Professional Documents
Culture Documents
Scanned Documents
Scanned Documents
Uploaded by
Kit Alizon Barredo0 ratings0% found this document useful (0 votes)
5 views22 pagesOriginal Title
Scanned-Documents
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
5 views22 pagesScanned Documents
Scanned Documents
Uploaded by
Kit Alizon BarredoCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 22
Heart Failure
HF is the inability of the heart to pump sufficient blood to
meet the needs of the tissues for oxygen and nutrients. In the
past, HF was often referred to as congestive heart failure
(CHEF), because many patients experience pulmonary of
peripheral congestion. Currently HF is recognized as a clin-
ical syndrome characterized by signs and symptoms of fluid
overload or of inadequate tissue perfusion. Eluid overload
and decreased tissue-perfusion result when the heart can-
not generate a CO sufficient to meet the body’s demands.
The term HF indicates myocardial disease in which there is
a problem with contraction of the heart (systolic dysfunc-
tion) or filling of the heart (diastolic dysfunction) that may
or may not cause pulmonary or systemic congestion. Some
cases of HF are reversible, depending on the cause. Most
often, HF is a progressive, life-long diagnosis that is man-_
aged_with lifestyle changes and medications to prevent
acute congestive episodes.
Chronic Heart Failure
Aswith coronary artery disease, the incidence of HF increases
with age. At least 5 million people in the United States have
HF, and 550,000 new cases are diagnosed each year
(American Heart Association [AHA], 2004). Although HF
can affect people of all ages, the prevalence in people older
than 75 years of age is about 10%, and as the U.S. popula-
tion ages, HF has become an epidemic that challenges the
country’s health care resources (AHA, 2004), HF is the most
common reason for hospitalization of people older than
65 years of age and the second most common reason for vis-
its to a physician’s office. The rate of hospital readmission
remains staggeringly high. The economic burden caused by
HF is estimated to be more than $25 billion in direct and
indirect costs and is expected to increase (AHA, 2004).
The increase in the incidence of HF reflects the increased
number of elderly people and improvements in treatment
of cardiac diseases, resulting in increased survival rates.
Many hospitalizations could be prevented by appropriate
outpatient care. Prevention and early intervention to arrest
the progression of HF are major health initiatives in the
United States.
There are two types of HF, which are identified by assess-
ment of left ventricular functioning, usually by echocardio-
gram. The more common type is an alteration in ventricular
contraction called systolic heart failure, which is charac-
terized by a weakened heart muscte-The less common alter-
ation is diastolic heart faline rice is characterized by a
stiffand noncompliant heart muscle, making it difficult for
the ventricle to fill. An assessment of the ejection fraction
(EF) is performed to assist in determining the type of HF.
EF, an indication of the volume of blood ejected with each
contraction, is calculated by subtracting the amount of blood
wat the end of systole from the amount at the end of diastole
and calculating the tcentage of blood that is ejected. A nor-
mal EF is 55% 10 6S Bot the ventricular volume; the ventri-
cle does not completely empty between contractions. The EF
is normal in diastolic HF but severely reduced in systolic HF.
Although ad is a hallmark » the severity of HE
is frequently Hotlied seem eee symptoms.
The New York Heart Association (NYHA) Classification is
described in Table 30-1, and the causes are explained in
subsequent sections of this chapter. The American College
of Cardiology and the American Heart Association (ACC/
AHA) have proposed a new HF classification system (Insti-
tute for Clinical Systems Improvement {ICSI}, 2004). This
system (Table 30-2) takes into consideration the natural
Pathophysiology
HF results from a variety of cardiovascular conditions, in-
cluding chronic hypertension, coronary artery disease, and
valvular disease. These conditions can result in decreased
caute HOR Coatsle decreased filling (diastole), or both.
Significant myocardial dysfunction most often occurs before
the patient copetiences Signs anid gns and symptoms of HF such as
Sere ea edema, or fatigue.
develops, the body activates neurohormonal com-
pensatory mechanisms. These mechanisms represent the
body's attempt to cope with the HF and are responsible for
the signs and symptoms that eventually develop. Under-
standing these mechanisms is important because the treat-
ment of HF is aimed at relieving them.
Systolic HF results in decreased blood volume being
ejected from the ventricle. icular stretch
is-sensed_by baroreceptors in the aortic and carotid bodie
(Piano & Prasun, 2003). The sympathetic nervous system
is then stimulated to i i eph-
rine (Fig. 30-2). The purpose of this initial response is to
igcrease-heart rate and contractility and support the failing
myocardium, but the continued response has multiple nega-
tive effects. Sympathetic stimulation causes vasoconstriction
of the skin, gastrointestinal tract, and kidneys. A decrease
in renal perfusion due to low CO and vasoconstriction then
causes the r in_by the kidney. Renin promotes
the formation of angiotensin I, a benign, inactive substance.
Angiotensin-converting enzyme (ACE) in the lumen of pul-
monary blood vessels converts angiotensin I to angiotensin
Il, a potent vasoconstrictor, which then increases the blood
pressure and afterload. Angiotensin II also stimulates the
release of aldosterone from the adrenal cortex, resulting in
sodium and fluid retention by the renal tubules and stimu-
lating the thirst center. This leads to the fluid volume over-
load commonly seen in HF. Angiotensin, aldosterone, and
other neurohormones (eg, endothelin, prostacyclin) lead to
an increase in preload and afterload, which increases stress
on the ventricular wall, causing an inc in the workload
of the heart. A counterregulatory mechanism is attempted
through the release of natriuretic peptides. Atrial natriuretic
peptide (ANP) and B-type natriuretic peptide (BNP) are re-
leased from the overdistended cardiac chambers, These sub-
stances promote vasodilation and diuresis. However, their
effect is usually not strong enough to overcome the negative
effects of the other mechanisms.
As the heart's wor increases, contractility of the myo-
ventricle aca os =diastol < blood volume in the
ieitased > Nursing Process
Assessment
The nursing assessment for the patient with HF fo-
cuses on observing for effectiveness of therapy and for
the patient’s ability to understand and implement self-
management strategies. Signs and symptoms of pul-
monary and systemic fluid overload are recorded and
reported immediately so that adjustments can be
made in therapy. The nurse also explores the patient’s
emotional response to the diagnosis of HF, a chronic
and often progressive condition.
| Health History
The health history focuses on the signs and symptoms
of HF, such as dyspnea,shortness of breath, and
cough. Sleep disturbances, particularly sleep suddenly
interrupted by shortness of breath, may be reported.
The nurse also asks about the number of pillows
needed for sleep (an indication of orthopnea), edema,
abdominal symptoms, altered mental status, activities
of daily living, and the activities that cause fatigue.
The nurse explores the patient's understanding of HF,
self-management strategies, and the desire to adhere
to those strategies. The nurse helps patients identify
the impact the illness has had on their quality of life
and successful coping skills that they have used.
Family and significant others are often included in
these discussions.
Physical Examination
The lungs are auscultated to detect crackles and
wheezes. Crackles, which are produced by the sudden
opening of edematous small airways and alveoli that
have adhered together by exudate, may be heard at the
end of inspiration and are not cleared with coughing.
Wheezing may also be heard in some patients. The
rate and depth of respirations are also documented.
The heart is auscultated for an S; heart sound,
a sign that the heart is beginning to fail and that
increased blood volume fills the ventricle with each
beat. HR and rhythm are also documented. When
the heart rate is rapid, the SV. decreases because the
ventricle has less time to fill. This in turn produces
increased pressure in the atria and eventually in the
pulmonary vascular bed.
" JVD is also assessed; distention greater than 3 cm
above the sternal angle is considered abnormal, This
is an estimate, not a precise measurement, of central
venous pressure.
Sensorium and level of consciousness must be eval-
uated. As the volume of blood ejected by the heart de-
creases, so does the amount of oxygen transported to
the brain.
The nurse assesses dependent parts of the patient's
body for perfusion and edema. With significant de-
creases in SV, there is a decrease in perfusion to the
periphery, causing the skin to feel cool and appear
pale or cyanotic. If the patient is sitting upright, the
feet and lower legs are examined for edema; if the
patient is supine in bed, the sacrum and back are also
assessed for edema. Fingers and hands may also be-
come edematous.
The liver is assessed for hepatojugular reflux. The
patient is asked to breathe normally while manual
pressure is applied over the right upper quadrant of
the abdomen for 30 to 60 seconds. If neck vein disten-
tion increases more than 1 cm, the finding is positive
for increased venous pressure.
If the patient is hospitalized, the nurse measures h
output carefully to establish a baseline against whic
to assess the effectiveness of diuretic therapy. Intake
and output records are rigorously maintained. It S
important to know whether the patient has ingen
more fluid than he or she has excreted (positive u
balance), which is then correlated with a gain a
weight. The patient must be monitored for oligu™
(diminished urine output, less than 400 mL/24 hours)
or anuria (urine output less than 50 mL/24 hours).
The patient is weighed daily in the hospital or at
home, at the same time of day, with the same type of
clothing, and on the same scale. If there is a signifi-
cant change in weight (ie, 2- to 3-Ib increase in a day
or 5-lb increase in a week), the patient is instructed
to notify the physician or to adjust the medications
(eg, increase the diuretic dose)
Diagnosis
Nursing Diagnoses
Based on the assessment data, major nursing diagnoses
for the patient with HF may include the following:
¢ Activity intolerance and fatigue related to imbal-
ance between oxygen supply and demand because
of decreased CO
* Excess fluid volume related to excess fluid or
sodium intake, and retention of fluid related to the
HF syndrome
* Anxiety related to breathlessness and restlessness
from inadequate oxygenation
* Powerlessness related to inability to perform role
responsibilities because of chronic illness and
hospitalizations
* Noncompliance related to lack of knowledge
Collaborative Problems,
Potential Complications
Based on the assessment data, potential complications
that may develop include the following:
* Cardiogenic shock (see also Chapter 15)
* Dysrhythmias (see Chapter 27)
* Thromboembolism (see Chapter 31)
* Pericardial effusion and cardiac tamponade (see
Chapter 29)
Planning and Goals
Major goals for the patient may include promoting ac-
tivity and reducing fatigue, relieving fluid overload
symptoms, decreasing the incidence of anxiety or in-
creasing the patient's ability to manage anxiety, en-
couraging the patient to verbalize his or her ability to
make decisions and influence outco
mes, and teaching
the patient about the self-care program.
Neosat 2
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Health Status ProblemDocument1 pageHealth Status ProblemKit Alizon BarredoNo ratings yet
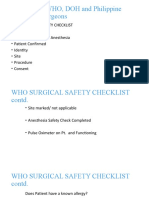
- Who Surgical Safety ChecklistDocument12 pagesWho Surgical Safety ChecklistKit Alizon BarredoNo ratings yet
- Conceptual Schemes (We Use The Terms InterDocument5 pagesConceptual Schemes (We Use The Terms InterKit Alizon BarredoNo ratings yet
- Oxygenation WorksheetDocument4 pagesOxygenation WorksheetKit Alizon Barredo100% (1)
- Postural DrainageDocument6 pagesPostural DrainageKit Alizon Barredo0% (1)
- FHP Guide QuestionsDocument1 pageFHP Guide QuestionsKit Alizon BarredoNo ratings yet
- Sleep and Activity PartialDocument1 pageSleep and Activity PartialKit Alizon BarredoNo ratings yet
- Clinical Objectives (Pediatrics)Document1 pageClinical Objectives (Pediatrics)Kit Alizon BarredoNo ratings yet
- Ethos-Customs, Habitual Usages, Conduct, and Character VisDocument2 pagesEthos-Customs, Habitual Usages, Conduct, and Character VisKit Alizon BarredoNo ratings yet
- Clinical Objectives (Pediatrics)Document1 pageClinical Objectives (Pediatrics)Kit Alizon BarredoNo ratings yet
- Ineffective Tissue Perfusion Related To Decrease Hemoglobin Concentration in The BloodDocument2 pagesIneffective Tissue Perfusion Related To Decrease Hemoglobin Concentration in The BloodKit Alizon BarredoNo ratings yet
- Clinical Objectives (Pediatrics)Document1 pageClinical Objectives (Pediatrics)Kit Alizon BarredoNo ratings yet