3 pagesPityriasis Versicolor: Avoiding Pitfalls in Disease Diagnosis and TherapypanduNo ratings yet
- Selling & Negotiation SkillsDocument70 pagesSelling & Negotiation SkillsMojo JOjoNo ratings yet
- Explicitation and Implicitation - Omission and Addition - in ENGLISHDocument63 pagesExplicitation and Implicitation - Omission and Addition - in ENGLISHdyna bookNo ratings yet
- The Cell Cycle: How Cells Grow and DivideDocument21 pagesThe Cell Cycle: How Cells Grow and DivideAqsa YaminNo ratings yet
- Students' Perception of Online English Learning During Covid-19 PandemicDocument5 pagesStudents' Perception of Online English Learning During Covid-19 Pandemicfadhilah santriNo ratings yet
- Sacha Doucet-Kim Cancer AssignmentDocument3 pagesSacha Doucet-Kim Cancer AssignmentSacha Doucet-KimNo ratings yet
- 5 All India Mobile Database SampleDocument15 pages5 All India Mobile Database Sampleali khan Saifi100% (1)
- Birla Sun Life Implements Talisma CRMDocument10 pagesBirla Sun Life Implements Talisma CRMvishuvamNo ratings yet