Professional Documents
Culture Documents
Nanda, Nic, and Noc Linkages: Home Care
Uploaded by
Lisa YusidaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nanda, Nic, and Noc Linkages: Home Care
Uploaded by
Lisa YusidaCopyright:
Available Formats
740 UNIT VII / Responses to Altered Urinary Elimination
• Refer client for urologic examination and incontinence evalu- (Johnson et al., 2000) when caring for the client with urinary
ation. Clients who assume that urinary incontinence is a nor- incontinence.
mal part of the aging may not be aware of treatment options.
• Explore alternative coping strategies with client, significant Home Care
other, staff, and other health team members. Protective pads Because urinary incontinence is a contributing factor in the in-
or shields, good perineal hygiene, scheduled voiding, and stitutionalization of many older people, client and family
clothing that does not interfere with toileting can enhance teaching can have a significant impact on maintaining inde-
continence. pendence and residence in the community. Address possible
causes of incontinence and appropriate treatment measures.
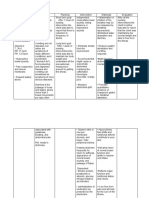
Using NANDA, NIC, and NOC Refer for urologic examination if not already completed. Dis-
Chart 26– 4 shows links between NANDA nursing diag- cuss fluid intake management, perineal care, and products for
noses, NIC (McCloskey & Bulechek, 2000), and NOC clothing protection.
CHART 26–4 NANDA, NIC, AND NOC LINKAGES
The Client with Urinary Retention or Incontinence
NURSING DIAGNOSES NURSING INTERVENTIONS NURSING OUTCOMES
• Urinary Retention • Urinary Bladder Training • Urinary Continence
• Urinary Catheterization: Intermittent • Urinary Elimination
• Urinary Retention Care
• Functional Urinary Incontinence • Prompted Voiding • Urinary Continence
• Urinary Habit Training • Urinary Elimination
• Urinary Elimination Management • Tissue Integrity: Skin & Mucous
Membranes
• Stress Urinary Incontinence • Pelvic Muscle Exercise • Urinary Continence
• Urinary Incontinence Care
• Weight Management
• Urge Urinary Incontinence • Fluid Management • Urinary Continence
• Medication Management
Note. Data from Nursing Outcomes Classification (NOC) by M. Johnson & M. Maas (Eds.), 1997, St. Louis: Mosby; Nursing Diagnoses: Definitions & Classification 2001–2002 by
North American Nursing Diagnosis Association, 2001, Philadelphia: NANDA; Nursing Interventions Classification (NIC) by J.C. McCloskey & G. M. Bulechek (Eds.), 2000, St. Louis:
Mosby. Reprinted by permission.
Nursing Care Plan
A Client with Urinary Incontinence
Anna Giovanni, a 76-year-old retired ment therapy for about 10 years afterward. She is taking digoxin
teacher, has been widowed for 10 years and 0.125 mg daily, furosemide 40 mg twice daily, and potassium
lives alone.Mrs.Giovanni’s eldest daughter expresses concern that chloride 20 mEq 3 times daily for mild heart failure.
her mother seems increasingly reluctant to leave her apartment to Physical assessment reveals a moderate cystourethrocele and
visit friends and family.She reports a strong odor of urine through- atrophy of vaginal and vulvar tissues. Moderate perineal dermati-
out her mother’s apartment and that her mother’s bed is often tis is noted.Pelvic floor strength is weak.Urinalysis is within normal
wet. She expresses worry about needing to place her mother in a limits, and postvoiding residual urine is 5 mL.
nursing home if she cannot continue to live independently. Analysis of Mrs. Giovanni’s voiding diary shows moderate con-
sumption of tea and juices throughout the day, nine daytime
ASSESSMENT voidings and four night voidings with an average volume of
Jane Oberle, RN, a nurse practitioner, examines Mrs. Giovanni who about 250 mL per void. She notices urine leakage most often in
admits that she has problems with urine leakage when laughing the late afternoon and at night. Ms. Oberle identifies a diagnoses
and coughing, and a strong urge to void on hearing the sound of of stress incontinence with an urgency component and decides
running water. At night, her urge to void is so strong that she of- to try a conservative approach before referring Mrs. Giovanni for
ten cannot reach the bathroom in time. Mrs. Giovanni denies a further testing and possible cystourethrocele repair. She pre-
history of UTIs, neurologic disorders, or difficulty with her bowels. scribes estrogen cream, tolterodine (Detrol), and a barrier cream
She had a hysterectomy at age 52 and was on hormone replace- to treat Mrs. Giovanni’s vulvitis.
CHAPTER 26 / Nursing Care of Clients with Urinary Tract Disorders 741
DIAGNOSIS • Introduce commercial products available for clothing and
Ms. Oberle identifies the following nursing diagnoses for Mrs. furniture protection, encouraging experimentation to identify
Giovanni. the most helpful product(s).
• Provide a commode for bedside at night and adequate lighting
• Stress urinary incontinence related to weak pelvic floor muscula-
to prevent injury.
ture and tissue atrophy
• Schedule follow-up visits and evaluations to reinforce teaching.
• Urge urinary incontinence related to excess intake of caffeine
and citrus juices EVALUATION
• Impaired skin integrity related to constant contact of urine with Three months after her initial visit, Mrs. Giovanni states that she is
perineal tissues doing very well, experiencing occasional leakage of small
• Ineffective coping related to inability to control urine leakage amounts of urine,primarily when sneezing,coughing,or laughing.
She finds a minipad adequate for protection and is often able to
EXPECTED OUTCOMES
remain dry all day. She has had no further problems with enuresis
The expected outcomes are that Mrs. Giovanni will:
since changing her evening furosemide dose to late afternoon
• Remain dry between voidings and at night. and limiting her fluids after dinner. She can make it to the bath-
• Demonstrate improved perineal muscle strength. room and no longer needs the bedside commode. Her perineal
• Regain and maintain perineal skin integrity. tissue is intact, and she demonstrates improved muscle strength.
• Return to her previous level of social activity. Anna’s daughter says her mother is beginning to resume her nor-
mal social activities, and that she is no longer worried about her
PLANNING AND IMPLEMENTATION
mother’s ability to care for herself independently.
Ms. Oberle and the clinic staff plan and implement the following
interventions with Mrs. Giovanni and her daughter. Critical Thinking in the Nursing Process
• Teach how to identify pelvic floor muscles and how to perform 1. What factors in Mrs. Giovanni’s past medical history and cur-
Kegel exercises. rent medication regimen contributed to her nighttime incon-
• Suggest drinking decaffeinated tea and noncitrus fruit juices tinence?
(grape, apple, and cranberry). 2. What is the rationale for including an intervention to teach
• Encourage to minimize fluid intake after evening meal. Mrs. Giovanni about perineal cleansing as part of her care
• Change afternoon dose of furosemide from 9:00 P.M. to 3:00 P.M. plan?
• Instruct to void by the clock, gradually increasing intervals from 3. Develop a care plan for Mrs. Giovanni for the nursing diagno-
every 45 to 60 minutes to every 2 to 2.5 hours. Advise to main- sis, Situational low self-esteem related to urinary incontinence.
tain shorter voiding intervals for 2 to 3 hours after furosemide
doses. See Evaluating Your Response in Appendix C.
• Teach to cleanse perineal area, wiping front to back, after each
voiding or incident of urine leakage.
EXPLORE MediaLink
NCLEX review questions, case studies, care plan activities, MediaLink Click on Chapter 26 to select the activities for this chapter. For ani-
applications, and other interactive resources for this chapter can be mations, video clips, more NCLEX review questions, and an audio
found on the Companion Website at www.prenhall.com/lemone. glossary, access the Student CD-ROM accompanying this textbook.
BIBLIOGRAPHY
Ackley, B. J., & Ladwig, G. B. (2002). Nursing Bardsley, A. (1999). Assessment of incontinence. Bullock, B. A., & Henze, R. L. (2000). Focus on
diagnosis handbook: A guide to planning care Elder Care, 11(9), 36–39. pathophysiology. Philadelphia: Lippincott.
(5th ed.). St. Louis: Mosby. Baxter, A. (1999). Bladder cancer: Its diagnosis Fontaine, K. L. (2000). Healing practices: Alterna-
Ahya, S. N., Flood, K., & Paranjothi, S. (Eds.). and treatment. Nursing Times, 95(41), 42–44. tive therapies for nursing. Upper Saddle River,
(2001). The Washington manual of medical Braunwald, E., Fauci, A. S., Kasper, D. L., Hauser, NJ: Prentice Hall Health.
therapeutics (30th ed.). Philadelphia: Lippin- S. L., Longo, D. L., & Jameson, J. L. (2001). Gallo, J. J., Busby-Whitehead, J., Rabins, P. V.,
cott Williams & Wilkins. Harrison’s principles of internal medicine Silliman, R. A., & Murphy, J. B. (Eds.). (1999).
American Cancer Society. (2002). Cancer facts (15th ed.). New York: McGraw-Hill. Reichel’s care of the elderly: Clinical aspects
and figures 2002. Atlanta: Author.
You might also like
- Urinary CalculiDocument2 pagesUrinary CalculiJayceeniPatricia CoronelNo ratings yet
- Week 11: Nursing Care of Patients With Intestinal and Rectal Disorders Abnormalities of Fecal EliminationDocument9 pagesWeek 11: Nursing Care of Patients With Intestinal and Rectal Disorders Abnormalities of Fecal Eliminationeliza luisNo ratings yet
- Triptico ITUDocument2 pagesTriptico ITUClaudi Tperez0% (1)
- Hand-Out - Alterations in Fluid and Electrolyte and Acid-Base Imbalance, Renal FunctionDocument8 pagesHand-Out - Alterations in Fluid and Electrolyte and Acid-Base Imbalance, Renal FunctionVIVIEN CONSIGNANo ratings yet
- Alterations in Fluid and Electrolyte and AcidDocument11 pagesAlterations in Fluid and Electrolyte and Acidlaurie.charlynjaneNo ratings yet
- Urinary System K.6Document20 pagesUrinary System K.6Ardila DilaNo ratings yet
- Clinical Review: Managing Urinary Incontinence in Older PeopleDocument15 pagesClinical Review: Managing Urinary Incontinence in Older PeopleMatthias WollfNo ratings yet
- Diverticulitis Case StudyDocument2 pagesDiverticulitis Case StudyAhmad RizkiNo ratings yet
- Group Iv - Urinary Elimination PDFDocument96 pagesGroup Iv - Urinary Elimination PDFMeshezabel AsentistaNo ratings yet
- Urinary Incontinence: Pathophysiology and Management OutlineDocument6 pagesUrinary Incontinence: Pathophysiology and Management OutlineNgurah AndhikaNo ratings yet
- Fundamentals of Nursing (NUR 101) : Prepared byDocument19 pagesFundamentals of Nursing (NUR 101) : Prepared bydoody7alaNo ratings yet
- Urinary EliminationDocument39 pagesUrinary EliminationSol Angelika G. SuropiaNo ratings yet
- Urinary Incontinence HandoutDocument6 pagesUrinary Incontinence HandoutGautam ReddyNo ratings yet
- Course Task 7Document3 pagesCourse Task 7Justine Dinice MunozNo ratings yet
- Bowel Elimination ProblemsDocument33 pagesBowel Elimination ProblemsAnonymous iG0DCOfNo ratings yet
- Group 1Document9 pagesGroup 1VIVIEN CONSIGNANo ratings yet
- Bedwetting in ChildrenDocument41 pagesBedwetting in ChildrenAnkit ManglaNo ratings yet
- 1 Urinary Incontinence in ChildrenDocument5 pages1 Urinary Incontinence in Childrenguido murrieta rojasNo ratings yet
- Urinary Incontinence in Women: DR Mangala DissanayakeDocument59 pagesUrinary Incontinence in Women: DR Mangala DissanayakeAdnan WalidNo ratings yet
- Health AssementDocument13 pagesHealth AssementClarence ViboraNo ratings yet
- Bladder Atony/Urinary RetentionDocument11 pagesBladder Atony/Urinary RetentionAngela CaguitlaNo ratings yet
- Urinary Tract Infection: Jenniferlee Dibernardo Pathophysiology ProjectDocument19 pagesUrinary Tract Infection: Jenniferlee Dibernardo Pathophysiology ProjectAhmad MatterNo ratings yet
- NCP BPHDocument1 pageNCP BPHyasiraNo ratings yet
- Masalah-Masalah Kesehatan Pada Lansia Dan Penanganannya: I Gede Putu Darma Suyasa, SKP, MNG, PHDDocument45 pagesMasalah-Masalah Kesehatan Pada Lansia Dan Penanganannya: I Gede Putu Darma Suyasa, SKP, MNG, PHDCok ArisaNo ratings yet
- Fecal Elimination EnemaDocument5 pagesFecal Elimination EnemaVia Kristel ZapantaNo ratings yet
- Il Effects of Dai Treatment FinalDocument96 pagesIl Effects of Dai Treatment FinalDr SadiaNo ratings yet
- Group-5 NCM-107 NCPDocument4 pagesGroup-5 NCM-107 NCPbulok netflakes100% (1)
- Altered Urinary Elimination - ADPCN Resource UnitDocument5 pagesAltered Urinary Elimination - ADPCN Resource UnitChillette FarraronsNo ratings yet
- Urinary EliminationDocument26 pagesUrinary EliminationyeshumasihNo ratings yet
- Neurogenic Bladder: Mobility Clinic Case-Based Learning ModuleDocument11 pagesNeurogenic Bladder: Mobility Clinic Case-Based Learning ModuleJamaicaNo ratings yet
- Urinary Incontinence in PregnancyDocument24 pagesUrinary Incontinence in PregnancyChidube UkachukwuNo ratings yet
- Genital Tract InjuriesDocument74 pagesGenital Tract InjuriesDevuchandana RNo ratings yet
- Encopresis, (Fecal Incontinence) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEncopresis, (Fecal Incontinence) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Bowel Elimination and Urinary Incontinence ProblemsDocument5 pagesBowel Elimination and Urinary Incontinence ProblemsMegan Rose MontillaNo ratings yet
- NCP 1Document3 pagesNCP 1Mary Antonette Adriano EnriquezNo ratings yet
- Managing Urinary Incontinence in Older PeopleDocument5 pagesManaging Urinary Incontinence in Older PeopleSarah Naura IrbahNo ratings yet
- Concept of EliminationDocument42 pagesConcept of EliminationOpen UserNo ratings yet
- Urinary Incontinence - MKLDocument42 pagesUrinary Incontinence - MKLFreeburn SimunchembuNo ratings yet
- Unit 6 Concet of EliminationDocument32 pagesUnit 6 Concet of EliminationAbdur Rehman100% (1)
- Urinary and Bowel Elimination Notes 2019Document8 pagesUrinary and Bowel Elimination Notes 2019claraenze mendozaNo ratings yet
- Bowel and Bladder Retraining: Causes of Urinary IncontinenceDocument3 pagesBowel and Bladder Retraining: Causes of Urinary IncontinencePiannsNo ratings yet
- Urinary EliminationDocument6 pagesUrinary EliminationryamonamourofficialNo ratings yet
- Fundamental in Nursing PracticeDocument5 pagesFundamental in Nursing PracticeSobani A. HadjiMotalibNo ratings yet
- Lecture 5 Urinary Incontinence-Part 1Document51 pagesLecture 5 Urinary Incontinence-Part 1fordsantiago01No ratings yet
- ProlapseDocument51 pagesProlapsejijaniNo ratings yet
- Perineal Care: Perineal Area Is A Conducive Environment To TheDocument4 pagesPerineal Care: Perineal Area Is A Conducive Environment To TheAbegail BalloranNo ratings yet
- Urinary Incontinence: 2 PathophysiologyDocument8 pagesUrinary Incontinence: 2 PathophysiologyZiedTrikiNo ratings yet
- Medsurg: 6.3 Urinary DisordersDocument5 pagesMedsurg: 6.3 Urinary DisordersIvy VillalobosNo ratings yet
- Chapter 45 Urinary EliminationDocument29 pagesChapter 45 Urinary EliminationKwenaNo ratings yet
- Altered Urinary EliminationDocument9 pagesAltered Urinary EliminationShamsa AfdalNo ratings yet
- Incontinence: DR - Swathi Singh MPT Orthopaedics, MiapDocument69 pagesIncontinence: DR - Swathi Singh MPT Orthopaedics, MiapSonu GuptaNo ratings yet
- KKKKDocument22 pagesKKKKMARY CLAIRE SUMILHIGNo ratings yet
- 53c. IMPERFORATE ANUS 2021 2022Document23 pages53c. IMPERFORATE ANUS 2021 2022coco brillqnteNo ratings yet
- Subjective: Long Term Objective: Long Term ObjectiveDocument2 pagesSubjective: Long Term Objective: Long Term ObjectiveRAFNo ratings yet
- Hygienic CareDocument5 pagesHygienic CareDanica DaniotNo ratings yet
- .-.Spina Bifida 2.Document31 pages.-.Spina Bifida 2.Ess IsnotyouNo ratings yet
- Cholelithiasis PDFDocument2 pagesCholelithiasis PDFVishal RamanNo ratings yet
- Bladder Extrophy: Medical ManagementDocument8 pagesBladder Extrophy: Medical ManagementChristian James CamaongayNo ratings yet
- Tog 12695Document9 pagesTog 12695saeed hasan saeedNo ratings yet
- Elimination - Urinary and BowelDocument58 pagesElimination - Urinary and BowelAnn A.No ratings yet
- Measuring Vital Signs: Lisa YusidaDocument12 pagesMeasuring Vital Signs: Lisa YusidaLisa YusidaNo ratings yet
- Measuring Vital Signs: Lisa YusidaDocument12 pagesMeasuring Vital Signs: Lisa YusidaLisa YusidaNo ratings yet
- Measuring Vital SignsDocument3 pagesMeasuring Vital SignsLisa YusidaNo ratings yet
- Nursing Management of Patients With Urinary Incontinence: Moh Nursing Clinical Practice Guidelines 1/2003Document45 pagesNursing Management of Patients With Urinary Incontinence: Moh Nursing Clinical Practice Guidelines 1/2003Lisa YusidaNo ratings yet
- Eye and Ears AssessmentDocument17 pagesEye and Ears AssessmentPrincess AñabezaNo ratings yet
- Triage Assessment of Psychiatric Patient LectureDocument31 pagesTriage Assessment of Psychiatric Patient Lectureهشام عفانه100% (1)
- What? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanDocument45 pagesWhat? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanM Rizky Assilmy LubisNo ratings yet
- Pressure Ulcer Assessment Chart & Body MapDocument2 pagesPressure Ulcer Assessment Chart & Body MapWidfdsafdsaNo ratings yet
- National Consolidated Guidelines For PMTCT and The Management of HIV in Children, Adolescents and AdultsDocument136 pagesNational Consolidated Guidelines For PMTCT and The Management of HIV in Children, Adolescents and AdultsLaura Lopez Gonzalez100% (12)
- Fetal DistressDocument111 pagesFetal DistressSakariye SuleimanNo ratings yet
- Seizure Disorders: Assessment and Diagnostic FindingsDocument3 pagesSeizure Disorders: Assessment and Diagnostic FindingsBlessed GarcianoNo ratings yet
- SOAP Vs HOPSDocument2 pagesSOAP Vs HOPSJehiah HopeNo ratings yet
- The Pediatric Physical Exam:: Who, When, What and Why?Document26 pagesThe Pediatric Physical Exam:: Who, When, What and Why?Carlo Emmanuel SantosNo ratings yet
- Health Grade10 4th QuarterDocument40 pagesHealth Grade10 4th QuarterYnjel HilarioNo ratings yet
- (BHU) DoneDocument6 pages(BHU) Donedr.venkat r singhNo ratings yet
- Fitzpatricks Dermatology in General Medicine 8ed 1Document10 pagesFitzpatricks Dermatology in General Medicine 8ed 1ANTINNo ratings yet
- Covid 19 WorksheetsDocument16 pagesCovid 19 WorksheetsKarla Paola MoralesNo ratings yet
- Liver BiopsyDocument3 pagesLiver BiopsyBiway RegalaNo ratings yet
- Therapeutic Plasma Exchange in Thrombotic Thrombocytopenic PurpuraDocument9 pagesTherapeutic Plasma Exchange in Thrombotic Thrombocytopenic Purpurasugi9namliNo ratings yet
- Re-Test SUBJECT-English Core Class - Xi Time: 2 Hrs. M.M: 50 General InstructionsDocument8 pagesRe-Test SUBJECT-English Core Class - Xi Time: 2 Hrs. M.M: 50 General InstructionsSunilDwivediNo ratings yet
- Effects of Advanced Carbohydrate Counting On Glucose Control and QolDocument9 pagesEffects of Advanced Carbohydrate Counting On Glucose Control and QollloplNo ratings yet
- FCPS SurgeryDocument106 pagesFCPS Surgeryrehan hayderNo ratings yet
- World AIDS Day 2023-21797Document3 pagesWorld AIDS Day 2023-21797shyamNo ratings yet
- TCM Acupoint TheoryDocument57 pagesTCM Acupoint Theorydishku100% (2)
- It Just Makes Sense 2012Document25 pagesIt Just Makes Sense 2012Emf RefugeeNo ratings yet
- Chandy C. John - Advances in The Diagnosis and Treatment of Pediatric Infectious Diseases - 2013Document212 pagesChandy C. John - Advances in The Diagnosis and Treatment of Pediatric Infectious Diseases - 2013Alla AlkateebNo ratings yet
- Buku Panduan Mahasiswa Blok 11 2021-2022 (Kurikulum 2012) - 25-34Document10 pagesBuku Panduan Mahasiswa Blok 11 2021-2022 (Kurikulum 2012) - 25-34Qonita AztNo ratings yet
- Tuesday 14 January 2020: BiologyDocument24 pagesTuesday 14 January 2020: Biologysham80% (5)
- Compilation AnesthesiaDocument5 pagesCompilation AnesthesiaNorjetalexis CabreraNo ratings yet
- Name: - Ecol, Shenna C. - Date: - November 16, 2020 - Year/Section: BS-Criminology IIIDocument3 pagesName: - Ecol, Shenna C. - Date: - November 16, 2020 - Year/Section: BS-Criminology IIIJoenetha Ann ApariciNo ratings yet
- Product CatalogDocument32 pagesProduct Catalogharshad koyandeNo ratings yet
- Incise Drapes UK GX750 6pDocument6 pagesIncise Drapes UK GX750 6pbouchra8blsNo ratings yet
- Bacte HandoutsDocument138 pagesBacte HandoutsCandy Lorraine Alicante PascoNo ratings yet
- Human Papillomavirus InfectionDocument78 pagesHuman Papillomavirus InfectionJoaquín PeñaNo ratings yet