Professional Documents
Culture Documents
(2013) Uncomplicated Urinary Tract Infection
(2013) Uncomplicated Urinary Tract Infection
Uploaded by
Wilsonne Chua0 ratings0% found this document useful (0 votes)
7 views12 pagesOriginal Title
[2013] Uncomplicated Urinary Tract Infection
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views12 pages(2013) Uncomplicated Urinary Tract Infection
(2013) Uncomplicated Urinary Tract Infection
Uploaded by
Wilsonne ChuaCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 12
~ Philippine Clinical Practice
Guidelines on the Diagnosis and
Management of Urinary Tract
Infections in Adults
2013 Update
Uncomplicated Urinary Tract Infection
Acute Uncomplicated Cystitis in Women - Diagnosis
Diagnosis of AUC
> Clinically, AUC is suspected in premenopausal non-pregnant women
presenting with acute onset of dysuria, frequency, urgency,
hematuria; and without vaginal discharge.
> Urinalysis is not necessary to confirm the diagnosis of AUC in women
presenting with one or more of the above symptoms of urinary tract
infection (UTI) in the absence of vaginal discharge and complicating
conditions enumerated in Table 1
Women presenting with urinary symptoms plus vaginal discharge
should undergo further evaluation to rule out or rule in other disease
conditions.
> Conditions that define complicated urinary tract infection (CUTI) must be
absent as obtained on history taking.
and gross
Strong recommendation, High quality of evidence
Table 1. Conditions that define complicated UTI
+ Presence of an indwelling urinary catheter or intermittent catheterization
+ Incomplete emptying of the bladder with >100 ml retained urine post-
voiding
+ Impaired voiding due to neurogenic bladder, cystocoele
+ Obstructive uropathy due to bladder outlet obstruction, calculus,
urethral or ureteric strictures, tumors
+ Vesicoureteral reflux & other urologic abnormalities including surgically
created abnormalities
+ Chemical or radiation injuries of the uroepithelium
+ Peri- or post-operative UT!
+ Azotemia due to intrinsic renal disease
+ Renal transplantation
+ Diabetes mellitus
+ Immunosuppressive conditions — e.g, febrile neutropenia, HIV-AIOS
UTI caused by unusual pathogens (M. tuberculosis, Candida spp.)
+ UTI caused by multi-drug resistant organisms (MDROs)
* UT! in males except in young males presenting exclusively with lower
UT! symptoms
+ Urosepsis
* Empiric antibiotic treatment is the most cost-effective approach in the
management of AUC.
* Pre-treatment urine culture and sensitivity is NOT recommended
* Sfandard urine microscopy and dipstick leukocyte esterase (LE) and
nitrite tests are not prerequisites for treatment
Strong recommendation, High quality of evidence
> Antibiotics recommended for use in AUC are presented in Table 2.
Efficacy in terms of clinical cure, cost effectiveness, safety and tolerability
were considered in the choice of antibiotics. In addition, the propensity to
cause collateral damage and local susceptibility rates were given greater
weights in the choice of antibiotic recommendations.
Comment: Collateral damage is the “ecological adverse effects” of antibiotic
therapy. Such adverse effects include selection of drug-resistant organisms
‘and colonization or infection with multi-drug resistant organisms
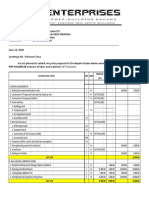
Antibiotics for acute uncomplicated cystitis
Primary Nitrofurantoin monohydrate’ | 100 mg BID for 5 days per orem (PO)
macrocrystals (not sold locally)
TNirofurantoin macrocrystals | 100 mg QIO for § days PO
Fosfomycin rometamol 3.g single dose PO
‘Alternative | Pivmecilinam (not sold ocally) | 400 mg BID for 3-7 days PO
‘Ofloxacin 200 mg BID for 3 days PO
Ciprofloxacin 250 mg BID for 3 days PO
Ciprofloxacin extended release _| 500 mg OD for 3 days PO.
Levofloxacin 250 mg OD for 3 days PO.
Norfloxacin 400 mg BID for 3 days PO
Amoxiilin-lavulanate 625 mg BID for7 days PO
Cefuroxime axeti 250 mg BID for 7 days PO
Cefacior 500 mg TID for? days PO 2]
Cetxime 200 mg BID for 7 days PO
Cefpodoxime proxeti 100 mg BID for 7 days PO
Cettbuten 200 mg BID for 7 days PO
‘ONLY if with | Trimethoprim-sulfamethoxazole | 160/800 mg BID for 3 days PO
proven (TMP-SMX)
susceptibility
> ‘Ampicilin or amoxicilin should NOT be used for empirical treatment
given the relatively poor efficacy and the very high prevalence of
antimicrobial resistance to these agents worldwide
Strong recommendation, High quality of evidence
» Trimethoprim-sulfamethoxazole 800/160 m:
be used ONLY for culture-proven suscepti hoger
eptible uropatt
high prevalence of local resistance and high failure rates, eae
Strong recommendation, High quality of evidence
19 BID for three days should
monohydrate/macrocrystals (100 mg twice daily for five
ays) is recommended as the frst line treatment for acute uncomplicated
Gyaits due 10 is high efficacy, minimal resistance, minimal adverse
Sects, low propensity for collateral damage, and reasonable cos
However, the nitrofurantoin monohydrate/macrocrystal formulation is not
locally available. Thus, the locally available nitrofurantoin macrocrystal
formulation 100 mg is recommended, but it should be given four times a
day for five days. .
‘Strong recommendation, High quality of evidence
> Fosfomycin (3 9 in a single dose) is also recommended for AUC due to its
‘efficacy, convenience of a single dose, low propensity for collateral
damage, good activity against multidrug-resistant uropathogens and
minimal adverse effects. However, there are no local resistance data to
date.
Strong recommendation, High quality of evidence
> Pivmecillinam (400 mg BID for three to seven days) can be used in areas
where it is available, as it has reasonable treatment efficacy. However,
it is not currently available in the country. Local resistance data is also
absent
‘Strong recommendation, High quality of evidence
Quinolones should NOT be used as a first line drug for acute
uncomplicated cystitis despite their efficacy due to its high propensity for
collateral damage.
‘Strong recommendation, High quality of evidence
> Beta-lactam agents, including amoxicilin-clavulanate, cefaclor,cefdinir,
i |, ceftibuten and cefuroxime are appropriate
alternative choices for therapy when the primary recommended agents
cannot be used.
‘Strong recommendation, High quality of evidence
Duration of treatment for elderly women with AUC
> Inclherwioe healthy siery wornen with AUC, the recommended duration
Gf teatment for elderly women is the same as the general population
Strong recommendation, High quality of evidence
2 ction fo cs : ;
‘tients whose symptoms worsen or do not improve after completion of
\teaiment should have a urine culture done, and, the antibiotic should be
> Panencaly changed pending result of sensitivity testing.
ae ee to resolve after treatment should be
‘Strong ‘
recommendation, Low quality of evidence
i: Urine culture and urinalysis in patients whose
S2mpletely resolved are NOT recommended as ft dOes
RnR CEC Ba UGS ee UEC
Diagnosis
> Acute uncomplicated pyelonephritis is suspected in otherwise healthy
women with no clinical or historical evidence of anatomic or functional
Urologic abnormalities, who present with the classic syndrome of fever
(T 2 38°C), chills, flank pain, costovertebral angle tenderness, nausea
and vomiting, with or without signs and symptoms of lower urinary tract
infection (UTI).
> Laboratory findings include pyuria (= 5 WBC/HPF of centrifuged urine) on
urinalysis and bacteriuria with counts of 210,000 CFU of uropathogen/ml.
on urine culture
Strong recommendation, Moderate quality of evidence
Pre-tre tests
> Urinalysis and Gram stain are recommended. Urine culture and sensitivity
test should also be performed routinely to facilitate cost-effective use of
antimicrobial agents and because of the potential for serious sequelae if
‘an inappropriate antimicrobial agent is used
Strong recommendation, Moderate quality of evidence
> Blood cultures are NOT routinely recommended except in patients with
signs of sepsis.
‘Strong recommendation, High quality of evidence
Table 3. Signs of sepsis
‘Any two of the following
+ Temperature >38 °C or <36°C
+ Leukopenia (WBC < 4,000) or leucocytosis (WBC > 12,000)
«Tachycardia (HR> 90 beats/min)
+ Tachpynea (RR> 20/min or PaCO,< 32 mmHg)
+ Hypotension (SBP < 90 mmHg or > 40 mmHg drop from baseline)
Biomarkers
Biomarkers (procalcitonin, mid-regional pro-atrial natriuretic peptide and
C-reactive protein) are NOT recommended since they are not clinically
useful in determining the need for admission or in predicting adverse
‘outcomes such as recurrence and prolonged hospitalization.
Strong recommendation, Low quality of evidence
The following are considered indications for admission:
> Inability to maintain oral hydration or take medications
> Concern about compliance
» Presence of possible complicating conditions
>
> Severe il
ee foe with high fever, severe pain, marked debility and signs of
‘Strong recommendation, Moderate quality of evidence
i al
Several regimens found to be effective in AUP are listed in Table 2. Efficacy,
cost effectiveness, safety, tolerability, local susceptibility, and propensity for
collateral damage were considered in the choice of the antibiotic.
Table 4, Empiric treatment regimens for uncomplicated acute pyelonephritis
ORAL
Primary | Ciprofoxacin '500 mg BID for 7-10 days
Ciprofoxacin extended release 1000 mg OD for7 days
Levofloxacin 250 mg OD for 7-10 days
750 mg OD for 5 days
Oforacin 400 mg BID for 14 days
Mtemaive | Cefxime 400 mg OD for 14 days
Ceftbuten 400 ig OD for 14 days
Cefuroxime axetil 500 mg BID for 14 days
(Co-amoxciav when GS shows gram-positive orgs) | 625 mg TID for 14 days
PARENTERAL (given until patient is afebrile)
Primary | Ceftiaxone 129924 hous
Cipooxacn 400mg q Whours
Levotoxacn 250-750 mg q 24 hours
Ofoxacn 200-400 mg q 12 hous
‘Amikacin 15 malig BW 9 24 hours
Gentamicin + ampiiin 3-5 mgikg BW q 24 hours
‘Atematve | Ampicilin-sutactam (when GS shows gram- | 159q6hous
postive orgs)
Reserved for|Ertapenem jf ESBL prevalence > 10%) 19424 hous
MOROs _| Piperacilivtazobactam 226-459 96-8 hous
» The aminopenicilins (ampicillin or amoxicillin) and first generation
cephalosporins are NOT recommended because of the high prevalence
of resistance and increased recurrence rates in patients given these
betatactams,
Strong recommendation, Moderate quality of evidence
* Because of high resistance rales to TMP-SMX, this drug is NOT
atria for empiric treatment but it can be used when the organism
‘Susceptible on urine Culture and Sensitivity.
Strong recommendation, Moderate quality of evidence
> Quinolones are recommended as the first line treatment for acute
uncomplicated pyelonephritis not requiring hospital admission.
‘Strong recommendation, High quality of evidence
> Inpatients not requiring hospital admission, an initial single IV/IM dose of
ceftriaxone or aminoglycoside may be considered followed by any of the
oral antibiotics recommended in Table 4.
‘Strong recommendation, Moderate quality of evidence
» For patients with acute uncomplicated pyelonephritis requiring
hospitalization, ceftriaxone, fluoroquinolones or aminoglycosides are
recommended as empiric first-line treatment.
Strong recommendation, Moderate quality of evidence
> Intravenous antibiotics can be shifted to any of the listed oral antibiotics
‘once the patient is afebrile and can tolerate oral drugs. The choice of
continued antibiotic therapy should be guided by the urine culture and
sensitivity results once available.
Strong recommendation, Moderate quality of evidence
» For suspected enterococcal infection, ampicillin may be combined with
an aminoglycoside.
Weak recommendation, Low quality of evidence
» Carbapenems and piperacillin-tazobactam should be reserved for
acute pyelonephritis caused by multi-drug resistant organisms that are
susceptible to either drug.
‘Strong recommendation, Moderate quality of evidence
Role of radiologic imaging
» Routine urologic evaluation and routine use of imaging procedures are
NOT recommended.
Strong recommendation, Moderate quality of evidence
> Consider early radiologic evaluation if the patient has a history of
Urolithiasis, urine pH 2 7.0 or renal insufficiency,
‘Strong recommendation, Moderate quality of evidence
> Consider radiologic evaluation if the patient remains febrile within 72
hours of treatment or if symptoms recur to rule out the presence of
Nephrolithiasis, urinary tract obstruction, renal or perinephric abscesses
or other complications of pyelonephritis.
Weak recommendation, Low quality of evidence
> Obtain urologic consultation if radiologic workup shows abnormalities,
Weak recommendation, Low quality of evidence
> In patients who are clinically responding to therapy (usually apparent in
<72 hours after initiation of treatment), a follow-up urine culture is NOT
necessary.
Weak recommendation, Low quality of evidence
> Routine post-treatment cultures in patients who are clinically improved
are also not recommended.
Weak recommendation, Low quality of evidence
> In women whose symptoms do not improve during therapy and in those
Whose symptoms recur after treatment, a repeat urine culture and
sensitivity test should be performed.
Weak recommendation, Low quality of evidence
Recurrence of symptoms
» Recurrence of symptoms requires antibiotic treatment based on urine
culture and sensitivity test results in addition to assessing for underlying
genitourologic abnormality
Weak recommendation, Low quality of evidence
> The duration of re-treatment in the absence of a urologic abnormality is
‘two weeks.
Weak recommendation, Low quality of evidence
* For patients whose symptoms recur and whose culture shows the same
organism as the initial infecting organism, a four- to six- week regimen is
recommended,
Weak recommendation, Low quality of evidence
it siecle
Evaluating a Woman with Symptoms of Acute
eer mera occa)
Algorithm 1
Do urinalysis, urine culture to establish diagnosis
annie Ppa nantes
fo [Consider Acute Uncomplicated Pyelonephritis
YEG | do urinalysis, urine culture to establish diagnosis
Consider empiri treatment
see Secton an Acute Uncomplicated ?ylonephris
Low to intermediate probability of UT (-20%)
Consider Sensally Transmitted Infections
Do pelvic examination linclusing cervical culture when
Appropriate), urinalysis, urine, culture, urine Chama
roestablish diagnosis
See Section on Acute Uncomplicated Cysts
with leat history of > 2
syptorsof UTI igh probability of AUC (-30%)
cate onset of dysura, start empiric treatment without urinalysis urine culture
frequency, wreendy, See Section on Acute Uncomplicated Cystitis
hematuria?
Perform dipstick urinalysis
WOR Her povsniny rane aon)
Sarcempiic eatment without wine cure
See Secon on heute Uncomplated Css
Low to intermediate probabilty of UT (20%) “ys, frequency, rgency
Consider urine culture o close cnc follow-up and pelvic hematuria, discomfort in tower
‘examination including cervical cuitures and radiologic ae
imaging when approprate
See section on Uncomplicated urinary Trac Infection
Healthy non-pregnant woman
with dysuria, frequency,
urgency or hematuria
Symptoms
resolved
cute uncomplica'
Tay
Healthy non-pregnant woman
with acute uncomplicated
pyelonephritis
Septic, too
ill or likely
to be non-
adherent?
‘Symptoms
improved
on Day 3?
rable 5. Strength of Recommendation and Quality of Evidence
toy inition
Strong Clear desirable or undesirable effects
Weak Desirable and undesirable effects closely balanced or uncertain
Quality of Evidence
High Consistent evidence from well-performed RCTs or exceptionally
strong evidence from unbiased observational studies
Moderato Evidence from RCTs with important limitations or moderately
strong evidence from unbiased observational studies
Low Evidence for. one critical outcome from observational studies,
{rom RCTS with serious flaws or from indirect evidence
Very Low Evidence for 2 one critical oulcome from unsystematic clinical
‘observation or very indirect evidence
Sources.
Task Force on Urinary Tract Infections, Philippine Practice Guideline Group
Infectious Disease. Philippine Clinical Practice Guidelines on the Diagnosis
and Management of Urinary Tract Infections in Adults 2013 Update. Quezon
City, Philippines: PPGG-ID Philippine Society for Microbiology and Infectious
Disease, 2013,
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P,
Schunemann HJ, GRADE Working Group. GRADE: an emerging consensus
on rating quality of evidence and strength of recommendations. BMJ 2008;
336: 924-926
Guyatt GH, Oxman AD, Kunz R, Falck-Ytter Y, Vist GE, Liberati A
Schiinemann HJ and for the GRADE Working Group. Going from evidence to
recommendations. BMJ 2008; 336: 1049-51
Philippine Practice Guidelines Group: Task Force on Urinary Tract Infections
Chair: Mediadora C. Saniel, MD
Co Chair: Marissa M. Alejandria, MD
Head, Uncomplicated UTI Cluster: Thea Chua Patino, MD
Evalyn A. Roxas , MD
Members: Karen Marie R. Gregorio, MD
Annabelle M-Laranio, MD
Kathryn U. Roa,
Femarel Paoio . Sumong. MD
‘Anna Marie S. Velasco.
Rosally P. Zamora, MD <
Grace Kathleen Serrano,
Richole Out NO eae
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Arterial Blood Gas: IM 2013 (AVM)Document66 pagesArterial Blood Gas: IM 2013 (AVM)Wilsonne ChuaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Guidelines On: Acute Kidney InjuryDocument52 pagesGuidelines On: Acute Kidney InjuryWilsonne ChuaNo ratings yet
- (2009) Gout PDFDocument11 pages(2009) Gout PDFWilsonne ChuaNo ratings yet
- Streptococcus Pneumoniae Serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14Document43 pagesStreptococcus Pneumoniae Serotypes 1, 3, 4, 5, 6A, 6B, 7F, 9V, 14Wilsonne ChuaNo ratings yet
- Philippine College of Chest Physicians: Media Kit For PneumoniaDocument4 pagesPhilippine College of Chest Physicians: Media Kit For PneumoniaWilsonne ChuaNo ratings yet
- TestDocument2 pagesTestWilsonne ChuaNo ratings yet
- Wilsonne Chua Home RepairDocument2 pagesWilsonne Chua Home RepairWilsonne ChuaNo ratings yet