Professional Documents
Culture Documents
Mitral
Uploaded by
Hugo AROriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mitral
Uploaded by
Hugo ARCopyright:
Available Formats
Journal of Geriatric Cardiology (2015) 12: 346−352
©2015 JGC All rights reserved; www.jgc301.com
Research Article •
Open Access •
Mitral peak early diastolic filling velocity to deceleration time ratio as a
predictor of prognosis in patients with chronic heart failure and preserved
or reduced ejection fraction
Flora Pirozzi, Antonella Paglia, Laura Sasso, Pasquale Abete, Angelo Carlomagno, Carlo G Tocchetti,
Domenico Bonaduce, Mario Petretta
Department of Translational Medical Sciences, Section of Internal Medicine, Federico II University, Naples, Italy
Abstract
Objective Doppler derived mitral peak early diastolic filling velocity to deceleration time ratio (E/DT) has been proposed as parameter for
predicting prognosis in general population. This study prospectively investigates the incremental prognostic value of E/DT over clinical, conven-
tional echocardiographic and mitral-Doppler variables in patients hospitalized for decompensated heart failure (HF). Methods We analyzed 95
HF patients (mean age 64.8 ± 12.2 years) hospitalized at our institution from January 2010 to March 2012. The primary end-point was cardiac
death or hospitalization, whichever occurred first. Cox regression analysis was performed to identify significant predictors of outcomes. Results
During follow-up (median 37.7 months) 13 patients died and 44 were hospitalized for a cardiac event. At univariable analysis, New York Heart
Association (NYHA) functional class, furosemide dosage, lateral tricuspidal annular plane systolic excursion, deceleration time and E/DT were
predictive of outcome. At multivariable analysis, E/DT was the only predictor of prognosis (hazard ratio = 1.02, P = 0.018), giving incremental
prognostic information to clinical and other echocardio-graphic measures (global chi-square from 15.4 to 25.2; P = 0.032). Conclusions E/DT
gives independent and incremental prognostic information in HF patients.
J Geriatr Cardiol 2015; 12: 346−352. doi:10.11909/j.issn.1671-5411.2015.04.006
Keywords: Echocardiographic evaluation; Left ventricular function; Risk stratification
1 Introduction and Doppler echocardiography, is a very useful test in the
evaluation of these patients. The addition of standard echo-
Predictors of poor outcome in patients with chronic heart cardiographic variables to multivariable risk score models
failure (HF) help physicians in medical decision making. results in a significant improvement in risk prediction.[8]
Previous studies have identified a number of epidemiologi- Many echocardiographic variables correlate with prognosis
cal, clinical and laboratory variables predictive of poor out- in HF, including left ventricular (LV) volumes and function,
come.[1−3] Multivariable models that incorporate clinical and pulmonary hypertension, right ventricular systolic function
laboratory variables, medications and devices have been and Doppler derived diastolic filling variables.[9−12] Recently,
developed to estimate survival of HF patients, in order to the ratio of mitral peak early diastolic filling velocity to de-
create a valid assessment of prognosis in patients with celeration time (E/DT) has been demonstrated to give im-
HF.[4−6] Several risk scores are available as an interactive portant prognostic information in a middle aged to elderly
application to calculate the risk of mortality in ambulatory population with a high prevalence of diabetes and hyperten-
patients with HF.[7] sion.[13] Our purpose was to evaluate the prognostic value of
Although a complete history and physical examination this parameter, after adjustment for conventional data, in HF
are important first steps in HF patients, a two-dimensional patients either with reduced ejection fraction (HFrEF) or
preserved ejection fraction (HFpEF).
Correspondence to: Mario Petretta, MD, Department of Translational Med-
ical Sciences, Section of Internal Medicine, Federico II University, Naples, 2 Methods
Italy. E-mail: petretta@unina.it
Telephone: +39-081-746-2262 Fax: +39-081-746-2282 2.1 Study population
Received: February 19, 2015 Revised: April 9, 2015
From January 2010 to March 2012, we prospectively
Accepted: June 1, 2015 Published online: July 6, 2015
http://www.jgc301.com; jgc@jgc301.com | Journal of Geriatric Cardiology
Pirozzi F, et al. Prognostic value of E/DT in HF patients 347
enrolled 120 patients admitted for acute decompensated rameters were measured: peak early (E) and late (A) dia-
heart failure to the Internal Medicine Section of our De- stolic filling velocities, E/A ratio, deceleration time of E
partment. All patients, after structured history and physical wave (DT), septal early diastolic mitral annular tissue ve-
examination, fulfilled the Framingham criteria for diagnosis locity (septal-e’), lateral early diastolic mitral annular tissue
of HF.[14] Demographic, clinical and laboratory data were velocity (lateral-e’). We also calculated E/e’ ratio by divid-
collected in all patients before discharge, and after clinical ing transmitral E peak by e’, this latter averaged from the
stabilization. Baseline characteristics included patients de- two acquisition sites. Right ventricular (RV) diameters were
mographics (age, gender), clinical data (height, weight, measured at end-diastole from a right ventricle focused api-
NYHA functional class, cardiac rhythm, blood pressure, cal 4-chamber view, as recommended by the American So-
history of coronary artery disease, smoking habits, diabetes, ciety of Echocardiography. Using M-mode echocardiogra-
presence of implantable cardioverter-defibrillator), and phy, lateral tricuspidal annular plane systolic excursion
laboratory data (serum hemoglobin, lymphocytes, choles- (TAPSE) was measured as the distance between the basal,
terol, urea nitrogen, sodium). Patients were considered to end-diastolic position of the tricuspid annulus taken at the
have idiopathic dilated cardiomyopathy when no obvious beginning of the electrocardiographic QRS complex and its
underlying cause of HF could be discovered during routine greatest apical long-axis movement. Two-dimensional
evaluation (electrocardiogram, two-dimensional echocardi- echocardiography-derived RV area measurements were
ography, stress test, perfusion imaging). The diagnosis of taken from the apical four-chamber view at end-diastole and
ischemic heart disease was based on clinical history, or evi- end-systole, and the fractional area change (FAC) was cal-
dence of previous Q-waves myocardial infarction. When culated (difference between end-diastolic and end-systolic
after routine evaluation the diagnosis was still uncertain, areas divided by end-diastole area × 100).[15] A TAPSE
coronary angiography was performed. Patients with hemo- value < 16 mm was considered abnormal, while a DT < 140
dynamically significant valvular disease, myocarditis, hy- ms was considered to predict an elevated LV filling pressure.
pertrophic obstructive cardiomyopathy, angina at rest, Pulmonary artery systolic pressure (PAPs) was estimated
myocardial infarction within six months before enrollment, using Doppler echocardiography by calculating the RV to
uncontrolled hypertension and patients undergoing biven- right atrial pressure gradient during systole, approximated
tricular pacing for resynchronization therapy were excluded. by the modified Bernoulli equation as 4v2, where v is the
We also excluded patients in chronic dialytic treatment velocity of the tricuspid regurgitation jet in m/s. The tricus-
and patients with major cerebrovascular diseases or other pid regurgitant signal was recorded by continuous wave
severe illness. Therapy for HF consisted of furosemide in Doppler echocardiography, and its maximal velocity was
all patients, anti-aldosteronic agents in 15%, angio- measured. Right atrial pressure, estimated on the basis of
tensin-converting enzyme inhibitors in 42%, β-blockers in echocardiographic characteristics of the inferior vena cava
70%, angiotensin AT1 receptor blockers in 31% of pa- and assigned a standardized value, was added to the calcu-
tients. lated gradient to give PAPs. All mean values were derived
The investigation conformed to the principles outlined in from ≥ 3 different measurements, and five if in presence of
the Declaration of Helsinki, and the study protocol was ap- arrhythmia. All recordings were analyzed by two operators
proved by our institutional committee on human research. and the results were averaged.
All patients provided their written informed consent.
2.3 Follow-up
2.2 Two-dimensional and Doppler echocardiography After discharge, patients periodically attended our insti-
Standard M-mode, two-dimensional and Doppler ex- tution outpatient unit for at least 24 months. For patients
aminations were performed during hospitalization after who died or were hospitalized during the follow-up, infor-
clinical stabilization. In all patients left and right ventricular mation was obtained from the attending physicians, or by
systolic and diastolic function were evaluated by M-mode, phone contact and by review of hospital, or physicians’ re-
two-dimensional and Doppler echocardiography using a cords by individuals blinded to the patient’s echocardio-
Philips digital ultrasound machine, Model i-E-33. Left ven- graphic data. The primary end-point was the occurrence of
tricular ejection fraction (LVEF) was calculated by Simp- cardiac death or hospitalization due to cardiac events, whi-
son’s methods. We categorized individuals with a LVEF of chever occurred first. Cardiac death, defined as due to acute
≤ 40% as having HFrEF, and those with ejection fraction of myocardial infarction, ventricular arrhythmias, refractory
> 40% as having HFpEF. For the study of diastolic function, HF, or cardiogenic shock, was confirmed by review of death
the following mitral wave Doppler and tissue Doppler pa- certificates, hospital charts, or physician’s records. Acute
http://www.jgc301.com; jgc@mail.sciencep.com | Journal of Geriatric Cardiology
348 Pirozzi F, et al. Prognostic value of E/DT in HF patients
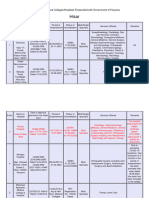
coronary syndrome was defined based on the criteria of Table 1. Echocardiographic parameters of patients with
typical chest pain, enzyme levels, and ECG alterations. The HFrEF and with HFpEF.
date of the last examination, or consultation, was used to HFpEF (n = 51) HFrEF (n = 44) P value
determine the length of follow-up. Left ventricle parameters
2.4 Statistical analysis LVEF (%) 47 ± 5 32 ± 5 0.000*
LVIDd (mm) 55 ± 6.3 60 ± 5.9 0.000*
Continuous variables were expressed as mean ± SD and
LVIDs (mm) 41 ± 6.2 49 ± 7.5 0.000*
categorical data as percentages. Differences between groups
LVEDV (mL) 138 ± 42 169 ± 42 0.001*
were analyzed by t-test and chi-square test, as appropriate.
A P value < 0.05 was considered statistically significant. LVESV (mL) 73 ± 26 116 ± 35 0.000*
Event-free survival curves were estimated with Kap- Mitral E-wave (cm/s) 73.6 ± 29.5 81.4 ± 31.6 0.21
lan-Meier analysis and compared by the log-rank test. Uni- Mitral DT (ms) 195 ± 62 212 ± 70 0.22
variable associations with cardiac events were determined E/e’ 16.2 ± 7.5 15.7 ± 6.7 0.68
by Cox proportional hazards regression. For this purpose, E/DT (m/s )2
50.5 ± 34.4 41.4 ± 27.1 0.15
clinical, laboratory and echocardiographic variables were Right ventricle parameters
considered. Before performing the regression analysis, the TAPSE 19 ± 4 19 ± 4 0.96
proportional hazard assumption was validated by visual Data are presented as mean ± SD. P < 0.05 compared with HFpEF
*
and
inspection of the log [−log(survivor function)] for categori- HFrEF groups. E/DT: mitral peak early diastolic filling velocity to
cal variables and with statistical tests based on Schoenfeld deceleration time ratio; E/e’: mitral peak early diastolic filling velocity and
residuals for continuous variables. The proportional hazard early diastolic velocity by Doppler tissue imaging ratio; HFpEF: heart fail-
assumption was not rejected for any covariate included in ure with preserved ejection fraction; HFrEF: heart failure with reduced
the Cox model. Finally, a stepwise multivariable Cox re- ejection fraction; LVEDV: left ventricular end diastolic volume; LVEF: left
gression analysis was performed (P < 0.10 for model entry ventricular ejection fraction; LVESV: left ventricular end systolic volume;
and P < 0.15 for model retention), considering all variables LVIDd: diastolic left ventricular internal diameter; LVIDs: systolic left
showing a P value < 0.10 at univariable analysis. ventricular internal diameter; Mitral E wave: peak early diastolic filling
velocity; TAPSE: tricuspid annular plane systolic excursion.
3 Results
cantly lower TAPSE (18.3 ± 3.4 mm vs. 20 ± 3.8 mm; P =
The study group consisted of 120 HF patients, 13 of
0.03) compared to patients without events was observed.
which were excluded because the diastolic function could
At univariable analysis we found that NYHA class (HR
not be reliably determined, whereas 12 were lost at fol-
low-up. Thus, the outcome cohort included 95 patients (69 = 1.76; P = 0.02), furosemide dosage (HR = 1.01; P =
men and 26 women, mean age 64.8 ± 12.2 years). The 0.04), TAPSE (HR = 0.93; P = 0.04), DT (HR = 0.99; P =
echocardiographic parameters of patients with HFrEF (n = 0.03) and E/DT (HR = 1.01; P = 0.017) were predictive
51) and patients with HFpEF (n = 44) are reported in Ta- for occurrence of events. Kaplan-Meyer survival estimates
ble 1. for TAPSE or DT are reported in Figure 1. As shown, pa-
During a median follow-up of 37.7 months (5th to 95th tients with TAPSE < 16 mm had lower event free survival
percentile, 24.7 to 49.5 months) we observed 57 combined than patients with TAPSE ≥ 16 mm (P = 0.02). Similarly,
events (death or cardiovascular hospitalization). A fatal car- the outcome was poorer in patients with DT < 140 ms than
diac event occurred in 13 patients, five sudden cardiac death in patients with DT ≥ 140 ms (P = 0.04).
and eight worsening of cardiac disease. Furthermore, 44 At multivariable analysis E/DT (HR = 1.02; P = 0.017)
patients were hospitalized, 41 for decompensated HF, two was the only independent predictor of poor prognosis after
for occurrence of acute coronary syndrome and one for ar- adjustment for NYHA class, furosemide dosage, TAPSE,
rhythmic episode. Baseline characteristics of patients with and DT (Table 4). Values for the chi-square statistics as an
or without events at follow-up are reported in Table 2. The index of the incremental predictive power of clinical vari-
two groups were comparable for demographic, clinical and ables, echocardiographic data, and E/DT are reported in
laboratory data. Also there was no significant difference for Figure 2. As shown, E/DT increased the prognostic power
medications between the two groups. The echocardio- of the model after considering clinical and echocardio-
graphic parameters in patients with, or without events, are graphic parameters (global chi-square from 15.4 to 25.2; P
reported in Table 3 in patients with cardiac events a signifi- = 0.032).
Journal of Geriatric Cardiology | jgc@jgc301.com; http://www.jgc301.com
Pirozzi F, et al. Prognostic value of E/DT in HF patients 349
Table 2. Baseline characteristics of patients with and without Table 3. Echocardiographic measures of patients with and
events at follow-up. without events at follow-up.
Clinical and laboratory No events P Events No-events P value
Events (n = 57)
characteristics (n = 38) value Left ventricular parameters
Age (yr) 65.9 ± 11.8 63.3 ± 12.6 0.3 LVEF (%) 40 ± 10 39 ± 9 0.53
Gender (M/F) 42/15 27/11 0.8 LVIDd (mm) 57.6 ± 6.7 57.8 ± 6.9 0.91
Weight (kg) 78.9 ± 17.1 74.5 ± 15.6 0.2 LVIDs (mm) 45.5 ± 7.9 46.2 ± 8 0.67
I = 1 (1.7) I = 3 (7.8) LVEDV (mL) 149.5 ± 45.5 162.9 ± 42.7 0.15
NYHA class 0.1 LVESV (mL) 91.6 ± 36.6 102.7 ± 40.1 0.17
II = 29 (50.8) II = 24 (63.2)
LVM (g/m2) 248.6 ± 65.3 246.6 ± 62.4 0.88
III = 27 (47.3) III = 11 (29)
Mitral E-wave (cm/s) 79.2 ± 31.2 74.1 ± 30 0.43
CAD 44 (57) 28 (74) 0.7
Mitral DT (ms) 197.2 ± 66.4 215.4± 65.9 0.2
Smoking 20 (35) 12 (32) 0.7
e’ (cm/s) 5.1 ± 1.2 5 ± 1.5 0.8
Diabetes 19 (33) 12 (32) 0.9
E/e’ 16.4 ± 7.8 15.3 ± 5.6 0.5
SBP (mmHg) 125 ± 17 124 ± 13 0.7
E/DT (m/s2) 49.16 ± 33.94 40.23 ± 25.11 0.17
Haemoglobin (g/dL) 12.7 ± 2.1 13.2 ± 1.7 0.2
Right ventricular parameters
Lymphocytes (%) 22.7 ± 7.5 22.2 ± 7.3 0.7
TAPSE (mm) 18.3 ± 3.4 20 ± 3.8 0.03*
Total cholesterol (mg/dL) 163.9 ± 50.8 179.7 ± 36.3 0.2
FAC (%) 35.4 ± 13.2 32.1 ± 11.8 0.2
Serum uric acid (mg/dL) 5.7 ± 1.9 6.2 ± 1.9 0.3
PAPs (mmHg) 35.4 ± 13.2 32.0 ± 11.7 0.2
Serum sodium (mEq/L) 140.4 ± 3.6 140.4 ± 2.8 0.9
RVD basal (mm) 38 ± 5.5 36.5 ± 4.5 0.2
Sinus rhythm 41 (72) 29 (76) 0.6
ICD 7 (12) 4 (10.5) 0.8 * P < 0.05. DT: deceleration time; E: mitral peak early diastolic filling velocity
Medications and early diastolic velocity by Doppler tissue imaging ratio; e’: early diastolic
velocity by Doppler tissue imaging; FAC: fractional area change; LVEDV: left
β-blockers 42 (74) 24 (63) 0.3
ventricular end diastolic volume; LVEF: left ventricular ejection fraction;
ACE-I 22 (39) 18 (47) 0.4
LVESV: left ventricular end systolic volume; LVIDd: diastolic left ventricular
ARB 19 (33) 11 (29) 0.6
internal diameter; LVIDs: systolic left ventricular internal diameter; LVM: left
Antialdosteronic agents 9 (16) 5 (13) 0.7 ventricular mass; Mitral E wave: peak early diastolic filling velocity; PAPs:
Statins 30 (53) 23 (61) 0.4 pulmonary artery systolic pressure; RVD: right ventricular diameter; TAPSE:
Allopurinol 7 (12) 6 (16) 0.6 tricuspid annular plane systolic excursion.
Furosemide (mg/day) 48.6 ± 94.1 29.8 ± 48.4 0.3
Data are presented as mean ± SD or n (%). ACE-I: Angiotensin converting 4 Discussion
enzyme-inhibitors; ARB: angiotensin receptor blockers; CAD: coronary artery
disease; ICD: implantable cardioverter defibrillator; NYHA: New York Heart This study demonstrates that E/DT gives independent
Association; SBP: systolic blood pressure; SD: standard deviation. and incremental prognostic information in a cohort of
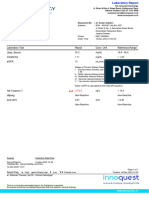
Figure 1. Kaplan-Meier event-free survival estimates. Kaplan-Meier plots showed the time of the combined end point of death and car-
diac hospitalization for patients with (A) TAPSE < 16 mm vs. ≥ 16 mm and (B) DT < 140 ms vs. ≥ 140 ms. DT: deceleration time; TAPSE:
tricuspid annular plane systolic excursion.
http://www.jgc301.com; jgc@mail.sciencep.com | Journal of Geriatric Cardiology
350 Pirozzi F, et al. Prognostic value of E/DT in HF patients
Table 4. Predictors of events at Cox univariable and multi- evaluation of LV function, and mitral Doppler vari-
variable analysis. ables.[18,19]
Univariable analysis In our two-dimensional Doppler echocardiographic study,
Hazard ratio 95% CI P value DT (a measure of LV relaxation) was shorter in patients
NYHA class I, II or III 1.76 1.09–2.84 0.02 with events at follow-up compared to those without events
Furosemide dosage (mg/day) 1.01 1.001–1.006 0.04 and was, therefore, a predictor of the outcome at follow-up
DT (ms) 0.99 0.991–0.910 0.03 either in HFrEF or in HFpEF patients (Figure. 1B). Several
TAPSE (mm) 0.93 0.88–0.99 0.04 studies have shown that noninvasive Doppler measurements
E/DT (m/s2) 1.01 1.001–1.018 0.017 of LV relaxation and filling pressures are predictors of out-
DT: deceleration time; E/DT: mitral peak early diastolic filling velocity and come in patients with HFrEF and HFpEF.[20,21] In particular,
deceleration time ratio; NYHA: New York Heart Association; TAPSE: tricus- Giannuzzi, et al.[22] found that in patients with LV systolic
pid annular plane systolic excursion. dysfunction a short DT adds important prognostic informa-
tion to the other clinical, functional and echocardiographic
variables.
Interestingly, our results do not confirm the prognostic
value of tissue Doppler echocardiography. Hirata, et al.[23]
found that E/e’ ratio > 15 was an excellent predictor of ad-
verse outcome in HF patients and demonstrated the useful-
ness of a combination of systolic function by LVEF and
diastolic function by E/e’. Nevertheless, it must be outlined
that the value of E/e’ has been recently questioned.[24,25] In
particular Mullens, et al.[25] demonstrated that E/e’ ratio may
not be reliable in predicting intra-cardiac filling pressures in
patients with severe HF and extensive reverse remodeling.
Instead, our study shows that an increase in E/DT is as-
sociated with a poor prognosis. Nguyen, et al.[26] in an ani-
mal model of pressure overload induced HF, found that the
Figure 2. Incremental prognostic value of clinical, echocar-
mitral Doppler parameter E/DT reliably predicts the pres-
diographic data and E/DT added sequentially. Global
ence of lung remodeling better than E/e’, suggesting that
Chi-square on Y axis indicates incremental prognostic value of
this parameter could be useful in other models of HF and in
clinical, echocardiographic data and E/DT added sequentially.
E/DT: mitral peak early diastolic filling velocity and deceleration humans.
time ratio. Opposite to our findings, Mishra, et al.[13] showed that
lower E/DT predicted cardiovascular events, whereas peak
patients hospitalized for HF after adjustment for clinical, E velocity and DT alone did not in a population of 3,102
laboratory and conventional echocardiographic parameters. subjects free of prevalent cardiovascular disease and after
Of note, we considered consecutive patients with reduced, adjustment for traditional clinical cardiovascular risk factors.
or preserved LVEF, so our data may be applied to a popula- These different results may be explained by taking into ac-
tion of HF patients with different LV functional abnormali- count the study population composition. Mishra, et al.[13]
ties. studied middle aged to elderly patients with high prevalence
In our study, among clinical variables, NYHA class and of diabetes or hypertension without prevalent cardiovascular
furosemide dosage were predictive of the outcome at uni- disease. In these patients active relaxation of LV is attenu-
variable analysis. The NYHA functional class and fu- ated, resulting in a reduced atrio-ventricular pressure gradi-
rosemide dosage have long been recognized in HF patients ent and in a decreased mitral peak early diastolic filling ve-
as important indicators of the severity of cardiovascular locity.[27] The slow ventricular filling also reduces the
impairment and of survival.[16,17] Our data also confirm the atrio-ventricular pressure gradient that, after peak E velocity,
prognostic utility of TAPSE (Figure 1A), an echocardio- is a determinant of DT; so this latter parameter is prolonged.
graphic parameter of RV function, easy to obtain in all pa- On the other hand, in our HF population, atrial pressure is
tients irrespective of heart rate and rhythm. Previous studies increased in account of loading conditions, atrio-ventricular
reported that TAPSE adds significant prognostic informa- gradient is higher irrespective of LV relaxation, and as a
tion to the NYHA functional class, echocardiographic consequence, peak E velocity increases. Under these cir-
Journal of Geriatric Cardiology | jgc@jgc301.com; http://www.jgc301.com
Pirozzi F, et al. Prognostic value of E/DT in HF patients 351
cumstances rapid ventricular filling time (DT) shortens. tricular remodeling defines outcomes and response to therapy
Therefore, in such conditions of increased loading, E/DT is in heart failure: Valsartan heart failure trial (Val-HeFT) echo-
increased. Of note, in our study population, DT was < 140 cardiographic data. J Am Coll Cardiol 2004; 43: 2022–2027.
ms in 32 out of 95 HF patients, a value that is a commonly 10 Bursi F, McNallan SM, Redfield MM, et al. Pulmonary pres-
sures and death in heart failure: a community study. J Am Coll
observed in patients with elevated filling pressures.[28]
Cardiol 2012; 59: 222–231.
There are limitations to this study. First, this is a single
11 Kjaergaard J, Akkan D, Iversen KK, et al. Right ventricular
centered study, with a small study population. For this rea-
dysfunction as an independent predictor of short- and
son, we did not perform separate analyses for patients with long-term mortality in patients with heart failure. Eur J Heart
HFrEF or HFpEF. Second, pseudo-normalization could be a Fail 2007; 9: 610–616.
problem in evaluating the prognostic value of E/DT in pa- 12 Xie GY, Berk MR, Smith MD, et al. Prognostic value of
tients with severe HF. Finally, the predictive value of echo- Doppler transmitral flow patterns in patients with congestive
cardiographic parameters was not compared with other heart failure. J Am Coll Cardiol 1994; 24: 132–139.
prognostic parameters, such as brain natriuretic peptide. 13 Mishra RK, Galloway JM, Lee ET, et al. The ratio of mitral
However, at our Institution, brain natriuretic peptide levels deceleration time to E-wave velocity and mitral deceleration
are not routinely evaluated, and thus, we cannot perform slope outperform deceleration time alone in predicting car-
this analysis. diovascular outcomes: the Strong Heart Study. J Am Soc
Echocardiogr 2007; 20: 1300–1306.
In conclusion, our results demonstrate that E/DT gives
14 Ho KK, Pinsky JL, Kannel WB, et al. The epidemiology of
independent and incremental prognostic information at fol-
heart failure: the Framingham Study. J Am Coll Cardiol 1993;
low-up after considering clinical and echocardiographic
22: 6A–13A
parameters in HF patients. 15 Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the
echocardiographic assessment of the right heart in adults: a
References report from the American Society of Echocardiography en-
dorsed by the European Association of Echocardiography, a
1 Lee DS, Austin PC, JL, et al. Predicting mortality among pa-
registered branch of the European Society of Cardiology, and
tients hospitalized for heart failure: derivation and validation of a
the Canadian Society of Echocardiography. J Am Soc Echo-
clinical model. JAMA 2003; 290: 2581–2587.
cardiogr 2010; 23: 685–713.
2 Bello NA, Claggett B, Desai AS, et al. Influence of previous
16 Madsen BK, Hansen JF, Stokholm KH, et al. Chronic conges-
heart failure hospitalization on cardiovascular events in patients
tive heart failure. Description and survival of 190 consecutive
with reduced and preserved ejection fraction. Circ Heart Fail
patients with a diagnosis of chronic congestive heart failure
2014; 7: 590–595. based on clinical signs and symptoms. Eur Heart J 1994; 15:
3 Zafrir B, Goren Y, Paz H, et al. Risk score model for predicting 303–310.
mortality in advanced heart failure patients followed in a heart 17 Cody RJ, Kubo SH, Pickworth KK. Diuretic treatment for the
failure clinic. Congest Heart Fail 2012; 18: 254–261. sodium retention of congestive heart failure. Arch Intern Med
4 Peterson PN, Rumsfeld JS, Liang L, et al. A validated risk score 1994; 154: 1905–1914.
for in-hospital mortality in patients with heart failure from the 18 Damy T, Kallvikbacka-Bennett A, Goode K, et al. Prevalence
American Heart Association get with the guidelines program. of, associations with, and prognostic value of tricuspid annular
Circ Cardiovasc Qual Outcomes 2010; 3: 25–32. plane systolic excursion (TAPSE) among out-patients referred
5 O'Connor CM, Abraham WT, Albert NM, et al. Predictors of for the evaluation of heart failure. J Card Fail 2012; 18:
mortality after discharge in patients hospitalized with heart 216–225.
failure: an analysis from the Organized Program to Initiate 19 Ghio S, Recusani F, Klersy C, et al. Prognostic usefulness of
Lifesaving Treatment in Hospitalized Patients with Heart the tricuspid annular plane systolic excursion in patients with
Failure (OPTIMIZE-HF). Am Heart J 2008; 156: 662–673. congestive heart failure secondary to idiopathic or ischemic
6 Pocock SJ, Wang D, Pfeffer MA, et al. Predictors of mortality dilated cardiomyopathy. Am J Cardiol 2000; 85: 837–842.
and morbidity in patients with chronic heart failure. Eur Heart 20 Ohtani T, Mohammed SF, Yamamoto K, et al. Diastolic
J 2006; 27: 65–75. stiffness as assessed by diastolic wall strain is associated with
7 Alba AC, Agoritsas T, Jankowski M, et al. Risk prediction adverse remodelling and poor outcomes in heart failure with
models for mortality in ambulatory patients with heart failure: preserved ejection fraction. Eur Heart J 2012; 33: 1742–1749.
a systematic review. Circ Heart Failure 2013; 6: 881–889. 21 Werner GS, Schaefer C, Dirks R, et al. Prognostic value of
8 Agha SA, Kalogeropoulos AP, Shih J, et al. Echocardiogra- Doppler echocardiographic assessment of left ventricular fill-
phy and risk prediction in advanced heart failure: incremental ing in idiopathic dilated cardiomyopathy. Am J Cardiol 1994;
value over clinical markers. J Card Fail 2009; 15: 586–592. 73: 792–798.
9 Wong M, Staszewsky L, Latini R, et al. Severity of left ven- 22 Giannuzzi P, Temporelli PL, Bosimini E, et al. Independent
http://www.jgc301.com; jgc@mail.sciencep.com | Journal of Geriatric Cardiology
352 Pirozzi F, et al. Prognostic value of E/DT in HF patients
and incremental prognostic value of Doppler-derived mitral aging in the estimation of intracardiac filling pressure in de-
deceleration time of early filling in both symptomatic and compensated patients with advanced systolic heart failure. Cir-
asymptomatic patients with left ventricular dysfunction. J Am culation 2009; 119: 62–70.
Coll Cardiol 1996; 28: 383–390. 26 Nguyen TD, Shingu Y, Schwarzer M, et al. The E-Wave
23 Hirata K, Hyodo E, Hozumi T, et al. Usefulness of a combi- deceleration rate E/DT outperforms the tissue doppler-derived
nation of systolic function by left ventricular ejection fraction index E/e' in characterizing lung remodeling in heart failure
and diastolic function by E/E' to predict prognosis in patients with preserved ejection fraction. PLoS One 2013; 8: e82077
with heart failure. Am J Cardiol 2009; 103: 1275–1279. 27 Lester SJ, Tajik AJ, Nishimura RA, et al. Unlocking the mys-
24 Dokainish H, Nguyen JS, Bobek J, et al. Assessment of the teries of diastolic function: deciphering the Rosetta Stone 10
American Society of Echocardiography-European Association years later. J Am Coll Cardiol 2008; 51: 679–689.
of Echocardiography guidelines for diastolic function in patients 28 Stoddard MF, Pearson AC, Kern MJ, et al. Left ventricular
with depressed ejection fraction: an echocardiographic and inva- diastolic function: comparison of pulsed Doppler echocardio-
sive haemodynamic study. Eur J Echocardiogr 2011; 12: graphic and hemodynamic indexes in subjects with and with-
857–864. out coronary artery disease. J Am Coll Cardiol 1989; 13:
25 Mullens W, Borowski AG, Curtin RJ et al. Tissue Doppler im- 327–336.
Journal of Geriatric Cardiology | jgc@jgc301.com; http://www.jgc301.com
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pass PACES in Single AttemptDocument101 pagesPass PACES in Single AttemptSOMNATHNo ratings yet
- Kidney Kard - 6th EditionDocument4 pagesKidney Kard - 6th EditionHamlot100% (1)
- Acute Decompensated Heart Failure Check for UnderstandingDocument3 pagesAcute Decompensated Heart Failure Check for UnderstandingSistine Rose LabajoNo ratings yet
- Impaired Myocardial Relaxation With Exercise Determines Peak Aerobic Exercise Capacity in Heart Failure With Preserved Ejection FractionDocument5 pagesImpaired Myocardial Relaxation With Exercise Determines Peak Aerobic Exercise Capacity in Heart Failure With Preserved Ejection FractionHugo ARNo ratings yet
- Nejm DeltaDocument10 pagesNejm DeltaTim MooreNo ratings yet
- MP Hospital CuernavacaDocument279 pagesMP Hospital CuernavacaHugo ARNo ratings yet
- Arya 08 130Document6 pagesArya 08 130Hugo ARNo ratings yet
- HHS Public Access: Common Findings in Late Gestation Fetal EchocardiographyDocument14 pagesHHS Public Access: Common Findings in Late Gestation Fetal EchocardiographyHugo ARNo ratings yet
- Covid PD Pnykt JNTG PDFDocument5 pagesCovid PD Pnykt JNTG PDFSri PertiwiNo ratings yet
- Uog 20167Document8 pagesUog 20167Hugo ARNo ratings yet
- Maximal Aortic Valve Cusp Separation and Severity of Aortic StenosisDocument4 pagesMaximal Aortic Valve Cusp Separation and Severity of Aortic StenosisHugo ARNo ratings yet
- Efficacy of Chloroquine and Hydroxychloroquine in The Treatment of COVID-19Document9 pagesEfficacy of Chloroquine and Hydroxychloroquine in The Treatment of COVID-19Anabel Guadalupe Timaná ChávezNo ratings yet
- Crocetin Protects Against Cardiac Hypertrophy by Blocking MEK-ERK1/2 Signalling PathwayDocument17 pagesCrocetin Protects Against Cardiac Hypertrophy by Blocking MEK-ERK1/2 Signalling PathwayHugo ARNo ratings yet
- MainDocument6 pagesMaingevowo3277No ratings yet
- Tenecteplae AlteplaseDocument7 pagesTenecteplae AlteplaseHugo ARNo ratings yet
- Efficacy of Chloroquine and Hydroxychloroquine in The Treatment of COVID-19Document9 pagesEfficacy of Chloroquine and Hydroxychloroquine in The Treatment of COVID-19Anabel Guadalupe Timaná ChávezNo ratings yet
- The Usefulness of sST2 and Galectin-3 As Novel Biomarkers For Better Risk Stratification in Hypertrophic CardiomyopathyDocument8 pagesThe Usefulness of sST2 and Galectin-3 As Novel Biomarkers For Better Risk Stratification in Hypertrophic CardiomyopathyHugo ARNo ratings yet
- Estudio Cochrane 1998 - Albumina Vs Salino PDFDocument6 pagesEstudio Cochrane 1998 - Albumina Vs Salino PDFHugo ARNo ratings yet
- Guideline ADA 2010 in Hyperglicemia CrisisDocument9 pagesGuideline ADA 2010 in Hyperglicemia CrisisAissyiyah Nur An NisaNo ratings yet
- Br. J. Anaesth.-2011-Spieth-bja - Aer144 PDFDocument10 pagesBr. J. Anaesth.-2011-Spieth-bja - Aer144 PDFHugo ARNo ratings yet
- Oncologic Emergency ReviewDocument11 pagesOncologic Emergency ReviewHugo ARNo ratings yet
- Chest Tube InsertionDocument4 pagesChest Tube InsertionHugo ARNo ratings yet
- Manejo de Fluidos en La Practica Diaria en La UCIDocument6 pagesManejo de Fluidos en La Practica Diaria en La UCIHugo ARNo ratings yet
- Angioplastia Vs Trombolisis en AncianoDocument10 pagesAngioplastia Vs Trombolisis en AncianoHugo ARNo ratings yet
- GOLD Report 2014 Jan23Document102 pagesGOLD Report 2014 Jan23Alex Corzo MarticorenaNo ratings yet
- Idsa 2010Document32 pagesIdsa 2010Monica S. SuarezNo ratings yet
- ECG Basics: A Concise Guide to ECG InterpretationDocument79 pagesECG Basics: A Concise Guide to ECG InterpretationMuhammad Yufimar Rizza FadilahNo ratings yet
- Hisar EmpanelledDocument21 pagesHisar EmpanelledGill Gauravdeep SinghNo ratings yet
- ECG QuizDocument3 pagesECG QuizRonnie LimNo ratings yet
- Jambi Cardiology Update WorkshopDocument3 pagesJambi Cardiology Update WorkshopFahrurrozi SyarifNo ratings yet
- AT Vs AVNRT ECGDocument10 pagesAT Vs AVNRT ECGRushil NundlallNo ratings yet
- Valvular Heart DiseaseDocument33 pagesValvular Heart Diseasesimran kaurNo ratings yet
- Myocardial Infarction (Stemi) - Tennessee: Statpearls PublishingDocument3 pagesMyocardial Infarction (Stemi) - Tennessee: Statpearls PublishingMery AlizaNo ratings yet
- Differential Diagnosis of CHDDocument42 pagesDifferential Diagnosis of CHDDr Piyush100% (1)
- Magdy El-Masry Prof. of Cardiology Tanta UniversityDocument55 pagesMagdy El-Masry Prof. of Cardiology Tanta UniversityPrabJot SinGhNo ratings yet
- 1 s2.0 S2772930322004367 MainDocument15 pages1 s2.0 S2772930322004367 MainVimal NishadNo ratings yet
- Coronary Sinus Aneurysm: Incidental Discovery During Coronary Artery Bypass GraftingDocument3 pagesCoronary Sinus Aneurysm: Incidental Discovery During Coronary Artery Bypass GraftingasclepiuspdfsNo ratings yet
- Nephrotic Nephritic SyndromeDocument15 pagesNephrotic Nephritic Syndromeshefalika mandremNo ratings yet
- Atrial Fibrillation CASE STUDYDocument2 pagesAtrial Fibrillation CASE STUDYChristianneMikeNo ratings yet
- Questions PharmcologyDocument17 pagesQuestions Pharmcologylalitrajindolia100% (2)
- Ventricular Septal DefectDocument4 pagesVentricular Septal DefectMarina RotaruNo ratings yet
- Av BlockDocument38 pagesAv BlockLanna Harumiya100% (1)
- Hafiz Abdul Rehman (1) - CompressedDocument1 pageHafiz Abdul Rehman (1) - CompressedFaisal BasharatNo ratings yet
- Coronary Artery Disease Symptoms, Causes, and TreatmentDocument6 pagesCoronary Artery Disease Symptoms, Causes, and TreatmentDivya PriyaNo ratings yet
- STEMI InferoposteriorDocument30 pagesSTEMI InferoposteriorKrisna PonggalungguNo ratings yet
- Vijayalakshmi 2008Document7 pagesVijayalakshmi 2008Rakesh DashNo ratings yet
- KB23BB393 HTS005 AshariDocument1 pageKB23BB393 HTS005 AshariI G. A. Ratna DewiNo ratings yet
- DialysisDocument6 pagesDialysisPrincess Joy Torrijas Factora0% (1)
- MTB Cardiology NotesDocument7 pagesMTB Cardiology Noteskabal321No ratings yet
- Pediatric Advanced Life Support (PALS) - UpToDateDocument51 pagesPediatric Advanced Life Support (PALS) - UpToDatenana100% (1)
- Diognosa Banding EdemaDocument1 pageDiognosa Banding EdemaMargareth SitorusNo ratings yet
- RDC 3385 Resolution Economic InfoDocument4 pagesRDC 3385 Resolution Economic InfoLackner MarceloNo ratings yet
- Bradicardy ManagementDocument7 pagesBradicardy ManagementMarshall ThompsonNo ratings yet