Professional Documents
Culture Documents
Servizi SRL
Uploaded by
Diogo SantosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Servizi SRL
Uploaded by
Diogo SantosCopyright:
Available Formats
ORIGINAL ARTICLE
Transfusion of ABO non-identical platelets does not influence the clinical
outcome of patients undergoing autologous haematopoietic stem cell
transplantation
Pilar Solves, Nelly Carpio, Aitana Balaguer, Samuel Romero, Gloria Iacoboni, Inés Gómez, Ignacio Lorenzo,
Federico Moscardó, Jaime Sanz, Francisca Lopez, Guillermo Martin, Isidro Jarque, Pau Montesinos,
Javier de la Rubia, Guillermo Sanz, Miguel A. Sanz
La Fe University Hospital, Valencia, Spain
Background. There are ABO antigens on the surface of platelets, but whether ABO compatible
platelets are necessary for transfusions is a matter of ongoing debate. We retrospectively reviewed the
ABO matching of platelet transfusions in a subset of patients undergoing autologous haematopoietic
progenitor cell transplantation during a 14-year period. Our aim was to analyse the characteristics
and outcomes of patients who received platelet transfusions that were or were not ABO identical.
l
Material and methods. We analysed 529 consecutive patients with various haematological and
Sr
non-haematological diseases who underwent 553 autologous progenitor stem cell transplants at the
University Hospital la Fe between January 2000 and December 2013. We retrospectively analysed
and compared transfusion and clinical outcomes of patients according to the ABO match of the
i
iz
platelet transfusions received. The period analysed was the time from transplantation until discharge.
Results. The patients received a total of 2,772 platelet concentrates, of which 2,053 (74.0%) were
v
ABO identical and 719 (26.0%) ABO non-identical; of these latter 309 were compatible and 410
incompatible with the patients' plasma. Considering all transplants, 36 (6.5%) did not require any
er
platelet transfusions, while in 246 (44.5%) cases, the patients were exclusively transfused with ABO
identical platelets and in 47 (8.5%) cases they received only ABO non-identical platelet transfusions.
S
The group of patients who received both ABO identical and ABO non-identical platelet transfusions
had higher transfusion needs and worse clinical outcomes compared to patients who received only
TI
ABO identical or ABO non-identical platelets.
Discussion. In our hospital, patients undergoing autologous haematopoietic stem cell transplanta-
M
tion who received ABO identical or ABO non-identical platelet transfusions had similar transfusion
and clinical outcomes. The isolated fact of receiving ABO non-identical platelets did not influence
morbidity or survival.
SI
Keywords: platelet transfusion, autologous haematopoietic stem cell transplantation, transfusion
outcome.
©
Introduction availability and better response in emergency situations,
Platelet transfusions are an important therapy for a avoiding wastage of platelets. However, some studies
large number of haemato-oncological diseases, but are have demonstrated higher post-transfusion platelet
also a valuable resource of limited availability and their increments after ABO identical platelet transfusions,
use should be optimised1. It has been demonstrated that supporting the practice of platelet matching5. The clinical
there are ABO antigens on the surface of platelets, but significance of the greater platelet increment has not
the need for ABO compatibility in platelet transfusions been elucidated6. In some reports, the transfusion of
remains a controversial issue and one that continues ABO-minor incompatible platelets has been associated
to be subject of debate2,3. A survey of a large number with acute haemolytic transfusion reactions due to the
of North American laboratories showed that 17% of exposure of recipients to ABO-incompatible plasma
transfusion services did not have a clear policy regarding containing anti-A or anti-B isoagglutinins7. In order to
the use of ABO non-identical platelets4. Although prevent this and other adverse effects, many transfusion
transfusion policy varies between centres, platelet centres suspend platelets in additive solutions that
transfusions are usually given across the ABO barrier. significantly reduce the quantity of plasma8. Despite
This strategy has some clear advantages, such as greater these considerations, there is little information about
Blood Transfus 2015; 13; 411-6 DOI 10.2450/2015.0195-14
© SIMTI Servizi Srl
411
All rights reserved - For personal use only
No other uses without permission
Solves P et al
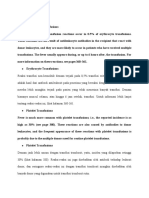
the relevance of ABO matching in platelet transfusions Table I - Characteristics of the patients divided according
in current clinical practise. to whether they received ABO identical platelet
transfusions, ABO non-identical platelets or both
We retrospectively reviewed the ABO matching of
ABO identical and ABO non-identical platelet
platelet transfusions in a subset of patients undergoing transfusions.
autologous haematopoietic progenitor cell transplantation Results are shown as mean±SD. Differences in
(APCT) during a 14-year period. Our objective was to variables between the ABO identical and ABO non-
identical groups are not statistically significant.
analyse the characteristics and outcomes of patients
who received platelet transfusions that were or were Characteristics Subsets of patients p
not ABO identical. who received platelets
ABO ABO non-
Both
Material and methods identical identical
Patients N. of patients/
238/246 45/47 246/260
transplants
We analysed 529 consecutive patients with various
Sex
haematological and non-haematological diseases who
Male/female 129/113 27/18 153/107 0.238
underwent 553 APCT in the period from January 2000
Age (years) 51.213.3 48.913.3 50.712.6 0.402
until December 2013 at the University Hospital la Fe.
N. of transplants
The patients' characteristics are shown in Table I. 1 234 45 241
2 8 2 14 0.503
l
Transfusion policy
Sr
ABO blood group 9
The policy regarding platelet transfusions in our O 99 6 5
centre followed the Standards developed by the Spanish A 129 21 119
B 7 13 25
Society of Blood Transfusion (SETS)9 and was based on
i
AB 3 5 7 <0.001
international guidelines. The policy can be summarised
as follows: (i) the threshold for prophylactic transfusion
v iz
Diagnosis
AML 13 3 56
was a pre-transfusion platelet count 10×109/L. If the Lymphoma 77 15 85
MM 99 19 66
patient had a fever 38.5 ºC, sepsis, mucositis grade
er
MS 16 1 7
2, uncontrolled high pressure, coagulopathy or acute Other* 33 6 32 <0.001
promyelocytic leukaemia, the threshold was increased
S
Positive indirect
4 2 7 0.518
to a pre-transfusion platelet count 20×109/L; (ii) the antiglobulin test
threshold for platelet transfusions with the aim of Days until
TI
controlling bleeding or increasing the platelet count neutrophils 12.94.8 13.22.4 14.59.6 0.006
>1×109/L
before an invasive procedure was <50×109/L. A standard
M
Days until
dose was considered to be one platelet concentrate, platelets* 17.315.6
19.6
23.320.4 <0.001
composed of platelets pooled from various buffy coats. 22.8
>20×109/L
Platelets for buffy coats were prepared from four to
SI
Fever up to 30
five donors per unit and suspended in platelet additive days after APCT
solution making up to two-thirds of the final volume10,11. Yes 60 9 50
No 161 33 179 0.117
Red blood cells were transfused if haemoglobin levels
©
Days in hospital 26.36.7 26.75.7 31.514.7 <0.001
were <80 g/dL. All blood components were leucocyte-
reduced and irradiated with 25 Gray. In our Institution, Follow-up (days) 1,071.4 1,662.1 1,006.9
0.059
1,176.3 1,673.7 1,174.2
ABO non-identical platelets can be transfused if ABO
Status 90 days
identical products are not available. after APCT
ABO and Rh typing and the indirect antiglobulin Death 7 0 23
test were performed in the automated system ORTHO Alive 219 47 215 0.003
Autovue Innova (Ortho Clinical Diagnostics, Inc., AML: acute myeloid leukaemia, MM: multiple myeloma, MS: multiple
sclerosis. *: acute lymphoblastic leukaemia, aplastic anaemia, chronic
Raritan, NJ, USA). The specificity of sera of patients myeloid leukaemia, myelodysplastic syndrome. APCT: autologous
with positive tests was investigated using panels of haematopoietic progenitor cell transplantation.
red blood cells with known antigens (Ortho Clinical
Diagnostics Inc.; Bio-Rad GmbH, Cressier-sur-Morat, ABO non-identical. The period analysed was the time
Switzerland; Sanquin, Amsterdam, The Netherlands). from transplantation until discharge.
We retrospectively analysed and compared transfusion
and clinical outcomes of patients according to the ABO Statistics
match of the platelet transfusions administered: ABO Computer software (SPSS, release 13.0, IBM
identical, ABO non-identical, or both ABO identical and Corporation, Armonk, NY, USA) was used to perform
Blood Transfus 2015; 13; 411-6 DOI 10.2450/2015.0195-14
412
All rights reserved - For personal use only
No other uses without permission
ABO-matched platelets in autologous stem cell transplantation
the statistical analyses. Descriptive statistics are Table II - Transfusion outcome of patients who received
presented for variables. Results are expressed as mean only ABO identical, only ABO non-identical
and both ABO identical and ABO non-identical
± standard deviation (SD) or median and range for
platelet transfusions. Results are shown as
continuous variables and as numbers with percentages median and range.
for categorical variables. The Kolmogorov-Smirnov test
Patients who received p
was employed to investigate the normality distribution platelet transfusions
of the variables. Categorical variables were compared ABO ABO non- Both
by means of the chi square test or Fisher's exact test. identical identical
The Mann-Whitney U-test and Kruskall-Wallis test Number 246 47 260
for continuous variables were used to compare the Red blood cells 2 (0-10) 2 (0-10) 4 (0-35)
groups when applicable. Variables that were statistically ABO identical
significant in the univariate models were included in a 2 (1-8) 3 (1-63) <0.001
platelets
stepwise binary logistic regression model to assess the ABO non-identical
1 (0-9) 1 (1-20)
risk of receiving ABO non-identical platelet transfusions. platelets
Univariate odds ratios (OR) and corresponding 95% Plasma compatible 0 (0-4) 1 (0-15)
confidence intervals (CI) were calculated. A survival Plasma incompatible 1 (0-9) 1 (0-17)
analysis was performed using the Kaplan-Meier method Total platelets 2 (0-10) 1 (0-9) 4 (1-86) <0.001
and compared with the log-rank test.
l
Fresh frozen plasma 0 (0-0) 0 (0-0) 0 (0-73) 0.010
Sr
Results
Table I shows the patients' characteristics according days after APCT), received more units of red blood cells
to whether they received ABO identical, ABO non- (5.24.5 vs 3.14.1 units), more ABO non-identical
i
identical or both types of platelet transfusions. As regards
ABO blood group, 200 patients (37.8%) were O, 269
v iz
platelet units (2.32.5 vs 1.01.9 units), a higher number
of overall platelet transfusions (8.99.0 vs 4.06.8 units)
(50.8 %) were A, 45 (8.5 %) were B and 15 (2.8 %) were and stayed longer in hospital (32.910.5 vs 28.111.1
AB. Patients who underwent APCT received a median days) than patients with other diagnoses (p<0.001 for
er
of two (range, 0-35) red blood cell concentrates and all variables). In the subset of patients with leukaemia,
three (range, 0-86) platelet concentrates, of which two there was no statistical difference in survival between
S
(range, 0-63) were ABO identical and one (range, 0-20) patients who did or did not receive ABO non-identical
was ABO non-identical. The patients received a total of platelets (p=0.364).
TI
2,772 platelet concentrates, of which 2,053 (74.0%) were Figure 1 illustrates the cumulative survival to 90 days
ABO identical and 719 not ABO identical (26.0%); 309 after APCT of all patients according to whether they
M
were compatible and 410 incompatible with the patients' received only ABO identical, only ABO non-identical
plasma. Considering all transplants, in 36 cases (6.5%) or both types of platelet transfusions.
no platelet transfusions were given, while in 246 cases Table III shows the clinical and transfusion outcomes
SI
(44.5%) the patients were exclusively transfused with of patients receiving three platelet transfusions, according
ABO identical platelets and in 47 cases (8.5%) received to whether they did or did not receive ABO identical
only ABO non-identical platelet transfusions. In the platelet transfusions. We performed this analysis to
©
241 (43.6%) transplants for which patients received circumvent the problem that patients with higher
both ABO identical and ABO non-identical platelets, transfusion requirements may be disproportionately
in 154 cases the patients received more ABO identical represented in the group of ABO non-identical recipients.
platelets, in 26 cases they received more ABO non- Results of the multivariate analysis showed that
identical platelets, and in 61 cases they received the a diagnosis of acute myeloid leukaemia was the only
same number of ABO identical and ABO non-identical variable that significantly increased the risk of receiving
platelet transfusions. Table II shows the blood product ABO non-identical platelet transfusions (Table IV).
requirements and clinical outcomes of patients according Among 112 patients who were RhD negative, 66
to whether they received ABO identical, ABO non- received RhD positive platelet transfusions (median
identical or both types of platelet transfusions. The 3; range, 1-25). One patient developed anti-D + anti-E
group of patients who received both ABO identical 10 months after one RhD positive platelet transfusion,
and ABO non-identical platelet transfusions had higher and another patient developed anti-D 30 days after
transfusion needs and worse clinical outcomes compared transfusion of 16 RhD positive platelet concentrates.
to patients who received only ABO identical or ABO The former patient received ABO identical platelet
non-identical platelets. Patients with acute leukaemia transfusions while the latter received ABO non-identical
had later platelet engraftment (36.432.0 vs 18.834.5 platelets.
Blood Transfus 2015; 13; 411-6 DOI 10.2450/2015.0195-14
413
All rights reserved - For personal use only
No other uses without permission
Solves P et al
Cumulative survival
l
i Sr
v iz
Days after transplant
er
Figure 1 - Cumulative survival 90 days after APCT of all patients according to whether they received
S
only ABO identical platelets, only ABO non-identical platelets or both ABO identical and
ABO non-identical platelets.
p=0.03 (p=0.255 between the ABO identical platelet and ABO non-identical platelet curves).
TI
PLTs: platelets.
M
Another three patients developed anti-erythrocyte patients undergoing APCT who did or did not receive
antibodies (2 anti-E, 1 anti-Kpa); all three had received ABO identical platelets.
mostly ABO-identical platelets (p=0.318). It seems reasonable that transfusion of ABO identical
SI
Among the recipients of ABO identical platelets, platelets should be a goal to reach in blood banks, but
three had allergic reactions, while there were seven the application of this strict policy in clinical practice
adverse reactions in the group of patients receiving is difficult because of the limited availability of platelet
©
ABO identical plus ABO non-identical platelets (4 concentrates, especially in emergency circumstances.
allergic reactions, 2 febrile non-haemolytic reactions In spite of this, some groups have shown that it can be
and 1 case of hypotension, p=0.139). In five cases, feasible to transfuse only ABO identical platelets by
adverse reactions occurred after ABO identical platelet changing ordering and inventorying procedures, with a
transfusions, and in another five cases after ABO non- minimum increase in wastage14. In fact, following our
identical platelet transfusions. centre's transfusion policy most platelet transfusions
performed in our patients were also ABO identical.
Discussion However, the largest group of patients received
ABO non-identical platelet transfusions have been both ABO identical and ABO non-identical platelet
associated with different adverse effects such as immune transfusions. This group comprised patients who
complex formation, platelet refractoriness and adverse engrafted neutrophils and platelets later, received more
clinical outcomes12. Results of some studies comparing red blood cell and total platelet transfusions, and stayed
ABO identical and ABO non-identical platelet longer in hospital than patients who received only ABO
transfusions in adult and childhood populations are identical or only ABO non-identical platelets. This
controversial4,13. Our study provides information about probably means that patients who receive ABO non-
clinical and transfusion outcomes of a large subset of identical platelets are a selected population with greater
Blood Transfus 2015; 13; 411-6 DOI 10.2450/2015.0195-14
414
All rights reserved - For personal use only
No other uses without permission
ABO-matched platelets in autologous stem cell transplantation
Table III - Clinical and transfusion outcomes of patients patients with different clinical conditions. However, the
who received three platelet transfusions, number of patients who received ABO non-identical
according to whether they received only ABO
platelets was sufficiently large for comparison with
identical or both identical ABO and non-identical
ABO platelet transfusions. Results are shown as the group of patients who received only ABO identical
mean ± standard deviation. platelets.
Characteristics Patients who received p Some literature data suggest that ABO non-
platelet transfusions identical platelet transfusions may contribute to
Only ABO Both allergic and febrile reactions and also increase the red
identical cell immunisation rate12. Our results, however, are in
Number 43 45 concordance with those of another study which failed
Sex to show these associations17. Considering the number
23/20 28/17 0.407
(male/female) of platelet transfusions received in each group of
Age (years) 53.611.5 48.913.6 0.102 patients, there was no difference in the incidence of
Days until neutrophils
12.51.8 13.53.0 0.111
adverse reactions to platelets in patients who did or did
>1×109/L not receive ABO non-identical platelets. Consistently
Days until platelets
17.611.1 16.06.7 0.611 with this fact, the RBC alloimmunisation rate was not
>20×109/L
statistically different between the groups in our study.
RBC transfusions 2.42.0 2.32.0 0.734 There are controversial data about an association of
l
ABO identical platelets 3.00.0 1.70.6 <0.001 ABO-mismatched platelet transfusions with morbidity
Sr
ABO non-identical
0 1.30.6 <0.001 and mortality5,18-23. In 153 patients undergoing cardiac
platelets
surgery, recipients of ABO identical platelets had a lower
Fever* mortality rate, fewer red blood cell transfusions, fewer
i
Yes 10 12 iz
No 23 33 0.817 mean days of antibiotics and a shorter stay in hospital19.
Days at hospital 28.09.3 26.07.6 0.062
In adult patients with leukaemia, a possible survival
v
advantage has been reported for those who receive ABO
Status 90 days after
identical platelet transfusions, without this having a
er
APCT
Death 1 0 clear explanation18. In the present study, red blood cell
Alive 42 45 0.314 and platelet requirements, hospital stay and mortality
S
RBC: red blood cells; *: fever in the first 30 days after transplantation; were similar in patients who received ABO identical
APCT: autologous haematopoietic progenitor cell transplantation.
or ABO non-identical platelet transfusions. Our results
TI
agree with those published by Lin et al.20, showing
transfusion requirements that cannot be met only by similar transfusions and clinical outcomes for a large
M
ABO identical platelets. In fact, these patients shared subset of patients undergoing cardiovascular surgery
some characteristics that justified greater transfusion
requirements, such as late neutrophil and platelet
SI
Table IV - Variables influencing the risk of receiving ABO
engraftment. This conclusion is also supported by the non-identical platelet transfusions: results of
analysis of patients who received the same number of multivariate analysis.
platelet transfusions. In this occasion, we failed to find
©
Variable OR 95% CI p
any difference in engraftment, time spent in hospital or
Age 0.997 0.981-1.013 0.703
survival between patients who did or who did not receive
Sex 1.318 0.844-2.060 0.225
ABO identical platelets.
ABO group O 0.332 0.7061-1.804 0.201
However, it cannot be excluded that ABO non-
identical platelet transfusions contribute to a worse ABO group A 0.382 0.071-2.049 0.261
outcome. The doubt also remains that the lower ABO group B 2.352 0.343-16.133 0.384
post-transfusion increments after ABO non-identical Diagnosis (AML) 3.879 1.555-9.672 0.004
platelet transfusions, observed previously15,16, may Days until platelets
1.008 0.991-1.025 0.345
have contributed to increase the number of total platelet >20×109/L
transfusions in the group of patients who received ABO Days until neutrophils
1.045 0.980-1.114 0.184
non-identical platelets. Unfortunately, we are unable >1×109/L
to demonstrate whether this was the case because we Fever* 1.062 0.658-1.716 0.805
did not systematically determine the corrected count N. of transplants (2) 1.654 0.546-5.008 0.373
increment after platelet transfusions.
OR: odds ratio; CI: confidence interval; AML: acute myeloid leukaemia.
We are well aware of the limitations of this analysis: Fever*: fever up to 30 days after autologous haematopoietic stem cell
this was a retrospective study of a large subset of transplantation.
Blood Transfus 2015; 13; 411-6 DOI 10.2450/2015.0195-14
415
All rights reserved - For personal use only
No other uses without permission
Solves P et al
and transfused with ABO identical platelets or ABO 11) Surowiecka M, Zantek N, Morgan S, et al. Anti-A and anti-B
mismatched platelets. However, their data have been titers in group O platelet units are reduced in PAS C versus
convencional plasma units. Transfusion 2014; 54: 255-6.
questioned because all group O platelet transfusions had 12) Kaufman RM. Platelet ABO matters. Transfusion 2009; 49: 5-7.
an anti-A or anti-B titre of 1 in 32 or less21. Exposure of 13) Julmy F, Ammann RA, Taleghani BM, et al. Transfusion
ABO antigen platelets to high titres of anti-A or anti-B efficacy of ABO major-mismatched platelets (PLTs) in
has been associated with alterations of platelet function children is inferior to that of ABO-identical PLTs. Transfusion
2009; 49: 21-33.
and clot formation kinetics24. In contrast, we do not 14) Henrichs KF, Howk N, Masel DS, et al. Providing ABO
have the titres of anti-A or anti-B in group O platelet identical platelets and cryoprecipitate to (almost) all patients
concentrates, so our results are more consistent than - approach, logistics and associated decreases in transfusion
those of the study by Lin et al.20 reaction and red cell alloimmunization incidence. Transfusion
2012; 52: 635-40.
15) Klumpp TR, Herman JH, Innis S, et al. Factors associated
Conclusion with response to platelet transfusion following hematopoietic
In our hospital, patients undergoing APCT who stem cell transplantation. Bone Marrow Transplant 1996; 17:
received ABO identical or ABO non-identical platelet 1035-41.
16) Triulzi DJ, Assmann SF, Strauss RG, et al. The impact
transfusions had similar transfusion and clinical of platelet transfusion characteristics on posttransfusion
outcomes. The isolated fact of receiving ABO non- platelet increment and clinical bleeding in patients with
identical platelet did not influence morbidity or survival. hypoproliferative thrombocytopenia. Blood 2012; 119:
Prospective studies are needed in order to confirm our 5553-62.
l
17) Yazer MH, Raval JS, Triulzi DJ, Blumberg N. ABO-
results and clarify whether a strategy of ABO identical
Sr
mismatched transfusions are not over-represented in febrile
platelet transfusions could reduce platelet transfusion non-haemolytic transfusion reactions to platelets. Vox Sang
requirements. 2012; 102: 175-7.
18) Heal JM, Kenmotsu N, Rowe JM, Blumberg N. A possible
i
izsurvival advantage in adults with acute leukemia receiving
Authorship contributions ABO-identical platelet transfusions. Am J Hematol 1994;
PS and NC participated in the study design, data 45: 189-90.
v
collection, data analysis and paper writing. AB, SR and 19) Heal JM, Rowe JM, McMican A, et al. The role of ABO matching
GI participated in data collection. IL participated in data in platelet transfusion. Eur J Haematol 1993; 50: 110-7.
er
20) Blumberg N, Heal JM, Hicks GL, Risher WH. Association
analysis. The rest of the Authors participated in writing of ABO-mismatched platelet transfusions with morbidity and
and critically reviewing the paper.
S
mortality in cardiac surgery. Transfusion 2001; 41: 790-3.
21) Lin Y, Callum JL, Coovadia AS, Murphy PM. Transfusion
The Authors declare no conflicts of interest. of ABO non-identical platelets is not associated with
TI
adverse clinical outcomes in cardiovascular surgery patients.
Transfusion 2002; 42: 166-72.
References 22) Blumberg N, Heal JM. ABO-mismatched platelet transfusions
M
1) Cid J, Harm SK, Yazer MH. Platelet transfusion: the art and science and clinical outcomes after cardiac surgery. Transfusion 2002;
of compromise. Transfus Med Hemother 2013; 40: 160-71. 42: 1527-8.
2) Cooling LL, Kelly K, Barton J, et al. Determinants of ABH 23) Refaai MA, Fialkow LB, Heal JM, et al. An association of
SI
expression on human blood platelets. Blood 2005; 15: 3356-64. ABO non-identical platelet and cryoprecipitate transfusions
3) Curtis BR, Edwards JT, Hessner MJ, et al. Blood group A with altered red cell transfusion needs in surgical patients. Vox
and B antigens are strongly expressed on platelets of some Sang 2011; 101: 55-60.
individuals. Blood 2000; 15: 1574-81. 24) Refaai MA, Carter J, Henrichs KF, et al. Alterations of platelet
©
4) Lozano M, Heddle N, Williamson LM, et al. Practices function and clot formation kinetics after in vitro exposure to
associated with ABO-incompatible platelets transfusions: a anti-A and -B. Transfusion 2013; 53: 382-93.
BEST collaborative international survey. Transfusion 2010;
50: 1743-8.
5) Shehata N, Tinmouth A, Naglie G, et al. ABO-identical
versus nonidentical platelet transfusion: a systematic review.
Transfusion 2009; 49: 2442-53.
6) Dunbar NM, Ornstein DL, Dumont L. ABO incompatible
platelets: risks versus benefits. Curr Opin Hematol 2012;
19: 475-9.
7) Cooling L. ABO and platelet transfusion therapy.
Immunohematology 2007; 23: 20-33.
8) Kacker S, Ness PM, Savage WJ, et al. The cost-effectiveness
of platelet additive solution to prevent allergic transfusion
reactions. Transfusion 2013; 53: 2609-19.
9) Sociedad Española de Transfusión Sanguínea y Terapia Arrived: 4 August 2014 - Revision accepted: 11 November 2014
Celular. Guía sobre la transfusión de componentes sanguíneos Correspondence: Pilar Solves
y derivados plasmáticos. Barcelona: SETS; 2010. Blood Bank
10) Larsson S, Sandgren P, Sjodin A, et al. Automated preparation Hospital Universitari I Politècnic La Fe
of platelet concentrates from pooled buffy coats: in vitro Bulevar del Sur
studies and experiences with the OrbiSac system. Transfusion Valencia 46026, Spain
e-mail: solves_pil@gva.es
2005; 45: 743-51.
Blood Transfus 2015; 13; 411-6 DOI 10.2450/2015.0195-14
416
All rights reserved - For personal use only
No other uses without permission
You might also like
- ABO Incompatible Platelets: Risks Versus Benefit: ReviewDocument5 pagesABO Incompatible Platelets: Risks Versus Benefit: Reviewmy accountNo ratings yet
- Mak Roo 2018Document7 pagesMak Roo 2018my accountNo ratings yet
- Ijhoscr: ABO Blood Grouping Mismatch in Hematopoietic Stem Cell Transplantation and Clinical GuidesDocument7 pagesIjhoscr: ABO Blood Grouping Mismatch in Hematopoietic Stem Cell Transplantation and Clinical GuidesMohana ReddyNo ratings yet
- SMLLDocument8 pagesSMLLArifa Al HusnahNo ratings yet
- The Critical Role of Plasmapheresis in ABO-incompatible Renal Transplantation.Document8 pagesThe Critical Role of Plasmapheresis in ABO-incompatible Renal Transplantation.Pritha BhuwapaksophonNo ratings yet
- Originalresearch: ABO-incompatible Platelets Are Associated With Increased Transfusion Reaction RatesDocument9 pagesOriginalresearch: ABO-incompatible Platelets Are Associated With Increased Transfusion Reaction Ratesmy accountNo ratings yet
- Pretransfusion or Compatibility Testing: NotesDocument7 pagesPretransfusion or Compatibility Testing: NotesABHINABA GUPTANo ratings yet
- Current Trends in Platelet Transfusions Practice - The Role of ABO-RhD and Human Leukocyte Antigen IncompatibilityDocument13 pagesCurrent Trends in Platelet Transfusions Practice - The Role of ABO-RhD and Human Leukocyte Antigen IncompatibilityRoberto GutierrezNo ratings yet
- Bahrain Medical Bulletin, Vol. 31, No. 4, December 2009Document6 pagesBahrain Medical Bulletin, Vol. 31, No. 4, December 2009Super StarNo ratings yet
- Continuing Education Activity: ABO Blood Group SystemDocument5 pagesContinuing Education Activity: ABO Blood Group SystemIhsanul Ma'arifNo ratings yet
- Compatibility Testing: Section 13Document19 pagesCompatibility Testing: Section 13Gretchel PontilarNo ratings yet
- Abo Incompatible Stem Cell Transplant - Laboratory Side BDocument28 pagesAbo Incompatible Stem Cell Transplant - Laboratory Side BAlita PalpialyNo ratings yet
- Review: ABO-identical Versus Nonidentical Platelet Transfusion: A Systematic ReviewDocument12 pagesReview: ABO-identical Versus Nonidentical Platelet Transfusion: A Systematic Reviewmy accountNo ratings yet
- Transfusion and Apheresis ScienceDocument6 pagesTransfusion and Apheresis Sciencemy accountNo ratings yet
- Transfusion of ABO-mismatched Platelets Leads To Early Platelet RefractorinessDocument6 pagesTransfusion of ABO-mismatched Platelets Leads To Early Platelet Refractorinessmy accountNo ratings yet
- Abo Incompatible Stem Cell Transplant - Laboratory Side BDocument28 pagesAbo Incompatible Stem Cell Transplant - Laboratory Side BAlita PalpialyNo ratings yet
- Gene Frequencies of Haemoglobin Genotype, ABO and Rhesus Blood Groups Among Students Population of A Private University in Nigeria-Implications For Blood BankingDocument7 pagesGene Frequencies of Haemoglobin Genotype, ABO and Rhesus Blood Groups Among Students Population of A Private University in Nigeria-Implications For Blood BankingSSR-IIJLS JournalNo ratings yet
- Platelet Transfusion - ABO Matching - Hem2020000135cDocument6 pagesPlatelet Transfusion - ABO Matching - Hem2020000135cJck YyNo ratings yet
- Does ABO and RHD Matching Matter For PlateletDocument6 pagesDoes ABO and RHD Matching Matter For Plateletشريف عبد المنعمNo ratings yet
- Singer-Alloimmunization and Erythrocyte Autoimmunization in Transfusion-DependentDocument5 pagesSinger-Alloimmunization and Erythrocyte Autoimmunization in Transfusion-DependentFatimatuzzahra ShahabNo ratings yet
- ABO-Mismatched Allogeneic Hematopoietic Stem Cell TransplantationDocument10 pagesABO-Mismatched Allogeneic Hematopoietic Stem Cell TransplantationMohana ReddyNo ratings yet
- (Dr. Teguh) 2021 TT Transf Lab Problem in Haema MalignancyDocument26 pages(Dr. Teguh) 2021 TT Transf Lab Problem in Haema MalignancyAmanda Sonia ArliestaNo ratings yet
- Antibody Titers Study in Group o Blood Donors Tube and Column Agglutination Techniques JTCOA 1000104Document6 pagesAntibody Titers Study in Group o Blood Donors Tube and Column Agglutination Techniques JTCOA 1000104DesiWidyaSariNo ratings yet
- Best Practices of Apheresis in Hematopoietic Cell TransplantationFrom EverandBest Practices of Apheresis in Hematopoietic Cell TransplantationSyed A. AbutalibNo ratings yet
- Red Cell Alloimmunization in A Transfused Patient Population A Study From A Tertiary Care Hospital in North IndiaDocument7 pagesRed Cell Alloimmunization in A Transfused Patient Population A Study From A Tertiary Care Hospital in North Indialutfi rinaldiNo ratings yet
- American J Transplantation - 2005 - Ackerman - Attitudes of Minority Patients With End Stage Renal Disease RegardingDocument6 pagesAmerican J Transplantation - 2005 - Ackerman - Attitudes of Minority Patients With End Stage Renal Disease RegardingsyamsaNo ratings yet
- IndianJNephrol32182-3307103 091111Document5 pagesIndianJNephrol32182-3307103 091111NUTS SAARCNo ratings yet
- BB - Lecture 9Document4 pagesBB - Lecture 9Claudette Jane SoNo ratings yet
- Lab - ABO - Does ABO and RHD Matching Matter For PlateletDocument6 pagesLab - ABO - Does ABO and RHD Matching Matter For PlateletManuel VelasquezNo ratings yet
- NP 08002Document4 pagesNP 08002Samehada SamaNo ratings yet
- ABO SUBTYPESpdfDocument2 pagesABO SUBTYPESpdfShawee GomezNo ratings yet
- Nej Mo A 1511812Document10 pagesNej Mo A 1511812anggiNo ratings yet
- Blood TypingDocument3 pagesBlood TypingNoriz Ember DominguezNo ratings yet
- Compatibility Testing: Dr. Mohammed H Saiem Aldahr Blood Bank 3 Medical TechnologyDocument44 pagesCompatibility Testing: Dr. Mohammed H Saiem Aldahr Blood Bank 3 Medical TechnologyAnne Lorraine Margarette DulayNo ratings yet
- Atvbaha 119 313658Document10 pagesAtvbaha 119 313658Sumeet TripathiNo ratings yet
- Shiwei Yang, Xiaoli Yuan, Rongjun Ma, Li Jiang, Jianmin Guo, Yuzhu Zang, Jie Shi, Jing Yang, Pingchong Lei, Zhongwen Liu, Yin Zhang, Zunmin ZhuDocument6 pagesShiwei Yang, Xiaoli Yuan, Rongjun Ma, Li Jiang, Jianmin Guo, Yuzhu Zang, Jie Shi, Jing Yang, Pingchong Lei, Zhongwen Liu, Yin Zhang, Zunmin ZhuAbdurrahman HasanuddinNo ratings yet
- Change of Hemoglobin and Albumin Serum Levels Before and After Caesarean SectionDocument4 pagesChange of Hemoglobin and Albumin Serum Levels Before and After Caesarean Sectionriri hardiantyNo ratings yet
- اسباب تغير فصائل الدمDocument1 pageاسباب تغير فصائل الدمأحمد عبدالرزاق الهمدانيNo ratings yet
- Ltoe 1Document2 pagesLtoe 1lexdei88No ratings yet
- Journal Pone 0251576Document16 pagesJournal Pone 0251576chidera nwekeNo ratings yet
- JIPMER Residents ManualDocument68 pagesJIPMER Residents ManualSaroj PandaNo ratings yet
- Haemostatic Abnormalities in Patients With Cirrhosis and Their Relation With Severity of Liver Dysfunction As Assessed by Child Pugh ScoreDocument6 pagesHaemostatic Abnormalities in Patients With Cirrhosis and Their Relation With Severity of Liver Dysfunction As Assessed by Child Pugh ScoreWahyu PerdakaNo ratings yet
- Predictors of Blood Loss During Orthognathic Surgery and The Need For Pre-Deposit Autologous Blood DonationDocument4 pagesPredictors of Blood Loss During Orthognathic Surgery and The Need For Pre-Deposit Autologous Blood DonationCaio GonçalvesNo ratings yet
- Medical Uses: Blood DonationDocument4 pagesMedical Uses: Blood DonationHerryanto SimanjuntakNo ratings yet
- Briggs2006 PDFDocument10 pagesBriggs2006 PDFRonal WinterNo ratings yet
- Blood Group SystemDocument33 pagesBlood Group SystemAJETUNMOBI IBRAHEEM AYODEJINo ratings yet
- Blood Transfusion PocedureDocument9 pagesBlood Transfusion PocedureRaman Samrao100% (1)
- RI, Hema&immnoDocument9 pagesRI, Hema&immnoHabtamu WondifrawNo ratings yet
- Piro Poi Quilo Cito Sis ArticuloDocument6 pagesPiro Poi Quilo Cito Sis ArticuloLaura HernandezNo ratings yet
- Abibakar Sheikaden Ismail 2019Document5 pagesAbibakar Sheikaden Ismail 2019Shafici CqadirNo ratings yet
- B Blab 6 Crossmatch SP 05Document14 pagesB Blab 6 Crossmatch SP 05Rutchelle Joyce PugoyNo ratings yet
- Shunkwiler Et Al-2017-Journal of Clinical ApheresisDocument10 pagesShunkwiler Et Al-2017-Journal of Clinical ApheresisVenkata Sreekanth SampathNo ratings yet
- Transfusion of Apheresis Platelets and Abo Groups 2005Document15 pagesTransfusion of Apheresis Platelets and Abo Groups 2005my accountNo ratings yet
- Pgina WebDocument9 pagesPgina WebLAYLA ANDREA CARRERA SALGUERONo ratings yet
- Cross-Match-Compatible Platelets Improve CorrectedDocument7 pagesCross-Match-Compatible Platelets Improve CorrectedKatherinne Alexandra Escárraga CorrealNo ratings yet
- BCR-ABL in ALLDocument12 pagesBCR-ABL in ALLLuana MNo ratings yet
- 1.5 Platelet Antibodies in Immune Thrombocytopenic Purpura and OnyalaiDocument4 pages1.5 Platelet Antibodies in Immune Thrombocytopenic Purpura and OnyalaianiminaminaNo ratings yet
- 血清学鉴定与基因检测互补验证ABO 疑难血型的应用探讨1Document5 pages血清学鉴定与基因检测互补验证ABO 疑难血型的应用探讨1kmbloodlzNo ratings yet
- Blood GroupingDocument27 pagesBlood Groupingcontact.elsen31No ratings yet
- 4694-PDF Galley-26743-2-10-20200702Document5 pages4694-PDF Galley-26743-2-10-20200702Sami UllahNo ratings yet
- BSMT ReviewerDocument3 pagesBSMT ReviewerLyudmyla GillegoNo ratings yet
- List of Culture Media Used in Microbiology With Their Uses - MicrobiologyDocument14 pagesList of Culture Media Used in Microbiology With Their Uses - MicrobiologyRatan YadavNo ratings yet
- Isolation PrecautionsDocument14 pagesIsolation PrecautionsEm CastilloNo ratings yet
- Seminar 1 - South - Assessment Examination - BacteriologyDocument12 pagesSeminar 1 - South - Assessment Examination - BacteriologyDevinViscarsNo ratings yet
- 5 GRAM-Positive - Cocci - Staphylococci 5 GRAM - Positive - Cocci - StaphylococciDocument5 pages5 GRAM-Positive - Cocci - Staphylococci 5 GRAM - Positive - Cocci - StaphylococciJoseline SorianoNo ratings yet
- Labreport V SMSH 23 21296371 PDFDocument2 pagesLabreport V SMSH 23 21296371 PDFPurnima Swami (Lecturer & Promoter)No ratings yet
- BIO 315 Final 2012Document12 pagesBIO 315 Final 2012Dahee LeeNo ratings yet
- Blood Service Facility OrdinanceDocument7 pagesBlood Service Facility OrdinanceJerome ProfetanaNo ratings yet
- Blood Transfusion - Marino - The Icu BookDocument3 pagesBlood Transfusion - Marino - The Icu BookWilliam OmarNo ratings yet
- 292710Document2 pages292710Drashua AshuaNo ratings yet
- Urine Culture: D.M.M. LabDocument15 pagesUrine Culture: D.M.M. LabTomi RahmadaniNo ratings yet
- 1522-1588 USMLE QuestionsDocument67 pages1522-1588 USMLE QuestionsKiran KrupaNo ratings yet
- Common NamesDocument1 pageCommon NamesPau ZaballeroNo ratings yet
- Blood - BLD 2022 016558 C MainDocument12 pagesBlood - BLD 2022 016558 C MaincnshematologiaNo ratings yet
- Sputum Culture TestDocument5 pagesSputum Culture TestpraveenASPNo ratings yet
- 04 MalasseziaDocument7 pages04 MalasseziaResty Agiastuty Eka PutriNo ratings yet
- Clinical Examination - A Systematic Guide To Physical Diagnosis, 7th Ed (PDF) (Tahir99) VRG - pdf1259358830Document55 pagesClinical Examination - A Systematic Guide To Physical Diagnosis, 7th Ed (PDF) (Tahir99) VRG - pdf1259358830Anonymous 5CdXo6j0nNo ratings yet
- Blood Bank 4 DiscpDocument20 pagesBlood Bank 4 DiscpHector de la CruzNo ratings yet
- Antihuman Globulin Testing - BOOKDocument12 pagesAntihuman Globulin Testing - BOOKANNE CZARINA RAMIELLE DE VILLANo ratings yet
- Cultural Characteristics of BacteriaDocument5 pagesCultural Characteristics of Bacteriacamz0460% (5)
- Soal UasDocument10 pagesSoal UasDila ZeinNo ratings yet
- Anaerobic Blood Culture Bottle IFU en July 18, 2012Document3 pagesAnaerobic Blood Culture Bottle IFU en July 18, 2012Hadi AlbitarNo ratings yet
- Typhoid FeverDocument30 pagesTyphoid FeversakuarNo ratings yet
- Spec FarmaDocument8 pagesSpec FarmaМилан ЂурђевићNo ratings yet
- Mls Imls Reading ListDocument3 pagesMls Imls Reading ListPeng KwanNo ratings yet
- Almustaqbal University Collage Department Semester Exam./ 1 Attempt Sample: Subject: Human Biology Code: Max. Time: 2 H. Class: First DateDocument3 pagesAlmustaqbal University Collage Department Semester Exam./ 1 Attempt Sample: Subject: Human Biology Code: Max. Time: 2 H. Class: First DateZainab HasanNo ratings yet
- Oxford - Blood CultureDocument8 pagesOxford - Blood CultureKhoa Vi Sinh BVCRNo ratings yet
- JBLMGH Rates For Laboratory Services: Jose B. Lingad Memorial General HospitalDocument4 pagesJBLMGH Rates For Laboratory Services: Jose B. Lingad Memorial General HospitalApril NNo ratings yet
- VirologyLearnTable 2017-Sketchy PDFDocument4 pagesVirologyLearnTable 2017-Sketchy PDFdfgbdfgNo ratings yet
- Shigella, ShigellosisDocument52 pagesShigella, Shigellosistummalapalli venkateswara raoNo ratings yet