Professional Documents
Culture Documents
773 - PDFsam - Morgan Anesthesia 6ed New
773 - PDFsam - Morgan Anesthesia 6ed New
Uploaded by
Berty FebriantiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
773 - PDFsam - Morgan Anesthesia 6ed New
773 - PDFsam - Morgan Anesthesia 6ed New
Uploaded by
Berty FebriantiCopyright:
Available Formats
Butterworth_Ch35_p0753-0772.
indd 772 09/05/18 4:54 pm
36
C H A P T E R
Anesthesia for
Ophthalmic Surgery
KEY CONCEPTS
1 Any factor that increases intraocular 5 Medications applied topically to mucosa are
pressure in the setting of an open globe absorbed systemically at a rate intermediate
may cause drainage of aqueous or extrusion between absorption following intravenous
of vitreous through the wound, serious and subcutaneous injection.
complications that can permanently worsen 6 Echothiophate is an irreversible
vision. cholinesterase inhibitor used in the
2 Succinylcholine increases intraocular treatment of glaucoma. Topical application
pressure by 5 to 10 mm Hg for 5 to 10 min leads to systemic absorption and an
after administration, principally through inhibition of plasma cholinesterase activity.
prolonged contracture of the extraocular Because succinylcholine is metabolized by
muscles. However, in studies of hundreds of this enzyme, echothiophate will prolong its
patients with open eye injuries, no patient duration of action.
experienced extrusion of ocular contents 7 The key to inducing anesthesia in a patient
after administration of succinylcholine. Thus, with an open eye injury is controlling
succinylcholine is not contraindicated in intraocular pressure with a smooth
cases of open eye injuries. induction. Coughing and gagging during
3 Traction on extraocular muscles, pressure on intubation is avoided by first achieving
the eyeball, administration of a retrobulbar a deep level of anesthesia and profound
block, and trauma to the eye can elicit a wide paralysis.
variety of cardiac arrhythmias ranging from 8 The postretrobulbar block apnea syndrome
bradycardia and ventricular ectopy to sinus is probably due to injection of local
arrest or ventricular fibrillation. anesthetic into the optic nerve sheath, with
4 Complications involving the intraocular spread into the cerebrospinal fluid.
expansion of gas bubbles injected by 9 Regardless of the anesthetic technique,
the ophthalmologist can be avoided American Society of Anesthesiologists
by discontinuing nitrous oxide at least standards for basic monitoring must be
15 min prior to the injection of air or sulfur employed, and equipment and drugs
hexafluoride, or by avoiding the use of necessary for airway management and
nitrous oxide entirely. resuscitation must be immediately available.
773
Butterworth_Ch36_p0773-0786.indd 773 08/05/18 4:06 pm
774 SECTION III Anesthetic Management
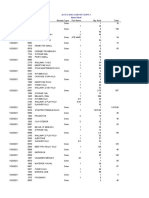
Ophthalmic surgery poses unique problems, includ- TABLE 36–1 The effect of cardiac and
ing regulation of intraocular pressure, control of respiratory variables on intraocular pressure
intraocular gas expansion, prevention of the oculo- (IOP).1
cardiac reflex and management of its consequences, Variable Effect on IOP
and management of systemic effects of ophthalmic
Central venous pressure
drugs. Mastery of general and sedation anesthesia
Increase ↑↑↑
techniques for ophthalmic surgery and a thorough Decrease ↓↓↓
understanding of potentially complicating issues— Arterial blood pressure
including the comorbidities of an increasing geri- Increase ↑
atric patient population—are necessary for optimal Decrease ↓
perioperative outcomes. In addition, the majority of PaCO2
Increase (hypoventilation) ↑↑
ophthalmic procedures are performed under topical Decrease (hyperventilation) ↓↓
or regional anesthesia. The anesthesiologist must be PaO2
familiar with their potential complications, includ- Increase 0
ing those of the accompanying sedation, even if not Decrease ↑
personally administering the topical anesthetic or ↓, decrease (mild, moderate, marked); ↑, increase (mild, moderate,
1
the block. marked); 0, no effect.
INTRAOCULAR PRESSURE
For example, blinking raises intraocular pressure by
DYNAMICS 5 mm Hg, and squinting (forced contraction of the
Physiology of Intraocular Pressure orbicularis oculi muscles) may transiently increase
The eye can be considered a hollow sphere with a intraocular pressure greater than 50 mm Hg. How-
rigid wall. If the contents of the sphere increase, the ever, even brief episodes of increased intraocular
normal intraocular pressure of 12 to 20 mm Hg will pressure in patients with underlying low ophthal-
rise. For example, glaucoma is caused by an obstruc- mic artery pressure (eg, from systemic hypotension,
tion to aqueous humor outflow. Similarly, intraocu- arteriosclerotic involvement of the retinal artery)
lar pressure will rise if the volume of blood within may cause retinal ischemia.
the globe is increased. A rise in venous pressure will When the globe is opened by surgical incision
increase intraocular pressure by decreasing aque- (Table 36–2) or traumatic perforation, intraocular
ous drainage and increasing choroidal blood vol- pressure approaches atmospheric pressure. Any fac-
ume. Any event that alters arterial blood pressure 1 tor that increases intraocular pressure in the
or ventilation (eg, laryngoscopy, intubation, airway setting of an open globe may cause drainage of
obstruction, coughing, Trendelenburg position) can aqueous or extrusion of vitreous through the wound,
also affect intraocular pressure (Table 36–1). serious complications that can permanently worsen
Alternatively, compressing the globe without a vision.
proportional change in the volume of its contents
will increase intraocular pressure. Pressure on the Effect of Anesthetic Drugs
eye from a malpositioned mask, improper prone on Intraocular Pressure
positioning, or retrobulbar hemorrhage can lead Most anesthetic drugs either reduce intraocular
to a marked increase in intraocular pressure, pos- pressure or have no effect (Table 36–3). Intraocular
sible eye pain, and temporary or permanent visual pressure decreases with inhalational anesthetics in
changes. proportion to anesthetic depth. There are multiple
Intraocular pressure helps to maintain the shape causes for this: A drop in blood pressure reduces
and the optical properties of the eye. Temporary choroidal volume, relaxation of the extraocular mus-
variations in pressure are normally well tolerated. cles lowers wall tension, and pupillary constriction
Butterworth_Ch36_p0773-0786.indd 774 08/05/18 4:06 pm
CHAPTER 36 Anesthesia for Ophthalmic Surgery 775
TABLE 36–2 Open-eye surgical procedures. TABLE 36–3 The effect of anesthetic agents
Cataract extraction
on intraocular pressure (IOP).1
Corneal laceration repair Drug Effect on IOP
Corneal transplant (penetrating keratoplasty) Inhaled anesthetics
Peripheral iridectomy Volatile agents ↓↓
Removal of foreign body Nitrous oxide ↓
Ruptured globe repair Intravenous anesthetics
Secondary intraocular lens implantation Propofol ↓↓
Benzodiazepines ↓↓
Trabeculectomy (and other filtering procedures) Ketamine ?
Vitrectomy (anterior and posterior) Opioids ↓
Wound leak repair Muscle relaxants
Succinylcholine ↑↑
Nondepolarizers 0/↓
1
↓, decrease (mild, moderate); ↑, increase (mild, moderate); 0/↓, no
facilitates aqueous outflow. Intravenous anesthetics change or mild decrease; ?, conflicting reports.
also decrease intraocular pressure, with the excep-
tion of ketamine, which usually raises arterial blood
pressure and does not relax extraocular muscles. imbalance and to determine the type of surgical cor-
Topically administered anticholinergic drugs rection. Nondepolarizing neuromuscular blockers
result in pupillary dilation (mydriasis), which may (NMBs) do not increase intraocular pressure, and we
precipitate or worsen angle-closure glaucoma. Sys- advocate that succinylcholine be reserved for rapid-
temically administered atropine or glycopyrrolate sequence induction.
for premedication are not associated with intraocu-
lar hypertension, even in patients with glaucoma.
THE OCULOCARDIAC REFLEX
2 Succinylcholine increases intraocular pressure
by 5 to 10 mm Hg for 5 to 10 min after admin-
istration, principally through prolonged contracture
3 Traction on extraocular muscles, pressure on
the eyeball, administration of a retrobulbar
of the extraocular muscles. However, in studies of block, and trauma to the eye can elicit a wide vari-
hundreds of patients with open eye injuries, no ety of cardiac arrhythmias ranging from bradycardia
patient experienced extrusion of ocular contents and ventricular ectopy to sinus arrest or ventricular
after administration of succinylcholine. Thus, succi- fibrillation. This reflex consists of a trigeminal (V1)
nylcholine is not contraindicated in cases of open eye afferent and a vagal efferent pathway. The oculocar-
injuries. Nevertheless, dogma often trumps data and diac reflex is most commonly encountered in chil-
ophthalmic surgeons may request that it not be dren undergoing strabismus surgery, although it can
administered in certain circumstances. Unlike other be evoked in all age groups and during a variety of
skeletal muscle, extraocular muscles contain myo- ocular procedures. In awake patients, the oculocar-
cytes with multiple neuromuscular junctions, and diac reflex may be accompanied by nausea.
depolarization of these cells by succinylcholine Routine prophylaxis for the oculocardiac reflex
causes prolonged contracture. The resulting increase is controversial, especially in adults. Anticholinergic
in intraocular pressure may have several effects: it medication is often helpful in preventing the oculo-
will cause spurious measurements of intraocular cardiac reflex, and intravenous atropine or glycopyr-
pressure during examinations under anesthesia in rolate immediately prior to surgery is more effective
glaucoma patients, potentially leading to unneces- than intramuscular premedication. However, anti-
sary surgery, and prolonged contracture of the extra- cholinergic medication should be administered with
ocular muscles may result in an abnormal forced caution to any patient who has, or may have, coronary
duction test, a maneuver utilized in strabismus sur- artery disease, because of the potential for increase in
gery to evaluate the cause of extraocular muscle heart rate sufficient to induce myocardial ischemia.
Butterworth_Ch36_p0773-0786.indd 775 08/05/18 4:06 pm
776 SECTION III Anesthetic Management
Ventricular tachycardia and ventricular fibrillation oxide concentration will almost triple the size of
following administration of anticholinergic medica- a 1-mL bubble and may double the pressure in a
tion has also been reported. Retrobulbar blockade or closed eye within 30 min. Subsequent discontinu-
deep inhalational anesthesia may also be of value in ation of nitrous oxide will lead to reabsorption of
preempting the oculocardiac reflex, although admin- the bubble, which has become a mixture of nitrous
istration of a retrobulbar block may itself initiate the oxide and sulfur hexafluoride. The consequent fall in
oculocardiac reflex. intraocular pressure may precipitate another retinal
Management of the oculocardiac reflex includes detachment.
(1) immediate notification of the surgeon and cessa- Complications involving the intraocular expan-
tion of surgical stimulation until heart rate increases;
4 sion of gas bubbles can be avoided by discon-
(2) confirmation of adequate ventilation, oxygen- tinuing nitrous oxide at least 15 min prior to
ation, and depth of anesthesia; (3) administration the injection of air or sulfur hexafluoride, or by
of intravenous atropine (10 mcg/kg) if bradycardia avoiding the use of nitrous oxide entirely. Nitrous
persists; and (4) in recalcitrant episodes, infiltration oxide should be avoided until the bubble is absorbed
of the rectus muscles with local anesthetic. (5 days after air and 10 days after sulfur hexafluoride
injection). Avoiding nitrous oxide seems the sim-
plest approach in these patients.
INTRAOCULAR GAS
EXPANSION
A gas bubble may be injected by the ophthalmolo-
SYSTEMIC EFFECTS OF
gist into the posterior chamber during vitreous sur- OPHTHALMIC DRUGS
gery. Intravitreal air injection will tend to flatten a Topically applied eye drops are systemically absorbed
detached retina and facilitate anatomically correct by vessels in the conjunctival sac and the nasolacri-
healing. Nitrous oxide administration is contraindi- mal duct mucosa (see Case Discussion, Chapter 13).
cated in this circumstance: The bubble will increase One drop (typically, approximately 1/20 mL) of 10%
in size if nitrous oxide is administered because phenylephrine contains approximately 5 mg of drug.
nitrous oxide is 35 times more soluble than nitro- Compare this dose with the intravenous dose of
gen in blood (see Chapter 8). Thus, it tends to dif- phenylephrine (0.05–0.1 mg) used to treat an adult
fuse into an air bubble more rapidly than nitrogen patient with acute hypotension. Medications applied
(the major component of air) is absorbed by the 5 topically to mucosa are absorbed systemically
bloodstream. If the bubble expands after the globe is at a rate intermediate between absorption fol-
closed, intraocular pressure will rise. lowing intravenous and subcutaneous injection. The
Sulfur hexafluoride is an inert gas that is less two patient populations most likely to require eye
soluble in blood than is nitrogen—and much less surgery, pediatric and geriatric, are at particular risk
soluble than nitrous oxide. Its longer duration of of the toxic effects of topically applied medications
action (up to 10 days) compared with an air bubble and should receive at most a 2.5% phenylephrine
can provide a therapeutic advantage. The bubble size solution (Table 36–4).
doubles within 24 h after injection, because nitro- Echothiophate (phospholine iodide) is an irre-
gen from inhaled air enters the bubble more rapidly 6 versible cholinesterase inhibitor used in the
than the sulfur hexafluoride diffuses into the blood- treatment of glaucoma. Topical application leads
stream. Even so, unless high volumes of pure sulfur to systemic absorption and an inhibition of plasma
hexafluoride are injected, the slow bubble expan- cholinesterase activity. Because succinylcholine is
sion does not typically raise intraocular pressure. If metabolized by this enzyme, echothiophate will
the patient is breathing nitrous oxide, however, the prolong its duration of action. Paralysis usually will
bubble will rapidly increase in size and may lead to not exceed 20 to 30 min and postoperative apnea is
intraocular hypertension. A 70% inspired nitrous unlikely. The inhibition of cholinesterase activity
Butterworth_Ch36_p0773-0786.indd 776 30/05/18 11:01 am
CHAPTER 36 Anesthesia for Ophthalmic Surgery 777
TABLE 36–4 Systemic effects of ophthalmic medications.
Drug Mechanism of Action Effect
Acetylcholine Cholinergic agonist (miosis) Bronchospasm, bradycardia, hypotension
Acetazolamide Carbonic anhydrase inhibitor (decreases IOP1) Diuresis, hypokalemic metabolic acidosis
Atropine Anticholinergic (mydriasis) Central anticholinergic syndrome2
Cyclopentolate Anticholinergic (mydriasis) Disorientation, psychosis, convulsions
Echothiophate Cholinesterase inhibitor (miosis, decreases IOP) Prolongation of succinylcholine and mivacurium
paralysis, bronchospasm
Epinephrine Sympathetic agonist (mydriasis, decreases IOP) Hypertension, bradycardia, tachycardia, headache
Phenylephrine α-Adrenergic agonist (mydriasis, vasoconstriction) Hypertension, tachycardia, dysrhythmias
Scopolamine Anticholinergic (mydriasis, vasoconstriction) Central anticholinergic syndrome2
Timolol β-Adrenergic blocking agent (decreases IOP) Bradycardia, asthma, congestive heart failure
1
IOP, intraocular pressure.
2
See Case Discussion, Chapter 13.
lasts for 3 to 7 weeks after discontinuation of echo- the operation, fear of the eye block procedure, or
thiophate drops. Muscarinic side effects of echothio- unpleasant recall of a previous eye block or local
phate, such as bradycardia during induction, can be eye procedure. General anesthesia is indicated in
prevented with intravenous anticholinergic drugs children and uncooperative patients, as even small
(eg, atropine, glycopyrrolate). head movements can prove disastrous during
Epinephrine eye drops can cause hyperten- microsurgery.
sion, tachycardia, and ventricular arrhythmias; the
arrhythmogenic effects are potentiated by halo-
thane. Direct instillation of epinephrine into the PREMEDICATION
anterior chamber of the eye has not been associated Patients undergoing eye surgery may be apprehen-
with cardiovascular toxicity. sive; however, premedication must be administered
Timolol, a nonselective β-adrenergic antago- with caution and only after careful consideration of
nist, reduces intraocular pressure by decreasing pro- the patient’s medical status. Adult patients are often
duction of aqueous humor. Topically applied timolol elderly, with systemic illnesses such as hypertension,
eye drops, commonly used to treat glaucoma, will diabetes mellitus, and coronary artery disease, and
often result in reduced heart rate. In rare cases, pediatric patients may have associated congenital
timolol has been associated with atropine-resistant disorders.
bradycardia, hypotension, and bronchospasm dur-
ing general anesthesia.
INDUCTION
The choice of induction technique for eye surgery
General Anesthesia for usually depends more on the patient’s other medical
Ophthalmic Surgery problems than on the patient’s eye disease or the
specific operation contemplated. One exception is
The choice between general and local anesthesia the patient with a ruptured globe. The key to induc-
should be made jointly by the patient, anesthesiolo-
7 ing anesthesia in a patient with an open eye
gist, and surgeon. Patients may refuse to consider injury is controlling intraocular pressure with
local anesthesia due to fear of being awake during a smooth induction. Specifically, coughing during
Butterworth_Ch36_p0773-0786.indd 777 30/05/18 11:01 am
778 SECTION III Anesthetic Management
intubation must be avoided by first achieving a deep by the oculocardiac reflex increases the importance
level of anesthesia and profound paralysis. The intra- of closely monitoring the electrocardiogram. In con-
ocular pressure response to laryngoscopy and endo- trast to most other types of pediatric surgery, infant
tracheal intubation can be moderated by prior body temperature may rise during ophthalmic
administration of intravenous lidocaine (1.5 mg/kg), surgery because of head-to-toe draping and mini-
an opioid (eg, remifentanil 0.5–1 mcg/kg or alfent- mal body surface exposure. End-tidal CO2 analysis
anil 20 mcg/kg), or esmolol (0.5–1.5 mg/kg). A non- helps to differentiate this situation from malignant
depolarizing muscle relaxant or succinylcholine may hyperthermia.
be used. Many patients with open globe injuries The pain and stress evoked by eye surgery are
have full stomachs and require a rapid-sequence considerably less than during a major surgical pro-
induction technique to avoid aspiration (see the cedure. “Lighter” anesthesia might be attractive if
later Case Discussion); despite theoretical concerns, the consequences of patient movement were not so
succinylcholine does not increase the likelihood of potentially catastrophic. The lack of cardiovascular
vitreous loss with open eye injuries. stimulation inherent in most eye procedures com-
bined with the need for adequate anesthetic depth
can result in hypotension in elderly individuals. This
MONITORING & problem is usually avoided by ensuring adequate
MAINTENANCE intravenous hydration and by administering small
doses of intravenous vasoconstrictors. Administra-
Eye surgery often necessitates positioning the anes-
tion of nondepolarizing muscle relaxants to avoid
thesia provider away from the patient’s airway, mak-
patient movement is often used in such circum-
ing close monitoring of pulse oximetry and the
stances in order to allow reduced depth of general
capnograph particularly important. Endotracheal
anesthesia.
tube kinking, breathing circuit disconnection, and
Emesis caused by vagal stimulation is a com-
unintentional extubation may be more likely because
mon postoperative problem following eye surgery,
of the surgeon working near the airway. Kinking and
particularly with strabismus repair. The Valsalva
obstruction can be minimized by using a preformed
effect and the increase in central venous pressure
oral RAE (Ring-Adair-Elwyn) endotracheal tube
that accompany vomiting can be detrimental to the
(Figure 36–1). The possibility of arrhythmias caused
surgical result. Intraoperative intravenous adminis-
tration of drugs that prevent postoperative nausea
and vomiting is strongly recommended.
EXTUBATION & EMERGENCE
A smooth emergence from general anesthesia is
important in order to minimize the risk of post-
operative wound dehiscence. Coughing or gagging
due to stimulus from the endotracheal tube can be
minimized by extubating the patient at a moder-
ately deep level of anesthesia. As the time of extuba-
tion approaches intravenous lidocaine (1.5 mg/kg)
may be given to blunt cough reflexes temporarily.
Extubation proceeds 1 to 2 min after the lidocaine
administration and during spontaneous respira-
FIGURE 36–1 An oral RAE endotracheal tube has a
preformed right-angle bend at the level of the teeth so tion with 100% oxygen. Proper airway maintenance
that it exits the mouth away from the surgical field during is crucial until the patient’s cough and swallowing
ophthalmic or nasal surgery. reflexes return.
Butterworth_Ch36_p0773-0786.indd 778 30/05/18 11:01 am
CHAPTER 36 Anesthesia for Ophthalmic Surgery 779
Severe discomfort is unusual following eye sur- anesthesia is preferred to general anesthesia for eye
gery. Scleral buckling procedures, enucleation, and surgery because local anesthesia involves less physi-
ruptured globe repair are the most painful opera- ological trespass and is less likely to be associated
tions. Modest incremental doses of intravenous opi- with postoperative nausea and vomiting. However,
oid usually provide sufficient analgesia. The surgeon eye block procedures have potential complications
should be alerted if severe pain is noted following and may not provide adequate ophthalmic akinesia
emergence from general anesthesia, as it may signal or analgesia. Some patients may be unable to lie per-
intraocular hypertension, corneal abrasion, or other fectly still for the duration of the surgery. For these
surgical complications. reasons, appropriate equipment and qualified per-
sonnel required to treat the complications of local
anesthesia and to induce general anesthesia must be
Regional Anesthesia for readily available.
Ophthalmic Surgery
Options for local anesthesia for eye surgery include RETROBULBAR BLOCKADE
topical application of local anesthetic or place- In this technique, local anesthetic is injected behind
ment of a retrobulbar, peribulbar, or sub-Tenon the eye into the cone formed by the extraocular mus-
(episcleral) block. All of these techniques are com- cles (Figure 36–2), and a facial nerve block is utilized
monly combined with intravenous sedation. Local to prevent blinking (Figure 36–3). A blunt-tipped
A B
FIGURE 36–2 A: During administration of a retrobulbar block, the patient looks supranasally as a needle is advanced
1.5 cm along the inferotemporal wall of the orbit. B: The needle is then redirected upward and nasally toward the apex of
the orbit and advanced until its tip penetrates the muscle cone.
Butterworth_Ch36_p0773-0786.indd 779 08/05/18 4:06 pm
780 SECTION III Anesthetic Management
injection with resultant convulsions, oculocardiac
reflex, trigeminal nerve block, respiratory arrest,
and, rarely, acute neurogenic pulmonary edema.
Forceful injection of local anesthetic into the oph-
thalmic artery causes retrograde flow toward the
brain and may result in an instantaneous seizure.
8 The postretrobulbar block apnea syndrome is
probably due to injection of local anesthetic
into the optic nerve sheath, with spread into the
1 cerebrospinal fluid. The central nervous system is
exposed to high concentrations of local anesthetic,
leading to mental status changes that may include
2
3 unconsciousness. Apnea occurs within 20 min and
resolves within an hour. Treatment is supportive,
with positive-pressure ventilation to prevent
hypoxia, bradycardia, and cardiac arrest. Adequacy
of ventilation must be constantly monitored in
patients who have received retrobulbar anesthesia.
The adjuvant hyaluronidase is frequently added
to local anesthetic solutions used in eye blocks
to enhance the spread and density of the block.
Patients may rarely experience an allergic reaction
to hyaluronidase. Retrobulbar hemorrhage, celluli-
FIGURE 36–3 Facial nerve block techniques: van Lint (1), tis, occult injury, and contact allergy to topical eye
Atkinson (2), and O’Brien (3). drops must be ruled out in the differential diagnosis.
Retrobulbar injection is usually not performed in
25-gauge needle penetrates the lower lid at the junc- patients with bleeding disorders or receiving antico-
tion of the middle and lateral one-third of the orbit agulation therapy because of the risk of retrobulbar
(usually 0.5 cm medial to the lateral canthus). Awake hemorrhage, extreme myopia because the elongated
patients are instructed to stare supranasally as the globe increases the risk of perforation, or an open
needle is advanced toward the apex of the muscle eye injury because the pressure from injecting fluid
cone. Commonly, patients undergoing such eye behind the eye may cause extrusion of intraocular
blocks will receive a brief period of deep sedation contents through the wound.
or general anesthesia during the block (using such
agents as etomidate, propofol, or remifentanil). After
aspiration to preclude intravascular injection, 2 to PERIBULBAR BLOCKADE
5 mL of local anesthetic is injected, and the needle is In contrast to retrobulbar blockade, in the peribul-
removed. Choice of local anesthetic varies, but lido- bar blockade technique, the needle does not pen-
caine 2% or bupivacaine (or ropivacaine) 0.75% are etrate the cone formed by the extraocular muscles.
common. Addition of epinephrine may reduce bleed- Advantages of the peribulbar technique include less
ing and prolong the anesthesia. A successful retrobul- risk of penetration of the globe, optic nerve, and
bar block is accompanied by anesthesia, akinesia, and artery, and less pain on injection. Disadvantages
abolishment of the oculocephalic reflex (ie, a blocked include a slower onset and an increased likelihood
eye does not move during head turning). of ecchymosis. Both techniques will have equal suc-
Complications of retrobulbar injection of local cess at producing akinesia of the eye.
anesthetics include retrobulbar hemorrhage, perfo- The peribulbar block is performed with the
ration of the globe, optic nerve injury, intravascular patient supine and looking directly ahead (or possibly
Butterworth_Ch36_p0773-0786.indd 780 08/05/18 4:06 pm
CHAPTER 36 Anesthesia for Ophthalmic Surgery 781
nick is then made with blunt-tipped scissors, which
are then slid underneath to create a path in Tenon’s
fascia that follows the contour of the globe and
extends past the equator. While the eye is still fixed
with forceps, the cannula is inserted, and 3 to 4 mL
of local anesthetic is injected. Complications with
2 sub-Tenon blocks are significantly less than with
retrobulbar and peribulbar techniques. Globe perfo-
1
ration, hemorrhage, cellulitis, permanent visual loss,
3 and local anesthetic spread into cerebrospinal fluid
5
4 have been reported.
FACIAL NERVE BLOCK
A facial nerve block prevents squinting of the eyelids
during surgery and allows placement of a lid specu-
FIGURE 36–4 Anatomic landmarks for the lum. There are several techniques of facial nerve
introduction of a needle or catheter in most frequently block: van Lint, Atkinson, and O’Brien (Figure 36–3).
employed eye blocks: (1) medial canthus peribulbar The major complication of these blocks is subcuta-
anesthesia, (2) lacrimal caruncle, (3) semilunaris fold of the
neous hemorrhage. The Nadbath technique blocks
conjunctiva, (4) medial canthus episcleral anesthesia, and
(5) inferior and temporal peribulbar anesthesia. the facial nerve as it exits the stylomastoid foramen
under the external auditory canal, in close proxim-
ity to the vagus and glossopharyngeal nerves. This
under a brief period of deep sedation). After topical block is not recommended because it has been asso-
anesthesia of the conjunctiva, one or two transcon- ciated with vocal cord paralysis, laryngospasm, dys-
junctival injections are administered (Figure 36–4). phagia, and respiratory distress.
As the eyelid is retracted, an inferotemporal injec-
tion is given halfway between the lateral canthus and
the lateral limbus. The needle is advanced under the TOPICAL ANESTHESIA
globe, parallel to the orbital floor; when it passes the OF THE EYE
equator of the eye, it is directed slightly medial (20°) Simple topical local anesthetic techniques have
and cephalad (10°), and 5 mL of local anesthetic is been used for anterior chamber (eg, cataract) and
injected. To ensure akinesia, a second 5-mL injection glaucoma operations, and, increasingly, the trend
may be given through the conjunctiva on the nasal has been to eliminate local anesthetic injections
side, medial to the caruncle, and directed straight entirely. A typical regimen for topical local anesthe-
back parallel to the medial orbital wall, pointing sia consists of application of 0.5% proparacaine (also
slightly cephalad (20°). known as proxymetacaine) local anesthetic drops,
repeated at 5-min intervals for five applications, fol-
Sub-Tenon (Episcleral) Block lowed by topical application of a local anesthetic gel
Tenon’s fascia surrounds the globe and extraocu- (lidocaine plus 2% methyl-cellulose) with a cotton
lar muscles. Local anesthetic injected beneath it swab to the inferior and superior conjunctival sacs.
into the episcleral space spreads circularly around Ophthalmic 0.5% tetracaine may also be utilized.
the sclera and to the extraocular muscle sheaths Topical anesthesia is not appropriate for posterior
(Figure 36–4). A special blunt curved cannula is chamber surgery (eg, retinal detachment repair with
used for a sub-Tenon block. After topical anesthe- a buckle), and it works best for faster surgeons with
sia, the conjunctiva is lifted along with Tenon’s fascia a gentle surgical technique that does not require aki-
in the inferonasal quadrant with forceps. A small nesia of the eye.
Butterworth_Ch36_p0773-0786.indd 781 08/05/18 4:06 pm
782 SECTION III Anesthetic Management
INTRAVENOUS SEDATION established. The patient must be considered to
Many techniques of intravenous sedation are avail- have a full stomach if the injury occurred within
able for eye surgery, and the particular drug used 8 h after the last meal, even if the patient did not
is less important than the dose. Deep sedation, eat for several hours after the injury: Gastric empty-
although sometimes used during placement of oph- ing is delayed by the pain and anxiety that follow
thalmic nerve blocks, is almost never used intraop- trauma.
eratively because of the risks of apnea, aspiration,
What is the significance of a full stomach
and unintentional patient movement during sur-
in a patient with an open globe injury?
gery. An intraoperative light sedation regimen that
includes small doses of midazolam, with or without Managing patients who have sustained pene-
fentanyl or sufentanil, is recommended. Doses vary trating eye injuries provides a challenge because of
considerably among patients but should be adminis- the need to deal with at least two conflicting objec-
tered in small increments. tives: (1) preventing further damage to the eye by
Patients may find administration of eye blocks avoiding increases in intraocular pressure, and
uncomfortable, and many anesthesia providers will (2) preventing pulmonary aspiration in a patient
administer small incremental doses of propofol to with a full stomach. However, many of the com-
produce a brief state of unconsciousness during the mon strategies used to achieve these objectives
regional block. Some will substitute a bolus of opioid are in conflict with one another (Tables 36–5 and
(remifentanil 0.1–0.5 mcg/kg or alfentanil 375–500 36–6). For example, although regional anesthesia
mcg) to produce a brief period of intense analgesia (eg, retrobulbar block) minimizes the risk of aspi-
during the eye block procedure. ration pneumonia, it is relatively contraindicated
Administration of an antiemetic should be in patients with penetrating eye injuries because
considered if an opioid is used. Regardless of the injecting local anesthetic behind the globe
increases intraocular pressure and may lead to
9 anesthetic technique, American Society of expulsion of intraocular contents. Therefore, these
Anesthesiologists standards for basic monitor-
ing must be employed, and equipment and drugs patients require general anesthesia—despite the
necessary for airway management and resuscitation increased risk of aspiration pneumonia.
must be immediately available. What preoperative preparation should be
considered in this patient?
CASE DISCUSSION One clearly will want to minimize the risk of
aspiration pneumonia by decreasing gastric volume
An Approach to a Patient with
an Open Eye & a Full Stomach
A 12-year-old boy is brought to the emergency TABLE 36–5 Strategies to prevent increases
department after being shot in the eye with a in intraocular pressure (IOP).
pellet gun. A brief examination by the ophthal- Avoid direct pressure on the globe
mologist reveals intraocular contents presenting Patch eye with Fox shield
No retrobulbar or peribulbar injections
at the wound. The boy is scheduled for emer- Careful face mask technique
gency repair of the ruptured globe. Avoid increases in central venous pressure
What should be emphasized in the preoperative Prevent coughing during induction and intubation
Ensure a deep level of anesthesia and relaxation prior to
evaluation of this patient?
laryngoscopy1
Aside from taking a medical history and per- Avoid head-down positions
Extubate under deep anesthesia1
forming a physical examination, the time of last
Avoid pharmacological agents that increase IOP
oral intake before or after the injury should be
These strategies are not recommended in patients with full stomachs.
1
Butterworth_Ch36_p0773-0786.indd 782 08/05/18 4:06 pm
CHAPTER 36 Anesthesia for Ophthalmic Surgery 783
TABLE 36–6 Strategies to prevent aspiration Which induction agents are recommended
pneumonia. in patients with penetrating eye injuries?
Regional anesthesia with minimal sedation1 The ideal induction agent for patients with full
Premedication stomachs would provide a rapid onset of action in
Metoclopramide
Histamine H2-receptor antagonists order to minimize the risk of regurgitation. Propo-
Nonparticulate antacids fol and etomidate have essentially equally rapid
Evacuation of gastric contents onsets of action and lower intraocular pressure.
Nasogastric tube1
Although investigations of the effects of ketamine
Rapid-sequence induction
Cricoid pressure on intraocular pressure have provided conflicting
Rapid induction with rapid onset of paralysis results, ketamine is not recommended in pene-
Avoidance of positive-pressure ventilation via mask trating eye injuries, owing to the increased risk of
Intubation as soon as possible
blepharospasm and nystagmus.
Extubation awake
Although etomidate may prove valuable in
1
These strategies are not recommended for patients with penetrating
eye injuries.
some patients with cardiac disease, it is associ-
ated with an incidence of myoclonus ranging from
10% to 60%. An episode of severe myoclonus may
have contributed to complete retinal detachment
and acidity (see Case Discussion, Chapter 17). The and vitreous prolapse in one patient with an open
risk of aspiration in patients with eye injuries is globe injury and limited cardiovascular reserve.
reduced by proper selection of drugs and anes- Propofol has a rapid onset of action and
thetic techniques. Evacuation of gastric contents decreases intraocular pressure; however, it does
with a nasogastric tube may lead to coughing, not entirely prevent the hypertensive response to
retching, and other responses that can dramatically laryngoscopy and intubation or entirely prevent
increase intraocular pressure. the increase in intraocular pressure that accom-
Metoclopramide increases lower esophageal panies laryngoscopy and intubation. Prior admin-
sphincter tone, speeds gastric emptying, low- istration of fentanyl (1–3 mcg/kg), remifentanil
ers gastric fluid volume, and exerts an antiemetic (0.5–1 mcg/kg), alfentanil (20 mcg/kg), esmolol
effect. It should be given intravenously (10 mg) as (0.5–1.5 mg/kg), or lidocaine (1.5 mg/kg) attenu-
soon as possible and repeated every 2 to 4 h until ates this response with varying degrees of success.
surgery.
Ranitidine (50 mg intravenously), cimetidine How does the choice of muscle relaxant differ
(300 mg intravenously), and famotidine (20 mg between these patients and other patients at risk
intravenously) are H2-receptor antagonists that of aspiration?
inhibit gastric acid secretion. Because they have no Succinylcholine moderately increases intra-
effect on the pH of gastric secretions present in the ocular pressure, but that is a small price to pay
stomach prior to their administration, they have for a rapid onset of action that decreases the risk
limited value in patients presenting for emergency of aspiration and profound muscle relaxation that
surgery. decreases the chance of a Valsalva response dur-
Unlike H2-receptor antagonists, antacids have ing intubation. Advocates of succinylcholine point
an immediate effect. Unfortunately, they increase to the lack of evidence documenting further eye
intragastric volume. Nonparticulate antacids injury when succinylcholine has been used with
(preparations of sodium citrate, potassium citrate, open eye injuries.
and citric acid) lose effectiveness within 30 to Nondepolarizing muscle relaxants do not
60 min and should be given immediately prior to increase intraocular pressure, but the onset of
induction (15–30 mL orally). deep muscle relaxation is much slower than with
Butterworth_Ch36_p0773-0786.indd 783 08/05/18 4:06 pm
784 SECTION III Anesthetic Management
succinylcholine. Regardless of the muscle relaxant SUGGESTED READINGS
chosen, intubation should not be attempted until Adams L. Adjuvants to local anaesthesia in ophthalmic
a level of paralysis is achieved that will reliably pre- surgery. Br J Ophthalmol. 2011;95:1345.
vent coughing on the endotracheal tube. Alhassan MB, Kyari F, Ejere HO. Peribulbar versus
retrobulbar anaesthesia for cataract surgery. Cochrane
How do induction strategies vary in pediatric Database Syst Rev. 2015;(7):CD004083.
patients without an intravenous line? Ascaso F, Peligero J, Longas J, et al. Regional anesthesia
A hysterical child with a penetrating eye injury of the eye, orbit, and periocular skin. Clin Dermatol.
and a full stomach provides an anesthetic chal- 2015;33:227.
Bhananker S, Posner K, Cheney F, et al. Injury and
lenge for which there is no perfect solution. Once
liability associated with monitored anesthesia care.
again, the dilemma is due to the need to avoid
Anesthesiology. 2006;104:228.
increases in intraocular pressure yet minimize the Bryant J, Busbee B, Reichel E. Overview of ocular
risk of aspiration. Screaming and crying can lead anesthesia: past and present. Curr Opin Ophthalmol.
to tremendous increases in intraocular pressure. 2011;22:180.
Attempting to sedate children with rectal supposi- Connor M, Menke A, Vrcek I, et al. Operating room
tories or intramuscular injections often heightens fires in periocular surgery. Int Ophthalmol. 2017; May
their state of agitation and may worsen the eye 20. doi 10.1007/s10792-017-0564-9. [Epub ahead of
injury. Similarly, although preoperative sedation print]
may increase the risk of aspiration by obtunding Delaere L, Zeyen T, Foets B, et al. Allergic reaction to
airway reflexes, it is often necessary for establish- hyaluronidase after retrobulbar anaesthesia: A case
series and review. Int Ophthalmol. 2009;29:521.
ing an intravenous line for a rapid-sequence induc-
Gayer S, Palte HD. Ultrasound-guided ophthalmic
tion. Although difficult to achieve, an ideal strategy
regional anesthesia. Curr Opin Anesthesiol.
would be to administer enough sedation painlessly 2016;29:655.
to allow the placement of an intravenous line, yet Greenhalgh D, Kumar C. Sedation during ophthalmic
maintain a level of consciousness adequate to surgery. Eur J Anaesthesiol. 2008;25:701.
protect airway reflexes. However, the most pru- Guise P. Sub-Tenon’s anesthesia: An update. Local Reg
dent strategy is to do everything reasonable to Anesth. 2012;5:35.
avoid aspiration—even at the cost of further eye Kong K, Khan J. Ophthalmic patients on antithrombotic
damage. drugs: A review and guide to perioperative
management. Br J Ophthalmol. 2015;99:1025.
Are there special considerations during Kumar C. Needle-based blocks for the 21st century
extubation and emergence? ophthalmology. Acta Ophthalmologica. 2011;89:5.
Patients at risk of aspiration during induction Kumar C, Dowd T. Complications of ophthalmic
are also at risk during extubation and emergence. regional blocks: Their treatment and prevention.
Therefore, extubation must be delayed until the Ophthalmologica. 2006;220:73.
Kumar C, Dowd T. Ophthalmic regional anaesthesia.
patient is awake and has intact airway reflexes (eg,
Curr Opin Anaesthesiol. 2008;21:632.
spontaneous swallowing and coughing on the
Kumar CM, Eid H, Dodds C. Sub-Tenon’s anaesthesia:
endotracheal tube). Deep extubation increases Complications and prevention. Eye. 2011;25:694.
the risk of vomiting and aspiration. Intraoperative Lee LA, Posner KL, Cheney FL, et al. Complications
administration of antiemetic medication and naso- associated with eye blocks and peripheral nerve
gastric or orogastric tube suctioning may decrease blocks: An American Society of Anesthesiologists
the incidence of emesis during emergence, but closed claim analysis. Reg Anesth Pain Med.
they do not guarantee an empty stomach. 2008;33:416.
Lee R, Thompson J, Eke T. Severe adverse events
associated with local anesthesia in cataract surgery:
Butterworth_Ch36_p0773-0786.indd 784 08/05/18 4:06 pm
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Reid J. Meloy - The Psychopathic Mind - Origins, Dynamics, and Treatment-Jason Aronson, Inc. (1988) PDFDocument497 pagesReid J. Meloy - The Psychopathic Mind - Origins, Dynamics, and Treatment-Jason Aronson, Inc. (1988) PDFvictorpsyche71% (7)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Muscular SystemDocument49 pagesMuscular SystemHindrix Mitch100% (1)
- Embryology of The HeartDocument16 pagesEmbryology of The HeartRut H. P. EkasiwiNo ratings yet
- Special and Abbreviated 510 (K)Document18 pagesSpecial and Abbreviated 510 (K)hemkenbpNo ratings yet
- Raising Meat RabbitsDocument4 pagesRaising Meat RabbitsMike NichlosNo ratings yet
- 5503 Vit C Chewable TabletsDocument5 pages5503 Vit C Chewable Tabletsamitaggarwal78100% (1)
- @MedicalBooksStore 2012 (ERS Monograph) TuberculosisDocument271 pages@MedicalBooksStore 2012 (ERS Monograph) TuberculosisHeri GunawanNo ratings yet
- Laboratory Information System PDFDocument96 pagesLaboratory Information System PDFTangled LimNo ratings yet
- Aflori, Magdalena - Intelligent Polymers For Nanomedicine and biotechnologies-CRC Press (2018) PDFDocument243 pagesAflori, Magdalena - Intelligent Polymers For Nanomedicine and biotechnologies-CRC Press (2018) PDFcarquerNo ratings yet
- The Menstrual CycleDocument4 pagesThe Menstrual CycleMotilaldassNo ratings yet
- Daftar Nama Obat Dan PengencernyaDocument15 pagesDaftar Nama Obat Dan PengencernyaMeta SuryantiNo ratings yet
- Icu Enteral Feeding GuidelinesDocument12 pagesIcu Enteral Feeding GuidelinesNofilia Citra CandraNo ratings yet
- Heart Specialist in Haldwani - Google SearchDocument1 pageHeart Specialist in Haldwani - Google SearchManoj UpadhyayNo ratings yet
- Minamata DiseasesDocument58 pagesMinamata DiseasesMuhammad Rahimi Bin SatarNo ratings yet
- Disney PrincessesDocument18 pagesDisney Princessesapi-214858613No ratings yet
- CPRils Trigger ListDocument1 pageCPRils Trigger ListMikeNo ratings yet
- SD BIOLINE HIV 12 3.0 BrochureDocument2 pagesSD BIOLINE HIV 12 3.0 BrochureDina Friance ManihurukNo ratings yet
- NGLRFWLR Facts 2015Document2 pagesNGLRFWLR Facts 2015Alex OnkenNo ratings yet
- Composite Resins and La Nueva Era Postamalgama PASCAL MAGNE PDFDocument13 pagesComposite Resins and La Nueva Era Postamalgama PASCAL MAGNE PDFXiomara Reyes PalominoNo ratings yet
- Kti DMDocument117 pagesKti DMYudhis BamsNo ratings yet
- Max 360mg/d Codein Max 12 Tabs/d Max 4g/d Max 1.2 G 2.4g/d Max 120mg/dDocument3 pagesMax 360mg/d Codein Max 12 Tabs/d Max 4g/d Max 1.2 G 2.4g/d Max 120mg/dSamantha LuiNo ratings yet
- Date Receipt # Receipt Type Full Name Qty Sold Total: JN Sto - Nino Agrivet Supply Sales DetailDocument6 pagesDate Receipt # Receipt Type Full Name Qty Sold Total: JN Sto - Nino Agrivet Supply Sales DetailNeil Dave SuarezNo ratings yet
- A Presentation On Congenital HyperthyroidismDocument26 pagesA Presentation On Congenital Hyperthyroidismkriti kaushalNo ratings yet
- Appendicitis in The Child With A Ventriculo-Peritoneal Shunt: A 30-Year ReviewDocument4 pagesAppendicitis in The Child With A Ventriculo-Peritoneal Shunt: A 30-Year ReviewAngel OlarteNo ratings yet
- Certificate of Professional Experience General Directorate of Health - ErbilDocument3 pagesCertificate of Professional Experience General Directorate of Health - ErbilAh MedNo ratings yet
- Biochemistry of NeurotransmissionDocument47 pagesBiochemistry of NeurotransmissionTariq MahmoodNo ratings yet
- 10 1111@jocd 13491Document28 pages10 1111@jocd 13491Emrys1987No ratings yet
- Honorhealth Scottsdale Shea Medical Center: Campus MapDocument1 pageHonorhealth Scottsdale Shea Medical Center: Campus MapFEALABREPORTSNo ratings yet
- Lesson 5 Venipuncture Steps NotesDocument3 pagesLesson 5 Venipuncture Steps NotesAlthea EspirituNo ratings yet
- Day2.2 - Lionberger - GDUFA Regulatory ScienceDocument37 pagesDay2.2 - Lionberger - GDUFA Regulatory ScienceMarkbot1999No ratings yet