Professional Documents
Culture Documents
Hyperkalaemia Formulary
Uploaded by
Miguel SanJuanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hyperkalaemia Formulary
Uploaded by
Miguel SanJuanCopyright:
Available Formats
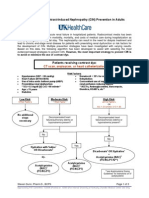
Initial Management of Acute Hyperkalaemia
(District)
Introduction
Acute hyperkalaemia is associated with cardiac arrhythmias and cardiac arrest. The risk is highest
in patients with:
K+ ≥7.0 mmol/l
A rapid and/or large rise from baseline K+ (some patients have a baseline K+ of 6-6.5 for
example
Pre-existing cardiac conduction disorders.
Life-threatening hyperkalaemia may also be heralded by ECG changes and symptoms (generalised
muscle weakness).
Assessment
1. Repeat the K+ level to confirm genuine hyperkalaemia. If initial K+ level is severe (≥7.0
mmol/l), the repeat blood test should be on an urgent venous blood gas sample (VBG).
2. Perform an immediate ECG: changes may or may not be present, and a normal ECG does
not guarantee patient safety. Abnormalities include (those in bold are highest risk for
progression to cardiac arrest):
a. T waves – narrow base, peaked
b. Wide QRS, long PR
c. Absent P waves, junctional rhythm
d. Broad bizarre QRS, “sine wave”
e. Variety of arrhythmias including sinus bradycardia, sinus tachycardia, AVN blocks,
asystole
3. Determine the underlying cause
The most common cause for isolate hyperkalaemia is a spurious – e.g. haemolysed sample, K+
containing iv fluid. Must recheck with VBG immediately for rapid confirmation
The majority will be related to acute or chronic kidney disease
Aggravated by dehydration (e.g. gastroenteritis)
Aggravated by potassium sparing drugs (e.g. ACE inhibitor, Angiotensin Blocker,
spironolactone).
Aggravated by high dietary potassium, potassium supplements
Other causes include:
a. Transcellular shift – e.g. acidosis (eg DKA), Digoxin toxicity
b. Tissue destruction – e.g. GI bleed, rhabdomyolysis, tumour lysis
c. Rare renal causes – e.g. renal tubular acidosis, hyperaldosteronism
Initial Management of Acute Hyperkalaemia Pharmacy (District)
Southern DHB 24297 V4 Released 17/07/2019 Page 1 of 3
Master Copy is Electronic
Indications for emergency treatment of acute hyperkalaemia (any of):
K+ ≥7.0 mmol/l
K+ >6.0 mmol/l with generalised muscle weakness (e.g. unable to sit up, difficulty
breathing)
K+ >6.0 mmol/l with ECG changes – esp. wide QRS, junctional rhythm, bradycardia
Management Priorities in Emergency Treatment
NB: All initial treatment is temporising until the underlying cause is managed.
1. Stabilisation of myocardium
a. Calcium Gluconate 10% x 10ml iv bolus over 2-3 min. Provides cardio-protection
with onset 1-3 minutes and duration 30-60 min
i. Calcium Gluconate may be ineffective in liver failure
ii. Calcium Gluconate has 1/3 the elemental Ca as Calcium Chloride
b. Calcium Chloride 10% is alternative if Gluconate unavailable/unsuitable, very
irritating to peripheral veins
c. Calcium dose can be repeated 1-2x at 30 min intervals
2. Temporizing measures – shift potassium intracellularly
a. Insulin Actrapid (alternatives Novorapid, Humalog, Humulin R) 10 units iv bolus,
with 50mL 50% Dextrose iv bolus (can omit Dextrose if already hyperglycaemic,
>15 mmol/l). Shifts Potassium intracellularly, onset 10-20 min, duration 2-4 hours
b. Salbutamol 5mg nebuliser, 20mg initially (4 doses). Shifts potassium intracellularly,
onset 15 min, duration 1-2 hours.
3. Potassium removal
a. Haemodialysis. The only definitive way to remove potassium from the body.
Indicated if above measures fail, or severe hyperkalaemia that is unlikely to resolve
quickly, especially in anuric renal failure (eg dialysis patients). Discuss with senior
clinicians early.
b. Frusemide will enhance renal excretion of potassium. Only use if volume overloaded
and not in ESRF.
Initial Management of Acute Hyperkalaemia Pharmacy (District)
Southern DHB 24297 V4 Released 17/07/2019 Page 2 of 3
Master Copy is Electronic
Notes:
1. Discuss with a senior clinician as soon as possible.
2. Monitor serum potassium and glucose frequently (1-2 hourly initially). Monitor blood
glucose for up to 24 hours in those with CKD as insulin effects will last longer than
glucose.)
3. Ensure adequate hydration and blood pressure for optimal renal perfusion Monitor urine
output (must avoid IDC if possible).
4. Determine cause of hyperkalaemia, and treat, including withholding exacerbating drugs
(esp. ACEI/ARB, spironolactone, potassium sparing diuretics, digoxin, NSAID).
5. Insulin and Salbutamol both produce reduce serum K+ 0.5-1.0 mmol/l, and are synergistic.
Both can be repeated as/when the potassium begins to rise again. Salbutamol is less
effective in the face of Beta Blockade.
6. Other therapies:
a. Sodium Bicarbonate is not recommended except in cases of severe acidosis. Discuss
with Critical Care.
b. Resonium (Sodium Polystyrene Sulfonate) is designed to absorb potassium in the gut
and promote excretion. Its effect is small, variable, very slow (days) and associated
with bowel necrosis. It is not recommended in the acute setting.
7. Digoxin toxicity can increase serum potassium, and intracellular calcium. Avoid iv Calcium,
or use with caution by slow infusion (20 min in bag of 5% Dextrose). Consider Digoxin Fab
antidote (Digibind) after d/w Medical Team.
Bibliography
1. Hyperkalemia Revisited, Parham WA, Tex Heart Inst J. 2006; 33(1): 40–47.
2. Guidelines for the treatment of hyperkalaemia in adults. Guidelines and Audit
Implementation Network, Dept of Health Social Services and Public Safety. Northern
Ireland 2014.
3. Up to Date.
Dr Chris Johnstone, Clinical Director Emergency Medicine. August 2018
Initial Management of Acute Hyperkalaemia Pharmacy (District)
Southern DHB 24297 V4 Released 17/07/2019 Page 3 of 3
Master Copy is Electronic
You might also like
- HyperkalaemiaDocument6 pagesHyperkalaemiaSSNo ratings yet
- Ascites, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAscites, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Management of Potassium Disorders 17706 ArticleDocument4 pagesManagement of Potassium Disorders 17706 ArticlealeNo ratings yet
- Arritmias X HipercalemiaDocument9 pagesArritmias X Hipercalemiafh2301lrNo ratings yet
- Nephrology DR ZeinabDocument101 pagesNephrology DR ZeinabZeinab Muhammad100% (1)
- HyperkalemiaDocument16 pagesHyperkalemiaNader Smadi100% (5)
- Malignant Hyperthermia AlgorithmDocument1 pageMalignant Hyperthermia AlgorithmCesar David CaceresNo ratings yet
- Treatment and Prevention of Hyperkalemia in Adults - UpToDateDocument24 pagesTreatment and Prevention of Hyperkalemia in Adults - UpToDateJosé Abraham Amaya DuarteNo ratings yet
- Hyperkalemia MCQs & TreatmentDocument23 pagesHyperkalemia MCQs & TreatmentPrass Ekasetia PoetraNo ratings yet
- Electrolyte Disturbance-1Document22 pagesElectrolyte Disturbance-1Doaa Abd El-WahabNo ratings yet
- Drugs For The Treatment of Bipolar DisordersDocument9 pagesDrugs For The Treatment of Bipolar Disordersrichardmd2No ratings yet
- Acute Renal FailureDocument5 pagesAcute Renal FailureSalman KhanNo ratings yet
- Hiperkalemia PDFDocument26 pagesHiperkalemia PDFJesús Arnoldo Vargas OntiverosNo ratings yet
- Hypokalemia & Hyperkalemia: Mohamed Umar Amoud School of Medicine Nov 13, 2018Document30 pagesHypokalemia & Hyperkalemia: Mohamed Umar Amoud School of Medicine Nov 13, 2018Abdisalan hassanNo ratings yet
- ERC Guidelines 2005 Cardiac Arrest in Special CircunstancesDocument36 pagesERC Guidelines 2005 Cardiac Arrest in Special CircunstancesJoãoBrasil100% (2)
- Potassium DisturbancesDocument23 pagesPotassium DisturbancesThien Nhan MaiNo ratings yet
- Hyperkalaemia: See Also BackgroundDocument6 pagesHyperkalaemia: See Also BackgroundamaliaNo ratings yet
- AKI Final by DR SDocument37 pagesAKI Final by DR SsirawNo ratings yet
- Managing Hyperkalemia in CKD PatientsDocument8 pagesManaging Hyperkalemia in CKD PatientsPratik TripathiNo ratings yet
- Sec1 Clinical2 (ARF)Document44 pagesSec1 Clinical2 (ARF)ahmedmohamed01153159469No ratings yet
- Potassium Homeostasis and Hypokalemia Hyperkalemia ManagementDocument20 pagesPotassium Homeostasis and Hypokalemia Hyperkalemia Managementdudi herlambangNo ratings yet
- Important Complications of Chronic Kidney Disease: Continuing Medical EducationDocument4 pagesImportant Complications of Chronic Kidney Disease: Continuing Medical EducationAn-Nisa Khoirun UmmiNo ratings yet
- ElectrolyteDocument86 pagesElectrolyteFaryalBalochNo ratings yet
- Toxicology Lecture 6 Medical Toxicology (Chapter 4)Document22 pagesToxicology Lecture 6 Medical Toxicology (Chapter 4)Hasan iimanNo ratings yet
- Hiperk PDFDocument26 pagesHiperk PDFmasranraisaNo ratings yet
- Treatment and Prevention of Hyperkalemia in AdultsDocument34 pagesTreatment and Prevention of Hyperkalemia in Adultsr33realNo ratings yet
- ACUTE RENAL FAILURE DIAGNOSIS & MANAGEMENTDocument2 pagesACUTE RENAL FAILURE DIAGNOSIS & MANAGEMENTSetiya Dini LarasatiNo ratings yet
- Potassium Chloride GuidelinesDocument25 pagesPotassium Chloride GuidelinesYasser Gebril86% (7)
- Based On Your Possible Final Diagnosis, What Are The Treatment Plans For Our Patient?Document63 pagesBased On Your Possible Final Diagnosis, What Are The Treatment Plans For Our Patient?Kita kitaNo ratings yet
- Acute Chronic Renal FailureDocument43 pagesAcute Chronic Renal FailureHigh Education100% (1)
- Chronic Liver DiseaseDocument6 pagesChronic Liver DiseasepraveenbhavniNo ratings yet
- Guidelines For The Management Of: Kurdistan Higher Council For Medical SpecialtiesDocument6 pagesGuidelines For The Management Of: Kurdistan Higher Council For Medical SpecialtiesCik JaaNo ratings yet
- CKD Part 2Document26 pagesCKD Part 2subha95No ratings yet
- Surgery YbDocument67 pagesSurgery YbTamirat geletaNo ratings yet
- Resuscitation GuidelineDocument34 pagesResuscitation GuidelineSari FitrianingsihNo ratings yet
- Pembahasan To Online 5Document522 pagesPembahasan To Online 5vanadiel4No ratings yet
- Clinical Case Reports - 2020 - Schnaubelt - Hyperkalemia A Persisting Risk A Case Report and Update On Current ManagementDocument6 pagesClinical Case Reports - 2020 - Schnaubelt - Hyperkalemia A Persisting Risk A Case Report and Update On Current ManagementDesi MeliaNo ratings yet
- Body FluidDocument37 pagesBody FluidBir Mohammad SonetNo ratings yet
- Chronic Renal Failure: A. DefinitionsDocument28 pagesChronic Renal Failure: A. Definitionssharu4291No ratings yet
- Fluids After Cardiac SurgeryDocument42 pagesFluids After Cardiac SurgerySophie ShopeNo ratings yet
- Acute Kidney Injury (Aki) : MBCHB ViDocument25 pagesAcute Kidney Injury (Aki) : MBCHB ViENOCK BENDERENo ratings yet
- Hyper Calc Emi ADocument26 pagesHyper Calc Emi AAman Tayal0% (1)
- Diabetic KetoacidosisDocument10 pagesDiabetic Ketoacidosisagar agarNo ratings yet
- DrugsDocument116 pagesDrugsRyan FlahertyNo ratings yet
- Anaestetic Management of Liver DiseaseDocument86 pagesAnaestetic Management of Liver DiseaseVarun Reddy VNo ratings yet
- Management of HypokalemiaDocument6 pagesManagement of HypokalemiaEsraa Abu elelaNo ratings yet
- Congestive Cardiac Failure (1)Document27 pagesCongestive Cardiac Failure (1)Krupasagar Pn PalegarNo ratings yet
- SimulationDocument5 pagesSimulationJessFriend100% (1)
- HipokalemiaDocument46 pagesHipokalemiaFransiskus Samuel RenaldiNo ratings yet
- Acute Hyperkalaemia in AdultsDocument12 pagesAcute Hyperkalaemia in AdultsMeilina FitrianiNo ratings yet
- Acute Chronic Renal FailureDocument41 pagesAcute Chronic Renal FailuresgolbariNo ratings yet
- Ascites, SBP, Encephlopathy 2Document78 pagesAscites, SBP, Encephlopathy 2Rida AkramNo ratings yet
- Renal Emergency RevisiDocument103 pagesRenal Emergency Revisidesy f sarahNo ratings yet
- Important Complications of Chronic Kidney Disease PDFDocument4 pagesImportant Complications of Chronic Kidney Disease PDFDrBishnu Prasad MahalaNo ratings yet
- Acute Metabolic Complications of Diabetes MellitusDocument54 pagesAcute Metabolic Complications of Diabetes MellitusPrincewill SeiyefaNo ratings yet
- Hippo EM Board Review - Electrolyte Emergencies Written SummaryDocument5 pagesHippo EM Board Review - Electrolyte Emergencies Written SummaryMichael IvanNo ratings yet
- Diabetic Ketoacidosis: Medical EmergencyDocument18 pagesDiabetic Ketoacidosis: Medical EmergencyKirsten Padilla ChuaNo ratings yet
- Hyperkalemia: Samir El AnsaryDocument43 pagesHyperkalemia: Samir El AnsaryStrept PneumoniaNo ratings yet
- Keith Hopcroft - Instant Wisdom For GPs - Pearls From All The Specialities-CRC Press (2024)Document274 pagesKeith Hopcroft - Instant Wisdom For GPs - Pearls From All The Specialities-CRC Press (2024)Adil Abdul SalamNo ratings yet
- Constipation Formulary (Otago) : DiagnosisDocument4 pagesConstipation Formulary (Otago) : DiagnosisMiguel SanJuanNo ratings yet
- QIToolkit FlowchartDocument4 pagesQIToolkit FlowchartmammutbalajiNo ratings yet
- Developing PGY2 Teaching ProgrammeDocument1 pageDeveloping PGY2 Teaching ProgrammeMiguel SanJuanNo ratings yet
- Hypokalaemia Formulary (Otago)Document1 pageHypokalaemia Formulary (Otago)Miguel SanJuanNo ratings yet
- Remove External Drain SafelyDocument4 pagesRemove External Drain SafelyDot DitNo ratings yet
- Orthopaedics Pearls PDFDocument375 pagesOrthopaedics Pearls PDFMiguel SanJuanNo ratings yet
- Patterns of Fat StrandingDocument16 pagesPatterns of Fat StrandingMiguel SanJuanNo ratings yet
- Orthopaedics Pearls PDFDocument375 pagesOrthopaedics Pearls PDFMiguel SanJuanNo ratings yet
- Guidance On Eligibility 2020Document2 pagesGuidance On Eligibility 2020Miguel SanJuanNo ratings yet
- Blood Draw, Appropriate TubesDocument61 pagesBlood Draw, Appropriate TubesMiguel SanJuanNo ratings yet
- 16 General Principles For The Management of Ruptured and Unruptured Intracranial AneurysmsDocument12 pages16 General Principles For The Management of Ruptured and Unruptured Intracranial AneurysmsMiguel SanJuan100% (1)
- 33 Spinal Cord InjuryDocument17 pages33 Spinal Cord InjuryMiguel SanJuanNo ratings yet
- 25 Closed Head InjuryDocument28 pages25 Closed Head InjuryMiguel SanJuanNo ratings yet
- 20 Vascular Malformations (Arteriovenous Malformations and Dural Arteriovenous Fistulas)Document14 pages20 Vascular Malformations (Arteriovenous Malformations and Dural Arteriovenous Fistulas)Miguel SanJuanNo ratings yet
- 17 Anterior Circulation AneurysmsDocument19 pages17 Anterior Circulation AneurysmsMiguel SanJuanNo ratings yet
- 15 Medical and Surgical Treatment of Cerebrovascular Occlusive DiseaseDocument16 pages15 Medical and Surgical Treatment of Cerebrovascular Occlusive DiseaseMiguel SanJuanNo ratings yet
- Find Biomime Morph - A Drug Eluting Stent Designed by Meril LifeDocument2 pagesFind Biomime Morph - A Drug Eluting Stent Designed by Meril LifeAnkit ShirkeNo ratings yet
- Jambi Cardiology Update WorkshopDocument3 pagesJambi Cardiology Update WorkshopFahrurrozi SyarifNo ratings yet
- ACLS PharmacologyDocument6 pagesACLS PharmacologyEunice Angela Fulgueras80% (5)
- Antiarrhythmic Drugs Classification and MechanismsDocument56 pagesAntiarrhythmic Drugs Classification and MechanismsHassan MohammadNo ratings yet
- Nephrology Certification Examination Blueprint - American Board of Internal MedicineDocument4 pagesNephrology Certification Examination Blueprint - American Board of Internal MedicineabimorgNo ratings yet
- Renal Disease: Acute Kidney Injury (AKI)Document5 pagesRenal Disease: Acute Kidney Injury (AKI)api-142637023No ratings yet
- Comprehensive Clinical Nephrology 6Th Edition John Feehally full chapterDocument51 pagesComprehensive Clinical Nephrology 6Th Edition John Feehally full chaptercynthia.casey475100% (13)
- 10 1016@j Biombioe 2020 105881Document1 page10 1016@j Biombioe 2020 105881Alex SmithNo ratings yet
- Resident/Fellow Member Application: CodeDocument2 pagesResident/Fellow Member Application: CodeKavya ShreeNo ratings yet
- Acute Decompensated Heart Failure Check for UnderstandingDocument3 pagesAcute Decompensated Heart Failure Check for UnderstandingSistine Rose LabajoNo ratings yet
- UHN Nephrology Manual July 2017Document215 pagesUHN Nephrology Manual July 2017be a doctor for you Medical studentNo ratings yet
- Acyanitic DefectsDocument9 pagesAcyanitic DefectsHalla BennaaNo ratings yet
- Stress Echo Cardiography (63328 - 1)Document18 pagesStress Echo Cardiography (63328 - 1)Griselda Maria Pinto SanchezNo ratings yet
- Kidney Function Test: What a Creatinine Test RevealsDocument3 pagesKidney Function Test: What a Creatinine Test RevealsElixirNo ratings yet
- Growing Burden of CKD in PakistanDocument14 pagesGrowing Burden of CKD in PakistanHamza RealionNo ratings yet
- Sindrom Nefrotik PerioperatifDocument13 pagesSindrom Nefrotik Perioperatiffauzi agung NugrohoNo ratings yet
- Code Blue Training and WorkshopDocument15 pagesCode Blue Training and WorkshopeychceeNo ratings yet
- Test Bank For Human Diseases 8th Edition ZelmanDocument22 pagesTest Bank For Human Diseases 8th Edition Zelmandenisedanielsbkgqyzmtr100% (29)
- Pulsenotes - Chronic Kidney Disease NotesDocument12 pagesPulsenotes - Chronic Kidney Disease NotesElay PedrosoNo ratings yet
- Hypertrophic CardiomyopathyDocument37 pagesHypertrophic CardiomyopathyMarko Vukovic100% (1)
- Atrial FlutterDocument38 pagesAtrial FlutterLady AngodNo ratings yet
- 12 Lead STEMI MimicsDocument22 pages12 Lead STEMI MimicscornondaNo ratings yet
- Cardiac ArrestDocument19 pagesCardiac ArrestHaimelien De LimosNo ratings yet
- Coronary Artery Disease Guide: Causes, Symptoms, Diagnosis & TreatmentDocument4 pagesCoronary Artery Disease Guide: Causes, Symptoms, Diagnosis & TreatmentViktoria Leeahna LehNo ratings yet
- Lecture Notes On CardiologyDocument31 pagesLecture Notes On CardiologyambiskuysNo ratings yet
- Junior Clerkship Med BooklistDocument3 pagesJunior Clerkship Med BooklistwisgeorgekwokNo ratings yet
- Acs PPT Final 6-14-10Document66 pagesAcs PPT Final 6-14-10Yoseph Arif PutraNo ratings yet
- Congenital Cardiac Defects PPT PDF 211Document47 pagesCongenital Cardiac Defects PPT PDF 211Ahmed YasserNo ratings yet
- Prinsip Dasar Dan Interpretasi EKGDocument44 pagesPrinsip Dasar Dan Interpretasi EKGFiraNo ratings yet
- Contrast NephRopathy GuidelinesDocument3 pagesContrast NephRopathy GuidelinesStacey WoodsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (20)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)