Professional Documents
Culture Documents
Neuromuscular Blocking Drugs
Uploaded by
Yogi drCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neuromuscular Blocking Drugs
Uploaded by
Yogi drCopyright:
Available Formats
Neuromuscular Blocking Drugs ( Post synaptic neuromuscular blockers )
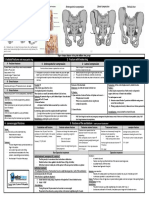
These drugs block cholinergic transmission between motor nerve endings and the nicotinic receptors on the neuromuscular end plate of skeletal muscle. These neuromuscular blockers are structural analogs of acetylcholine,
and they act either as antagonists (nondepolarizing type) or agonists (depolarizing type) at the receptors on the end plate of the neuromuscular junction.
Dr.Ahmados Nondepolarizing (competitive) blockers Depolarizing agents
tubocurarine is considered to be the prototype agent in this class, it has been largely replaced by
other agents due to side effects
1- At low doses: The depolarizing neuromuscular blocking drug succinylcholine attaches to
- Nondepolarizing neuromuscular blocking drugs interact with the nicotinic the nicotinic receptor and acts like acetylcholine to depolarize the junction.
receptors to prevent the binding of acetylcholine thus prevent depolarization
of the muscle cell membrane and inhibit muscular contraction. Unlike acetylcholine, which is instantly destroyed by acetylcholinesterase,
the depolarizing agent persists at high concentrations in the synaptic cleft,
- Because these agents compete with acetylcholine at the receptor without remaining attached to the receptor for a relatively longer time and
Mechanism of
stimulating the receptor, they are called competitive blockers. providing a constant stimulation of the receptor.
action:
N.B. Their action can be overcome by increasing the concentration of The depolarizing agent first causes the opening of the sodium channel
acetylcholine in the synaptic gap for example, by administration of associated with the nicotinic receptors which results in depolarization of
cholinesterase inhibitors, such as neostigmine, pyridostigmine, or the receptor (Phase I) This leads to a transient twitching of the muscle
edrophonium. (fasciculations).
2- At high doses: Continued binding of the depolarizing agent renders the receptor incapable
Nondepolarizing blockers can block the ion channels of the end plate. This leads of transmitting further impulses. With time, continuous depolarization gives
to further weakening of neuromuscular transmission, and it reduces the ability way to gradual repolarization as the sodium channel closes or is blocked
of acetylcholinesterase inhibitors to reverse the actions of nondepolarizing This causes a resistance to depolarization (Phase II) and a flaccid paralysis.
muscle relaxants.
Not all muscles are equally sensitive to blockade by competitive blockers. - The sequence of paralysis may be slightly different, but as with the
competitive blockers, the respiratory muscles are paralyzed last.
- Small, rapidly contracting muscles of the face and eye are most susceptible
and are paralyzed first, followed by the fingers. - Succinylcholine initially produces short-lasting muscle fasciculations,
followed within a few minutes by paralysis.
Actions: - Thereafter, the limbs, neck, and trunk muscles are paralyzed.
- The drug does not produce a ganglionic block except at high doses, but it
- Then the intercostal muscles are affected, and lastly, the diaphragm muscles does have weak histamine-releasing action.
are paralyzed.
- However, succinylcholine that gets to the neuromusclular junction is not
- Those agents (for example, tubocurarine, mivacurium, and atracurium), metabolized by acetylcholinesterase, allowing the agent to bind to nicotinic
which release histamine, can produce a fall in blood pressure, flushing, and receptors, and redistribution to plasma is necessary for metabolism
bronchoconstriction. (therapeutic benefits last only for a few minutes).]
1- These blockers are used therapeutically as adjuvant drugs in anesthesia - Because of its rapid onset and short duration of action, succinylcholine is
during surgery to relax skeletal muscle. useful when rapid endotracheal intubation is required during the induction
Therapeutic of anesthesia
uses: 2- These agents are also used to facilitate intubation as well as during (a rapid action is essential if aspiration of gastric contents is to be avoided
orthopedic surgery. during intubation).
- It is also employed during electroconvulsive shock treatment.
All are injected intravenously, because their uptake via oral absorption is
Route of admin. minimal BECAUSE:
These agents possess two or more quaternary amines in their bulky ring
structure, making them orally ineffective.
They penetrate membranes very poorly and do not enter cells or cross the - Normally, the duration of action of succinylcholine is extremely short,
Distribution blood-brain barrier.
because this drug is rapidly broken down by plasma cholinesterase.
- tubocurarine, pancuronium, mivacurium, metocurine, doxacurium
are not metabolized; their actions are terminated by redistribution and are - Succinylcholine is injected intravenously. Its brief duration of action
excreted in the urine unchanged. (several minutes) results from:
- Atracurium : 1-redistribution
Pharmaco- is degraded spontaneously in the plasma and by ester hydrolysis. 2-and rapid hydrolysis by plasma cholinesterase.
kinetics:
N.B. Atracurium has been replaced by its isomer, cisatracurium BECAUSE
Metabolism & Atracurium releases histamine and is metabolized to laudanosine, which can It therefore is usually given by continuous infusion.
Excretion provoke seizures.
- isatracurium,
has the same pharmacokinetic properties as atracurium, is less likely to have
these effects.
- vecuronium, rocuronium (The aminosteroid drugs)
are deacetylated in the liver, and their clearance may be prolonged in
patients with hepatic disease.
These drugs are also excreted unchanged in the bile.
1- Histamine release and promote ganglion blocker. Adverse effects:
tubocurarin
Adverse 2- Decrease blood pressure.
effects: a.Hyperthermia:
pancuronium Increased heart rate. When halothane is used as an anesthetic, administration of succinylcholine has
- Drugs: neostigmine, physostigmine, pyridostigmine, and edrophonium
occasionally caused malignant hyperthermia (with muscular rigidity and
can overcome the action of nondepolarizing neuromuscular blockers, hyperpyrexia) in genetically susceptible people (see Figure 5.10).
This is treated by rapidly cooling the patient and by administration of dantrolene, which
- but with increased dosage, cholinesterase inhibitors can cause a
Cholinesterase blocks release of Ca2+ from the sarcoplasmic reticulum of muscle cells, thus reducing heat
depolarizing block as a result of elevated acetylcholine concentrations
inhibitors: production and relaxing muscle tone.
at the end-plate membrane.
- If the neuromuscular blocker has entered the ion channel, cholinesterase b.Apnea:
inhibitors are not as effective in overcoming blockade.
Drug Administration of succinylcholine to a patient who is genetically deficient in plasma
Drugs: halothane act to enhance neuromuscular blockade by cholinesterase or has an atypical form of the enzyme can lead to prolonged apnea
interactions: Halogenated
exerting a stabilizing action at the neuromuscular junction. due to paralysis of the diaphragm.
hydrocarbon
anesthetics: These agents sensitize the neuromusclular junction to the effects of
neuromuscular blockers. c.Hyperkalemia:
Drugs: gentamicin or tobramycin inhibit acetylcholine release from Succinylcholine increases potassium release from intracellular stores.
Aminoglycoside
cholinergic nerves by competing with calcium ions.
antibiotics:
They synergize with tubocurarine and other competitive blockers, This may be particularly dangerous in:
enhancing the blockade. 1- burn patients or
These agents may increase the neuromuscular block of tubocurarine 2- patients with massive tissue damage
Ca–channel bloc. and other competitive blockers as well as depolarizing blockers. in which postassium is been rapidly lost from within cells.
You might also like
- Use This File If Printing The Whole WorkbookDocument819 pagesUse This File If Printing The Whole WorkbookAndrewNo ratings yet
- 15 LECTURE's Final For PrintDocument147 pages15 LECTURE's Final For PrintSaad Abdullah100% (9)
- Chapter 30 NotesDocument4 pagesChapter 30 NotesMariah Jane TaladuaNo ratings yet
- Neurovascular Assessment PresentationDocument39 pagesNeurovascular Assessment PresentationiiTzZ CaRfTNo ratings yet
- Intrapartum HandoutDocument29 pagesIntrapartum HandoutZahNo ratings yet
- Autonomic Nervous SystemDocument13 pagesAutonomic Nervous SystemDimple CosNo ratings yet
- Case Report - Perianal AbscessDocument18 pagesCase Report - Perianal AbscessViras VitrianiNo ratings yet
- (PHARMA) 1.12 Cholinergic Drugs (LReyes) v2 PDFDocument15 pages(PHARMA) 1.12 Cholinergic Drugs (LReyes) v2 PDFNoreenNo ratings yet
- NEUROMUSCULAR BLOCKING DRUG Lecture NoteDocument6 pagesNEUROMUSCULAR BLOCKING DRUG Lecture NoteOladotun AwoleyeNo ratings yet
- Chapter 5 (Cholinergic Antagonists)Document42 pagesChapter 5 (Cholinergic Antagonists)Aneeza AhmadNo ratings yet
- NMJ Blocking Agents GuideDocument69 pagesNMJ Blocking Agents Guidevvb_frndNo ratings yet
- Neuromuscular Blocking DrugsDocument22 pagesNeuromuscular Blocking DrugsMuhammad Shahid BilalNo ratings yet
- Neuromuscular Blocking Drugs and Anticholinesterases UpdateDocument4 pagesNeuromuscular Blocking Drugs and Anticholinesterases UpdateAuliaNo ratings yet
- Neuromuscular Blocking Drugs: Dr. Anil Kumar SaxenaDocument21 pagesNeuromuscular Blocking Drugs: Dr. Anil Kumar SaxenaLuqman Al-Bashir FauziNo ratings yet
- Mpharm Year 1 Integrated Therapeutics Workshop 3Document29 pagesMpharm Year 1 Integrated Therapeutics Workshop 3Thao NguyenNo ratings yet
- Skeletal Muscle RelaxantDocument18 pagesSkeletal Muscle Relaxantswaroop ranjan nandaNo ratings yet
- The Cholinergic Antagonists: PharmacologyDocument5 pagesThe Cholinergic Antagonists: PharmacologyDr-Dalya ShakirNo ratings yet
- 4.muscle RelaxantsDocument23 pages4.muscle Relaxantskarim hassanNo ratings yet
- Pharm 3 IDocument3 pagesPharm 3 Iravi2like100% (1)
- Neuromuscular Blocking Agents and SpasmolyticsDocument22 pagesNeuromuscular Blocking Agents and Spasmolyticsjanemwanza003No ratings yet
- 4.neuromuscular Blocking Agents For BDS 3Document13 pages4.neuromuscular Blocking Agents For BDS 3ireneNo ratings yet
- Drugs Acting On Somatic Nervous SystemDocument25 pagesDrugs Acting On Somatic Nervous SystemcchatrumaNo ratings yet
- Neuromuscular Blockers: Presented By: Patel OmkumarDocument23 pagesNeuromuscular Blockers: Presented By: Patel OmkumarVivek PandeyNo ratings yet
- Anaesthetics and Cns Frcem SuccessDocument215 pagesAnaesthetics and Cns Frcem SuccessAbidi HichemNo ratings yet
- Katz 1Document16 pagesKatz 1Vienna TulauanNo ratings yet
- Stages of Anesthesia and Succinylcholine EffectsDocument7 pagesStages of Anesthesia and Succinylcholine EffectsJanice SolamilloNo ratings yet
- Group 6Document37 pagesGroup 6LohithNo ratings yet
- 4.Ghafez-Cholinergic Neurotransmission and Related Drugs-2022 - 2Document27 pages4.Ghafez-Cholinergic Neurotransmission and Related Drugs-2022 - 2yasmin.rahmany03No ratings yet
- Types:: Cholinergic ReceptorsDocument7 pagesTypes:: Cholinergic Receptorsaiesha.khalid.1980No ratings yet
- Skeletal Muscle Relaxants 1Document21 pagesSkeletal Muscle Relaxants 1pooja sureshNo ratings yet
- Pancuronium: "Pavulon - Bromurex"Document33 pagesPancuronium: "Pavulon - Bromurex"Bahaa ShaabanNo ratings yet
- BSCN NMBDocument11 pagesBSCN NMBMuhammad Abbas WaliNo ratings yet
- Skeletal Muscle Relaxant (Lecture Notes QIUP 2017)Document9 pagesSkeletal Muscle Relaxant (Lecture Notes QIUP 2017)Monissha ThiaguNo ratings yet
- Al-Bayan University Pharmacy College 3 Stage Pharmacy: 5 Drugs Acting On ANS DR - Khulood SaadoonDocument42 pagesAl-Bayan University Pharmacy College 3 Stage Pharmacy: 5 Drugs Acting On ANS DR - Khulood SaadoonAsdar LeaqerNo ratings yet
- Pharmacology of autonomous nervous systemDocument107 pagesPharmacology of autonomous nervous systemtekaayele77No ratings yet
- Muscle Relaxants and Neuromuscular Blocking AgentsDocument45 pagesMuscle Relaxants and Neuromuscular Blocking AgentsSomesh SharmaNo ratings yet
- Cholinergic TransmissionDocument43 pagesCholinergic TransmissionAjay SinghNo ratings yet
- Dr. D.K. Katiyar Skeletal - Muscle - RelaxantsDocument36 pagesDr. D.K. Katiyar Skeletal - Muscle - RelaxantsAlexander BandaNo ratings yet
- L9 Skeletal Muscle Relaxants & Local AnestheticsDocument49 pagesL9 Skeletal Muscle Relaxants & Local AnestheticsWejdan AlotaibiNo ratings yet
- Anticholinergic AgentsDocument36 pagesAnticholinergic AgentsNicole GalvezNo ratings yet
- Definitions and classifications of muscle relaxantsDocument42 pagesDefinitions and classifications of muscle relaxantsMirza Shaharyar BaigNo ratings yet
- FarmakoDocument31 pagesFarmakoHany Theresya ViliensterNo ratings yet
- Pharmacology NMB Ds and Anti Cholinesterase S FinalDocument8 pagesPharmacology NMB Ds and Anti Cholinesterase S FinalPamella Kusuma WerdanieNo ratings yet
- First Page PDFDocument1 pageFirst Page PDFferhanmu419No ratings yet
- Relação Estrutura AtividadeDocument25 pagesRelação Estrutura AtividadeFábioNo ratings yet
- Pcol 1 Ans Midterm PDFDocument9 pagesPcol 1 Ans Midterm PDFJillian Mae DacerNo ratings yet
- Sosiologi KesehatanDocument62 pagesSosiologi KesehatanLucy WijayaNo ratings yet
- Muscle RelaxantsDocument49 pagesMuscle RelaxantsApriani MargastutieNo ratings yet
- Table I Nicotinic and Muscarinic Receptors and Their ActionsDocument3 pagesTable I Nicotinic and Muscarinic Receptors and Their ActionsMegha Kulkarni FPS PES UniversityNo ratings yet
- Exp. 12 Neuromuscular BlockersDocument12 pagesExp. 12 Neuromuscular BlockersLuigi MendozaNo ratings yet
- Slide Jurnal AnestesiDocument11 pagesSlide Jurnal AnestesiAdin Es En CheNo ratings yet
- Skeletal Muscle Relaxants: DR RC AnakwueDocument24 pagesSkeletal Muscle Relaxants: DR RC AnakwuetemitopeNo ratings yet
- Acetylcholine and Autonomic DrugsDocument20 pagesAcetylcholine and Autonomic DrugsPrincess Mara DuranNo ratings yet
- Muscle Relaxants Classification and Mechanisms of ActionDocument22 pagesMuscle Relaxants Classification and Mechanisms of Actionvinay0717100% (1)
- Neuromuscular Blocking AgentsDocument13 pagesNeuromuscular Blocking AgentsSamer AlBaghdadiNo ratings yet
- Cholinergic AgonistsDocument1 pageCholinergic AgonistsAlexandra AlexaNo ratings yet
- Unit 3 Drugs Acting of Autonomic Nervous System: StructureDocument12 pagesUnit 3 Drugs Acting of Autonomic Nervous System: StructureSwapnilPagareNo ratings yet
- Drugs Acting On Autonomic GangliaDocument9 pagesDrugs Acting On Autonomic GangliaDita Hasni100% (1)
- Suxamethonium Apnoea Update 2003Document2 pagesSuxamethonium Apnoea Update 2003jira neaNo ratings yet
- Suxamethonium Apnoea Update 2003Document2 pagesSuxamethonium Apnoea Update 2003Nomathamsanqa KhumaloNo ratings yet
- Neuropharma AntidementiaDocument29 pagesNeuropharma AntidementiaKeanne Paula AmamanglonNo ratings yet
- Adjuvants in Central Neuraxial BlockadeDocument29 pagesAdjuvants in Central Neuraxial BlockadepriyadikkalaNo ratings yet
- Fractures of FemurDocument1 pageFractures of FemurYogi drNo ratings yet
- Fractures of Arm Forearm PDFDocument3 pagesFractures of Arm Forearm PDFjimNo ratings yet
- Fractures of FemurDocument1 pageFractures of FemurYogi drNo ratings yet
- Maternal and Neonatal Outcomes of Pregnant Women With COVID-19 Pneumonia: A Case-Control StudyDocument20 pagesMaternal and Neonatal Outcomes of Pregnant Women With COVID-19 Pneumonia: A Case-Control StudyYogi drNo ratings yet
- Muscles of The Gluteal RegionDocument2 pagesMuscles of The Gluteal RegionYogi drNo ratings yet
- Gastrointestinal Bleeding PDFDocument1 pageGastrointestinal Bleeding PDFYogi drNo ratings yet
- Axonal degeneration: causes, effects and regenerationDocument1 pageAxonal degeneration: causes, effects and regenerationYogi drNo ratings yet
- Cardiac Arrest PDFDocument4 pagesCardiac Arrest PDFYogi drNo ratings yet
- Cardiac Arrest PDFDocument4 pagesCardiac Arrest PDFYogi drNo ratings yet
- 9164 62159 1 PBDocument12 pages9164 62159 1 PBjenegneNo ratings yet
- Bone fracture causes and healing processDocument3 pagesBone fracture causes and healing processYogi drNo ratings yet
- Pathology of OsteoarthritisDocument2 pagesPathology of OsteoarthritisYogi drNo ratings yet
- Trauma TriageDocument2 pagesTrauma TriageYogi drNo ratings yet
- Nonsteroidal Anti-Inflamatory DrugsDocument4 pagesNonsteroidal Anti-Inflamatory DrugsYogi drNo ratings yet
- 1 PB PDFDocument9 pages1 PB PDFTiaNo ratings yet
- 1 PB PDFDocument9 pages1 PB PDFTiaNo ratings yet
- Fracturte of Pelvis PDFDocument2 pagesFracturte of Pelvis PDFYogi drNo ratings yet
- Imaging in Acute Abdomen: Dr. Wan Najwa Zaini Wan Mohamed Radiologist, Hospital Queen Elizabeth IiDocument70 pagesImaging in Acute Abdomen: Dr. Wan Najwa Zaini Wan Mohamed Radiologist, Hospital Queen Elizabeth IiYogi drNo ratings yet
- Musculoskeletal System Short NotesDocument36 pagesMusculoskeletal System Short NotesYogi drNo ratings yet
- Cardiac Arrest PDFDocument4 pagesCardiac Arrest PDFYogi drNo ratings yet
- Axonal degeneration: causes, effects and regenerationDocument1 pageAxonal degeneration: causes, effects and regenerationYogi drNo ratings yet
- Surgical Anatomy-Anal Canal: Dr. Belal MansoorDocument79 pagesSurgical Anatomy-Anal Canal: Dr. Belal MansoorYogi drNo ratings yet
- 926 1861 1 PBDocument9 pages926 1861 1 PBERNANo ratings yet
- Axonal degeneration: causes, effects and regenerationDocument1 pageAxonal degeneration: causes, effects and regenerationYogi drNo ratings yet
- Abdominal Wall Defects: Omphalocele GastroschisisDocument20 pagesAbdominal Wall Defects: Omphalocele GastroschisisYogi drNo ratings yet
- 9164 62159 1 PBDocument12 pages9164 62159 1 PBjenegneNo ratings yet
- Differential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersDocument3 pagesDifferential Diagnosis of Genital Ulcer Differential Diagnosis of Genital UlcersNurhayati HasanahNo ratings yet
- Comments, Opinions, and Reviews: Vascular Syndromes of The ThalamusDocument15 pagesComments, Opinions, and Reviews: Vascular Syndromes of The ThalamusYogi drNo ratings yet
- Human Kidney Is A Target For Novel Severe Acute Respiratory Syndrome Coronavirus 2 (Sars-Cov-2) InfectionDocument16 pagesHuman Kidney Is A Target For Novel Severe Acute Respiratory Syndrome Coronavirus 2 (Sars-Cov-2) InfectionYogi drNo ratings yet
- Final Research Thesis Og Milignant HyperthermiaDocument38 pagesFinal Research Thesis Og Milignant HyperthermiaImran MukhlessNo ratings yet
- Drugs in CPR - M.H.farjooDocument37 pagesDrugs in CPR - M.H.farjooAnonymous 34umhBmBENo ratings yet
- Rapid Sequence Induction and Intubation (RSII) For Anesthesia - UpToDateDocument35 pagesRapid Sequence Induction and Intubation (RSII) For Anesthesia - UpToDateSofíaNo ratings yet
- Anesthesia One Liner PDFDocument13 pagesAnesthesia One Liner PDFMinaz PatelNo ratings yet
- Pharm Exam #2Document9 pagesPharm Exam #2Taylor SolomonNo ratings yet
- Neuromuscular BlockersDocument49 pagesNeuromuscular Blockerssongo sorshimaNo ratings yet
- Dantrolene Malignant Hyperthermia 2020Document8 pagesDantrolene Malignant Hyperthermia 2020JoelGámezNo ratings yet
- Malignant Hyperthermia Fact SheetDocument2 pagesMalignant Hyperthermia Fact Sheetapi-301819201No ratings yet
- Malignant Hyperthermia - Diagnosis and Management of Acute Crisis - UpToDateDocument43 pagesMalignant Hyperthermia - Diagnosis and Management of Acute Crisis - UpToDateMaría Augusta Robayo Uvilluz100% (2)
- Airway ManagementDocument86 pagesAirway ManagementMUKESH SUNDARARAJANNo ratings yet
- Anesthetic Consideration For Neuromuscular DiseasesDocument6 pagesAnesthetic Consideration For Neuromuscular DiseasesALEJANDRO BOTERO FERNANDEZNo ratings yet
- Platinum Notes - AnaesthesiaDocument46 pagesPlatinum Notes - AnaesthesiaANMOLNo ratings yet
- Muscle Relaxants: Uses, Types, Monitoring and ReversalDocument33 pagesMuscle Relaxants: Uses, Types, Monitoring and ReversalFady Jehad ZabenNo ratings yet
- Definitions and classifications of muscle relaxantsDocument42 pagesDefinitions and classifications of muscle relaxantsMirza Shaharyar BaigNo ratings yet
- Baromtric (89 Pages)Document89 pagesBaromtric (89 Pages)jahangirealamNo ratings yet
- SuccinylcholineDocument2 pagesSuccinylcholineSalma KarimahNo ratings yet
- Drugs Used in Critica Care SettingDocument54 pagesDrugs Used in Critica Care SettingChandan KumarNo ratings yet
- Miller Airway ManagementDocument65 pagesMiller Airway ManagementBenediktus BayuNo ratings yet
- Pharma McqsDocument45 pagesPharma McqsFarah IqbalNo ratings yet
- نكلكس سايك 5Document11 pagesنكلكس سايك 5Ayah NaemNo ratings yet
- Neuromuscular Disorders & Anaesthesia Anaesthesia Tutorial of The Week 126Document9 pagesNeuromuscular Disorders & Anaesthesia Anaesthesia Tutorial of The Week 126friday ChitsongaNo ratings yet
- Malignant Hyperthermia: Pre-Hospital Emergency Care Recommendations Recommendations For Hospital Emergency DepartmentsDocument6 pagesMalignant Hyperthermia: Pre-Hospital Emergency Care Recommendations Recommendations For Hospital Emergency DepartmentsHelend Ndra TaribukaNo ratings yet
- Neuromuscular Blocking AgentsDocument89 pagesNeuromuscular Blocking Agentslorenzo08No ratings yet
- Basic Anaesthetic Drugs - SheetDocument1 pageBasic Anaesthetic Drugs - SheetOxigen XenonNo ratings yet
- UVA Surgery Residents and Faculty Contribute to New Anesthesiology TextbookDocument774 pagesUVA Surgery Residents and Faculty Contribute to New Anesthesiology TextbookDexter LimNo ratings yet
- 17-18 Chong Kar Mun's Anaesthesia NotesDocument32 pages17-18 Chong Kar Mun's Anaesthesia NotesElaineNo ratings yet
- Anaesthesia Considerations for Myasthenia Gravis Patients Undergoing ThymectomyDocument11 pagesAnaesthesia Considerations for Myasthenia Gravis Patients Undergoing ThymectomyParvathy RNo ratings yet
- Essential Drug List: (Accessed 24 April 2007)Document47 pagesEssential Drug List: (Accessed 24 April 2007)Ryan Noel Perez de TagleNo ratings yet