Professional Documents
Culture Documents
Common Electrolytes - Imbalances, Normal Ranges and Disturbances
Uploaded by
Brent KoboroffCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Common Electrolytes - Imbalances, Normal Ranges and Disturbances
Uploaded by
Brent KoboroffCopyright:
Available Formats
This CPD site is for Australian health professionals
! Latest CPD " Learning Hubs # Online C
Online CPD · Articles · Electrolyte Imbalance + Normal Ranges and D
Electrolyte Imbalance + Normal
Ranges and Disturbances for
Common Electrolytes
CPD 16m Published: 16 May 2018
Electrolyte imbalances can occur due to
hundreds of factors, none of which line up
in neat, tidy queues.
Look at a few of the most common examples:
Patients suffering from congestive heart failure often
end up as rebound hospitalisations due to abnormal
sodium and potassium levels.
A grandmother with diabetes or hypertension may
eventually find herself on the business end of a
calcium or magnesium imbalance.
The toddler with explosive diarrhoea and the elite
Australian athlete, otherwise wildly unalike, both
routinely find themselves on the business end of
electrolyte imbalances.
A proper understanding of these imbalances is
essential for current management and future
prevention.
5:32
Facts and Figures
Electrolyte imbalances occur across many different
diagnostic categories.
In Australia, harsh summer environmental exposure,
with resulting dehydration, is just one example of a
potential root cause1; sadly, more Australians are
killed from the ill-effects of heatwaves than all other
natural hazards, combined.2
This is just potential cause, however. There are
hundreds of other root causes for fluid and
electrolyte imbalances, including:
In children: a leading cause of dehydration and
electrolyte imbalance in children is acute
gastroenteritis, a disorder which can be
effectively treated with oral rehydration.3
In the older adult: one of the primary reasons
older populations are at an elevated risk of
dehydration and electrolyte imbalance is a
diminished thirst response.4
In the athlete: Electrolyte imbalances during
exercise come from multiple sources.
Strangely, the muscles doing work do not lose
water content during exercise; rather, the
muscles dehydrate during the immediate post-
exercise recovery period, presumably in an
effort to restore plasma volume and to stabilise
the cardiovascular system.5,6
What is an Electrolyte
Imbalance?
Put simply, electrolytes are naturally occurring
minerals with an electric charge.
They exist in the human body and they are also
present in food and fluids we ingest every day.
Potassium, magnesium, and sodium are several
commonly known electrolytes, but they are not
alone; calcium and phosphate also play critical roles.
These electrolytes serve crucial functions in the
body such as keeping water in balance, regulating
the body’s base pH levels, and moving nutrients and
waste to and from cells.7
Electrolyte Imbalance
Symptoms
Electrolyte imbalance can be a marker of many
common diseases and illnesses.
Assessing a patient for electrolyte imbalance can
give practitioners an insight into the homeostasis of
the body and can serve as a marker or proxy for the
presence of other illnesses.
Practitioners can use physical examination, ECGs,
serum electrolyte levels and pathologic signs as
methods to assess for electrolyte imbalance.
Certain symptoms can even point to a specific
electrolyte that is out of balance in a patient. For
example, confusion is a common symptom of
hypocalcaemia.8
By using the aforementioned examination
techniques, practitioners can pinpoint which
electrolytes are out of balance and thus craft a more
effective treatment plan for the patient.
There are many different symptoms of electrolyte
imbalance that can present themselves in a patient.
Some Common Electrolyte
Imbalance Symptoms are:8
Dyspnoea
Fever
Systemic deterioration
Confusion
Oedema
Rales
Tachycardia
Atrial fibrillation
Vomiting
Abdominal pain
What Causes an Electrolyte
Imbalance?
Dehydration does not occur at some standardised
setpoint; it is caused by consuming too little fluid for
the present needs of the body.
This can happen by either decreased consumption
or outside factors that cause the body to require
more water than normal.
When the body becomes dehydrated, certain
symptoms can arise such as dry mouth or increased
thirst. However, these are not universal indicators of
dehydration. In fact, they may not be clinically useful
for diagnosing dehydration.9
Whenever the body is overhydrated or
underhydrated – or when the body’s filtration
systems do not operate normally – electrolytes no
longer function as they should.
Abnormal electrolyte levels can occur anytime the
body’s fluid levels fluctuate outside of norms such
as after serious burns, vomiting, diarrhoea, and
excessive sweating.
Infrequently, overhydration can also result in serious
repercussions. Certain medicines and dysfunctions
of the liver and kidneys can also throw the body’s
electrolytes out of normal range.
Electrolyte Imbalance Risk
Factors
While absolutely anyone can develop an electrolyte
disorder, the older population are at an increased
risk.
Some factors that can increase the risk of an
electrolyte imbalance in older populations include:10
Diabetes
Hypertension
Use of diuretics (which promote fluid excretion
by the kidneys)
Within these risk factors there is increased risk to
those who use certain combinations of diuretics and
to those with diabetes. Patients who use both
thiazides and benzodiazepines are associated with
higher rates of hyponatremia, which in turn, is
associated with a higher mortality risk.10
The use of angiotensin-converting enzyme inhibitors
(ACE inhibitors), potassium and calcium
supplements and certain hormones, which are
classified as ‘potassium-sparing’, can also lead to
imbalances.
Other conditions that can increase the risk of an
electrolyte disorder include:
Significant burns
Significant trauma (such as broken bones)
Congestive heart failure
Abuse of alcohol (especially long-term abuse)
Kidney disorders
Diarrhoea or vomiting
Heat exhaustion
Eating disorders (such as anorexia or bulimia)
Thyroid, parathyroid and adrenal gland
disorders (such as Addison’s disease)
Diagnosing an Electrolyte
Imbalance
There are several types of tests that can be used to
diagnose electrolyte imbalance.
Each type of test has its own pros and cons for
detecting various types of imbalances. Here are just
a few of the ways practitioners test for electrolyte
dysfunction:7
The Anion Gap Blood Test is a blood test that
analyses the levels of acid in the blood. This
can indicate an electrolyte imbalance, as one
of the functions of electrolytes is balancing the
pH of the blood.
Carbon Dioxide Blood Tests are used to
measure CO2 levels in the blood. CO2 in the
blood is often in the form of an electrolyte
called bicarbonate.
Chloride Tests measure the levels of chloride,
another electrolyte, in the blood.
Sodium Blood Tests analyse sodium levels in
the blood, another common portion of an
electrolyte blood panel.
Electrolyte Imbalance
Treatment
Individuals who experience serious symptoms,
tachycardia, mental confusion, sunken eyes,
reduced elasticity of the skin and/or a loss of
consciousness need immediate medical attention.
Individuals who dehydrate through exercise or
activity can typically look to the electrolyte
restoration possibilities of sports drinks. An excellent
guide to the use of such sports drinks was put out
by Australia’s AIS Sports Supplement Framework, an
initiative of AIS Sports Nutrition.6
Between these two extremes is a vast middle ground
with some patients requiring rapid – though not
emergency – medical assistance, and some patients
self-correcting without ever knowing anything more
than that they ‘felt a bit off’.
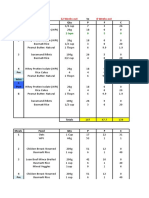
Normal Ranges and
Disturbances of Common
Electrolytes
Although there are many trace elements that keep
the body healthy, several important electrolytes can
severely affect patients when they are either too
high (hyper…) or too low (hypo…).
Understanding what each electrolyte does, what
happens when there isn’t enough of one or too
much of another, is essential knowledge for nurses
and can help guide electrolyte therapy.
Sodium
Sodium, or Na, is one of the most important
electrolytes in the body and is responsible for a
number of important functions, mostly related to
fluid and water regulation. The normal accepted
range for sodium is 134 to 145 mEq/L.
Hyponatraemia is considered to be a serum sodium
below 134 mEq/L. A common cause of
hyponatraemia is water retention due to cardiac or
renal or hepatic failure.
Other causes of hyponatraemia include some
medicines, psychogenic polydipsia (excessive water
intake) and syndrome of inappropriate ADH
(antidiuretic hormone) secretion, and chronic or
severe vomiting and diarrhoea.
Common symptoms of hyponatraemia include
confusion, agitation, nausea and vomiting, muscle
weakness, spasms or cramps.
Hypernatraemia is defined as a serum sodium
greater than 145 mEq/L.
Causes of hypernatraemia can be thought of simply
as anything that leads to excessive water loss or salt
gain. For example, water depletion or dehydration
may be caused by vomiting or diarrhoea.
Excessive ingestion of sodium is rare, but the
administration of infusions containing sodium such
as sodium chloride or sodium bicarbonate may lead
to hypernatraemia.
Clinical features of hypernatraemia may include
fever, irritability, drowsiness, irritability, lethargy and
confusion.
Potassium
Potassium, or K, is responsible for the functioning of
excitable tissues such as skeletal and cardiac
muscle and nerves. The normal range for
potassium is 3.5 to 5.0 mmol/L.
Hypokalaemia is defined as a serum potassium less
than 3.5 mmol/L. A low serum potassium may be
caused by decreased oral intake, increased renal or
gastrointestinal loss of potassium, or a shift of
potassium within the body’s fluid compartments
(from outside the cell where it should be, to inside
the cell).
Common clinical features of hypokalaemia range
from muscle weakness and ileus (lack of peristalsis),
to serious cardiac arrhythmias such as ventricular
tachycardias.
Hyperkalaemia, a serum potassium greater than 5.0
mmol/L, may be caused by excessive intake, tissue
damage from burns or trauma, medicines such as
potassium sparing diuretics, and most commonly,
due to renal failure.
Clinical signs of hyperkalaemia include muscle
weakness, hypotension, bradycardia and loss of
cardiac output, and ECG changes may include
peaked T waves and flattened P waves.
Magnesium
Magnesium, or Mg, is another element that has a
strong effect on muscle contractions. The normal
plasma range for magnesium is 0.70 to 0.95
mmol/L.
Hypomagnesaemia, or a decreased plasma
magnesium level, may be caused by decreased
intake or increased loss of magnesium. Clinical signs
include confusion, irritability, delirium, muscle
tremors and tachyarrhythmias.
Hypermagnesaemia is when the level of magnesium
in the blood is above the normal range. Fortunately,
this is uncommon. Symptoms include poor reflexes,
low blood pressure, respiratory depression, and
cardiac arrest. This is usually caused by the
excessive administration of magnesium and lithium
therapy, often in the presence of renal failure.
Calcium
Calcium, or Ca, is an important element in the body
as it helps to control nerve impulses, muscle
contractions and has a role in clotting. The serum
calcium range should be between 2.20 to 2.55
mmol/L when normal.
Hypocalcaemia, the presence of low serum calcium
levels in the blood, is relatively rare because the
bones always act as a reservoir for this electrolyte.
However, parathyroid disease, vitamin D deficiency,
septic shock and acute pancreatitis can cause this
problem. Some symptoms include tetany
(involuntary muscle contraction), mental changes
and decreased cardiac output.
Hypercalcaemia, elevated levels of calcium in the
blood, again arises from parathyroid problems and
vitamin D issues. Signs of this form of electrolyte
imbalance include nausea, vomiting, polyuria,
muscular weakness and mental disturbance.
Phosphate
Phosphate, or P, is an electrolyte used in several
functions throughout the body. Although a
phosphate imbalance isn’t as well known as some of
the other imbalances, it can still cause problems
with your patient’s condition. The normal range of
phosphate in the plasma is generally between 0.8
to 1.3 mmol/L. The signs and symptoms of either
abnormal reading are usually subtle.
For hypophosphataemia, when levels of phosphate
in the blood are below the normal range, the
symptoms generally include muscle weakness, heart
failure, seizure, and coma. It may be caused by
vitamin D deficiency, hyperparathyroidism, or
alcoholism. Hypophosphataemia may also be
present, in addition to other electrolyte
disturbances, in re-feeding syndrome, which is
associated with the commencement of total parental
nutrition (TPN).
Hyperphosphataemia, when levels of phosphate in
the blood are above the normal range, can be
caused by kidney disease, parathyroid issues, and
metabolic or respiratory acidosis. Symptoms are
usually not present, and they are related to
hypocalcaemia. Renal patients can experience
hardened calcium deposits when this condition goes
untreated.
Electrolyte Imbalance
Complications
Improper management of electrolyte imbalances can
worsen the baseline condition.
For example, overly aggressive treatment of hypo-
and hyperkalemia can cause cardiac arrhythmias.11
Some additional complications that can be caused
by electrolyte imbalance include:11
Arreflexic weakness due to hypermagnesemia,
hyperkalemia, and hypophosphatemia
Epileptic encephalopathies from
hypomagnesemia, dysnatremias and
hypocalcemia
Visual loss due to intracranial hypertension
caused by respiratory acidosis
Quadriplegia due to hypermagnesemia
Central pontine myelinolisis due to
mistreatment of hyponatremia
Conclusion
Many electrolyte imbalances self-correct without
any ill-effects. A simple drink of water can correct
others.
However, electrolyte imbalances can be much more
than just a nuisance – they can cause severe
complications when left untreated. It is important for
practitioners to correctly test for and diagnose
electrolyte imbalances in order to treat them in an
appropriate and timely fashion.
References
Roumelioti, ME, Glew, RH, Khitan, ZJ, Rondon-Berrios, H,
Argyropoulos, CP, Malhotra, D, Raj, DS, Agaba, EI,
Rohrscheib, M, Murata, GH, Shapiro, JI & Tzamaloukas
2018, ‘Fluid balance concepts in medicine: Principles and
practice’, World Journal of Nephrology, vol. 7, no. 1, pp. 1,
viewed 15 May 2018,
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760509/
Health Direct Australia 2016, Hot weather risks and staying
cool, Australian Government Department of Health, viewed
15 May 2018, https://www.healthdirect.gov.au/hot-
weather-risks-and-staying-cool
Santillanes, G & Rose, E 2018, ‘Evaluation and
Management of Dehydration in Children’, Emergency
Medicine Clinics, vol. 36, no. 2, pp. 259-73, viewed 15 May
2018,
https://www.sciencedirect.com/science/article/pii/S07338
62717301396?via%3Dihub
Curulli, S 2013, ‘Balancing act’, in Aged Care Insite, 2
December, viewed 15 May 2018,
https://www.agedcareinsite.com.au/2013/12/balancing-act/
Mora Rodríguez, R, Fernández Elías, VE, Hamouti, N &
Ortega, JF 2015, ‘Skeletal muscle water and electrolytes
following prolonged dehydrating exercise’, Scandinavian
journal of medicine & science in sports, vol. 25, no. 3, e.
274-82, viewed 15 May 2018,
https://onlinelibrary.wiley.com/doi/abs/10.1111/sms.12316
AID Sports Nutrition 2017, Sports drinks (carbohydrate-
electrolyte drinks), Australian Sports Commission, viewed
15 May 2018,
https://www.ausport.gov.au/__data/assets/pdf_file/0008/59
4170/Sports_drinks_carbohydrate-electrolyte_drinks_-
_June_2017.pdf
Medline Plus 2018, Fluid and electrolyte balance, US
National Library of Medicine, viewed 15 May 2018,
https://medlineplus.gov/fluidandelectrolytebalance.html
Balci, AK, Koksal, O, Kose, A, Armagan, E, Ozdemir, F, Inal,
T & Oner, N 2013, ‘General characteristics of patients with
electrolyte imbalance admitted to emergency department’,
World journal of emergency medicine, vol. 4, no. 2, p. 113,
viewed 15 May 2018,
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4129840/
Hooper, L, Attreed, NJ, Campbell, WW, Channell, AM,
Chassagne, P, Culp, KR & Heathcote, AC 2012, ‘Clinical and
Need
physical signs for an easy way
identification to manage
of impending and your
current
CPD?
water-loss dehydration in older people’, Cochrane
Sign up to
Database of Systematic Ausmed2,for
Reviews, Free 15
viewed to May
take2018,
control of your CPD
http://cochranelibrary-
wiley.com/doi/10.1002/14651858.CD009647/full
No Thanks Join Ausmed Free
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Cure For Cancer Hidden in Plain Sight July 2019 DR David WilliamsDocument8 pagesA Cure For Cancer Hidden in Plain Sight July 2019 DR David WilliamsThomas Van Beek100% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Brooks Kubik - The Dinosaur Strength Training NotebookDocument100 pagesBrooks Kubik - The Dinosaur Strength Training NotebookAlJ79100% (21)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Chapmans ReflexesDocument10 pagesChapmans ReflexesNickosteo100% (9)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Power Bodybuilding 12 Week Logs PDFDocument15 pagesPower Bodybuilding 12 Week Logs PDFAndy PaineNo ratings yet
- Power Bodybuilding 12 Week Logs PDFDocument15 pagesPower Bodybuilding 12 Week Logs PDFAndy PaineNo ratings yet
- Legal MedicineDocument107 pagesLegal MedicineKrist Chan RCrimNo ratings yet
- Getting Ripped EbookDocument14 pagesGetting Ripped EbookBrent Koboroff100% (1)
- Tips To Diagnose & Address Common Horse AilmentsDocument6 pagesTips To Diagnose & Address Common Horse AilmentsMark GebhardNo ratings yet
- Kangaroo Mother Care (KMC)Document40 pagesKangaroo Mother Care (KMC)subinj_350% (2)
- AFMC PrimerDocument523 pagesAFMC PrimerFajar Nurrachman100% (1)
- Public–private PartnershipDocument18 pagesPublic–private PartnershipAAKASH SHARMANo ratings yet
- Physiology of Thermoregulation (Dr. Herman)Document59 pagesPhysiology of Thermoregulation (Dr. Herman)stella pangestikaNo ratings yet
- Adr ReportingDocument12 pagesAdr Reportinguss uusNo ratings yet
- Bodybuilding - Weightlifting Training Database BookDocument239 pagesBodybuilding - Weightlifting Training Database BookRavi Yalala100% (2)
- Controlling Drug Delivery SystemsDocument24 pagesControlling Drug Delivery SystemsYuppie RajNo ratings yet
- 1 of 41 © Boardworks LTD 2008Document41 pages1 of 41 © Boardworks LTD 2008Hanifa Uly AmrinaNo ratings yet
- Exclusive Prepared Document for kennethtm159 Transaction 0036057220Document19 pagesExclusive Prepared Document for kennethtm159 Transaction 0036057220Paras BansalNo ratings yet
- Prelim Revision Booklet Core 1Document7 pagesPrelim Revision Booklet Core 1Brent KoboroffNo ratings yet
- Secure Shopping: Free ShippingDocument1 pageSecure Shopping: Free ShippingBrent KoboroffNo ratings yet
- Brochure Jimny WebVDocument13 pagesBrochure Jimny WebVBrent KoboroffNo ratings yet
- ST Johns Park High School Smart Sheet: Term 4 - Week 2Document2 pagesST Johns Park High School Smart Sheet: Term 4 - Week 2Brent KoboroffNo ratings yet
- FREEMAN Film Study - DiversityDocument2 pagesFREEMAN Film Study - DiversityBrent KoboroffNo ratings yet
- FREEMAN Film Study - DiversityDocument2 pagesFREEMAN Film Study - DiversityBrent KoboroffNo ratings yet
- 12PD4B - Thursday 3 Roll Marking - PXP PDFDocument1 page12PD4B - Thursday 3 Roll Marking - PXP PDFBrent KoboroffNo ratings yet
- ST Johns Park High School Smart Sheet: Term 4 - Week 5Document2 pagesST Johns Park High School Smart Sheet: Term 4 - Week 5Brent KoboroffNo ratings yet
- ST Johns Park High School: Staff Development Day - Term 3Document1 pageST Johns Park High School: Staff Development Day - Term 3Brent KoboroffNo ratings yet
- Benefits and limitations of always being contactable on mobile phonesDocument1 pageBenefits and limitations of always being contactable on mobile phonesBrent KoboroffNo ratings yet
- Aborigonanals and Physical ActiviityDocument8 pagesAborigonanals and Physical ActiviityBrent KoboroffNo ratings yet
- Fiona Comp Diet 2018Document10 pagesFiona Comp Diet 2018Brent KoboroffNo ratings yet
- 4 Wave TrainingDocument4 pages4 Wave TrainingBrent KoboroffNo ratings yet
- TrigonometryDocument5 pagesTrigonometryraomavuri8631No ratings yet
- Vestibular NeuritisDocument2 pagesVestibular NeuritisElsa Nabila YumezaNo ratings yet
- Jewish Standard, May 24, 2019Document48 pagesJewish Standard, May 24, 2019New Jersey Jewish StandardNo ratings yet
- Electrodiagnosisofcervical Radiculopathy: Kevin Hakimi,, David SpanierDocument12 pagesElectrodiagnosisofcervical Radiculopathy: Kevin Hakimi,, David Spanierkashif mansoorNo ratings yet
- AcuPulse Versatility SupplementDocument16 pagesAcuPulse Versatility SupplementSD DSNo ratings yet
- NCP RenalDocument22 pagesNCP Renalمحمود على ما تفرجNo ratings yet
- N, N-Dimethyltryptamine and The Pineal Gland - Separating Fact From MythDocument7 pagesN, N-Dimethyltryptamine and The Pineal Gland - Separating Fact From MythHamilton MorrisNo ratings yet
- 7 Final SubmissionDocument8 pages7 Final SubmissionNguyễn ThuNo ratings yet
- Utah KidneyDocument16 pagesUtah KidneyChristineGonzalesNo ratings yet
- Cell Bio Lecture 1Document40 pagesCell Bio Lecture 1Yashika HandaNo ratings yet
- Mini CasesDocument3 pagesMini CasesPravasini SahooNo ratings yet
- Patient Monitoring 1Document32 pagesPatient Monitoring 1janvenuNo ratings yet
- Abdurrehman's Resume for Biotechnology CareerDocument2 pagesAbdurrehman's Resume for Biotechnology CareerQasim KhanNo ratings yet
- The Beer Geek Handbook - Living A Life Ruled by Beer (2016)Document58 pagesThe Beer Geek Handbook - Living A Life Ruled by Beer (2016)zaratustra21No ratings yet
- Survivorfinal28 01 2020 PDFDocument25 pagesSurvivorfinal28 01 2020 PDFYogitaNo ratings yet
- Health Education Interventions For Older Adults With Hypertension: A Systematic Review and Meta-AnalysisDocument9 pagesHealth Education Interventions For Older Adults With Hypertension: A Systematic Review and Meta-AnalysisJosé Carlos Sánchez-RamirezNo ratings yet
- Bab 1 Normal KGBDocument14 pagesBab 1 Normal KGBukhtianitaNo ratings yet
- MYIASISDocument2 pagesMYIASISMirna HusseinNo ratings yet
- Beauty and Body Image in The MediaDocument3 pagesBeauty and Body Image in The MediaSuvradipNo ratings yet
- Histology of Sebaceous Glands and Nails by Dr. RoomiDocument10 pagesHistology of Sebaceous Glands and Nails by Dr. RoomiMudassar Roomi100% (1)